Abstract
Purpose
Studies were conducted to test whether fever-range whole body hyperthermia, rationally combined with oxaliplatin chemotherapy, would boost its efficacy without substantial toxicity.
Materials and Methods
The effect of heat on oxaliplatin cytotoxicity, cellular uptake, and platinum-DNA adduct formation was studied in vitro using the MTLn3 tumor cell line. In vivo, oxaliplatin was given with thermal therapy to rats bearing highly treatment-resistant MTLn3 mammary adenocarcinomas at various doses and times before, during, and after heating. Tumor growth, survival, and toxicity were measured to determine treatment outcome.
Results
Heating for 6h at 40°C halved the oxaliplatin IC-50 dose for MTLn3 cells. Cellular uptake of platinum and platinum adducts increased by 34% and 36%, respectively, with heat. In vivo, 50% of all rats given 10 mg/kg oxaliplatin 24h before 6h of fever-range thermal therapy were completely, immunologically, cured while a further 11% regressed their primary tumor but ultimately succumbed to metastases, and 17% experienced a limited response with increased survival. The curative response occurred only in a narrow range of doses, with most cures at 10 mg/kg. Thermochemotherapy-treated, but uncured, animals had delayed incidence and slowed growth of metastases. Anti-tumor efficacy was greatest, and toxicity was least, when oxaliplatin was administered 12 or 24 hours before FR-WB-TT.
Conclusions
When properly dosed and scheduled, oxaliplatin thermochemotherapy achieved permanent eradication of all primary and metastatic tumors in 50% of animals, seemingly through an immune response. Successful clinical translation of this protocol would yield hitherto unseen cures and substantial improvement in quality of life.
Keywords: Hyperthermia, oxaliplatin, thermochemotherapy, tumor, cure
Introduction
The holy grail of cancer therapy is to effect complete cures or at least durable cancer responses. While surgery, radiation, and chemotherapy, singly or in combination, can achieve complete responses in many localized primary cancers, rarely is a durable disease-free state achieved in patients with advanced metastatic cancers. This paper presents pre-clinical studies in an orthotopic rat model of metastatic breast cancer, closely resembling clinical inflammatory breast cancer, that reveal the curative potential of a multi-modality treatment combining whole body thermal therapy (hyperthermia) with chemotherapy.
Thermal therapy, or hyperthermia, for cancer treatment was originally developed on the premise that tumor cells have intrinsically higher heat sensitivity than normal cells. This is not universally true, and clinical hyperthermia often results in tumor cell kill as much because of heat effects on aberrant tumor vasculature as due to direct thermal destruction of tumor cells. Hyperthermia also enhances tumor sensitivity to radiation, and loco-regional hyperthermia is now an established adjunct to radiotherapy [1, 2]. Whole body thermal therapy, the deliberate heating of the entire body to achieve an elevated core temperature, can treat not only primary tumors but also metastatic disease. By increasing systemic blood flow, increasing tumor blood vessel permeability, and decreasing tumor interstitial pressure, whole body hyperthermia enhances the delivery of chemotherapy agents to tumors, sometimes directly augmenting the mechanism of drug action [3]. Combined with chemotherapy against cancer, systemic temperatures of 39.5°C – 40.5°C maintained for 4 – 6 hours, much like a fever, result in better or equal anti-tumor efficacy than maximally tolerated systemic thermal therapy, generally result in less toxicity, and reduce the requirements for intensive patient care [4, 5]. Studies of numerous chemotherapy drugs combined with fever-range whole body thermal therapy in animal models have defined effective combinations [6, 7] and led to a number of successful clinical whole body thermochemotherapy regimens [8, 9, 10]. Bull et al. have demonstrated the critical influence of the timing of chemotherapy with respect to whole body hyperthermia in determining both the efficacy and toxicity of thermochemotherapy treatments [11, 12, 13].
The effect of fever-range temperatures on the immune system is less well investigated. Fever-range whole body thermal therapy has been shown to enhance the host immune response, whereas extreme systemic thermal therapy (41.5– 42°C) may impair immune function [14,15]. Fever-range hyperthermia can induce expression of heat shock proteins [16, 17], enhance antigen presentation by dendritic cells [18, 15], promote dendritic cell maturation [18, 14] and activate immune effector cells (T lymphocytes and NK cells) [15, 19, 20]. New studies suggest that fever-like temperatures also activate an innate immune response by promoting toll-like receptor 4 (TLR4) signaling [21]. Furthermore, dying tumor cells resulting from some cancer chemotherapy agents can cause surface expression of chaperones that determine the uptake of tumor antigens by dendritic cells and affect dendritic cell maturation via interaction with TLR4 receptors [22]. Indeed, it appears that such immune responses are required for a successful anti-cancer response [23, 24, 25] and that low, non-cytotoxic, doses of some chemotherapeutic drugs, including oxaliplatin, cause cell death with immunostimulatory consequences [26, 27]. Oxaliplatin is a third generation platinum agent with broader clinical efficacy than the heat-interactive drugs cisplatin and carboplatin [6, 7] whose cytotoxicity has likewise been correlated with platinum-DNA adduct formation [28].
We therefore hypothesized that combining the immune stimulus of fever-range whole body thermal therapy with that of moderate doses of the immunogenic cell death causing chemotherapy agent oxaliplatin [29, 30], could produce durable responses in a clinically relevant model of advanced breast cancer. We first examined the effect of heat treatment on oxaliplatin-induced tumor cell kill, cellular platinum uptake, and platinum-DNA adduct formation in vitro. In vivo, combining oxaliplatin with fever-range whole body thermal therapy (FR-WB-TT) in the MTLn3 rat model of metastatic breast cancer, we demonstrated a substantial, apparently immune-mediated, critically dose-and schedule-dependent, anti-tumor effect of the thermochemotherapy that, when optimally dosed and scheduled, reproducibly achieved complete immunologic cures.
Methods
In vitro studies
Oxaliplatin Cytotoxicity
MTLn3 tumor cells (obtained from DR Welch, Department of Pathology, University of Pittsburgh; characterized by LC Stephens, Division of Veterinary Medicine and Surgery, M.D. Anderson Cancer Center [31]) were treated in a 96-well plate with doses of oxaliplatin (Sigma-Aldrich, St. Louis, MO; CAS# 61825-94-3) ranging from .0005 to 100 µg/mL (480 cells per well, one dose per well, repeated in triplicate) then placed in a water-jacketed incubator with 5% CO2 for 6 h at 37 °C (normothermia) or 40 °C (fever-range thermal therapy). Oxaliplatin was obtained as a lyophilized powder and reconstituted to 5 mg/ml in sterile water USP according to the manufacturer’s recommendations. A concentration of 2.5 mg/ml was prepared for bolus intravenous injection (see below) by dilution with equal parts 5% dextrose in water USP (D5W) and sterile water, and further diluted as necessary for in vitro studies. The platinum content of the stock solution was checked by atomic absorption spectrophotometry (see below). 72 h later, cells were incubated for 4 h with MTT [3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide]. Cell survival was determined from absorbance at 570 nm. A sigmoid curve of the form y = a*[1 − (1/(1 + b*exp(-cx)))] was least-squares fitted to the cell survival vs. dose curves. The IC-50 dose was determined as that dose resulting in 50% cell survival on the curve fit over the range 0.0001 to 100 µg/mL oxaliplatin.
Cellular Uptake of Oxaliplatin
Ten million MTLn3 tumor cells were treated with 200 µM (0.0795 mg/mL) oxaliplatin for 6 h at 37°C or 40°C. The cell pellet was re-suspended in 2N NaOH to a volume of 1.6mL of which 0.3mL was used for cellular uptake measurement, 0.2mL for determination of protein concentration, and 1.1mL for DNA concentration and DNA adduct measurement. After incubating the cell suspension at 50°C for 2h, protein concentration was determined by absorbance at 570nm compared to protein standards, and intracellular platinum was measured in pelletized cells solubilized in hyamine hydroxide (methylbenzethonium hydroxide) by graphite furnace atomic absorption spectrophotometry (see below) and normalized to the protein content to yield the cellular uptake as ng/mg protein.
Platinum-DNA Adducts
Cell pellets were re-suspended overnight in TE buffer with SDS, RNase A, and proteinase K. DNA was extracted from lysed tumor cells by phenol-chloroform-isoamylalcohol extraction. DNA concentration was determined by spectrophotometric measurement of UV absorbance at 260 nm. Platinum bound to DNA (Pt-DNA adducts) was measured as ng/mg DNA by graphite furnace absorption spectrophotometry.
Graphite Furnace Atomic Absorption Spectroscopy
Cells were dissolved in hyamine hydroxide in a 55oC water bath overnight and acidified with 0.3 N HCl. Cellular platinum concentration (ng/mg protein) in cell lysates or bound to DNA (ng/mg DNA) was determined by measurement of light absorption at 265.9 nm with a spectrophotometer (Varian AA 300, Varian Inc., Palo Alto, CA) equipped with a graphite furnace (Varian model GTA-96) for flameless sample vaporization. Cellular and DNA platinum levels were calculated by comparison with platinum standards by a method developed previously for cisplatin [32].
