Abstract
Background
The use of e-prescribing is increasing annually, with over 788 million e-prescriptions received in US pharmacies in 2012. Approximately 9% of e-prescriptions have medication errors.
Objective
To describe the process used by community pharmacy staff to detect, explain, and correct e-prescription errors.
Methods
The error recovery conceptual framework was employed for data collection and analysis. 13 pharmacists and 14 technicians from five community pharmacies in Wisconsin participated in the study. A combination of data collection methods were utilized, including direct observations, interviews, and focus groups. The transcription and content analysis of recordings were guided by the three-step error recovery model.
Results
Most of the e-prescription errors were detected during the entering of information into the pharmacy system. These errors were detected by both pharmacists and technicians using a variety of strategies which included: (1) performing double checks of e-prescription information; (2) printing the e-prescription to paper and confirming the information on the computer screen with information from the paper printout; and (3) using colored pens to highlight important information. Strategies used for explaining errors included: (1) careful review of patient’ medication history; (2) pharmacist consultation with patients; (3) consultation with another pharmacy team member; and (4) use of online resources. In order to correct e-prescription errors, participants made educated guesses of the prescriber’s intent or contacted the prescriber via telephone or fax. When e-prescription errors were encountered in the community pharmacies, the primary goal of participants was to get the order right for patients by verifying the prescriber’s intent.
Conclusion
Pharmacists and technicians play an important role in preventing e-prescription errors through the detection of errors and the verification of prescribers’ intent. Future studies are needed to examine factors that facilitate or hinder recovery from e-prescription errors.
Keywords: Electronic prescribing, E-prescribing, Medication Errors, Error Recovery, Community Pharmacy
INTRODUCTION
Medical errors are frequent in the U.S. healthcare system and are a known barrier to safe delivery of patient care. More than a decade ago, the Institute of Medicine (IOM) reported that medical errors are the cause of severe harm and even death for a large number of patients.1 Both widely prevalent and capable of severe harm, medical errors injure one million patients and cause at least 44,000 deaths annually.1–3 Medication errors are a major category of medical errors and are defined as errors that occur at any stage of the medication-use process, such as prescribing, dispensing, and administration of medications.4 Of the 44,000 deaths caused by medical errors annually, over 7,000 of these deaths have been attributed to medication errors.1
There are two major approaches used by healthcare systems to address medication errors and improve patient safety: error elimination and error management.2, 3 In an effort to eliminate errors, many healthcare settings have implemented new health information technologies (health IT) into their work environment. One such type of health IT is electronic prescribing (e-prescribing), which has been recommended to help reduce medication errors.5, 6 In order to incentivize use, e-prescribing has been included as a core measure for achieving the policy on meaningful use of health IT by physicians; consequently, a physician is required to transmit at least 40% of prescriptions to pharmacies using a certified e-prescribing system.7
E-prescribing in the U.S. generally involves the transmission of prescription or prescription-related information, between a prescriber and a pharmacy through an intermediary e-prescribing network.6, 8 Thus, pharmacies receive electronic prescriptions (e-prescriptions) from prescriber offices in addition to more traditional methods of transmission, including paper, faxed, or phoned prescriptions. Despite the recent introduction of e-prescribing, medication errors still occur with prescriptions received in community pharmacies.9 Of particular concern are new types of medication errors that have emerged as a result of e-prescribing. These medication errors due to e-prescriptions in community pharmacies are especially troubling because the health IT was adopted as a means of eliminating errors.
One study estimated that 11.7% of e-prescriptions received in community pharmacies have errors that require intervention by pharmacists.8 Researchers in this study found that the rate of pharmacists’ intervention on medication errors was similar for e-prescriptions and traditional paper prescriptions. Pharmacists play a pivotal role in preventing e-prescription errors from resulting in patient harm because they are the last point of review for prescriptions before medications are dispensed to patients. It is well established that in the healthcare system, community pharmacists have the ability to intercept medication errors before they reach the patient.10–12 Indeed, pharmacist intervention on prescription-related medication errors can prevent negative consequences, such as adverse drug reactions, from reaching patients.13, 14
Most studies on errors in community pharmacies have focused primarily on quantifying errors and pharmacy interventions rather than understanding the process used by pharmacists and technicians to recover from errors.10, 15 Investigating the process used for recovering from e-prescription errors in community pharmacies can provide valuable insight into how to design pharmacy work systems to maximize the recovery of errors by community pharmacy staff. Therefore, understanding how pharmacists and technicians recover from e-prescription errors is an important step in identifying potential strategies to enhance patient safety.
Within the field of safety science, errors intercepted before reaching patients (near misses) are conceptualized as proactive opportunities and recovery processes.16, 17 Error management, through error recovery processes, are strategies used to prevent or minimize errors from reaching patients.18 The examination of e-prescription error management through the study of error recovery processes in pharmacies may help reduce the number of errors that lead to negative consequences for patients and provide guidance on the redesign of systems that ensure safety.
OBJECTIVES
The mechanisms used by pharmacists and technicians (pharmacy personnel) in community settings to recover from e-prescription errors are largely unknown. The purpose of this study is to gain insight into the error recovery processes used in community pharmacies to address e-prescription errors. Specifically, this study aims to explore the research question: how do pharmacists and technicians in community settings detect, explain, and correct e-prescription errors?
CONCEPTUAL FRAMEWORK
Human factors concepts and techniques have been widely used to examine safety issues in hospital settings but have been rarely applied in community pharmacy research.2, 19–21 Human factors and ergonomics, commonly referred to as “human factors,” is the scientific discipline that seeks to understand interactions among humans and other elements of the systems by applying theoretical principles and techniques to design in order to optimize human well-being and system performance.22 Thus, the science of human factors plays an important role in examining human error and its role in patient safety. Various patient safety researchers have employed concepts from human factors to study safety issues in healthcare settings.23–25
The application of human factors concepts offers a novel approach to improving patient safety in community pharmacies. To explore e-prescription error recovery in community pharmacies, a human factors approach was employed. Most error recovery studies have been carried out in other industries, with minimal error recovery research in healthcare settings.26–31 For example, the examination of error recovery processes is commonly applied in the aviation industry to develop system designs and training solutions for managing errors in unforeseen situations.32 The examination of error recovery processes has also been used to investigate causation of accidents in the chemical industry.33 This line of research has provided insight for redesign of information systems in order to minimize negative consequences.
Error recovery has been defined as the process of detecting, explaining, and correcting an error.34 The error recovery process starts with a failure in the work system that leads to an error. The error must then be detected and actions must be taken to correct the error, or prevent or repair any negative outcomes that occur as a result of the error.18 Error detection also sometimes referred to as error identification, has been defined as realizing or suspecting that an error has occurred or knowing (either consciously or subconsciously) that an error has occurred. Detection of an error is the process of identifying or recognizing an actual or potentially dangerous situation. After error detection, the individual will go through a process of determining why the error occurred; this process is referred to as diagnosis or explanation. This process may occur during or after error correction or not at all. Error explanation also referred to as error diagnosis, is defined as identifying the nature of the error and explaining why it occurred. Error correction can simply be defined as the process of taking definitive steps to remedy an actual or potential error. The concept of error recovery was employed to guide the exploration of the e-prescription error recovery process in community pharmacies.
METHODS
The research coordinator contacted pharmacy managers of five community pharmacy sites in Southwest Wisconsin community pharmacies where prior existing relationships had been established. Pharmacists and technicians from these five community pharmacies in Wisconsin were invited to participate in this research from October 2012 to April 2013. Two of the study sites were chain pharmacies and three of the pharmacies were independent pharmacies. Informed consent was obtained from all participants. Each participant was remunerated $50 for participating in the study. This research was approved by the University of Wisconsin-Madison Institution Review Board.
