Abstract
Background
The presence of nerve damage plays a key role in the development and prognosis of chronic pain states. Assessment of the presence and severity of a neuropathic pain component (NePC) is key in diagnosing chronic pain patients. Low back pain (LBP) and neck and shoulder pain (NSP) are highly prevalent and clinically important medical and societal problems in which a NePC is frequently present. The more severe the NePC, the worse the course of the pain, its prognosis and the results of treatment. Reliable and standardised diagnosis of the NePC remains difficult to achieve. Standardized and validated screening tools may help to reliably identify the NePC in individual chronic pain patients. The aim of this study is to validate the Dutch language versions of the PainDETECT Questionnaire (PDQ-Dlv) and the ‘Douleur Neuropathique 4 Questions’ (DN4-Dlv) for use in primary and specialist medical care settings to screen for a NePC in patients with chronic pain due to (1) LBP, (2) NSP or (3) known peripheral nerve damage (PND).
Methods/design
The study design is cross-sectional to assess the validity of the PDQ-Dlv and the DN4-Dlv with 2 weeks follow-up for test-retest reliability and 3 months follow-up for monitoring and prognosis. 438 patients with chronic pain due to (1) LBP, (2) NSP or (3) PND. will be included in this study. Based on the IASP definition of neuropathic pain, two physicians will independently assess whether the patient has a NEPC or not. This result will be compared with the outcome of the PDQ-Dlv & DN4-Dlv, the grading system for neuropathic pain, bed side examination and quantitative sensory testing. This study will further collect data regarding prevalence of NePC, general health status, mental health status, functioning, pain attribution and quality of life.
Discussion
The rationale for this study is to provide detailed information on the clinimetric quality of the PDQ-Dlv and DN4-Dlv in Dutch speaking countries. Our innovative multi-factorial approach should help achieve more reliable diagnosis and quantification of a NePC in patients with chronic pain.
Trial registration
The Netherlands National Trial Register (NTR3030).
Keywords: PainDETECT questionnaire, PDQ, DN4, Validation, Low back pain, Neck-shoulder pain, Peripheral nerve damage
Background
The International Association for the Study of Pain (IASP, 2011) defines Neuropathic Pain (NeP) as ‘pain caused by a lesion or disease of the somatosensory nervous system’ (http://www.iasp-pain.org/Education/Content.aspx?ItemNumber=1698#Neuropathicpain). This definition will be used in this study because of its diagnostic specificity, anatomic precision and the usefulness in clinical as well as research conditions [1]. NeP plays an important role in the development and prognosis of chronic pain states. A relevant example is patients with low back pain (LBP) and neck-shoulder pain (NSP), which are both highly prevalent and clinically important medical and societal problems: In this context, the more severe the NeP, the worse the pain course, the prognosis and the results of treatment [2-5].
The incidence of NeP in the Dutch general population is 0.81% or 130.000 new patients in the Netherlands per year. NeP is 63% more common in women than in men and peaks between 70 and 79 years of age [6]. LBP as well as NSP are among the top 10 health problems encountered in general practice. For men and women, respectively, the prevalence of LBP and/or NSP in the general practice is in the range of 55 – 86 and 24 - 113 per 1000 patients a year. In general practice, radiating pain from the low back or neck occurs in men and women in respectively 4 - 8 and 10 patients per 1000 patients [7]/(http://www.nationaalkompas.nl/gezondheid-en-ziekte/ziekten-en-aandoeningen/bewegingsstelsel-en-bindweefsel/nek-en-rugklachten/omvang/). The prevalence of chronic pain syndromes due to peripheral nerve damage (PND) is 3,3 per 1000 per year [8].
Strictly speaking, the diagnosis of neuropathic pain is a patho-anatomical diagnosis presuming knowledge regarding nerve injury which is difficult to obtain in the clinical situation. Thus in the clinical context it is better to speak of a neuropathic pain component (NePC), which is a clinical syndrome based on a typical set of clinical symptoms and signs. Clinically, a NePC is characterized by spontaneous pain and abnormal pain sensations [9]. NeP is typically described as a spontaneous ongoing burning or shooting pain with spontaneous sharp exacerbations and somatosensory abnormalities after a (non-) noxious stimulus [10].
As a rule, a NePC has a considerable impact on the quality of daily life [6]. Hence it is important for physicians in daily practice (specialist care as well as primay care) to diagnose the presence and severity of a NePC in individual patients. In clinical practice it is, however, often difficult to reliably diagnose a NePC in (sub)acute and chronic pain of the low back and neck shoulder region. The diagnosis of a NePC is at present primarily based on clinical examination by a physician including sensory examination. Quantitative sensory testing (QST) may provide extra information for selected clinical cases and in the research context [11,12].
Because a reliable diagnosis of the neuropathic pain component is often difficult to accomplish in routine practice [2], it would be helpful to have a screening tool to detect such a component for clinical triage and epidemiological purposes [12,13]. Apart from optimal sensitivity and specificity, such a screening tool should be easy to use in clinical practice, not only for the first visit but also during follow up. The availability of such a simple, validated, Dutch language screening tool should improve diagnosis and quantification of a NePC and hence lead to better therapy. At present, no specific (validated) instrument to determine the neuropathic component in LBP, NSP and PND is available in the Dutch language. The PainDETECT-Questionnaire (PDQ) [2] and the Douleur Neuropatique 4 Questions (DN4) [14] were originally developed and validated in Germany and France, respectively. Both are considered to be reliable screening tools with a high sensitivity, specificity and positive predictive value. Recently, the DN4 and the PDQ have been translated into a Dutch language version (Dlv) by Van Seventer et al [15] and Timmerman et al [16], respectively.
