Abstract
Purpose/Objective
Although home exercises are commonly prescribed following anterior cruciate ligament (ACL) reconstruction and are considered important in obtaining successful rehabilitation outcomes, little is known about factors associated with the completion of such exercises. Consequently, this study was designed to identify predictors of adherence to home rehabilitation exercises after ACL surgery.
Research Method/Design
Participants (33 women, 58 men) completed indices of athletic identity, neuroticism, optimism, and pessimism before ACL surgery and measures of daily pain, negative mood, stress, and home exercise completion for 42 days postoperatively.
Results
Participants reported a high level of adherence to the prescribed regimen. Home exercise completion increased significantly over time as the number of sets of prescribed home exercises declined. Personal factors were not predictive of home exercise completion. Participants completed fewer home exercises on days when they experienced more stress or negative mood.
Conclusions/Implications
Day-to-day variations in negative mood and stress may contribute to adherence to prescribed home exercises.
Keywords: compliance, knee, surgery, psychology
Impact
Despite the potential importance of adhering to home exercise programs after anterior cruciate ligament surgery, little research has examined predictors of adherence to such programs and no previous studies have investigated predictors of day-to-day fluctuations in adherence. This study extends the literature by identifying predictors of adherence to home exercises following anterior cruciate ligament surgery through a daily process analysis.
The results of this study demonstrate that potentially fleeting thoughts and moods reflecting the current situation and their interaction with enduring personal attributes contribute to the prediction of adherence to home exercise prescriptions after anterior cruciate ligament surgery.
Interventions directed at enhancing completion of home rehabilitation exercises after anterior cruciate ligament surgery should take into account the associations of day-to-day fluctuations in situational factors such as pain, negative mood, and stress with adherence.
Surgical reconstruction of the anterior cruciate ligament (ACL) is typically followed by a rigorous rehabilitation regimen designed to help patients regain strength and range of motion over an extended period of time before returning to sport activities (Kvist, 2004). Participation in postoperative rehabilitation activities is considered essential to achieving desired outcomes (Blair & Willis, 1991). Positive associations between adherence to ACL rehabilitation programs and clinical outcomes have been documented in several studies (Brewer, Cornelius, Van Raalte, Brickner, Sklar et al., 2004; Brewer, Van Raalte, Cornelius et al., 2000; Derscheid & Feiring, 1987; Pizzari, Taylor, McBurney, & Feller, 2005; Treacy, Barron, Brunet, & Barrack, 1997). Given the apparent benefits of adhering to ACL rehabilitation programs, it is important to determine factors associated with adherence to such programs. Although ACL rehabilitation programs have traditionally had both clinic- and home-based components, changes in the health care climate have prompted an increased emphasis on home rehabilitation activities (Beard & Dodd, 1998; DeCarlo & Sell, 1997; Fischer, Tewes, Boyd, Smith, & Quick, 1998; Grant & Mohtadi, 2010; Grant, Mohtadi, Maitland, & Zernicke, 2005; Schenck, Blaschak, Lance, Turturro, & Holmes, 1997; Treacy et al., 1997). Consequently, the current investigation focused on identifying predictors of adherence to home rehabilitation exercises following ACL reconstruction.
Adapted from theoretical perspectives that have been widely applied across the literature on stress and coping (Lazarus & Folkman, 1984) and are consistent with the interactive patient X context approach that has been advocated to study patient adherence behavior (Christensen, 2004), contemporary models of psychological response to sport-related injury hold that behavioral responses to injury are influenced by the stable personal characteristics of athletes (e.g., personality) and the more transitory cognitive and emotional responses to the situations they encounter during rehabilitation and daily living (Wiese-Bjornstal, Smith, Shaffer, & Morrey, 1998). Thus, in the context of rehabilitation following ACL surgery, it would be expected that enduring personal attributes, potentially fleeting thoughts and moods reflecting the current situation, and the interaction of these two types of factors would contribute to the behavior of adhering to home exercise prescriptions. In support of this hypothesis, research has documented associations between numerous personal, situational, cognitive, and emotional factors and adherence to medical regimens in general (Christensen, 2004) and sport injury rehabilitation programs in particular (Brewer & Cornelius, 2003). For example, an inverse relationship between mood disturbance and sport injury rehabilitation adherence has been documented in two studies (Alzate Saez de Heredia, Ramirez, & Lazaro, 2004; Daly, Brewer, Van Raalte, & Petitpas, 1995).
Despite the abundance of research on factors associated with sport injury rehabilitation adherence (Brewer & Cornelius, 2003), there have been few studies aimed at identifying predictors of adherence to postoperative ACL rehabilitation programs (e.g., Brewer, Cornelius, Van Raalte, Brickner, Sklar et al., 2004; Brewer, Van Raalte, Cornelius et al., 2000; Derscheid & Feiring, 1987; Pizzari et al., 2005; Treacy et al., 1997). Moreover, investigations of adherence to sport injury rehabilitation have targeted clinic-based components of rehabilitation to a greater extent than home-based components and have used research designs that have precluded examination of the relationship between situational factors and day-to-day fluctuations in adherence behavior. In a typical sport injury rehabilitation adherence prediction study, measures of predictor variables are administered prior to and/or shortly after the onset of rehabilitation and adherence variables are assessed over the course of rehabilitation. Such a prospective approach is appropriate for personal characteristics that would not be expected to change over time (e.g., personality variables), but does not permit an assessment of the hypothesized dynamic influence of cognitions and emotions reflecting the current rehabilitation situation on adherence behavior. Consequently, to address these limitations in the extant literature, daily process methods (Affleck, Zautra, Tennen, & Armeli, 1999; Tennen, Affleck, Armeli, & Carney, 2000) were applied in the current study in an attempt to identify predictors of adherence to a postoperative ACL home rehabilitation program. These methods have demonstrated their unique value in numerous areas of psychological inquiry relevant to rehabilitation outcomes including emotional reactivity in daily life (Gunthert, Conner, Armeli, Tennen, Covault, & Kranzler, 2007), daily variability in health behavior (Kiene, Tennen, & Armeli, 2008), situational predictors of risky alcohol use (Armeli, Conner, Cullum, & Tennen, 2010), and coping with chronic pain (Conner, Tennen, Zautra, Affleck, Armeli, & Fifield (2006).
Specifically, measures of personal factors linked theoretically and empirically with psychological adjustment to sport injury and other medical conditions were taken prior to ACL reconstructive surgery, and indices of cognitive and emotional factors reflecting the vicissitudes of rehabilitation (i.e., negative mood, pain, and stress) and home exercise completion were administered on a daily basis over the first six weeks of postoperative rehabilitation. In addition to enabling the identification of both personality and proximal predictors of adherence to a home rehabilitation exercise program, the research design afforded an exploration of the pattern of adherence as the nature and demands of the home program changed over time.
