Abstract
Obesity is a risk factor for sepsis morbidity and mortality, whereas the hypothalamic–pituitary–adrenal (HPA) axis plays a protective role in the body's defence against sepsis. Sepsis induces a profound systemic immune response and cytokines serve as excellent markers for sepsis as they act as mediators of the immune response. Evidence suggests that the adipokine leptin may play a pathogenic role in sepsis. Mouse endotoxaemic models present with elevated leptin levels and exogenously added leptin increased mortality whereas human septic patients have elevated circulating levels of the soluble leptin receptor (Ob-Re). Evidence suggests that leptin can inhibit the regulation of the HPA axis. Thus, leptin may suppress the HPA axis, impairing its protective role in sepsis. We hypothesised that leptin would attenuate the HPA axis response to sepsis. We investigated the direct effects of an i.p. injection of 2 mg/kg leptin on the HPA axis response to intraperitoneally injected 25 μg/kg lipopolysaccharide (LPS) in the male Wistar rat. We found that LPS potently activated the HPA axis, as shown by significantly increased plasma stress hormones, ACTH and corticosterone, and increased plasma interleukin 1β (IL1β) levels, 2 h after administration. Pre-treatment with leptin, 2 h before LPS administration, did not influence the HPA axis response to LPS. In turn, LPS did not affect plasma leptin levels. Our findings suggest that leptin does not influence HPA function or IL1β secretion in a rat model of LPS-induced sepsis, and thus that leptin is unlikely to be involved in the acute-phase endocrine response to bacterial infection in rats.
Keywords: stress, leptin, HPA, sepsis
Introduction
Sepsis is the result of an over-activation of the innate immune response against bacterial infections (Matot & Sprung 2001) and can result in fever, tachypnea, tachycardia, deregulated organ perfusion, renal failure, hypoxaemia and altered mental state (Bone et al. 1989). Biomarkers of sepsis include cytokines such as interleukin 1B (IL1β; Sankar & Webster 2012), as well as other receptor and cell marker biomarkers (Heuer et al. 2004). Sepsis progression can result in immune dysfunction (Tschop et al. 2010), which is the leading cause for mortality in non-coronary patients in non-Western countries (Arabi et al. 2003), comparable with annual death rates from acute myocardial infarction in Western countries. Obesity is a risk factor for sepsis morbidity and mortality. Morbid obesity increases the risk of death by sepsis following major surgery by 50% (Prabhakar et al. 2002). It is thought that the pro-inflammatory phenotype that accompanies obesity creates a context in which any additional inflammatory stimulus results in an exaggerated inflammatory response (Vachharajani 2008).
The adipose tissue-derived hormone leptin has a well-characterised role in energy homoeostasis, but has also been suggested to play a pathogenic role in sepsis (Shapiro et al. 2010). Mouse endotoxaemia and caecal ligation puncture models of sepsis present with elevated levels of leptin, while exogenous administration of leptin to endotoxaemic mice increases mortality (Shapiro et al. 2010). Human septic patients have elevated circulating levels of the soluble leptin receptor (Ob-Re), which correlate with disease severity indices (Shapiro et al. 2010). Leptin has been reported to serve as an early biomarker of sepsis in patients, allowing differentiation between patients with systemic inflammatory response syndrome and patients with sepsis (Yousef et al. 2010). The hypothalamic–pituitary–adrenal (HPA) axis plays an important protective role in the body's defence against sepsis during a bacterial infection. Bacterial proteins stimulate the release of cytokines, including tumour necrosis factor α (TNFα), IL1 and IL6 (John & Buckingham 2003), which can modulate the HPA axis increasing expression of corticotrophin-releasing hormone (CRH) and arginine vasopressin in the hypothalamus, and adrenocorticotropic hormone (ACTH) in the pituitary gland (John & Buckingham 2003) and increasing circulating glucocorticoid levels (Besedovsky et al. 1986). Glucocorticoids themselves act in a negative feedback loop to suppress the HPA axis, leading to a shift from pro-inflammatory immune responses to anti-inflammatory immune responses (Elenkov & Chrousos 1999). There is evidence to suggest that leptin has an inhibitory role in the regulation of the HPA axis (Maffei et al. 1995). Leptin administration blunts the restraint stress-induced activation of the HPA axis in mice (Heiman et al. 1997) and can directly inhibit ACTH-stimulated cortisol/corticosterone release from human and rat adrenal cells in vitro (Gaillard et al. 2000). Thus, the possible pathogenic role for leptin in sepsis may be linked to leptin-induced suppression of the HPA axis impairing the protective role of the HPA axis in sepsis.