Validation of the Dutch versions of DN4-Dlv and PDQ-Dlv will improve the identification of a NePC in Dutch primary and specialist medical care, also facilitating remote follow up evaluation by telephone, internet or post for clinical and scientific purposes. We chose an innovative approach which should lead to a more reliable identification and quantification of a NePC in patients with chronic pain. This study will help define patient groups at risk for a NePC and will help to understand and assess the variability and burden of a NePC in individual patients.
The aim of this study is to establish the clinimetric quality, including 2-weeks test-retest reliability, of the PDQ-Dlv and the DN4-Dlv for use in primary care and specialist medical care settings in Dutch speaking countries for patients with chronic pain due to LBP, NSP or known peripheral nerve damage (PND). Follow-up for monitoring and prognosis properties of DN4-Dlv and PDQ-Dlv for a NePC will be done over a period of 3 months. Additional data will be collected regarding NEPC prevalence, general health status, mental health status, functioning, pain attribution and health related quality of life in patients with chronic pain.
Methods
The medical and ethical review board Committee on Research Involving Human Subjects region Arnhem-Nijmegen, Nijmegen, the Netherlands, has given approval to conduct this study, Dossier number: 2008/348; NL 25343.091.08; The Netherlands National Trial Register NTR3030.
Design
In this study a cross-sectional, observational, research design with 3-months follow up will be used to study the clinimetric quality of the DN4-Dlv and PDQ-Dlv (Figure 1).
Figure 1.
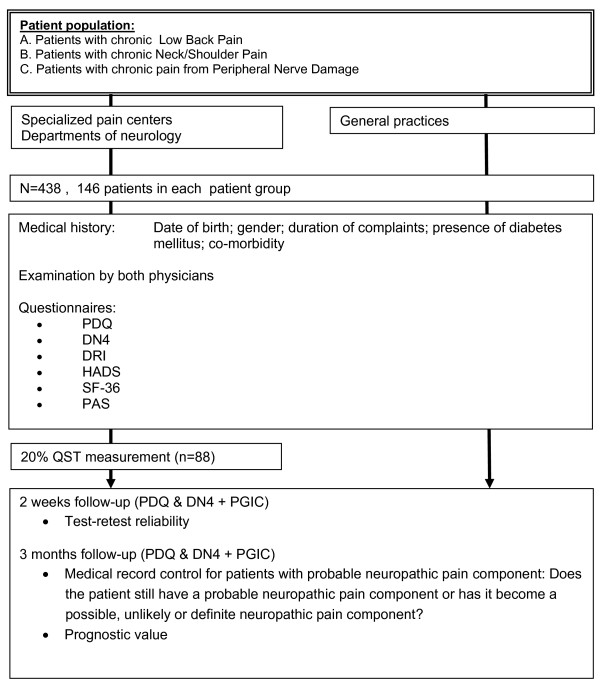
Flow-diagram of the study. PDQ: PainDETECT questionnaire; DN4: Douleur neuropatique 4 questions; DRI : Disability rating index; HADS: Hospital anxiety depression scale; RAND-36 : RAND 36-item health survey; PAS: Pain attribution scale; QST: Quantitative sensory testing; PGIC: Patients global impression of change.
Setting
Multicenter recruitment will be take place in academic pain centres, non-academic pain centres and non-academic departments of neurology. Patients will be seen by the two physicians during normal office hours, or when that is not possible during a special office hour for this study. Furthermore, patients willing to participate in this study from general practices will also be included in this study via a special office hour in the clinical trainings centre of Radboud university medical center (Radboudumc). Each patient will be seen by two physicians, independently of each other, working in the same institute. The medical background of the participating physicians is diverse (experienced pain specialists, pain specialist trainees, experienced neurologists and experienced general practitioners).
Participants
The patients will be recruited non-selectively and consecutively in the period from September 2009 till July 2013. Inclusion criteria: Male and female adult patients (>18 years of age) with chronic (>3 months) LBP or NSP radiating into respectively leg(s) or arm(s) or patients with chronic pain due to PND. Exclusion criteria: Patients diagnosed with malignancy, compression fractures, patients with painful syndromes of unknown origin or associated with diffuse pains (such as ankylosing spondylitis or fibromyalgia), severe mental illness, chronic alcoholism or substance abuse, inability to fill in the questionnaire adequately, or incapable of understanding Dutch. Subjects can leave the study at any time for any reason without any consequences. The investigator can decide to withdraw a subject from the study for urgent medical reasons. When an individual subject leaves the study all the information from the patient will be kept in the database, and possibly be used for data analysis or withdrawal analysis. Such patients will be replaced.
Measurements
At the first visit, each patient will be seen by two physicians who will question and examine the patients. They will then independently classify the patients’ pain as pain with or without a NePC, based in the IASP NeP criteria and supported by a standardized assessment form. Next, the patient will complete seven questionnaires (including the PDQ and the DN4). Twenty percent of the patients will additionally undergo QST measurement following the first visit. Two weeks and three months after the initial visit three follow-up questionnaires will be sent to the patient by mail.
Demographics
Date of birth, gender, weight (Kg), length (m), nationality, nationality of origin, pain medication, smoking (cigarettes a day), alcohol consumption (units per day) and education level will be assessed by use of a self completed questionnaire. Pain at this moment will be assessed by use of a numeric rating scale (0-10, NRS) Medical co-morbidity, duration of complaints (years/months), presence of diabetes mellitus (yes/no), presence of HIV (yes/no), presence of herpes (yes/no) and undergoing of chemotherapy (yes/no) are based on interview by the physician and noted by the physician on the standardized assessment form.