Athletic identity, neuroticism, and optimism/pessimism were the personal factors examined as predictors of adherence. Individuals high in athletic identity, for whom physical activity is a central source of self-definition (Brewer, Van Raalte, & Linder, 1993), were expected to demonstrate greater adherence than individuals lower in athletic identity, presumably due to the adherence-enhancing effects of attaching higher value to the pursuit of rehabilitation goals (Taylor & May, 1996). Given the association of neuroticism with avoidance-related goals (Robinson, Ode, Wilkowski, & Amodio, 2007), an inverse relationship between neuroticism and adherence was hypothesized. Because optimists tend to cope more adaptively with stressful situations (such as surgery and rehabilitation) and expect more favorable outcomes from their health-promoting behavior than pessimists (Scheier & Carver, 1992), it was hypothesized that optimism would be positively associated and pessimism would be negatively associated with adherence. Associations with adherence to health behavior in the expected direction have been documented for each of the personal variables—athletic identity (Anderson, 2004; Roche, 2004), neuroticism (Potgieter & Venter, 1995; Booth-Kewley & Vickers, 1994), and optimism/pessimism (Friedman, Webb, Bruce, Weinberg, & Cooper, 1995; Larney, 2002; Milam, Richardson, Marks, Kemper, & McCutchan, 2004).
Negative mood, pain, and stress were the situational factors assessed as potential predictors of home exercise completion. Given that coping with negative emotions, pain, and stress likely consumes resources that could otherwise be applied to the self-control required to maintain adherence to a rehabilitation regimen (Muraven & Baumeister, 2000), it was predicted that participants would report adhering less well to their rehabilitation protocol on days when they experienced more negative mood, more pain, or greater stress than usual. Negative associations between adherence and each of the situational factors—negative mood (Alzate Saez de Heredia et al., 2004; Daly et al. 1995), pain (Dobkin, Abrahamowicz, Fitzcharles, Dritsa, & da Costa, 2005; Papaioannou, Kennedy, Dolovich, Lau, & Adachi, 2007), and stress (Dobkin et al., 2005; Stetson, Rahn, Dubbert, Wilner, & Mercury, 1997; Farrell, Hains, Davies, Smith, & Parton, 2004)—have been reported in previous quantitative investigations. Qualitative inquiry has identified pain as a barrier to adherence in sport injury rehabilitation (Levy, Polman, Nicholls, & Marchant, 2009). Moreover, in accordance with the interactive approach and with research suggesting that optimists tend to persist in their efforts toward achieving important goals when they encounter obstacles whereas pessimists are more likely to diminish their efforts in such circumstances (Carver & Scheier, 1998), the anticipated associations of optimism and pessimism with adherence were expected to be especially pronounced under conditions of greater negative mood, pain, and stress. Persistence in the face of negative mood, pain, and stress was also hypothesized for participants high in athletic identity, whose pursuit of rehabilitation goals would be less likely to waver than that of participants low in athletic identity due to increased motivation to affirm their sense of self through sport-related activity (Brewer et al., 1993).
Method
Participants
From a sample of 108 consecutive patients who (a) had ACL reconstruction surgery with one of the three orthopedic surgeons involved with the project; (b) enrolled in a postoperative rehabilitation program at one of the three physical therapy clinics affiliated with the project (two of which were in suburban locations and one of which was in an urban location in close proximity to the orthopedic practice); and (c) agreed to participate in a longitudinal study of psychological factors in ACL surgery and rehabilitation, 91 patients (33 women and 58 men) elected to complete the daily self-report portion of the study. Participants were recruited on a consecutive patient basis to allow the results to be generalized to the population of people who have ACL surgery. Participants ranged in age from 14 to 54 years (M = 29.73, SD = 10.24 years), were predominantly White (92%), and reported involvement in competitive (43%) or recreational (54%) sport. Half of the participants indicated that they were married (50%) and half of the participants stated that they were single (46%) or divorced (4%). The majority of participants (54%) reported that the ACL reconstruction was their first encounter with orthopedic surgery.
Measures
Personal variables
Demographic and injury-related information (e.g., age, gender, race/ethnicity, date of ACL surgery) was obtained with a questionnaire. The Athletic Identity Measurement Scale (AIMS) (Brewer & Cornelius, 2001) was used to measure athletic identity, which pertains to the extent of identification with the athlete role. The AIMS has 7 items on which respondents use a scale from 1 (strongly disagree) to 7 (strongly agree) to rate their level of agreement with statements about various aspects of identification with the athlete role. Higher AIMS scores correspond with stronger and more exclusive identification with the athlete role. Coefficient alpha was .85 for the AIMS in the current study. The neuroticism subscale of the NEO Five-Factor Inventory (NEO-FFI) (Costa & McRae, 1991) was used to measure neuroticism. High scores on the 12-item subscale correspond with an increased tendency to experience psychological distress. Items are scored on a 5-point Likert scale from strongly disagree to strongly agree. Evidence supporting the internal consistency (alphas ranging from .86 to .92), test-retest reliability (r = .79 over a 3-month period), and construct validity of the neuroticism subscale has been obtained (Costa & McRae, 1992). Coefficient alpha was .79 for the NEO neuroticism subscale in the current study. The Life Orientation Test-Revised (LOT-R) (Scheier, Carver, & Bridges, 1994) was used to assess optimism and pessimism, which refer to the generalized expectations that good outcomes and bad outcomes, respectively, will occur. In the current study, the 3 optimism items (α = .62) and the 3 pessimism items (α = .78) demonstrated acceptable levels of internal consistency.
Situational variables
A single item on which participants were asked to indicate on a scale from 1 (not) to 5 (very) how stressful their day was served as a measure of perceived daily stress. A numerical rating scale (NRS) with endpoints of 0 (no pain) and 10 (pain as bad as it can be) was used to enable participants to rate how much knee pain they “experienced today on the average over the day.” Jensen and Karoly (2001) presented strong support for the reliability and validity of the NRS. Negative mood was measured with an abbreviated version of the Profile of Mood States—B (POMS-B) (Lorr & McNai, 1982) that has 9 items assessing 3 negative mood states (i.e., anxiety, depression, and hostility). Items from the original POMS-B that had high item-total correlations in a sample of patients with rheumatoid arthritis were selected for the abbreviated version of the instrument (Affleck, Tennen, Pfeiffer, & Fifield, 1987). Item response options range from 0 (very much unlike this) to 3 (very much like this) (Affleck, Tennen, Urrows, & Higgins, 1992). Coefficient alpha was .86 for the negative mood scale at the preoperative assessment in the current study.
Criterion variable
Participants were prescribed an adaptation of the accelerated ACL rehabilitation protocol that Shelbourne and his colleagues (DeCarlo, Sell, Shelbourne, & Klootwyk, 1994; DeCarlo, Shelbourne, McCarroll, & Rettig, 1992; Shelbourne, Klootwyk, & DeCarlo, 1992; Shelbourne & Nitz, 1990; Shelbourne & Wilckens, 1990) developed. Emphases of the protocol, which typically has home- and clinic-based components, include early attainment of range of motion, quadriceps strength, and normal gait (Decarlo et al., 1994; Shelbourne et al., 1992; Shelbourne & Nitz, 1990). During their clinic appointments (which occur approximately twice per week), patients are given instruction in various exercises designed to facilitate accomplishment of the protocol’s objectives. As patients progress through the protocol, the specific exercises and number of sets of exercises prescribed change. Early in rehabilitation, up to five sets of home exercises per day (at 10 to 15 minutes per set) are prescribed, whereas later in rehabilitation, a single, more involved daily set is prescribed. Although patients undertaking the accelerated protocol are strongly cautioned against engaging in “cutting” activities that could compromise their grafts, no similar warnings are given about doing more than their prescribed number of sets of exercises. Because the activities involved in the exercises are tailored to and considered safe for the patients’ stage of recovery, patients may even be encouraged to exceed the prescribed number of sets to hasten their recovery. Such encouragement is consistent with the origins of the accelerated protocol, which evolved from the observation that the patients who were least compliant with the activity modifications of the previously popular (conservative) rehabilitation protocol tended to achieve the best outcomes (Shelbourne & Wilckens, 1990).