In vivo studies
Tumor Model
The rat MTLn3 orthotopic mammary adenocarcinoma model used for the in vivo studies has been described in depth previously [33, 34]. It is a syngeneic, highly aggressive, metastatic, mammary tumor with many of the characteristics of advanced human breast cancer. Spontaneous metastases in inguinal and axillary lymph nodes are palpable by 3 weeks after tumor inoculation, while macroscopic lung metastases are present at 4 weeks. 5 × 105 tumor cells were inoculated subcutaneously into the mammary fat pad of 6–7 week-old, immunologically normal, female, Fischer 344 rats (Harlan Sprague-Dawley Inc, Indianapolis, IN) weighing 100 – 120g. Palpable tumors developed by day 10. Animals with progressive disease were subsequently euthanized according to institutional animal welfare guidelines if, in the absence of signs of treatment response, tumors reached either the smaller of 2.5 cm3 or 10% of body weight, and if there were any signs of morbidity. The animal treatment protocol was approved by the University of Texas Health Science Center Animal Welfare Committee.
Treatment
On day 10 after tumor inoculation, rats with primary tumors around 100 mm3 in volume were randomized to treatment and control groups. At this time there was no overt evidence of metastases, however, microscopic inguinal and/or axillary lymph node metastases, but no microscopically visible metastatic lung deposits, would have been established [34]. For dose-response, toxicity, and curative response studies the groups were control and oxaliplatin administered 24h before fever-range whole body thermal therapy (FR-WB-TT). Control; oxaliplatin alone; oxaliplatin 24h before, 12h before, 3h before, simultaneously with, and 24h after (FR-WB-TT) were investigated for the schedule-dependency study. Control animals received sham treatment comprising injection of the same solution used to dilute the oxaliplatin (D5W in water) on the same days after tumor inoculation, and the same anesthesia protocol, as treated animals. They were maintained at a normal body temperature by placement on a microprocessor-controlled, warmed, water blanket (Blanketrol II Hyper-Hypothermia System and PlastiPad®, Cincinnati Sub-Zero Products, Inc., Cincinnati, OH].
Anesthesia
All animals received inhalation halothane or, more recently, isoflurane anesthesia during the 6h hyperthermia treatments, as well as during the corresponding 6h sham treatments as described previously [35]. Halothane anesthesia in combination with whole body hyperthermia is safe even when administered for many hours and affects neither tumor growth nor normal tissue toxicity [35]. Isoflurane anesthesia is similarly safe and appears not to affect tumor response. The rats were initially exposed to 3% halothane or isoflurane in pure oxygen in an induction chamber for approximately 10 minutes in order to induce surgical level anesthesia prior to the start of hyperthermia or sham treatment. 1.5% halothane, or 2% isoflurane, mixed with pure oxygen in a standard hospital grade vaporizer was delivered through a custom-made polymethyl methacrylate mask throughout the warm-up and treatment time, or equivalent sham treatment. The rats showed no evidence of discomfort during anesthesia and after treatment they recovered without ill effects, quickly becoming ambulatory.
Oxaliplatin
Oxaliplatin, prepared as described above to a concentration of 2.5 mg/mL, was injected into the lateral tail vein as a slow bolus (of around 0.6ml volume for 10mg/kg dose). To assess dose response, doses of 6, 8, 10, 12, and 14 mg/kg were administered. The maximally tolerated dose (MTD) of oxaliplatin given 24h before fever-range whole body thermal therapy is around 14 mg/kg. For tumor response and toxicity experiments, a dose of 10 mg/kg was used.
Thermal Therapy
Fever-range whole body thermal therapy (FR-WB-TT) was administered by partially immersing halothane or isoflurane-anesthetized rats into a thermostatically controlled circulating water bath maintained at 40.0°C ± 0.1°C as described previously [11, 13]. Rectal temperature was monitored continuously in each rat using small animal rectal thermistor probes (YSI model 402, Yellow Springs Instrument Co, Yellow Springs, OH) connected to a 12-channel switch box (YSI model 4002, Yellow Springs Instrument Co, Yellow Springs, OH) and digital tele-thermometer (YSI model 49A, Yellow Springs Instrument Co, Yellow Springs, OH), and was recorded every 5–10 min. The probes were calibrated against a mercury thermometer (Etrco ASTM 64°C) certified by the National Bureau of Standards. Approximately 15 min was required for the rectal temperature to reach 40.0°C. Each rat was individually maintained at 40.0°C ± 0.1°C for 6 hours by covering with foil and/or adjusting the depth of immersion in the water bath. The optimal duration of FR-WB-TT in these rats was previously determined to be 6 to 8 h [4, 31]. For logistical reasons, 6h of hyperthermia treatment was chosen.
Tumor Assessment
Tumor size (primary and inguinal and axillary metastases) was measured every 2 days using a vernier caliper to determine three orthogonal dimensions (d), and the tumor volume (V) was approximated according to the formula V = (d1 × 2 × d3) / 2. The incidence and size of any axillary and inguinal lymph node metastases were recorded.
Photographic image capture and processing
2272 × 1704 pixel color images of primary and metastatic tumors were recorded with a pocket digital camera (Canon Powershot SD10). For publication purposes, each original jpeg image was processed with Microsoft Office Picture Manager software (i) to standardize the white balance by making the center of the upper ruler white, and then (ii) to convert the white-balanced image to grey-scale. The grey-scale images were imported into Microsoft Publisher, resized, and arranged to fit the page in a 3 × 3 grid. Grid lines were superimposed on the images and cell titles added in text boxes. Arrows and corresponding labels in text boxes were superimposed on the images. The composite image was saved in Tagged Image File Format (TIFF).
Treatment response criteria
Animal response to treatment was graded into one of four categories by taking into account primary tumor and metastatic tumor response, body weight change, and survival:
| Cure | complete regression of all primary and metastatic tumors, normal life span and/or immune to MTLn3 tumor re-challenge; |
| CR | complete regression of primary tumor, weight gain, but eventual late death from new metastatic disease; |
| LR | limited response comprising temporary regression or growth arrest of primary tumor and/or metastases, weight gain or stabilization, some increase in survival; |
| NR | no reduction of primary tumor or metastases, weight loss, no increase in survival. |
Note that these are not the same as standard, clinical, oncologic response designations.
Toxicity Assessment
Rat body weight was recorded every other day as a general indication of treatment-induced toxicity. Hematocrit, an indicator of hematological toxicity, was measured in centrifuged blood samples withdrawn on days 8, 15, and 22 after treatment.
Statistical Analysis
The significance of differences in oxaliplatin IC-50 dose between 37°C and 40°C, and in primary tumor and metastatic lymph node tumor size, body weight, hematocrit, and survival between the experimental groups was calculated by an appropriate Student’s t test. A P-value of <0.05 was considered statistically significant.
RESULTS
In vitro
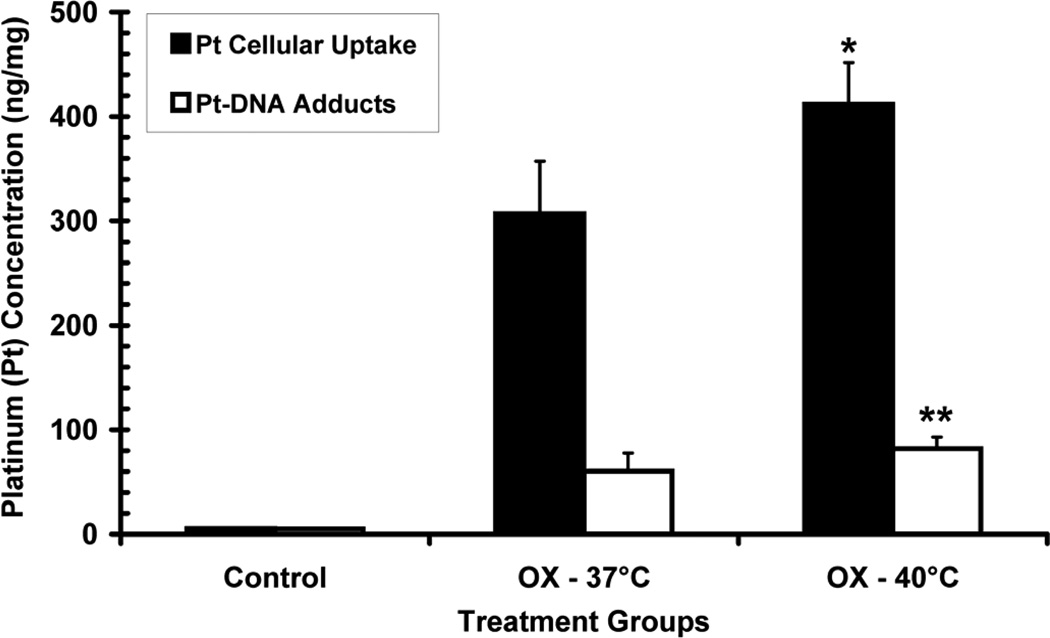
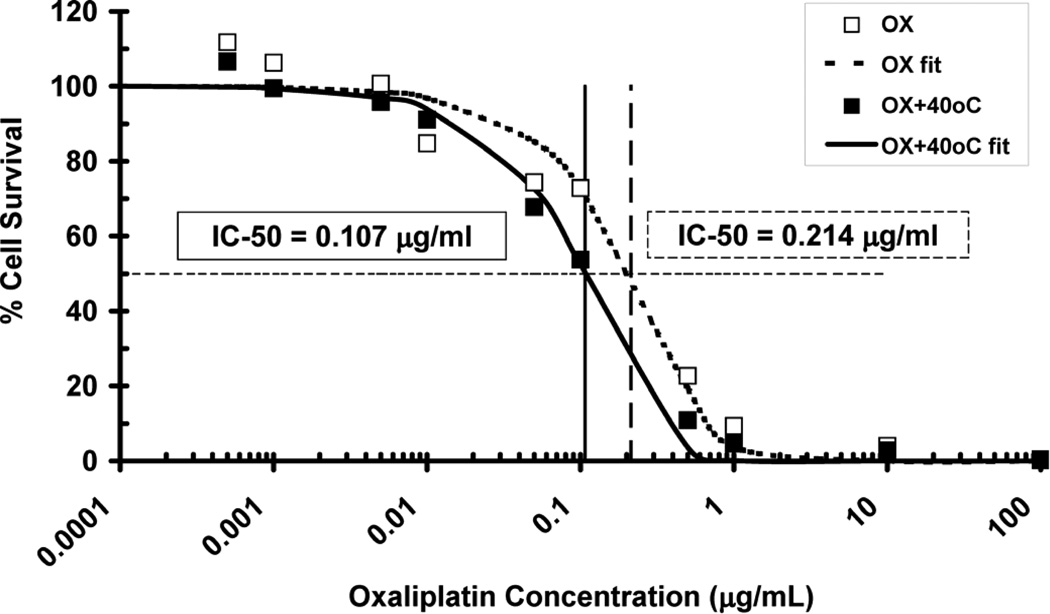
6h of heating to 40°C following oxaliplatin administration increased the intracellular concentration of platinum by 34% from 307 to 412 ng/mg protein (p=0.008) by as shown in Figure 1. The number of platinum-DNA adducts also increased 36% from 60 to 82 ng/mg DNA (p=0.039) in cells heated for 6h at 40°C. The ratio of cellular platinum uptake to DNA adducts was, however, unchanged by the higher temperature (5.09 at 37°C and 5.02 at 40 °C). MTLn3 cells treated with oxaliplatin at doses from 0.0005 to100 µg/mL were more effectively killed when incubated for 6h at 40°C compared to 37°C. The oxaliplatin dose at which half the cells were killed (IC-50 dose) was halved from 0.214 µg/ml at 37°C to 0.107 µg/ml at 40°C (Figure 2).