We hypothesised that leptin attenuates the HPA axis response to sepsis. We investigated the direct effects of leptin on the HPA axis response to acute lipopolysaccharide (LPS) administration in rats, a model of the neuroimmunological changes observed in sepsis in both rodents and humans. Acute LPS administration increases circulating levels of the cytokines IL1β, IL6 and TNFα and up-regulates the HPA axis (Besedovsky et al. 1986, Rivier et al. 1989, Takao et al. 1993, Csontos et al. 2010). If leptin acts to exacerbate the pathophysiological response to LPS, it would suggest a possible role for anti-leptin therapy in high-risk septic patients.
Materials and methods
Animals
Male Wistar rats (specifically pathogen free; Charles River, Margate, UK) weighing 170–210 g and at 7 weeks of age were maintained in groups of four under controlled temperature (21±1 °C) and light (12 h light:12 h darkness cycle; lights on at 0700 h) with access to food (RM1 diet, Special Diet Services Ltd, Witham, Essex, UK) and water and were allowed to feed ad libitum. They were handled daily for 2 weeks before the study. All animal procedures conducted were approved by the British Home Office under the Animals (Scientific Procedures) Act 1986.
Materials
LPS from Escherichia coli was supplied by Sigma–Aldrich Ltd. Recombinant rat leptin was supplied by R&D Systems (Abingdon, UK).
Study design
Leptin has been shown to significantly reduce basal plasma corticosterone levels, 3–4 h after administration (Clark et al. 2008). Plasma stress hormone levels peak at 1–2 h after i.p. LPS administration, at doses ranging from 10.5 to 250 μg/kg (Takemura et al. 1997, Gaillard et al. 2000, Tolchard et al. 2009), to levels comparable with those observed in septic rats (Carlson et al. 2007). Rats (n=10/group) were administered with either 100 μl vehicle (saline) or 2 mg/kg recombinant rat leptin intraperitoneally, a dose previously shown to suppress the HPA axis response to acute restraint stress (Heiman et al. 1997) and to activate regions of the brain involved in the regulation of energy balance (Elmquist et al. 1997). After 2 h, rats received a second i.p. injection of either 100 μl vehicle (saline) or 25 μg/kg LPS, a dose that induces a significant, albeit reversible, increase in HPA activity (Huang et al. 1998). All rats were killed by decapitation 2 h after the second injection and trunk blood was immediately collected into plastic potassium-EDTA tubes (1.6 mg EDTA/mm of blood). Plasma was separated by centrifugation for 10 min at 2000 r.p.m. (Boeco Centrifuge S-8, Boeco, Hamburg, Germany) and stored at −70 °C for measurement of ACTH, corticosterone, leptin and IL1β concentrations.
Plasma hormone measurements
Plasma ACTH levels were measured by IRMA (DiaSorin, Stillwater, MN, USA); intra-assay variation was 3.5–4.8% and inter-assay variation was 3.2–5.7%. Plasma corticosterone levels were determined by enzyme immunoassay (Cayman Chemical Company, Cambridge, UK); intra-assay variation was 8% and inter-assay variation was 9.8%. Plasma leptin levels were determined by ELISA (Crystal Chem, Inc., Downers Grove, IL, USA); both intra-assay and inter-assay variations were ≤10%. Plasma IL1β levels were determined by ELISA R&D Systems; intra-assay variation was 3.9–8.8% and inter-assay variation was 4.1–5.7%. All assays were performed according to the manufacturers' instructions.
Statistical analysis
All data are presented as mean±s.e.m. Groups were compared using one-way ANOVA followed by Tukey's post-hoc test with GraphPad Prism version 5 (GraphPad Software, Inc., La Jolla, CA, USA). In all cases, P<0.05 was considered statistically significant.
