Abstract
Introduction
Mindfulness meditation training is garnering increasing empirical interest as an intervention for attention-deficit/hyperactivity disorder (ADHD) in adulthood, although no studies of mindfulness as a standalone treatment have included a sample composed entirely of adults with ADHD or a comparison group. The aim of this study was to assess the feasibility, acceptability, and preliminary efficacy of mindfulness meditation for ADHD, executive functioning (EF), and emotion dysregulation symptoms in an adult ADHD sample.
Methods
Adults with ADHD were stratified by ADHD medication status and otherwise randomized into an eight-week group-based mindfulness treatment (n=11) or waitlist (n=9) group.
Results
Treatment feasibility and acceptability were positive. In addition, self-reported ADHD and EF symptoms (assessed in the laboratory and ecological momentary assessment), clinician ratings of ADHD and EF symptoms, and self-reported emotion dysregulation improved for the treatment group relative to the waitlist group over time with large effect sizes. Improvement was not observed for EF tasks.
Conclusions
Findings support preliminary treatment efficacy, though require larger trials.
Keywords: attention-deficit/hyperactivity disorder, adults, mindfulness meditation training, executive functioning, emotion dysregulation, ecological momentary assessment
Introduction
Attention-deficit/hyperactivity disorder (ADHD) is a developmental disorder that persists into adulthood for the majority of cases (Barkley, Murphy, & Fischer, 2008) and occurs in approximately 4% of the adult population (Fayyad et al., 2007; Kessler et al., 2006). Diagnostic conceptualizations require age-inappropriate symptoms in at least one of two symptom clusters: inattention and hyperactivity-impulsivity. Although these are the core symptoms according to current diagnostic guidelines (American Psychiatric Association [APA], 2000, 2013; World Health Organization, 1992), executive functioning (EF) deficits and emotion dysregulation are also key areas of impairment for many patients (e.g., Barkley, 2010; Boonstra, Oosterlaan, Sergeant, & Buitelaar, 2005; Martel, 2009). For instance, symptoms of EF are more consistent and discriminating predictors of ADHD into adulthood than inattentive and hyperactive-impulsive symptoms (Kessler et al., 2010). In addition, symptoms of emotional impulsivity, which involves the ability to self-regulate emotional functioning, uniquely contribute to impairment in a variety of functional domains (e.g., occupational, educational, criminal, driving, and financial) beyond core ADHD symptoms (Barkley & Fischer, 2010; Barkley & Murphy, 2010a). Therefore, it would be beneficial for ADHD treatments to expand beyond core symptoms, and target EF and emotion dysregulation as well. The primary aim of the current study was to assess the feasibility, treatment acceptability, and preliminary efficacy of a novel intervention on core symptoms of ADHD, EF, and emotion dysregulation in an adult ADHD sample.
Stimulant and nonstimulant pharmacotherapies are efficacious for improving core ADHD symptoms in adults diagnosed with the disorder (Faraone & Glatt, 2010). However, such treatments have limitations, including nonresponsiveness to medication, insufficient symptom remission, and intolerable adverse medication effects (Prince, Wilens, Spencer, & Biederman, 2006; Steele, Jensen, & Quinn, 2006; Wender, 1998; Wilens, Spencer, & Biederman, 2002). In addition, with exceptions (Reimherr et al., 2010; Reimherr et al., 2005), there are relatively few studies that have investigated the impact of pharmacotherapy on EF, emotion dysregulation, or other impairments often observed among adults diagnosed with ADHD.
Mindfulness meditation training may be particularly well-suited to address core symptoms and related impairments in adults diagnosed with ADHD. Mindfulness meditation involves the formal practice of adopting a nonjudgmental attention to one’s experience(s) in the present moment (Kabat-Zinn, 1990). It has been conceptualized as a two-component model that involves (a) orienting one’s attention purposefully to the present moment and (b) approaching one’s experience in the present moment with curiosity, openness, and acceptance (Bishop et al., 2004). Mindfulness-based therapies are effective in managing a variety of symptoms in psychiatric samples, including anxiety and depression (see Chiesa & Serretti, 2011 and Fjorback, Arendt, Ornbol, Fink, & Walach, 2011) for reviews). Mindfulness training is particularly promising for those diagnosed with ADHD since one proposed mechanism of action is enhancement of attentional regulation involving EF processes (Hölzel et al., 2011; Keng, Smoski, & Robins, 2011). For example, four 20-minute sessions composed of brief mindfulness training significantly improved visuo-spatial processing, working memory, and EF task performance in mindfulness-naïve participants (Zeidan, Johnson, Diamond, David, & Goolkasian, 2010). In another study, mindfulness training improved teacher and parental reports of EF in second- and third-grade children (Flook et al., 2010).
Mindfulness-based interventions are also promising for ADHD since another proposed mechanism of action is improvement in ability to regulate emotions (Hölzel, et al., 2011; Shapiro, Carlson, Astin, & Freedman, 2006). For example, a mindfulness-based intervention improved emotional reactivity to stress in a clinical sample with recurrent depression (Britton, Shahar, Szepsenwol, & Jacobs, 2012). Neuroimaging studies also indicate that mindfulness meditation training improves activation of executive attention networks and those associated with emotion regulation (see Hölzel, et al., 2011 for a review). Further, across nonclinical samples, effect sizes are medium to large for changes in emotionality and attention (Sedlmeier et al., 2012). Overall, given that (a) attentional functioning including EF and emotion dysregulation are implicated as potential mechanisms through which mindfulness exerts its impact and (b) these domains overlap with core symptoms or associated features of ADHD, mindfulness meditation training is a conceptually plausible approach for treating adults with ADHD.
Several studies provide preliminary support for the potential efficacy of mindfulness meditation training in individuals with ADHD (see Mitchell, Zylowska, & Kollins, submitted, for a review). In one study of adults and adolescents with ADHD who completed a group-based mindfulness training (Zylowska et al., 2008), post-treatment scores improved for self-reported ADHD, depression, and anxiety symptoms, and performance on tasks measuring attention and cognitive inhibition. Improvements in ADHD, anxiety, and depressive symptoms were sustained at 3-month follow-up (Zylowska, Smalley, & Schwartz, 2009). Mindfulness is also one component of a modified dialectical behavior therapy group skills training program for ADHD in adulthood that has received empirical support. These studies indicate improvement in self-reported ADHD symptoms (Hesslinger et al., 2002; Hirvikoski et al., 2011; Philipsen et al., 2007). Although promising, overall these studies have either included a heterogeneous sample of adults and adolescents, did not include a control group, or did not isolate the impact of mindfulness from other behavioral techniques. Also, few studies have expanded beyond targeting core ADHD symptoms.
Further, although rating scales and clinician-administered interviews are commonly implemented in treatment outcome research, these assessments rely on retrospective reporting. Assessment methods that target behavior in the natural setting may provide a more ecologically valid assessment (Barkley, 1991). Therefore, ecological momentary assessment (EMA) was utilized for the current study in addition to more traditional assessment approaches. EMA is a within-day self-assessment technique in which participants are prompted at random and/or predetermined intervals to assess their current behavior. EMA addresses limitations of traditional assessment techniques, including repeated assessment of participants in their normal daily environment (enhancing ecological validity) and assessment of behavior at the time of occurrence (minimizing the need to retrospectively recall) (Csikszentmihalyi & Larson, 1987; deVries, 1992; Reis & Gable, 2000; Shiffman, Stone, & Hufford, 2008).
Goals and Hypotheses
Mindfulness meditation training has received preliminary support as a treatment for ADHD in adulthood, though to date there have been no trials evaluating the impact of a mindfulness meditation training-only intervention against a comparison condition. Further, no studies to date have included a homogenous sample composed solely of adults diagnosed with ADHD or have incorporated EMA. Therefore, the aim of the current study was to assess the preliminary efficacy of a group-based mindfulness meditation training for adults with ADHD in comparison to a waitlist control group. Assessments included self-report rating scales, clinician rating scales, laboratory tasks of EF, and EMA. We hypothesized that ADHD symptoms, functional impairment associated with ADHD symptoms, EF, and emotion dysregulation would improve in the treatment group over time in comparison to a waitlist control group. We also conducted an exploratory analysis of EF and emotion dysregulation subscales. Since this is the first trial of a mindfulness meditation training-only intervention in a sample composed entirely of adults with ADHD, we assessed feasibility and treatment acceptability.
Methods
Participants
The sample for the current study was composed of adults diagnosed with ADHD (see Table 1 for a summary). Participants were recruited from the community via advertisements, word of mouth, and referrals from local clinics. Inclusion criteria included age 18–50 years; met DSM-IV (APA, 1994) criteria for ADHD; intellectual functioning ≥ 80; T-score ≥ 65 on the Conners’ Adult ADHD Rating Scale-Self-Report (CAARS; Conners, Erhardt, & Sparrow, 1999) for either the Inattentive Symptoms subscale, Hyperactive-Impulsive Symptoms subscale, Total DSM-IV Symptoms subscale, or ADHD Index; Clinical Global Impression score ≥ 4; and were generally healthy (i.e., no major medical problems). Participants were not required to have received a diagnosis of ADHD prior to study participation. Exclusion criteria included: met criteria for an DSM-IV Axis I disorder other than ADHD that was the primary diagnosis and required clinical intervention; an Axis II disorder diagnosis; unable to attend sessions; and anticipated substantial changes in psychiatric medication treatment status (i.e., changes in type or dose of medication in the next six months). Comorbidity was not an exclusion criterion providing that ADHD symptoms were the primary concern and target for treatment according to the clinician performing the assessment (a PhD-level licensed clinical psychologist) and study participant. Participants taking psychotropic medications were allowed to participate and encouraged to continue their treatment with minimal changes throughout the study—any changes during the course of the study were recorded. Two participants in the treatment group reported changes in their psychiatric medication regimen during their enrollment. One participant was prescribed Percocet (five 2.5mg/325mg tablets) to take for tooth pain during week two of treatment, whereas another participant stopped taking a prescription for Adderall XR for seven days during week six of treatment. The latter change in medication status was unplanned. None of the participants in the waitlist reported any changes in medication use during their enrollment. This study was approved by the local IRB.
Table 1.
