Abstract
Acute kidney injury (AKI) is a common complication in cirrhotic patients. Serum creatinine is a poor biomarker for detection of renal impairment in cirrhotic patients. This study aimed to evaluate urinary neutrophil gelatinase-associated lipocalin (NGAL) and urinary interleukin-18 (IL-18) as early biomarkers of acute kidney injury in cirrhotic patients. 160 patients with cirrhosis admitted to the Liver Units at Zagazig University Hospitals were classified into three groups: (I) nonascitic patients, (II) ascitic patients without renal impairment, and (III) ascitic patients with renal impairment. Patients with renal impairment were further divided into four subgroups: [A] prerenal azotemia, [B] chronic kidney disease (CKD), [C] hepatorenal syndrome (HRS), and [D] acute tubular necrosis (ATN). Significant elevation of both urinary NGAL and urinary IL-18 in cirrhotic patients with renal impairment especially in patients with ATN was observed. Urinary NGAL and urinary IL-18 have the ability to differentiate between AKI types in patients with cirrhosis. This could improve risk stratification for patients admitted to the hospital with cirrhosis, perhaps leading to early ICU admission, transplant evaluation, and prompt initiation of HRS therapy and early management of AKI.
1. Introduction
Egypt was blessed with the River Nile and ancient culture but was deemed with liver diseases. Liver cirrhosis is a common disease in Egypt as Egypt has the highest incidence rate of HCV infection worldwide [1].
Acute kidney injury (AKI) in patients with cirrhosis is common. Up to 20% of hospitalized patients with cirrhosis develop AKI [2] and once AKI occurs, there is a reported fourfold increased risk of mortality [3].
Typically, patients with decompensated liver cirrhosis have significant circulatory dysfunction, which is characterized by a vasodilatory state, lower total peripheral resistance, activated renin-angiotensin-aldosterone system (RAAS), and finally renal arterial vasoconstriction [4].
In cirrhosis, AKI types include prerenal azotemia, hepatorenal syndrome (HRS), and acute tubular necrosis (ATN) with prevalence rates of 68%, 25%, and 33%, respectively, but their effect on mortality risk varies [2]. Unfortunately, these forms of AKI are difficult to distinguish clinically as serum creatinine (sCr), the clinical standard to define kidney function, poorly discriminates AKI type in cirrhosis [5]. Furthermore, various factors can affect serum creatinine in cirrhotic patients such as age, gender, nutritional status, muscle mass, and drug and volume distribution; in addition, deranged hepatic synthesis of the creatine may contribute to impaired creatinine production in liver cirrhosis so utilization of serum creatinine concentration for diagnosing renal dysfunction could be even more unsatisfactory [4].
Recently, in an effort to improve the definition of AKI and to highlight the importance of non-HRS kidney dysfunction in cirrhosis, the Acute Dialysis Quality Initiative (ADQI) and the International Ascites Club (IAC) jointly published a consensus statement regarding AKI classification [6], incorporating the Risk, Injury, Failure, Loss, and End-Stage Disease (RIFLE) and the Acute Kidney Injury Network (AKIN) guidelines. IAC definition of HRS [7] was classified as a specific form of AKI [8].
Management of AKI in the setting of cirrhotic patients depends primarily on the detection of the cause. HRS is treated pharmacologically whereas prerenal azotemia is treated with plasma volume expansion which is not suitable in the management of ATN [9, 10].
Neutrophil-gelatinase-associated lipocalin (NGAL) is a novel biomarker for diagnosing acute kidney injury (AKI). Several studies have demonstrated the utility of early NGAL measurements for predicting the severity and clinical outcomes of AKI [11–14].
In fact, urine interleukin-18 (IL-18) has been shown to serve as an accurate biomarker to differentiate ATN from other etiological factors of renal disease [15]. Moreover, the prognostic role of urine IL-18 has been validated in general patient groups admitted to ICU [16].
Therefore, this study was to assess the ability of urinary NGAL and IL-18 as early biomarkers of AKI in patients with cirrhosis.
2. Patients and Methods
2.1. Study Protocol
This is a cross-sectional study including 160 patients with cirrhosis admitted to the Liver Units at Zagazig University Hospitals from July 2012 to December 2012 with history of follow-up in outpatient clinics. The majority of patients were hospitalized for treatment of complications of cirrhosis. Exclusion criteria include (1) patients with hepatocellular carcinoma or cholangiocarcinoma, (2) liver transplant patients, (3) chronic kidney diseases patients maintained on regular hemodialysis before admission, and (4) kidney transplant patients.
The study design was approved by an Institutional Review Board (IRB) of Faculty of Medicine, Zagazig University. Patients included in the study gave informed written consent in accordance with the Declaration of Helsinki.