Results
Effect of leptin on the HPA axis response to LPS
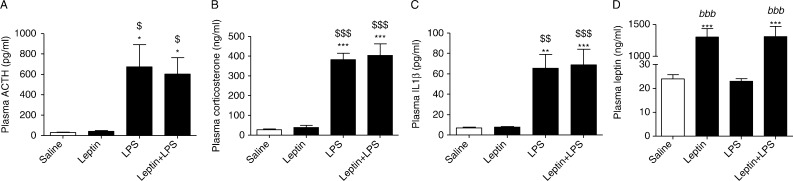
At 2 h after administration, 25 μg/kg LPS significantly increased plasma ACTH (674±217 pg/ml) and corticosterone (381.8±32.6 ng/ml) levels (Fig. 1A and B). Pre-treatment with 2 mg/kg leptin, 2 h before LPS administration, did not significantly influence the HPA axis response to LPS (ACTH, 608±160 pg/ml; corticosterone, 403.3±59.2 ng/ml) (Fig. 1A and B). LPS did not affect plasma leptin (23±1.09 ng/ml) levels (Fig. 1D) but did significantly increase plasma IL1β (65.5±13.6 pg/ml) levels (Fig. 1C) compared with untreated controls. Leptin had no effect on basal (7.77±0.714 pg/ml) or LPS-stimulated (68.8±15.5 pg/ml) plasma IL1β concentrations (Fig. 1C). As expected, plasma leptin levels were significantly higher in rats that received leptin compared with rats that did not receive leptin (Fig. 1D).
Figure 1.
The effect of leptin on LPS-stimulated increases in ACTH, corticosterone and IL1β concentrations. Male Wistar rats were intraperitoneally injected with 100 μl saline or 2 mg/kg leptin 2 h before being intraperitoneally injected with 100 μl saline or 25 μg/kg LPS. Rats were decapitated 2 h after LPS injection and plasma (A) ACTH, (B) corticosterone, (C) IL1β and (D) leptin concentrations were measured. Data are presented as mean±s.e.m. one-way ANOVA. *P<0.05 vs saline; **P<0.01 vs saline; ***P<0.001 vs saline; $ P<0.05 vs leptin; $$ P<0.01 vs leptin; $$$ P<0.001 vs leptin; bbb P<0.001 vs LPS and n=8–10.
Discussion
We aimed to investigate the effect of leptin on the neuroendocrine response to LPS in the male Wistar rat. Our studies suggest that peripheral leptin administration does not affect the HPA axis or the cytokine response to LPS-induced endotoxaemia.
Based on the evidence in the literature that LPS activates the HPA axis at doses ranging from 10.5 to 250 μg/kg in rats, we initially carried out a dose–response study investigating the effects of various doses of LPS (10, 25, 100, 250 μg/kg) on HPA axis activation (S Basharat, KG Murphy, SR Bloom, JC Buckingham & CD John, 2012, unpublished observations). We found 25 μg/kg LPS to be the lowest dose that significantly elevated plasma ACTH and corticosterone levels at the pertinent time points in our model (n=10). Others have previously shown that our chosen dose of LPS induces a strong but reversible stress response, as demonstrated by the inhibition of 25 μg/kg LPS-induced fever by systemic administration of α-MSH in rats (Huang et al. 1998). Plasma ACTH and corticosterone levels measured 2 h after i.p. LPS administration within the study by Huang and colleagues were similar to those achieved in our study. We measured IL1β as an early marker of sepsis in our model as it is one of the cytokines most strongly associated with sepsis and, in both human and experimental septic models, has been shown to act as an ‘initiator’ cytokine that stimulates a cytokine cascade, ultimately driving many of the physiological changes seen in sepsis (Blackwell & Christman 1996). The plasma IL1β levels achieved in our LPS-treated rats are similar to levels observed in septic humans (Kurt et al. 2007, Sankar & Webster 2012) and fall into the range of IL1β levels observed in animal models of sepsis (Rodríguez-Wilhelmi et al. 2002). Our chosen dose of leptin was the same as that used in the study carried out by Heiman et al. (1997), which demonstrates that leptin can blunt restraint stress-induced HPA activation in mice 3–4 h after its administration. Our study was designed to use the same time points but with a different stressor (LPS), given that interpreting the contradictory literature regarding the effects of leptin on the HPA axis is difficult due to the variations in the time points investigated, mode of plasma and tissue collection and animal model used. Clark et al. (2008) also utilised the same leptin dose and time point as our study. In contrast to our finding, they found that leptin suppressed baseline corticosterone levels, perhaps because their rats had higher basal corticosterone levels (200 ng/ml compared with 25 ng/ml in our study (Clark et al. 2008)), which may perhaps reflect differences in housing or strain. It may be difficult to detectably suppress corticosterone concentrations below relatively low basal levels. In our study, 2 mg/kg leptin induced circulating plasma leptin levels well above those seen in obese rats (Beck & Richy 2009).