Pain classification
At each centre participating patients will be examined by two (rater A and B) independent and trained pain physicians, two experienced neurologists or two experienced general practitioners, working independently of each other and blinded to the diagnosis of the other physician. To achieve standardization of the history and clinical examination all participating physicians will be trained at the sites. Both physicians will classify the pain regarding the presence or absence of a NePC based on history and clinical examination. Level of certainty of the physicians regarding the pain component classification will be assessed by use of a Visual Analogue Scale (VAS, range 0-100). The findings are noted on the standardized assessment form by the physician. To monitor the quality of the clinical examination random quality checks, by expected/ unexpected visits, will be used.
Grading system
The grading system for neuropathic pain as proposed by Treede et al. [1] will be used as a secondary comparison with the outcome of both the PDQ-Dlv and DN4-Dlv and with the outcome of the original pain classification by the two physicians. This system provides a working hypothesis for the origin of patients’ pain. The criteria are graded on basis of history and testing in medical examination [1]: (1) Pain with a distinct neuroanatomically plausible distribution; (2) A history suggestive of a relevant lesion or disease affecting the peripheral or central somatosensory system; (3) Demonstration of the distinct neuroanatomically plausible distribution by at least one confirmatory test; (4) Demonstration of the relevant lesion or disease by at least one confirmatory test lesion or disease explaining NeP. When the criteria 1-4 are all fulfilled the pain will be graded as possessing a ‘definite NePC’. Criteria 1 and 2 and either 3 or 4 will be graded as ‘probable NePC’. Criteria 1 & 2 without criteria 3 or 4 will be graded as ‘possible NePC’. The pain is ‘unlikely to have a NePC’ when no criteria, or only criteria 1 or 2, are graded as present (Table 1). The answers (yes or no) to the four criteria are noted by the physician on the standardized assessment form. Three months after the first consultation by the two physicians the medical record of patients with ‘probable NePC’ according to the grading system will be controlled: i.e. does the patient still have probable NePC, or does he now have definite NePC?.
Table 1.
Outcome of the grading system [1]
|
Criteria 1:
|
Criteria 2:
|
Criteria 3:
|
Criteria 4:
|
Outcome of the grading system
|
|---|---|---|---|---|
| Pain with a distinct neuro-anatomically plausible distribution | History suggestive of a relevant lesion or disease affecting the peripheral or central somatosensory system | Demonstration of the distinct neuroanatomically plausible distribution by at least one confirmatory test | Demonstration of the relevant lesion or disease by at least one confirmatory test lesion or disease explaining NeP | |
|
- |
- |
- |
- |
Unlikely to be NeP
|
|
V |
- |
- |
- |
Unlikely to be NeP
|
|
- |
V |
- |
- |
Unlikely to be NeP
|
|
V |
V |
- |
- |
Possible NeP
|
|
V |
V |
V |
- |
Probable NeP
|
|
V |
V |
- |
V |
Probable NeP
|
| V | V | V | V | Definite NeP |
NeP: Neuropathic Pain; V: present; -: absent.
Bedside examination
Bed-side examination of the patient is performed by both physicians. The aim of this examination is to find possible abnormalities suggestive for a relevant lesion or disease which affects the peripheral or central somatosensory system [17]. The value of bed-side examination within the clinical examination is that it will give insight in the pathology and the localization of the lesion or disease which is causing the pain. Touch, pin prick, pressure, cold, heath, vibration and temporal summation were included in the examination to provide proof of a NePC [10,12,18]. This evaluation will be assessed in a standardized way. The location indicated by the patient as the one with maximum pain will be compared with the mirrored location on the contra lateral side. If the pain has a double sided character a location without pain as close as possible to the original mirror site will be tested for comparison. The outcome is noted by the physician on the standardized assessment form: a) Is there a sensation b) is the sensation unpleasant or c) is the sensation painful (all scored as Yes, No or Unclear). The response of the patient will be noted on the assessment form. The following tests will be performed in all patients: Mechanical static allodynia by blunt pressure with a finger at a force which normally doesn’t evoke pain; Dynamic mechanical allodynia by stroking the skin with a Soft Brush (SENSElabTM, Brush-05, Somedic AB, Hörby, Sweden), one movement of 1-2 centimeter and three movements of 1-2 centimeters (wind-up response); Mechanical pinprick allodynia by touch of the skin with a plastic safety pin and a Von Frey hair (TOUCH TESTR, 5.07, 10.0 g, North Coast Medical Inc., Gilroy, USA). Heat allodynia by using TipThermR (TipTherm, Brüggen, Germany) in a baby-bottle warmer (ISI mini Baby Bottle Warmer, Assen, the Netherlands) set at 45 degrees Celsius; Cold allodynia with an ice cube placed on the skin for 2 seconds and Vibration with a Tuning fork (128 Hz; Medipharchem, Wormerveer, the Netherlands) applied to joint, bone or soft tissue in the region of the pain.