Participant baseline characteristics for treatment (n = 11) and waitlist (n = 9) groups
| Treatment | Waitlist | Test Statistic | p-value | |
|---|---|---|---|---|
| Age (SD) | 40.55 (6.83) | 36.22 (6.92) | t (18) = 1.40 | .18 |
| Sex (%) | χ2 (1) = .30 | .58 | ||
| Males | 5 (45.5%) | 3 (33.3%) | ||
| Females | 6 (54.5%) | 6 (66.7%) | ||
| Race (%) | χ2 (2) = .86 | .65 | ||
| White | 9 (81.8%) | 8 (88.9%) | ||
| Black | 1 (9.1%) | 1 (11.1%) | ||
| Native Haw./Pac. Isl. | 1 (9.1%) | 0 (0%) | ||
| Ethnicity (%) | χ2 (1) = .86 | .35 | ||
| Not Hispanic or Latino | 10 (90.9%) | 9 (100%) | ||
| Hispanic or Latino | 0 (0%) | 0 (0%) | ||
| Did not specify | 1 (9.1%) | 0 (0%) | ||
| Marital Status (%) | χ2 (1) = .74 | .39 | ||
| Married | 7 (63.6%) | 4 (44.4%) | ||
| Unmarried | 4 (36.4%) | 5 (55.6%) | ||
| Employment Status (%) | χ2 (3) = 1.41 | .70 | ||
| Full-time | 9 (81.8%) | 6 (66.7%) | ||
| Part-time | 1 (9.1%) | 1 (11.1%) | ||
| Unemployed | 0 (0%) | 1 (11.1%) | ||
| Other | 1 (9.1%) | 1 (11.1%) | ||
| Salary Range (%) | χ2 (3) = 4.66 | .19 | ||
| ≤ $10K | 2 (18.2%) | 4 (44.4%) | ||
| $10K – $25K | 3 (27.3%) | 0 (0%) | ||
| $25K – $50K | 3 (27.3%) | 4 (44.4%) | ||
| > $50K | 3 (27.3%) | 1 (11.1%) | ||
| Highest Degree Earned (%) | χ2 (2) = 2.97 | .23 | ||
| High school degree | 3 (27.3%) | 0 (0%) | ||
| College degree | 3 (27.3%) | 4 (44.4%) | ||
| Graduate degree | 5 (45.5%) | 5 (55.6%) | ||
| KBIT (SD) | 117.45 (15.49) | 125.44 (10.44) | t (18) = −1.32 | .20 |
| ADHD Subtype (%) | χ2 (1) = .29 | .77 | ||
| Combined | 3 (27.3%) | 3 (33.3%) | ||
| Inattentive | 8 (72.7%) | 6 (66.7%) | ||
| CGI (SD) | 4.91 (0.70) | 4.67 (0.71) | t (18) = .77 | .45 |
| Comorbid Diagnosis (%) | χ2 (1) = 2.15 | .14 | ||
| Yes | 6 (54.5%) | 2 (22.2%) | ||
| No | 5 (45.5%) | 7 (77.8%) | ||
| ADHD Med. Status (%) | χ2 (1) = .002 | .96 | ||
| Yes (stimulant) | 6 (54.5%) | 5 (55.6%) | ||
| No | 5 (45.5%) | 4 (44.4%) | ||
| Non-ADHD Med. Status (%) | χ2 (1) = .02 | .88 | ||
| Yes | 4 (36.4%) | 3 (33.3%) | ||
| No | 7 (63.4%) | 6 (66.7%) | ||
| CAARS (SD) | ||||
| DSM-IV Inattentive T-score | 85.45 (7.01) | 84.00 (8.41) | t (18) = .42 | .68 |
| DSM-IV Hyp-Imp T-score | 73.00 (9.97) | 66.22 (10.78) | t (18) = 1.46 | .16 |
| Beck Depression Inventory (SD) | 14.55 (7.26) | 11.89 (5.97) | t (18) = .88 | .39 |
| Beck Anxiety Inventory (SD) | 10.46 (7.45) | 6.44 (5.00) | t (18) = 1.38 | .19 |
Note. Native Haw./Pac. Isl. = Native Hawaiian/Pacific Islander; KBIT = Kaufman Brief Intelligence Test, Second Edition, CAARS = Conners’ Adult ADHD Rating Scale, CGI = Clinical Global Impression, Hyp-Imp = Hyperactive-Impulsive.
Measures
Screening and Diagnostic Measures
Following informed consent, demographic information and medical, psychiatric, and substance use histories were collected at a screening visit. IQ was assessed by the Kaufman Brief Intelligence Test, Second Edition (Kaufman & Kaufman, 2004). The Childhood ADHD Symptom Scale-Self-Report (Barkley & Murphy, 2006) and the Conners Adult ADHD Rating Scale (CAARS)-Self-Report (Conners et al., 1999) were administered, followed by the Conners Adult Diagnostic Interview for DSM-IV (CAADID; Epstein, Johnson, & Conners, 2000) to assess full ADHD diagnostic criteria. The computerized Structured Clinical Interview for the DSM-IV (SCID; First, Spitzer, Williams, & Gibbon, 2002) and follow-up clinical interviewing to assess Axis I disorders was also conducted. All interviews were administered by a PhD-level clinical psychologist.
Treatment outcome
Assessments of response to treatment included (a) self-report rating scales and clinician-administered interviews completed in the laboratory, (b) EF laboratory tasks, and (c) self-report rating scales completed via electronic diary outside of the laboratory.
Treatment outcome: Rating scales and clinician interviews
ADHD symptoms were assessed in the laboratory with the self-report and un-blinded clinician rating versions of the Current ADHD Symptoms Scale (Barkley & Murphy, 2006). In addition to assessing all 18 symptoms for ADHD from the DSM-IV, this measure assesses 10 different domains that could be impacted by these symptoms (e.g., “In your home life with your immediate family”). Participant ratings for this scale ranged from 1 (“not all or rarely”) to 4 (“very often”). This scale or similar versions are widely administered in adult ADHD psychosocial treatment outcome research (e.g., Hirvikoski et al., 2011; Safren et al., 2005, 2010; Zylowska et al., 2008). Similar to past treatment outcome studies (e.g., Safren et al., 2005, 2010), ADHD symptoms were assessed within the past week.
EF rating scales included the Deficits in Executive Functioning Scale (DEFS; Barkley, 2011) and the Behavior Rating Inventory of Executive Functioning-Adult Version (BRIEF-A; Roth, Isquith, & Gioia, 2005). The DEFS included the 89-item self-report form and the 20-item clinician interview form. Response options for both versions of the DEFS ranged from 1 (“never or rarely”) to 4 (“very often”). The DEFS includes five subscales measuring various facets of EF and an overall total score. The DEFS has high internal consistency (Biederman et al., 2008; Fedele, Hartung, Canu, & Wilkowski, 2010), good test-retest reliability (Barkley, 2011), good discriminant validity (Biederman, et al., 2008; Fedele, et al., 2010), and is associated with various indices of impairment that suggests good ecological validity (Barkley & Fischer, 2011; Barkley & Murphy, 2010b; Biederman, et al., 2008). For the current study, the DEFS was modified to assess EF behaviors over the past week. The BRIEF-A is a 75-item self-report form with response options ranging from 1 (“never”) to 3 (“often”). The BRIEF-A assesses EF behaviors over the past 30 days. The BRIEF-A yields an overall total score (i.e., Global Executive Composite) that is composed of two index scores (i.e., the Behavioral Regulation Index and Metacognitive Index). The Behavioral Regulation index contains four subscales (Inhibit, Shift, Emotional Control, and Self-Monitor) and the Metacognitive Index is composed of five subscales (Initiate, Working Memory, Plan/Organize, Task Monitor, and Organization of Materials). The BRIEF-A has excellent internal consistency for the three main higher order indices, excellent test-retest reliability, and has demonstrated convergent and divergent validity (Roth, et al., 2005). Internal consistency of the nine subscales ranges from acceptable to good (Giancola, Godlaski, & Roth, 2012).
Emotion dysregulation was assessed by the Difficulties in Emotion Regulation Scale (DERS; Gratz & Roemer, 2004) and the Distress Tolerance Scale (DTS; Simons & Gaher, 2005).The DERS is a 36-item scale that assesses how often emotionally dysregulated behavior occurs on a scale from 1 (“almost never”) to 5 (“almost always”). The DERS has high internal consistency, good test-retest reliability, and adequate construct and predictive validity (Gratz & Roemer, 2004). The DTS is a 15-item scale with response options ranging from 1 (“strongly agree”) to 5 (“strongly disagree”). The DTS measures distress tolerance, which is a construct proposed to be a component of emotional dysregulation (Leyro, Zvolensky, & Bernstein, 2010). Higher scores on this scale indicate higher tolerance for psychological distress. The DTS has demonstrated good internal consistency, in addition to convergent and discriminant validity (Simons & Gaher, 2005). Both the DERS and DTS were modified to assess behavior over the past week.
Treatment outcome: Laboratory tasks
To measure components of EF, the following laboratory tasks were administered: the Attention Network Task (ANT; Fan & Posner, 2004), which is a computerized test measuring alerting (maintaining a vigilant state of preparedness), orienting (selecting a stimulus among multiple inputs), and conflict (prioritizing among competing tasks); Conners’ Continuous Performance Test (CPT; Conners, 1995), which is a measure of response inhibition; the Digit Span Test (Wechsler, 2008), which is a measure of working memory; and the Trail Making Test (Reitan, 1979), which assesses attentional set-shifting and inhibition. These tasks were selected primarily based on findings from Zylowska et al. (2008).
Treatment outcome: EMA
ADHD and EF symptoms were assessed via electronic diary as well. All 18 DSM-defined ADHD symptoms (APA, 2000) were administered to assess inattentive and hyperactive-impulsive ADHD symptoms at the moment of each assessment on a scale from 1 (“not at all”) to 5 (“extremely”). The DEFS (20-item) and an abbreviated BRIEF-A (27-item) were administered to assess EF at the moment of each assessment on a scale from 1 (“not at all”) to 5 (“extremely”). For the BRIEF-A, three items from each subscale were selected. These items were selected based on the magnitude of the correlation that item had with total scores (self-reported) reported in the BRIEF-A manual (Roth et al., 2005). The three highest magnitudes were chosen for each subscale.
