Abstract
This study examined the intensity of activity contributing to physical activity energy expenditure in older adults. In 57 men and women aged ≥65, total energy expenditure (TEE) was measured using doubly labeled water, and resting metabolic rate was measured using indirect calorimetry to calculate a physical activity index (PAI). Sedentary time, and physical activity of light and moderate/vigorous (mod/vig) intensity was measured using an accelerometer. The subjects were 75 ± 7 yrs (mean ± SD) of age and 79% female. Subjects spent 66 ± 8, 25 ± 5, and 9 ± 4% of monitor wear time in sedentary, light, and mod/vig activity per day, respectively. In a mixture regression model, both light (β=29.6 (15.6 – 43.6, 95%CI)), p<0.001) and mod/vig intensity activity (β=28.7 (7.4 – 50.0, 95%CI)), p=0.01) were strongly associated with PAI, suggesting that both light and mod/vig intensity activities are major determinants of their physical activity energy expenditure.
INTRODUCTION
There are both direct and indirect ways to measure physical activity (PA) behaviors (LaMonte & Ainsworth, 2001); one indirect method is to measure PA energy expenditure (PAEE). This can be accurately derived through the measurement of the components of daily energy expenditure including the use of doubly labeled water (DLW) measures of total energy expenditure, indirect calorimetric measurement of resting metabolic rate (RMR), and an estimation of the thermic effect of food (Schutz, Weinsier, & Hunter, 2001). One drawback to this method, however, is that the type, frequency, intensity, and duration of the activities that contribute to the total PAEE are unknown. Given that higher PAEE has been linked to reduced mobility limitations and mortality rates in older adults, as well as a reduced risk of many chronic diseases,(Manini et al., 2006; Manini et al., 2009; U.S. Department of Health and Human Services, 2008) it is important to gain a better understanding of the characteristics of the physical activities that contribute to higher PAEE.
Regarding PA intensity, current PA recommendations for adults focus primarily on activities of moderate or greater intensity, and suggest that more research is needed to better understand the potential for common daily activities to contribute to health (U.S. Department of Health and Human Services, 2008). It has previously been shown that moderate intensity activity contributes more to increasing daily PAEE in younger adults than does high or low intensity activity (Westerterp, 2001). The intensity of activity that contributes to higher levels of PAEE in older adults is not clear. Previous studies that have addressed this have combined sedentary and light intensity activities (<3 MET) into one category (Meijer, Goris, Wouters, & Westererp, 2001; Johannsen et al., 2008) which does not allow for an evaluation of independent contributions of these very different behaviors. Studies describing PA in older adults have suggested that considerable time is spent in sedentary and light behaviors (Harris, Lanningham-Foster, McCrady, & Levine, 2007; Matthews et al., 2008; Copeland & Esliger, 2009; Buman et al., 2010), and these should be examined separately given the negative impact of sedentary behavior on overall PAEE and health (Owen, Sparling, Healy, Dunstan, & Matthews, 2010) and the potential benefit of light activity in older adults (Buman et al., 2010). Clearly if the time spent is equivalent, mod/vig intensity activity would result in greater energy expenditure than light; however, it may be easier for older adults to shift some of their sedentary time to light rather than higher intensity activities(Hooker et al., 2005). If this shift to light intensity activities were as important as promoting moderate or greater intensity activity for PAEE, and would have similar health benefits, this could have meaningful impact on PA recommendations for older adults which currently focus on activities of moderate or greater intensity as for adults in general. The primary purpose of this study is to determine the relationship between daily time spent in activities of various intensity and PAEE in older adults. We hypothesized that light intensity activity would be as important as moderate or greater intensity activity for the PAEE of older adults.