Figure 1.
Comparison of in vitro cellular platinum uptake (solid black bars) and platinum-DNA adducts (open bars) between cells incubated with 200 µM oxaliplatin (OX) for 6h at 37°C and 40°C. Cellular uptake of platinum (ng/mg protein) was significantly increased in heated cells (*p < 0.01) and platinum-DNA adducts (ng/mg DNA) were also increased (**p < 0.04) compared to oxaliplatin alone. Error bars indicate standard deviation.
Figure 2.
Percentage of surviving MTLn3 tumor cells in vitro, as measured by MTT assay, after administration of oxaliplatin in the dose range 0.0005 to 100 µg/mL, with (■) and without (□) 6h of 40°C heating, along with sigmoid curves fit to the measured data (--- OX, —OX+40°C). Heat treatment increased the efficacy of cell killing by oxaliplatin as evidenced by a shift to the left of the survival curve. The IC-50 dose was halved from 0.214µg/mL to 0.107µg/mL.
In vivo
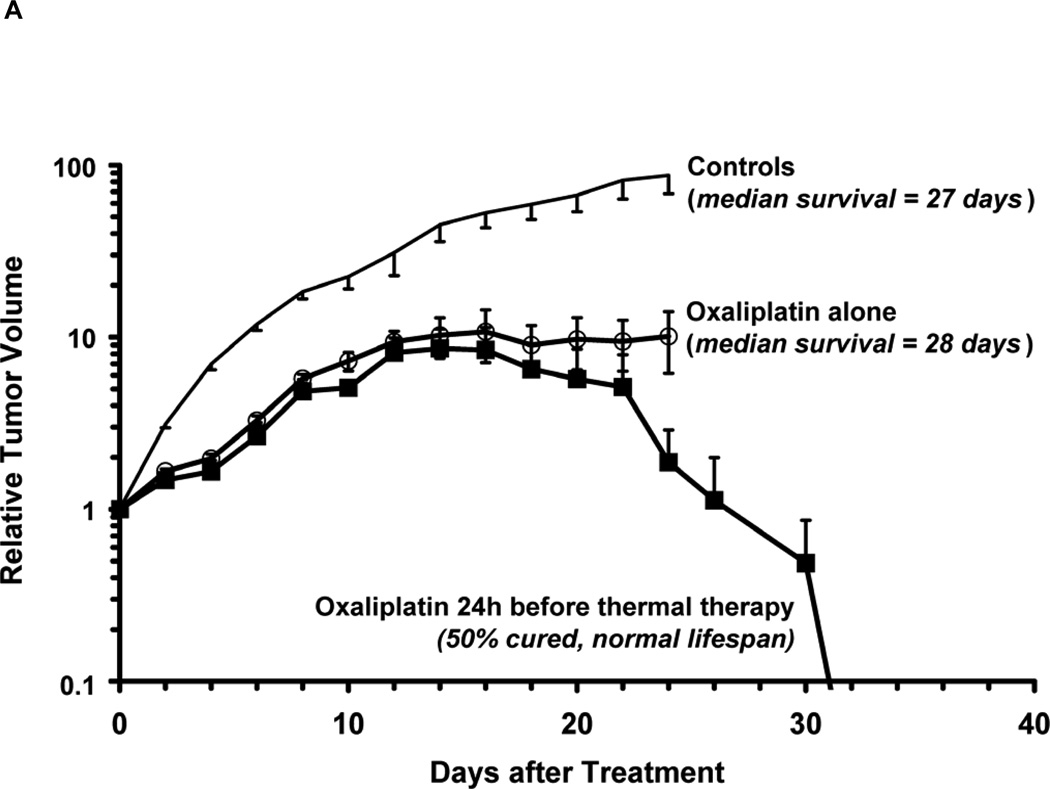
Figure 3A compares the average MTLn3 tumor growth in controls with rats in a representative experiment in which 6 rats were treated with 10 mg/kg oxaliplatin alone, and 6 rats were given 10 mg/kg oxaliplatin followed 24 hours later by 6h of fever-range whole body thermal therapy at 40°C. The tumor grew rapidly in control animals to almost 100 times the initial tumor volume and the rats died between day 20 and day 28 (median survival 27 days). Animals treated with oxaliplatin alone showed initial slowing of tumor growth for few days but the tumors soon began to grow rapidly again and survival was barely longer than in controls (median survival 28 days). In animals treated with oxaliplatin and thermal therapy, tumor growth was initially much the same as in those animals given oxaliplatin alone, but between day 10 and 16 there was a further slowing of tumor growth and 5 out of 6 animals (83%) began to regress their primary tumors. Three of these rats (50%) went on to be completely cured of all primary and metastatic tumors and live a normal life span.
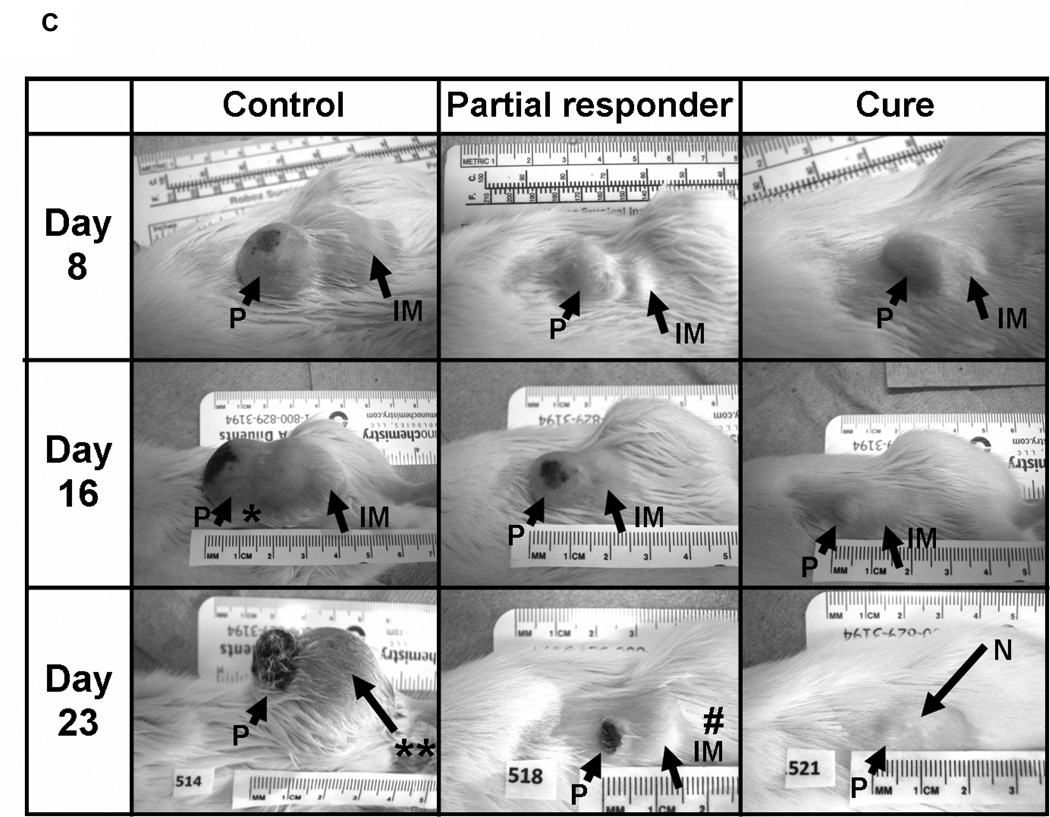
Figure 3.