Three methods of data collection were used for the study: observation, interviews, and focus groups. The combination of data collection methods enabled the researchers to capture e-prescription error recovery in real time and also to obtain data on strategies used by participants through their recall of past events with e-prescription errors. For this study, an e-prescription error was defined as an omission, inaccuracy, or ambiguity in e-prescription information identified by pharmacy personnel that may lead to inappropriate medication use by patients. The data collection instruments developed for this study as shown in the appendices were designed to elicit information about the different phases of error recovery (detection, explanation, and correction).
Direct Observations
Observation is a research method that is commonly used to understand and interpret human behavior and how people function within a particular context or process.35 Observations were used to understand how pharmacists and technicians responded to e-prescription errors in their natural work environment. Direct observations of pharmacists and technicians were conducted primarily on weekdays between 8am and 8pm. Pharmacy personnel in each pharmacy were observed on two separate days for a period of 4 hours each day. A total of 26 pharmacy personnel participated in the direct observations (11 pharmacists and 15 technicians). On the first day of observation, the pharmacy was observed during early hours of operation and during later hours of operation on the second day of observation. Two researchers with experience in patient safety research (one pharmacist - OO and one human factors engineer - JS) observed how participants responded to e-prescriptions errors they encountered in their practice setting. Participants were instructed to inform the researchers whenever they encountered an e-prescription error. OO and JS took extensive field notes on how the e-prescriptions were processed by the pharmacy staff, the types of e-prescription errors that were encountered, and how these errors were resolved.35, 36 Field notes of each observation were transcribed within 24 hours of the observation period.
Direct observations were done prior to interviewing participants to identify how e-prescriptions errors were recovered in real-time at each particular pharmacy. In addition, data from the observation field notes served as a background to inform the follow-up semi-structured interviews and provided appropriate context of information described by participants during these interviews.
Interviews
The second phase of data collection involved semi-structured interviews to obtain additional in-depth information about how pharmacists and technicians recovered from e-prescription errors. Data were collected using an interview guide that consisted of predetermined questions (see appendix A). The error recovery model constructs were used to develop the interview guide and helped to create probes to the interview questions37 since participants were asked to describe their experience in detecting and correcting e-prescription errors. Prompts and probes shown in the interview guide were used to elicit information about recovery processes used by participants. Questions were structured to be neutral and open in an effort to avoid eliciting socially desirable responses.38 Questions were reviewed for content validity by 5 experts: 4 pharmacists, and 1 human factors engineer.
Twenty participants (11 pharmacists and 9 technicians) were interviewed; seventeen of these individuals had participated in the direct observations. The interview guide was sent to participants one week prior to the scheduled interview. OO and JS conducted the interviews. One researcher facilitated the interview while the second researcher took notes and assisted in asking questions and using prompts and probes to elicit more information from the interviewees. Each interview lasted about one hour. The interviews were audio-taped and audio recordings were professionally transcribed. OO selected and listened to eight audio-recorded interviews (40%) to verify the accuracy of the transcription process. The transcripts were found to be an accurate representation of the interview audio-recordings. OO and JS met with a third researcher (MC) to discuss the interview transcripts and data analysis plan.
Focus Groups
After all pharmacy participants were interviewed, two separate in-person focus groups (a pharmacist focus group and a technician focus group) were conducted. A focus group guide (see appendix B) was then developed to: (1) summarize and verify data obtained from observations and interviews, ensure that data were interpreted correctly, provide participants the opportunity to give feedback on data obtained, see data from other pharmacies, and provide additional information not captured during observations and interviews; and (2) to examine in more depth the role of technicians and pharmacists in e-prescription error recovery. The focus group guide was created by triangulating and summarizing the data from interviews and observations to reflect information received from all pharmacies. Three researchers (OO, JS, MC) met to review the focus group questions and summary data documents. These data were presented to participants in the form of summaries of the strategies used to address e-prescription errors from all pharmacies during focus group.
The technician focus group took place in late March 2013, (eight weeks after the last interview) while the pharmacist focus group was held in early April 2013. Four technicians participated in the technician focus group and eight pharmacists participated in the pharmacist focus group. All of these individuals had previously participated in the one-on-one interviews. The focus groups were facilitated by OO. Participants were emailed the focus group questions and documents one week prior to the focus group.
Each in-person focus group lasted for approximately 90 minutes. One pharmacist joined the focus group via telephone. Immediately following the first focus group, the research team held a debriefing session to address issues that came up during the first focus group held with technicians. The researcher team reviewed the focus group questions and discussed changes to be made to improve clarity for participants in the second focus group held with pharmacists. All responses were tape-recorded and transcribed verbatim by a professional transcriptionist. OO listened to the tape recordings from the two focus groups and read through the transcripts to ensure the accuracy of the transcriptions. At the completion of both focus groups, a comprehensive summary was generated. This summary included transcripts of audiotapes as well as anecdotal and field notes.
Data Analysis
Observation field notes, interview transcripts, and focus group transcripts were imported into the qualitative analysis software NVivo 10. Field notes and transcripts were subjected to content analysis.39 This analytical process involved OO and JS reviewing field notes and transcripts line by line to identify sections of the text that were assigned as codes. The codes were conceptualized by using constructs of the three-step error recovery framework, that is, detection, explanation, and correction. The data was also coded for emergent codes that were not reflected by these three main phases of error recovery. For example, the data were coded to identify specific strategies used at different phases of e-prescription error recovery. Following the creation of codes, two researchers (OO and JS) reviewed field notes within each code to identify patterns and trends in the data which were then summarized into higher-level themes. These themes were further reviewed by a third researcher (MC). The research team met to address disparities and inconsistencies within the data and create final descriptions of the study findings.
RESULTS
A total of 13 pharmacists and 14 pharmacy technicians from five pharmacies (two chains and three independents) participated in the study. The age range of participants was 27 to 69 years old (mean age: 45.6 years) for pharmacists and 22 to 59 years old (mean: 36.8 years) for technicians. Participants’ pharmacy experience ranged from 3 to 44 years (mean: 20.6 years) for pharmacists and 3 to 30 years (mean: 18.1 years) or technicians. In Wisconsin, technicians were not required to receive formal training to practice as pharmacy technicians. While some technicians stated they had received formal training, technician participants mainly received “on the job” pharmacy training.
All participants have encountered e-prescription errors in their practice settings. Participants reported that e-prescription errors were encountered on a daily or weekly basis, but stated that the number of e-prescription errors encountered was hard to predict. Participants reported that most e-prescription errors were attributed to poor design of physicians’ e-prescribing systems or inability of the pharmacy computer to translate e-prescription information correctly into their own e-prescribing system.
Error Recovery Process
Pharmacy personnel expressed that once e-prescription errors were detected they focused on getting the right order for the patient and understanding and verifying the prescriber’s intent. Participants ensured that they were giving the correct drug and dosing regimen to prevent any negative consequences for their patients.