METHODS
Subjects and Experimental Design
Men and women were recruited for a study examining the comparative validity of different PA measures in older adults (Colbert et al., 2011) For the purposes of that study, three different activity monitors, including an accelerometer, and three different surveys were administered at the timepoints described here. To address the current question, data from the accelerometer (which provides valid information on activity intensity) and one of the surveys (which provides a comprehensive list of activities) was used, and only the relevant methodology is described here. Community-dwelling older adults were recruited from the Madison, WI area through flyers posted at various community sites and through word of mouth. Interested subjects were screened for the inclusion criteria of ≥65 yrs and able to walk unassisted, and were excluded if they reported any of the following: an implanted defibrillator or pacemaker; diabetes; an unstable thyroid condition; or the use of beta-blockers, weight loss supplements, or oral steroids. Eligible and interested participants were scheduled for a study run-in period that was ~4 days long. Subjects signed an informed consent form, were fitted with the accelerometer, told to wear it during waking hours (except for during water-based activities including showering and swimming), and given a log sheet on which to record the times they wore the accelerometer. At the close of the run-in period, logs and accelerometer data were examined for compliance with the instructions, and subjects who complied and were willing to wear the accelerometer for 10 days were scheduled for two study visits. At study visit one, the DLW protocol was started after a minimum eight hour fast, and participants were fitted with the accelerometer, and given a log. At study visit two, ten days later, subjects provided final urine samples, returned the accelerometer and log, completed the CHAMPS PA questionnaire(Stewart et al., 2001) and a basic demographic and health history questionnaire, and had their RMR measured. Subjects came to study visit two having fasted for at least eight hours, and having refrained from vigorous exercise and alcohol consumption for at least 24 hours. The study protocol was approved by the University of Wisconsin Health Sciences Institutional Review Board, and all subjects provided written informed consent.
Physical Activity Energy Expenditure
Total energy expenditure (TEE) was determined using the DLW method (Schoeller & van Santen, 1982). Subjects provided a baseline urine sample and were given an oral dose containing an estimated 0.18 g/kg total body water (TBW) of 18O labeled water and 0.16 g/kg TBW of 2H labeled water. Urine samples were collected at 2, 3, and 4 hours post-dosing. Subjects were allowed a maximum of 500 ml of liquid at the 1-hr post-dose-time point. At the second study visit, subjects provided two urine samples, one hour apart. Urine samples were stored at −20°C until the stable isotope abundances of the physiologic samples were measured by isotope ratio mass spectrometry. Isotope dilution spaces were calculated by the plateau method according to Cole & Coward (Cole & Coward, 1992). Carbon dioxide production was calculated using equation A6 of Schoeller et al. (Schoeller et al., 1986) and energy expenditure using the modified Weir equation. RMR was measured via indirect calorimetry using either a Deltatrac I or II respiratory gas analyzer (VIASYS Healthcare Inc., SensorMedics, Yorba Linda, CA). Subjects quietly rested in a supine position for at least 10 minutes prior to the 30 minute respiratory gas collection period. The final 20 minutes of recordings were used to calculate RMR using the modified Weir equation (Weir, 1949). Periodic methanol burns were used to calculate correction factors which were applied to the data. A standard calculation was used to derive PA energy expenditure (PAEE) with the assumption of 10% of TEE as the thermic effect of food (i.e. PAEE=(TEE × 0.9)−RMR). We then created a PA index (PAI) (i.e. PAI=PAEE/body wgt (kg)), so that the increase in caloric expenditure for the same activity with greater body weight did not confound our intensity and energy expenditure associations. A rationale is well described elsewhere, but briefly, the energy costs of light intensity activities have largely been found to be proportional to body weight (Schoeller & Jefford, 2002). However, given the lack of agreement on the most appropriate way to adjust for the contribution of body weight to energy expenditure (Schutz et al., 2001; Schoeller & Jefford, 2002; Mâsse et al., 2004), we additionally examined PA level (PAL; i.e., TEE/RMR) as an alternative dependent variable.
Physical Activity Assessment
A GT1M uniaxial accelerometer (Actigraph, Pensacola, FL), was used to quantify the intensity of PA. The accelerometer was worn on an elastic belt around the waist, over the right hip. Data was collected in 10-second epochs, but integrated into one minute epochs for the analysis. An established algorithm was used to estimate nonwear periods using 60 min of 0 count/min and 50-counts per minute thresholds (Troiano et al., 2008). Days with less than 10 hours of wear time were excluded from the calculation of average daily time spent at a given intensity. Count/minute cutpoints used to define sedentary, light, moderate, and vigorous activity in the primary analysis were ≤100, 101–760, 761–5724, and ≥ 5725 (Matthews, 2005; Freedson, Melanson, & Sirard, 1998). Unfortunately, there are no currently agreed upon intensity cutpoints for older adults (Strath, Pfeiffer, & Whitt-Glover, 2012). The 760 moderate intensity cutpoint was derived through an examination of 28 different light and moderate intensity activities that included non-ambulatory activities not typically included in original regression-derived cutpoints (Matthews, 2005), while the 5725 vigorous cutpoint is from Freedson et al. (Freedson et al., 1998). To assure ourselves that the results were not dependent on the cutpoint chosen for moderate intensity, we also used 574 (Swartz et al., 2000) and 1041 (Copeland & Esliger, 2009) in separate analyses. The CHAMPS questionnaire was used in this analysis to identify the types of activities that are reported by the subjects. The questionnaire was self-administed and then checked by study personnel for completeness. Individual activities on the CHAMPS are categorized in this analysis into light, moderate, or vigorous intensity based on the MET values (<3, 3–5.9, 6.0+, respectively) assigned in the scoring scheme (Stewart et al., 2001).
