Introduction
Parry-Romberg syndrome is characterized by hemifacial atrophy involving skin, subcutaneous tissue, muscle, and bone. The cause is unknown although variable association with morphea or localized scleroderma has raised the possibility of autoimmune process1. Seizures and headaches are the most frequent co-morbidities of Parry-Romberg syndrome2 although a variety of neurologic syndromes have been reported. These are usually attributed to intracranial lesions,2,3 and include progressive hemispheric atrophy with inflammation resembling Rasmussen’s encephalitis.4 Movement disorders have rarely been reported with Parry-Romberg syndrome.5–7 We report a 39 year old subject with Parry-Romberg syndrome with dystonia, tremor, and levodopa-responsive hemiparkinsonism.
Case report
A 39 year old man first developed muscle spasms of right hand when bowling at the age of 19, followed by cramping of the right foot and spasms of left jaw. Neurologic examination at age 32 demonstrated right hemidystonia, and dystonic, left hemifacial stiffening.
At the age of 36 he started having occasional episodes of light headedness rarely associated with loss of consciousness that were presumed to be seizures and which responded to phenytoin treatment. At 39 years he developed skin discoloration and morphea of the left face. He noted atrophy of the left side of his face and lost the eyelashes on his left eyelid. He also developed mild weakness of right arm.
MRI of the brain with contrast and electroencephalography were normal. Complete blood count, serum chemistry, ceruloplasmin, Lyme titres, anti-nuclear antibodies, anti-centrimere, anti-ENA, complement and HIV were normal.
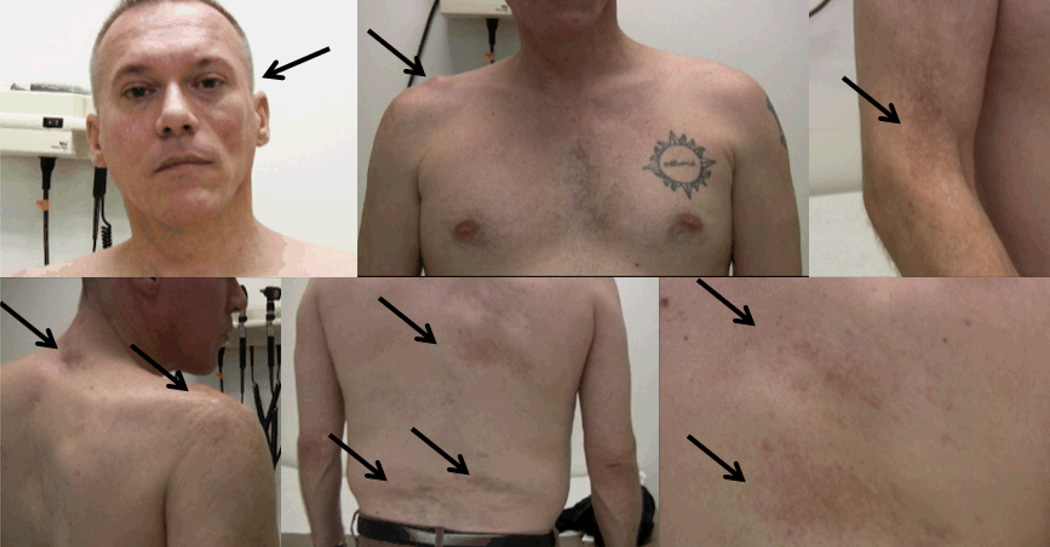
Examination at age 39 demonstrated marked atrophy of the left lower face, absent lashes on the left eyelid and decreased hair on the right forearm (Fig. 1). There were areas of brown discoloration and induration of the skin on the lateral aspect of the right upper arm, the posterior aspect of the neck and the back, that were asymmetric and not in dermatomal distributions, but which tended to respect the midline. The right deltoid, posterior neck, and supraspinatus muscles were atrophied. Facial movements were symmetric. There was a slight head tilt to the right with elevation of the left shoulder. In right upper and lower limbs muscle strength was 5-/5 and muscle tone was mildly increased. He had small amplitude myoclonic jerks of the right arm with sustained postures and at rest, although no abnormal posturing was noted. There was subtle bradykinesia of the right hand and synkinesia of both feet. Deep tendon reflexes were reduced in the left arm, but were otherwise normal. There was slight decrease in pinprick distally on the left. Gait examination revealed decreased right arms wing. At this time he was taking baclofen 10mg bid, gabapentin 120mg bid, quetiapine 50mg daily, buproprion 100mg bid, sodium divalproate 300mg bid, and diclofenac 75mg bid. On these medications, some of which were for his mood disorder and some for chronic pain, he reported a reduction in limb dystonia.
Figure 1.
Regions of focal atrophy of subcutaneous tissues, muscle and fat, with scleroderma, indicated by arrows.
Treatment with carbidopa/levo-dopa (25/100) bid reduced the bradykinesia and tremor of the right hand. Some twitching and contractions in right arm and turning out of the right foot when running persisted. At age 41 he developed a pulmonary embolus, for which he was started on coumadin, and was found to have anti-phospholipid antibodies. He also reported sudden onset of spasms of the right thoracic muscles close to the axilla, which responded to low dose clonazepam
Discussion
This patient had multifocal dermatological and neurological symptoms in the absence of intracerebral lesions. The distribution of the movement disorders (left lower face and right upper and lower extremities and right trunk) suggested a lesion in the brainstem. However, the cutaneous and subcutaneous features appeared to be in the same regions as the muscles affected by the movement disorder, implicating a possible local mechanism.