Specifically, participants indicated that their goals for the e-prescription error recovery process were to:
-
-
Correct the error and obtain a new e-prescription before the patient arrives in the pharmacy
-
-
Minimize confusion for the patient and improve the patient’s understanding of the prescriber’s intention of how the medication is to be taken
-
-
Ensure that both patient and pharmacy were billed correctly
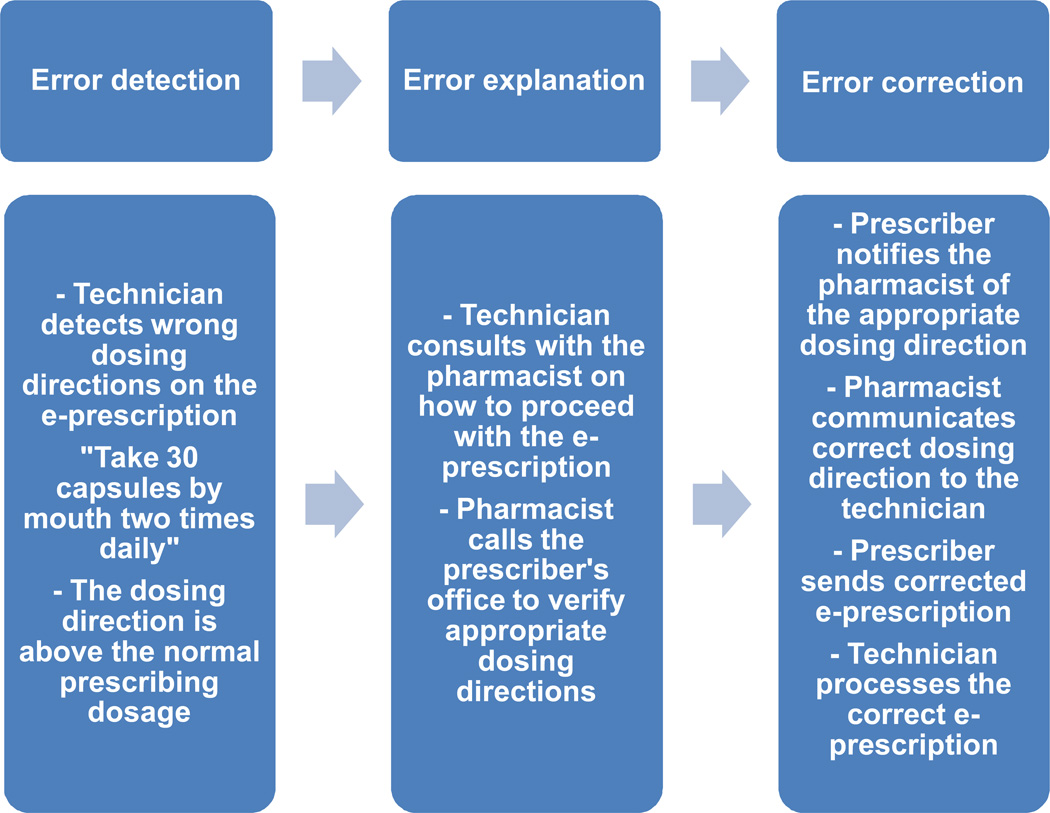
The e-prescription error recovery process was conceptualized as three main phases: detection, explanation, and correction shown in Figure 1.
Figure 1.
Process for e-prescription error recovery
Detecting the error
Participants perceived that it was their responsibility to detect e-prescription errors and that it was rare for e-prescription errors to go undetected in the pharmacy. However, one participant stated that the pharmacy may not catch all e-prescription errors. Pharmacists and technicians reported encountering e-prescription errors on a daily (approximately 5 errors out of 100 e-prescriptions) or weekly basis (5 to 15 errors per week) in their practice setting. Participants reported that the frequency of e-prescription errors encountered varied by time of day and the number of e-prescriptions sent from physician offices. Pharmacists and technicians encountered a variety of errors: wrong drug quantity, wrong dosing directions, wrong dosage formulation, wrong patient, duplicate therapy, wrong drug, wrong strength, wrong pharmacy, and wrong prescriber notes.
Most e-prescription errors were detected during the inputting of the e-prescription information into the pharmacy systems. Of the 75 errors that were detected during the observation period, 92 % were detected at the inputting phase of processing the e-prescription. Fewer errors (7%) were detected during pharmacist review of the prescription and 1% of the errors were detected by patients. One technician described how errors are often addressed before the patient comes into the pharmacy: “If we haven't caught it up on the processing portion, [patients will] come in and say, I’m not supposed to have a change, and then we'll stop and call the doctor. But generally, we try to notice it before it gets to the patient level.”
Since the input technician first encounters the e-prescription, 76% of observed errors were detected by technicians, while 23% were detected by the pharmacist (in one pharmacy, only pharmacists input e-prescriptions into the pharmacy system). Most errors detected by technicians were related to wrong quantity or wrong duration of therapy. Pharmacists detected errors related mostly to wrong dosing directions and wrong dosage formulation. Although technicians detected e-prescription errors, one participant stated that technicians were not expected to detect e-prescription errors due to their limited pharmacy education and training.
Explaining and correcting the error
Participants described the process of explaining the e-prescription error as, “you need to do some detective work.” Once the error had been detected by one pharmacy staff, explaining and correcting the error usually involved a team approach.
Technician: “I would say it usually involves more than one staff person. I will usually enter the instructions that I think are most reasonable and then consult the pharmacist who will, in turn, either have me or they call the doctor's office for the clarification.”
E-prescriptions errors were usually corrected before the patient arrived at the pharmacy. If the patient arrived in the pharmacy before the error was addressed, patients were either dispensed some medication to last for a short period of time (less preferred alternative) or were called to pick up their medications after the error had been corrected in the pharmacy. Participants stated that they appreciated when prescriber offices also contacted patients to communicate that the e-prescription error was being addressed.
Pharmacist: “If we can't resolve it, patients have to come back. Occasionally, I have dispensed it and basically, if the directions didn't make any sense, I will dispense it the way the directions said as long as I know that they have enough drug…But I don't like to do that, things go out the door not right…If the doctor's office calls back after the drug has been dispensed, I let patients know that we dispensed the drug as [the doctor office] prescribed, and that we would call … the patient, but they should call the patient too.”
Variation in error recovery process
The recovery process used by participants for all e-prescriptions errors were generally similar; however e-prescription error recovery varied based on participants’ past experience, type of error, and individual preferences. For example, some participants preferred faxing the prescriber the e-prescription error while others preferred calling the prescriber. Some participants perceived that calling rather than faxing the prescriber helped to correct e-prescription errors faster. While other participants preferred to fax or combine faxing and calling the prescriber about the e-prescription error so that the prescriber could see the error and possibly prevent future similar errors. All participants preferred calling the prescriber to address errors for antibiotic medications to ensure patient could begin drug therapy as soon as possible.
Technician: “Prescribers just don't respond. And we had a file system, and we'd write the date when we'd fax it. And that's when I just call, because otherwise it's going to be sitting there three days later when I come back to work. So, I mean, if you need them to see the error, I usually would fax it, like circle it, and then call them right away. ”
Pharmacist: “It’s hard to do via fax, so, yeah, but I prefer the fax over calling, just because it's simpler. It's easier for everyone. It works into their workflow, and it works into my workflow better.”
For certain errors such as wrong quantity package size (i.e., e-prescription received with quantity “1” when the intent was #1 inhaler) participants did not contact the prescriber but corrected the error in the pharmacy by using the medication package size available from the drug manufacturers.
Participants provided a wide variety of explanations and interpretations for the e-prescription errors encountered in their respective practice settings based on their past experience and communication with prescribers. Their explanations were often dependent on the type of error. As shown in Table 1 examples of e-prescription errors detected by pharmacy personnel included: wrong strength (abnormal dosing – dose too low or too high), wrong pharmacy (e-prescription sent to the wrong pharmacy that was previously used by the patient), wrong dosing directions (prescriber forgets to remove incorrectly auto-populated information), and wrong quantity (incorrectly calculated or inputted by prescriber, or prescriber does not know quantity unit package size available).
Table 1.