Statistical Analysis
The primary objective of this analysis was to evaluate the contribution of the amount of time spent in different intensities of PA to PAI in older adults. The sample size was estimated to provide appropriate power for the main study (Colbert et al., 2011). We examined the normality assumption prior to analysis for the intensity and energy expenditure data and found the data to be sufficiently normal to support analysis without transformation. We calculated the percent of time spent at a given intensity using the average minutes spent at each intensity and the average wear time from the accelerometer. As only six subjects recorded any vigorous activity (from a total of 1 to 7 minutes/day) the moderate and vigorous levels were combined. Given our samples size, the low level of vigorous compared to moderate minutes of activity, and that recommendations for PA include both moderate and vigorous activity or some combination, we felt there was little chance of bias by collapsing these intensities. Crude associations between PAI and intensity of activity were assessed using Pearson correlations. The percent of time spent at one intensity level is necessarily related to and constrained by the time spent at other levels. The percent of time spent at the various intensity levels is 100% for each subject (known as compositional data), and as such, standard regression models with these as independent variables do not work. Therefore, we have analyzed PAI/PAL using mixture regression models with percent of time spent at three intensity levels as independent variables (Cornell, 2002). In our models we are examining the contributions of time spent at a given intensity on the subjects’ PAI (as Y), as indicated below:
where Xs, Xl and Xm represent the percent time spent at intensity level, sedentary, light and moderate/vigorous, respectively, with the regression coefficients, βs, βl and βm and the error term ε.
The regression coefficients in these models are interpreted as the value of PAI if one were to spend 100% of their monitor wear time at that intensity of activity. We have also explored the role of age, gender, and separately, in models of PAEE, the role of body weight. Additionally, we re-ran the mixture analysis using the 574 and 1041 cutpoints to define moderate intensity activity. Finally, we repeated the mixture analysis with PAL as the dependent variable.
RESULTS
A total of 70 men and women initially consented. Ten subjects dropped out of the study for the following reasons: lost interest/didn’t have time, n=4; couldn’t provide necessary urine samples, n=2; developed health conditions between run-in and study period, n=2; found to be ineligible, n=1; reason unknown, n=1; for a total sample size of 60. Of these 60, three were not included in this analysis as two DLW doses didn’t equilibrate, and there was one non-physiologic value for the energy expenditure measure, leaving 57 for analysis. Monitor compliance was very good, as reported in the main study (Colbert et al., 2011), with 13+ hrs wear/day and 6+days/week on average. Subjects were predominantly female and White, with an average age of 75 ± 7, with other characteristics found in Table 1. The average total daily energy expenditure was 2139 ± 434, and the PAEE was 724 ± 253. The majority of monitor wear-time was spent sedentary (Table 1), with the average amount of sedentary, light, and moderate-vigorous activity recorded at 548 ± 73, 209 ± 45, and 71 ± 36 min/day, respectively. The correlations between PAI and sedentary behavior, light intensity, and moderate-vigorous intensity activity were −0.60, 0.53, and 0.49, respectively (all p<0.001). In the mixture regression analysis, neither age (p=0.41) nor sex (p=0.80) made any meaningful difference in predicting PAI, and as such, the models without adjustment for these factors are presented here. Similarly, although regression adjustment by sex and age produced slightly different results qualitatively, the confidence intervals overlapped substantially and so these results are not presented here.
Table 1.