Quantitative sensory testing
Over the last two decades, QST has been developed to complement traditional neurological bedside examination in the analysis of somatosensory aberrations [19,20]. In theory, greater precision in assessing the functionality of the somatosensory systems is the main advantage of QST over standard bedside examination. QST improves diagnostic procedures and can be helpful for treatment monitoring [11,21]. The protocol we chose is the Nijmegen Aalborg Screening QST Paradigm (NASQ Paradigm) [22]. This maps pain sensitivity at multiple sites by measuring the responses (i.e. painful sensations) evoked by mechanical and electrical non invasive stimuli and measures the patient’s capacity to modulate pain using the Conditioned Pain Modulation [23], previously termed Diffuse Noxious Inhibitory controls (DNIC) or Heterotopic Noxious Conditioning Stimulation (HNCS) [24]. In this study the QST is used to quantify alterations in sensory processing due to the NePC (sensory profiling) in a sub-sample of patients with LBP, NSP and PND (20% of the total population under study, n = 88, equally but randomly divided over all three pain syndromes). Instructions are standardized and will be read to the patient from an instruction sheet. Pressure Pain Thresholds (PPT) will be tested by use of an pressure algometer (Somedic sales AB, Hörby, Sweden). PPT will be measured on the left and right bodyside once at each location: Thenar (middle part), musculus trapezius pars median (middle part), musculus rectus femoral (15 cm above patella) and m. abductor hallucis (middle part). Electrical pain thresholds (EPT) will be tested by use of the QST-3 device (JNI Biomedical ApS, Klarup, Denmark) on the left and right body side. Measurement locations are the musculus trapezius pars median (middle part) and the musculus rectus femoris (20 cm above patella). Electrical pain thresholds (EPT) are assessed and expressed in milli-Ampère. Single pulse evoked pain measurement is performed by one pulse at 150% of the EPT and assessed on a VAS. Summation (i.e. Electric Wind-Up response (E-WUR)) is measured by a train of five pulses at 150% of the EPT and assessed on as VAS. Conditioned Pain Modulation (CPM) [23,25] will be assessed. Electrical Pain Tolerance Thresholds (EPTT) (test stimulation) are assessed and expressed in milli-Ampère on the m. Rectus femoris contralateral to the dominant hand. The noxious stimulus (conditioning stimulation) is to immerse the dominant hand until the wrist in a bucket filled with water and icecubes (‘Ice water bucket test’) [24] for ‘as long as possible, until the moment that the sensation becomes unbearable and you want to stop directly”. The pain will be recorded every 10 seconds on a NRS. The duration of the immersion (with a maximum of three minutes) will be recorded and the pain at the end of the immersion will be asked. Afterwards, again the EPTT and the PPT on the contra lateral m. rectus femoris are assessed.
Douleur neuropathique 4 questions (DN4)
The DN4 [14,15] (© Pfizer bv. Capelle a/d IJssel, the Netherlands) consists of 10 items in total, divided in two questions and two physical examination tests, and is developed to screen components of NeP resulting in a yes/no answer for the presence of NeP. Questions 1 & 2 are sensory descriptors and have to be filled in by the patient or assessed by the physician by interview; questions 3 & 4 are based on a sensory examination by the physician. Question 3 includes two items related to sensory deficits: ‘Is the pain located in an area where the physical examination may reveal one or more of the following characteristics? Touch hypoesthesia and/or pricking hypoesthesia. Question 4 includes 1 item related to evoked pain: ‘In the painful area, can the pain be caused or increased by brushing? Examination of sensitivity to touch (one movement) will be performed with the use of a soft brush (SENSElabTM, Brush-05, Somedic AB, Hörby, Sweden). The soft brush will also be used to evaluate tactile (i.e. dynamic mechanical) allodynia (wind-up, with three movements). Examination of sensitivity to touch and pricking will be performed with the use of a Von Frey hair (TOUCH TESTR, 5.07, 10.0 g, North Coast Medical Inc., Gilroy, USA). Pressure allodynia (i.e. static mechanical allodynia) is tested by blunt pressure with a finger at a pressure that does not provoke pain in a normally sensitive area [14]. The findings in the physical tests are noted by the physician on the standardized assessment form. The cut-off score for the diagnosis of NeP for the 10-item’ DN4 was determined on 4 times ‘yes’ out of 10 (score range 0-10). This score gave the highest percentage of correctly identified patients (86%), sensitivity (82,9%) and specificity (89,9%). The 7-item’ DN4-interview (score range 0-7) has a cut-off score of 3 times ’yes’ out of 7 which resulted in a percentage of correctly identified patients of 79, 5%, 78% sensitivity and 81,2% specificity [14].
PainDetect-Questionnaire (PDQ)
The PDQ (© Pfizer Pharma GmbH 2005, Pfizer bv 2009. Cappelle a/d IJssel, the Netherlands) was developed in Germany [2,16]. The PDQ (© Pfizer Pharma GmbH 2005, Pfizer bv 2009. Cappelle a/d IJssel, the Netherlands) was developed in Germany [2]. The questionnaire can be filled in by the patients themselves and was devised to screen for the presence of a NePC without physical examination. Scoring is performed using a scoring manual and results in a final screening score for the presence of a NePC: ‘negative’, a NePC is unlikely (<15%, score range 0-12); ‘unclear’, result is ambiguous, however a NePC can be present (score range 13-18); or ‘positive’, a NePC is likely (>90%, score range 19-38). The PDQ was tested as a reliable screening tool with a percentage of correctly identified patients of 83% for NeP, sensitivity of 85% and a specificity of 80% [2].
