Abstract
Over three decades have passed since the first report on the expression of CA125 by ovarian tumors. Since that time our understanding of ovarian cancer biology has changed significantly to the point that these tumors are now classified based on molecular phenotype and not purely on histological attributes. However, CA125 continues to be, with the recent exception of HE4, the only clinically reliable diagnostic marker for ovarian cancer. Many large-scale clinical trials have been conducted or are underway to determine potential use of serum CA125 levels as a screening modality or to distinguish between benign and malignant pelvic masses. CA125 is a peptide epitope of a 3–5 million Da mucin, MUC16. Here we provide an in-depth review of the literature to highlight the importance of CA125 as a prognostic and diagnostic marker for ovarian cancer. We focus on the increasing body of literature describing the biological role of MUC16 in the progression and metastasis of ovarian tumors. Finally, we consider previous and on-going efforts to develop therapeutic approaches to eradicate ovarian tumors by targeting MUC16. Even though CA125 is a crucial marker for ovarian cancer, the exact structural definition of this antigen continues to be elusive. The importance of MUC16/CA125 in the diagnosis, progression and therapy of ovarian cancer warrants the need for in-depth research on the biochemistry and biology of this mucin. A renewed focus on MUC16 is likely to culminate in novel and more efficient strategies for the detection and treatment of ovarian cancer.
Keywords: Ovarian cancer, CA125, MUC16, Cancer biomarker, Metastasis, Immunesupression, Natural killer cells
Introduction
CA125 is best known as a biomarker to monitor epithelial ovarian cancer and for the differential diagnosis of pelvic masses [1,2]. Serum levels of CA125 are routinely monitored in patients with ovarian cancer, and an increase from an individualized nadir concentration is a prognostic indicator of cancer recurrence. An extensive body of work has been published on the interpretation of CA125 assay results, with particular focus given to CA125 in ovarian cancer patients undergoing therapy [1-12]. Understanding of the clinical applicability of the CA125 assay has come from basic, translational, and clinical studies conducted since the early 1980’s [13-20]. However, what remains underappreciated is that the assay to measure CA125 in clinical samples is limited by an incomplete understanding of the biochemical structure of this antigen. Here, we will review the current knowledge of the structure of CA125 and provide critical appraisal of factors that may interfere with accurate and sensitive measurement of this biomarker.
CA125 is a repeating peptide epitope of the mucin MUC16 [21,22], which promotes cancer cell proliferation and inhibits anti-cancer immune responses [23-26]. Our discussion of the biological role of MUC16 will focus on its importance in cancer cell signaling, metastasis, regulation of immune responses and on anti-cancer therapeutic strategies that target this mucin. A major goal of this review is to highlight gaps in our knowledge of the biochemistry and biology of MUC16/CA125 to provide a framework of unanswered questions to be addressed in future studies.
CA125 as a clinical biomarker
CA125 has been extensively investigated as a biomarker in three separate clinical scenarios: (1) as a screening test for the early detection of ovarian cancer, (2) to distinguish between benign and malignant disease in pre- and post-menopausal women presenting with pelvic masses, and (3) to monitor response to therapy in women with ovarian cancer.
CA125 as a screening modality for ovarian cancer
An increase (beyond a cut-off of 30–35 U/ml) is generally observed in blood samples that are serially obtained from women with ovarian cancer [27]. Therefore, for screening, longitudinal monitoring of serum CA125 levels is likely to be more useful than a single measurement. The Risk of Ovarian Cancer Algorithm (ROCA) predicts the probability of ovarian cancer based on such longitudinal monitoring of CA125 [27,28]. ROCA allows triaging of patients into groups with low, intermediate and high risk of ovarian cancer.
ROCA was developed after retrospective analysis of serum samples obtained from an ovarian cancer screening trial of 5550 women conducted in Sweden [29,30]. This trial concluded that serum CA125 monitoring will be most beneficial in post-menopausal women. In this cohort, the serum CA125 test provides sensitivity and specificity of 91 and 94.5%, respectively.
The largest fully reported ovarian cancer screening trial that used CA125 as a biomarker (in combination with ultrasonography) was conducted in the United Kingdom with a cohort of 22,000 women [31]. A total of 41 women tested positive for ovarian cancer based on CA125 and ultrasound. Only eleven of these 41 cases were found to be truly positive for ovarian cancer after subsequent surgical investigation. Eight women who had screened negative for ovarian cancer developed the disease 12–22 months after the initial screen.
Enthusiasm for the success of combination of CA125 assay and transvaginal ultrasound screening is tempered by the negative results from the Prostate, Lung, Colorectal, and Ovarian Cancer (PLCO) trial [32-34]. In this randomized control trial of 78,216 subjects, women in the intervention arm were screened for CA125 levels and transvaginal ultrasound. There was no improvement in mortality (the primary endpoint of this study) in this trial. The PLCO trial did not employ ROCA. A retrospective analysis [35] has suggested that the use of ROCA in PLCO would not have led to statistically significant mortality benefit of screening, in part because of the long delay (one year) between screens and the absence of a standardized diagnostic algorithm [32].
Given the low prevalence of ovarian cancer in the general population, it is estimated that a good clinical trial to develop a screening paradigm for ovarian cancer would require recruitment of >150,000 women [30,36]. The United Kingdom Collaborative Trial of Ovarian Cancer Screening (UKCTOCS) accrued a total of 202,638 post-menopausal women between 2001 and 2005 [37]. Subjects were randomized into (1) control, (2) serum CA125 plus transvaginal ultrasound, and (3) transvaginal ultrasound only groups [38]. The ROCA was used to triage women in the second group to low, intermediate and high-risk categories. Subjects in the intermediate-risk category were monitored for CA125 levels every 4 months, and if they continued to show increased risk for ovarian cancer, were monitored by ultrasound scans. The subjects in the high-risk category underwent transvaginal ultrasound scans [38]. Final results from this trial are expected in 2015. Interim analysis from this trial has led to the promising finding that 47.1% of women testing positive after combined assessment with CA125 test and transvaginal ultrasound had stage I or II disease [38]. The combined use of ROCA and ultrasound, strict guidelines for follow up in 3–4 months after elevated CA125 is detected and a well-coordinated plan for screening patients across all participating sites are advantages of the UKCTOCS over the PLCO study design that are expected to contribute to successful identification of a screening strategy for ovarian cancer [35,39]. Survival data from the UKCTOCS trial is expected in 2015.
CA125 as a diagnostic marker for ovarian cancer
The majority of patients with ovarian cancer are periodically assayed for CA125. An increase in concentration of CA125 above a nadir is an indicator of disease recurrence [40-42]. Another important potential application of the CA125 assay is in distinguishing benign pelvic masses from ovarian cancer [43]. The Risk of Malignancy Index (RMI) combines serum CA125 concentrations with ultrasound and menopausal status to distinguish between benign disease and cancer [44]. Recent studies suggest that a Risk of Ovarian Malignancy Algorithm (ROMA) incorporating CA125 and HE4 levels in serum is likely to produce a test of high sensitivity and specificity in identifying ovarian cancer patients [45-47].
Currently, HE4 is the only biomarker, other than CA125, that has been approved by the U.S. Food and Drug Administration as a diagnostic marker for ovarian cancer [48,49]. Another algorithm, OVA1, uses CA125, apolipoprotein A1, transthyretin, transferrin and β2-microglobulin and takes into account data from ultrasound imaging and menopausal status of patients [50].
Mesothelin, osteopontin, CA15.3, CA19.9, AFP, KLK6 and several others have been investigated and suggested as potential biomarkers for ovarian malignancy. A recent multi-center effort to test the sensitivity and specificity of panels of markers conducted using the serum samples obtained from PLCO has been reported [51]. None of the panels of markers tested in this trial improve on the sensitivity and specificity of CA125 in screening or ovarian cancer diagnosis [52,53]. The conclusion from the important trials and studies described in this section is that CA125 continues to be, and for the foreseeable future will persist as, the predominant and most clinically useful biomarker for ovarian cancer. It is therefore imperative that significant effort be put forth to clearly understand the chemical nature of this antigen with the express intent of improving the widely used CA125 assay.
Biochemistry of CA125
CA125 was first identified in a screen of monoclonal antibodies raised against the ovarian cancer cell line OVCA433 [13,54]. One antibody, OC125, recognized an antigen in ovarian cancer specimens which was designated as CA125 [13-17,55]. Several antibodies, M11, VK8 and OV197 among them, were subsequently developed against CA125 [56,57]. Based on their binding specificities, CA125-specific antibodies are grouped as belonging to the OC125, M11 or OV197 families [58-61].
Initial gel filtration experiments suggested that CA125 had a molecular weight as high as 2 million Da [62]. Hanisch and colleagues demonstrated that CA125 activity was contained in a high molecular weight mucinous fraction isolated from human milk [63]. Isopycnic density gradient centrifugation led to isolation of CA125 activity in a fraction with the buoyant density of 1.41 g/ml, a density that is typically observed for most human mucinous glycoproteins [63].
A more definitive study on the molecular characterization of CA125 by Davis et al. showed that CA125 isolated from OVCA433 cells had a buoyant density of 1.42 g/ml whereas the antigen in human serum and milk had a density of 1.46 g/ml and 1.39 g/ml, respectively [64]. Davis and co-workers also performed size exclusion chromatography of OVCA433 cell culture supernatant on a Sepharose CL-4B column, a matrix with a size exclusion limit of 6 × 104 – 2 × 107 Da for globular proteins. These chromatography studies demonstrated that CA125 activity was contained in fractions having molecular masses of 200,000-1 million Da [64].