It is possible that investigating the effects of different doses of LPS and leptin, and/or measuring HPA axis activation at different time points might reveal effects of leptin that we do not detect in this study. Conflicting reports suggest that leptin can stimulate or suppress the HPA axis in different contexts (Maffei et al. 1995, Heiman et al. 1997, Nishiyama et al. 1999, Jethwa et al. 2006) and suggest that animal model, type of stressor and route of leptin administration can greatly influence study outcome. Evidence for the suppressive effects of leptin on the HPA axis includes the ability of leptin to blunt the stress-induced activation of the HPA axis in mice (Heiman et al. 1997), inhibit CRH release from stimulated ex vivo rat hypothalamic explants (Heiman et al. 1997) and attenuate ACTH-stimulated cortisol release from adrenal cells in vitro (Bornstein et al. 1997, Gaillard et al. 2000). The presence of the leptin receptor (LEPR) in ACTH-producing cells of the anterior pituitary gland (Zamorano et al. 1997) suggests that they are targets of leptin signalling, though incubation of primary rat pituitary cells with leptin does not influence CRH-induced ACTH release (Heiman et al. 1997). Peripheral leptin administration to fasted mice attenuates the fasting-induced activation of the HPA axis as demonstrated by normalised plasma ACTH and corticosterone levels comparable to those seen in fed mice (Ahima et al. 1996), while systemic administration of leptin in male Sprague–Dawley rats decreases baseline plasma corticosterone levels (Clark et al. 2008).
However, under specific conditions, leptin can stimulate the HPA axis. I.c.v. administration of leptin has been shown to increase Crh and CRH receptor (Crhr2) mRNA expression in the rat hypothalamic paraventricular nucleus and ventromedial nucleus (Nishiyama et al. 1999). Leptin also stimulates CRH release from hypothalamic explants (Costa et al. 1997, Raber et al. 1997, Jethwa et al. 2006) and Jethwa et al. (2006) reported an acute stimulatory effect of peripheral leptin on the HPA axis in rats.
Such variable findings stem from the absence of uniformly designed and directly comparable in vivo leptin-stress experiments. Most studies have focused on the ability of leptin to influence the HPA response to mild stressors, whereas our study has focused on the effects of leptin on the HPA response to a powerful immunological stressor. It is interesting to note that while different stressor types, e.g. head trauma (Ott et al. 1987), stroke (Kang et al. 2008), autoimmune diseases (Hu et al. 1993) and psychological stress (Connor & Leonard 1998), ultimately activate the HPA axis via a convergence at the hypothalamus to precipitate the CRH–ACTH–glucocorticoid cascade, there is surprisingly little overlap in the sets of genes within the brain that are induced/repressed by severe immunological stress compared with mild psychological stressors such as restraint stress (Reyes et al. 2003). Furthermore, in addition to the convergent effect at the hypothalamus, LPS can act directly at the pituitary gland to stimulate the inter-pituitary release of IL6, which subsequently up-regulates ACTH secretion (Gloddek et al. 2001, Watanobe & Yoneda 2003), and also within the adrenal cortex (Andreis et al. 1991, Pournajafi Nazarloo et al. 2003, Mohn et al. 2011). Leptin could feasibly reduce adrenal gland sensitivity to ACTH stimulation, though correlation analyses of plasma ACTH and corticosterone concentrations in our animals indicate a moderate positive correlation, suggesting that there is not a marked reduction in ACTH sensitivity at the adrenal gland. Therefore, the fact that LPS i) induces a different activational response within the brain compared with mild stressors and ii) activates the HPA axis at multiple levels may provide an explanation as to why leptin failed to attenuate the LPS-induced HPA response.