Additional questionnaires
Functioning: Disability Rating Index (DRI) [26]. The self-administered DRI inquires, in a clinical setting, in 12 items about specified activities (Dressing, Out-door walks, Climbing stairs, Sitting longer time, Standing bent over a sink, Carrying a bag, Making a bed, Running, Light work, Heavy work, Lifting heave objects, Participating in exercise/sports). Score range is from 0 to 100 for each item on a Visual Analogue Scale (VAS). A higher score indicates more disability. The DRI has a good responsiveness (p = 0,0001) and a good test-retest correlation of 0,95. The inter- and Intra-rater reproducibility were respectively 0.99 and 0.98 [26]. Mental health status: The Hospital Anxiety Depression Scale (HADS) [27] will be used to assess the presence of anxiety and depressive states of patients. This self-administered questionnaire is divided into an anxiety subscale (HADS-A) and a depression subscale (HADS-D), both containing 7-items with a score range of 0-21. The HADS-Dlv[28] has a good test-retest reliability for HADS-A, HADS-D and the total HADS (respectively 0.89; 0.86 and 0.91 p =0.001). The correlation between the anxiety and the depression subscale was high (0.43 to 0.73) [28]. Based on the review by Bjelland [29] a cut-off score for both the HADS-A and the HADS-D of 8+ gives the best balance in sensitivity and specificity (approximately 0.80 for sensitivity and specificity). Pain Attribution: Pain Attribution Scale (PAS) Additional questions to study the attribution of the pain in patients. On a 5-point Likert-scale the patient is asked to rate the influence of several items on the pain complaints. Rating is from ‘totally not of influence on the pain complaints’ to ‘very much of influence on the pain complaints’. Quality of life: The RAND 36-item Health Survey (RAND-36) [30] is developed to investigate the health related quality of life. The short, self-administered questionnaire consists of 8 different scales: Physical functioning, social functioning, role limitations (physical problem), role limitations (emotional problem), mental health, pain, general health perception and health change. The psychometric quality of the RAND-36-Dlv was studied by van der Zee [31,32]. Change (Follow-up, 2 weeks and 3 months): The Patients Global Impression of Change (PGIC) is a patient rated instrument which measures changes over time on a seven-points scale. Score range is from 1 (very much worse) to 7 (very much improved) [33-35].
Power calculation
In an unselected cohort of chronic LBP patients, 37% had a high probability of a NePC [2]. Sensitivity and specificity of the PDQ is respectively 85% and 80% [2] and the sensitivity and specificity of the DN4 are respectively 83% and 90% [14]. The expected sensitivity and specificity of the Dutch versions of both questionnaires is set at 80% with an prevalence of 37% and the required lower 95% confidence limit > 0.55. According to Flahault et al the N cases is 40. From the equation in the first formula by Flahault, the Ncontrols = 68 [36]. Without prior knowledge of the individual case-control status, the sample size must be determined such that, with high probability (e.g. 95%), the sample contains sufficient numbers of cases and controls. According to the second formula by Flahault et al: Ntotal = 132, in each group. Thus in each group 146 patients will be included (10% drop out). It is expected that this recruitment will be achievable in the 10 general practices, 4 pain treatment centres and 2 departments of neurology chosen.
Data
All data will be collected from the patients and the physicians on paper and stored by Radboudumc. Data management and monitoring will be performed within MACRO (MACRO, version 4.1.1.3720, Infermed, London, United Kingdom).
Statistical analysis
To establish the clinimetric quality of the PDQ-Dlv and the DN4-Dlv a comparison will be made between the outcome of both the screening questionnaires and the original pain classification, the Grading system by Treede at al. [1], the bedside examination and the QST measurements. The prevalence of a NePC in patients with LBP and NSP in the Netherlands will be assessed by extrapolating the outcome of this study to the Dutch population. The monitoring and prognosis of the patient over a period of three months by use of the PDQ-Dlv and the DN4-Dlv will be recorded. Data analysis and statistics will be performed by use of Statistical Package for the Social Sciences (SPSS version 18.0, SPSS Inc., Chicago, Illinois, USA). All statistical tests will be two-tailed, for all statistical analysis the type 1 error will be set on 5%.
Descriptive statistics: The quantitative variables will be described using mean, standard deviation (SD) and range; Qualitative variables will be described using frequency and percentages. To assess central position, dispersion and distribution of variables, the Kolmogorov-Smirnov test will be used.
Univariate analysis: Both the physicians assessments (by rater A and B) will serve as the ‘gold standard’ to assess the presence of a NePC. The internal consistency of both the physicians assessments and the physical examination tests of the DN4 will be separately established for rater A and B by calculating Cronbach’s α that assesses the contribution of each item to the precision of the measurement by both the physicians assessments and the examination items of the DN4 questionnaire.
Inter-rater reliability: will be assessed by the agreement of the results obtained by raters A and B for both the physicians assessments and the examination items of the DN4. Agreement was determined by calculating the Cohen’s kappa coefficient.
Test-retest reliability: will be assessed for the PDQ and DN4, after two weeks of completion of the questionnaires during the first visit. Stability of the questionnaire will be analyzed by measuring the intra-class correlation coefficient and by use of Cohen’s kappa coefficient of agreement.
Prognosis and monitoring: will be assessed for the PDQ and DN4, after three months of completion of the questionnaires during the first visit. Stability of the questionnaire will be analyzed by measuring the intra-class correlation coefficient and by use of Cohen’s kappa coefficient of agreement.
Correlations: will be calculated between scores and continuous variables using Pearson correlation coefficient (i.e. correlation between DN4, PDQ and both the physicians assessments). A students-t test for independent groups or a Mann-Whitney’s U test (non-normal distribution) will be used to compare respectively continuous or ordinal variables between patients with and without a neuropatic pain component
Multivariate analysis: Sensitivity and specificity percentage of well classified observations and Youden index (i.e. sensitivity + specificity-1) will be calculated for different values of the score of the questionnaire by logistical regression analysis. Positive and negative predictive value for both instruments will also be calculated. The corresponding ROC (receiver operating characteristics) curves will be plotted and AUC calculated using the trapezoid method. Discriminant analysis will be used to analyze complementarily of PDQ and DN4 to each other.
Discussion
The rationale for this study is to provide detailed information on the clinimetric quality, including test-retest reliability, of the PDQ-Dlv and DN4-Dlv in patients with LBP, NSP or PND regarding of diagnosing a NePC. A validation of these questionnaires is necessary for its use in everyday clinical practice and also in (inter-)national research to make the outcome comparable in different countries. The key question of this study is whether a NePC as assessed by the physician is reflected in the outcome of the PDQ-Dlv and DN4-Dlv. In already published articles both questionnaires have proven to be useful in daily clinical practice and for research purposes with good clinimetric qualities [2,14].