Clinical and biochemical data were collected at the time of admission to Liver Units at Zagazig University Hospitals with reference to previous patients' data done in outpatient clinics. Child-Pugh score and MELD score were calculated for admission [17, 18]. Estimated GFR was calculated using MDRD equation [19]. A fresh urine sample was taken to measure the urinary levels of sodium, creatinine, NGAL, and IL-18. Venous blood samples were drawn from all participants, and sera were separated immediately.
2.2. Classification of Patients
Patients were classified into three groups: (I) nonascitic patients (n = 42), (II) ascitic patients without renal impairment (n = 50), and (III) ascitic patients with renal impairment (n = 68).
This classification was used because it reflects the different stages of cirrhosis [20]. Patients with renal impairment were further divided into four subgroups: [A] prerenal azotemia, [B] chronic kidney disease (CKD) [21], [C] HRS [7], and [D] ATN [22]. The definitions for these different causes of renal impairment are shown in Section 5.
2.3. Analytic Procedures
Urine samples for NGAL and IL-18 levels were immediately centrifuged, separated, and stored at −80°C until further analysis. Urinary NGAL was measured using a NGAL ELISA kit (BioVendor GmbH, Germany) in relation to urinary creatinine. Urinary IL-18 was measured using a human IL-18 enzyme-linked immunosorbent assay kit (Medical and Biologic Laboratory, Nagoya, Japan) in relation to urinary creatinine.
Routine biochemical parameters were measured by colorimetric methods (Spinreact, SA Ctra, and Santa Coloma, Spain).
2.4. Statistical Analysis
Results are expressed as means ± SD (standard deviation) for continuous variables, while Counts and percentages for categorical variables. Analysis of variance (ANOVA) was used to examine the difference between means of continuous normal-distributed variables.and Chi-square test was used to compare categorical variables. Correlations were evaluated by nonparametric Spearman's correlation. The significance level for all statistical two-tailed tests were accepted as P < 0.05. The statistical analyses were conducted using SPSS for Windows (version 19.0; SPSS Inc., Chicago, IL, USA).
3. Results
3.1. Characteristics of the Patient Population
The demographic, clinical data and biochemical parameters of all patients are shown in Table 1. Patients with renal impairment were divided into the four subgroups as shown in Table 2.
Table 1.
Demographic, clinical, and laboratory data of all patients.
| No ascites (n = 42) | Ascites without impairment of kidney function (n = 50) | Ascites with impairment of kidney function (n = 68) | P | |
|---|---|---|---|---|
| Age (years) | 53.3 ± 9.6 | 54.04 ± 11.03 | 52.95 ± 9.74 | 0.85 |
| Gender, male | 24 (57%) | 30 (60%) | 49 (72%) | 0.21 |
| Etiology of cirrhosis HCV/HBV/others | 32/7/3 | 39/8/3 | 54/10/4 | 0.99 |
| Hepatic encephalopathy, n (%) | 6 (14%) | 19 (38%) | 32 (47%) | 0.004 |
| Gastrointestinal bleeding, n (%) | 7 (16%) | 13 (26%) | 25 (36%) | 0.173 |
| Serum bilirubin (mg/dL) | 2.8 ± 1.76 | 4.4 ± 2.6 | 6.9±4 | 0.0001 |
| Serum albumin (g/L) | 31.5 ± 6.1 | 25.58 ± 3.69 | 27.72 ± 5.61 | 0.0001 |
| Prothrombin time (%) | 67.14 ± 18.4 | 58.18 ± 8.84 | 47.91 ± 15.92 | 0.0001 |
| Serum creatinine (mg/dL) | 0.761 ± 0.19 | 1.045 ± 0.26 | 2.38 ± 0.95 | 0.0001 |
| Glomerular filtration rate (mL/min/1.73 m2) | 119.53 ± 33.57 | 85 ± 21.87 | 45.18 ± 21.28 | 0.0001 |
| Serum sodium (mEq/L) | 135.26 ± 3.8 | 134.92 ± 4.96 | 131.72 ± 6.46 | 0.001 |
| Serum potassium (mEq/L) | 3.979 ± 0.42 | 4 ± 0.54 | 4.39 ± 0.78 | 0.001 |
| Child-Pugh score | 7.48 ± 1.86 | 9.86 ± 1.22 | 10 ± 2 | 0.0001 |
| MELD score | 13.54 ± 3.06 | 16. ± 4.81 | 25.74 ± 7.76 | 0.0001 |
| Mean arterial pressure (mmHg) | 83.76 ± 13.9 | 82.66 ± 15.5 | 77 ± 14.8 | 0.035 |
| Urine sodium (mEq/L) | 49.71 ± 34.5 | 47.34 ± 29.34 | 36.6 ± 21.27 | 0.029 |
| Urinary IL-18 (µg/g creatinine) | 254.5 ± 77.9 | 296.56 ± 113 | 983.48 ± 594.43 | 0.001 |
| Urinary NGAL (µg/g creatinine) | 96.84 ± 35.58 | 113.76 ± 47.98 | 357.78 ± 228.51 | 0.001 |
MELD: Model for End-Stage Liver Disease and NGAL: neutrophil-gelatinase-associated lipocalin.