Importantly, the report by Davis et al. conclusively refuted a previous claim that CA125 was a carbohydrate epitope [63,64]. Oxidation of the CA125-containing fractions at pH 4.5 with 1 mM and 10 mM sodium periodate—conditions that oxidize vicinal hydroxyls of terminal sialic acid or those present in the entire oligosaccharide chains, respectively [65,66]—did not result in significant loss of OC125 binding to the antigen. Instead, exposure to heat and low pH (100°C, 3.3 pH), protease digestion, reduction and alkylation in buffer containing 4 M guanidine hydrochloride abrogated binding of OC125 to the antigen. These crucial observations suggested that CA125 was a conformationally dependent peptide epitope present in a high molecular weight mucin. Although some incremental advances in our understanding of the molecule were gained from important fundamental research conducted independently by Lloyd and O’Brien [20,56,57,62,67-70], major advance in our understanding of the biochemistry of CA125 was gained from the identification of MUC16 as the mucin that contained this antigen.
MUC16, a large molecular weight membrane-spanning mucin
Molecular cloning of MUC16 revealed it to be a mucinous glycoprotein with an average molecular weight between 3–5 million Da [21,22,71,72]. Similar to other membrane-spanning mucins, MUC16 (Figure 1) is composed of a tandem repeat region sandwiched between N-terminal and C-terminal domains [21,22]. The C-terminal domain is the smallest part of the molecule and is composed of 284 amino acids (Figure 1). While it has been proposed that this C-terminal domain can be phosphorylated under specific conditions, conclusive proof is lacking [21,73,74].
Figure 1.
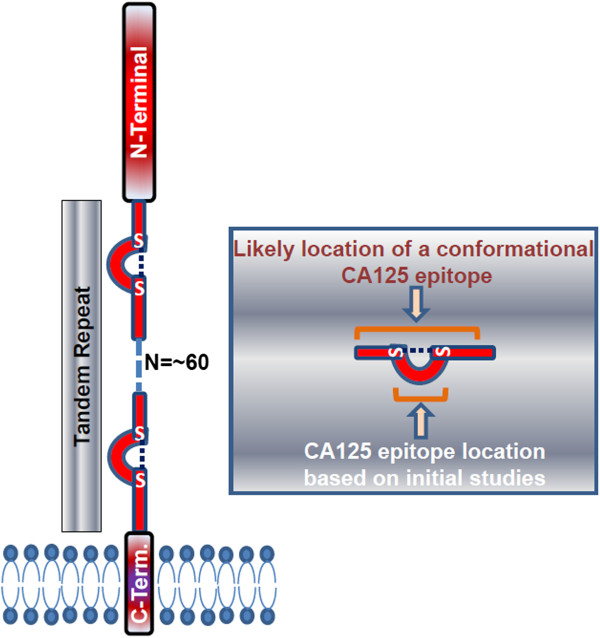
MUC16 structure. Model shows the three domains of MUC16 and potential location of the CA125 epitope in a tandem repeat.
The N-terminal region is composed of 12,068 amino acids [71]. Other than potential sites for both N-linked and O-linked glycosylation, there are no major structural features identified in this domain. The tandem repeat domain is composed of up to 60 repeats (Figure 1). Each repeat has 156 amino acids [21]. The primary amino acid sequence in each repeat is not identical but is homologous. Two conserved cysteines, at positions 59 and 79 of each repeat, are proposed to have structural significance [21]. These cysteines could form intra- as well as inter-molecular disulfide bonds. While the intramolecular disulfide bonds could form loops within each MUC16 molecule, intermolecular disulfide linkages may contribute to formation of an extracellular matrix [71].
Evidence supporting the location of CA125 antigen in the MUC16 tandem repeat came from two initial studies where the tandem repeats were expressed in E. coli or in human ovarian cancer cell lines [21,72]. In the first study, the 11th MUC16 tandem repeat (R11) was expressed and isolated from E. coli [21]. This recombinant R11 protein was recognized by the three anti-CA125 antibodies M11, OC125 and OV197. In another study, a recombinant protein containing three of the MUC16 tandem repeats was produced in two cell lines—SW626 and SKOV-3—that do not express MUC16 [72]. The recombinant proteins expressed in these cell lines were detected by M11 and OC125 but not by the VK8 antibody. This finding was interesting because VK8 was initially classified as an M11-type antibody, but studies with the recombinant MUC16 fragments demonstrated clear differences in the epitope specificities of M11 and VK8 [72].
Digestion of the recombinant R11 tandem repeat by the endoproteases Lys-C or Asp-D completely destroyed the CA125 epitope as demonstrated by the observation that the resulting fragments were not detected by the OC125 or M11 antibodies [21]. It was primarily this one experiment that led to the prevalent viewpoint that the CA125 epitope is located in the 21-amino acid loop of the tandem repeats formed by disulfide bridging of cysteines located at positions 59 and 79. Recent experiments conducted by us and by Bressan et al. [75] have led us to believe that this model is inaccurate and that the CA125 epitope has not been sufficiently characterized.
In our experiments we did not observe binding of OC125 and M11 antibodies to a synthetic 21-mer peptide sequence (Peptide 1) comprising the loop region shared by eight of the 60 MUC16 tandem repeats. We also investigated OC125 and M11 binding to three variants of Peptide 1 that differ in single amino acids (C21A, Peptide 3; P8S, Peptide 4) or in two amino acids (P8S and C21A, Peptide 5). These variants were selected because their sequences are also found in the MUC16 repeats (Ser appears in position 8 in ~25% of tandem repeats) or they produce specific modifications in the secondary structures of the peptides (replacing Cys with Ala removes the possibility of intramolecular disulfide bonding) [76]. In five independent assay protocols—Silicon Photonic Microring Resonator Immunoassay, Surface Plasmon Resonance Immunoassay, ELISA, Competitive ELISA and Affinity Probe Capillary Electrophoresis—none of these four peptides were recognized by OC125 and M11 antibodies.
Not all of the MUC16 repeats are recognized to the same extent by these antibodies [75]. Recombinant proteins containing either R2, R7, R9, R11, R25, or R51 repeats were recognized by M11 in Western blot assays. However, only a subset of these repeats (R9, R11, R25, and R51) were detected strongly by OC125 and a partially overlapping subset (R2, R9, R25, and R51) were detected by OV197 antibodies. Deletion mutants of the 156 amino acid R25 repeat that are missing residues 129–156 from the C-terminal end retain binding by OC125, M11 and OV-197. However, deletion of the amino acids 1–30 from the N-terminal end of this truncated mutant abrogated binding by all three antibodies. Thus the CA125 epitope is likely localized between amino acids 1–128 of the MUC16 repeats [75]. However, any further refined characterization of the CA125 epitope has not been achieved.
Incidentally, the region 1–128 of R25 contains the Sea urchin Enterokinase and Agrin (SEA) domain [71,77,78]. In fact BLAST protein homology search shows the presence of SEA domains in each of the MUC16 tandem repeats (Additional file 1). In addition, one SEA domain is also located in the C-terminal region of the mucin. While MUC1 and some other mucins are known to contain a single or limited number of SEA domains, such extensive presentation of these structural units is unique to MUC16 among all of the identified mammalian mucins. One SEA domain from the murine Muc16 ortholog has been structurally characterized [78]. While SEA domains can exhibit autoproteolytic activity, any potential importance of this domain in the shedding of MUC16 is not clear.
Antibodies that recognize continuous epitopes are likely to bind sequences that are composed of not more than 15–22 amino acids of which 5–6 residues are critical as they provide maximum binding energy [79]. However, deletion of even 30 amino acids from the N- or the C-terminal end of the 128 amino acid recombinant repeat domain abrogates antibody binding [75]. These results have prompted the suggestion that the CA125 epitope is not continuous but is instead a discontinuous epitope that is dependent on the secondary conformational structure of the MUC16 tandem repeat [75]. While this suggestion is consistent with our studies with the C-loop peptides, its acceptance relies on the proposal that detection of the 1–128 deletion mutant by the CA125 antibodies in western blots follows renaturation during transfer to the nitrocellulose membrane [75]. One important conclusion drawn from our studies with the peptides and those reported by Bressan et al. is that the CA125 epitope most likely does not reside in the loop region of the tandem repeat as predicted initially [21,75]. The implications of this conclusion are serious as it indicates that even though the CA125 assay is routinely used to monitor the vast majority of patients with serous ovarian cancer, the exact molecular nature of the antigen is not accurately characterized.
The CA125 II assay currently used to measure serum concentrations of this biomarker in patients uses M11 as a capture antibody and OC125 as a tracer [13,56,70]. Studies with recombinant R11 indicate that binding of OC125 to this antigen is enhanced several-fold after pre-binding of M11 [61]. Whether enhancement—or inhibition—of OC125 binding is also observed with other recombinant repeats of MUC16, or the entire molecule in patient sera, needs to be determined. A corollary to this statement is that since OC125 binding is sensitive to the molecular environment of its epitope, other factors such as post-translational modification may influence detection of CA125 in patient sera.
In our experiments with ovarian cancer cell lines, we have observed that OC125 weakly binds to the surface of cells—SKOV-3 and A2780—that are generally considered to be non-expressors of MUC16. However, under the same conditions another anti-CA125 antibody, VK8, which was used in the initial cloning experiments [22,57], does not recognize SKOV-3 (Figure 2). The marginal binding of OC125 to SKOV-3 cells corresponds to weak expression of MUC16 as determined by RT-PCR (data not shown).We observe that trypsin digestion significantly reduces VK8 binding to MUC16-expressing cells, but only slightly reduces OC125 binding to cells under the same conditions (Figure 3). We tested the possibility that even after trypsin digestion the OC125 epitopes remain bound to the cell surface via disulfide bridges. Mild treatment of the cells with mercaptoethanol or dithiothreitol to release disulfide-bound moieties did not decrease OC125 binding to the trypsinized OVCAR-3 cells (Figure 3).
Figure 2.