Adherence to postoperative home rehabilitation exercises (HOMEXRAT) was assessed by dividing the number of sets of home exercises that participants reported that they completed each day (labeled HOMEX) by the number of sets of home exercises that they had been prescribed to perform on those days (labeled SPOSTO). For the number of sets of home exercises completed, participants were advised to include sets that they performed both with and without the videocassettes on which the home exercises were prescribed through audiovisual means.
Procedure
The procedures used in this study were approved by the Institutional Review Board at the host institution and were performed in accordance with the ethical standards specified in the 1964 Declaration of Helsinki. Prior to ACL reconstruction surgery, participants (and their parent/guardian if they were minors) signed an informed consent document and completed a battery of questionnaires that included items requesting demographic and injury-related information, the AIMS, the NEO-FFI, and the LOT-R. A research participation incentive of 15 dollars was provided for completion of the preoperative battery.
At their first physical therapy appointment after surgery, participants were given 42 questionnaire booklets that included the item assessing perceived stress, the items constituting the HOMEX variable, the NRS, and the abbreviated POMS-B. Participants were asked to fill out the questionnaires at the end of each day and return them the next day to the research team through the postal mail in one of the 42 business reply envelopes they were given. To strengthen the response rate, participants were informed that they would be paid one dollar for each questionnaire booklet returned and a bonus of seven dollars for each week in which they mailed in all seven daily questionnaire booklets. Participants returned 3,628 of the 3,822 (95%) booklets that were distributed. Participants were fully debriefed at the conclusion of their involvement in the study.
Analytical Scheme
The home exercise ratio variable HOMEXRAT is an indicator of how the number of sets of home exercises performed compares to the number that was prescribed by the physical therapist. A ratio of 1.00 would indicate that the person performed exactly the prescribed number of sets of home exercises; a ratio greater than 1.00 would indicate performing more than the prescribed number; and a ratio of less than 1.00 would indicate performing less than the prescribed number. Given the emphasis of the accelerated protocol on the importance of regaining function through completion of daily exercises, higher HOMEXRAT values (even those in excess of 1.00) were considered higher levels of adherence. A series of multilevel models was calculated to examine the relations of HOMEXRAT with personal variables and daily situational variables. In this series of multilevel models, each successive model contains all the variables of previous models, which controls for the effects of the variables that were entered into previous models.
An unconditional model was estimated to establish that HOMEXRAT varied over days and across people (Model 1). Model 2 included a predictor variable indicating how many sets of home exercises were prescribed on each day (SPOSTO). Model 3 included two variables reflecting the amount of time that had elapsed since surgery—DAYS and DAYSSQR. DAYS was the number of days that had elapsed since surgery and was mean-centered (based on each person’s mean number of days since surgery), DAYSSQR was the square of DAYS. These variables allowed for the investigation of both linear and quadratic trends. The fourth model (Model 4) included the personal variables of age, gender, athletic identity (AIMS), optimism (OPTIM), pessimism (PESS), and Neuroticism (NEURO). Age and gender were included in the model as control variables. The next model (Model 5) examined how HOMEXRAT was related to daily situational variables: measures of daily pain (PAINAVE), daily stress (STRESS), and negative mood (NEGMOOD). The sixth model (Model 6) added the interaction terms between the daily situational variables (SPOSTO, DAYS, DAYSSQR, PAIN, STRESS, and NEGMOOD) and the personal variables. All situational variables were person-mean centered and all personal variables were grand centered, except for gender, which was dummy coded as 0 or 1 (female and male).
All analyses were conducted with HLM software (HLM 5.5) (Raudenbush, Bryk, Cheong, & Congdon, 2001). Models were analyzed using restricted maximum likelihood estimation and all level 1 slopes were treated as random effects. The proportion reduction in within-person (i.e., reporting day) and between-person variance (Bryk & Raudenbush, 1992) was used as a measure of effect size for each set of variables added in sequential models. These models allowed investigation of the relationships between HOMEXRAT and (a) prescribed home exercises, (b) personal variables, (c) time since surgery variables, (d) daily situational variables, and (e) the interactions of these variables.
Results
Due to the way in which the post office handles business reply mail addressed to the institution where the research was conducted (i.e., only the top envelope in each batch of business reply envelopes delivered to the institution each day is date-stamped), it was not possible to determine precisely when participants returned their daily self-reports. Nevertheless, 90% of the 2,884 self-reports for which postal data were available were postmarked or received by the researchers within 5 days of the date on which they were supposed to have been completed.
A series of t-tests comparing the 91 participants who chose to be involved in the daily self-report portion of the study with the 17 participants who elected not to be so involved revealed no significant differences for the personal variables assessed preoperatively (i.e., age, athletic identity, neuroticism, optimism, and pessimism), all ps > .05. Mean values for HOMEXRAT, the personal variables, and the daily situational variables are presented in Table 1. These means are based on the 86 participants who had sufficient data for the multilevel analysis. For daily variables, these are grand mean values averaged across days and participants.
Table 1.
Means and Standard Deviations of Measured Variables
| Variable | M | SD |
|---|---|---|
| Age | 29.56 | 9.95 |
| Athletic identity (AIMS) | 30.07 | 9.73 |
| Optimism (OPTIM) | 11.08 | 2.00 |
| Pessimism (PESS) | 7.52 | 2.33 |
| Neuroticism (NEURO) | 16.83 | 6.30 |
| Number of sets of home exercises prescribed (SPOSTO) | 2.38 | 1.60 |
| Daily negative mood (NEGMOOD) | 3.69 | 4.56 |
| Daily average pain (PAIN) | 2.11 | 2.11 |
| Daily stress (STRESS) | 2.38 | 1.25 |
| Ratio of adherence (HOMEXRAT) | 1.43 | 1.44 |
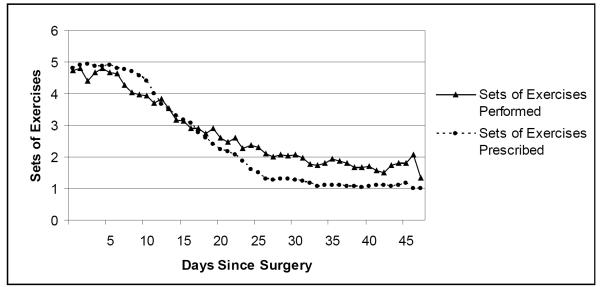
Results from Model 1 indicated that HOMEXRAT varied across both people and time since surgery. The intraclass correlation (Raudenbush et al., 2001) indicates that 43% of the variability in HOMEXRAT was accounted for by differences between people [τ/(τ + σ2), 0.89/(0.89+1.19) = 0.43] and 57% of the variability was due to differences in reporting day. Model 2 examined the relationship between HOMEXRAT and the prescribed number of sets of home exercises (SPOSTO). The results indicated a significant negative relationship that accounted for 44% of the reporting-day variability in HOMEXRAT [(σ2Model 1 − σ2Model 2)/ σ2Model 1, (1.19 − 0.67)/1.19 = 0.44], suggesting that when more sets of exercises are prescribed, patients perform fewer than the prescription. This relationship can be seen in Figure 1, which displays the number of sets of home exercises prescribed and the number completed across days since surgery. When greater numbers of sets of exercise are prescribed (the left side of the figure), the number performed is less than the prescription. When fewer sets of exercises are prescribed (right side of figure), more sets of exercises are performed than are prescribed.