Characteristics of Participants (n=57)
| Characteristic | Mean ± SD or % |
|---|---|
| Female | 79% |
| White | 98% |
| Age (yrs) | 75 ± 7 |
| Body mass (kg) | 69.0 ± 14.5 |
| Body mass index (kg/m2) | 25.7 ± 4.2 |
| Current smoker | 4% |
| Education | |
| ≤ High School | 21% |
| College | 43% |
| ≥Graduate work | 36% |
| Current Diseasea | |
| Arthritis | 49% |
| Back Pain | 11% |
| Hip/Knee Pain | 25% |
| Osteoporosis | 23% |
| Lung Disease | 8% |
| Cancer | 15% |
| Hypertension | 34% |
| Physical Activity Energy | 724 ± 253 |
| Expenditure (kcal/d) | |
| Monitor Wear time (min) | 828 ± 73 |
| % Monitor Wear time by Intensityb | |
| Sedentary | 66 ± 8 |
| Light Intensity | 25 ± 5 |
| Moderate/Vigorous Intensity | 9 ± 4 |
Data is missing for smoking, education, and current diseases in 4 subject, with the exception of hip/knee pain, which has 5 missing data points.
Using the 760 cpm cutpoint to define moderate intensity activity.
Figure 1 and Table 2 present the results of the mixture regression analysis. Figure 1 shows the range of PAIs measured in relation to the percent of time the study subjects spent at a given activity level. Each dot represents a given subject. The vertices represent where a subject would fall if they spent 100% of their monitor time at that intensity activity (i.e. sedentary, light activity, mod/vig activity (760 cutpoint)). As can be seen from the distribution, the subjects in our study fall more towards the sedentary end of the spectrum, with a tendency towards more light than moderate/vigorous intensity activity. PAI is higher as subjects move away from sedentary behavior. The flat slope of the isolines predicted by the mixture regression analysis shows that PAI increases as one moves away from sedentary behavior towards either light or moderate/vigorous intensity activity. Table 2 presents the results of the mixture regression analysis of the relationship between intensity of activity and PAI by cutpoint of moderate activity used. The regression coefficients for light activity and moderate/vigorous activity are both significantly different from 0 with both light and mod/vig intensity activities contributing similarly to an increase in PAI, regardless of the cutpoint chosen, confirming the impression from Figure 1. There were no appreciable differences in the results when PAL was used as the dependent variable.
Figure 1.
Triangle plot of the mixture regression model. Each subject is represented by a single dot, with the Physical Activity Index (PAI) indicated by degree of shading. The vertices represent spending 100% of time at a given intensity level (i.e. sedentary, light intensity, moderate-vigorous intensity (760 cpm cutpoint)). The isolines represent the PAI predicted by the mixture regression analysis summarized in Table 2.
Table 2.
Results from the Mixture Regression Analysis of PAI with the Percent of Time Spent with PA Intensity as Independent Variables, Using Different Moderate Cutpoints
| Cutpoint | Parameter | Coefficient | 95% C.I. | p-value |
|---|---|---|---|---|
| 574 | Sedentary | 0.93 | −3.27, 5.13 | 0.66 |
| Light activity | 30.70 | 14.01, 47.39 | <0.001 | |
| Mod/Vig activity | 27.88 | 11.42, 44.34 | 0.001 | |
|
| ||||
| 760 | Sedentary | 1.09 | −2.98, 5.16 | 0.59 |
| Light activity | 29.62 | 15.64, 43.60 | <0.001 | |
| Mod/Vig activity | 28.71 | 7.44, 50.00 | 0.01 | |
|
| ||||
| 1041 | Sedentary | 1.23 | −2.67, 5.14 | 0.53 |
| Light activity | 28.80 | 17.34, 40.26 | <0.001 | |
| Mod/Vig activity | 30.73 | 2.61, 58.84 | 0.03 | |
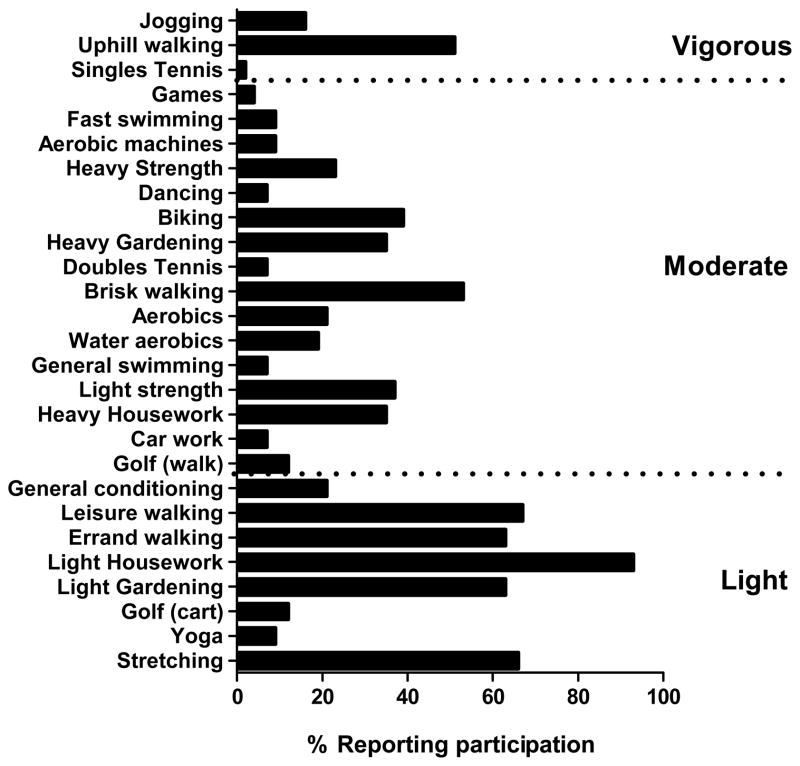