This study chose an innovative and wide ranging approach to diagnose a NePC in patients in based on a more reliable identification and qualification of a NePC. In the absence of an internationally accepted ‘gold standard’ [12] the challenge was to find a method to examine the patients in a standardized manner to assess a NePC. The opinion of two physicians about a NePC, the most frequently used standard, will be used in this study and is also used in the original validation studies by Freynhagen et al [2] and Bouhassira et al. [14]. Together with the grading system [1], sensory bed-side examination and QST we will aim to confirm the diagnosis of a NePC, also following the NeuPSIG guidelines for the assessment of neuropathic pain [12]. Screening for nerve damage on basis of sensory bed side examination will be performed by both the physicians. The aim of this examination is to find possible abnormalities suggestive for a relevant lesion or disease which affects the peripheral or central somatosensory system [17]. The value of bed-side examination within the clinical examination is that it will give insight into the pathology and the localization of the lesion or disease which is causing the pain. Touch, pin prick, pressure, cold, heath, vibration and temporal summation were included in the examination to assess the NePC of pain [10,12,18]. For heat allodynia we use a Tip-ThermR in a baby-bottle warmer at 45 degrees Celsius. To our knowledge we are the first to use this method. Because a bottle warmer has a reasonably good thermostat, the temperature of the water inside, and thus the TipThermR, will be kept at the set temperature. In this study we did not use the DFNS sensory testing protocol [19,20] but our own NASQ-protocol. This because we were interested in using QST to assess the altered pain processing, including changes in function of endogenous pain modulation, that may underlie chronic pain conditions, instead of testing small and large nerve-fibre function and the nerve damage related sensory changes [21].
This study will aim to try to define patient groups at risk and to understand and assess the variability and burden of a NePC in individual patients. The PDQ [2] outcome is an ordinal scale, ranging from zero to thirty-eight (a neuropathic pain component is unlikely-neuropathic pain component is likely) and thus the question logically arises whether the PDQ is suitable for the assessment of the amount of nerve damage.
By the choice for a non-selective consecutive patient recruitment in specialized pain clinics, neurology clinics as well as general practices this study aims to validate the PDQ-Dlv and DN4-Dlv in a general, unselected choronic pain population. To date, almost all screening questionnaires are validated in a defined, restricted, population, recruited in specialized pain clinics and pre-selected by precise medical diagnosis (lumbar radicular pain, diabetic polyneuropathy, postherpetic neuralgia etc.). Our choice of a non-selcted population might lead to a lower sensitivity and specificity of the PDQ-Dlv and DN4-Dlv in this study than published in the original validation studies [2,14]. However, the choice for a non-consecutive population has the advantage of providing more information relevant to ordinary clinical practice, in that it is relevant to the unselected ‘general population’.
In conclusion, this study seeks to identify the association between patient’ symptoms, the signs as found in the bedside examination and outcome of the QST measurements, the general and mental health status, functioning, pain attribution and quality of life with regard to the outcome of the PDQ-Dlv and DN4-Dlv in patients with chronic pain due to LBP, NSP or PND.
Trial status
This study is ongoing. The expected end date of patient recruitment in this study is July 1, 2013.
Abbreviations
CPM: Conditioned pain modulation; DN4: Douleur neuropathique 4 questions; DN4-Dlv: Douleur neuropathique 4 questions dutch language version; DNIC: Diffuse noxious inhibitory control; DRI: Disability rating index; HADS: Hospital anxiety depression scale; LBP: Low back pain; NASQ paradigm: Nijmegen aalborg screening QST paradigm; NeP: Neuropathic pain; NePC: Neuropathic pain component; NRS: Numeric rating scale; NSP: Neck shoulder pain; PAS: Pain attribution scale; PDQ: Pain detect questionnaire; PDQ-Dlv: Pain detect questionnaire dutch language version; PGIC: Patients global impression of change; RAND-36: RAND 36-item health survey; Radboudumc: Radboud University medical center; QST: Quantitative sensory testing; VAS: Visual analogue scale.
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
HT, AW, OWS, CvW and KV designed the trial protocol. AW and KV secured funding for the validation study. HT, OWS and KV drafted the manuscript. AW and CvW contributed to the manuscript. All authors read and approved the final manuscript.
Pre-publication history
The pre-publication history for this paper can be accessed here:
Contributor Information
Hans Timmerman, Email: hans.timmerman@radboudumc.nl.
Oliver Wilder-Smith, Email: oliver.wilder-smith@radboudumc.nl.
Chris van Weel, Email: chris.vanweel@radboudumc.nl.
André Wolff, Email: andre.wolff@radboudumc.nl.
Kris Vissers, Email: kris.vissers@radboudumc.nl.
Acknowledgements
Thanks to Radboud University medical center, Nijmegen; University Medical Center Utrecht, Utrecht, Erasmus University Medical Centre, Rotterdam, Ziekenhuis Bernhoven, Oss/Veghel; Reinier de Graaf Gasthuis, Delft, St. Anna ziekenhuis, Geldrop, Rijnstate Hospital, Arnhem, and the general practices, all in the Netherlands, for participating in this study. This study was performed within DALI for PAIN, a national program that focuses on neuropathic paincare optimalisation. DALI for PAIN is an initiative of Pfizer. This project is supported by an unrestricted grant from Pfizer.