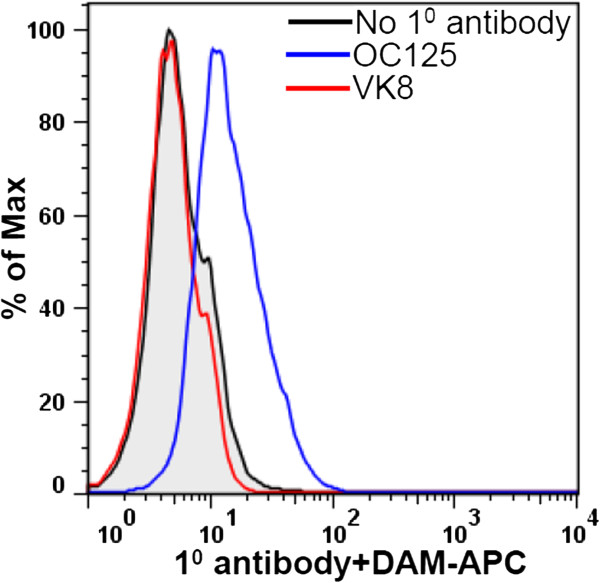
OC125 weakly binds to cells that are generally considered negative for MUC16. SKOV-3 cells (identity confirmed by STR analysis) were stained with the primary (1°) antibodies OC125 or VK8 followed by incubation with allophycocyanine (APC)-labeled donkey anti-mouse (DAM) secondary antibody. Binding of the antibodies to SKOV-3 cells was determined on a LSR-II flow cytometer. RT-PCR using MUC16 primers previously reported [178], was used to determine expression of MUC16 in OVCAR-3, ECC-1 and SKOV-3 cells (data not shown).
Figure 3.
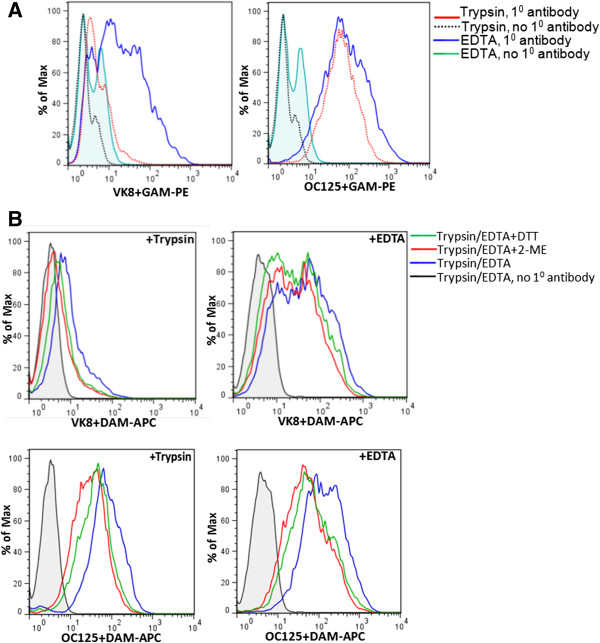
Cell surface MUC16 is sensitive to proteolysis. A, Binding of OC125 and VK8 to OVCAR-3 cells that were harvested with trypsin or EDTA containing media was determined by flow cytometry. A significant decrease in VK8 binding to cells harvested after trypsin treatment was observed whereas under these conditions, OC125 binding was less affected. B, Reduction of the trypsinized OVCAR-3 cells with dithiothreitol (DTT) or 2-mercaptoethanol (2-ME) did not result in additional loss of OC125 binding to the cells. In all experiments, a fluorescently tagged goat anti-mouse antibody was used for detection.
If CA125 is indeed a discontinuous epitope, it is not clear if the O- or N-glycosylation of the tandem repeat will influence binding of OC125, M11 or OV197. Most studies characterizing the MUC16 repeats have been conducted with recombinant proteins produced in bacterial cells [21,75] and therefore lacking native glycosylation. Similarly our 21mer peptides, assembled by solid-phase peptide synthesis, are not glycosylated. After initial characterization of the glycosylation of MUC16 [80], there has not been a robust and systematic characterization of the glycan chains attached to each domain of the mucin or of the glycan site occupancy in mucin molecules produced by tumor versus normal epithelial cells. Attempts to identify disease-specific MUC16 glycoforms by glycomic analysis are producing interesting results that may enhance the diagnostic potential of this mucin [81-88]. However, with the enormous potential diversity in glycan chains and glycoforms a significant effort will be required to fully understand the post-translational status of this mucin and its effect on detection in the CA125 assay and systemic half-life of the MUC16 glycoforms.
Mucins in systemic circulation are rapidly processed by the reticulo-endothelial cells, leaving behind only a fraction of the mucins in circulation to be detected in clinical assays such as the CA125 test [89]. The combined effects of MUC16 clearance—reducing the amount of circulating MUC16 to miniscule levels—and the inability of the antibodies to uniformly bind all tandem repeats and isoforms—undercounting circulating MUC16—suggests that the CA125 assay significantly underestimates the concentration of this biomarker. New generation of reagents and assay protocols that can capture and more accurately quantify a larger cohort of the MUC16 molecules will likely add to the clinical significance of this biomarker.
To date, the majority of the anti-MUC16 antibodies raised against full-length mucin recognize regions within the tandem repeat domains [58,59]. An explanation for the bias toward antibodies that recognize the tandem repeat region of MUC16 is not available but is likely due to higher immunogenicity of these epitopes. Antibodies against defined epitopes that are outside of the tandem repeat region (against peptides from the carboxy terminal end [90,91], for example) will serve an important purpose in modifying the CA125 assays and also in attempts to understand the biology of this mucin.
Biological role of MUC16
MUC16 is expressed by normal bronchial, endometrial, ovarian and corneal epithelial cells and has evolved from the proteoglycan, agrin [24,92-98]. A transmembrane region anchors the mucin in the cell membrane and as a result the mucin can be detected on the cell surface (Figure 4).
Figure 4.
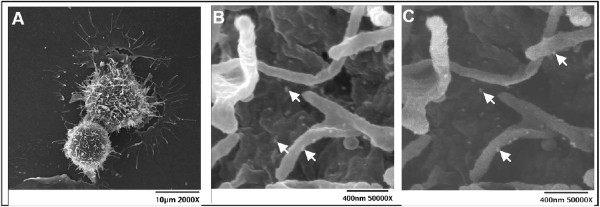
MUC16 on the surface of ovarian cancer cells. OVCAR-3 cells were labeled with VK8 followed by colloidal gold nanoparticles conjugated with goat anti-mouse secondary antibody. A, low magnification secondary electron image of two labeled OVCAR-3 cells. B, Scanning Electron Microscopy (SEM) image of OVCAR-3 showing colloidal gold nanoparticles binding to cell surface and microvilli. C, Back scattered electron image of same cell surface shown in B, clearly showing the colloidal gold nanoparticles. Bright spots (some indicated by bright arrows) in B and C are the colloidal gold nanoparticles. OVCAR-3 cells are not labeled with colloidal gold nanoparticles in the absence of VK-8 (data not shown).
MUC16 is released from the cell surface following proteolytic cleavage at a site presumably 50 amino acids upstream of its transmembrane segment [21]. As a result the proteolytically released ectodomain of MUC16 is not significantly different in molecular weight than the cell surface-bound intact mucin.
Neutrophil elastase, MMP-7, MMP-9 and bacterial metalloprotease (ZmpC) can release the ectodomain of MUC16 [99-101]. Post-translational modifications (especially glycosylation) around the site of cleavage are thought to regulate the release of the ectodomains of these mucins [100]. Post-translational modifications around the cleavage site may be a variable that impacts the sensitivity of the CA125 assay.
In corneal epithelial cells, MUC16-Galectin-3 interaction has been shown to serve as a barrier for bacterial and viral infections in ocular epithelia [102,103]. These are the first studies to show a potential biological role for MUC16 in non-cancer cells. However, knockdown of murine Muc16 does not result in any obvious functional deficit [104,105]. Since these knockout mice were maintained in a pathogen free environment and were not otherwise challenged with chemical or biological agents, the potential impact of Muc16 knockdown in specific pathological states remains unknown. Further exploration into the normal physiologic role(s) of human and murine MUC16 is warranted.
Immunoprotection of cancer cell cells
Innate immune cells, Natural Killer (NK) cells and monocytes are unable to attack tumor cells expressing high levels of MUC16 [106]. Knockdown of MUC16 results in increased lysis of the ovarian cancer cells by the cytolytic NK cells. The mechanism by which MUC16 inhibits NK cell-mediated killing of cancer cells is under investigation. One proposal is that MUC16 acts as a barrier that prevents interaction between the NK cells and their targets [106]. NK cells require physical contact with the target cells for cytolysis to occur. NK cell immunologic synapse is defined by polarization of cytoskeletal and cell signaling molecules along with cytolytic granules of the effector cells to the site of contact [107-109]. The NK cell cytolytic granules are released into the target cells, triggering cell death via apoptosis. MUC16 with its ~5 million Da molecular size is expected to have a linear length of 1–5 μm [106,110]. Due to its extended structure and overall negative charge (due to the presence of terminal sialic acid residues [80]), MUC16 may inhibit intimate interactions between NK and cancer cells. This situation is analogous to the mechanism of immuneprotection demonstrated for MUC4 [111].
Imunoprotective effect by MUC16 may also arise from its interaction with the NK cell inhibitory receptor, Siglec-9 (Figure 5) [112]. NK cells express both activating (NKG2D, CD16, DNAM-1, for example) and inhibitory receptors (Killer Immunoglobulin-like Receptors (KIR’s), Siglec-9, and Siglec-7, for example) on their cell surface. Interaction of activating and inhibiting receptors with their corresponding ligands on target cells leads to either activation or inhibition of the NK cell cytolytic response (reviewed in [113] and other articles). The interplay between the activating and inhibitory receptors controls the cytolytic activity of NK cells.
Figure 5.