Significant at P < 0.05; P < 0.01; and P < 0.001.
Table 2.
Characteristics of renal impairment patients.
| CKD (n = 15) | Prerenal (n = 17) | HRS (n = 14) | ATN (n = 22) | P | |
|---|---|---|---|---|---|
| Serum creatinine (mg/dL) | 2.79 ± 0.8 | 1.76 ± 0.2 | 2.21 ± 0.79 | 2.7 ± 1.23 | 0.003 |
| Sodium (mEq/L) | 132 ± 6.71 | 132 ± 4.93 | 129 ± 5 | 133 ± 7.77 | 0.257 |
| Potassium (mEq/L) | 4.94 ± 0.8 | 4.39 ± 0.61 | 4.41 ± 0.955 | 4 ± 0.54 | 0.004 |
| Glomerular filtration rate (mL/min/1.73 m2) | 35.6 ± 20.5 | 53.2 ± 13.84 | 44.3 ± 22.8 | 45.98 ± 47.48 | 0.475 |
| Mean arterial pressure (mmHg) | 89.5 ± 11.49 | 77.2 ± 14.2 | 74.86 ± 9.17 | 69.78 ± 15.35 | 0.0001 |
| Urine sodium (mEq/L) | 29.2 ± 7.81 | 29.3 ± 13.18 | 12.4 ± 5.6 | 62.68 ± 8.17 | 0.0001 |
| Urinary IL-18 (µg/g creatinine) | 582.34 ± 98.24 | 451.47 ± 121.73 | 953.5 ± 273 | 1687.1 ± 447 | 0.0001 |
| Urinary NGAL (µg/g creatinine) | 232.63 ± 41.31 | 161.15 ± 60.75 | 380.6 ± 132.32 | 580.51 ± 238.75 | 0.0001 |
| Fractional excretion of sodium (FeNa) (%) | 0.32 ± 0.17 | 0.54 ± 0.24 | 0.15 ± 0.07 | 4.05 ± 1.05 | 0.0001 |
CKD: chronic kidney disease, HRS: hepatorenal syndrome, and ATN: acute tubular necrosis.
Significant at P < 0.05; P < 0.01; and P < 0.001.
3.2. Urinary Neutrophil-Gelatinase-Associated Lipocalin (NGAL)
Patients with renal impairment had higher urinary NGAL levels (357.78 ± 228.51 μg/g creatinine) compared to those of patients without renal impairment, either with or without ascites (96.84 ± 35.58, 113.76 ± 47.98 μg/g creatinine, resp.).
The mean value of urinary NGAL in HRS (380.6 ± 132.32 μg/g creatinine) was significantly higher compared to prerenal azotemia patients (161.15 ± 60.75 μg/g creatinine, P = 0.0015) and significantly lower compared to ATN patients (580.51 ± 238.75, P = 0.0001). Furthermore, urinary NGAL levels in patients with CKD (232.63 ± 41.31 μg/g creatinine) were significantly different from those of patients with HRS (P = 0.003) (Figure 1).
Figure 1.
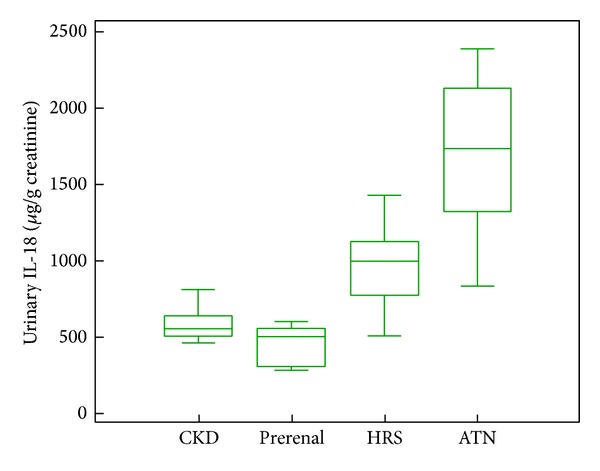
Box-plot of urinary NGAL levels, according to the study subgroups of impairment of kidney function.