The CHAMPS questionnaire provided information on the types of activities engaged in by the study subjects and the self-reported time spent in each activity, and the prevalence of any participation in individual activities is depicted in Figure 2. The activities most commonly reported by the subjects were from the light intensity category, including light housework, stretching, light gardening, and walking for leisure or errands. Brisk walking and uphill walking were commonly reported from the moderate and vigorous categories. Among those who reported participation in a given activity, the median values for weekly participation in the most commonly reported individual activities were 1.75 hrs/wk in light housework, light walking for leisure, brisk walking, and light gardening, and 0.5 hr/wk each in walking for errands, uphill walking, and stretching.
Figure 2.
Individual activity items from the CHAMPS questionnaire are found on the y-axis. The bars represent the % of the subjects who reported any participation in a given activity.
DISCUSSION
The older adults in the current study spent a substantial portion of their day sedentary, while active time was predominantly spent in light intensity activity. Smaller amounts of moderate activity were recorded, and only a few persons participated in vigorous activity. In terms of energy expenditure, both light and moderate-vigorous activity contributed approximately equally towards PA energy expenditure in this sample. Based on self-reports, the majority of activities were of light intensity and came from non-exercise realms such as light house-keeping, light gardening, stretching, and walking for either leisure or errands.
The amount of sedentary behavior reported by our study participants is in line with estimates of similarly aged U.S. adults from other studies using accelerometry (Matthews et al., 2008; Buman et al., 2010). In the 2003–2004 NHANES study, adults aged 60–69 and 70–85 were sedentary for 8.4 and 9.3 hrs/day, respectively (Matthews et al., 2008), while our subjects were sedentary for 9.1 hrs/day. Similarly, in a study of 862 older adults from the Seattle, WA and Baltimore, MD areas, 9.4 hrs/day of sedentary behavior was recorded (Buman et al., 2010). Although monitor wear time can significantly affect estimates of sedentary behavior, monitors were worn ~14 hrs/day in all of these studies. The lack of vigorous intensity activity is also consistent with prior studies. In the 2003–2004 NHANES sample, adults aged 60 and older had less than 1 minute/day of vigorous activity (Troiano et al., 2008), and in a study of 58 subjects aged 60–74 from the Louisiana Healthy Aging Study (LHAS), there was no recorded vigorous activity (Johannsen et al., 2008). Estimates of moderate activity are more susceptible to variability due to differences in the cut points selected. Our estimate of 71 min/day using 760 cpm yielded higher estimates of moderate activity in this age group than was seen in NHANES with a cut point of 2020 (~10 minutes/day), in Buman et al. using the Freedson 1951 cut point (12 minutes/day), or in a European study (Davis & Fox, 2007) with a cut point of 1,999 (20 min/day), but lower than the 126 min/day seen in the LHAS where a cut point of 574 cpm was used. Few studies have focused on defining the appropriate cut points to define PA intensity in older adults, and a recent review confirms that there are no universally accepted cutpoints for older adults (Strath et al., 2012). Importantly, our primary conclusions regarding the contribution of activity intensity to physical activity energy expenditure were unchanged when we used either the 574 or 1041 cutpoints that have been previously used in older adults (Swartz et al., 2000; Copeland & Esliger, 2009).