A. Average relative primary tumor volume (RTV) in a representative experiment in controls, animals treated with 10 mg oxaliplatin alone (○), and after treatment with 10 mg oxaliplatin followed 24h later by 6h of fever-range whole body thermal therapy at 40°C (■, n=6 per group). Day 0 is the day of oxaliplatin treatment. Error bars indicate standard error; B. Primary tumor growth averaged over 6 experiments comprising 36 treated animals that either did not regress their tumors (○, 22%), were limited responders that temporarily regressed their tumors (□, 17%), or completely regressed their primary tumors (■, 61%), compared to controls (no symbol). Error bars indicate standard error. 18 of the 22 complete responders (50% of treated rats) were completely cured of all primary and metastatic tumors and went on to live a normal life span; C. photographic comparison of tumors in an untreated control animal (left-hand column), a treated animal with limited response (center column), and an animal that was ultimately cured (right-hand column) on day 8 (top row), day 16 (middle row), and day 23 (bottom row) after oxaliplatin treatment followed 24 h later by fever-range whole body thermal therapy. Arrows point to the primary tumor (P) and an inguinal lymph node metastasis (IM); *indicates remodeling and ulceration of the progressing primary tumor on day 16 in the control rat, while ** illustrates how the primary tumor and inguinal metastasis in the control rat have merged by day 23, the day of death; # in the limited responder’s day 23 image denotes regrowth of the initially responding inguinal metastasis at the same time as regression of the primary tumor. In the bottom right image, N indicates the nipple, now visible thanks to substantial regression of the primary tumor and inguinal metastasis by day 23 (complete disappearance of tumors in cured animals typically occurred around day 30).
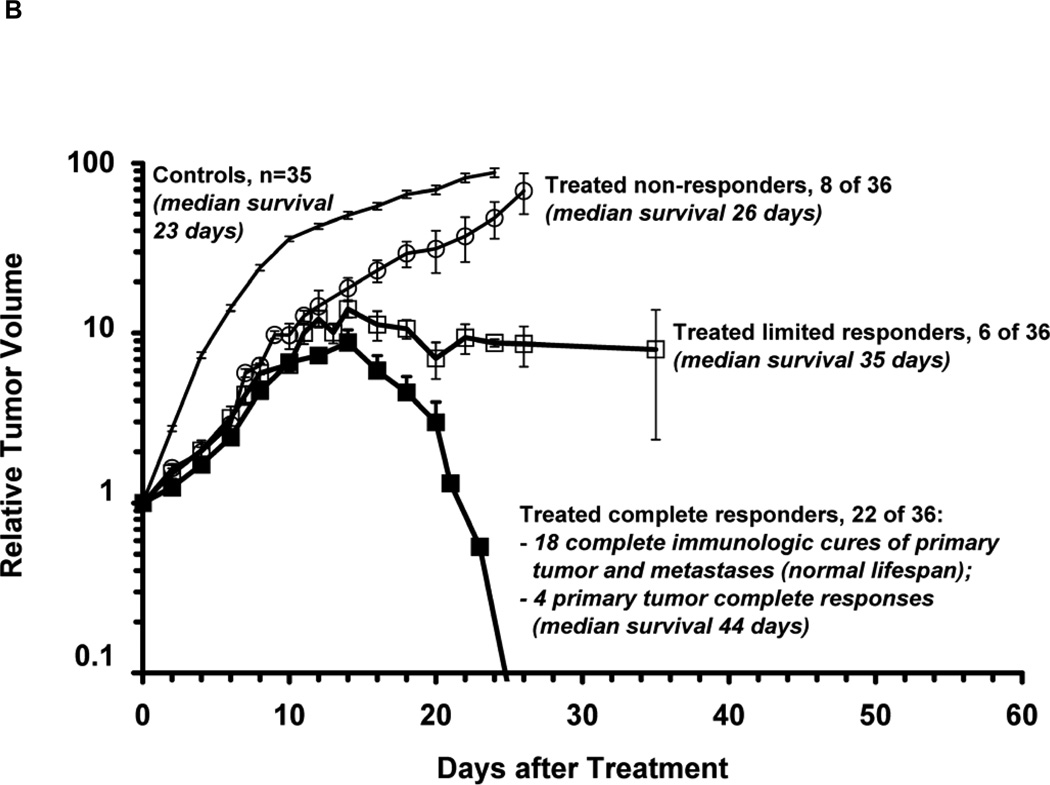
Panel 3B plots the average tumor response in a series of six experiments conducted over a period of three years in which animals were treated with 10 mg/kg oxaliplatin followed 24 hours later by 6h of fever-range whole body thermal therapy at 40°C. In all treated animals there was an initial growth inhibition compared to controls but in 8 of the 36 treated animals (22%) rapid tumor growth resumed after day 4 and the animals went on to die of their tumors between day 22 and 30 after oxaliplatin treatment (NR). Another 6 animals (17%) displayed a limited response (LR) in which tumor growth slowed again after day 10 and there was tumor regression or control for some time, leading to increased survival compared to control animals (median survival = 35 days, see Table 1). However, in 22 of the 36 treated animals (61%) a late slowing of tumor growth around day 10 was followed by complete regression of the primary tumors, although 4 animals (11%) later succumbed to metastases after an average survival of 50 days post-treatment. The other 18 animals (50%; from 33% – 67% in any single experiment with 6 animals) were completely cured of all primary and metastatic tumors and lived out an essentially normal life-span. These animals were immune to multiple up to 4) re-challenges with MTLn3 cells yet grew a control tumor (glioblastoma), suggesting a complete tumor-specific immunologic cure. Figure 3C illustrates representative tumor appearance in situ on days 8, 15, and 22 after oxaliplatin administration in a control animal, a treated animal that didn’t respond beyond early growth suppression, and an animal that went on to be cured.
Table I. Treatment outcome after oxaliplatin given 24 h before fever-range whole body thermal therapy.