In conclusion, our findings show that an acute dose of 2 mg/kg leptin fails to influence HPA function or IL1β secretion, 4 h after injection, in a rat model of acute 25 μg/kg LPS-induced sepsis. This suggests that leptin may not to be involved in the acute-phase response to bacterial infection in rats.
Author contribution statement
S B, C D J and K G M designed the study, S B was responsible for the animal management, S B and J A P administered the injections, S B conducted the plasma assays and S B, C D J and K G M wrote the paper.
Declaration of interest
The authors declare that there is no conflict of interest that could be perceived as prejudicing the impartiality of the research reported.
Funding
The section is funded by grants from the MRC, BBSRC, NIHR and an Integrative Mammalian Biology (IMB) Capacity Building Award, and by a FP7-HEALTH-2009-241592 EuroCHIP grant and is supported by the NIHR Imperial Biomedical Research Centre Funding Scheme. This work is supported by a BBSRC Doctoral Training-Strategic Skills Award grant (BB/F017340/1).
References
- Ahima RS, Prabakaran D, Mantzoros C, Qu D, Lowell B, Maratos-Flier E, Flier JS. Role of leptin in the neuroendocrine response to fasting. Nature. 1996;382:250–252. doi: 10.1038/382250a0. [DOI] [PubMed] [Google Scholar]
- Andreis PG, Neri G, Belloni AS, Mazzocchi G, Kasprzak A, Nussdorfer GG. Interleukin-1β enhances corticosterone secretion by acting directly on the rat adrenal gland. Endocrinology. 1991;129:53–57. doi: 10.1210/endo-129-1-53. [DOI] [PubMed] [Google Scholar]
- Arabi Y, Al Shirawi N, Memish Z, Venkatesh S, Al-Shimemeri A. Assessment of six mortality prediction models in patients admitted with severe sepsis and septic shock to the intensive care unit: a prospective cohort study. Critical Care. 2003;7:R116–R122. doi: 10.1186/cc2373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck B, Richy S. Dietary modulation of ghrelin and leptin and gorging behavior after weight loss in the obese Zucker rat. Journal of Endocrinology. 2009;202:29–34. doi: 10.1677/JOE-09-0080. [DOI] [PubMed] [Google Scholar]
- Besedovsky H, Del Rey A, Sorkin E, Dinarello CA. Immunoregulatory feedback between interleukin-1 and glucocorticoid hormones. Science. 1986;233:652–654. doi: 10.1126/science.3014662. [DOI] [PubMed] [Google Scholar]
- Blackwell TS, Christman JW. Sepsis and cytokines: current status. British Journal of Anaesthesia. 1996;77:110–117. doi: 10.1093/bja/77.1.110. [DOI] [PubMed] [Google Scholar]
- Bone RC, Fisher CJ, Jr, Clemmer TP, Slotman GJ, Metz CA, Balk RA. Sepsis syndrome: a valid clinical entity. Methylprednisolone Severe Sepsis Study Group. Critical Care Medicine. 1989;17:389–393. doi: 10.1097/00003246-198905000-00002. [DOI] [PubMed] [Google Scholar]
- Bornstein SR, Uhlmann K, Haidan A, Ehrhart-Bornstein M, Scherbaum WA. Evidence for a novel peripheral action of leptin as a metabolic signal to the adrenal gland: leptin inhibits cortisol release directly. Diabetes. 1997;46:1235–1238. doi: 10.2337/diab.46.7.1235. [DOI] [PubMed] [Google Scholar]