Parry-Romberg syndrome is considered to be closely related to scleroderma and therefore likely attributable to an autoimmune disturbance1. Parry-Romberg is often associated with linear scleroderma on the head, known as en coup de sabre. Morphea refers to regions of scleroderma which may be linear, superficial circumscribed, or pansclerotic. Most of our patient’s lesions fell into the latter category as there was significant subcutaneous tissue loss and muscle wasting.
Patients with morphea may have anti-phospholipid antibodies.8,9 These autoantibodies are more typically associated with chorea, but have rarely been reported to cause dystonia associated with ischemic lesions on brain MRI. The normal brain MRI in our patient may argue against the clinical significance of the antiphospholipid antibodies, at least with respect to the movement disorder. Seizures (73%) and headaches (29%) were the most frequent neurologic manifestations among 54 subjects with localized scleroderma.2 In most cases these symptoms appeared to be secondary to intracerebral lesions. Only 11% of patients in a large series2 had neurologic symptoms with normal brain MRI, as did our subject. Our patient was also unusual in having bilateral findings, seen in 10/54 cases,2 and in having both cranial and non-cranial symptoms (found in 18% of cases2).
There are few reported cases of dystonia or muscle spasms associated with Parry-Romberg syndrome. One case in the series of 8 patients with unilateral jaw dystonia or hemi-masticatory spasm is reported, who had hemi-masticatory spasm with facial hemiatrophy and patchy pigmentation of face.5 (This report also refers to “masticatory spasm of Romberg” described by Gowers in 1899). There is one case of child of 8 with Parry-Romberg and torticollis in association with strabismus6. Focal dystonia is very rare in children, and the limited details provided make it hard to determine whether this was true dystonia.
Focal dystonia of the arm was confirmed by EMG in one patient with localized scleroderma7, but local nerve irritation causing muscle cramps7 and neuromyotonia10 have been also reported.
A local etiology, as is true in the current case, is suggested by the observation that muscle spasms are invariably localized to areas affected by the skin changes7. Peripheral and sympathetic nerve involvement is clearly related to skin and subcutaneous tissue involvement in other cases. However, confounding this mechanism is the improvement in spasms with l-dopa, which suggests a central origin, as does the hemi-parkinsonism, albeit in light of the absence of any intracerebral lesions.
In conclusion, these autoimmune skin processes can be associated with complex movement disorders, the pathophysiology of which is not yet clear.
Acknowledgment
We thank the patient for his cooperation.
References
- 1.Tollefson MM, Witman PM. En coup de sabre morphea and Parry-Romberg syndrome: a retrospective review of 54 patients. J Am Acad Dermatol. 2007;56:257–263. doi: 10.1016/j.jaad.2006.10.959. [DOI] [PubMed] [Google Scholar]
- 2.Kister I, Inglese M, Laxer RM, et al. Neurologic manifestations of localized scleroderma: a case report and literature review. Neurology. 2008;71:1538–1545. doi: 10.1212/01.wnl.0000334474.88923.e3. [DOI] [PubMed] [Google Scholar]
- 3.Stone J, Franks AJ, Guthrie JA, et al. Scleroderma “en coup de sabre”: pathological evidence of intracerebral inflammation. J Neurol Neurosurg Psychiatry. 2001;70:382–385. doi: 10.1136/jnnp.70.3.382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Carreno M, Donaire A, Barcelo MI, et al. Parry Romberg syndrome and linear scleroderma in coup de sabre mimicking Rasmussen encephalitis. Neurology. 2007;68:1308–1310. doi: 10.1212/01.wnl.0000259523.09001.7a. [DOI] [PubMed] [Google Scholar]
- 5.Thompson PD, Obeso JA, Delgado G, et al. Focal dystonia of the jaw and the differential diagnosis of unilateral jaw and masticatory spasm. J Neurol Neurosurg Psychiatry. 1986;49:651–656. doi: 10.1136/jnnp.49.6.651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kee C, Hwang JM. Parry-Romberg syndrome presenting with recurrent exotropia and torticollis. J Pediatr Ophthalmol Strabismus. 2008;45:368–370. doi: 10.3928/01913913-20081101-10. [DOI] [PubMed] [Google Scholar]
- 7.Zivkovic SA, Lacomis D, Medsger TA., Jr Muscle cramps associated with localized scleroderma skin lesions: focal dystonia, neuromyotonia, or nerve entrapment? J Rheumatol. 2006;33:2549-. [PubMed] [Google Scholar]
- 8.Sato S, Fujimoto M, Hasegawa M, et al. Antiphospholipid antibody in localised scleroderma. Ann Rheum Dis. 2003;62:771–774. doi: 10.1136/ard.62.8.771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Penmetcha M, Rosenbush SW, Harris CA. Cardiac valvular disease in scleroderma and systemic lupus erythematosus/scleroderma overlap associated with antiphospholipid antibodies. J Rheumatol. 1996;23:2171–2174. [PubMed] [Google Scholar]
- 10.Kumar A, Jain R, Daga J. Simultaneous occurrence of neuromyotonia and morphoea: a cause-effect relationship? J Neurol Neurosurg Psychiatry. 2006;77:802-. doi: 10.1136/jnnp.2005.083683. [DOI] [PMC free article] [PubMed] [Google Scholar]