Example of e-prescription errors
| Type of errors | Examples |
|---|---|
| Wrong quantity | Technician observation: Trimethoprim-sulfamethoxazole (bactrim DS) 800–160 tablet, the sig (dosing direction) states “take 1 tab by mouth 2 times daily for 10 days, Qty 10. As the input technician is entering the prescription she notices the quantity should have been 20 to have enough medication for 10 days. The technician immediately calls the doctor’s office and the nurse picks up, who transfers the phone to the doctor. The doctor says he is “not so good at math.” |
| Technician interview: “I don't know how they see it on their end. I just don't think they know how things are packaged. It's just like eye drops, they're either 5 ml or 10 ml or 15 ml. You know, and then they send over one [quantity 1]. Which one? You know, you can have three eye drops with three different sizes. Or creams too.” | |
| Wrong dosing directions | Technician interview: “If we had given her ten days, and she only needed five days, then she had 20 extra pills lying around, and now what's she going to do with them, so?” |
| Wrong strength | Pharmacist interview: “It was an unintended dose increase [I think the omeprazole had simply gone from a 20 mg capsule to a 40mg].” |
| Wrong pharmacy | Pharmacist interview: “ The e-prescription was sent to another pharmacy instead of our pharmacy” |
Strategies Used to Recover from E-Prescription Errors
Participants identified a number of strategies to recover from e-prescription errors. These strategies can be used to detect, explain, and/or correct error.
Detecting E-Prescription Errors
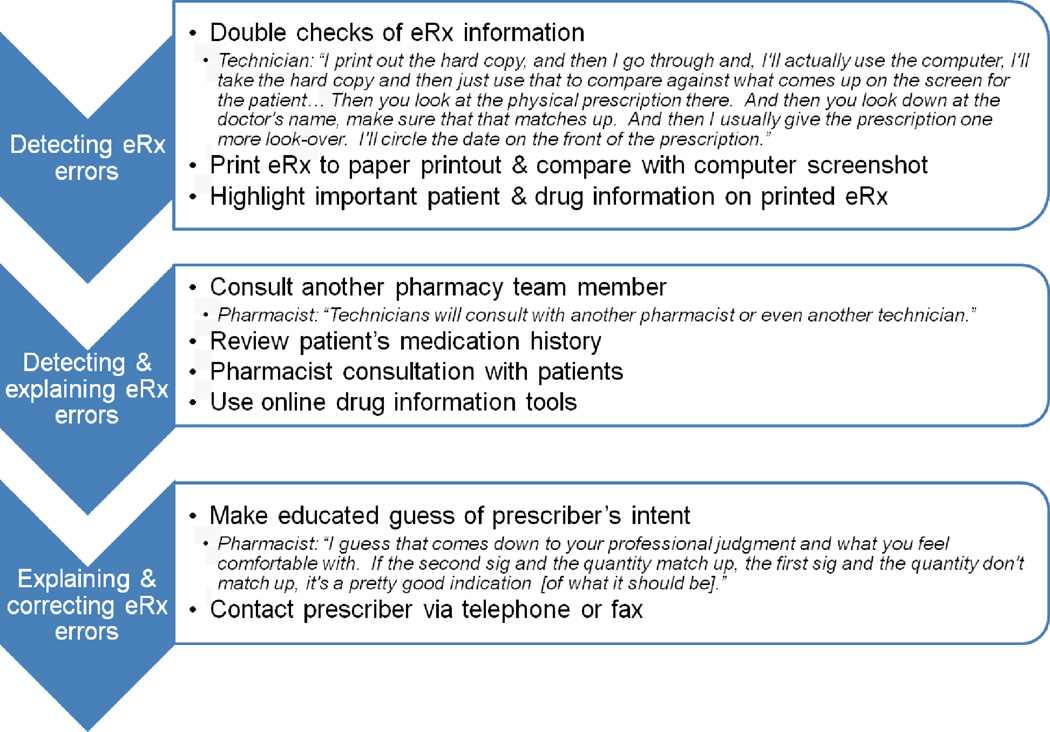
As shown in Figure 2, three main strategies were used to detect e-prescription errors in all five pharmacies.
Figure 2.
Strategies for e-prescription error recovery
1. Double checks
There are several accuracy checks that have been built into the e-prescription processing workflow in the pharmacy. The e-prescription received from physician offices is typically reviewed by three pharmacy staff (two technicians and one pharmacist). Participants noted that these built-in double checks in the e-prescription workflow and a team approach to handling e-prescriptions helped pharmacy staff to detect e-prescription errors before they reached the patient. Based on their previous experience and suspicion that an e-prescription error was likely to happen, pharmacy personnel performed additional double checks when dealing with e-prescriptions for certain drugs. Pharmacists mentioned that they tended to perform additional checks when dealing with e-prescriptions for drugs with a narrow therapeutic index (such as warfarin), drugs that typically have wrong dosing directions, and drugs with multiple dosage forms. For example, for drugs with multiple dosage forms, participants ensured they verified what dosage form the patient had had in the past with the form that was prescribed on the e-prescription. This verification process typically clued in pharmacists to wrong dosage form errors.
Technician: “The quantity thing, like on a Prednisone prescription that comes through, I'll always do the math myself just to double check it. I never sort of assume that the doctor or even, I mean, I'll always, I'll double check the pharmacist, because I know they do it as well but just another set of eyes, just making sure that, you know, take three for three days, because you'll sometimes end up with five or six lines with a taper. I'll just make sure that there's actually enough medicine there to do what they want. So that's another eyes-on sort of thing.”
2. Print e-prescription to paper hardcopy
Participants perceived that having a printed version as opposed to an electronic version of the e-prescription made it easier to detect errors. Participants also stated that printing the e-prescription helped them to perform double checks of the information. One technician stated that many errors would not be detected if the pharmacy did not print e-prescriptions. Some participants thought that printing the e-prescription, inputting the information into the computer, and then verifying patient and drug information allowed them to more easily identify discrepancies between the original and inputted prescription. This is in contrast to viewing the inputted e-prescription next to the original text e-prescription on the same screen because information was sometimes cut off on the computer screen. One pharmacist stated that it was harder for her to detect e-prescription errors on the computer because she wasn’t born in a generation that frequently used computer screens.
Technician: “The easiest way to identify the error is the actual printed version of it, because it's just all right there and you can just look at all the patient information. And then you just go down to the drug and then down to the doctor. So I guess the easiest way to determine the error would just be looking at it at that time, right at the paper. And I always do look at the paper before I actually look at the screen, just because usually when you start to enter the e-prescription, the thing pops up for you to pick the drug.
3. Highlight information on the printed e-prescription
Participants stated that it was important for pharmacy staff to be aware of what information was reviewed when other staff processed e-prescriptions. Therefore, another strategy used to detect errors was highlighting relevant drug or patient information on printed e-prescription using colored pens when processing e-prescriptions. For example, participants highlighted the drug dosing directions, the type of drug formulation, the drug strength, and the patient’s name. Highlighting these key parts of the e-prescription made information easier to read and errors easier to identify. Also, participants highlighted drug and patient information on e-prescriptions with errors that were faxed back to prescribers.
Pharmacist: “We actually use highlighters when the prescription is input by either a pharmacist or an input technician, and then the technician who fills it is another person [fill technician]. And then the person who's filling it actually, we like them to match the label with the hard copy and highlight it as they read it, showing that they did double check it. So it's a part of our process. And when the pharmacist checks it, it shows us that two sets of eyes looked at it, or you know there was another set of eyes that looked at it and checked it for errors.”
Detecting and Explaining E-Prescription Errors
In all five pharmacies, four strategies were identified as strategies used to detect and explain e-prescription errors as shown in Figure 2.