Figure 1.
Sets of exercises prescribed and sets of exercises completed following surgery.
Adding the time variables to create Model 3 accounted for an additional 13% of the reporting-day variability in HOMEXRAT [(σ2Model 2 − σ2Model 3)/σ2Model 1, (0.67 − 0.52)/1.19 = 0.13]. The analysis revealed a relationship with a significant negative linear component (DAYS) and a significant positive quadratic component (DAYSSQR) between HOMEXRAT and days since surgery. This trend can be interpreted by examining Figure 1. Early after surgery (up to about 12 days), participants did fewer sets than prescribed. After nearly one week of doing approximately the prescribed number of sets of exercises, they tended to do more sets than prescribed for the remainder of the assessment period.
Model 4 examined the relationship between personal variables and HOMEXRAT, and the results indicated that none of the personal variables was significantly related to HOMEXRAT. Model 5 examined the relations between HOMEXRAT and daily stress (STRESS), average pain (PAIN), and negative mood (NEGMOOD). These variables accounted for 2.5% of the variability in HOMEXRAT across days [(σ2Model 4 − σ2Model 5)/ σ2Model 1, (0.52 − 0.49)/1.19 = 0.025]. Daily stress and negative mood were both negatively related to HOMEXRAT, indicating that participants’ adherence to their prescribed number of home exercises was lower than usual on stressful days and on days with greater than usual negative mood.
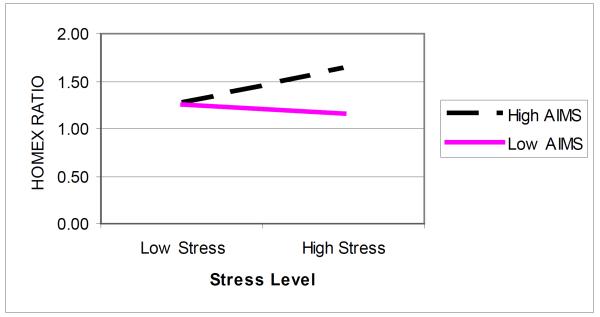
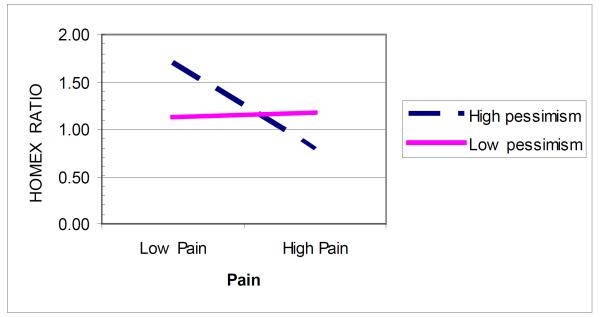
Model 6 examined the interactions between the person variables and the prescribed number of exercises (SPOSTO), time since surgery variables (DAYS and DAYSSQR), and the daily variables (PAIN, STRESS, and NEGMOOD) when predicting HOMEXRAT. There were two significant interactions, depicted in Figures 2 and 3. The interaction between AIMS and STRESS indicated that there was little difference in adherence to prescribed exercises between high AIMS and low AIMS participants on days with low stress, but that on high stress days, high AIMS participants tended to do a larger portion of their prescribed exercises than did low AIMS participants. The PESS and PAIN interaction indicates that whereas less pessimistic participants reported maintaining their adherence with prescribed exercises regardless of their pain level, more pessimistic participants reported performing a smaller proportion of their prescribed exercises on higher pain days.
Figure 2.
Interaction between athletic identity and stress in predicting HOMEXRAT (home exercise ratio).
Figure 3.
Interaction between pessimism and pain in predicting HOMEXRAT (home exercise ratio).
Discussion
The current study is the first of which we are aware to examine adherence to a postoperative ACL rehabilitation program on a daily basis. Adopting a daily process approach afforded a glimpse at day-to-day changes in completion of home rehabilitation exercises and at factors associated with such changes. From a purely descriptive standpoint, it is striking how closely the number of sets of home rehabilitation exercises participants reported having completed approximated the number that was prescribed over the course of the study. At a minimum, the data displayed in Figure 1 suggest that participants understood the numerical aspect of their home exercise prescription at the set level, a noteworthy finding in light of previous research showing that patients undergoing rehabilitation of sport injuries do not consistently demonstrate understanding of the requirements of their home programs (Webborn, Carbon, & Miller, 1997). The correspondence between completed sets of exercises reported and sets of exercises prescribed notwithstanding, there was substantial variability in HOMEXRAT, both across and within participants, over the 42-day assessment period. The median for HOMEXRAT was 1.02 (indicating a central tendency of full adherence rather than overadherence), with values ranging from 0.00 to 5.37.
Based on contemporary models of psychological response to sport injury (Wiese-Bjornstal et al., 1998), it was predicted that selected personal and situational variables correlated with adherence to medical regimens in previous research would be associated with adherence to home rehabilitation exercise completion following ACL surgery. None of the personal factors assessed was directly related to home exercise completion. Significant associations with home exercise completion were found for several situational factors, however, reflecting the disproportionate representation of situational variables relative to personal variables among predictors of adherence to sport injury rehabilitation programs in general (Brewer & Cornelius, 2003). Consistent with the notion that coping with stress and negative mood occupies self-control resources that could otherwise be devoted to treatment adherence (Muraven & Baumeister, 2000) and with previous prospective research documenting an inverse relationship between mood disturbance and sport injury rehabilitation adherence (Alzate Saez de Heredia, 2004; Daly et al., 1995), participants reported completing a lower percentage of their home exercises on days when they reported experiencing elevated levels of stress and negative mood. The negative association between pain and home exercise completion mirrors that for maintenance of aerobic exercise among women with fibromyalgia (Dobkin et al., 2005). The number of days since surgery was also a situational factor associated with percentage of home exercises completed, but was confounded with another situational factor—the number of sets of home rehabilitation exercises prescribed, which diminished over the course of the observation period. It is likely that the rise in the number of sets of home exercises competed relative to the number of sets prescribed is more attributable to the decreasing number of sets in the home exercise prescription than to the passage of time, although it is certainly possible that participants approached their rehabilitation with greater enthusiasm as their pain decreased and evidence of their recovery progress became more apparent.