Feasibility and treatment acceptability
Feasibility was assessed by examining treatment group attrition and session attendance. Consistent with past adult ADHD treatment outcome research (Hirvikoski et al., 2011), attrition of <25% and attendance of ≥ 75% of sessions were set to establish feasibility. Homework compliance was also considered for feasibility. Therapists completed an item assessing the degree to which each group member was compliant with homework immediately after each session. Therapists provided a rating on a scale of 1 (not at all) to 5 (extremely strong). Treatment acceptability was evaluated based on responses to an evaluation questionnaire adapted from (Bramham et al., 2009), which assessed how satisfactory participants felt that the treatment was overall (ranging from 1–7 with 7 indicating the highest rating of treatment satisfaction). Additional acceptability items assessed participant perceptions about the extent of ADHD psychoeducation they received, how the content was relevant to their experiences, whether the techniques/strategies introduced were understandable, if they were confident about regularly using the techniques taught, and if they would recommend mindfulness training to other adults with ADHD (on a scale ranging from 1 [not at all] to 4 [extremely]).
Procedures
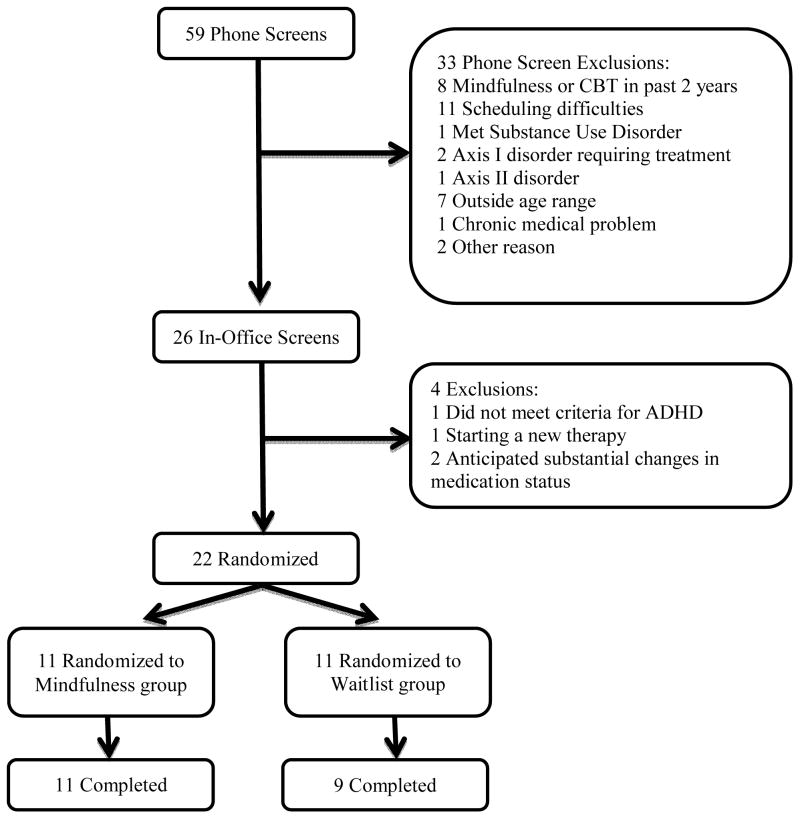
Three laboratory visits were required: screening, baseline assessment, and eight-week assessment. Fifty-nine potential participants completed a telephone prescreen and 26 were invited for an in-person screening. Among the reasons for being excluded following telephone prescreening included: received cognitive-behavioral therapy for ADHD or mindfulness training in the past two years (n = 8), scheduling difficulty (n = 11), diagnosed with a substance use disorder requiting treatment (n = 1), outside of required age range (n = 7), diagnosed with a non-substance use Axis I disorder other than ADHD requiring treatment (n = 2), chronic medical problems (n = 1), diagnosed with an Axis II disorder (n = 1), and other reasons (n = 2)1. Among the 26 invited for the in-person screening, four failed the in-person screening for various reasons (n = 2 for anticipated substantial changes in their psychiatric medication status, n = 1 for not meeting diagnostic criteria for ADHD, and n = 1 for initiating psychotherapy involving aspects of mindfulness at the time of the assessment). A total of 22 subjects were enrolled. Participants were stratified by ADHD medication status and otherwise randomized to the treatment group (n = 11) or waitlist control group (n = 11). Two participants in the waitlist group dropped out soon after randomization due to (a) a substantial change in psychiatric medication status and (b) time constraints that restricted participation. Figure 1 summarizes sample recruitment. Table 1 summarizes sample characteristics.
Figure 1.
Sample recruitment and participation flowchart. CBT = Cognitive-Behavioral Therapy
Following office screening visits conducted by a Master’s level research coordinator and a Ph.D. clinical psychologist, participants were stratified by ADHD medication status and randomized to a treatment or waitlist group. A waitlist group was chosen to control for the effects of time between assessments. Baseline and eight-week assessments were conducted within two weeks immediately prior to and following treatment for the treatment group. During both visits, medications were taken as prescribed. Dosage amount and timing of dosage was assessed to ensure uniformity. Ecological momentary assessments for two-day periods during baseline and eight-week assessments were also conducted. For these assessments, participants carried an electronic diary with them for two days and completed questionnaires about their behavior at that moment when prompted by an audible alarm (see below).
EMA Procedures
Participants received individual electronic diary training during baseline assessment visits. Assessment questionnaire and a random alarm mechanism were designed with Entryware Designer software version 6.3 developed by Techneos Systems, Inc. The electronic diaries were administered on Treo 755P handheld computers. After completing training in the use of the handheld electronic diaries (approximately 30 minutes), participants began a two-day sampling period. During this period, participants were prompted to complete an EMA entry by alarm. Alarm entries took approximately 2–4 minutes. These entries included questions about the participant’s situation, affect, ADHD symptoms, and EF symptoms. ADHD and EF symptoms were considered in the current study. Alarm entries were initiated by an audible alarm approximately every 1.25 hours during waking hours to result in approximately 10 alarms daily. If participants did not respond within two minutes after the alarm sounded (six audible beeps), the electronic diary would not allow the participant to respond, a missed alarm was recorded, and the alarm would reset to go off approximately 10 to 20 minutes later. If participants did respond within two minutes of an alarm, they were provided the option to choose “snooze” (the alarm would sound five minutes later), “skip” (the alarm would be delayed and sound 30–40 minutes later) or “answer.” Participants were instructed on how to turn off the audible alarm while they slept, and for short periods during the day when it may be dangerous (e.g., driving) or inappropriate (e.g., showering) to respond. Participants were allowed to choose how long to temporarily turn off the alarm, though the alarm did not require reactivation as it was programmed to automatically resume.
Mindfulness Meditation Training
The Mindful Awareness Practices (MAPs) for ADHD program (Zylowska et al., 2008) was administered (see (Mitchell, et al., submitted) and Zylowska et al., 2008, for more thorough descriptions) by a PhD-level clinical psychologist. This eight-week program was composed of weekly group therapy sessions lasting 2.5hrs and involved daily at-home practice. To complement material discussed in session, participants received a resource that facilitates use of mindfulness skills and is based on the MAPs program: The Mindfulness Prescription for Adult ADHD (Zylowska, 2012). This included a book that details various mindfulness practices taught in the group and a CD audio program that provided instruction for formal mindfulness meditation exercises (ranging from approximately 5–15 minutes). Any explicit directions on cognitive-behavioral therapy techniques within the book were removed prior to dispensing them to participants to minimize the potential influence of other treatment modalities. In the treatment itself, cognitive-behavioral therapy techniques are introduced during the final session (e.g., use of a calendar and reminders to encourage mindfulness meditation practices). Although this is an application of skills that are also taught in manualized cognitive behavioral approaches (e.g., Safren, Perlman, Sprich, & Otto, 2005; Solanto, 2011), these skills are introduced in the context of supporting mindfulness practice only. Explicit instruction and demonstration of these cognitive-behavioral strategies are not provided as they are in manualized CBT interventions for adult ADHD.
Waitlist participants did not engage in any changes to any pre-existing treatments during the eight week period. After the eight-week assessment, waitlist group participants were administered the same treatment as the treatment group.
Participants were compensated up to US$115 for completing the study and an additional US$50 for returning electronic diary equipment at the end of the study.
Data Reduction and Analysis
Electronic diary data reduction
EMA entries that were not completed within 25 minutes were removed. This time restriction resulted in removal of 26 alarm entries across the entire sample. A total of 797 readings were analyzed for the current study. Across the baseline and eight-week assessments (i.e., four days of EMA entries), the mean number of EMA entries was 39.85 (SD = 5.37, range 26–48).
Data analysis
A repeated measures mixed design analysis of variance (ANOVA) was conducted with group status (treatment, waitlist) as the between subjects factor and time (baseline assessment, 8-week assessment) as the within subjects factor. Group by time interactions were considered to assess changes between groups over the two time points. Dependent variables included ADHD symptoms, functioning associated with ADHD symptoms, EF, and emotion dysregulation. All analyses were conducted with SPSS 19.0, with the exception of EMA analyses, which were conducted with SAS 9.2 (SAS Inc., 2008). To account for the nesting of multiple observations within subjects, EMA data were analyzed using generalized estimating equations (Zeger, Liang, & Albert, 1988). Group by time interactions were considered for these analyses. Effect sizes were also computed for continuous outcome variables (d = Meanchangescore treatment group − Meanchangescore comparison group/SDpooled). A decrease of ≥ 30% of symptom severity scores was also considered for ADHD symptoms, EF and emotion dysregulation total scale scores, which is consistent with guidelines used in other adult ADHD psychosocial treatment trials (Safren et al., 2010; Solanto et al., 2010; Zylowska, et al., 2008).
Results
Feasibility and Acceptability
In terms of feasibility, all participants randomized to the treatment group completed the study, whereas two of 11 in the waitlist group did not complete the study (see above). Among the treatment group, they attended 7.2 (SD = 0.87) out of 8 sessions, which was an overall attendance rate of 89.8% of sessions. In terms of compliance with homework assignments, participants averaged a homework completion score of 3.9 (SD = 0.36) on a scale of 1 to 5.