1. Consult another pharmacy team member
The processing of e-prescriptions involved technicians and pharmacists taking a team approach to verifying e-prescription information. Such team work helped to detect errors as technicians and pharmacists exchanged information about details of the drug or patient on the e-prescription. In addition, technicians often investigated e-prescription errors by consulting with another technician or pharmacist. Technicians tended to consult with a pharmacist rather than another technician because they perceived that the pharmacist had more pharmacy educational training about drugs.
Technician: “Especially on e-prescriptions, it isn't like you're going to your fellow tech and saying, what do you think that says on there? You know, so you would be checking with the pharmacist on an e-prescription. If I had a question I think I always went to the pharmacist.”
Technicians expressed that they did not always ask the pharmacist about the e-prescription errors but sometimes directly contacted the prescriber. Pharmacists were less likely to consult another pharmacy staff but relied more on immediately contacting the prescriber to explain the error. However, one pharmacist stated that it was helpful when the pharmacy had more than one pharmacist on duty to consult with on e-prescription errors.
2. Review patient’s medication history
Another common strategy used by pharmacy staff to explain or interpret e-prescription errors involved carefully reviewing the patient medication history or profile available in the pharmacy database. This was only useful if the patient typically used the pharmacy. This strategy was also used to detect e-prescription errors. E-prescription information which appeared different from what was presented in the patient’s pharmacy medication profile was an indication to pharmacy staff that there might have been an unintended or inadvertent error.
Pharmacist: “One time we had a hydralazine that was supposed to be hydroxyzine. And if you look at the dosage, there's a hydralazine 25, there's a hydroxyzine 25, which makes it really nice, [sarcastic]. And I believe that there's also a hydroxyzine 10 and a hydralazine 10 too. In other words, one thing you could look at as well, the tablet strengths may be different. In this case, it matched up, literally. And we just noticed this simply because when we looked at the profile review. We noticed that they'd been getting hydralazine all the time. Where is this hydroxyzine coming from all of a sudden? Same directions, quantity, so you're thinking, okay, did something happen?”
3. Pharmacist consultation with patients
Participants stated that patient information, such as diagnosis, would be helpful to assess the accuracy of an e-prescription and this was rarely present on e-prescriptions. Consequently, one of the common strategies used by pharmacists and technicians to detect or explain e-prescription errors was talking to patients when they arrived at the pharmacy to pick up their medications. It was an important procedure for pharmacist to perform consultation with patients before medications were dispensed. During the course of pharmacist consultation, the pharmacist could elicit information about patient’s interaction with the prescriber. Thus, pharmacy personnel inquired from the patient about the appropriate drug treatment regimen intended by the prescriber. This strategy was particularly useful if the patient did not have a medication profile or history in the pharmacy. During pharmacists’ consultation with patients, pharmacists performed “show and tell,” which involved showing patients their medications and counseling them on how to take these medications. Participants stated that performing show and tell helped patients to identify if there was an e-prescription error. One pharmacist stated that performing show and tell in addition to reviewing the patient’s medication profile were the two biggest areas that helped detect e-prescription errors in the pharmacy.
Pharmacist: “Patient consultation as well, asking them questions about, if we identify anything in the profile review that maybe sets off a small alarm, we can ask the patient. And sometimes the patients will say, yes, this was intended, or sometimes they'll just [say], I have no idea what you're talking about, this wasn't supposed to be changed. And that will cue us to an error as well.”
Although pharmacy staff communicated with patients about e-prescription errors, they did not always rely on statements from patients to correct the error; pharmacists preferred clarifying with prescribers.
4. Use of online drug information tools
Another strategy used by pharmacists and technicians was to use resources such as online drug references, and the manufacturer’s or wholesale’s drug database. When pharmacy personnel detected an e-prescription error they sometimes sought out possible explanations of the prescriber’s intent using appropriate online drug information tools. Tools such as Micromedex® were used to verify prescribed drug doses for certain diagnoses. Checking the manufacturer database was useful in detecting or explaining wrong drug formulation errors. Pharmacy personnel used this strategy especially when dealing with dosing direction errors with duplicate or conflicting directions.
Pharmacist: “Well, first thing, we look in our database to find the drug, and it wasn't in there. Then we go to the wholesaler's order entry system to see if it's available from the manufacturers or our wholesaler. And if we see it there and see that it's an injectable-only drug, and it's not usually given by people themselves, or in this case we couldn't even find it, then we figure there must be a mistake.”
Explaining and Correcting E-Prescription Errors
The two main strategies used by pharmacy personnel in all five pharmacies to explain and correct e-prescription errors as shown in Figure 2.
1. Make educated guess of prescriber’s intent
In order to correct some e-prescription errors, pharmacy staff sometimes made educated guesses of the prescriber’s intent based on past experience and professional judgment. For some errors, such as conflicting or poorly worded dosing directions, pharmacists decided not to make any changes and to dispense “as is” to the patient, assuming that the prescriber made it clear to the patient how to use the medications. This was common with errors related to wrong quantity “quantity 1,” and duplicate dosing directions. When e-prescription errors were corrected (therefore changed) by making educated guesses, participants sent prescribers the notification of changes via fax. Participants stated that they did not want to make a habit of making assumptions of the prescriber’s intent but sometimes it was a waste of time to call the prescriber on every e-prescription error. This was particularly common with “wrong quantity” errors for creams and ointments. Participants made educated guesses also based on other details about the drug information provided on the e-prescription. For example, participants used the dosing directions to estimate the intended quantity prescribed. One participant noted that it was preferable to contact the prescriber rather than make an educated guess to correct the e-prescription error.
Pharmacist: “So we get prescriptions for all those different quantities. And if we called every time to verify what they really meant, it would just be a huge waste of time. So, you know, we go with the best guess as what they meant. One box, they meant five pens, they meant 15 mL. It's funny when they do these insulin pens, for instance, they want a 90-day supply, but they can't figure out mathematically how many units that takes.”
2. Contact prescriber via telephone or fax
Participants reported that their main way of explaining and determining corrections to e-prescription errors encountered was to contact the prescriber via telephone call or faxing the e-prescription back to the prescriber. However, some participants preferred using a combination of both telephone and fax to obtain a quicker response from the prescriber, while others preferred using only one method. Of all the strategies used to correct e-prescription errors, contacting the prescriber was the most frequently used by pharmacists and technicians, particularly accessing the prescriber’s office via telephone calls. Some participants perceived that telephone calls elicited a faster response from the prescriber, especially if the patient had arrived in the pharmacy to pick up the medications.
Other participants preferred faxing the e-prescription error so that the prescriber could see the e-prescription error. This saved pharmacists the time required to call on every e-prescription error. One participant stated that it was important for the prescriber to see the e-prescription error to prevent future errors. Thus, participants included details of e-prescription error that required clarification from the prescriber and highlighted important information for the prescriber by underlining or circling the relevant part of the e-prescription. Thus, faxing the e-prescription error was useful because it: (1) enabled the prescriber to view the e-prescription error and hopefully prevent future errors; (2) minimized misunderstanding during communication between prescriber and pharmacist; and (3) was useful for relaying information when prescriber office was closed and pharmacists could not get hold of prescriber via phone. Participants perceived that prescribers were not aware of some of the e-prescription errors encountered in pharmacies. When participants called prescriber offices to address errors, the receptionist or nurse had to relay the e-prescription error to the prescriber. Prescriber offices sometimes faxed revised e-prescriptions back to the pharmacy or contacted the pharmacy via phone to address the error.
Pharmacist: “My favorite still is faxing the prescribing physician the e-prescription, so that they can see what is coming through. I still think that's the most effective, so that they can hopefully change the behavior or change the order is what we're going for on their end.”