We observed that light intensity activity was as important for PAEE as was activity of moderate or greater intensity. Though a prior study suggested that moderate intensity PA was most important to PAEE in younger adults, that study used a combined category of sedentary and light intensity activity (Westerterp, 2001). Similarly, a previous study in elderly adults grouped sedentary and light activity, and concluded that time spent in light intensity activity negatively impacted PAEE (Meijer et al., 2001). This grouping of sedentary and light activities likely led to erroneous conclusions regarding the potential benefit of light intensity activity in older adults. This is particularly meaningful given recent findings by Buman et al. (Buman et al., 2010) showing significant associations of objectively measured light intensity PA with both physical and psychosocial well-being in older adults. Also, some exercise intervention studies in older adults using moderate or greater intensity exercise have found no change in total TEE or activity, suggesting that older adults may compensate for the increased exercise behavior by reducing their non-exercise PA, though the results have not been consistent (Meijer, Westerterp, & Verstappen, 1999; Baker et al., 2007; Opdenacker, Boen, Coorevits, & Delecluse, 2008). Perhaps a suggestion to spend less time sedentary, in favor of light intensity activities, will have an important impact on overall PAEE, in addition to the positive effect of activities of moderate or greater intensity. Given that subjects in the current study voluntarily participated in mostly activities of light intensity, this type of recommendation may be more palatable than the standard recommendation focused on moderate intensity activities(Hooker et al., 2005).
We found no significant interactions by either age or sex with the relationships explored in our data. The lack of interaction by sex may mean that there really is no difference between men and women in how intensity of activity is associated with PAI, or it is also possible that our sample size was not adequate to detect real differences. Qualitatively, we saw a tendency for moderate intensity activity to be more important for PAEE in males, but the confidence intervals surrounding these estimates were wide. This should be examined in studies with larger samples of men. We also tried to eliminate the effects of body weight on the intensity and PAEE relationship by creating the PAI index, which factored out body weight (Schoeller & Jefford, 2002). When we have compared this type of energy expenditure expression with that of PAL or through the use of body weight as a covariate in other analyses, we have not found that the manner of accounting for body weight altered our results (Colbert et al., 2011). Similarly, when we used PAL as our dependent variable in the current analysis, our results were unchanged (data not shown). We feel that body weight is not influencing our results, but acknowledge it may be important in studies with a greater range of BMIs.
We acknowledge limitations to our study. Accelerometers cannot capture all types of activities, and therefore, while PAI included energy expenditure from all activities, our categorization of intensity did not, which may have biased our associations somewhat. Our study is also limited by the small number of male participants. Future studies should further explore effect modification of the PAEE and intensity relationship by sex. Most importantly, our analysis is cross sectional, and as such we can only speculate that if we intervened on either light or mod-vig intensity activity that we could increase PAEE. An important strength of our study is that we separated sedentary and light behaviors, with the idea that these may have very different and important influences on PAEE and potentially, health. Also, our use of the CHAMPS questionnaire allowed us to examine the types of activities engaged in by our subjects, which complements the findings obtained through accelerometry. Though the amount of activity may not be accurately self-reported (Colbert et al., 2011), an understanding of the types of activities that they engaged in is useful information provided by the CHAMPS questionnaire. Finally, our sample appears to be representative of similarly aged individuals in terms of total energy expenditure (TEE). The TEE of our group measured by DLW was 2140 ± 434 (mean ± SD) vs. 2280 ± 446 as estimated by IOM equations (Institute of Medicine of the National Academies: Food and Nutrition Board, 2005), a difference of only 6%.
Consistent with other studies, we found that older adults spend the majority of their day sedentary. Most of their active time was spent in light intensity activity, and this appeared to be as important as moderate to vigorous intensity activity in their daily PAEE. While it is clear from past research that participation in moderate intensity activity is important for older adults, future work is necessary to determine if the light intensity activity that contributes to their PAEE has beneficial effects on relevant health outcomes.