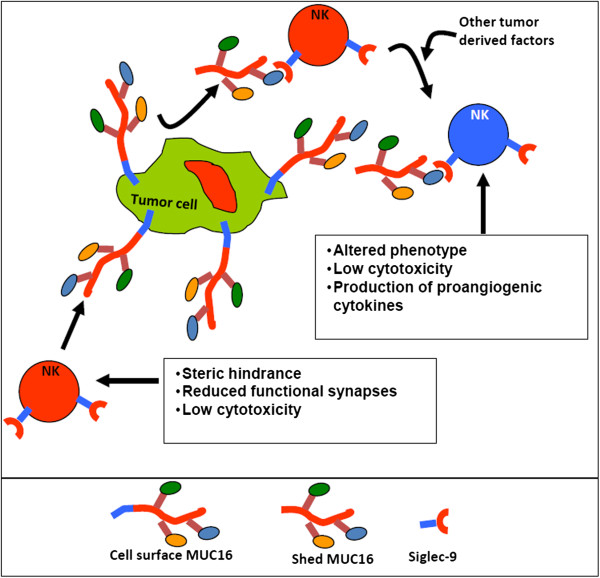
Model for MUC16-induced NK cell inhibition. MUC16 released from tumors binds to naïve NK cells (shown in red) and along with other tumor derived factors induces a phenotypic and functional change. The altered NK cells (shown in blue) secrete cytokines that promote angiogenesis. The cell surface bound MUC16, on the other hand, acts as an anti-adhesive mucin and blocks the interaction between the NK cells and ovarian tumor cells thereby preventing cancer cell cytolysis.
Siglecs are a class of inhibitory receptors that bind to negatively charged sialic acid ligands [114-119]. MUC16 oligosaccharides carry sialic acid in a terminal α2-3 linkage [80]. Oligosaccharides terminated with α2-3-linked sialic acids are recognized as ligands by the inhibitory Siglec-9 receptor [120]. Our work demonstrates that MUC16-Siglec-9 interaction protects cancer cells from NK cell attack. Siglec-9 is also expressed on monocytes and MUC16 promotes binding of monocytes to cancer cells. Upon binding to its ligand, Siglec-9 is phosphorylated on its Immunoreceptor Tyrosine-based Inhibition Motif (ITIM) tail, triggering an inhibitory signaling cascade that results in inhibition of the NK cell response [121]. Ovarian cancer cells are therefore likely to be protected from NK cell and monocyte attack due to the negative signaling induced via MUC16-Siglec-9 interaction (Figure 5). This type of protection can occur from interaction of the NK and monocyte Siglec-9 with MUC16 on the surface of cancer cells and also from circulating MUC16 molecules cleaved from the cancer cells via proteolysis.
MUC16 protects ovarian cancer cells from naïve unstimulated NK cells as well as IL-2 stimulated NK cells. A recent study has implicated MUC16 in inhibiting target cell killing via Antibody-dependent Cell-Mediated Cytotoxicity (ADCC) [122], suggesting that the mucin may dampen the response of immunotherapeutic antibodies.
NK cells preferentially target ovarian tumor cells that express low levels of MUC16 on their cell surface [106]. As a result, tumor cells surviving NK cell attack are high expressors of MUC16 that are more resistant to immune attack. We have proposed that NK cells contribute to immune editing [123-125] by selectively lysing cancer cells expressing lower levels of MUC16. As a result, those cancer cells with high levels of MUC16, the subset that is most likely to resist immune attack, survive.
Pro-metastasis role of MUC16
Immune editing in favor of cancer cells expressing higher levels of MUC16 may also increase peritoneal metastasis of ovarian tumors [126-129]. MUC16 binds to mesothelin, a GPI-anchored glycoprotein found on the surface of mesothelial cells and also overexpressed by ovarian tumors, with an apparent Kd of 5 nM [23,130,131]. MUC16-mesothelin interaction allows tumor cells to bind to themselves (likely increasing tumor mass at metastatic sites) and also allows attachment of ovarian cancer cells to the mesothelial lining [130]. Removal of N-glycans from MUC16 attenuates its interaction with mesothelin [132]. Mesothelin, similar to other members of its superfamily, contains superhelical ARM-type repeats that could potentially recognize carbohydrate ligands presented by MUC16 [132].
MUC16, via its sialofucosylated oligosaccharides, binds to both E- and L-selectin even under shear stress conditions [133]. Contribution of MUC16-selectin interaction to ovarian cancer progression or metastasis is not known. Even after MUC16 knockdown, E- and L-selectin binding is observed to cancer cells, presumably via other glycolipid, mucin, or glycoprotein ligands [133]. Therefore, interpretation of results MUC16-selectin interactions and their possible roles in metastasis are complicated by presence of such redundant binding mechanisms.
MUC16 associated cell signaling
MUC1 and MUC4 undergo auto-cleavage during their synthesis to generate α- and β-subunits [134-136]. The β-subunit of MUC1 and MUC4 is involved in intracellular signaling. For example, EGF stimulation causes the MUC1 β-subunit to signal via PI3K and MAPK [137,138] MUC1 β-subunit also interacts with p53, NF-κB, β-catenin and STAT1 [139,140].
Phosphorylation of the cytoplasmic portion of C-terminal domain of MUC16 increases shedding of the ectodomain of this mucin [74]. Specific serine, threonine and tyrosine residues in the cytoplasmic tail of MUC16 have been proposed as likely candidates for phosphorylation [21].
Knockdown of MUC16 inhibits in vitro and in vivo proliferation of cancer cells [141-143] MUC16-triggered activation of STAT3 via JAK2 results in increasing cancer cell proliferation. On the other hand, knockdown of MUC16 causes cell cycle arrest (either in G2/M or G1 phase) and apoptosis [143,144].
Expression of the C-terminal domain of the mucin in the MUC16neg SKOV-3 cells increases their proliferation with 2–3 fold increase in tumor weight and a significant decrease in survival of tumor-bearing mice [142]. MUC16 knockdown causes a decrease in the expression of matrix metalloproteases (MMP-2), a class of proteolytic enzymes that plays a crucial role in cancer cell metastasis [144-146]. A recent report suggests that the cytoplasmic tail of MUC16 interacts with Src-family kinases and induces E-cadherin-mediated cell invasion and migration [147].
MUC16 is overexpressed but not associated with decreased survival or chemoresistance
Silencing of MUC16 increased the sensitivity of OVCAR-3 cells to cisplatin and doxorubicin but not to paclitaxel [141]. However, bioinformatics analysis of MUC16 expression and mutations available through The Cancer Genome Atlas (TCGA) [148] does not support a major effect of MUC16 on overall survival in ovarian cancer patients (Figure 6). No correlation is observed between MUC16 expression and resistance to chemotherapy in the ovarian cancer cohorts. Of the patients on whom MUC16 data has been deposited in TCGA, mutations in the mucin were identified in fifteen of 196 patients (Additional file 2). Patients with mutated MUC16 had a slightly lower survival than patients with wild-type MUC16; however the difference was not statistically significant (Figure 6).
Figure 6.
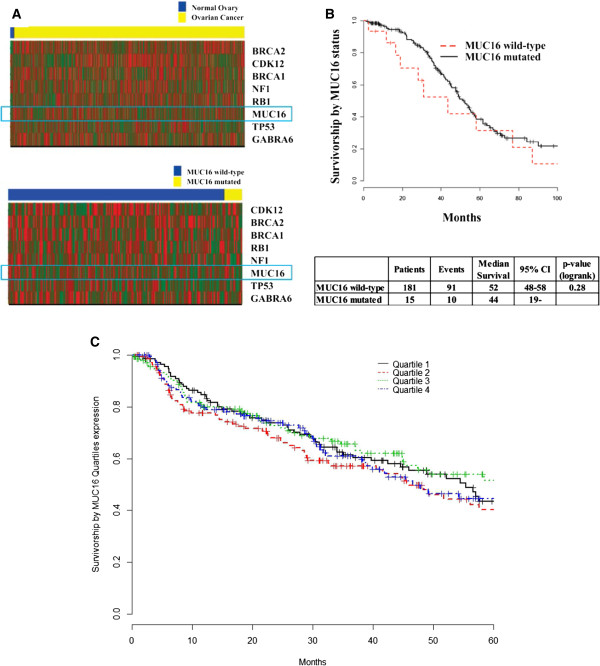
Analysis of data on MUC16 available through TCGA analysis of ovarian cancer samples. A TCGA data set [148] was analyzed to determine differential expression of prominent cancer-related genes between normal ovarian tissue and ovarian carcinoma (heat map in top panel). Although MUC16 is upregulated in the cancer samples (expression in cancer specimens is double than in normal) this difference is not significant (p-value = 0.1), probably because there were only 8 normal samples in TCGA dataset. MUC16 is compared to other prominent mutated genes reported in the original TCGA report [148]. Of these genes, only BRCA2 is differentially expressed between normal and cancer (p-value <0.001) samples. Analysis of mutated and wild-type MUC16 expression in samples from ovarian cancer patients listed in TCGA is shown in the heat map in the lower panel. Mutated MUC16 is also mildly over-expressed as compared to wild-type mucin (expression Wild-type/Mutated = 0.94), however this difference is not significant (p-value = 0.84). MUC16 is compared to other genes reported to be highly mutated at the original report of TCGA. None of the other genes is differentially expressed between MUC16-wild-type and MUC16-mutated ovarian cancer specimens, indicating no association between MUC16 mutation status and key genes expression in this dataset (p-value <0.05). B, Survival of ovarian cancer patients with wild-type and mutated MUC16 was compared. Although a trend was observed suggesting worse outcome in patients with mutated MUC16, the difference was not statistically significant (p-value = 0.28). C, MUC16 (both mutated and wild-type) expression was divided into quartiles. Survival of patients in each of these quartiles was not significantly different.
MUC16 as a target for therapy
The lack of significant effect of MUC16 observed in our analysis of TCGA data is inconsistent with the effect of MUC16 observed in in vitro and in vivo studies with ovarian and breast cancer cells, described above, where the expression of this mucin was attenuated. This dichotomy may potentially arise from the fact that only eight healthy donor samples are reported in the TCGA database for ovarian cancer. We estimate that data from 40 individuals each in the healthy control and ovarian cancer group will be required to attain 90% power to demonstrate the effect of differential MUC16 gene expression on patient survival. If no correlation between MUC16 expression and survival is demonstrated in a larger study, an intriguing possibility that will have to be considered is that MUC16 may be a factor whose presence (in terms of biological significance) is felt only by its absence (as shown by the knockdown experiments). If true, this model suggests that significant effect on ovarian tumors may be achieved by the application of small molecule agents and other strategies for in vivo knockdown of MUC16 or inhibition of its biological function. In this scenario, tumors will be subject to increased apoptosis, decreased proliferation, increased sensitivity to chemotherapy, and reduced efficiency in subverting innate immune responses and immunotherapeutic agents. In this context it is interesting to note that microRNA-200c regulates expression of both MUC4 and MUC16 [149].