Regarding treatment acceptability, treatment group participants completed a treatment satisfaction scale. One item assessed how well participants felt that the treatment was overall (ranging from 1–7 with 7 indicating the highest satisfaction), which indicated that overall treatment was well-liked (M = 5.91, SD = 1.14). On a scale ranging from 1 (not at all) to 4 (extremely), participants reported that they learned more about ADHD (M = 3.27, SD = 0.91), the content they learned was relevant to their experiences (M = 3.55, SD = 0.93), the techniques/strategies introduced were understandable (M = 3.82, SD = 0.41), they were confident about regularly using the techniques taught (M = 3.36, SD = 0.67), and they would recommend mindfulness training to other adults with ADHD (M = 3.64, SD = 0.92).
Outcome Variables
ADHD symptoms and functioning
Interaction terms were significant for self-reported inattentive ADHD symptoms (p = .002), clinician ratings of inattentive ADHD symptoms (p < .001), and self-reported EMA ratings of inattentive ADHD symptoms (p = .002). These scores demonstrated an improvement in symptoms for the treatment group over time relative to the waitlist group. Effect sizes were in the large range (d = 1.66, 3.14, and 1.09, respectively). Similar group differences emerged when hyperactive-impulsive ADHD symptoms were considered (self-reported: p = .001; clinician rating: p = .008; and EMA rating: p = .003). Effect sizes for between groups change scores were in the large range for these analyses (d = 1.76, 1.35, and 0.75, respectively). Functional impairment related to ADHD symptoms also improved in the treatment group according to self-report (p = .002) and clinician ratings (p = .003) with large effect sizes (d = 1.66 and 1.52, respectively). See Tables 2 for a summary of self-report and clinician ratings of ADHD symptoms and Table 4 for a summary of EMA ratings of ADHD symptoms.
Table 2.
Rating scale scores (self-report and clinician ratings)
| Treatment Group (n = 11) | Waitlist Control Group (n = 9) | p-value | Cohen’s d | |||
|---|---|---|---|---|---|---|
| Baseline | 8 Week Assessment | Baseline | 8 Week Assessment | |||
| M (SD) | M (SD) | M (SD) | M (SD) | |||
| ADHD Symptoms (self-report) | ||||||
| Inattention | 26.46 (4.85) | 17.27 (4.88) | 27.44 (3.68) | 26.11 (5.01) | .002 | 1.66 |
| Hyperactive-Impulsive | 23.09 (5.32) | 13.73 (3.66) | 20.56 (3.54) | 20.11 (5.49) | .001 | 1.76 |
| ADHD Symptoms (clinician) | ||||||
| Inattention | 29.00 (3.63) | 17.18 (4.26) | 27.78 (3.42) | 27.44 (3.84) | <.001 | 3.14 |
| Hyperactive-Impulsive | 22.27 (6.71) | 13.46 (2.77) | 18.89 (4.20) | 17.67 (4.64) | .008 | 1.35 |
| ADHD Functioning (self) | 28.64 (6.10) | 18.55 (3.86) | 26.11 (5.30) | 26.33 (6.61) | .002 | 1.66 |
| ADHD Functioning (clinician) | 26.73 (4.34) | 18.91 (3.62) | 26.56 (4.36) | 25.89 (6.01) | .003 | 1.52 |
| DEFS (self-report) | ||||||
| Total | 238.36 (41.41) | 174.36 (29.32) | 224.78 (39.81) | 215.44 (31.72) | .005 | 1.45 |
| Self-Management to Time | 68.55 (12.90) | 48.73 (9.01) | 68.00 (8.86) | 65.22 (8.57) | <.001 | 1.90 |
| Self-Organization | 61.00 (16.06) | 45.09 (9.28) | 57.67 (12.68) | 56.89 (9.93) | .03 | 1.09 |
| Self-Discipline | 47.09 (11.23) | 36.18 (6.54) | 40.44 (8.34) | 40.67 (8.53) | .03 | 1.04 |
| Self-Motivation | 29.09 (11.26) | 22.46 (7.58) | 32.56 (6.69) | 29.67 (6.61) | .12 | 0.73 |
| Self-Regulation of Emotion | 32.64 (11.65) | 21.91 (5.01) | 26.11 (9.60) | 23.00 (7.38) | .10 | 1.09 |
| DEFS (clinician) | ||||||
| Total | 52.36 (7.71) | 31.73 (4.67) | 50.22 (8.73) | 48.22 (9.76) | <.001 | 2.67 |
| Self-Management to Time | 13.18 (1.72) | 8.18 (1.94) | 13.33 (1.58) | 12.89 (1.62) | <.001 | 2.91 |
| Self-Organization | 9.46 (3.24) | 6.36 (2.01) | 9.78 (2.64) | 9.33 (3.16) | .01 | 1.30 |
| Self-Discipline | 10.09 (2.70) | 6.00 (1.79) | 8.11 (2.21) | 8.44 (3.01) | .001 | 1.75 |
| Self-Motivation | 9.64 (3.83) | 5.91 (2.07) | 10.22 (2.82) | 9.33 (2.74) | .03 | 1.05 |
| Self-Regulation of Emotion | 10.00 (3.13) | 5.27 (1.49) | 8.78 (3.27) | 8.22 (3.46) | .003 | 1.56 |
| BRIEF-A | ||||||
| Total | 158.36 (15.59) | 137.09 (20.29) | 153.89 (19.30) | 157.89 (18.33) | .003 | 1.55 |
| Inhibit | 18.55 (2.38) | 15.73 (2.83) | 16.00 (2.35) | 16.67 (2.40) | .008 | 1.35 |
| Shift | 12.36 (2.50) | 10.91 (1.64) | 13.11 (3.14) | 14.22 (2.49) | .046 | 0.96 |
| Emotional Control | 20.18 (5.55) | 16.82 (2.79) | 15.44 (4.59) | 15.56 (5.03) | .09 | 0.81 |
| Self-Monitor | 12.91 (2.77) | 9.91 (1.92) | 11.44 (3.05) | 11.89 (2.57) | .001 | 1.72 |
| Behavioral Regulation Index | 64.00 (10.13) | 53.36 (6.33) | 56.00 (9.98) | 58.33 (8.76) | .003 | 1.53 |
| Initiate | 17.64 (3.35) | 16.09 (3.05) | 19.22 (3.03) | 19.56 (2.96) | .10 | 0.78 |
| Working Memory | 18.64 (3.01) | 17.00 (3.22) | 19.89 (2.03) | 20.00 (2.12) | .14 | 0.69 |
| Plan/Organize | 25.18 (2.60) | 22.36 (4.39) | 25.11 (2.32) | 24.44 (3.13) | .15 | 0.67 |
| Task Monitor | 14.91 (1.76) | 13.00 (2.53) | 14.67 (2.18) | 14.22 (2.11) | .07 | 0.85 |
| Organization of Materials | 18.00 (4.96) | 15.46 (5.32) | 19.78 (3.35) | 20.22 (3.19) | .04 | 1.00 |
| Metacognition Index | 94.36 (11.72) | 83.73 (15.31) | 98.67 (10.25) | 98.44 (11.05) | .02 | 1.21 |
| DERS | ||||||
| Total | 99.27 (19.31) | 74.00 (17.03) | 95.78 (21.32) | 91.44 (19.44) | .002 | 1.63 |
| Nonacceptance of Emotion Responses | 15.36 (4.18) | 11.64 (4.37) | 17.11 (7.13) | 14.11 (6.68) | .63 | 0.22 |
| Difficulty Engaging in Goal-Directed Behavior | 18.27 (5.46) | 13.46 (5.37) | 20.33 (3.43) | 18.67 (4.00) | .14 | 0.70 |
| Impulse Control Difficulties | 14.09 (4.61) | 8.73 (2.49) | 11.67 (3.61) | 12.44 (3.75) | .002 | 1.60 |
| Lack of Emotional Awareness | 17.00 (4.05) | 15.18 (4.26) | 16.89 (5.37) | 15.67 (5.17) | .71 | 0.17 |
| Limited Access to Emotion Regulation Strategies | 20.73 (7.49) | 13.82 (6.18) | 17.44 (6.27) | 18.44 (7.14) | .007 | 1.38 |
| Lack of Clarity | 13.82 (3.49) | 11.18 (3.13) | 12.33 (3.71) | 12.11 (4.43) | .07 | 0.86 |
| Distress Tolerance Scale | ||||||
| Total | 47.00 (13.25) | 59.27 (10.12) | 46.11 (15.96) | 48.44 (13.31) | .01 | 1.27 |
Note. A decrease in scores is indicative of improvement for all rating scales with the exception of the Distress Tolerance Scale (higher scores = higher levels of distress tolerance); DEFS = Deficits in Executive Functioning Scale; BRIEF-A = Behavior Rating Inventory of Executive Functioning-Adult Version; DERS = Difficulties in Emotion Regulation Scale.
Table 4.