Although personal factors were not directly related to adherence to the home rehabilitation exercise program, several cross-level interactions between personal factors and situational factors were obtained. Daily stress interacted with athletic identity such that participants high in athletic identity were more likely than those low in athletic identity to report completing their home exercises on days when stress was reported as high and equally likely to report completing their home exercises on days when stress was reported as low. One interpretation of this finding is that individuals for whom being an athlete is a central part of their self-identity tend not to allow stress to deter them from doing their home rehabilitation exercises. Similarly, daily pain interacted with pessimism such that participants high in pessimism were less likely than participants low in pessimism to report completing their prescribed home exercises on days when they reported experiencing elevated pain. For individuals high in pessimism, elevations in pain may trigger catastrophizing cognitions (Sullivan, Tripp, Rodgers, & Stanish, 2000) that impede their ability to perform their home exercises, a possibility that should be examined in future research. When coupled with the lack of a direct association between optimism and home exercise completion, the absence of significant cross-level interactions between optimism and pain, negative mood, and stress suggests that optimism may not play an important role in adherence to home exercises after ACL surgery.
Several limitations of the current study should be taken into account when considering the results. First, the adherence data were based on self-report, which is susceptible to the effects of bias, distortion, and forgetting. We attempted to reduce error due to memory loss by instructing participants to complete and return their self-reports on a daily basis. Nevertheless, given a tendency of participants to overreport completion of their home exercises with the videotapes (Brewer et al., 2004), the current findings for adherence are best viewed cautiously as an overestimate of what was actually done. Even so, in light of the general trend of participants to report completing a high percentage of their home exercise protocol over the course of the study (see Figure 1) and the documented correspondence between self-report and objective measures of home exercise completion in ACL rehabilitation (Brewer et al., 2004), it is reasonable to infer that participants did a substantial portion of their prescribed home rehabilitation exercises. Although completing daily self-reports may have served as a self-monitoring intervention (Christensen, 2004) that boosted the completion of home exercises, several diary studies (Cruise, Broderick, Porter, Kaell, & Stone, 1996; Hufford, Shields, Shiffman, Paty, & Balabanis, 2002; Aaron, Turner, Mancl, Brister, & Sawchuk, 2005) suggest that reactivity to the repeated data collection method used in the current investigation does not affect the monitored behavior.
Second, although participants were instructed to complete and return their self-reports on a daily basis, it was not possible to confirm that they completed their self-reports on the dates indicated in their questionnaire booklets. Participants typically sent in their self-reports one at a time, but some participants noted that they mailed multiple self-reports on the same day (or brought them to research staff at their physical therapy appointments) due to factors such as inclement weather, postoperative restrictions in mobility, and no weekend postal service. The potential for hoarding of diary responses in paper diary studies has been documented (Gable, Reis, & Elliot, 2000; Stone, Shiffman, Schwartz, Broderick, & Hufford, 2002) , which leads us to urge investigators who wish to use paper diaries to employ readily available and inexpensive electronic time stamps as part of their diary methods (Fuligni, Telzer, Bower, Cole, Kiang, & Irwin, 2009; Tennen, Affleck, Coyne, Larsen, & DeLongis, 2006).
Third, assessment of home exercise completion was restricted to the early stages of rehabilitation. Adherence to the home exercise prescription and the factors related to it may change as the rehabilitation program progresses and further time elapses. Finally, the home exercise regimen examined in the current study was an adaptation of the accelerated ACL rehabilitation protocol (Decarlo et al., 1994; Shelbourne et al., 1992; Shelbourne & Nitz, 1990). Predictors of home exercise completion may differ for a more conservative rehabilitation program than that implemented in this investigation.
The correlational nature of the present study does not allow us to draw causal inferences. The inverse relations of stress and negative mood with home exercise completion are suggestive, but it is possible that failing to complete one’s home rehabilitation exercises increases stress and negative mood. Nevertheless, given the documented utility of psychological interventions in enhancing adherence to sport injury rehabilitation programs (Evans & Hardy, 2002; Penpraze & Mutrie, 1999), interventions aimed at reducing stress and negative mood could have a beneficial effect on postoperative completion of prescribed home exercises in ACL rehabilitation. Multimodal approaches featuring techniques such as guided imagery, relaxation training, goal setting, and cognitive control have been found useful in improving sport injury rehabilitation outcomes (Cupal & Brewer, 2001; Johnson, 2000; Ross & Berger, 1996), an effect that may be, at least in part, mediated by increased adherence to the rehabilitation protocol. Future experimental investigations should examine the potential of psychological interventions to enhance completion of home rehabilitation exercises and, ultimately, clinical outcomes following postoperative ACL rehabilitation.
Overall, the findings highlight the potential utility of adopting an approach in which the contributions of personal factors, daily variations in situational factors, and their interactions (Christensen, 2004) are considered in examining adherence to acute rehabilitative interventions with a home activity component. Further inquiry is needed to assess the extent to which the current approach and the specific relationships observed therein generalize to other orthopedic and nonorthopedic conditions. In future research, inclusion of theoretically-meaningful predictor variables not examined in the current study (e.g., attitudes toward adherence, perceived social pressures, readiness, self-efficacy) merits consideration.
Table 2.
Results of Models for Predicting HOMEXRAT
| Model | Variable | Coefficient | t | Between- person variance (τ) |
Within-person variance (σ2) |
|---|---|---|---|---|---|
| Model 1 | 0.89 | 1.19 | |||
| HOMEXRAT | 1.411 | 13.52*** | |||
|
| |||||
| Model 2 | 0.91 | 0.67 | |||
| SPOSTO | −0.251 | −5.74*** | |||
|
| |||||
| Model 3 | 0.92 | 0.52 | |||
| DAYS | −0.033 | −6.12*** | |||
| DAYSSQR | 0.001 | 2.85** | |||
|
| |||||
| Model 4 | 0.96 | 0.52 | |||
| AIMS | −0.0003 | −0.06 | |||
| PESS | −0.032 | −1.17 | |||
| OPTIM | 0.030 | 0.98 | |||
| NEURO | −0.014 | −1.55 | |||
|
| |||||
| Model 5 | 0.96 | 0.49 | |||
| PAIN | −0.023 | −1.19 | |||
| STRESS | −0.049 | −2.45* | |||
| NEGMOOD | −0.011 | −2.03* | |||
|
| |||||
| Model 6 a | 0.91 | 0.49 | |||
| PESS × PAIN | −0.020 | −2.09* | |||
| AIMS × STRESS | 0.005 | 2.18* | |||
< .05.
p < .01.
p < .001
Each model contains all variables of preceding model.
Note. HOMEXRAT = home exercise ratio; SPOSTO = number of sets of home exercises that participants had been prescribed to perform; DAYS = number of days elapsed since surgery; DAYSSQR = DAYS squared; AIMS = athletic identity; PESS = pessimism; OPTIM = optimism; NEURO = neuroticism; PAIN = pain; STRESS = stress; NEGMOOD = negative mood.