MUC16 as a target for immunotherapy
Anti-mesothelin antibodies that interfere with mesothelin-MUC16 binding have been developed as immunotherapeutic agents [150-153]. A novel immunoadhesin, HN125, contains the MUC16 binding epitope of mesothelin fused to the Fc portion of human IgG1 antibody has been developed [154,155]. However, additional work is required to increase the potency of HN125 to produce a stronger anti-cancer response.
Oregovomab and Abgovomab are two antibodies developed for ovarian cancer immunotherapy. Oregovomab, (B43.13, OVAREX) is a mouse anti-MUC16 antibody developed for the in vivo detection of ovarian tumors [156]. A retrospective analysis of results trials designed to test the use of B43.13 as an imaging agent suggested increased survival in patients developing a human anti-mouse antibody (HAMA) response [157]. Repeated administration of the anti-CA125 antibodies results in increased anti-tumor T cell responses and the generation of anti-idiotypic antibodies [158-165]. These positive results led to the testing of Oregovomab in larger clinical trials in ovarian cancer patients [166,167]. Overall the results of these trials were disappointing as no benefit of Oregovomab was observed.
Abgovomab has met a similar fate in clinical trials. Abgovomab is an anti-idiotype antibody that was developed as a targeting agent against MUC16 [168-172]. Here again, clinical trials showed no difference in the overall survival of ovarian cancer patients as compared to patients in the control arm of the study [173-176].
One potential reason for Oregovomab and Abgovomab being unsuccessful in inhibiting tumor growth is that these antibodies may conjugate with the circulating ectodomain of MUC16 reducing the amount of antibody available to target the cancer cells. Additionally, shedding of the ectodomain may release the antibodies bound to the cell surface associated mucin. The rate at which the ectodomain is shed and the factors controlling the proteolysis of MUC16 are not clearly defined. It will be interesting to determine the efficacy of treatment regimens that combine anti-MUC16 antibodies with agents that can inhibit MUC16 release in controlling the growth of ovarian tumors.
Targeting MUC16 with antibody-drug conjugates
Two anti-MUC16 antibodies, 3A5 and 11D10, were developed and conjugated to the cytotoxic drug Monomethyl auristatin E (MMAE). 3A5 targets MUC16 tandem repeats and is more effective than 11D10 in delivering MMAE to cancer cells and inducing cell death. The 3A5-MMAE conjugate (now referred to as DMUC5754A) is being tested in a Phase I clinical trial. Twenty two of the 44 patients recruited in this trial received DMUC5754A [177]. The antibody drug conjugate produced minimal toxicity and, importantly, one patient showed complete response and five patients experienced a reduction in tumor. These results are encouraging and support further development of MUC16-targeted therapies for cancer.
Conclusion
Recent studies on MUC16 indicate that this mucin is not only important because it contains the biomarker CA125 but also for its role in contributing to ovarian tumor growth and metastasis. The complex biochemical structure of this mucin continues to provide major challenges to efforts being undertaken to make improvements to the CA125 assay and to understand the biological role of MUC16. The complexity of this antigen however also provides multiple opportunities that can be exploited to develop a test that can monitor this mucin even at low concentrations and, as the encouraging results with DMUC5754A suggest, developing novel anti-cancer therapeutic strategies. A sustained and systematic effort will be required to fully understand and exploit MUC16 to realize a benefit for patients with ovarian and other malignancies.
Abbreviations
CA125: Cancer Antigen 125; MMAE: Monomethyl Auristatin E; MUC16: Mucin 16; NK: Natural killer cells; PLCO: Prostate, lung, colorectal and ovarian cancer; RMI: Risk of malignancy index; ROCA: Risk of ovarian cancer algorithm; ROMA: Risk of ovarian malignancy algorithm; SEA: Sea urchin Enterokinase and Agrin; TCGA: The cancer genome atlas; UKCTOCS: United Kingdom Collaborative Trial of Ovarian Cancer Screening.
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
MF conducted the flow cytometry experiments; AK conducted flow cytometry experiments and MUC16 mutation analysis; JGB conducted the TCGA data analysis and helped with writing of the manuscript; SH, JH and RA helped with obtaining the electron microscopy data; LF and JK conducted MUC16 mutation analysis; KH helped with the analysis of antibody binding to CA125 peptides; HS assisted in the writing of the manuscript; RJW and MSP conceptualized the idea for this review and wrote the manuscript. All authors read and approved the final manuscript.
Supplementary Material
BLAST analysis showing location of SEA domains in each of the repeat and the C-terminal domain of MUC16.
MUC16 mutations listed in TCGA data on ovarain cancer samples.
Contributor Information
Mildred Felder, Email: mfelder@wisc.edu.
Arvinder Kapur, Email: akaur@wisc.edu.
Jesus Gonzalez-Bosquet, Email: jesus.gonzalezbosquet@gmail.com.
Sachi Horibata, Email: sh744@cornell.edu.
Joseph Heintz, Email: jheintz@wisc.edu.
Ralph Albrecht, Email: Albrecht@ansci.wisc.edu.
Lucas Fass, Email: lfass@wisc.edu.
Justanjyot Kaur, Email: jkaur4@wisc.edu.
Kevin Hu, Email: hukevinxiaochen@gmail.com.
Hadi Shojaei, Email: hshojaei@wisc.edu.
Rebecca J Whelan, Email: rwhelan@oberlin.edu.
Manish S Patankar, Email: patankar@wisc.edu.
Acknowledgements
We sincerely thank Drs. Ryan Bailey and Adam Washburn for their help with antibody-peptide binding assays. Funding for this research was provided by grants from the National Institutes of Health (1R21CA143616-01 and 1R41CA132520-01A2), Department of Defense (W81XWH-04-1-0102), and the Department of Obstetrics and Gynecology to MSP, charitable donation from Jean McKenzie, and research grants from the Wisconsin Ovarian Cancer Alliance to MSP. Funding was also provided by a grant from the National Institutes of Health (1R15CA161970-01), grants from the Camille and Henry Dreyfus Foundation, Research Corporation, and an Oberlin-Kalamazoo-University of Michigan (OKUM) faculty exchange grant to RJW. We are deeply grateful to Dagna Sheerar (University of Wisconsin-Madison Paul P. Carbone Comprehensive Cancer Center, Flow Cytometry Facility) for advice and assistance with the flow cytometry assays. We also acknowledge the support provided by the University of Wisconsin Comprehensive Cancer Centers Flow Cytometry facility which is supported by a core grant (CA14520) from the National Institutes of Health.
References
- Duffy MJ, Bonfrer JM, Kulpa J, Rustin GJ, Soletormos G, Torre GC, Tuxen MK, Zwirner M. CA125 in ovarian cancer: European group on tumor markers guidelines for clinical use. Int J Gynecol Cancer. 2005;15:679–691. doi: 10.1111/j.1525-1438.2005.00130.x. [DOI] [PubMed] [Google Scholar]
- Sturgeon CM, Duffy MJ, Stenman UH, Lilja H, Brunner N, Chan DW, Babaian R, Bast RC Jr, Dowell B, Esteva FJ, Haglund C, Harbeck N, Hayes DF, Holten-Andersen M, Klee GG, Lamerz R, Looijenga LH, Molina R, Nielsen HJ, Rittenhouse H, Semjonow A, Shih Ie M, Sibley P, Soletormos G, Stephan C, Sokoll L, Hoffman BR, Diamandis EP. National Academy of Clinical Biochemistry laboratory medicine practice guidelines for use of tumor markers in testicular, prostate, colorectal, breast, and ovarian cancers. Clin Chem. 2008;54:e11–e79. doi: 10.1373/clinchem.2008.105601. [DOI] [PubMed] [Google Scholar]
- Seltzer V, Drukker BH, Gillespie BW, Gossfeld LM, Grigsby PW, Harvey HA, Hendricks CB, Hummel S, Makuch RW, Monaco GP, Parham GP, Sawyers CL, West RJ, Alberts DS, Anderson B, Averette HE, Bast RC, Christian MC, Colombo N, Creasman WT, John P, Curtin JP, Gershenson DM, Hoskins WJ, Karlan BY, Kramer BS, Markman M, McGuire WP, Ozols RF, Pecorelli S. et al. NIH consensus conference: ovarian cancer: screening, treatment, and follow-up. NIH consensus development panel on ovarian cancer. JAMA. 1995;273:491–497. doi: 10.1001/jama.1995.03520300065039. [DOI] [PubMed] [Google Scholar]