Pharmacist: “Well, we frequently fax a doctor if, and we can put notes on the fax that would indicate what our question is, and then they get back to us. So we don't always have to call.”
DISCUSSION
E-prescribing, like other types of health IT systems, has the potential to improve patient safety in community pharmacies. Nevertheless, errors still occur with e-prescriptions received in pharmacies.8,9 Now that e-prescribing is the primary way prescriptions are received in pharmacies,6 it is important for community pharmacies to focus on e-prescription error recovery because recovered errors are more common than errors that result in actual preventable adverse events40 and can be revealing in learning how to prevent future errors from harming patients.41 Recovered errors are instructive as to the strengths and weaknesses in a system or process.42 For instance, documented errors can be examined by root cause analysis to identify issues in the health care systems that contribute such errors. By examining how e-prescription errors were detected and corrected by pharmacy personnel, findings of this study provide evidence of the role played by pharmacists and technicians in the recovery of e-prescription errors.9
This study found that pharmacy personnel frequently recovered from e-prescription errors. This result is consistent with the literature on error recovery by nurses, physicians, and pharmacists in hospital settings which generally evaluated whether or not error recovery occurred.16, 34, 37–41 Specific to pharmacists, past research has examined the pharmacists’ role in recovery from errors in hospital settings,16, 38 describing how emergency departments and hospitals can best support pharmacists’ detection of medication errors. These studies focused on the occurrence of error recovery rather than the steps necessary for effective error recovery. Thus, past findings have described the fact that error recovery is taking place, but has not gone farther to shed light on error recovery processes to identify effective strategies that can be used by healthcare professionals to reduce errors.
This study is novel in its contribution to the literature as it is the first to study how community pharmacies intervene on e-prescription errors. Specifically, e-prescription error recovery was examined using the human factors engineering perspective (the three-step error recovery framework) which revealed specific strategies used for this process that have not been previous reported in the literature. This is important because error recovery has not received as much attention as the error detection process in the literature. Unlike past studies that have typically assessed the stages of detection, explanation, or correction in isolation43, this study found that a combination of strategies is sometimes used in each phase of recovery. For example, a pharmacist may check a patient’s profile and still use online resources to explain an e-prescription error. Pharmacists or technicians may also skip the explaining step and move from detecting directly to correcting errors, particularly in the case of wrong drug quantity. Consistent with studies that show that detection and correction of potential errors are integral parts of cognitive work in the complex, critical care workplace.44 This study provides additional evidence that the recovery of errors is a complex process requiring the ability to identify an error as well as intercede and assist in remedying the situation. In the future, this framework can be used as a guiding tool to: (1) study error management in pharmacies; and (2) train pharmacy students on error prevention.
Pharmacists and technicians in this study clearly play an active role in the recovery of e-prescription errors. Community pharmacy personnel were aware of the potential for e-prescription errors and could easily explicate the strategies they used and their reasons for using these strategies. These strategies represent deliberate and thoughtful approaches that pharmacists and technicians use to keep their patients safe in environments that are prone to errors. These results, taken together with other studies examining pharmacist intervention of e-prescription errors,8,9 provide evidence that pharmacist and technician vigilance prevents many potentially dangerous situations from reaching and harming patients. The recovery strategies adopted by pharmacy personnel appear to be strongly influenced by their past experiences with e-prescription error recovery, some of which may be positive or negative.
A number of the error recovery strategies reported in this study are similar to strategies used by other healthcare professionals. First, multiple checks in the medication use system has been recommended as a way to help identify system weaknesses and recover from errors.45
Specifically, the use of “double checking” to detect errors has been reported as a strategy used by nurses in critical care and emergency departments.34, 46 Second, the ability for pharmacists and technicians to actively collaborate to address e-prescription errors appears to be an essential element in error recovery. This collaboration requires experience and expertise in work tasks and the ability to communicate questions or concerns.
This study also identified a number of barriers to error recovery. First, addressing some e-prescription errors requires a significant amount of time to reconcile and has the potential to create a burdensome workload.9 The fact that the error recovery process may increase workload is a double-edged sword because during times of high workload, pharmacists are at risk of focusing on fewer cues. As a result, they might miss things they would normally notice, thus miss opportunities to recover from other errors.47, 48Second, a significant barrier identified from this study is that community pharmacies do not have immediate access to prescribers to address errors. This is relevant because a key strategy that pharmacy personnel used to explain and correct errors was to contact the physician office to clarify the intention of the prescriber. Strategies to improve error recovery should identify seamless and efficient ways of communicating common e-prescription errors identified in community pharmacies to prevent future errors.
Third, this study found that organizational culture appeared to influence error recovery strategies. This is consistent with a study that examined error recovery in a hospital pharmacy that found that the pharmacy needed to reduce negative influences, such as organizational culture, on recovery and reinforce positive influences.16 There has been limited research on the role pharmacy organizations should play in training pharmacists and technicians on best practices to detect and prevent e-prescription errors.
The study of error recovery is important as it increases the awareness for healthcare professionals of potential errors in their work environment. Since the knowledge of error recovery mechanisms aids pharmacists and safety researchers identifying recommendations for redesign of systems to reduce the risk of errors reaching patients. It is important for pharmacy organizations to begin identifying aspects of the work environment that promote all stages of error recovery. The findings from this support can be used as a guiding framework on how to support error recovery in pharmacies. In addition, research in human error provides useful tools for designing procedures, training for detecting and recovery from errors.32 Pharmacy managers and pharmacy organizations need to support error recovery and design safe environments for rendering patient care.
Research on the pharmacist and technician roles in e-prescription error recovery is in its infancy. More information is needed on the success of strategies described by pharmacists and on the work environment characteristics that support the recovery process. Although pharmacists and technicians described many similar strategies of error recovery, the effectiveness of those strategies in minimizing errors is unknown. Further study is needed to identify approaches to recover errors that maximize positive outcomes and satisfaction for all involved parties. Detection of e-prescription errors is sometimes based on a feeling or suspicion that the e-prescription information was inaccurate. Researchers noted that e-prescription errors detected by pharmacy personnel were not tracked or reported in any error reporting system and their past encounters with such errors easily enabled them to look out for such errors during the inputting of an e-prescription. It is important for pharmacy organizations to track common e-prescription errors. Such trending of e-prescription errors can be disseminated and used as a form of training to other pharmacy staff to increase awareness of how best to manage errors and prevent future errors.
The recovery process can be also influenced by human, technical, and organizational factors, yet the impact of those factors on patients and pharmacy staff remains unclear. Future research may drill down on barriers and facilitators to recovery from e-prescription errors in community pharmacies. For instance, future research can examine the relationship between e-prescription error recovery and community pharmacy staff experience and their work environment. In addition, further understanding of how e-prescriptions are generated and transferred between prescriber offices and community pharmacies is needed to develop effective interventions strategies to e-prescription errors. Lastly, understanding the limits and failures of human decision-making is important if we are to build robust decision-support systems to manage the boundaries of the risk of error in decision-making.44 Therefore, consideration of pharmacists’ recovery from e-prescription errors has implications for system and design of health IT to improve safety.
Limitations
The study findings should be considered in light of the following limitations. First, the findings are limited to e-prescription error recovery in five Wisconsin community pharmacies. Given the exploratory, sensitive, and time consuming nature of the research, only community pharmacies that were willing to participate were included.
Second, the fact that the pharmacy staff members were observed may have had an impact of their behavior. Participants were not blinded to observations by researchers and may have been biased toward achieving higher e-prescription error recovery during the study. Finally, the responses of participants during the interviews were based on their recall of e-prescription errors that could have occurred just before the interview took place or years before the interview. The recency of the experience may have biased their perspective. In addition, participants may have discussed errors that were not recently experienced but were most memorable because they were perceived as major errors.