Ecological momentary assessment scores
| Treatment Group (n = 11) | Waitlist Control Group (n = 9) | p-value | Cohen’s d | |||
|---|---|---|---|---|---|---|
| Baseline | 8 Week Assessment | Baseline | 8 Week Assessment | |||
| M (SD) | M (SD) | M (SD) | M (SD) | |||
| Inattentive ADHD Symptoms | 16.85 (6.52) | 14.40 (3.53) | 19.06 (5.28) | 20.73 (3.68) | .002 | 1.09 |
| Hyp-Imp ADHD Symptoms | 14.77 (5.49) | 12.10 (2.80) | 12.73 (2.25) | 13.08 (2.19) | .003 | 0.75 |
| DEFS | ||||||
| Total | 33.49 (9.42) | 29.21 (5.24) | 37.02 (8.75) | 37.66 (4.61) | .045 | 0.65 |
| Self-Management to Time | 9.84 (3.34) | 7.57 (1.89) | 10.60 (2.94) | 11.85 (1.92) | .001 | 1.36 |
| Self-Organization | 5.62 (1.94) | 5.19 (1.28) | 7.47 (2.63) | 7.52 (1.96) | .13 | 0.34 |
| Self-Discipline | 6.61 (2.52) | 5.65 (1.50) | 6.25 (2.08) | 6.31 (1.32) | .11 | 0.49 |
| Self-Motivation | 6.34 (2.25) | 5.51 (1.49) | 7.21 (1.55) | 6.95 (1.83) | .42 | 0.29 |
| Self-Regulation of Emotion | 5.10 (1.56) | 5.30 (1.59) | 5.48 (.83) | 5.03 (.69) | .22 | −0.36 |
| BRIEF-A | ||||||
| Total | 53.06 (18.21) | 44.68 (9.70) | 57.91 (16.45) | 57.20 (9.95) | .11 | 0.55 |
| Inhibit | 5.75 (2.31) | 4.41 (1.18) | 4.72 (1.11) | 4.87 (1.18) | .001 | 0.84 |
| Shift | 5.83 (2.23) | 5.05 (1.38) | 6.45 (2.24) | 6.15 (.93) | .40 | 0.26 |
| Emotional Control | 4.03 (1.40) | 3.94 (.99) | 4.75 (1.94) | 4.44 (1.02) | .38 | −0.13 |
| Self-Monitor | 3.97 (1.34) | 3.49 (.72) | 3.84 (.94) | 3.65 (.50) | .27 | 0.24 |
| Initiate | 7.37 (2.80) | 6.18 (1.98) | 8.39 (2.75) | 8.47 (2.14) | .15 | 0.53 |
| Working Memory | 6.01 (2.49) | 4.70 (1.25) | 6.46 (2.37) | 6.62 (1.57) | .01 | 0.83 |
| Plan/Organize | 7.52 (3.26) | 6.41 (2.02) | 8.40 (2.43) | 8.86 (2.42) | .06 | 0.56 |
| Task Monitor | 6.46 (2.92) | 5.44 (1.59) | 7.61 (2.06) | 7.72 (1.84) | .11 | 0.56 |
| Organization of Materials | 6.12 (2.96) | 5.06 (2.14) | 7.29 (2.30) | 6.42 (1.96) | .81 | 0.09 |
Note. Hyp-Imp = Hyperactive-Impulsive symptoms; DEFS = Deficits in Executive Functioning Scale; BRIEF-A = Behavior Rating Inventory of Executive Functioning-Adult Version (27 items total, 3 items per subscale). There was a total of 797 entries. Means were calculated from summing items composing each respective scale and subscale (response options ranging from 1 to 5 for each item). The scales or subscale, and items they contained were: Inattentive ADHD Symptoms (9 items), Hyperactive-Impulsive ADHD Symptoms (9 items), DEFS total score (20 items), Self-Management (4 items), Self-Organization (4 items), Self-Discipline (4 items), Self-Motivation (4 items), Self-Regulation of Emotion (4 items), BRIEF-A total score (27 items), Inhibit (3 items), Shift (3 items), Emotional Control (3 items), Self-Monitor (3 items), Initiate (3 items), Working Memory (3 items), Plan/Organize (3 items), Task Monitor (3 items), Organization of Materials (3 items).
Regarding symptom reduction, 63.6% in the treatment group exhibited 30% reduction for self-reported inattentive and hyperactive-impulsive symptoms in comparison to 0% in the waitlist group (χ2 = 8.81, p = .003 for both analyses). Similar findings emerged for clinician ratings (inattention: 81.8% treatment group, 0% waitlist, χ2 = 13.39, p < .001; hyperactive-impulsive: 72.7% treatment group, 11.1% waitlist, χ2 = 7.59, p = .006). For EMA ratings, 27.3% from the treatment group and 0% from the waitlist group improved for both inattentive and hyperactive-impulsive symptoms separately (χ2 = 2.89, p = .09 for inattentive and hyperactive-impulsive symptoms).
Executive functioning
When interaction terms were considered for EF, total scale scores for self-reported DEFS (p = .005), clinician rated DEFS (p < .001), and self-reported BRIEF-A (p = .003) scores were statistically significant and indicated that the treatment group improved relative to the waitlist group over time (Table 2). Effect sizes for these scales were large (d = 1.45, 2.67 and 1.55, respectively). None of the EF lab tasks differed between groups across time (Table 3).
Table 3.
Executive functioning laboratory task scores
| Treatment Group (n = 11) | Waitlist Control Group (n = 9) | p-value | Cohen’s d | |||
|---|---|---|---|---|---|---|
| Baseline | 8 Week Assessment | Baseline | 8 Week Assessment | |||
| M (SD) | M (SD) | M (SD) | M (SD) | |||
| ANT | ||||||
| Alerting | 50.11 (13.69) | 48.03 (24.73) | 32.96 (38.13) | 30.07 (26.57) | .96 | −0.02 |
| Orienting | 69.95 (29.07) | 64.78 (34.73) | 75.00 (40.53) | 72.60 (31.47) | .84 | 0.09 |
| Conflict | 110.31 (23.42) | 95.57 (25.44) | 125.08 (65.47) | 106.08 (30.98) | .81 | −0.11 |
| Trail Making Test | ||||||
| Trial A | 27.80 (7.34) | 26.45 (5.85) | 34.01 (7.96) | 27.11 (8.34) | .18 | −0.64 |
| Trial Ba | 58.71 (20.14) | 56.70 (13.02) | 64.08 (35.35) | 49.78 (12.23) | .30 | −0.50 |
| Digit Span | ||||||
| Forward | 11.45 (2.73) | 12.36 (2.25) | 11.11 (2.47) | 12.22 (2.17) | .84 | 0.09 |
| Backward | 9.00 (1.84) | 9.27 (2.61) | 8.67 (1.87) | 9.44 (1.24) | .60 | 0.24 |
| Mixed | 10.27 (1.68) | 10.09 (1.76) | 10.33 (3.00) | 10.33 (1.23) | .86 | 0.08 |
| CPTa | ||||||
| Omission | 1.10 (2.18) | 0.90 (1.29) | 1.11 (1.36) | 1.22 (2.28) | .79 | 0.13 |
| Commission | 13.50 (9.83) | 10.70 (9.36) | 11.44 (5.94) | 10.11 (9.23) | .63 | 0.23 |
| RT | 389.27 (66.79) | 388.61 (51.77) | 404.45 (46.21) | 419.69 (63.93) | .42 | 0.39 |
| RT SE | 4.48 (1.35) | 4.03 (0.80) | 4.87 (1.33) | 5.04 (1.89) | .30 | 0.51 |
| Variability | 5.29 (2.26) | 4.76 (1.66) | 6.13 (3.07) | 5.97 (3.63) | .81 | 0.11 |
| Detectability | 0.85 (0.57) | 0.88 (0.60) | 0.82 (0.41) | 0.97 (0.55) | .84 | 0.21 |
| Response style (beta) | 0.55 (0.45) | 0.85 (0.65) | 0.34 (0.41) | 0.52 (0.57) | .71 | −0.18 |
| Perseverations | 0.20 (0.42) | 0.70 (1.57) | 0.56 (1.01) | 0.22 (0.67) | .19 | −0.65 |
Note. ANT = Attention Network Task; CPT = Conners’ Continuous Performance Test; RT = Reaction Time; RT SE = Reaction Time Standard Error.
Treatment sample size varies for analysis of Trial B (n = 10) due to testing error and CPT (n = 10) due to poor participant compliance.
Exploratory analysis of subscale scores indicated that the following group by time interactions were statistically significant: DEFS Self-Management to Time (self-report) (p < .001), DEFS Self-Organization (self-report) (p = .03), DEFS Self-Discipline (self-report) (p = .03), DEFS Self-Management to Time (clinician report) (p < .001), DEFS Self-Organization (clinician report) (p = .01), DEFS Self-Discipline (clinician report) (p = .001), DEFS Self-Motivation (clinician report) (p = = .03), DEFS Self-Regulation of Emotion (p = .003), BRIEF-A Inhibit (p = .008), BRIEF-A Shift (p = .046), BRIEF-A Self-Monitor (p = .001), BRIEF-A Behavioral Regulation Index (p = .003), BRIEF-A Organization of Materials (p = .04), and BRIEF-A Metacognitive Index (p = .003). Scores indicated that the treatment group improved relative to the waitlist group over time. Effect sizes for these subscale scores ranged from 0.96 to 2.91, which are considered large. See Table 2 for a summary.
When EMA ratings of EF were considered, the interaction for BRIEF-A total scores did not reach statistical significance (p = .11), though the effect size was large (d = .55). Scores on the DEFS total did improve (p = .045, d = .65). Exploratory analysis of subscale scores indicated that the following scores improved for the treatment group relative to the waitlist control group over time: DEFS Self-Management to Time (p = .001), BRIEF-A Inhibit (p = .001), BRIEF-A Working Memory (p = .01). Effect sizes for these subscales were in the large range (d = 1.36, 0.84, and 0.83, respectively; Table 4).
For EF symptom reduction, 27.3% in the treatment group exhibited ≥ 30% reduction for DEFS self-report total scores in comparison to 0% in the waitlist group (χ2 = 2.89, p = .09), 72.7% for the treatment group and 0% for the DEFS clinician ratings for total score (χ2 = 10.91, p = .001), and 9.1% for the treatment group and 0% for the BRIEF-A total score (χ2 = 0.86, p = .35), Regarding EMA EF measures, 18.2% from the treatment group and 0% for the waitlist group improved on the DEFS (χ2 = 1.82, p = .18), and 36.4% from the treatment group and 0% for the waitlist group improved on the BRIEF-A (χ2 = 4.09, p = .043).
Emotion dysregulation
Interaction terms were statistically significant for self-reported emotion dysregulation symptoms according to the DERS and DTS total scores (p = .002 and .01, respectively). Effect size scores were considered large (d = 1.63 and 1.27, respectively). Analysis of DERS subscale scores indicated that group by time interactions were statistically significant for Impulse Control Difficulties and Limited Access to Emotion Regulation Strategies with large effect sizes (p = .002 and .007, and d = 1.60 and 1.38, respectively). See Table 2 for a summary. Regarding symptom reduction on the DERS, 27.3% of the treatment group were responsive in comparison to 0% of the waitlist group (χ2 = 2.89, p = .089). On the DTS, 45.5% in the treatment group were responsive in comparison to 0% of the waitlist group (χ2 = 5.46, p = .02).