References
- Treede RD, Jensen TS, Campbell JN, Cruccu G, Dostrovsky JO, Griffin JW, Hansson P, Hughes R, Nurmikko T, Serra J. Neuropathic pain: redefinition and a grading system for clinical and research purposes. Neurology. 2008;70(18):1630–1635. doi: 10.1212/01.wnl.0000282763.29778.59. [DOI] [PubMed] [Google Scholar]
- Freynhagen R, Baron R, Gockel U, Tolle TR. painDETECT: a new screening questionnaire to identify neuropathic components in patients with back pain. Curr Med Res Opin. 2006;22(10):1911–1920. doi: 10.1185/030079906X132488. [DOI] [PubMed] [Google Scholar]
- Freynhagen R, Baron R. The evaluation of neuropathic components in low back pain. Curr Pain Headache Rep. 2009;13(3):185–190. doi: 10.1007/s11916-009-0032-y. [DOI] [PubMed] [Google Scholar]
- Pinto RZ, Maher CG, Ferreira ML, Ferreira PH, Hancock M, Oliveira VC, McLachlan AJ, Koes B. Drugs for relief of pain in patients with sciatica: systematic review and meta-analysis. BMJ. 2012;344:e497. doi: 10.1136/bmj.e497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Attal N, Cruccu G, Baron R, Haanpaa M, Hansson P, Jensen TS, Nurmikko T. European Federation of Neurological S: EFNS guidelines on the pharmacological treatment of neuropathic pain: 2010 revision. Eur J Neurol. 2010;17(9):1113–e1188. doi: 10.1111/j.1468-1331.2010.02999.x. [DOI] [PubMed] [Google Scholar]
- Dieleman JP, Kerklaan J, Huygen FJ, Bouma PA, Sturkenboom MC. Incidence rates and treatment of neuropathic pain conditions in the general population. Pain. 2008;137(3):681–688. doi: 10.1016/j.pain.2008.03.002. [DOI] [PubMed] [Google Scholar]
- Schers H, Bor H, van den Hoogen H, van Weel C. What went and what came? Morbidity trends in general practice from the Netherlands. Eur J Gen Pract. 2008;14(Suppl 1):13–24. doi: 10.1080/13814780802436051. [DOI] [PubMed] [Google Scholar]
- Van Den Linden MWWGP, De Bakker DH, Schellevis FG. Tweede nationale studie naar ziekten en verrichtingen in de huisartsenpraktijk: klachten een aandoeningen in de bevolking en in de huisartspraktijk. Utrecht/Bilthoven: NIVEL/RIVM; 2004. [Google Scholar]
- Vissers KC. The clinical challenge of chronic neuropathic pain. Disabil Rehabil. 2006;28(6):343–349. doi: 10.1080/09638280500287270. [DOI] [PubMed] [Google Scholar]
- Baron R, Binder A, Wasner G. Neuropathic pain: diagnosis, pathophysiological mechanisms, and treatment. Lancet Neurol. 2010;9(8):807–819. doi: 10.1016/S1474-4422(10)70143-5. [DOI] [PubMed] [Google Scholar]
- Cruccu G, Sommer C, Anand P, Attal N, Baron R, Garcia-Larrea L, Haanpaa M, Jensen TS, Serra J, Treede RD. EFNS guidelines on neuropathic pain assessment: revised 2009. Eur J Neurol. 2010;17(8):1010–1018. doi: 10.1111/j.1468-1331.2010.02969.x. [DOI] [PubMed] [Google Scholar]
- Haanpaa M, Attal N, Backonja M, Baron R, Bennett M, Bouhassira D, Cruccu G, Hansson P, Haythornthwaite JA, Iannetti GD, Jensen TS, Kauppila T, Nurmikko TJ, Rice AS, Rowbotham M, Serra J, Sommer C, Smith BH, Treede RD. NeuPSIG guidelines on neuropathic pain assessment. Pain. 2011;152(1):14–27. doi: 10.1016/j.pain.2010.07.031. [DOI] [PubMed] [Google Scholar]
- Bennett MI, Attal N, Backonja MM, Baron R, Bouhassira D, Freynhagen R, Scholz J, Tolle TR, Wittchen HU, Jensen TS. Using screening tools to identify neuropathic pain. Pain. 2007;127(3):199–203. doi: 10.1016/j.pain.2006.10.034. [DOI] [PubMed] [Google Scholar]
- Bouhassira D, Attal N, Alchaar H, Boureau F, Brochet B, Bruxelle J, Cunin G, Fermanian J, Ginies P, Grun-Overdyking A, Jafari-Schluep H, Lantéri-Minet M, Laurent B, Mick G, Serrie A, Valade D, Vicaut E. Comparison of pain syndromes associated with nervous or somatic lesions and development of a new neuropathic pain diagnostic questionnaire (DN4) Pain. 2005;114(1–2):29–36. doi: 10.1016/j.pain.2004.12.010. [DOI] [PubMed] [Google Scholar]
- Van Seventer R, Vos C, Meerding W, Mear I, Le Gal M, Bouhassira D, Huygen FJ. Linguistic validation of the DN4 for use in international studies. Eur J Pain. 2010;14(1):58–63. doi: 10.1016/j.ejpain.2009.01.005. [DOI] [PubMed] [Google Scholar]
- Timmerman H, Wolff AP, Schreyer T, Outermans J, Evers AW, Freynhagen R, Wilder Smith OH, Van Zundert J, Vissers KC. Cross-Cultural Adaptation to the Dutch Language of the PainDETECT-Questionnaire. Pain Pract. 2013;13(3):206–214. doi: 10.1111/j.1533-2500.2012.00577.x. [DOI] [PubMed] [Google Scholar]
- Haanpaa ML, Backonja MM, Bennett MI, Bouhassira D, Cruccu G, Hansson PT, Jensen TS, Kauppila T, Rice AS, Smith BH, Treede RD, Baron R. Assessment of neuropathic pain in primary care. Am J Med. 2009;122(10 Suppl):S13–S21. doi: 10.1016/j.amjmed.2009.04.006. [DOI] [PubMed] [Google Scholar]