Third, e-prescription errors discussed in this study focus mainly on errors that are detected by pharmacy personnel. It is possible that study findings do not reflect e-prescription errors that were difficult to detect, rarely corrected errors, or events not viewed as errors by pharmacy personnel.
CONCLUSION
The results of this study provide preliminary yet compelling evidence of the unique role that community pharmacy staff play in e-prescription error recovery and preventing adverse events. Several strategies by pharmacists and technicians were identified for detecting, explaining, and correcting e-prescription errors. Findings from this study suggest that pharmacists and technicians in community settings play an important role in detection and correction of e-prescription errors. Since this was an exploratory study, the role of community pharmacy staff in e-prescription error recovery deserves further investigation. Further research is needed to be able generalize these findings to other community pharmacy settings. Knowledge of effective recovery strategies can ultimately be used to develop interventions for reducing e-prescription errors and improving patient safety.
ACKNOWLEDGEMENT
This research was funded by the Community Pharmacy Foundation. The authors would like to thank the staff at the community pharmacies that supported and participated in this research. We would also like to thank Drs. Tosha Wetterneck, David Mott, Henry Young, and Pascale Carayon for contribution in conceptualizing the research and providing feedback during manuscript preparation. Michelle Chui was supported by the Clinical and Translational Science Award (CTSA) program, previously through the National Center for Research Resources (NCRR), grant 1UL1RR025011, and now by the National Center for Advancing Translational Sciences (NCATS), grant 9U54TR000021. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
APPENDICES
Appendix A: Interview Guide
E-prescription errors
Do you encounter e-prescription errors? If you do, can you tell me about these errors and why you think they occurred?
Thinking of e-prescriptions errors you encountered with the last 30 days, describe two specific incident were by you had to deal with a challenging e-prescription error.
Probes
What type of error occurred?
How did you realize or suspect the prescription had an error?
Was there any information that helped you detect there was an error?
How did you go about understanding why it occurred?
What was your goal for addressing the error?
What did you consider as possible ways to achieve this goal?
What did you do decide to do about the error?
What was the final outcome?
Was there any other information that helped you resolve the error? [Make sure participants elicit steps they went through to resolve e-prescription error]
How long did it take to resolve the error? Thinking of from the time you detected the error to the time it was resolved.
Did this error remind you of any previous experience?
Was there any specific training or experience that was necessary or helpful in detecting or resolving this error?
Thinking of what was going on in the pharmacy at the time the error took place, on a scale of 1 to 5, 1 being very low and 5 being very high, how much time pressure did you feel when you were addressing this error?
Appendix B: Focus Group Guide
Discuss findings from observation and interviews
Working definitions
E-prescription error is any omission, inaccuracy, or ambiguity in e-prescription information that may lead to inappropriate medication use by a patient.
Identifying means recognizing or sensing there is an error
Resolving means an actual decision or action to do something about the error or fix the error
Present information on error recovery from observation and interviews to participants
Probe questions to determine if everyone identifies and corrects errors the same way
Let’s go around the room and each person mention:
What is your initial gut reaction to these findings?
Is there one way that you use the most?
If you were to pick the best approach, which would you choose?
Are there other strategies used not yet discussed?
Let’s go around the room and each person mention one thing you learned from this focus group.
Contributor Information
Olufunmilola K. Odukoya, School of Pharmacy, Department of Pharmacy and Therapeutics, University of Pittsburgh, Pittsburgh, Pennsylvania.
Jamie A. Stone, School of Pharmacy, Social and Administrative Sciences Division, University of Wisconsin-Madison, Madison, Wisconsin.
Michelle A. Chui, School of Pharmacy, Social and Administrative Sciences Division, University of Wisconsin-Madison, Madison, Wisconsin.
REFERENCES
- 1.Kohn LT, Corrigan JM, Donaldson MS. To err is human: building a safer health system. National Academies Press; 2000. [PubMed] [Google Scholar]
- 2.Leape LL, Berwick DM. Five years after to err is human. JAMA. 2005;293(19):2384–2390. doi: 10.1001/jama.293.19.2384. [DOI] [PubMed] [Google Scholar]
- 3.Amalberti R, Auroy Y, Berwick D, Barach P. Five system barriers to achieving ultrasafe health care. Ann Intern Med. 2005;142:756–764. doi: 10.7326/0003-4819-142-9-200505030-00012. [DOI] [PubMed] [Google Scholar]
- 4.Aspden P, Wolcott J, Bootman JL, Cronenwett LR. Preventing medication errors: quality chasm series. National Academies Press; 2006. [Google Scholar]
- 5.Bell DS, Friedman MA. E-prescribing and the medicare modernization act of 2003. Health affairs (Project Hope) 2005;24:1159–1169. doi: 10.1377/hlthaff.24.5.1159. [DOI] [PubMed] [Google Scholar]
- 6.Surescripts 2012. The National Progress Report on E-prescribing and Safe-Rx Rankings. [Accessed June 10, 2013]; Available at: http://www.surescripts.com/about-e-prescribing/progress-reports/national-progress-reports#downloads. [Google Scholar]
- 7.Crosson JC, Etz RS, Wu S, Straus SG, Eisenman D, Bell DS. Meaningful use of electronic prescribing in 5 exemplar primary care practices. Annals of family medicine. 2011;9:392–397. doi: 10.1370/afm.1261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gilligan AM, Miller K, Mohney A, Montenegro C, Schwarz J, Warholak TL. Analysis of pharmacists’ interventions on electronic versus traditional prescriptions in 2 community pharmacies. Res Soc Adm Pharm. 2012;8:523–532. doi: 10.1016/j.sapharm.2011.12.005. [DOI] [PubMed] [Google Scholar]
- 9.Warholak TL, Rupp MT. Analysis of community chain pharmacists' interventions on electronic prescriptions. JAPhA. 2009;49:59–64. doi: 10.1331/JAPhA.2009.08013. [DOI] [PubMed] [Google Scholar]
- 10.Knudsen P, Herborg H, Mortensen AR, Knudsen M, Hellebek A. Preventing medication errors in community pharmacy: frequency and seriousness of medication errors. Quality and Safety in Health Care. 2007;16:291–296. doi: 10.1136/qshc.2006.018770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chen YF, Neil KE, Avery AJ, Dewey ME, Johnson C. Prescribing errors and other problems reported by community pharmacists. Therapeutics and clinical risk management. 2005;1:4, 333. [PMC free article] [PubMed] [Google Scholar]
- 12.Knudsen P, Herborg H, Mortensen AR, Knudsen M, Hellebek A. Preventing medication errors in community pharmacy: root-cause analysis of transcription errors. Quality and Safety in Health Care. 2007;16:285–290. doi: 10.1136/qshc.2006.022053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Buurma H, De Smet PAGM, Van Den Hoff OP, Egberts ACG. Nature, frequency and determinants of prescription modifications in Dutch community pharmacies. British journal of clinical pharmacology. 2001;52:85–91. doi: 10.1046/j.0306-5251.2001.01406.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pottegård A, Hallas J, Søndergaard J. Pharmaceutical interventions on prescription problems in a Danish pharmacy setting. International journal of clinical pharmacy. 2011:1–9. doi: 10.1007/s11096-011-9580-4. [DOI] [PubMed] [Google Scholar]