Discussion
The present study assessed the feasibility, treatment acceptability, and preliminary efficacy of a group-based mindfulness meditation training for adults diagnosed with ADHD on core symptoms, functional impairment associated with core symptoms, EF, and emotion dysregulation. The current study builds upon previous findings by including a comparison group, a sample composed solely of adults diagnosed with ADHD, not explicitly introducing other treatment modalities, incorporating an ecologically-valid assessment approach, and expanding treatment targets beyond core ADHD symptoms to include EF and emotion dysregulation.
Our analysis indicated that the MAPs program is a feasible and acceptable treatment. This feasibility and acceptability replicated findings from Zylowska et al. (2008), including low levels of attrition, high levels of attendance, moderate levels of homework compliance, and high overall treatment acceptability. Additional items assessing treatment were strong as well, including participants reporting that the content was relevant to their experiences, the techniques were understandable, they were confident about regularly using the techniques, and they would recommend mindfulness training to other adults with ADHD.
The hypothesis that ADHD symptoms, related functional impairment, EF, and emotion dysregulation would improve in the treatment group in comparison to waitlist subjects over time was generally supported with large effect sizes. Regarding ADHD symptoms based on self-report forms completed in the laboratory, clinician ratings, and EMA ratings, both inattentive and hyperactive-impulsive symptoms improved for the treatment group relative to the waitlist control group over time. Also, significantly more in the treatment group were considered responders than the waitlist group across self-report forms and clinician ratings, and trended in the predicted direction for EMA ratings for ADHD symptoms. Related functional impairment improved based on self-report forms completed in the laboratory and clinician ratings. These findings are consistent with Zylowska et al.’s (2008) findings in a mixed sample of adolescents and adults diagnosed with ADHD. In the latter study, self-report assessment forms of ADHD symptoms were utilized. Findings from the current study also indicate that EMA-based ADHD symptom ratings, clinician ratings of ADHD symptoms, and self-reported functional impairment associated with ADHD symptoms improve as well. Further, since a comparison group was included, these findings indicate that pre- to post-assessments changes in the treatment group are not attributable to the effects of time.
Regarding the hypothesis that EF would improve for the treatment group, our analyses yielded partial support. That is, total EF scores based on self-report and clinician ratings improved in the treatment group relative to the waitlist control group. The percentage of those considered treatment responders was statistically significant for clinician ratings, but not for self-report scales despite trending in the predicted direction. In addition, EF laboratory tasks yielded no statistically significant differences. These latter findings are in contrast to findings from Zylowska et al. (2008). Even though medication dosage levels did not change for any subjects taking ADHD medications at either assessment period, a parsimonious explanation for this discrepancy involves the lack of any medication washout period for the current study and that the majority of participants in each group were taking a prescribed stimulant medication at the time of their baseline and eight-week assessments. It is likely that these medications improved EF task performance, though future studies are warranted to address these findings and rule out other explanations. Should these differential findings between rating scales (self-report and clinician) and laboratory tasks be supported, analyses of EF symptoms should consider issues related to ecological validity in accordance with differing methods of assessment. For example, some have argued that daily EF deficits in ADHD are not captured by EF laboratory tasks (Barkley & Fischer, 2011; Brown, 2008). Consistent with this, EF behaviors assessed via the DEFS (i.e., a paper-and-pencil questionnaire that was also used in the current study) were more highly associated with poor functional outcomes (e.g., antisocial acts and poor driving) than a series of EF laboratory tasks (Barkley & Murphy, 2011). Further, both methods of EF assessment yielded low and predominantly non-significant correlations. In another study examining occupational functioning in a longitudinally assessed sample of hyperactive children, EF self-reported ratings were a stronger predictor than EF laboratory task scores in adulthood (Barkley & Fischer, 2011).
Although EMA analysis yielded EF total score group differences for one scale but not another, EF subscale analysis of EMA ratings indicated improvement in self-management to time (DEFS), inhibit (i.e., ability to appropriately stop engagement in a particular behavior at a certain time, BRIEF-A), and working memory (i.e., ability to hold information in one’s mind for the purpose of completing a task, BRIEF-A) scores. The former two subscale scores were consistent with findings from self-reported rating scale scores completed in the laboratory. When percentage of participants who were considered treatment responders was assessed, significantly more were within the treatment group for one scale, but not the other.
Finally, the hypothesis that emotion dysregulation would improve for the treatment group in comparison to a waitlist group over time was supported. Two self-report rating scales completed in the laboratory indicated improvement in ability to regulate behavior in the context of experiencing an aversive emotional state. When percentage of participants who were considered treatment responders was assessed, significantly more were within the treatment group for one scale, but not the other. However, the latter scale trended in the predicted direction. Subscale exploratory analysis of one of these measures indicated that the treatment group improved in perceived ability to remain in control of behavior when experiencing negative emotions and to regulate emotions effectively when feeling upset relative to the waitlist control group over time. As opposed to our analysis of EF, laboratory task performance, clinician ratings, and EMA ratings were not conducted for emotion dysregulation. However, self-reported emotion dysregulation scores tell a consistent story about feeling more in control of emotional functioning following mindfulness meditation training.
Limitations and Future Directions
Limitations of findings from the current study should be considered. First, the final sample size was small. Although the aim was to conduct a pilot trial to assess feasibility, treatment acceptability, and preliminary efficacy, future studies need to include larger sample sizes to ensure greater statistical power. Second, raters were aware of group status. Future studies should include raters who are blind to group status. Third, although outside the scope and design of the current study, mediators and moderators were not considered. For instance, some have argued that ADHD subtypes represent qualitatively different disorders (e.g., Grizenko, Paci, & Joober, 2010), which would suggest that findings from the current study may vary as a function of ADHD subtype status. Additional factors, such as gender, comorbidity, or race/ethnicity could be considered as well. Such analyses were not conducted so as to minimize the likelihood of Type I error, though should be explored in future investigations. Fourth, despite that the current study is the first mindfulness-only treatment study in adults with ADHD to include a comparison group, the comparison group was a waitlist condition. An active treatment comparison group should be conducted in future studies (Safren et al., 2010; Solanto et al., 2010). Relatedly, an active treatment comparison group would address whether any improvements were derived from participating in a therapeutic group. Fifth, immediate post-treatment outcome up to two weeks after treatment was conducted, although the long-term effects of mindfulness meditation training were not considered. Therefore, future studies should consider follow-up assessments. Sixth, in terms of null results involving the EF laboratory tasks, a limited number of tasks were administered. Future studies should consider a larger battery of EF tasks. Relatedly, a medication washout period should be considered. Seventh, corrections for multiple comparisons were not made given the preliminary nature of this study. However, using a less stringent correction than Bonferroni, such as the modified false discovery rate method (Narum, 2006) for 31 comparisons using ANOVA would adjust the p-value for statistical significance to .0124 and yield a similar interpretation of the results. Finally, the current study attempted to assess outcome variables from multiple sources (i.e., self-report and clinician) and methods of assessment (i.e., rating scale, interview, laboratory task performance, EMA). However, not all outcome variables were assessed accordingly. For example, emotion dysregulation was assessed only via two self-report rating scales.
One issue for future research involves how mindfulness training is administered in clinical practice: as a standalone treatment or as a supplement to existing therapies. Although the goal of the current study was to assess the preliminary efficacy of mindfulness without introducing other treatment modalities, given that cognitive-behavioral therapy is an efficacious treatment option for adults with ADHD (see Knouse & Safren, 2010 and Mongia & Hechtman, 2012, for reviews), any additive benefit of supplementing mindfulness to create a mindfulness-based cognitive-behavioral therapy approach for ADHD is worth consideration. Clarification of mechanisms of change attributable to mindfulness meditation training should be pursued in future studies as well. For example, although assessed as outcome variables in the current study, EF and emotion dysregulation have been proposed as mechanisms of change in mindfulness treatments (Hölzel, et al., 2011). Additional hypothesized mechanisms should also be considered and assess uniqueness to mindfulness (see (Mitchell, et al., submitted) for a review). For example, a number of mechanisms of change in cognitive-behavioral therapy for adults with ADHD has been proposed (Ramsay, 2010). Future studies should consider these constructs (e.g., maladaptive cognitions) and if they mediate improvement in treatment outcome variables for adults with ADHD.
Conclusions
The current study provides support for the feasibility, treatment acceptability, and preliminary treatment efficacy of mindfulness meditation training for adult ADHD. The current study overcomes past limitations, including the inclusion of a comparison group, administering mindfulness meditation training without introducing additional treatment modalities, inclusion of a homogenous sample composed solely of adults diagnosed with ADHD, and incorporation of EMA. In addition, treatment outcome variables expanded beyond core ADHD symptoms and considered the impact of mindfulness on EF and emotion dysregulation. These findings add to a growing literature suggesting that mindfulness meditation for ADHD in adulthood is a promising intervention and indicate that a larger, randomized clinical trial is warranted.
Acknowledgments
Funding
This study was primarily supported by the American Professional Society of ADHD and Related Disorders/Pond Family Foundation (J.T.M.). Additional funding support provided by the National Institute on Drug Abuse (K23 DA032577 to J.T.M., K24 DA023464 to S.H.K., and K24 DA016388 to J.C.B.).
We thank Lidia Zylowska, M.D., for providing the MAPs treatment manual and consultation during the early planning phase of this study, and Alaattin Erkanli, Ph.D., and Paul Dennis, Ph.D., for statistical consultation.
Biographies
John T. Mitchell, Ph.D., is an Assistant Professor of Psychiatry at Duke University School of Medicine and the Duke ADHD Program. His research interests include ADHD in adulthood, ADHD-smoking comorbidity, emotion dysregulation, and treatment development.
Elizabeth M. McIntyre, B.A., is a Clinical Trials Assistant in the Duke ADHD Program.
Joseph S. English, M.A., is a Clinical Research Coordinator in the Duke ADHD Program.
Michelle F. Dennis, B.A., is an Associate in Research in the Department of Psychiatry and Behavioral Sciences at Duke University Medical Center.