- Cruccu G, Truini A. Tools for assessing neuropathic pain. PLoS Med. 2009;6(4):e1000045. doi: 10.1371/journal.pmed.1000045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rolke R, Baron R, Maier C, Tolle TR, Treede RD, Beyer A, Binder A, Birbaumer N, Birklein F, Bötefür IC, Braune S, Flor H, Huge V, Klug R, Landwehrmeyer GB, Magerl W, Maihöfner C, Rolko C, Schaub C, Scherens A, Sprenger T, Valet M, Wasserka B. Quantitative sensory testing in the German Research Network on Neuropathic Pain (DFNS): standardized protocol and reference values. Pain. 2006;123(3):231–243. doi: 10.1016/j.pain.2006.01.041. [DOI] [PubMed] [Google Scholar]
- Rolke R, Magerl W, Campbell KA, Schalber C, Caspari S, Birklein F, Treede RD. Quantitative sensory testing: a comprehensive protocol for clinical trials. Eur J Pain. 2006;10(1):77–88. doi: 10.1016/j.ejpain.2005.02.003. [DOI] [PubMed] [Google Scholar]
- Krumova EK, Geber C, Westermann A, Maier C. Neuropathic pain: is quantitative sensory testing helpful? Curr Diabetes Reports. 2012;12(4):393–402. doi: 10.1007/s11892-012-0282-7. [DOI] [PubMed] [Google Scholar]
- Wilder Smith OH. A Paradigm-Shift in Pain Medicine: Implementing a Systematic Approach to Altered Pain Processing in Everyday Clinical Practice Based on Quantitative Sensory Testing. Aalborg, Denmark: Center for Sensory-Motor Interaction (SMI), Department of Health Science and Technology, Aalborg University; 2013. [Google Scholar]
- Yarnitsky D. Conditioned pain modulation (the diffuse noxious inhibitory control-like effect): its relevance for acute and chronic pain states. Curr Opin Anaesthesiol. 2010;23(5):611–615. doi: 10.1097/ACO.0b013e32833c348b. [DOI] [PubMed] [Google Scholar]
- Pud D, Granovsky Y, Yarnitsky D. The methodology of experimentally induced diffuse noxious inhibitory control (DNIC)-like effect in humans. Pain. 2009;144(1–2):16–19. doi: 10.1016/j.pain.2009.02.015. [DOI] [PubMed] [Google Scholar]
- Yarnitsky D, Arendt-Nielsen L, Bouhassira D, Edwards RR, Fillingim RB, Granot M, Hansson P, Lautenbacher S, Marchand S, Wilder-Smith O. Recommendations on terminology and practice of psychophysical DNIC testing. Eur J Pain. 2010;14(4):339. doi: 10.1016/j.ejpain.2010.02.004. [DOI] [PubMed] [Google Scholar]
- Salen BA, Spangfort EV, Nygren AL, Nordemar R. The disability rating index: an instrument for the assessment of disability in clinical settings. J Clin Epidemiol. 1994;47(12):1423–1435. doi: 10.1016/0895-4356(94)90086-8. [DOI] [PubMed] [Google Scholar]
- Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67(6):361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- Spinhoven P, Ormel J, Sloekers PP, Kempen GI, Speckens AE, Van Hemert AM. A validation study of the Hospital Anxiety and Depression Scale (HADS) in different groups of Dutch subjects. Psychol Med. 1997;27(2):363–370. doi: 10.1017/S0033291796004382. [DOI] [PubMed] [Google Scholar]
- Bjelland I, Dahl AA, Haug TT, Neckelmann D. The validity of the Hospital Anxiety and Depression Scale. An updated literature review. J Psychosom Res. 2002;52(2):69–77. doi: 10.1016/S0022-3999(01)00296-3. [DOI] [PubMed] [Google Scholar]
- Hays RD, Sherbourne CD, Mazel RM. The RAND 36-Item Health Survey 1.0. Health Econ. 1993;2(3):217–227. doi: 10.1002/hec.4730020305. [DOI] [PubMed] [Google Scholar]
- VanderZee KI, Sanderman R, Heyink J. A comparison of two multidimensional measures of health status: the Nottingham Health Profile and the RAND 36-Item Health Survey 1.0. Qual Life Res. 1996;5(1):165–174. doi: 10.1007/BF00435982. [DOI] [PubMed] [Google Scholar]
- VanderZee KI, Sanderman R, Heyink JW, De Haes H. Psychometric qualities of the RAND 36-Item Health Survey 1.0: a multidimensional measure of general health status. Int J Behav Med. 1996;3(2):104–122. doi: 10.1207/s15327558ijbm0302_2. [DOI] [PubMed] [Google Scholar]
- Collins SL, Edwards J, Moore RA, Smith LA, McQuay HJ. Seeking a simple measure of analgesia for mega-trials: is a single global assessment good enough? Pain. 2001;91(1–2):189–194. doi: 10.1016/s0304-3959(00)00435-8. [DOI] [PubMed] [Google Scholar]
- Farrar JT, Young JP Jr, LaMoreaux L, Werth JL, Poole RM. Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain. 2001;94(2):149–158. doi: 10.1016/S0304-3959(01)00349-9. [DOI] [PubMed] [Google Scholar]
- Fischer D, Stewart AL, Bloch DA, Lorig K, Laurent D, Holman H. Capturing the patient's view of change as a clinical outcome measure. JAMA. 1999;282(12):1157–1162. doi: 10.1001/jama.282.12.1157. [DOI] [PubMed] [Google Scholar]
- Flahault A, Cadilhac M, Thomas G. Sample size calculation should be performed for design accuracy in diagnostic test studies. J Clin Epidemiol. 2005;58(8):859–862. doi: 10.1016/j.jclinepi.2004.12.009. [DOI] [PubMed] [Google Scholar]