Treatment outcome measures of 36 rats treated with oxaliplatin 24 hours before fever-range whole body thermal therapy: maximum relative tumor volume, median, and mean survival in controls, non-responder (NR), limited responder (LR), complete responder (CR), and cured rats.
| Group, Outcome | Number (% of treated) |
Maximum relative tumor volume (average for group) |
Median Survival (days [range]) |
Mean Survival (days) |
|---|---|---|---|---|
| Untreated controls | 35 | 91.6 | 23 [19–30] | 24 |
| Treated, non-responders (NR) | 8 (22%) | 51.4§ | 26 [21–30] | 27 |
| Treated, limited responders (LR) |
6 (17%) | 15.2§§ | 35 [25–41] | 33§ |
| Treated, complete responders (CR) |
4 (11%) | 17.3§§ | 44 [26–84] | 50§ |
| Treated, cures | 18 (50%) | 8.5§§ | 588 [224–729]* | 588§§,^ |
p<0.05,
p<0.00001 compared to controls,
7 rats are still alive
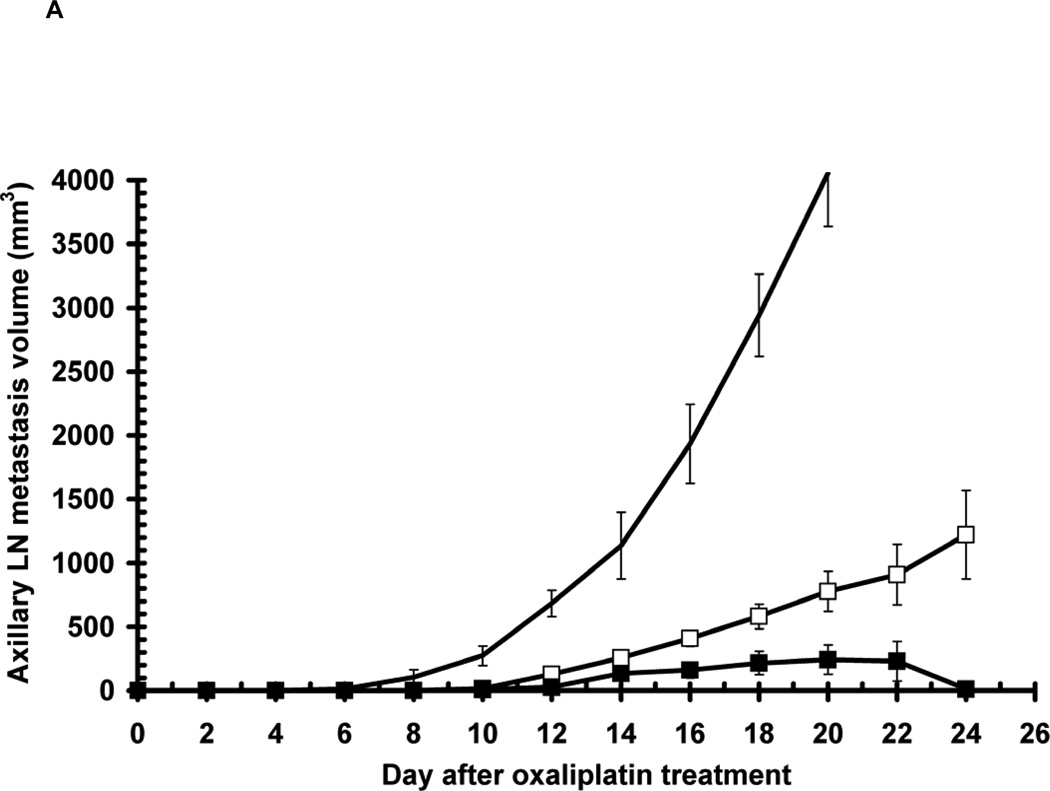
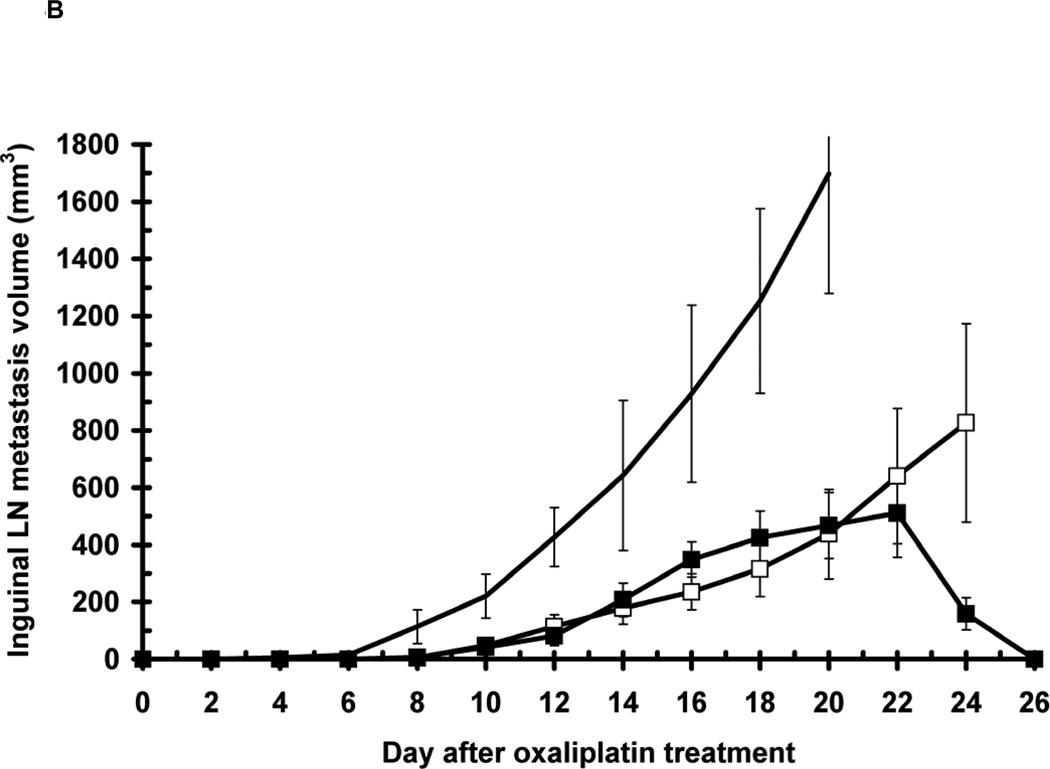
Oxaliplatin thermochemotherapy was also effective against metastases that appeared after treatment as seen in Figure 4. Axillary and inguinal metastases were completely eliminated in animals cured by oxaliplatin 24h before FR-WB-TT. In animals that weren’t cured, both axillary and inguinal metastases appeared later, and grew more slowly, than in rats treated with oxaliplatin alone. The median day on which inguinal metastases first could be measured was day 6, 8, and 10, respectively in control, oxaliplatin, and oxaliplatin 24h before FR-WB-TT groups, while axillary metastases were first seen on median day 7, 11, and 13, respectively. Even in the uncured animals, metastases began to regress late after treatment, around day 20 – 22, much like the primary tumors. In contrast, in animals treated with oxaliplatin alone, both axillary and inguinal metastases grew steadily until the animal’s death, albeit at a slower rate than in controls.
Figure 4.
Metastatic tumor growth in uncured animals in a representative experiment: controls (no symbol, n=6), 10 mg/kg oxaliplatin (○, n=5), 10 mg/kg oxaliplatin 24 h before FR-WB-TT (■, n=3). A. axillary metastases; B. inguinal metastases Error bars represent standard error.
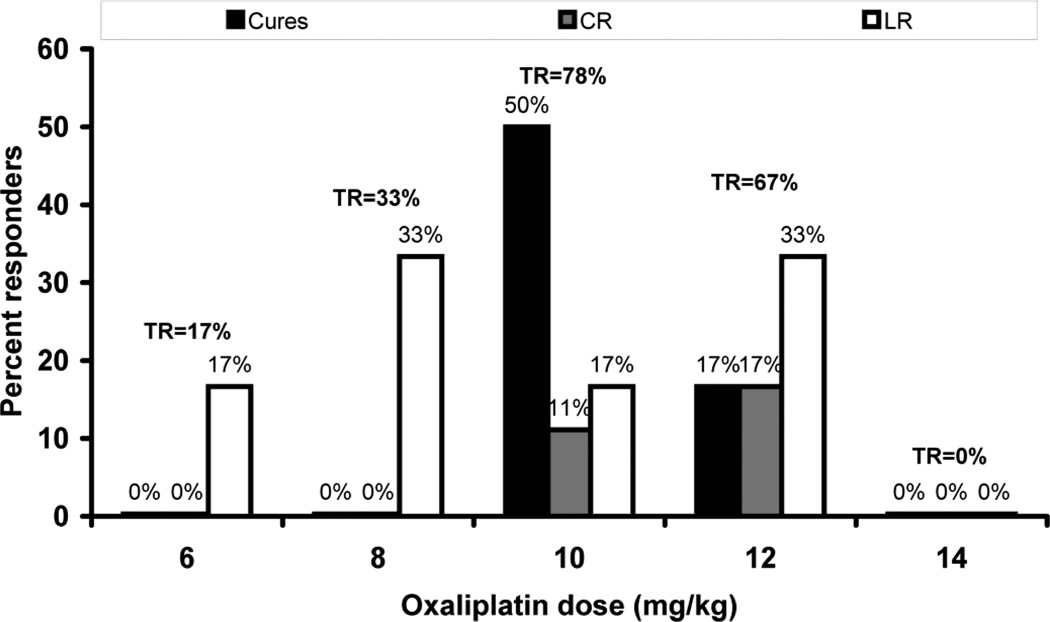
As shown in Figure 5, the number of curative and complete responses was highly dose-dependent. Cures occurred only at 10, and 12 mg/kg of oxaliplatin administered 24h before thermal therapy, with the highest cure rate resulting from 10 mg/kg. Similarly, complete responses were observed at an oxaliplatin dose of 10 and 12 mg/kg only. At 6 and 8 mg/kg there were only a few partial responses, while at 14 mg/kg, close to the MTD dose, there were no responses at all.
Figure 5.
Dependence of tumor response on dose of oxaliplatin given 24 hours before fever-range whole body thermal therapy. Percent limited responses (LR, white bars), complete responses (CR, grey bars) and cures (black bars) are shown for each of 5 doses: 6, 8, 10, 12, and 14 mg/kg (n = 6, 8, 36, 8, 6 respectively). Total response, TR = cures + CR + LR.
The efficacy of oxaliplatin combined with fever-range whole body thermal therapy was also dependent on the schedule of administration of the drug with respect to the thermal therapy. Table II compares the survival and cure rate of rats treated with various relative timings of oxaliplatin with respect to thermal therapy to survival with oxaliplatin alone and in untreated control animals. 10 mg/kg oxaliplatin given 12h and 24h before thermal therapy resulted in a significant increase in median survival over controls, and compared to oxaliplatin alone, with 50% of rats being cured and living out a normal life-span. There was one cure in the 10 mg/kg oxaliplatin alone group, but the other 5 rats had an average survival only 15% greater than controls (not significant), much shorter than rats receiving the drug 12 or 24 h before thermal therapy.
Table II. Survival and toxicity measures for different schedules of oxaliplatin thermochemotherap.