Acknowledgments
This research was supported in part by grant R29 AR44484 from the National Institute of Arthritis and Musculoskeletal and Skin Diseases. Its contents are solely the responsibility of the authors and do not represent the official views of the National Institute of Arthritis and Musculoskeletal and Skin Diseases. We gratefully acknowledge the cooperation of Joseph Sklar, M.D., Mark Pohlman, M.D., and John Corsetti, M.D. in conducting this research and thank Josh Avondoglio, Lisa Benjamin, Jeff Benoit, Kathy Bernardini, Jim Biron, Ruth Brennan, John Brickner, Matt Buman, Judy Catalano, Tarra Cemborski, Kim Cochrane, Rosa Correa, Bob Crawford, Candi Daniele, Amie Dillman, Joann Golden, Reubin Gonzalez, Bryan Gross, Stephanie Habif, Whitney Hartmann, Jay Hatten, Carter Hunt, Jean Hutchinson, Angie Jensen, Aaron Kopish, Dawn Kresge, Ellie Laino, Amy Lowery, Kevin McAllister, Thomas Melvin, Alexa Mignano, Joe Monserrat, Liz Montemagni, Jonna Mullane, Rob Olenchak, Jens Omli, Scott Quarforth, Alice Robitaille, Raylene Ross, Carrie Scherzer, Josie Scibelli, Wendy Sewack, Ben Shachar, Sumiyo Shiina, and Marie Trombley for their assistance in data collection.
References
- Aaron LA, Turner JA, Mancl L, Brister H, Sawchuk CN. Electronic diary assessment of pain-related variables: is reactivity a problem? Journal of Pain. 2005;6:107–115. doi: 10.1016/j.jpain.2004.11.003. doi:10.1016/j.jpain.2004.11.003. [DOI] [PubMed] [Google Scholar]
- Affleck G, Tennen H, Pfeiffer C, Fifield J. Appraisals of control and predictability in adapting to a chronic disease. Journal of Personality and Social Psychology. 1987;53:273–279. doi: 10.1037//0022-3514.53.2.273. doi:10.1037/0022-3514.53.2.273. [DOI] [PubMed] [Google Scholar]
- Affleck G, Tennen H, Urrows S, Higgins P. Neuroticism and the pain-mood relation in rheumatoid arthritis: Insights from a prospective daily study. Journal of Consulting and Clinical Psychology. 1992;60:119–126. doi: 10.1037//0022-006x.60.1.119. doi:10.1037/0022-006X.60.1.119. [DOI] [PubMed] [Google Scholar]
- Affleck G, Zautra A, Tennen H, Armeli S. Multilevel daily process designs for consulting and clinical psychology: A preface for the perplexed. Journal of Consulting and Clinical Psychology. 1999;67:746–754. doi: 10.1037//0022-006x.67.5.746. doi:10.1037/0022-006X.67.5.746. [DOI] [PubMed] [Google Scholar]
- Alzate Saez de Heredia R, Ramirez A, Lazaro I. The effect of psychological response on recovery of sport injury. Research in Sports Medicine. 2004;12:15–31. doi: 10.1080/15438620490280567. [Google Scholar]
- Anderson CB. Athletic identity and its relation to exercise behavior: Scale development and initial validation. Journal of Sport and Exercise Psychology. 2004;26:39–56. [Google Scholar]
- Armeli S, Conner TS, Cullum J, Tennen H. A longitudinal analysis of drinking motives moderating the negative affect-drinking association among college students. Psychology of Addictive Behaviors. 2010;24:38–47. doi: 10.1037/a0017530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beard DJ, Dodd CAF. Home or supervised rehabilitation following anterior cruciate ligament reconstruction: A randomized controlled trial. Journal of Orthopaedic & Sports Physical Therapy. 1998;27:134–143. doi: 10.2519/jospt.1998.27.2.134. [DOI] [PubMed] [Google Scholar]
- Blair DF, Wills RP. Rapid rehabilitation following anterior cruciate ligament reconstruction. Athletic Training. 1991;26:32–43. [Google Scholar]
- Booth-Kewley S, Vickers RS., Jr. Associations between major domains of personality and health behavior. Journal of Personality Assessment. 1994;62:281–298. doi: 10.1111/j.1467-6494.1994.tb00298.x. doi:10.1111/1467-6494.ep9411045399. [DOI] [PubMed] [Google Scholar]
- Brewer BW, Cornelius AE. Norms and factorial invariance of the Athletic Identity Measurement Scale. Academic Athletic Journal. 2001;16:103–113. [Google Scholar]
- Brewer BW, Cornelius AE. Psychological factors in sports injury rehabilitation. In: Frontera WR, editor. Rehabilitation of sports injuries: Scientific basis. Blackwell Science; Malden, MA: 2003. pp. 160–183. [Google Scholar]
- Brewer BW, Cornelius AE, Van Raalte JL, Brickner JC, Sklar JH, Corsetti JR. Rehabilitation adherence and anterior cruciate ligament outcome. Psychology, Health & Medicine. 2004;9:163–175. doi: 10.1080/13548500410001670690. [Google Scholar]
- Brewer BW, Van Raalte JL, Linder DE. Athletic identity: Hercules’ muscles or Achilles heel? International Journal of Sport Psychology. 1993;24:237–254. [Google Scholar]
- Brewer BW, Van Raalte JL, Cornelius AE, Petitpas AJ, Sklar JH, Pohlman MH. Psychological factors, rehabilitation adherence, and rehabilitation outcome following anterior cruciate ligament reconstruction. Rehabilitation Psychology. 2000;45:20–37. doi: 10.1037/0090-5550.45.1.20. [Google Scholar]
- Bryk AS, Raudenbush SW. Hierarchical linear models: Applications and data analysis methods. Sage; Newbury Park: 1992. [Google Scholar]
- Carver CS, Scheier MF. On the self-regulation of behavior. Cambridge University Press; New York: 1998. [Google Scholar]
- Christensen AJ. Patient adherence to medical treatment regimens: Bridging the gap between behavioral science and biomedicine. Yale University Press; New Haven: 2004. [Google Scholar]
- Conner T, Tennen H, Zautra A, Affleck G, Armeli S, Fifield J. Coping with rheumatoid arthritis pain in daily life: Within-person analyses reveal hidden vulnerability for the formerly depressed. Pain. 2006;126:198–209. doi: 10.1016/j.pain.2006.06.033. [DOI] [PubMed] [Google Scholar]
- Costa PT, Jr., McRae RR. NEO Five-Factor Inventory: Form S. Psychological Assessment Resources; Odessa, FL: 1991. [Google Scholar]
- Costa PT, Jr., McRae RR. NEO PI-R professional manual. Psychological Assessment Resources; Odessa, FL: 1992. [Google Scholar]
- Cruise CE, Broderick J, Porter L, Kaell A, Stone AA. Reactive effects of diary assessment in chronic pain patients. Journal of Pain. 1996;67:253–258. doi: 10.1016/0304-3959(96)03125-9. doi:10.1016/0304-3959(96)03125-9. [DOI] [PubMed] [Google Scholar]