- Rustin GJ, Quinn M, Thigpen T, du Bois A, Pujade-Lauraine E, Jakobsen A, Eisenhauer E, Sagae S, Greven K, Vergote I, Cervantes A, Vermorken J. Re: new guidelines to evaluate the response to treatment in solid tumors (ovarian cancer) J Natl Cancer Inst. 2004;96:487–488. doi: 10.1093/jnci/djh081. [DOI] [PubMed] [Google Scholar]
- Vasudev NS, Trigonis I, Cairns DA, Hall GD, Jackson DP, Broadhead T, Buxton J, Hutson R, Nugent D, Perren TJ. The prognostic and predictive value of CA-125 regression during neoadjuvant chemotherapy for advanced ovarian or primary peritoneal carcinoma. Arch Gynecol Obstet. 2011;284:221–227. doi: 10.1007/s00404-010-1655-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rustin GJ. Follow-up with CA125 after primary therapy of advanced ovarian cancer has major implications for treatment outcome and trial performances and should not be routinely performed. Ann Oncol. 2011;22(Suppl 8):viii45–viii48. doi: 10.1093/annonc/mdr471. [DOI] [PubMed] [Google Scholar]
- Herzog TJ, Vermorken JB, Pujade-Lauraine E, Provencher DM, Jagiello-Gruszfeld A, Kong B, Boman K, Park YC, Parekh T, Lebedinsky C, Gomez J, Monk BJ. Correlation between CA-125 serum level and response by RECIST in a phase III recurrent ovarian cancer study. Gynecol Oncol. 2011;122:350–355. doi: 10.1016/j.ygyno.2011.04.005. [DOI] [PubMed] [Google Scholar]
- Miller RE, Rustin GJ. How to follow-up patients with epithelial ovarian cancer. Curr Opin Oncol. 2010;22:498–502. doi: 10.1097/CCO.0b013e32833ae8b6. [DOI] [PubMed] [Google Scholar]
- Gossner G, Coleman RL, Mutch DG, Horowitz NS, Rader JS, Gibb RK, Powell MA, Herzog TJ. CA-125 response in patients with recurrent ovarian or primary peritoneal cancer treated with pegylated liposomal doxorubicin or topotecan. Gynecol Oncol. 2006;103:212–218. doi: 10.1016/j.ygyno.2006.02.026. [DOI] [PubMed] [Google Scholar]
- Guppy AE, Nathan PD, Rustin GJ. Epithelial ovarian cancer: a review of current management. Clin Oncol (R Coll Radiol) 2005;17:399–411. doi: 10.1016/j.clon.2005.05.009. [DOI] [PubMed] [Google Scholar]
- Bridgewater JA, Nelstrop AE, Rustin GJ, Gore ME, McGuire WP, Hoskins WJ. Comparison of standard and CA-125 response criteria in patients with epithelial ovarian cancer treated with platinum or paclitaxel. J Clin Oncol. 1999;17:501–508. doi: 10.1200/JCO.1999.17.2.501. [DOI] [PubMed] [Google Scholar]
- Rustin G, Tuxen M. Use of CA 125 in follow-up of ovarian cancer. Lancet. 1996;348:191–192. doi: 10.1016/s0140-6736(05)66133-8. [DOI] [PubMed] [Google Scholar]
- Bast RC Jr, Feeney M, Lazarus H, Nadler LM, Colvin RB, Knapp RC. Reactivity of a monoclonal antibody with human ovarian carcinoma. J Clin Invest. 1981;68:1331–1337. doi: 10.1172/JCI110380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bast RC Jr, Klug TL, St John E, Jenison E, Niloff JM, Lazarus H, Berkowitz RS, Leavitt T, Griffiths CT, Parker L, Zurawski VR Jr, Knapp RC. A radioimmunoassay using a monoclonal antibody to monitor the course of epithelial ovarian cancer. N Engl J Med. 1983;309:883–887. doi: 10.1056/NEJM198310133091503. [DOI] [PubMed] [Google Scholar]
- Kabawat SE, Bast RC Jr, Bhan AK, Welch WR, Knapp RC, Colvin RB. Tissue distribution of a coelomic-epithelium-related antigen recognized by the monoclonal antibody OC125. Int J Gynecol Pathol. 1983;2:275–285. doi: 10.1097/00004347-198303000-00005. [DOI] [PubMed] [Google Scholar]
- Kabawat SE, Bast RC, Welch WR, Knapp RC, Colvin RB. Immunopathologic characterization of a monoclonal antibody that recognizes common surface antigens of human ovarian tumors of serous, endometrioid, and clear cell types. Am J Clin Pathol. 1983;79:98–104. doi: 10.1093/ajcp/79.1.98. [DOI] [PubMed] [Google Scholar]
- Niloff JM, Knapp RC, Schaetzl E, Reynolds C, Bast RC Jr. CA125 antigen levels in obstetric and gynecologic patients. Obstet Gynecol. 1984;64:703–707. [PubMed] [Google Scholar]
- Bast RC Jr, Xu FJ, Yu YH, Barnhill S, Zhang Z, Mills GB. CA 125: the past and the future. Int J Biol Markers. 1998;13:179–187. doi: 10.1177/172460089801300402. [DOI] [PubMed] [Google Scholar]
- Fritsche HA, Bast RC. CA 125 in ovarian cancer: advances and controversy. Clin Chem. 1998;44:1379–1380. [PubMed] [Google Scholar]
- O'Brien TJ, Tanimoto H, Konishi I, Gee M. More than 15 years of CA 125: what is known about the antigen, its structure and its function. Int J Biol Markers. 1998;13:188–195. doi: 10.1177/172460089801300403. [DOI] [PubMed] [Google Scholar]
- O'Brien TJ, Beard JB, Underwood LJ, Dennis RA, Santin AD, York L. The CA 125 gene: an extracellular superstructure dominated by repeat sequences. Tumour Biol. 2001;22:348–366. doi: 10.1159/000050638. [DOI] [PubMed] [Google Scholar]
- Yin BW, Lloyd KO. Molecular cloning of the ca125 ovarian cancer antigen. identification as a new mucin, muc16. J Biol Chem. 2001;276:27371–27375. doi: 10.1074/jbc.M103554200. [DOI] [PubMed] [Google Scholar]
- Rump A, Morikawa Y, Tanaka M, Minami S, Umesaki N, Takeuchi M, Miyajima A. Binding of ovarian cancer antigen CA125/MUC16 to mesothelin mediates cell adhesion. J Biol Chem. 2004;279:9190–9198. doi: 10.1074/jbc.M312372200. [DOI] [PubMed] [Google Scholar]
- Hattrup CL, Gendler SJ. Structure and function of the cell surface (Tethered) Mucins. Annu Rev Physiol. 2007;70:431–457. doi: 10.1146/annurev.physiol.70.113006.100659. [DOI] [PubMed] [Google Scholar]
- Comamala M, Pinard M, Theriault C, Matte I, Albert A, Boivin M, Beaudin J, Piche A, Rancourt C. Downregulation of cell surface CA125/MUC16 induces epithelial-to-mesenchymal transition and restores EGFR signalling in NIH:OVCAR3 ovarian carcinoma cells. Br J Cancer. 2011;104:989–999. doi: 10.1038/bjc.2011.34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bast RC Jr, Spriggs DR. More than a biomarker: CA125 may contribute to ovarian cancer pathogenesis. Gynecol Oncol. 2011;121:429–430. doi: 10.1016/j.ygyno.2011.04.032. [DOI] [PubMed] [Google Scholar]
- Skates SJ, Xu FJ, Yu YH, Sjovall K, Einhorn N, Chang Y, Bast RC Jr, Knapp RC. Toward an optimal algorithm for ovarian cancer screening with longitudinal tumor markers. Cancer. 1995;76:2004–2010. doi: 10.1002/1097-0142(19951115)76:10+<2004::AID-CNCR2820761317>3.0.CO;2-G. [DOI] [PubMed] [Google Scholar]
- Skates SJ, Pauler D, Jacobs I. Screening based on the risk of cancer calculation from Bayesian heirarchical changepoint and mixture models of longitudinal markers. J. 2001;96:429–439. doi: 10.1198/016214501753168145. [DOI] [Google Scholar]
- Einhorn N, Bast R, Knapp R, Nilsson B, Zurawski V Jr, Sjovall K. Long-term follow-up of the Stockholm screening study on ovarian cancer. Gynecol Oncol. 2000;79:466–470. doi: 10.1006/gyno.2000.5983. [DOI] [PubMed] [Google Scholar]
- Einhorn N, Sjovall K, Knapp RC, Hall P, Scully RE, Bast RC Jr, Zurawski VR Jr. Prospective evaluation of serum CA 125 levels for early detection of ovarian cancer. Obstet Gynecol. 1992;80:14–18. [PubMed] [Google Scholar]
- Jacobs I, Davies AP, Bridges J, Stabile I, Fay T, Lower A, Grudzinskas JG, Oram D. Prevalence screening for ovarian cancer in postmenopausal women by CA 125 measurement and ultrasonography. BMJ. 1993;306:1030–1034. doi: 10.1136/bmj.306.6884.1030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buys SS, Partridge E, Black A, Johnson CC, Lamerato L, Isaacs C, Reding DJ, Greenlee RT, Yokochi LA, Kessel B, Crawford ED, Church TR, Andriole GL, Weissfeld JL, Fouad MN, Chia D, O'Brien B, Ragard LR, Clapp JD, Rathmell JM, Riley TL, Hartge P, Pinsky PF, Zhu CS, Izmirlian G, Kramer BS, Miller AB, Xu JL, Prorok PC, Gohagan JK. et al. Effect of screening on ovarian cancer mortality: the Prostate, Lung, Colorectal and Ovarian (PLCO) Cancer Screening Randomized Controlled Trial. JAMA. 2011;305:2295–2303. doi: 10.1001/jama.2011.766. [DOI] [PubMed] [Google Scholar]
- Partridge E, Kreimer AR, Greenlee RT, Williams C, Xu JL, Church TR, Kessel B, Johnson CC, Weissfeld JL, Isaacs C, Andriole GL, Ogden S, Ragard LR, Buys SS, Team PP. Results from four rounds of ovarian cancer screening in a randomized trial. Obstet Gynecol. 2009;113:775–782. doi: 10.1097/AOG.0b013e31819cda77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buys SS, Partridge E, Greene MH, Prorok PC, Reding D, Riley TL, Hartge P, Fagerstrom RM, Ragard LR, Chia D, Izmirlian G, Fouad M, Johnson CC, Gohagan JK, Team PP. Ovarian cancer screening in the Prostate, Lung, Colorectal and Ovarian (PLCO) cancer screening trial: findings from the initial screen of a randomized trial. Am J Obstet Gynecol. 2005;193:1630–1639. doi: 10.1016/j.ajog.2005.05.005. [DOI] [PubMed] [Google Scholar]