Survival and toxicity measures from two experiments for different schedules of oxaliplatin thermochemotherapy: average median survival, percent cures, maximum body weight loss, and decrease in hematocrit to nadir for rats treated with fever-range whole body thermal therapy before, simultaneously with, and after oxaliplatin. The doseof oxaliplatin was either 10 mg/kg or 12 mg/kg.
| Group/Schedule | Median survival (days) |
Cured %) |
Maximum body weight loss (%) |
Decrease in hematocrit to nadir (%) |
|---|---|---|---|---|
| Untreated controls1,2 | 23, 27 | 0 | 14.1, 15.2 | 29.01 |
| FR-WB-TT1 | 27 | 0 | 14.2 | 22.9 |
| OX + FR-WB-TT simultaneously1 | 28 | 0 | 12.2 | 22.0 |
| Oxaliplatin (10 mg/kg)2 | 29.5 | 17 | 12.5 | |
| Oxaliplatin (12 mg/kg)1 | 31.5 | 0 | 9.9§ | 13.2 |
| Oxaliplatin 3h before FR-WB-TT2 | 28 | 0 | 13.5 | |
| Oxaliplatin 12h before FR-WB-TT2 | 225§ | 50 | 5.6§§§,* | |
| OX 24h before FR-WB-TT(10 mg/kg)2 | 309.5§,* | 50 | 6.0§§§,* | |
| OX 24h before FR-WB-TT(12 mg/kg)1 | 37§ | 17 | 7.9§§§,* | 4.2§§, ** |
| OX 24h after FR-WB-TT1 | 28.5 | 0 | 15.2 | 8.2§,* |
Data presented from two experiments:
experiment 1, 12 mg/kg oxaliplatin;
experiment 2, 10 mg.kg oxaliplatin
p < 0.05,
p < 0.001,
p < 0.0001 vs. control;
p < 0.05;
p < 0.01 vs. OX alone
Not only was anti-tumor efficacy and survival schedule-dependent, but so also was toxicity. Table II gives three measures of toxicity after various schedules of oxaliplatin thermochemotherapy: nadir body weight loss, nadir hematocrit decrease, and change in white blood cell number (as indicated by the Buffy coat thickness) between day 8 and 15 after treatment. Oxaliplatin given 24 hours before thermal therapy resulted in the least body weight loss, the least decrease in hematocrit, and the greatest increase in white blood cell count of all the tested schedules.
Discussion
Oxaliplatin forms intra-strand platinum-DNA adducts that induce a number of signal transduction pathways leading to apoptosis [36]. Enhanced oxaliplatin efficacy against ovarian carcinoma cells following 1h of concurrent, moderate, 42°C hyperthermia, along with increased G2/M arrest has been reported [37]. Our in vitro data indicate that 40°C heat increases the sensitivity of MTLn3 tumor cells to oxaliplatin by increasing intracellular uptake of platinum and formation of platinum adducts. Since the ratio of platinum adducts to intracellular platinum remained unchanged after heating (Figure 1) it would appear that heat did not increase the reaction rate between platinum and DNA, rather that the increased adduct formation was due to a thermally induced increase in cellular drug uptake, presumably because of increased cell permeability. Heat-induced, and exposure-related, increases in cell membrane permeability have been reported at temperatures as low as 40°C [38]. Increased nanoparticle extravasation from tumor vasculature in response to loco-regional and fever-range hyperthermia have also been reported [39, 40]. Even greater cellular uptake of oxaliplatin, and consequent tumor cytotoxicity, is to be expected from thermal therapy in vivo. Hyperthermia may also inhibit repair of DNA adducts.
The remarkable tumor responses observed in vivo as illustrated in Figure 3 cannot, however, be explained by increased drug uptake and heat augmentation of drug action alone. The late tumor regression observed in so many of the rats treated with oxaliplatin 24 h before FR-WB-TT, together with the inability of cured rats to grow tumors even when re-challenged multiple times with the same tumor type, suggests an immune response that led to formation of memory T-cells. The cured animals that were re-challenged with MTLn3 tumor cells displayed marked skin reactivity on days 3–5 after inoculation, also indicative of an immune response. There was also a significant difference in peripheral white blood cell count between responders and non-responders. Furthermore, our preliminary data from ongoing flow cytometry and immunoblot studies suggest that (i) while in vitro stimulation of peripheral blood mononuclear cells with irradiated MTLn3 tumor cells results in a marked increase in the number of CD8+ cells in both cured rats and limited responders compared to controls with progressing tumors, the number of CD25-expressing CD8+, i.e. functionally activated, T-cells increases only in cured rats; and (ii) lymphocytes extracted from peripheral blood of cured animals and stimulated with irradiated MTLn3 cells show interferon-γ activity. The precise mechanism of immune activation has yet to be elucidated, but we hypothesize that oxaliplatin-induced cell kill, largely by apoptosis, causes tumor antigen cross-presentation to dendritic cells. Thermal stimulation of both dendritic and NK cells [18,19], and possible down-regulation of regulatory T-cells [41], may additionally lead to an increased anti-tumor response. Additional immunotherapy might result in an even higher cure rate.
Tumors in all the treated animals followed the same initial growth pattern with some growth inhibition on days 2–4, followed by tumor re-growth (Figure 3a). Regression of responding tumors did not begin until around day 10 and tumor cure or complete response could only be distinguished on the basis of tumor volume after about day 16. Indeed, the first sign of long-term response was generally a gain in the animal’s weight beginning around day 12. Similarly late responses with oxaliplatin in both a fibrosarcoma and a pancreas cancer model, and with gemcitabine in the MTLn3 model, have been seen. Despite the initial tumor growth inhibition, there was no significant survival advantage of animals treated with oxaliplatin alone, or those thermochemotherapy-treated non-responders. While limited responders had only slightly increased survival, the sustained tumor growth inhibition throughout their remaining life, and their reduced maximum tumor volume (Table I), likely translated into an improved quality of life. Complete responders had durable regression of their primary tumors, but like the majority of advanced cancer patients, ultimately succumbed to metastases. Notably, 78% of the rats were cured, complete responders, or limited responders, a substantially higher response rate than observed with other heat-interactive chemotherapy agents, perhaps due to the particular immunogenicity of oxaliplatin cell death [29]. Since the studies reported here, we have been using the clinical formulation of oxaliplatin (Eloxatin, Sanofi Aventis) and continue to see a consistently high cure rate, in one experiment as high as 83%.
Also important is the effect of thermochemotherapy on the subsequent appearance and course of metastases. Metastasis appearance was delayed after oxaliplatin 24h before FR-WB-TT compared to oxaliplatin alone. Cured animals completely regressed their metastases as well as their primary tumors. Notably, both inguinal and axillary metastasis volume was lower in uncured animals treated with oxaliplatin 24h before FR-WB-TT than in those animals treated with oxaliplatin alone (Figure 4). Delayed incidence of metastases has also been reported for irinotecan combined with fever-range whole body thermal therapy [34]. Control of metastatic disease is extremely important for increased survival, and also determines quality of life.
The dose of oxaliplatin administered prior to thermal therapy is critically important to outcome. Cures and complete responses occurred only within a narrow window of doses, between 70% and 85% of the maximally tolerated dose (MTD). At lower doses, around 40–60% of MTD) little acute tumor growth delay, no long term responses, and no cures occurred (Figure 5). When the dose approached the MTD, despite significant short term tumor growth arrest, no animals had long term tumor responses. We hypothesize that sufficient tumor cell kill by oxaliplatin is required for effective antigen cross-presentation, but that too high a drug dose, while resulting in initial tumor killing or growth arrest, also kills many antigen-presenting and immune effector cells and thus disables a curative immune response, leading to rapid, fatal, tumor re-growth. Multiple low dose chemotherapy treatments, as in metronomic therapy, may, cumulatively, be sufficiently tumoricidal to initiate an immune response.
The relative timing of thermal therapy with respect to oxaliplatin is very important for anti-tumor efficacy (Table II), as has been observed with other chemotherapy agents [11, 12, 13]. When 10 mg/kg oxaliplatin was administered simultaneously with, or after, thermal therapy the tumor response and survival was no different than with oxaliplatin alone. Similarly, oxaliplatin given 3h or 48 hours before thermal therapy was no more effective than oxaliplatin alone. However, when oxaliplatin was given 12 or 24 hours before thermal therapy there was significantly increased survival and 50% of the animals were completely cured. The need for a substantial delay between oxaliplatin treatment and subsequent thermal therapy is consistent with the hypothesis that oxaliplatin-induced cell cycle arrest and tumor cell death initiates an immune stimulus that is then augmented by thermal therapy to cause substantial tumor responses. While platinum-DNA adducts form immediately after oxaliplatin administration, induction of apoptosis is a later event following S phase delay and G2/M phase arrest [42, 43]. Cisplatin-induced apoptosis of MTLn3 cells has been detected 16 hours after treatment [44], but as oxaliplatin-DNA adducts are more efficient at producing irreparable cellular damage than cisplatin, oxaliplatin-induced apoptosis may occur sooner. Actually, full progression to apoptosis may not be necessary to initiate immune activation since damage response-associated expression of NKG2D receptor ligand may decrease regulatory T-cells enough to expand the effector cell population [45], and/or increased expression of cyclins during G2/M arrest may act as tumor antigens [46].
T-cell activation follows pro-inflammatory maturation signals (here presumably heat-induced), and efficient T-cell cross-priming requires fully mature dendritic cells [18, 19]; dendritic cell maturation in vivo can take 7–10 days [18, 47]. Activation of T-cells after satisfactory contact with primed dendritic cells [48] is then a rapid process of a few hours [49]. The tumor responses reported here, typically occurring around day 14–16 after oxaliplatin treatment, but occasionally much later, are consistent with T-cell activation following a prolonged period of dendritic cell maturation after drug-induced tumor cell death. Interestingly, the kinetics of our curative tumor response are virtually identical to those of Kelly et al. following NK cell-mediated tumor rejection [50] which may argue towards a significant contribution of NK cells. Stimulation of NK cell activity after fever-range thermal therapy has been reported [51, 19].