Jean C. Beckham, Ph.D., is a Professor of Psychiatry at the Duke University School of Medicine. Her research interests primarily involve the assessment and treatment of trauma, particularly as it occurs for men and women in military service and has published over 100 papers in peer-r journals.
Scott H. Kollins, Ph.D., is a Professor of Psychiatry and Director of the Duke ADHD Program at the Duke University School of Medicine. He has worked with adults, adolescents, and children with ADHD for over 15 years and has published over 100 papers in the areas of ADHD and psychopharmacology.
Footnotes
Other reasons included (a) one participant living in another state from where the study was conducted and therefore being unable to attend the group therapy regularly and (b) one participant calling soon after a phone screen citing “personal reasons” for not being able to potentially participate in the study (additional details were not provided).
Declaration of Interests
In the past 2 years, Dr. Kollins has received research support and/or consulting fees from the following: Addrenex/Shionogi, Akili Interactive, NIH/NIDA, Otsuka, Pfizer, Purdue Canada, Rhodes, Shire, Sunovion, and Supernus.
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 4th edition, Text Revision (DSM-IV-TR) Washington, D.C: American Psychiatric Association; 2000. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5) Washington, D.C: American Psychiatric Association; 2013. [Google Scholar]
- Barkley RA. The ecological validity of laboratory and analogue assessment methods of ADHD symptoms. Journal of Abnormal Child Psychology. 1991;19(2):149–178. doi: 10.1007/BF00909976. [DOI] [PubMed] [Google Scholar]
- Barkley RA. Deficient emotional self-regulation is a core component of Attention-Deficit/Hyperactivity Disorder. Journal of ADHD & Related Disorders. 2010;1(2):5–37. [Google Scholar]
- Barkley RA. The Deficits in Executive Functioning Scale (DEFS): Assessing Problems in Executive Functioning in Daily Life Activities. New York: Guilford Press; 2011. [Google Scholar]
- Barkley RA, Fischer M. The unique contribution of emotional impulsiveness to impairment in major life activities in hyperactive children as adults. Journal of the American Academy of Child & Adolescent Psychiatry. 2010;49(5):503–513. doi: 10.1016/j.jaac.2010.01.019. [DOI] [PubMed] [Google Scholar]
- Barkley RA, Fischer M. Predicting impairment in major life activities and occupational functioning in hyperactive children as adults: Self-reported executive function (EF) deficits versus EF tests. Developmental Neuropsychology. 2011;36(2):137–161. doi: 10.1080/87565641.2010.549877. [DOI] [PubMed] [Google Scholar]
- Barkley RA, Murphy KR. Attention-Deficit/Hyperactivity Disorder: A Clinical Workbook. Vol. 3. New York, NY: Guilford Press; 2006. [Google Scholar]
- Barkley RA, Murphy KR. Deficient emotional self-regulation in adults with attention-deficit/hyperactivity disorder (ADHD): The relative contributions of emotional impulsiveness and ADHD symptoms to adaptive impairments in major life activities. Journal of ADHD & Related Disorders. 2010a;1(4):5–28. [Google Scholar]
- Barkley RA, Murphy KR. Impairment in occupational functioning and adult ADHD: The predictive utility of executive function (EF) ratings versus EF tests. Archives of Clinical Neuropsychology. 2010b;25(3):157–173. doi: 10.1093/arclin/acq014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barkley RA, Murphy KR. The nature of executive function (EF) deficits in daily life activities in adults with ADHD and their relationship to performance on EF tests. Journal of Psychopathology and Behavioral Assessment. 2011;33(2):137–158. doi: 10.1007/s10862-011-9217-x. [DOI] [Google Scholar]
- Barkley RA, Murphy KR, Fischer M. ADHD in adults: What the science says. New York: The Guilford Press; 2008. [Google Scholar]
- Biederman J, Petty CR, Fried R, Black S, Faneuil A, Doyle AE, Faraone SV. Discordance between psychometric testing and questionnaire-based definitions of executive function deficits in individuals with ADHD. J Atten Disord. 2008;12(1):92–102. doi: 10.1177/1087054707305111. [DOI] [PubMed] [Google Scholar]
- Bishop SR, Lau M, Shapiro S, Carlson L, Anderson ND, Carmody J, Devins G. Mindfulness: A proposed operational definition. Clinical Psychology: Science and Practice. 2004;11(3):230–241. doi: 10.1093/clipsy.bph077. [DOI] [Google Scholar]
- Boonstra AM, Oosterlaan J, Sergeant JA, Buitelaar JK. Executive functioning in adult ADHD: A meta-analytic review. Psychological Medicine. 2005;35(8):1097–1108. doi: 10.1017/S003329170500499X. [DOI] [PubMed] [Google Scholar]
- Bramham J, Young S, Bickerdike A, Spain D, McCartan D, Xenitidis K. Evaluation of group cognitive behavioral therapy for adults with ADHD. J Atten Disord. 2009;12(5):434–441. doi: 10.1177/1087054708314596. [DOI] [PubMed] [Google Scholar]
- Britton WB, Shahar B, Szepsenwol O, Jacobs WJ. Mindfulness-based cognitive therapy improves emotional reactivity to social stress: Results from a randomized controlled trial. Behavior Therapy. 2012;43(2):365–380. doi: 10.1016/j.beth.2011.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown TE. ADD/ADHD and impaired executive function in clinical practice. Current Psychiatry Reports. 2008;10(5):407–411. doi: 10.1007/s12618-009-0006-3. [DOI] [PubMed] [Google Scholar]
- Chiesa A, Serretti A. Mindfulness based cognitive therapy for psychiatric disorders: A systematic review and meta-analysis. Psychiatry Research. 2011;187(3):441–453. doi: 10.1016/j.psychres.2010.08.011. [DOI] [PubMed] [Google Scholar]
- Conners CK, Erhardt D, Sparrow E. Conners’ Adult ADHD Rating Scales (CAARS) technical manual. North Tonawanda, NY: Multi-Health Systems, Inc; 1999. [Google Scholar]
- Conners CK. The Conners Continuous Performance Test. Toronto: Multi-Health Systems; 1995. [Google Scholar]
- Csikszentmihalyi M, Larson R. Validity and reliability of the experience-sampling method. The Journal of Nervous and Mental Disease. 1987;175(9):526–536. doi: 10.1097/00005053-198709000-00004. [DOI] [PubMed] [Google Scholar]
- deVries M. The experience of psychopathology: Investigating mental disorders in their natural settings. Cambridge: Cambridge University Press; 1992. [Google Scholar]
- Epstein JN, Johnson D, Conners CK. Conners’ Adult ADHD Diagnostic Interview for DSM-IV. North Tonawanda, NY: Multi-Health Systems, Inc; 2000. [Google Scholar]
- Fan J, Posner M. Human attentional networks. Psychiatrische Praxis. 2004;31(Suppl 2):S210–214. doi: 10.1055/s-2004-828484. [DOI] [PubMed] [Google Scholar]
- Faraone SV, Glatt SJ. A comparison of the efficacy of medications for adult attention-deficit/hyperactivity disorder using meta-analysis of effect sizes. The Journal of Clinical Psychiatry. 2010;71(6):754–763. doi: 10.4088/JCP.08m04902pur. [DOI] [PubMed] [Google Scholar]
- Fayyad J, De Graaf R, Kessler R, Alonso J, Angermeyer M, Demyttenaere K, Jin R. Cross-national prevalence and correlates of adult attention-deficit hyperactivity disorder. British Journal of Psychiatry. 2007;190:402–409. doi: 10.1192/bjp.bp.106.034389. [DOI] [PubMed] [Google Scholar]
- Fedele DA, Hartung CM, Canu WH, Wilkowski BM. Potential symptoms of ADHD for emerging adults. Journal of Psychopathology and Behavioral Assessment. 2010;32(3):385–396. doi: 10.1007/s10862-009-9173-x. [DOI] [Google Scholar]
- First MB, Spitzer RL, Williams JBW, Gibbon M. Structured Clinical Interview for DSM-IV-TR (SCID-I) - research version. New York: Biometrics Research; 2002. [Google Scholar]
- Fjorback LO, Arendt M, Ornbol E, Fink P, Walach H. Mindfulness-based stress reduction and mindfulness-based cognitive therapy: A systematic review of randomized controlled trials. Acta Psychiatrica Scandinavica. 2011;124(2):102–119. doi: 10.1111/j.1600-0447.2011.01704.x. [DOI] [PubMed] [Google Scholar]
- Flook L, Smalley SL, Kitil MJ, Galla BM, Kaiser-Greenland S, Locke J, Kasari C. Effects of mindful awareness practices on executive functions in elementary school children. Journal of Applied School Psychology. 2010;26(1):70–95. doi: 10.1080/15377900903379125. [DOI] [Google Scholar]
- Giancola PR, Godlaski AJ, Roth RM. Identifying component-processes of executive functioning that serve as risk factors for the alcohol-aggression relation. Psychology of Addictive Behaviors. 2012;26(2):201–211. doi: 10.1037/a0025207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gratz KL, Roemer L. Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the Difficulties in Emotion Regulation Scale. Journal of Psychopathology and Behavioral Assessment. 2004;26:41–54. doi: 10.1023/B:JOBA.0000007455.08539.94. [DOI] [Google Scholar]
- Grizenko N, Paci M, Joober R. Is the inattentive subtype of ADHD different from the combined/hyperactive subtype? J Atten Disord. 2010;13(6):649–657. doi: 10.1177/1087054709347200. [DOI] [PubMed] [Google Scholar]
- Hesslinger B, Tebartz van Elst L, Nyberg E, Dykierek P, Richter H, Berner M, Ebert D. Psychotherapy of attention deficit hyperactivity disorder in adults: A pilot study using a structured skills training program. European Archives of Psychiatry and Clinical Neuroscience. 2002;252(4):177–184. doi: 10.1007/s00406-002-0379-0. [DOI] [PubMed] [Google Scholar]