- Carlson DE, Chiu WC, Fiedler SM, Hoffman GE. Central neural distribution of immunoreactive Fos and CRH in relation to plasma ACTH and corticosterone during sepsis in the rat. Experimental Neurology. 2007;205:485–500. doi: 10.1016/j.expneurol.2007.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark KA, Shin AC, Sirivelu MP, Mohankumar SM, Mohankumar PS. Systemic administration of leptin decreases plasma corticosterone levels: role of hypothalamic norepinephrine. Brain Research. 2008;1195:89–95. doi: 10.1016/j.brainres.2007.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connor TJ, Leonard BE. Depression, stress and immunological activation: the role of cytokines in depressive disorders. Life Sciences. 1998;62:583–606. doi: 10.1016/S0024-3205(97)00990-9. [DOI] [PubMed] [Google Scholar]
- Costa A, Poma A, Martignoni E, Nappi G, Ur E, Grossman A. Stimulation of corticotrophin-releasing hormone release by the obese (ob) gene product, leptin, from hypothalamic explants. Neuroreport. 1997;8:1131–1134. doi: 10.1097/00001756-199703240-00014. [DOI] [PubMed] [Google Scholar]
- Csontos C, Foldi V, Palinkas L, Bogar L, Roth E, Weber G, Lantos J. Time course of pro- and anti-inflammatory cytokine levels in patients with burns – prognostic value of interleukin-10. Burns. 2010;36:483–494. doi: 10.1016/j.burns.2009.10.009. [DOI] [PubMed] [Google Scholar]
- Elenkov IJ, Chrousos GP. Stress hormones, Th1/Th2 patterns, pro/anti-inflammatory cytokines and susceptibility to disease. Trends in Endocrinology and Metabolism. 1999;10:359–368. doi: 10.1016/S1043-2760(99)00188-5REF14=10.1016/S1043-2760(99)00188-5. [DOI] [PubMed] [Google Scholar]
- Elmquist JK, Ahima RS, Maratos-Flier E, Flier JS, Saper CB. Leptin activates neurons in ventrobasal hypothalamus and brainstem. Endocrinology. 1997;138:839–842. doi: 10.1210/endo.138.2.5033. [DOI] [PubMed] [Google Scholar]
- Gaillard RC, Spinedi E, Chautard T, Pralong FP. Cytokines, leptin, and the hypothalamo–pituitary–adrenal axis. Annals of the New York Academy of Sciences. 2000;917:647–657. doi: 10.1111/j.1749-6632.2000.tb05430.x. [DOI] [PubMed] [Google Scholar]
- Gloddek J, Lohrer P, Stalla J, Arzt E, Stalla GK, Renner U. The intrapituitary stimulatory effect of lipopolysaccharide on ACTH secretion is mediated by paracrine-acting IL-6. Experimental and Clinical Endocrinology and Diabetes. 2001;109:410–415. doi: 10.1055/s-2001-18995. [DOI] [PubMed] [Google Scholar]
- Heiman ML, Ahima RS, Craft LS, Schoner B, Stephens TW, Flier JS. Leptin inhibition of the hypothalamic–pituitary–adrenal axis in response to stress. Endocrinology. 1997;138:3859–3863. doi: 10.1210/en.138.9.3859. [DOI] [PubMed] [Google Scholar]
- Heuer JG, Sharma GR, Gerlitz B, Zhang T, Bailey DL, Ding C, Berg DT, Perkins D, Stephens EJ, Holmes KC, et al. Evaluation of protein C and other biomarkers as predictors of mortality in a rat cecal ligation and puncture model of sepsis. Critical Care Medicine. 2004;32:1570–1578. doi: 10.1097/01.CCM.0000129488.54282.1A. [DOI] [PubMed] [Google Scholar]
- Hu Y, Dietrich H, Herold M, Heinrich PC, Wick G. Disturbed immuno-endocrine communication via the hypothalamo–pituitary–adrenal axis in autoimmune disease. International Archives of Allergy and Immunology. 1993;102:232–241. doi: 10.1159/000236531. [DOI] [PubMed] [Google Scholar]
- Huang QH, Hruby VJ, Tatro JB. Systemic α-MSH suppresses LPS fever via central melanocortin receptors independently of its suppression of corticosterone and IL-6 release. American Journal of Physiology. Regulatory, Integrative, and Comparative Physiology. 1998;275:R524–R530. doi: 10.1152/ajpregu.1998.275.2.R524. [DOI] [PubMed] [Google Scholar]