In simple regression analysis, urinary NGAL was positively correlated with serum creatinine (r = 0.465, P < 0.001), urinary IL-18 (r = 0.9, P < 0.001), fractional excretion of Na (FeNa) (r = 0.687, P < 0.001), and mean blood pressure (r = 0.339, P = 0.005) in patient subgroups with renal impairment (Table 3).
Table 3.
Simple linear regression of urinary IL-18 and urinary NGAL in renal impairment patients.
| Urinary NGAL (µg/g creatinine) | Urinary IL-18 (µg/g creatinine) | |||
|---|---|---|---|---|
| β(r) | P | β(r) | P | |
| Serum albumin (g/L) | 0.129 | 0.293 | 0.114 | 0.355 |
| Serum creatinine (mg/dL) | 0.465 | <0.001 | 0.422 | <0.001 |
| Serum bilirubin(mg/dL) | 0.1212 | 0.325 | 0.0502 | 0.668 |
| Urinary IL-18 (µg/g creatinine) | 0.9 | <0.001 | ||
| Urinary NGAL (µg/g creatinine) | 0.9 | <0.001 | ||
| Fractional excretion of sodium (%) | 0.687 | <0.001 | 0.807 | <0.001 |
| Mean arterial pressure (mmHg) | 0.339 | 0.005 | 0.329 | 0.006 |
β: regression coefficient.
The cut-off value of urinary NGAL that differentiates between patients with AKI and those with other causes of renal impairment was 286.3 μg/g creatinine (area under ROC curve is 0.909) (sensitivity 95.5% and specificity 76.1%) with a positive predictive value (PPV) of 65.6 and negative predictive value (NPV) of 99.2 (Figure 3).
Figure 3.
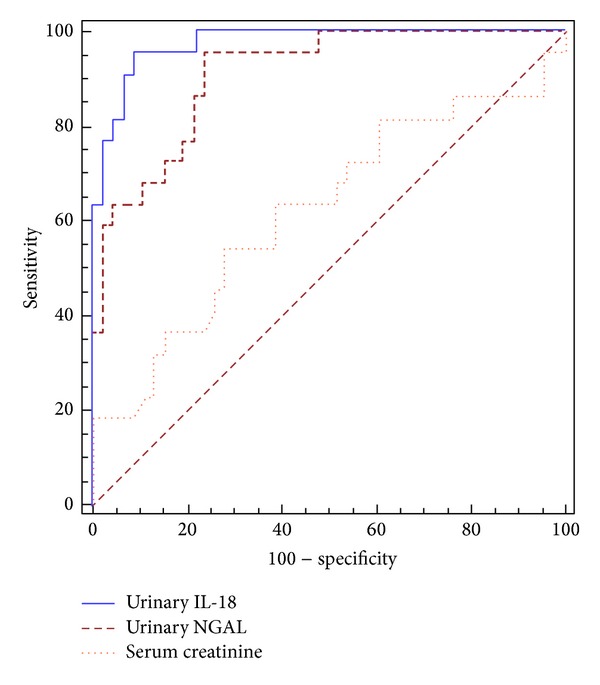
Receiver operating characteristic (ROC) curves to evaluate the capability of urinary IL-18, urinary NGAL, and serum creatinine to diagnose acute tubular injury.
3.3. Urinary Interleukin-18 (IL-18)
Patients with renal impairment had higher urinary IL-18 levels (983 ± 594 μg/g creatinine) compared to those of patients without renal impairment, either with or without ascites (296.56 ± 113, 254.5 ± 77.9 μg/g creatinine, resp.).
Urinary IL-18 levels were analyzed in renal impairment patients' subgroups. We observed that patients with ATN had the highest values of urinary IL-18, while patients with prerenal azotemia had the lowest values (1687 ± 447 versus 451.47 ± 121.73 μg/g creatinine, resp.; P = 0.0001). Patients with HRS had intermediate values (953 ± 273 μg/g creatinine), which were significantly higher than those of patients with prerenal azotemia (P = 0.0015) and lower than those of patients with ATN (P = 0.0001). Urinary IL-18 levels in patients with CKD (582 ± 98.24 μg/g creatinine) were significantly different from those of patients with HRS (P = 0.001) (Figure 2).
Figure 2.