References
- Baker MK, Kennedy DJ, Bohle PL, Campbell DS, Knapman L, Grady J, et al. Efficacy and feasibility of a novel tri-modal robust exercise prescription in a retirement community: a randomized, controlled trial. Journal of the American Geriatrics Society. 2007;55:1–10. doi: 10.1111/j.1532-5415.2006.01031.x. [DOI] [PubMed] [Google Scholar]
- Buman MP, Hekler EB, Haskell WL, Pruitt L, Conway TL, Cain KL, et al. Objective light-intensity physical activity associations with rated health in older adults. Am J Epidemiol. 2010;172:1155–1165. doi: 10.1093/aje/kwq249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colbert LH, Matthews CE, Havighurst TC, Kim K, Schoeller DA. Comparative Validity of Physical Activity Measures in Older Adults. Med Sci Sports Exerc. 2011;43:867–876. doi: 10.1249/MSS.0b013e3181fc7162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cole T, Coward W. Precision and accuracy of doubly labeled water energy expenditure by multipoint and two-point methods. Am J Physiol. 1992;263:E965–E973. doi: 10.1152/ajpendo.1992.263.5.E965. [DOI] [PubMed] [Google Scholar]
- Copeland JL, Esliger DW. Accelerometer assessment of physical activity in active, healthy older adults. Journal of Aging and Physical Activity. 2009;17:17–30. doi: 10.1123/japa.17.1.17. [DOI] [PubMed] [Google Scholar]
- Cornell J. Experiments with Mixtures: Designs, Models, and the Analysis of Mixture Data. 3. New York: John Wiley & Sons, Inc; 2002. [Google Scholar]
- Davis MG, Fox KR. Physical activity patterns assessed by accelerometry in older people. Eur J Appl Physiol. 2007;100:581–589. doi: 10.1007/s00421-006-0320-8. [DOI] [PubMed] [Google Scholar]
- Freedson PS, Melanson E, Sirard J. Calibration of the Computer Science and Applications, Inc. accelerometer. Med Sci Sports Exerc. 1998;30:777–781. doi: 10.1097/00005768-199805000-00021. [DOI] [PubMed] [Google Scholar]
- Harris AM, Lanningham-Foster LM, McCrady SK, Levine JA. Nonexercise movement in elderly compared with young people. Am J Physiol Endocrinol Metab. 2007;292:E1207–E1212. doi: 10.1152/ajpendo.00509.2006. [DOI] [PubMed] [Google Scholar]
- Hooker S, Seavey W, Weidmer C, Harvey D, Stewart A, Gillis D, et al. The California Active Aging Community Grant Program: translating science into practice to promote physical activity in older adults. Ann Behav Med. 2005;29:155–165. doi: 10.1207/s15324796abm2903_1. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine of the National Academies: Food and Nutrition Board. Dietary reference intakes for energy, carbohydrate, fiber, fat, fatty acids, cholesterol, protein, and amino acids. Washington DC: The National Academies Press; 2005. [Google Scholar]
- Johannsen DL, DeLany JP, Frisard MI, Welsch MA, Rowley CK, Fang X, et al. Physical activity in aging: comparison among young, aged, and nonagenarian individuals. Journal of Applied Physiology. 2008;105:495–501. doi: 10.1152/japplphysiol.90450.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LaMonte M, Ainsworth B. Quantifying energy expenditure and physical activity in the context of dose response. Med Sci Sports Exerc. 2001;33:S370–S378. doi: 10.1097/00005768-200106001-00006. [DOI] [PubMed] [Google Scholar]
- Manini TM, Everhart JE, Patel KV, Schoeller DA, Cummings S, Mackey DC, et al. Activity energy expenditure and mobility limitation in older adults: differential associations by sex. Am J Epidemiol. 2009;169:1507–1516. doi: 10.1093/aje/kwp069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manini T, Everhart J, Patel K, Schoeller D, Colbert L, Visser M, et al. Daily activity energy expenditure and mortality among older adults. JAMA. 2006;296:171–179. doi: 10.1001/jama.296.2.171. [DOI] [PubMed] [Google Scholar]
- Mâsse L, Fulton J, Watson K, Mahar M, Meyers M, Wong W. Influence of body composition on physical activity validation studies using doubly labeled water. J Appl Physiol. 2004;96:1357–1364. doi: 10.1152/japplphysiol.00901.2003. [DOI] [PubMed] [Google Scholar]