- Hirvikoski T, Waaler E, Alfredsson J, Pihlgren C, Holmstrom A, Johnson A, Nordstrom AL. Reduced ADHD symptoms in adults with ADHD after structured skills training group: Results from a randomized controlled trial. Behaviour Research and Therapy. 2011;49(3):175–185. doi: 10.1016/j.brat.2011.01.001. [DOI] [PubMed] [Google Scholar]
- Hölzel BK, Lazar SW, Gard T, Schuman-Olivier Z, Vago DR, Ott U. How does mindfulness meditation work? Proposing mechanisms of action from a conceptual and neural perspective. Perspectives on Psychological Science. 2011;6(6):537–559. doi: 10.1177/1745691611419671. [DOI] [PubMed] [Google Scholar]
- Kabat-Zinn J. Full catastrophe living: Using the wisdom of your body and mind to face stress, pain, and illness. New York: Deltacorte Press; 1990. [Google Scholar]
- Kaufman A, Kaufman N. Kaufman Brief Intelligence Test. 2. Circle Pines, MN: AGP publishing; 2004. [Google Scholar]
- Keng SL, Smoski MJ, Robins CJ. Effects of mindfulness on psychological health: A review of empirical studies. Clinical Psychology Review. 2011;31(6):1041–1056. doi: 10.1016/j.cpr.2011.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Adler L, Barkley R, Biederman J, Conners CK, Demler O, Zaslavsky AM. The prevalence and correlates of adult ADHD in the United States: Results from the National Comorbidity Survey Replication. American Journal of Psychiatry. 2006;163(4):716–723. doi: 10.1176/appi.ajp.163.4.716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Green JG, Adler LA, Barkley RA, Chatterji S, Faraone SV, Van Brunt DL. Structure and diagnosis of adult attention-deficit/hyperactivity disorder: Analysis of expanded symptom criteria from the Adult ADHD Clinical Diagnostic Scale. Archives of General Psychiatry. 2010;67(11):1168–1178. doi: 10.1001/archgenpsychiatry.2010.146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knouse LE, Safren SA. Current status of cognitive behavioral therapy for adult attention-deficit hyperactivity disorder. Psychiatric Clinics of North America. 2010;33(3):497–509. doi: 10.1016/j.psc.2010.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leyro TM, Zvolensky MJ, Bernstein A. Distress tolerance and psychopathological symptoms and disorders: A review of the empirical literature among adults. Psychological Bulletin. 2010;136(4):576–600. doi: 10.1037/a0019712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martel MM. Research review: A new perspective on attention-deficit/hyperactivity disorder: Emotion dysregulation and trait models. Journal of Child Psychology and Psychiatry. 2009;50(9):1042–1051. doi: 10.1111/j.1469-7610.2009.02105.x. [DOI] [PubMed] [Google Scholar]
- Mitchell JT, Zylowska L, Kollins SH. Mindfulness meditation training for attention-deficit/hyperactivity disorder in adulthood: Current empirical support, treatment overview, and future directions. doi: 10.1016/j.cbpra.2014.10.002. submitted. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mongia M, Hechtman L. Cognitive behavior therapy for adults with attention-deficit/hyperactivity disorder: A review of recent randomized controlled trials. Current Psychiatry Reports. 2012;14(5):561–567. doi: 10.1007/s11920-012-0303-x. [DOI] [PubMed] [Google Scholar]
- Narum SR. Beyond Bonferroni: Less conservative analyses for conservative genetics. Conservation Genetics. 2006;7(5):783–787. doi: 10.1007/s10592-005-9056-y. [DOI] [Google Scholar]
- Philipsen A, Richter H, Peters J, Alm B, Sobanski E, Colla M, Hesslinger B. Structured group psychotherapy in adults with attention deficit hyperactivity disorder: Results of an open multicentre study. Journal of Nervous and Mental Disease. 2007;195(12):1013–1019. doi: 10.1097/NMD.0b013e31815c088b. [DOI] [PubMed] [Google Scholar]
- Prince J, Wilens T, Spencer T, Biederman J. Pharmacotherapy of ADHD in adults. In: Barkley RA, editor. Attention-Deficit/Hyperactivity Disorder: A Handbook for Diagnosis and Treatment. 3. New York, NY: Guilford; 2006. pp. 704–736. [Google Scholar]
- Ramsay JR. CBT for adult ADHD: Adaptations and hypothesized mechanisms of change. Journal of Cognitive Psychotherapy: An International Quarterly. 2010;24(1):37–45. doi: 10.1891/0889-8391.24.1.37. [DOI] [Google Scholar]
- Reimherr FW, Marchant BK, Olsen JL, Halls C, Kondo DG, Williams ED, Robinson RJ. Emotional dysregulation as a core feature of adult ADHD: Its relationship with clinical variables and treatment response in two methylphenidate trials. Journal of ADHD & Related Disorders. 2010;1(4):53–64. [Google Scholar]
- Reimherr FW, Marchant BK, Strong RE, Hedges DW, Adler L, Spencer TJ, Soni P. Emotional dysregulation in adult ADHD and response to atomoxetine. Biol Psychiatry. 2005;58:125–131. doi: 10.1016/j.biopsych.2005.04.040. [DOI] [PubMed] [Google Scholar]
- Reis HT, Gable SL. Event-sampling and other methods for studying everyday experience. In: Reis HT, Judd CM, editors. Handbook of research methods in social and personality psychology. Cambridge: Cambridge University Press; 2000. pp. 190–221. [Google Scholar]
- Reitan RM. Manual for administration of neuropsychological test battery for adults and children. Tucson, AZ: Neuropsychology Laboratory; 1979. [Google Scholar]
- Roth RM, Isquith PK, Gioia GA. Behavior Rating Inventory of Executive Function–Adult Version (BRIEF-A) Lutz, FL: Psychological Assessment Resources; 2005. [Google Scholar]
- Safren SA, Perlman CA, Sprich S, Otto MW. Mastering your adult ADHD: A cognitive-behavioral treatment program therapist guide. New York, NY: Oxford University Press; 2005. [Google Scholar]
- Safren SA, Sprich S, Mimiaga MJ, Surman C, Knouse L, Groves M, Otto MW. Cognitive behavioral therapy vs relaxation with educational support for medication-treated adults with ADHD and persistent symptoms: A randomized controlled trial. Journal of the American Medical Association. 2010;304(8):875–880. doi: 10.1001/jama.2010.1192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SAS Institute Inc. SAS/STAT 9.2 User’s Guide. Cary, NC: SAS Institute Inc; 2008. [Google Scholar]
- Sedlmeier P, Eberth J, Schwarz M, Zimmermann D, Haarig F, Jaeger S, Kunze S. The psychological effects of meditation: A meta-analysis. Psychological Bulletin. 2012;138(6):1139–1171. doi: 10.1037/a0028168. [DOI] [PubMed] [Google Scholar]
- Shapiro SL, Carlson LE, Astin JA, Freedman B. Mechanisms of mindfulness. J Clin Psychol. 2006;62(3):373–386. doi: 10.1002/jclp.20237. [DOI] [PubMed] [Google Scholar]
- Shiffman S, Stone AA, Hufford MR. Ecological momentary assessment. Annual Review of Clinical Psychology. 2008;4:1–32. doi: 10.1146/annurev.clinpsy.3.022806.091415. [DOI] [PubMed] [Google Scholar]
- Simons JS, Gaher RM. The Distress Tolerance Scale: Development and validation of a self-report measure. Motivation and Emotion. 2005;29(2):83–102. doi: 10.1007/s11031-005-7955-3. [DOI] [Google Scholar]
- Solanto MV. Cognitive-behavioral therapy for adult ADHD: Targeting executive dysfunction. New York, NY: Guilford Press; 2011. [Google Scholar]
- Solanto MV, Marks DJ, Wasserstein J, Mitchell K, Abikoff H, Alvir JM, Kofman MD. Efficacy of meta-cognitive therapy for adult ADHD. American Journal of Psychiatry. 2010;167(8):958–968. doi: 10.1176/appi.ajp.2009.09081123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steele M, Jensen PS, Quinn DM. Remission versus response as the goal of therapy in ADHD: A new standard for the field? Clinical Therapeutics. 2006;28(11):1892–1908. doi: 10.1016/j.clinthera.2006.11.006. [DOI] [PubMed] [Google Scholar]
- Wechsler D. Wechsler Adult Intelligence Scale—Fourth Edition (WAIS–IV) San Antonio, TX: The Psychological Corporation; 2008. [Google Scholar]
- Wender PH. Attention-deficit hyperactivity disorder in adults. The Psychiatric Clinics of North America. 1998;21(4):761–774. v. doi: 10.1016/S0193-953X(05)70039-3. [DOI] [PubMed] [Google Scholar]
- Wilens TE, Spencer TJ, Biederman J. A review of the pharmacotherapy of adults with attention-deficit/hyperactivity disorder. J Atten Disord. 2002;5(4):189–202. doi: 10.1177/108705470100500401. [DOI] [PubMed] [Google Scholar]
- World Health Organization. Clinical descriptions and diagnostic guidelines. Geneva: World Health Organization; 1992. The ICD-10 Classification of Mental and Behavioural Disorders. [Google Scholar]
- Zeger SL, Liang KY, Albert PS. Models for longitudinal data: A generalized estimating equation approach. Biometrics. 1988;44(4):1049–1060. [PubMed] [Google Scholar]
- Zeidan F, Johnson SK, Diamond BJ, David Z, Goolkasian P. Mindfulness meditation improves cognition: Evidence of brief mental training. Consciousness and Cognition. 2010;19(2):597–605. doi: 10.1016/j.concog.2010.03.014. [DOI] [PubMed] [Google Scholar]
- Zylowska L. The mindfulness prescription for adult ADHD: An 8-step program for strengthening attention, managing emotions, and achieving your goals. Boston: Shambhala; 2012. [Google Scholar]
- Zylowska L, Ackerman DL, Yang MH, Futrell JL, Horton NL, Hale TS, Smalley SL. Mindfulness meditation training in adults and adolescents with ADHD: A feasibility study. J Atten Disord. 2008;11(6):737–746. doi: 10.1177/1087054707308502. [DOI] [PubMed] [Google Scholar]
- Zylowska L, Smalley SL, Schwartz JM. Mindful awarenes and ADHD. In: Didonna F, editor. Clinical handbook of mindfulness. New York: Springer; 2009. pp. 319–338. [Google Scholar]