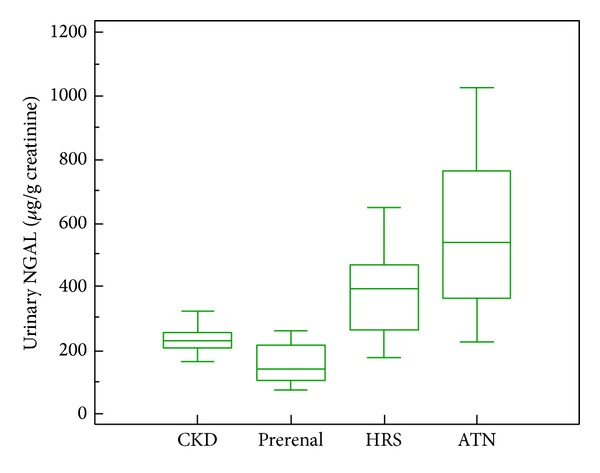
Box-plot of urinary IL-18 levels, according to the study subgroups of impairment of kidney function.
In simple regression analysis, urinary IL-18 was positively correlated with serum creatinine (r = 0.422, P < 0.001), FeNa (r = 0.807, P < 0.001), and mean blood pressure (r = 0.329, P = 0.006) in patient subgroups with renal impairment (Table 3).
The cut-off value of urinary IL-18 that differentiates between patients with AKI and those with other causes of renal impairment was 1119.6 μg/g creatinine (area under ROC curve is 0.975) (sensitivity 95.5% and specificity 91.3%) with PPV of 84 and NPV of 99.3 (Figure 3).
4. Discussion
AKI is a common condition in cirrhotic patients admitted to ICU. It is now recognized that AKI can significantly impact patients' outcomes [21]. In fact, ATN is an important precipitating factor for the development of HRS [2, 18]. It has been proposed that intense renal vasoconstriction in HRS, if prolonged, may lead to tubular ischemia and ultimately progress into ATN [23–25]. Therefore, it may be difficult to distinguish HRS from ATN in clinical settings.
In general, patients without liver cirrhosis, urine sediment and FeNa may help make the diagnosis of ATN. However, confounding results may be encountered in cirrhotic patients that may not correspond to the usual range for general patients with ATN. Therefore, FeNa is a less useful diagnostic tool for tubular injury in patients with advanced liver diseases, whose pre-existing hemodynamic states make them sodium-avid [26, 27].
Our study demonstrated a significant difference of urinary NGAL and IL-18 in each category of AKI: highest in ATN, intermediate in HRS, and low in prerenal disease. Moreover, urinary NGAL and IL-18 levels in patients with prerenal azotemia were similar to those with normal kidney function and stable CKD. In contrast, sCr was not different between patients with ATN and HRS.
The mechanism by which patients with HRS have intermediate urinary NGAL and IL-18 levels remains unclear. HRS physiology is thought to be an extreme prerenal state [27, 28] with severe renovascular vasoconstriction and decreased GFR, but normal intrinsic kidney function. Kidney function can return to normal after improvement of hepatic hemodynamics [27–29] or after renal transplantation into a recipient with normal hepatic function [30, 31].
However, pathologic investigations have reported subtle kidney tubular and glomerular damage in HRS kidneys, some seen only by electron microscopy [23, 32], perhaps resulting from the cellular changes associated with chronic activation of angiotensin-aldosterone signaling [33]. It is conceivable that profound renovascular constriction may cause subclinical tubular damage in at least a subset of nephrons, not detectable by urinary sodium, which is not sensitive enough to detect mild or patchy tubular epithelial damage.
Our study also confirms previous studies demonstrating that a single urinary NGAL or urinary IL-18 measurement on hospital admission has the potential to assist in determining the type of kidney dysfunction, perhaps improving patient management and outcomes [13, 34, 35].
Urinary NGAL and urinary IL-18 demonstrated an excellent discriminating power compared to serum creatinine (AUROC 0.909 for NGAL, 0.975 for IL-18, and 0.622 for Cr) for discriminating ATN from HRS in our patients. This is in contrast to traditional measurements of kidney and liver disease severity including sCr and MELD score.
Our data demonstrate that patients with cirrhosis are at a high risk for acute renal impairment (33.1% of the patients, 41% of them diagnosed as ATN and 26.4% diagnosed as HRS). The present findings seem to be consistent with previous studies [3, 36] which confirm that non-HRS types of AKI are common in patients with cirrhosis and further studies are needed to determine inciting factors of AKI in this population.
This study has some limitations. First, sCr inaccurately measures kidney function in cirrhosis [5, 37, 38], and there is no widely available technique to accurately measure GFR in these patients. Second, absence of kidney biopsy, which is rarely performed in this population, because of the high risk of bleeding tendency, therefore, there is a lack of correlation between renal pathology and urinary NGAL and urinary IL-18.