- Matthews CE. Calibration of accelerometer output for adults. Med Sci Sports Exerc. 2005;37:S512–S522. doi: 10.1249/01.mss.0000185659.11982.3d. [DOI] [PubMed] [Google Scholar]
- Matthews CE, Chen KY, Freedson PS, Buchowski MS, Beech BM, Pate RR, et al. Amount of time spent in sedentary behaviors in the United States, 2003–2004. Am J Epidemiol. 2008;167:875–881. doi: 10.1093/aje/kwm390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meijer EP, Goris AHC, Wouters L, Westererp K. Physical inactivity as a determinant of the physical activity in the elderly. Int J Obes. 2001;25:935–939. doi: 10.1038/sj.ijo.0801644. [DOI] [PubMed] [Google Scholar]
- Meijer EP, Westerterp KR, Verstappen FT. Effect of exercise training on total daily physical activity in elderly humans. Eur J Appl Physiol Occup Physiol. 1999;80:16–21. doi: 10.1007/s004210050552. [DOI] [PubMed] [Google Scholar]
- Opdenacker J, Boen F, Coorevits N, Delecluse C. Effectiveness of a lifestyle intervention and a structured exercise intervention in older adults. Preventive medicine. 2008;46:518–524. doi: 10.1016/j.ypmed.2008.02.017. [DOI] [PubMed] [Google Scholar]
- Owen N, Sparling PB, Healy GN, Dunstan DW, Matthews CE. Sedentary behavior: emerging evidence for a new health risk. Mayo Clin Proc. 2010;85:1138–1141. doi: 10.4065/mcp.2010.0444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schoeller D, Jefford G. Determinants of the energy costs of light activities: inferences for interpreting doubly labeled water data. Int J Obes. 2002;26:97–101. doi: 10.1038/sj.ijo.0801851. [DOI] [PubMed] [Google Scholar]
- Schoeller D, Ravussin E, Schutz Y, Acheson K, Baertschi P, Jequier E. Energy expenditure by doubly labeled water: validation in humans and proposed calculation. Am J Physiol. 1986;250:R823–R830. doi: 10.1152/ajpregu.1986.250.5.R823. [DOI] [PubMed] [Google Scholar]
- Schoeller D, van Santen E. Measurement of energy expenditure in humans by doubly labeled water method. J Appl Physiol. 1982;53:955–959. doi: 10.1152/jappl.1982.53.4.955. [DOI] [PubMed] [Google Scholar]
- Schutz Y, Weinsier R, Hunter G. Assessment of free-living physical activity in humans: an overview of currently available and proposed new measures. Obes Res. 2001;9:368–379. doi: 10.1038/oby.2001.48. [DOI] [PubMed] [Google Scholar]
- Stewart AL, Mills KM, King AC, Haskell WL, Gillis D, Ritter PL. CHAMPS physical activity questionnaire for older adults: outcomes for interventions. Med Sci Sports Exerc. 2001;33:1126–1141. doi: 10.1097/00005768-200107000-00010. [DOI] [PubMed] [Google Scholar]
- Strath SJ, Pfeiffer KA, Whitt-Glover MC. Accelerometer use with children, older adults, and adults with functional limitations. Med Sci Sports Exerc. 2012;44:S77–S85. doi: 10.1249/MSS.0b013e3182399eb1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swartz A, Strath S, Bassett D, Jr, O’Brien W, King G, Ainsworth B. Estimation of energy expenditure using CSA accelerometers at hip and wrist sites. Med Sci Sports Exerc. 2000;32:S450–S456. doi: 10.1097/00005768-200009001-00003. [DOI] [PubMed] [Google Scholar]
- Troiano RP, Berrigan D, Dodd KW, Masse LC, Tilert T, McDowell M. Physical Activity in the United States Measured by Accelerometer. Medicine & Science in Sports & Exercise. 2008;40:181–188. doi: 10.1249/mss.0b013e31815a51b3. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services, P. A. G. A. C. Physical Activity Guidelines Committee Report, 2008. Washington, DC: 2008. [Google Scholar]
- Weir J. New methods for calculating metabolic rate with special reference to protein metabolism. J Physiol. 1949;109:1–9. doi: 10.1113/jphysiol.1949.sp004363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Westerterp KR. Pattern and intensity of physical activity. Nature. 2001;410:539–540. doi: 10.1038/35069142. [DOI] [PubMed] [Google Scholar]