Not only did oxaliplatin thermochemotherapy result in impressive anti-tumor responses, but toxicity was also reduced in comparison to oxaliplatin alone. A decline in body weight was observed over several weeks after treatment in all groups including controls, suggesting that weight loss was due to increasing tumor burden rather than toxicity of the treatment itself. In treated animals, body weight reached a nadir, usually between days 7 and 14, increasing again sooner rather than later with the more efficacious treatments. The changes in body weight shown in Table II appear to correlate inversely with treatment efficacy, i.e. reflect decreased tumor burden. Indeed, increasing body weight was generally the first sign when treatment led to a complete response or cure. The least weight loss of all the schedules was observed for oxaliplatin followed 24 hours later by thermal therapy. Hematocrit, which also decreases to a nadir after chemotherapy, fell significantly less when oxaliplatin preceded hyperthermia than after oxaliplatin alone and in controls.
Given the impressive tumor responses obtained with oxaliplatin thermochemotherapy, along with the acceptable toxicity, and the fact that several clinical protocols have already been successfully translated from promising pre-clinical results in this clinically relevant tumor model, oxaliplatin combined with fever-range whole body thermal therapy can be expected to form the basis of a superior clinical treatment protocol for advanced metastatic cancers. Furthermore, the concept of harnessing the innate immune system through lower-than-MTD chemotherapy combined with immune-enhancing therapy such as thermal therapy, suggests a new paradigm for treatment of patients with cancer that could change clinical practice. The goal of complete cures, or at least significantly extended survival along with improved quality of life following treatment, may no longer be so elusive.
Conclusion
Mild heating in vitro of MTLn3 tumor cells exposed to oxaliplatin increased tumor cell kill through increased uptake of oxaliplatin by tumor cells and subsequent formation of oxaliplatin-DNA adducts. In vivo, in an animal model that closely parallels rapidly progressing inflammatory human breast cancer, fever-range whole body thermal therapy combined with properly dosed and scheduled oxaliplatin chemotherapy consistently achieved a hitherto unseen level of tumor responses, delayed appearance and slowed growth of metastases, reduced toxicity, and increased survival. Complete, durable, immunologic, cures were achieved in 50% of animals. A further 11% of animals completely regressed their primary tumors although they ultimately succumbed to metastases, and 17% showed limited tumor responses. Fever-range thermal therapy, when optimally timed with respect to correctly dosed oxaliplatin chemotherapy, appears to augment the immune response to drug-induced cell death sufficiently to result in tumor cures. Thermochemotherapy with sub-MTD oxaliplatin and fever-range whole body thermal therapy therefore holds great potential as a safe and effective clinical treatment against advanced, metastatic cancer.
Acknowledgements
The authors gratefully acknowledge the support of research grants from the National Institutes of Health, the Susan G. Komen Breast Cancer Foundation, and Sanofi-Aventis.
Financial support:
The work reported was supported from the following sources:
NIH grant CA 43090
(Bull JMC, Deng W, Proett, J, Rowe RW, Strebel F);
Susan G. Komen Foundation Research Grant, 2006–2007 cycle
(Bull JMC, Chan D, Rowe RW, Strebel F);
NIH grant CA127263
(Siddik ZH, He G);
Sanofi-Aventis research grant
(Bull JMC, Deng W, Rowe RW, Strebel F);
The University of Texas Hyperthermia Research Laboratory Miscellaneous Donors Fund
(Chan D, Deng W, Rowe RW, Strebel F).
References
- 1.Kampinga HH. Cell biological effects of hyperthermia alone or combined with radiation or drugs: a short introduction to newcomers in the field. Int J Hyperthermia. 2006;22(3):191–196. doi: 10.1080/02656730500532028. [DOI] [PubMed] [Google Scholar]
- 2.Hehr T, Wust P, Bamberg M, Budach W. Current and potential role of thermoradiotherapy for solid tumours. Onkologie. 2003;26:295–302. doi: 10.1159/000071628. [DOI] [PubMed] [Google Scholar]
- 3.Rowe RW. Hyperthermia, Systemic. In: Webster JG, editor. Encyclopedia of Medical Devices and Instrumentation. 2nd ed. New York: Wiley; 2006. p. p57. (Table 6) [Google Scholar]
- 4.Matsuda H, Strebel FR, Kaneko T, Danhauser LL, Jenkins GN, Toyota N, Bull JM. Long duration-mild whole body hyperthermia of up to 12 hours in rats: feasibility, and efficacy on primary tumour and axillary lymph node metastases of a mammary adenocarcinoma: implications for adjuvant therapy. Int J Hyperthermia. 1997;13:89–98. doi: 10.3109/02656739709056433. [DOI] [PubMed] [Google Scholar]
- 5.Yamada Y, Itoh Y, Aoki S, et al. Preliminary results of M-VAC chemotherapy combined with mild hyperthermia, a new therapeutic strategy for advanced or metastatic transitional cell carcinoma of the urothelium. Cancer Chemother Pharmacol. 2009;64:1079–1083. doi: 10.1007/s00280-009-0964-2. [DOI] [PubMed] [Google Scholar]
- 6.Sakaguchi Y, Makino M, Kaneko T, et al. Therapeutic efficacy of long duration-low temperature whole body hyperthermia when combined with tumor necrosis factor and carboplatin in rats. Cancer Res. 1994;54:2223–2227. [PubMed] [Google Scholar]
- 7.Toyota N, Strebel FR, Stephens LC, Matsuda H, Bull JM. Long-duration, mild whole body hyperthermia with cisplatin: tumour response and kinetics of apoptosis and necrosis in a metastatic rat mammary adenocarcinoma. Int J Hyperthermia. 1997;13(5):497–506. doi: 10.3109/02656739709023548. [DOI] [PubMed] [Google Scholar]
- 8.Nagle V, Berry J, Bull JM. Whole body hyperthermia with carboplatin (CBDCA) for treatment of advanced or metastatic GI adenocarcinomas. Proc Am Assoc Ca Res. 1999;40:345. [Google Scholar]
- 9.Bull JM, Scott GL, Nagle VL, Strebel FR, Koch SM. Phase I study of long-duration, low-temperature whole-body hyperthermia (LL-WBH) with liposomal doxorubicin (Doxil-5-fluorouracil (5-FU), & interferon-a (IFN-a) Proc Am Soc Clin Oncol. 2002;21 (abstract). [Google Scholar]
- 10.Bull JM, Scott GL, Strebel FR, et al. Fever-range whol-body thermal therapy combined with cisplatin, gemcitabine, and daily interferon-alpha: a description of a phase I–II protocol. Int J Hyperthermia. 2008;24:649–662. doi: 10.1080/02656730802104740. [DOI] [PubMed] [Google Scholar]
- 11.Baba H, Siddik ZH, Strebel FR, Jenkins GN, Bull JM. Increased therapeutic gain of combined cis-diamminedichloroplatinum (II) and whole body hyperthermia therapy by optimal heat/drug scheduling. Cancer Res. 1989;49(24 Pt 1):7041–7044. [PubMed] [Google Scholar]
- 12.Strebel FR, Sumiyoshi K, Jenkins GN, Rowe RW, Bull JMC. Drug sequence effect on therapeutic outcome (tumor growth, toxicity, and survival) of Irinotecan combined with Epirubicin in the in vivo MTLn3 rat mammary adenocarcinoma. Proc Amer Assoc Cancer Res. 2002;43:587. [Google Scholar]
- 13.Bull JMC, Strebel FR, Jenkins GN, Deng W, Rowe RW. The importance of schedule in whole body thermochemotherapy. Int J Hyperthermia. 2008;24:171–181. doi: 10.1080/02656730701883212. [DOI] [PubMed] [Google Scholar]
- 14.Skitzki JJ, Repasky EA, Evans SS. Hyperthermia as an immunotherapy strategy for cancer. Curr Opin Investig Drugs. 2009;10:550–558. [PMC free article] [PubMed] [Google Scholar]
- 15.Zhang H-G, Mehta K, Cohen P, Guha C. Hyperthermia on immune regulation: A temperature’s story. Cancer Letters. 2008;271:191–204. doi: 10.1016/j.canlet.2008.05.026. [DOI] [PubMed] [Google Scholar]
- 16.Tulapurkar ME, Asiegbu BE, Singh IS, Hasday JD. Hyperthermia in the febrile range induces HSP72 expression proportional to exposure temperature but not to HSF-1 DNA-binding activity in human lung epithelial A549 cells. Cell Stress Chaperones. 2009;14:499–508. doi: 10.1007/s12192-009-0103-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Murapa P, Gandhapudi S, Skaggs HS, Sarge KD, Woodward JG. Physiological fever temperature induces a protective stress response in T lymphocytes mediated by heat shock factor-1 (HSF1) 2007;179:8305–8312. doi: 10.4049/jimmunol.179.12.8305. [DOI] [PubMed] [Google Scholar]