In conclusion, urinary NGAL and urinary IL-18 have the ability to differentiate between AKI types in patients with cirrhosis. This could improve risk stratification for patients admitted to the hospital with cirrhosis, perhaps leading to early ICU admission, transplant evaluation, and prompt initiation of HRS therapy and early management of AKI. These findings, if confirmed in larger cohorts, could lead to the development of biomarker algorithms to rapidly identify patients with HRS and ATN and accurately predict prognosis.
5. Definitions
5.1. Cirrhosis
The diagnosis of cirrhosis was based on a combination of clinical, biochemical, ultrasonographic, and endoscopic findings.
5.2. Impairment of Kidney Function
Impairment of kidney function was diagnosed when serum creatinine concentration was greater than 1.5 mg/dL. This value of serum creatinine was chosen because it has been selected in several consensus conferences as cut-off to define impairment of kidney function in cirrhosis [7, 20].
5.3. Causes of Impairment of Kidney Function
The definitions used for the different causes of impairment of kidney function were as follows. Briefly, (1) prerenal azotemia due to volume depletion was considered when patients had a history of fluid losses in the preceding days (due to either bleeding, diuretic overdose, or other causes), together with compatible findings, absence of other causes of impairment of kidney function, and reversibility of kidney impairment as indicated by decrease of serum creatinine below 1.5 mg/dL after fluid resuscitation; (2) chronic kidney disease (CKD) was defined by evidence of structural kidney abnormalities (imaging studies), proteinuria, and/or abnormal urinalysis, with a glomerular filtration rate of less than 60 mL/min per 1.73 m2, as assessed by MDRD formula [38]; (3) HRS was defined using the current definition of the International Ascites Club [7]; and (4) ATN was diagnosed in patients who had at least three of the following: hypovolemic and/or septic shock or treatment with potentially nephrotoxic agents, urine sodium greater than 40 mEq/L, urine osmolality lower than 400 mOsm/kg, and fractional excretion of sodium greater than 2% without diuretics [22, 39].
Conflict of Interests
The authors declare that there is no conflict of interests regarding the publication of this paper.
Authors' Contribution
Anass Ahmed Qasem and Salama Elsayed Farag conceived and designed the study and were involved in the acquisition of data, analysis and interpretation of data, statistical analysis, drafting the paper, study supervision, and critical revision of this paper for important intellectual content. Emad Hamed, Mohamed Emara, Ahmed Bihery, and Heba Pasha were involved in the acquisition of data and critical revision of the paper for important intellectual content.
References
- 1.El Gaafary MM, Rekacewicz C, Abdel-Rahman AG, et al. Surveillance of acute hepatitis C in Cairo, Egypt. Journal of Medical Virology. 2005;76(4):520–525. doi: 10.1002/jmv.20392. [DOI] [PubMed] [Google Scholar]
- 2.Garcia-Tsao G, Parikh CR, Viola A. Acute kidney injury in cirrhosis. Hepatology. 2008;48(6):2064–2077. doi: 10.1002/hep.22605. [DOI] [PubMed] [Google Scholar]
- 3.du Cheyron D, Bouchet B, Parienti J, Ramakers M, Charbonneau P. The attributable mortality of acute renal failure in critically ill patients with liver cirrhosis. Intensive Care Medicine. 2005;31(12):1693–1699. doi: 10.1007/s00134-005-2842-7. [DOI] [PubMed] [Google Scholar]
- 4.Iwakiri Y, Groszmann RJ. The hyperdynamic circulation of chronic liver diseases: from the patient to the molecule. Hepatology. 2006;43:S121–S131. doi: 10.1002/hep.20993. [DOI] [PubMed] [Google Scholar]
- 5.Cholongitas E, Shusang V, Marelli L, et al. Review article: renal function assessment in cirrhosis—difficulties and alternative measurements. Alimentary Pharmacology and Therapeutics. 2007;26(7):969–978. doi: 10.1111/j.1365-2036.2007.03443.x. [DOI] [PubMed] [Google Scholar]
- 6.Wong F, Nadim MK, Kellum JA, et al. Working Party proposal for a revised classification system of renal dysfunction in patients with cirrhosis. Gut. 2011;60(5):702–709. doi: 10.1136/gut.2010.236133. [DOI] [PubMed] [Google Scholar]