- Cupal DD, Brewer BW. Effects of relaxation and guided imagery on knee strength, reinjury anxiety, and pain following anterior cruciate ligament reconstruction. Rehabilitation Psychology. 2001;46:28–43. doi:10.1037/0090-5550.46.1.28. [Google Scholar]
- Daly JM, Brewer BW, Van Raalte JL, Petitpas AJ, Sklar JH. Cognitive appraisal, emotional adjustment, and adherence to rehabilitation following knee surgery. Journal of Sport Rehabilitation. 1995;4:23–30. [Google Scholar]
- DeCarlo MS, Sell DE. The effects of number and frequency of physical therapy treatments on selected outcomes of treatment in patients with anterior cruciate ligament reconstruction. Journal of Orthopaedic & Sports Physical Therapy. 1997;26:332–339. doi: 10.2519/jospt.1997.26.6.332. [DOI] [PubMed] [Google Scholar]
- DeCarlo MS, Sell DE, Shelbourne KD, Klootwyk TE. Current concepts on accelerated ACL rehabilitation. Journal of Sport Rehabilitation. 1994;3:304–318. [Google Scholar]
- DeCarlo MS, Shelbourne KD, McCarroll JR, Rettig AC. Traditional versus accelerated rehabilitation following ACL reconstruction: A one-year follow-up. Journal of Orthopaedic & Sports Physical Therapy. 1992;15:309–316. doi: 10.2519/jospt.1992.15.6.309. [DOI] [PubMed] [Google Scholar]
- Derscheid GL, Feiring DC. A statistical analysis to characterize treatment adherence of the 18 most common diagnoses seen at a sports medicine clinic. Journal of Orthopaedic & Sports Physical Therapy. 1987;9:40–46. doi: 10.2519/jospt.1987.9.1.40. [DOI] [PubMed] [Google Scholar]
- Dobkin PL, Abrahamowicz M, Fitzcharles MA, Dritsa M, da Costa D. Maintenance of exercise in women with fibromyalgia. Arthritis Rheum. 2005;53:724–731. doi: 10.1002/art.21470. doi:10.1002/art.21470. [DOI] [PubMed] [Google Scholar]
- Evans L, Hardy L. Injury rehabilitation: A goal-setting intervention study. Research Quarterly for Exercise & Sport. 2002;73:310–319. doi: 10.1080/02701367.2002.10609025. doi:10.1177/1466424008094802. [DOI] [PubMed] [Google Scholar]
- Farrell SP, Hains AA, Davies WH, Smith P, Parton E. The impact of cognitive distortions, stress, and adherence on metabolic control in youths with type 1 diabetes. Journal of Adolescent Health. 2004;34:461–467. doi: 10.1016/S1054-139X(03)00215-5. doi:10.1016/S1054-139X(03)00215-5. [DOI] [PubMed] [Google Scholar]
- Fischer DA, Tewes DP, Boyd JL, Smith JP, Quick DC. Home based rehabilitation for anterior cruciate ligament reconstruction. Clinical Orthopaedics & Related Research. 1998;347:194–199. [PubMed] [Google Scholar]
- Friedman LC, Webb JA, Bruce S, Weinberg AD, Cooper HP. Skin cancer prevention and early detection intentions and behavior. American Journal of Preventive Medicine. 1995;11:59–65. [PubMed] [Google Scholar]
- Fuligni AJ, Telzer EH, Bower J, Cole SW, Kiang L, Irwin MR. A preliminary study of daily interpersonal stress and c-reactive protein levels among adolescents from Latin American and European Backgrounds. Psychosomatic Medicine. 2009;71:329–333. doi: 10.1097/PSY.0b013e3181921b1f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gable SL, Reis HT, Elliot AJ. Behavioral activation and inhibition in everyday life. Journal of Personality and Social Psychology. 2000;78:1135–1149. doi: 10.1037//0022-3514.78.6.1135. doi:10.1037/0022-3514.78.6.1135. [DOI] [PubMed] [Google Scholar]
- Grant JA, Mohtadi NGH. Two- to 4-year follow-up to a comparison of home versus physical therapy-supervised rehabilitation programs after anterior cruciate ligament reconstruction. American Journal of Sports Medicine. 2010;38:1389–1394. doi: 10.1177/0363546509359763. doi:10.1177/0363546509359763. [DOI] [PubMed] [Google Scholar]
- Grant JA, Mohtadi NG, Maitland ME, Zernicke RF. Comparison of home versus physical therapy-supervised rehabilitation programs after anterior cruciate ligament reconstruction: A randomized clinical trial. American Journal of Sports Medicine. 2005;33:1288–1297. doi: 10.1177/0363546504273051. doi:10.1177/0363546504273051. [DOI] [PubMed] [Google Scholar]
- Green AS, Rafaeli E, Bolger N, Shrout PE, Reis HT. Paper or plastic? Data equivalence in paper and electronic diaries. Psychological Methods. 2006;11:87–105. doi: 10.1037/1082-989X.11.1.87. doi: 10.1037/1082-989X.11.1.87. [DOI] [PubMed] [Google Scholar]
- Gunthert KC, Conner TS, Armeli S, Tennen H, Covault J, Kranzler HR. The serotonin transporter gene polymorphism (5-HTTLPR) and anxiety reactivity in daily life: A daily process approach to gene-environment interaction. Psychosomatic Medicine. 2007;69:762–768. doi: 10.1097/PSY.0b013e318157ad42. [DOI] [PubMed] [Google Scholar]
- Hufford MR, Shields AL, Shiffman S, Paty J, Balabanis M. Reactivity to ecological momentary assessment: An example using undergraduate problem drinkers. Psychology of Addictive Behaviors. 2002;16:205–211. [PubMed] [Google Scholar]
- Jensen MP, Karoly P. Self-report scales and procedures for assessing pain in adults. In: Turk DC, Melzack R, editors. Handbook of pain assessment. 2nd ed Guilford Press; New York, NY: 2001. pp. 15–34. [Google Scholar]
- Johnson U. Short-term psychological intervention: A study of long-term-injured competitive athletes. Journal of Sport Rehabilitation. 2000;9:207–218. [Google Scholar]
- Kvist J. Rehabilitation following anterior cruciate ligament injury: Current recommendations for sports participation. Sports Medicine. 2004;34:269–290. doi: 10.2165/00007256-200434040-00006. [DOI] [PubMed] [Google Scholar]
- Larney LC. Do depression, anxiety, hostility, coping style and dispositional outlook predict adherence to prescribed rehabilitation program and recovery outcomes for cardiac rehabilitation outpatients? Dissertation Abstract International. 2002;62(7-B):3382. [Google Scholar]
- Lazarus RS, Folkman S. Stress, appraisal and coping. Springer; New York: 1984. [Google Scholar]
- Levy AR, Polman RCJ, Nicholls AR, Marchant DC. Sport injury rehabilitation adherence: Perspectives of recreational athletes. International Journal of Sport & Exercise Psychology. 2009;7:212–229. doi: 10.1080/1612197X.2009.9671901. [Google Scholar]
- Lorr M, McNair D. Profile of Mood States—B. Educational and Industrial Testing Service; San Diego: 1982. [Google Scholar]