- Pinsky PF, Zhu C, Skates SJ, Black A, Partridge E, Buys SS, Berg CD. Potential effect of the risk of ovarian cancer algorithm (ROCA) on the mortality outcome of the Prostate, Lung, Colorectal and Ovarian (PLCO) trial. Int J Cancer. 2013;132:2127–2133. doi: 10.1002/ijc.27909. [DOI] [PubMed] [Google Scholar]
- Urban N. Screening for ovarian cancer: We now need a definitive randomised trial. BMJ. 1999;319:1317–1318. doi: 10.1136/bmj.319.7221.1317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Menon U, Gentry-Maharaj A, Ryan A, Sharma A, Burnell M, Hallett R, Lewis S, Lopez A, Godfrey K, Oram D, Herod J, Williamson K, Seif M, Scott I, Mould T, Woolas R, Murdoch J, Dobbs S, Amso N, Leeson S, Cruickshank D, McGuire A, Campbell S, Fallowfield L, Skates S, Parmar M, Jacobs I. Recruitment to multicentre trials–lessons from UKCTOCS: descriptive study. BMJ. 2008;337:a2079. doi: 10.1136/bmj.a2079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Menon U, Gentry-Maharaj A, Hallett R, Ryan A, Burnell M, Sharma A, Lewis S, Davies S, Philpott S, Lopes A, Godfrey K, Oram D, Herod J, Williamson K, Seif MW, Scott I, Mould T, Woolas R, Murdoch J, Dobbs S, Amso NN, Leeson S, Cruickshank D, McGuire A, Campbell S, Fallowfield L, Singh N, Dawnay A, Skates SJ, Parmar M. et al. Sensitivity and specificity of multimodal and ultrasound screening for ovarian cancer, and stage distribution of detected cancers: results of the prevalence screen of the UK Collaborative Trial of Ovarian Cancer Screening (UKCTOCS) Lancet Oncol. 2009;10:327–340. doi: 10.1016/S1470-2045(09)70026-9. [DOI] [PubMed] [Google Scholar]
- Menon U, Kalsi J, Jacobs I. The UKCTOCS experience–reasons for hope? Int J Gynecol Cancer. 2012;22(Suppl 1):S18–S20. doi: 10.1097/IGC.0b013e318251cb47. [DOI] [PubMed] [Google Scholar]
- van der Burg ME, Lammes FB, Verweij J. The role of CA 125 and conventional examinations in diagnosing progressive carcinoma of the ovary. Surg Gynecol Obstet. 1993;176:310–314. [PubMed] [Google Scholar]
- van der Burg ME, Lammes FB, Verweij J. CA 125 in ovarian cancer. Neth J Med. 1992;40:36–51. [PubMed] [Google Scholar]
- van der Burg ME, Lammes FB, Verweij J. The role of CA 125 in the early diagnosis of progressive disease in ovarian cancer. Ann Oncol. 1990;1:301–302. doi: 10.1093/oxfordjournals.annonc.a057754. [DOI] [PubMed] [Google Scholar]
- Tholander B, Taube A, Lindgren A, Sjoberg O, Stendahl U, Tamsen L. Pretreatment serum levels of CA-125, carcinoembryonic antigen, tissue polypeptide antigen, and placental alkaline phosphatase in patients with ovarian carcinoma: influence of histological type, grade of differentiation, and clinical stage of disease. Gynecol Oncol. 1990;39:26–33. doi: 10.1016/0090-8258(90)90394-Z. [DOI] [PubMed] [Google Scholar]
- Jacobs I, Oram D, Fairbanks J, Turner J, Frost C, Grudzinskas JG. A risk of malignancy index incorporating CA 125, ultrasound and menopausal status for the accurate preoperative diagnosis of ovarian cancer. Br J Obstet Gynaecol. 1990;97:922–929. doi: 10.1111/j.1471-0528.1990.tb02448.x. [DOI] [PubMed] [Google Scholar]
- Moore RG, Miller MC, Disilvestro P, Landrum LM, Gajewski W, Ball JJ, Skates SJ. Evaluation of the diagnostic accuracy of the risk of ovarian malignancy algorithm in women with a pelvic mass. Obstet Gynecol. 2011;118:280–288. doi: 10.1097/AOG.0b013e318224fce2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore RG, McMeekin DS, Brown AK, DiSilvestro P, Miller MC, Allard WJ, Gajewski W, Kurman R, Bast RC Jr, Skates SJ. A novel multiple marker bioassay utilizing HE4 and CA125 for the prediction of ovarian cancer in patients with a pelvic mass. Gynecol Oncol. 2009;112:40–46. doi: 10.1016/j.ygyno.2008.08.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore RG, Brown AK, Miller MC, Skates S, Allard WJ, Verch T, Steinhoff M, Messerlian G, DiSilvestro P, Granai CO, Bast RC Jr. The use of multiple novel tumor biomarkers for the detection of ovarian carcinoma in patients with a pelvic mass. Gynecol Oncol. 2008;108:402–408. doi: 10.1016/j.ygyno.2007.10.017. [DOI] [PubMed] [Google Scholar]
- Hellstrom I, Raycraft J, Hayden-Ledbetter M, Ledbetter JA, Schummer M, McIntosh M, Drescher C, Urban N, Hellstrom KE. The HE4 (WFDC2) protein is a biomarker for ovarian carcinoma. Cancer Res. 2003;63:3695–3700. [PubMed] [Google Scholar]
- Simmons AR, Baggerly K, Bast RC Jr. The emerging role of HE4 in the evaluation of epithelial ovarian and endometrial carcinomas. Oncology (Williston Park) 2013;27:548–556. [PMC free article] [PubMed] [Google Scholar]
- Bast RC Jr, Skates S, Lokshin A, Moore RG. Differential diagnosis of a pelvic mass: improved algorithms and novel biomarkers. Int J Gynecol Cancer. 2012;22(Suppl 1):S5–S8. doi: 10.1097/IGC.0b013e318251c97d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu CS, Pinsky PF, Cramer DW, Ransohoff DF, Hartge P, Pfeiffer RM, Urban N, Mor G, Bast RC Jr, Moore LE, Lokshin AE, McIntosh MW, Skates SJ, Vitonis A, Zhang Z, Ward DC, Symanowski JT, Lomakin A, Fung ET, Sluss PM, Scholler N, Lu KH, Marrangoni AM, Patriotis C, Srivastava S, Buys SS, Berg CD. A framework for evaluating biomarkers for early detection: validation of biomarker panels for ovarian cancer. Cancer Prev Res (Phila) 2011;4:375–383. doi: 10.1158/1940-6207.CAPR-10-0193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cramer DW, Bast RC Jr, Berg CD, Diamandis EP, Godwin AK, Hartge P, Lokshin AE, Lu KH, McIntosh MW, Mor G, Patriotis C, Pinsky PF, Thornquist MD, Scholler N, Skates SJ, Sluss PM, Srivastava S, Ward DC, Zhang Z, Zhu CS, Urban N. Ovarian cancer biomarker performance in prostate, lung, colorectal, and ovarian cancer screening trial specimens. Cancer Prev Res (Phila) 2011;4:365–374. doi: 10.1158/1940-6207.CAPR-10-0195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobs I, Menon U. The sine qua non of discovering novel biomarkers for early detection of ovarian cancer: carefully selected preclinical samples. Cancer Prev Res (Phila) 2011;4:299–302. doi: 10.1158/1940-6207.CAPR-11-0048. [DOI] [PubMed] [Google Scholar]
- Diamandis EP, Bast RC Jr, Gold P, Chu TM, Magnani JL. Reflection on the discovery of carcinoembryonic antigen, prostate-specific antigen, and cancer antigens CA125 and CA19-9. Clin Chem. 2013;59:22–31. doi: 10.1373/clinchem.2012.187047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niloff JM, Klug TL, Schaetzl E, Zurawski VR Jr, Knapp RC, Bast RC Jr. Elevation of serum CA125 in carcinomas of the fallopian tube, endometrium, and endocervix. Am J Obstet Gynecol. 1984;148:1057–1058. doi: 10.1016/s0002-9378(84)90444-7. [DOI] [PubMed] [Google Scholar]
- O'Brien TJ, Raymond LM, Bannon GA, Ford DH, Hardardottir H, Miller FC, Quirk JG Jr. New monoclonal antibodies identify the glycoprotein carrying the CA 125 epitope. Am J Obstet Gynecol. 1991;165:1857–1864. doi: 10.1016/0002-9378(91)90046-t. [DOI] [PubMed] [Google Scholar]
- Lloyd KO, Yin BW, Kudryashov V. Isolation and characterization of ovarian cancer antigen CA 125 using a new monoclonal antibody (VK-8): identification as a mucin-type molecule. Int J Cancer. 1997;71:842–850. doi: 10.1002/(SICI)1097-0215(19970529)71:5<842::AID-IJC24>3.0.CO;2-8. [DOI] [PubMed] [Google Scholar]
- Nap M, Vitali A, Nustad K, Bast RC Jr, O'Brien TJ, Nilsson O, Seguin P, Suresh MR, Bormer OP, Saga T, de Bruijn HW, Nozawa S, Kreutz FT, Jette D, Sakahara H, Gadnell M, Endo K, Barlow EH, Warren D, Paus E, Hammarstrom S, Kenemans P, Hilgers J. Immunohistochemical characterization of 22 monoclonal antibodies against the CA125 antigen: 2nd report from the ISOBM TD-1 Workshop. Tumour Biol. 1996;17:325–331. [PubMed] [Google Scholar]