- 7.Salerno F, Gerbes A, Ginès P, Wong F, Arroyo V. Diagnosis, prevention and treatment of hepatorenal syndrome in cirrhosis. Gut. 2007;56(9):1310–1318. doi: 10.1136/gut.2006.107789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bellomo R, Ronco C, Kellum JA, Mehta RL, Palevsky P. Acute renal failure—definition, outcome measures, animal models, fluid therapy and information technology needs: the Second International Consensus Conference of the Acute Dialysis Quality Initiative (ADQI) Group. Critical Care. 2004;8(4):R204–R212. doi: 10.1186/cc2872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mehta RL, Bouchard J. Controversies in acute kidney injury: effects of fluid overload on outcome. Contributions to Nephrology. 2011;174:200–211. doi: 10.1159/000329410. [DOI] [PubMed] [Google Scholar]
- 10.Ginès P, Angeli P, Lenz K, et al. EASL clinical practice guidelines on the management of ascites, spontaneous bacterial peritonitis, and hepatorenal syndrome in cirrhosis. Journal of Hepatology. 2010;53(3):397–417. doi: 10.1016/j.jhep.2010.05.004. [DOI] [PubMed] [Google Scholar]
- 11.Bachorzewska-Gajewska H, Malyszko J, Sitniewska E, Malyszko JS, Dobrzycki S. Neutrophil-gelatinase-associated lipocalin and renal function after percutaneous coronary interventions. American Journal of Nephrology. 2006;26(3):287–292. doi: 10.1159/000093961. [DOI] [PubMed] [Google Scholar]
- 12.Makris K, Markou N, Evodia E, et al. Urinary neutrophil gelatinase-associated lipocalin (NGAL) as an early marker of acute kidney injury in critically ill multiple trauma patients. Clinical Chemistry and Laboratory Medicine. 2009;47(1):79–82. doi: 10.1515/CCLM.2009.004. [DOI] [PubMed] [Google Scholar]
- 13.Nickolas TL, O’Rourke MJ, Yang J, et al. Sensitivity and specificity of a single emergency department measurement of urinary neutrophil gelatinase-associated lipocalin for diagnosing acute kidney injury. Annals of Internal Medicine. 2008;148(11):810–819. doi: 10.7326/0003-4819-148-11-200806030-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jeong T, Kim S, Lee W, et al. Neutrophil gelatinase-associated lipocalin as an early biomarker of acute kidney injury in liver transplantation. Clinical Transplantation. 2012;26:775–781. doi: 10.1111/j.1399-0012.2012.01610.x. [DOI] [PubMed] [Google Scholar]
- 15.Parikh CR, Jani A, Melnikov VY, Faubel S, Edelstein CL. Urinary interleukin-18 is a marker of human acute tubular necrosis. American Journal of Kidney Diseases. 2004;43(3):405–414. doi: 10.1053/j.ajkd.2003.10.040. [DOI] [PubMed] [Google Scholar]
- 16.Parikh CR, Devarajan P. New biomarkers of acute kidney injury. Critical Care Medicine. 2008;36:S159–S165. doi: 10.1097/CCM.0b013e318168c652. [DOI] [PubMed] [Google Scholar]
- 17.Pugh RN, Murray-Lyon IM, Dawson JL, et al. Transection of the esophagus in the bleeding esophageal varices. British Journal of Surgery. 1973;60:648–652. doi: 10.1002/bjs.1800600817. [DOI] [PubMed] [Google Scholar]
- 18.Moreau R, Lebrec D. Acute renal failure in patients with cirrhosis: perspectives in the age of MELD. Hepatology. 2003;37(2):233–243. doi: 10.1053/jhep.2003.50084. [DOI] [PubMed] [Google Scholar]
- 19.Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D. A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Annals of Internal Medicine. 1999;130(6):461–470. doi: 10.7326/0003-4819-130-6-199903160-00002. [DOI] [PubMed] [Google Scholar]
- 20.Arroyo V, Terra C, Ginès P. Advances in the pathogenesis and treatment of type-1 and type-2 hepatorenal syndrome. Journal of Hepatology. 2007;46(5):935–946. doi: 10.1016/j.jhep.2007.02.001. [DOI] [PubMed] [Google Scholar]
- 21.Levey AS, Coresh J, Balk E, et al. National Kidney Foundation practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Annals of Internal Medicine. 2003;139:137–147. doi: 10.7326/0003-4819-139-2-200307150-00013. [DOI] [PubMed] [Google Scholar]
- 22.Schrier RW. Diagnostic value of urinary sodium, chloride, urea, and flow. Journal of the American Society of Nephrology. 2011;22(9):1610–1613. doi: 10.1681/ASN.2010121289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mandal AK, Lansing M, Fahmy A. Acute tubular necrosis in hepatorenal syndrome: an electron microscopy study. American Journal of Kidney Diseases. 1982;2(3):363–374. doi: 10.1016/s0272-6386(82)80096-6. [DOI] [PubMed] [Google Scholar]