- 18.Ostberg JR, Repasky EA. Emerging evidence indicates that physiologically relevant thermal stress regulates dendritic cell function. Cancer Immunol Immunother. 2005;55:292–298. doi: 10.1007/s00262-005-0689-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Milani V, Noessner E. Effects of thermal stress on tumor antigenicity and recognition by immune effector cells. Cancer Immunol Immunother. 2005;55:312–319. doi: 10.1007/s00262-005-0052-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chen Q, Fisher DT, Kucinska SA, Wang WC, Evans SS. Dynamic control of lymphocyte trafficking by fever-range thermal stress. Cancer Immunol Immunother. 2006;55:299–311. doi: 10.1007/s00262-005-0022-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zhao W, An H, Zhou J, Xu H, Yu Y, Cao X. Hyperthermia differentially regulates TLR4 and TLR2-mediated innate immune response. Immunol Let. 2007;108:137–142. doi: 10.1016/j.imlet.2006.11.008. [DOI] [PubMed] [Google Scholar]
- 22.Van der Most RG, Currie AJ, Robinson BWS, Lake RA. Decoding dangerous cell death: how cytotoxic chemotherapy invokes inflammation, immunity, or nothing at all. Cell Death and Differentiation. 2008;15:13–20. doi: 10.1038/sj.cdd.4402255. [DOI] [PubMed] [Google Scholar]
- 23.Tesniere A, Panaretakis T, Kepp O, et al. Molecular characteristics of immunogenic cancer cell death. Cell Death and Differentiation. 2008;15:3–12. doi: 10.1038/sj.cdd.4402269. [DOI] [PubMed] [Google Scholar]
- 24.Ullrich E, Bonmort M, Mignot G, Kroemer G, Zitvogel L. Tumor stress, cell death, and the ensuing immune response. Cell Death and Differentiation. 2008;15:21–28. doi: 10.1038/sj.cdd.4402266. [DOI] [PubMed] [Google Scholar]
- 25.Kepp O, Tesniere A, Zitvogel L, Kroemer G. The immunogenicity of tumor cell death. Current Opin Oncol. 2009;21:71–76. doi: 10.1097/CCO.0b013e32831bc375. [DOI] [PubMed] [Google Scholar]
- 26.Shurin GV, Tourkova IL, Kaneno R, Shurin MR. Chemotherapeutic Agents in Noncytotoxic Concentrations Increase Antigen Presentation by Dendritic Cells via an IL-12-Dependent Mechanism. The Journal of Immunology. 2009;183:137–144. doi: 10.4049/jimmunol.0900734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tesniere A, Schlemmer F, Boige V, Kepp O, Martins I, Ghiringhelli F, Aymeric L, Michaud M, Apetoh L, Barault L, Mendiboure J, Pignon JP, Jooste V, van Endert P, Ducreux M, Zitvogel L, Piard F, Kroemer G. Immunogenic death of colon cancer cells treated with oxaliplatin. Oncogene. 2010;29:482–491. doi: 10.1038/onc.2009.356. [DOI] [PubMed] [Google Scholar]
- 28.Raymond E, Faivre S, Chaney S, Woynarowsky J, Cvitkovic E. Cellular and molecular pharmacology of oxaliplatin. Mol Cancer Ther. 2002;1:227–235. [PubMed] [Google Scholar]
- 29.Apetoh L, Tesniere A, Ghiringhelli F, Kroemer G, Zitvogel L. Molecular Interactions between Dying Tumor Cells and the Innate Immune System Determine the Efficacy of Conventional Anticancer Therapies. Cancer Research. 2008;68:4026–4030. doi: 10.1158/0008-5472.CAN-08-0427. [DOI] [PubMed] [Google Scholar]
- 30.Dong XE, Ito N, Lotze MT, et al. High mobility group box I (HMGB1) release from tumor cells after treatment: implications for development of targeted chemoimmunotherapy. J Immunother. 2007;30:596–606. doi: 10.1097/CJI.0b013e31804efc76. [DOI] [PubMed] [Google Scholar]
- 31.Matsuda H, Strebel FR, Kaneko T, et al. Apoptosis and necrosis occurring during different stages of primary and metastatic tumor growth of a rat mammary adenocarcinoma. Anticancer Res. 1996;16:1117–1122. [PubMed] [Google Scholar]
- 32.Siddik ZH, Boxall FE, Harrap KR. Flameless atomic absorption spectrophotometric determination of platinum in tissues solubilized in hyaminehydroxide. Anal Biochem. 1987;163:21–26. doi: 10.1016/0003-2697(87)90087-x. [DOI] [PubMed] [Google Scholar]
- 33.Neri A, Welch D, Kawaguchi T, Nicolson GL. Development and biologic properties of malignant cell sublines and clones of a spontaneously metastasizing rat mammary adenocarcinoma. J. Natl Cancer Inst. 1982;68:507–517. [PubMed] [Google Scholar]
- 34.Sumiyoshi K, Strebel FR, Rowe RW, Bull JM. The effect of whole-body hyperthermia combined with 'metronomic' chemotherapy on rat mammary adenocarcinoma metastases. Intl J Hyperthermia. 2003;19(2):103–118. doi: 10.1080/0265673021000017091. [DOI] [PubMed] [Google Scholar]
- 35.Wondergem J, Siddik ZH, Strebel FR, Bull JM. Effect of whole body hyperthermia on cis-diamminedichloroplatinum (II)-induced antitumour activity and tissue Pt-distribution: do anaesthetics influence the therapeutic ratio? Eur J Cancer. 1993;29A(4):549–554. doi: 10.1016/s0959-8049(05)80149-2. [DOI] [PubMed] [Google Scholar]
- 36.Nehmé A, Baskaran R, Nebel S, et al. Induction of JNK and c-Abl signalling by cisplatin and oxaliplatin in mismatch repair-proficient and -deficient cells. Brit J Cancer. 1999;79:1104–1110. doi: 10.1038/sj.bjc.6690176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Atallah D, Marsaud V, Radanyi, et al. Thermal enhancement of oxaliplatin-induced inhibition of cell cycle progression in human carcinoma cell lines. Int J Hyperthermia. 2004;20:405–419. doi: 10.1080/02656730310001637325. [DOI] [PubMed] [Google Scholar]
- 38.Bischof JC, Padanilam WH, Holmes RM, et al. Dynamics of cell membrane permeability changes at supraphysiological temperatures. Biophys J. 1995;68:2608–2614. doi: 10.1016/S0006-3495(95)80445-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kong G, Braun RD, Dewhirst MW. Characterization of the effect of hyperthermia on nanoparticle extravasation from tumor vasculature. Cancer Res. 2001;61:3027–3032. [PubMed] [Google Scholar]
- 40.Rowe RW, Strebel FR, Sumiyoshi K, Kirpotin DB, Bull JMC. Time-course of liposome uptake in MTLn3 tumors and normal tissue with and without whole body hyperthermia. Proc. American Assoc Cancer Res. 2002;43:417. (abstract) [Google Scholar]
- 41.Terunuma H, Wada A, Deng X, et al. Mild Hyperthermia Modulates the Relative Frequency of Lymphocyte Cell Subpopulations: an Increase in a Cytolytic NK Cell Subset and a Decrease in a Regulatory T Cell Subset. Thermal Med (Jap J Hyperthermic Oncol) 2007;23:41–47. [Google Scholar]
- 42.William-Faltaos S, Rouillard D, Lechat P, Bastian G. Cell cycle arrest by oxaliplatin on cancer cells. Fundam Clin Pharmacol. 2007;21:165–172. doi: 10.1111/j.1472-8206.2007.00462.x. [DOI] [PubMed] [Google Scholar]
- 43.Toscano F, Parmentier B, El Fajoui Z, et al. p53 dependent and independent sensitivity to oxaliplatin of colon cancer cells. Biochem Pharmacol. 2007;74:392–406. doi: 10.1016/j.bcp.2007.05.001. [DOI] [PubMed] [Google Scholar]
- 44.van Nimwegen MJ, Huigsloot M, Camier A, Tijdens IB, van de Water B. Focal Adhesion Kinase and Protein Kinase B Cooperate to Suppress Doxorubicin-Induced Apoptosis of Breast Tumor Cells. Mol Pharmacol. 2006;70:1330–1339. doi: 10.1124/mol.106.026195. [DOI] [PubMed] [Google Scholar]
- 45.Gasser S, Raule DH. The DNA Damage Response Arouses the Immune System. Cancer Res. 2006;66:3959–3962. doi: 10.1158/0008-5472.CAN-05-4603. [DOI] [PubMed] [Google Scholar]
- 46.Egloff AM, Vella LA, Oliver JF. Cyclin B1 and Other Cyclins as Tumor Antigens in Immunosurveillance and Immunotherapy of Cancer. Cancer Res. 2006;66:6–9. doi: 10.1158/0008-5472.CAN-05-3389. [DOI] [PubMed] [Google Scholar]
- 47.Camporeale A, Boni A, Iezzi G, et al. Critical Impact of the Kinetics of Dendritic Cells Activation on the in Vivo Induction of Tumor-specific T Lymphocytes. Cancer Res. 2003;63:3688–3694. [PubMed] [Google Scholar]
- 48.Bousso P, Robey E. Dynamics of CD8+ T cell priming by dendritic cells in intact lymph nodes. Nature Immunol. 2003;4:579–585. doi: 10.1038/ni928. J Immunol 1988; 140.4079–4082. [DOI] [PubMed] [Google Scholar]
- 49.Roosnek E, Demotz S, Corradin G, Lanzavecchia A. Kinetics of MHC-antigen complex formation on antigen-presenting cells. [PubMed] [Google Scholar]
- 50.Kelly JM, Darcy PK, Markby JL, et al. Induction of tumor-specific T cell memory by NK cell-mediated tumor rejection. Nat Immunol. 3:83–90. doi: 10.1038/ni746. 200. [DOI] [PubMed] [Google Scholar]
- 51.Dayanc BE, Beachy SH, Ostberg JR, Repasky EA. Dissection the role of hyperthermia in natural killer cell mediated anti-tumor responses. Int J Hyperthermia. 2008;24:41–56. doi: 10.1080/02656730701858297. [DOI] [PubMed] [Google Scholar]