- Jethwa PH, Smith KL, Small CJ, Abbott CR, Darch SJ, Murphy KG, Seth A, Semjonous NM, Patel SR, Todd JF, et al. Neuromedin U partially mediates leptin-induced hypothalamo–pituitary adrenal (HPA) stimulation and has a physiological role in the regulation of the HPA axis in the rat. Endocrinology. 2006;147:2886–2892. doi: 10.1210/en.2005-0983. [DOI] [PubMed] [Google Scholar]
- John CD, Buckingham JC. Cytokines: regulation of the hypothalamo–pituitary–adrenocortical axis. Current Opinion in Pharmacology. 2003;3:78–84. doi: 10.1016/S1471-4892(02)00009-7. [DOI] [PubMed] [Google Scholar]
- Kang YM, Zhang ZH, Xue B, Weiss RM, Felder RB. Inhibition of brain proinflammatory cytokine synthesis reduces hypothalamic excitation in rats with ischemia-induced heart failure. American Journal of Physiology. Heart and Circulatory Physiology. 2008;295:H227–H236. doi: 10.1152/ajpheart.01157.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kurt AN, Aygun AD, Godekmerdan A, Kurt A, Dogan Y, Yilmaz E. Serum IL-1β, IL-6, IL-8, and TNF-α levels in early diagnosis and management of neonatal sepsis. Mediators of Inflammation. 2007;2007:31397. doi: 10.1155/2007/31397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maffei M, Halaas J, Ravussin E, Pratley RE, Lee GH, Zhang Y, Fei H, Kim S, Lallone R, Ranganathan S, et al. Leptin levels in human and rodent: measurement of plasma leptin and ob RNA in obese and weight-reduced subjects. Nature Medicine. 1995;1:1155–1161. doi: 10.1038/nm1195-1155. [DOI] [PubMed] [Google Scholar]
- Matot I, Sprung CL. Definition of sepsis. Intensive Care Medicine. 2001;27:S3–S9. doi: 10.1007/PL00003795. [DOI] [PubMed] [Google Scholar]
- Mohn CE, Fernandez-Solari J, De Laurentiis A, Bornstein SR, Ehrhart-Bornstein M, Rettori V. Adrenal gland responses to lipopolysaccharide after stress and ethanol administration in male rats. Stress. 2011;14:216–226. doi: 10.3109/10253890.2010.532254. [DOI] [PubMed] [Google Scholar]
- Nishiyama M, Makino S, Asaba K, Hashimoto K. Leptin effects on the expression of type-2 CRH receptor mRNA in the ventromedial hypothalamus in the rat. Journal of Neuroendocrinology. 1999;11:307–314. doi: 10.1046/j.1365-2826.1999.00331.x. [DOI] [PubMed] [Google Scholar]
- Ott L, Young B, McClain C. The metabolic response to brain injury. Journal of Parenteral and Enteral Nutrition. 1987;11:488–493. doi: 10.1177/0148607187011005488. [DOI] [PubMed] [Google Scholar]
- Pournajafi Nazarloo H, Takao T, Taguchi T, Ito H, Hashimoto K. Modulation of type I IL-1 receptor and IL-1β mRNA expression followed by endotoxin treatment in the corticotropin-releasing hormone-deficient mouse. Journal of Neuroimmunology. 2003;140:102–108. doi: 10.1016/S0165-5728(03)00176-0. [DOI] [PubMed] [Google Scholar]
- Prabhakar G, Haan CK, Peterson ED, Coombs LP, Cruzzavala JL, Murray GF. The risks of moderate and extreme obesity for coronary artery bypass grafting outcomes: a study from the Society of Thoracic Surgeons' database. Annals of Thoracic Surgery. 2002;74:1130–1131. doi: 10.1016/S0003-4975(02)03899-7. discussion 1130–1. [DOI] [PubMed] [Google Scholar]
- Raber J, Chen S, Mucke L, Feng L. Corticotropin-releasing factor and adrenocorticotrophic hormone as potential central mediators of OB effects. Journal of Biological Chemistry. 1997;272:15057–15060. doi: 10.1074/jbc.272.24.15057. [DOI] [PubMed] [Google Scholar]