- 24.Rector WG, Jr., Kanel GC, Rakela J, Reynolds TB. Tubular dysfunction in the deeply jaundiced patient with hepatorenal syndrome. Hepatology. 1985;5(2):321–326. doi: 10.1002/hep.1840050229. [DOI] [PubMed] [Google Scholar]
- 25.Angeli P, Volpin R, Gerunda G, et al. Reversal of type 1 hepatorenal syndrome with the administration of midodrine and octreotide. Hepatology. 1999;29(6):1690–1697. doi: 10.1002/hep.510290629. [DOI] [PubMed] [Google Scholar]
- 26.Esson ML, Schrier RW. Diagnosis and treatment of acute tubular necrosis. Annals of Internal Medicine. 2002;137(9):744–752. doi: 10.7326/0003-4819-137-9-200211050-00010. [DOI] [PubMed] [Google Scholar]
- 27.Ochs A, Rossle M, Haag K, et al. The transjugular intrahepatic portosystemic stent-shunt procedure for refractory ascites. The New England Journal of Medicine. 1995;332(18):1192–1197. doi: 10.1056/NEJM199505043321803. [DOI] [PubMed] [Google Scholar]
- 28.Iwatsuki S, Popovtzer MM, Corman JL. Recovery from “hepatorenal syndrome” after orthotopic liver transplantation. The New England Journal of Medicine. 1973;289(22):1155–1159. doi: 10.1056/NEJM197311292892201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cassinello C, Moreno E, Gozalo A, Ortuño B, Cuenca B, Solís-Herruzo JA. Effects of Orthotopic liver transplantation on vasoactive systems and renal function in patients with advanced liver cirrhosis. Digestive Diseases and Sciences. 2003;48(1):179–186. doi: 10.1023/a:1021763221337. [DOI] [PubMed] [Google Scholar]
- 30.McDonald FD, Brennan LA, Turcotte JG. Severe hypertension and elevated plasma renin activity following transplantation of “hepatorenal donor” kidneys into anephric recipients. The American Journal of Medicine. 1973;54(1):39–43. doi: 10.1016/0002-9343(73)90081-8. [DOI] [PubMed] [Google Scholar]
- 31.Koppel MH, Coburn JW, Mims MM, Goldstein H, Boyle JD, Rubini ME. Transplantation of cadaveric kidneys from patients with hepatorenal syndrome. Evidence for the functionalnature of renal failure in advanced liver disease. The New England Journal of Medicine. 1969;280(25):1367–1371. doi: 10.1056/NEJM196906192802501. [DOI] [PubMed] [Google Scholar]
- 32.Kanel GC, Peter RL. Glomerular tubular reflex. A morphologic renal lesion associated with the hepatorenal syndrome. Hepatology. 1984;4(2):242–246. doi: 10.1002/hep.1840040212. [DOI] [PubMed] [Google Scholar]
- 33.Hollenberg NK. Aldosterone in the development and progression of renal injury. Kidney International. 2004;66(1):1–9. doi: 10.1111/j.1523-1755.2004.00701.x. [DOI] [PubMed] [Google Scholar]
- 34.Siew ED, Ikizler TA, Gebretsadik T, et al. Elevated urinary IL-18 levels at the time of ICU admission predict adverse clinical outcomes. Clinical Journal of the American Society of Nephrology. 2010;5(8):1497–1505. doi: 10.2215/CJN.09061209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Devarajan P. Biomarkers for the early detection of acute kidney injury. Current Opinion in Pediatrics. 2011;23(2):194–200. doi: 10.1097/MOP.0b013e328343f4dd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Verna EC, Brown RS, Farrand E, et al. Urinary neutrophil gelatinase-associated lipocalin predicts mortality and identifies acute kidney injury in cirrhosis. Digestive Diseases and Sciences. 2012;57:2362–2370. doi: 10.1007/s10620-012-2180-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Papadakis MA, Arieff AI. Unpredictability of clinical evaluation of renal function in cirrhosis. Prospective study. The American Journal of Medicine. 1987;82(5):945–952. doi: 10.1016/0002-9343(87)90156-2. [DOI] [PubMed] [Google Scholar]
- 38.Levey AS, Coresh J, Greene T, et al. Expressing the modification of diet in renal disease study equation for estimating glomerular filtration rate with standardized serum creatinine values. Clinical Chemistry. 2007;53(4):766–772. doi: 10.1373/clinchem.2006.077180. [DOI] [PubMed] [Google Scholar]
- 39.Gill N, Natty JV, Jr., Fatica RA. Renal failure secondary to acute tubular necrosis: epidemiology, diagnosis, and management. Chest. 2005;128(4):2847–2863. doi: 10.1378/chest.128.4.2847. [DOI] [PubMed] [Google Scholar]