- 15.Flynn EA, Barker KN, Carnahan BJ. JAPhA. Vol. 43. Washington, DC: 2003. National observational study of prescription dispensing accuracy and safety in 50 pharmacies; pp. 191–200. 1996. [DOI] [PubMed] [Google Scholar]
- 16.Kanse L, Van Der Schaaf TW, Vrijland ND, Van Mierlo H. Error recovery in a hospital pharmacy. Ergonomics. 2006;49:503–516. doi: 10.1080/00140130600568741. [DOI] [PubMed] [Google Scholar]
- 17.Mick JM, Wood GL, Massey RL. The good catch pilot program: increasing potential error reporting. Journal of Nursing Administration. 2007;37:499–503. doi: 10.1097/01.NNA.0000295611.40441.1b. [DOI] [PubMed] [Google Scholar]
- 18.Wetterneck TB. Handbook of human factors and ergonomics in health care and patient safety. Second ed. CRC PressI LIC; 2011. Error Recovery in Health Care; pp. 449–461. [Google Scholar]
- 19.Carayon P, Wetterneck TB, Hundt AS, Ozkaynak M, Ram P, DeSilvey J. Assessing nurse interaction with medication administration technologies: the development of observation methodologies. Work With Computing Systems. 2004:319–324. [Google Scholar]
- 20.Wetterneck TB, Walker JM, Blosky MA, et al. Factors contributing to an increase in duplicate medication order errors after CPOE implementation. JAMIA. 2011;18:774–782. doi: 10.1136/amiajnl-2011-000255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chui MA, Stone JA. The prescription handoff in community pharmacy: A study of its form and function. JAPhA. 2012;52:e161–e167. doi: 10.1331/JAPhA.2012.11233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Carayon P, Wetterneck TB, Rivera-Rodriguez AJ, Hundt AS, Hoonakker P, Holden R, Gurses AP. Human factors systems approach to healthcare quality and patient safety. Applied ergonomics. 2014;45:14–25. doi: 10.1016/j.apergo.2013.04.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pennathur PR, Thompson D, Abernathy JH, III, Martinez EA, Pronovost PJ, Kim GR, Gurses AP. Technologies in the wild (TiW): human factors implications for patient safety in the cardiovascular operating room. Ergonomics. 2013;56:205–219. doi: 10.1080/00140139.2012.757655. [DOI] [PubMed] [Google Scholar]
- 24.Hundt AS, Adams JA, Schmid JA, Musser LM, Walker JM, Wetterneck TB, Carayon P. Conducting an efficient proactive risk assessment prior to CPOE implementation in an intensive care unit. International Journal of Medical Informatics. 2013;82:25–38. doi: 10.1016/j.ijmedinf.2012.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Carayon P, Wetterneck TB, Cartmill R, Blosky MA, Brown R, Kim R, Walker J. Characterising the complexity of medication safety using a human factors approach: an observational study in two intensive care units. BMJ Quality & Safety. 2013:56–65. doi: 10.1136/bmjqs-2013-001828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Frese M. Error management or error prevention: Two strategies to deal with errors in software design. Human aspects in computing: Design and use of interactive systems and work with terminals. 1991;776:782. [Google Scholar]
- 27.Sellen AJ. Detection of everyday errors. Applied Psychology. 1994;43:475–498. [Google Scholar]
- 28.Van der Schaaf T. Human recovery of errors in man-machine systems; Proceedings of the 6th IFAC Symposium on Analysis, Design, and Evaluation of Man-Machine Systems; 1995. pp. 27–29. [Google Scholar]
- 29.Allwood CM. Error detection processes in statistical problem solving. Cognitive science. 1984;8:413–437. [Google Scholar]
- 30.Bagnara S, Stablum F, Rizzo A, Fontana A, Ruo M. Error detection and correction: A study on human-computer interaction in a hot strip mill production planning and control system. Preprints of the First European Meeting on Cognitive Science Approaches to Process Control. 1987 [Google Scholar]
- 31.Shaffer L, Hardwick J. Errors and error detection in typing. The Quarterly Journal of Experimental Psychology. 1969;21:209–213. doi: 10.1080/14640746908400215. [DOI] [PubMed] [Google Scholar]
- 32.Kontogiannis T. A systems perspective of managing error recovery and tactical re-planning of operating teams in safety critical domains. Journal of Safety Research. 2011;42:73–85. doi: 10.1016/j.jsr.2011.01.003. [DOI] [PubMed] [Google Scholar]
- 33.Van der schaaf TW. Near miss reporting in the chemical process industry [dissertation] Eindhoven, the Netherlands: Eindhoven University of Technology; 1992. [Google Scholar]
- 34.Henneman EA, Roche JP, Fisher DL, et al. Error identification and recovery by student nurses using human patient simulation: opportunity to improve patient safety. Appl Nurs Res. 2010;23:11–21. doi: 10.1016/j.apnr.2008.02.004. [DOI] [PubMed] [Google Scholar]
- 35.Mulhall A. In the field: notes on observation in qualitative research. Journal of advanced nursing. 2003;41:306–313. doi: 10.1046/j.1365-2648.2003.02514.x. [DOI] [PubMed] [Google Scholar]
- 36.Mays N, Pope C. Qualitative research: Observational methods in health care settings. BMJ. 1995 Jul;311:182–184. doi: 10.1136/bmj.311.6998.182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Maxwell JA. Understanding and validity in qualitative research. Harvard educational review. 1992;62:279–301. [Google Scholar]
- 38.Roulston K. Interviews in Qualitative Research. The Encyclopedia of Applied Linguistics. 2013 [Google Scholar]
- 39.Graneheim UH, Lundman B. Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse education today. 2004;24:105–112. doi: 10.1016/j.nedt.2003.10.001. [DOI] [PubMed] [Google Scholar]
- 40.Bates DW, Boyle DL, Vander Vliet MB, Leape L. Relationship between medication errors and adverse drug events. Journal of General Internal Medicine. 1995;10:199–205. doi: 10.1007/BF02600255. [DOI] [PubMed] [Google Scholar]
- 41.Blumenthal D. Making medical errors into 'medical treasures'. JAMA. 1994;272:1867–1868. [PubMed] [Google Scholar]
- 42.Rothschild JM, Hurley AC, Landrigan CP, et al. Recovery from medical errors: the critical care nursing safety net. Joint Commission Journal on Quality and Patient Safety. 2006;32:63–72. doi: 10.1016/s1553-7250(06)32009-0. [DOI] [PubMed] [Google Scholar]
- 43.Henneman EA, Gawlinski A. A “near-miss” model for describing the nurse’s role in the recovery of medical errors. Journal of Professional Nursing. 2004;20:196–201. doi: 10.1016/j.profnurs.2004.04.006. [DOI] [PubMed] [Google Scholar]
- 44.Patel VL, Cohen T, Murarka T, et al. Recovery at the edge of error: Debunking the myth of the infallible expert. Journal of Biomedical Informatics. 2011;44(3):413–424. doi: 10.1016/j.jbi.2010.09.005. [DOI] [PubMed] [Google Scholar]
- 45.ASHP. ASHP guidelines on preventing medication errors in hospitals. Am J Hosp Pharm. 1993;50:305–314. [PubMed] [Google Scholar]
- 46.Henneman EA, Blank FSJ, Gawlinski A, Henneman PL. Strategies used by nurses to recover medical errors in an academic emergency department setting. Applied Nursing Research. 2006;19:70–77. doi: 10.1016/j.apnr.2005.05.006. [DOI] [PubMed] [Google Scholar]
- 47.Bertram DA, Hershey CO, Opila DA, Quirin O. A measure of physician mental work load in internal medicine ambulatory care clinics. Medical care. 1990:458–467. doi: 10.1097/00005650-199005000-00005. [DOI] [PubMed] [Google Scholar]
- 48.Kahneman D, Slovic P, Tversky A. Judgment under uncertainty. Cambridge University Press; 1982. [Google Scholar]