- Milam JE, Richardson JL, Marks G, Kemper CA, McCutchan AJ. The roles of dispositional optimism and pessimism in HIV disease progression. Psychology & Health. 2004;19:167–181. doi:10.1080/08870440310001652696. [Google Scholar]
- Muraven M, Baumeister RF. Self-regulation and depletion of limited resources: Does self-control resemble a muscle? Psychological Bulletin. 2000;126:247–259. doi: 10.1037/0033-2909.126.2.247. doi: I0.I037//0033-2909.126.2.247. [DOI] [PubMed] [Google Scholar]
- Papaioannou A, Kennedy CC, Dolovich L, Lau E, Adachi JD. Patient adherence to osteoporosis medications: Problems, consequences and management strategies. Drugs & Aging. 2007;24:37–55. doi: 10.2165/00002512-200724010-00003. [DOI] [PubMed] [Google Scholar]
- Penpraze P, Mutrie N. Effectiveness of goal setting in an injury rehabilitation programme for increasing patient understanding and compliance [Abstract] British Journal of Sports Medicine. 1999;33:60. doi: 10.1002/9780470757178.ch8. [Google Scholar]
- Pizzari T, Taylor NF, McBurney H, Feller JA. Adherence to rehabilitation after anterior cruciate ligament reconstructive surgery: Implications for outcome. Journal of Sport Rehabilitation. 2005;14:201–214. [Google Scholar]
- Potgieter JR, Venter RF. Relationship between adherence to exercise and scores on extraversion and neuroticism. Perceptual & Motor Skills. 1995;81:520–522. doi: 10.1177/003151259508100233. [DOI] [PubMed] [Google Scholar]
- Raudenbush S, Bryk A, Cheong YF, Congdon R. HLM 5 hierarchical linear and nonlinear modeling. Scientific Software International; Lincolnwood, IL: 2001. [Google Scholar]
- Robinson MD, Ode S, Wilkowski BM, Amodio DM. Neurotic contentment: A self-regulation view of neuroticism-linked distress. Emotion. 2007;7:579–591. doi: 10.1037/1528-3542.7.3.579. doi: 10.1037/1528-3542.7.3.579. [DOI] [PubMed] [Google Scholar]
- Roche DN. Unpublished doctoral dissertation. State University of New York at Buffalo; 2004. Athletic injury: Understanding the impact of athletic identity and emotional responses on rehabilitation adherence in Division I athletes. [Google Scholar]
- Ross MJ, Berger RS. Effects of stress inoculation on athletes’ postsurgical pain and rehabilitation after orthopedic injury. Journal of Consultation and Clinical Psychology. 1996;64:406–410. doi: 10.1037//0022-006x.64.2.406. doi: 10.1037/0022-006X.64.2.406. [DOI] [PubMed] [Google Scholar]
- Scheier MF, Carver CS. Effects of optimism on psychological and physical well-being: theoretical overview and empirical update. Cognitive Therapy and Research. 1992;16:201–228. doi: 10.1007/BF01173489. [Google Scholar]
- Scheier MF, Carver CS, Bridges MW. Distinguishing optimism from neuroticism (and trait anxiety, self-mastery, and self-esteem): A reevaluation of the Life Orientation Test. Journal of Personality and Social Psychology. 1994;67:1063–1078. doi: 10.1037//0022-3514.67.6.1063. doi: 10.1037/0022-3514.67.6.1063. [DOI] [PubMed] [Google Scholar]
- Schenck RC, Jr., Blaschak MJ, Lance ED, Turturro T, Holmes C. A prospective outcome study of rehabilitation programs and anterior cruciate ligament reconstruction. Arthroscopy. 1997;13:285–290. doi: 10.1016/s0749-8063(97)90022-0. [DOI] [PubMed] [Google Scholar]
- Shelbourne KD, Klootwyk TE, DeCarlo MS. Update on accelerated rehabilitation after anterior cruciate ligament reconstruction. Journal of Orthopaedic Sports Physical Therapy. 1992;15:303–308. doi: 10.2519/jospt.1992.15.6.303. [DOI] [PubMed] [Google Scholar]
- Shelbourne KD, Nitz P. Accelerated rehabilitation after anterior cruciate ligament reconstruction. American Journal of Sports Medicine. 1990;18:292–299. doi: 10.1177/036354659001800313. doi: 10.1177/036354659001800313. [DOI] [PubMed] [Google Scholar]
- Shelbourne KD, Wilckens JH. Current concepts in anterior cruciate ligament rehabilitation. Orthopaedic Review. 1990;19:957–964. [PubMed] [Google Scholar]
- Stetson BA, Rahn JM, Dubbert PM, Wilner BI, Mercury MG. Prospective evaluation of the effects of stress on exercise adherence in community-residing women. Health Psychology. 1997;16:515–520. doi: 10.1037//0278-6133.16.6.515. doi: 10.1037/0278-6133.16.6.515. [DOI] [PubMed] [Google Scholar]
- Stone AA, Shiffman S, Schwartz JE, Broderick JE, Hufford MR. Patient non-compliance with paper diaries. British Medical Journal. 2002;324:1193–1194. doi: 10.1136/bmj.324.7347.1193. doi: 10.1136/bmj.324.7347.1193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sullivan MJ, Tripp DA, Rodgers WM, Stanish W. Catastrophizing and pain perception in sport participants. Journal of Applied Sport Psychology. 2000;12:151–167. doi: 10.1080/10413200008404220. [Google Scholar]
- Taylor AH, May S. Threat and coping appraisal as determinants of compliance to sports injury rehabilitation: An application of protection motivation theory. Journal of Sports Sciences. 1996;14:471–482. doi: 10.1080/02640419608727734. doi: 10.1080/02640419608727734. [DOI] [PubMed] [Google Scholar]
- Tennen H, Affleck G, Armeli S, Carney MA. A daily process approach to coping: Linking theory, research, and practice. American Psychologist. 2000;55:626–636. doi: 10.1037//0003-066x.55.6.626. doi: 10.1037/0003-066X.55.6.626. [DOI] [PubMed] [Google Scholar]
- Tennen H, Affleck GT, Coyne JC, Larsen RJ, DeLongis A. Paper and plastic in daily diary research: Comment on Green, Rafaeli, Bolger, Shrout, and Reis (2006) Psychological Methods. 2006;11:112–118. doi: 10.1037/1082-989X.11.1.112. doi: 10.1037/1082-989X.11.1.112. [DOI] [PubMed] [Google Scholar]
- Treacy SH, Barron OA, Brunet ME, Barrack R. Assessing the need for extensive supervised rehabilitation following arthroscopic ACL reconstruction. American Journal of Orthopedics. 1997;26:25–29. [PubMed] [Google Scholar]
- Webborn AD, Carbon RJ, Miller BP. Injury rehabilitation programs: “What are we talking about?”. Journal of Sport Rehabilitation. 1997;6:54–61. [Google Scholar]
- Wiese-Bjornstal DM, Smith AM, Shaffer SM, Morrey MA. An integrated model of response to sport injury: Psychological and sociological dimensions. Journal of Applied Sport Psychology. 1998;10:46–69. doi: 10.1080/10413209808406377. [Google Scholar]