- Reyes TM, Walker JR, Decino C, Hogenesch JB, Sawchenko PE. Categorically distinct acute stressors elicit dissimilar transcriptional profiles in the paraventricular nucleus of the hypothalamus. Journal of Neuroscience. 2003;23:5607–5616. doi: 10.1523/JNEUROSCI.23-13-05607.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rivier C, Chizzonite R, Vale W. In the mouse, the activation of the hypothalamic–pituitary–adrenal axis by a lipopolysaccharide (endotoxin) is mediated through interleukin-1. Endocrinology. 1989;125:2800–2805. doi: 10.1210/endo-125-6-2800. [DOI] [PubMed] [Google Scholar]
- Rodríguez-Wilhelmi P, Montes R, Matsukawa A, Hurtado V, Montes M, Hermida J, Rocha E. Interleukin (IL)-8 and growth related oncogene-α in severe endotoxemia and the effects of a tumor necrosis factor-α/IL-1β inhibitor on these chemokines. Experimental and Molecular Pathology. 2002;73:220–229. doi: 10.1006/exmp.2002.2467. [DOI] [PubMed] [Google Scholar]
- Sankar V, Webster NR. Clinical application of sepsis biomarkers. Journal of Anesthesia. 2012;27:269–283. doi: 10.1007/s00540-012-1502-7. [DOI] [PubMed] [Google Scholar]
- Shapiro NI, Khankin EV, Van Meurs M, Shih SC, Lu S, Yano M, Castro PR, Maratos-Flier E, Parikh SM, Karumanchi SA, et al. Leptin exacerbates sepsis-mediated morbidity and mortality. Journal of Immunology. 2010;185:517–524. doi: 10.4049/jimmunol.0903975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takao T, Culp SG, De Souza EB. Reciprocal modulation of interleukin-1β (IL-1β) and IL-1 receptors by lipopolysaccharide (endotoxin) treatment in the mouse brain–endocrine–immune axis. Endocrinology. 1993;132:1497–1504. doi: 10.1210/endo.132.4.8462448. [DOI] [PubMed] [Google Scholar]
- Takemura T, Makino S, Takao T, Asaba K, Suemaru S, Hashimoto K. Hypothalamic–pituitary–adrenocortical responses to single vs. repeated endotoxin lipopolysaccharide administration in the rat. Brain Research. 1997;767:181–191. doi: 10.1016/S0006-8993(97)00460-5. [DOI] [PubMed] [Google Scholar]
- Tolchard S, Burns PA, Nutt DJ, Fitzjohn SM. Hypothermic responses to infection are inhibited by α2-adrenoceptor agonists with possible clinical implications. British Journal of Anaesthesia. 2009;103:554–560. doi: 10.1093/bja/aep199. [DOI] [PubMed] [Google Scholar]
- Tschop J, Dattilo JR, Prakash PS, Kasten KR, Tschop MH, Caldwell CC. The leptin system: a potential target for sepsis induced immune suppression. Endocrine, Metabolic & Immune Disorders Drug Targets. 2010;10:336–347. doi: 10.2174/1871530311006040336. [DOI] [PubMed] [Google Scholar]
- Vachharajani V. Influence of obesity on sepsis. Pathophysiology. 2008;15:123–134. doi: 10.1016/j.pathophys.2008.04.008. [DOI] [PubMed] [Google Scholar]
- Watanobe H, Yoneda M. A mechanism underlying the sexually dimorphic ACTH response to lipopolysaccharide in rats: sex steroid modulation of cytokine binding sites in the hypothalamus. Journal of Physiology. 2003;547:221–232. doi: 10.1113/jphysiol.2002.032169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yousef AA, Amr YM, Suliman GA. The diagnostic value of serum leptin monitoring and its correlation with tumor necrosis factor-α in critically ill patients: a prospective observational study. Critical Care. 2010;14:R33. doi: 10.1186/cc8911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zamorano PL, Mahesh VB, De Sevilla LM, Chorich LP, Bhat GK, Brann DW. Expression and localization of the leptin receptor in endocrine and neuroendocrine tissues of the rat. Neuroendocrinology. 1997;65:223–228. doi: 10.1159/000127276. [DOI] [PubMed] [Google Scholar]



 This work is licensed under a
This work is licensed under a