- Nustad K, Bast RC Jr, Brien TJ, Nilsson O, Seguin P, Suresh MR, Saga T, Nozawa S, Bormer OP, de Bruijn HW, Nap M, Vitali A, Gadnell M, Clark J, Shigemasa K, Karlsson B, Kreutz FT, Jette D, Sakahara H, Endo K, Paus E, Warren D, Hammarstrom S, Kenemans P, Hilgers J. Specificity and affinity of 26 monoclonal antibodies against the CA 125 antigen: first report from the ISOBM TD-1 workshop: International Society for Oncodevelopmental Biology and Medicine. Tumour Biol. 1996;17:196–219. doi: 10.1159/000217982. [DOI] [PubMed] [Google Scholar]
- Nustad K, Lebedin Y, Lloyd KO, Shigemasa K, de Bruijn HW, Jansson B, Nilsson O, Olsen KH, O'Brien TJ. Epitopes on CA 125 from cervical mucus and ascites fluid and characterization of six new antibodies. Third report from the ISOBM TD-1 workshop. Tumour Biol. 2002;23:303–314. doi: 10.1159/000068570. [DOI] [PubMed] [Google Scholar]
- Warren DJ, Nustad K, Beard JB, O'Brien TJ. Expression and epitope characterization of a recombinant CA 125 repeat: fourth report from the ISOBM TD-1 workshop. Tumour Biol. 2009;30:51–60. doi: 10.1159/000209988. [DOI] [PubMed] [Google Scholar]
- O'Brien TJ, Hardin JW, Bannon GA, Norris JS, Quirk JG Jr. CA 125 antigen in human amniotic fluid and fetal membranes. Am J Obstet Gynecol. 1986;155:50–55. doi: 10.1016/0002-9378(86)90076-1. [DOI] [PubMed] [Google Scholar]
- Hanisch FG, Uhlenbruck G, Peter-Katalinic J, Egge H. Structural studies on oncofetal carbohydrate antigens (Ca 19–9, Ca 50, and Ca 125) carried by O-linked sialyloligosaccharides on human amniotic mucins. Carbohydr Res. 1988;178:29–47. doi: 10.1016/0008-6215(88)80100-9. [DOI] [PubMed] [Google Scholar]
- Davis HM, Zurawski VR Jr, Bast RC Jr, Klug TL. Characterization of the CA 125 antigen associated with human epithelial ovarian carcinomas. Cancer Res. 1986;46:6143–6148. [PubMed] [Google Scholar]
- Van Lenten L, Ashwell G. Studies on the chemical and enzymatic modification of glycoproteins. A general method for the tritiation of sialic acid-containing glycoproteins. J Biol Chem. 1971;246:1889–1894. [PubMed] [Google Scholar]
- Ozgur K, Patankar MS, Oehninger S, Clark GF. Direct evidence for the involvement of carbohydrate sequences in human sperm-zona pellucida binding. Mol Hum Reprod. 1998;4:318–324. doi: 10.1093/molehr/4.4.318. [DOI] [PubMed] [Google Scholar]
- Lloyd KO, Yin BW. Synthesis and secretion of the ovarian cancer antigen CA 125 by the human cancer cell line NIH:OVCAR-3. Tumour Biol. 2001;22:77–82. doi: 10.1159/000050600. [DOI] [PubMed] [Google Scholar]
- Quirk JG Jr, Brunson GL, Long CA, Bannon GA, Sanders MM, O'Brien TJ. CA 125 in tissues and amniotic fluid during pregnancy. Am J Obstet Gynecol. 1988;159:644–649. doi: 10.1016/s0002-9378(88)80026-7. [DOI] [PubMed] [Google Scholar]
- Hardardottir H, Parmley TH 2nd, Quirk JG Jr, Sanders MM, Miller FC, O'Brien TJ. Distribution of CA 125 in embryonic tissues and adult derivatives of the fetal periderm. Am J Obstet Gynecol. 1990;163:1925–1931. doi: 10.1016/0002-9378(90)90775-3. [DOI] [PubMed] [Google Scholar]
- Fendrick JL, Staley KA, Gee MK, McDougald SR, Quirk JG Jr, O'Brien TJ. Characterization of CA 125 synthesized by the human epithelial amnion WISH cell line. Tumour Biol. 1993;14:310–318. doi: 10.1159/000217844. [DOI] [PubMed] [Google Scholar]
- O'Brien TJ, Beard JB, Underwood LJ, Shigemasa K. The CA 125 gene: a newly discovered extension of the glycosylated N- terminal domain doubles the size of this extracellular superstructure. Tumour Biol. 2002;23:154–169. doi: 10.1159/000064032. [DOI] [PubMed] [Google Scholar]
- Yin BW, Dnistrian A, Lloyd KO. Ovarian cancer antigen CA125 is encoded by the MUC16 mucin gene. Int J Cancer. 2002;98:737–740. doi: 10.1002/ijc.10250. [DOI] [PubMed] [Google Scholar]
- Konishi I, Fendrick JL, Parmley TH, Quirk JG Jr, O'Brien TJ. Epidermal growth factor enhances secretion of the ovarian tumor- associated cancer antigen CA125 from the human amnion WISH cell line. J Soc Gynecol Investig. 1994;1:89–96. doi: 10.1177/107155769400100118. [DOI] [PubMed] [Google Scholar]
- Fendrick JL, Konishi I, Geary SM, Parmley TH, Quirk JG Jr, O'Brien TJ. CA125 phosphorylation is associated with its secretion from the WISH human amnion cell line. Tumour Biol. 1997;18:278–289. doi: 10.1159/000218041. [DOI] [PubMed] [Google Scholar]
- Bressan A, Bozzo F, Maggi CA, Binaschi M. OC125, M11 and OV197 epitopes are not uniformly distributed in the tandem-repeat region of CA125 and require the entire SEA domain. Dis Markers. 2013;34:257–267. doi: 10.1155/2013/917898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berman ZT, Moore LJ, Knudson KE, Whelan RJ. Synthesis and structural characterization of the peptide epitope of the ovarian cancer biomarker CA125 (MUC16) Tumour Biol. 2010;31:495–502. doi: 10.1007/s13277-010-0062-4. [DOI] [PubMed] [Google Scholar]
- Bork P, Patthy L. The SEA module: a new extracellular domain associated with O-glycosylation. Protein Sci. 1995;4:1421–1425. doi: 10.1002/pro.5560040716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maeda T, Inoue M, Koshiba S, Yabuki T, Aoki M, Nunokawa E, Seki E, Matsuda T, Motoda Y, Kobayashi A, Hiroyasu F, Shirouzu M, Terada T, Hayami N, Ishizuka Y, Shinya N, Tatsuguchi A, Yoshida M, Hirota H, Matsuo Y, Tani K, Arakawa T, Carninci P, Kawai J, Hayashizaki Y, Kigawa T, Yokoyama S. Solution structure of the SEA domain from the murine homologue of ovarian cancer antigen CA125 (MUC16) J Biol Chem. 2004;279:13174–13182. doi: 10.1074/jbc.M309417200. [DOI] [PubMed] [Google Scholar]
- Laver WG, Air GM, Webster RG, Smith-Gill SJ. Epitopes on protein antigens: misconceptions and realities. Cell. 1990;61:553–556. doi: 10.1016/0092-8674(90)90464-P. [DOI] [PubMed] [Google Scholar]
- Kui Wong N, Easton RL, Panico M, Sutton-Smith M, Morrison JC, Lattanzio FA, Morris HR, Clark GF, Dell A, Patankar MS. Characterization of the oligosaccharides associated with the human ovarian tumor marker CA125. J Biol Chem. 2003;278:28619–28634. doi: 10.1074/jbc.M302741200. [DOI] [PubMed] [Google Scholar]
- Chen K, Gentry-Maharaj A, Burnell M, Steentoft C, Marcos-Silva L, Mandel U, Jacobs I, Dawnay A, Menon U, Blixt O. Microarray Glycoprofiling of CA125 improves differential diagnosis of ovarian cancer. J Proteome Res. 2013;12:1408–1418. doi: 10.1021/pr3010474. [DOI] [PubMed] [Google Scholar]
- Akita K, Yoshida S, Ikehara Y, Shirakawa S, Toda M, Inoue M, Kitawaki J, Nakanishi H, Narimatsu H, Nakada H. Different levels of sialyl-Tn antigen expressed on MUC16 in patients with endometriosis and ovarian cancer. Int J Gynecol Cancer. 2012;22:531–538. doi: 10.1097/IGC.0b013e3182473292. [DOI] [PubMed] [Google Scholar]
- Saldova R, Struwe WB, Wynne K, Elia G, Duffy MJ, Rudd PM. Exploring the glycosylation of serum CA125. Int J Mol Sci. 2013;14:15636–15654. doi: 10.3390/ijms140815636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jankovic MM, Milutinovic BS. Glycoforms of CA125 antigen as a possible cancer marker. Cancer Biomark. 2008;4:35–42. doi: 10.3233/cbm-2008-4104. [DOI] [PubMed] [Google Scholar]
- Mitic N, Milutinovic B, Jankovic M. Assessment of sialic acid diversity in cancer- and non-cancer related CA125 antigen using sialic acid-binding Ig-like lectins (Siglecs) Dis Markers. 2012;32:187–194. doi: 10.1155/2012/309203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milutinovic B, Mitic N, Jankovic M. Identification of pregnancy-associated CA125-reactive protein as a carbohydrate-binding immunoglobulin G. Arch Biochem Biophys. 2010;499:69–76. doi: 10.1016/j.abb.2010.05.011. [DOI] [PubMed] [Google Scholar]
- Jankovic MM, Milutinovic BS. Pregnancy-associated CA125 antigen as mucin: evaluation of ferning morphology. Mol Hum Reprod. 2007;13:405–408. doi: 10.1093/molehr/gam022. [DOI] [PubMed] [Google Scholar]
- Jankovic MM, Tapuskovic BS. Molecular forms and microheterogeneity of the oligosaccharide chains of pregnancy-associated CA125 antigen. Hum Reprod. 2005;20:2632–2638. doi: 10.1093/humrep/dei095. [DOI] [PubMed] [Google Scholar]
- Wahrenbrock MG, Varki A. Multiple hepatic receptors cooperate to eliminate secretory mucins aberrantly entering the bloodstream: are circulating cancer mucins the “tip of the iceberg”? Cancer Res. 2006;66:2433–2441. doi: 10.1158/0008-5472.CAN-05-3851. [DOI] [PubMed] [Google Scholar]
- Chen Y, Clark S, Wong T, Chen Y, Chen Y, Dennis MS, Luis E, Zhong F, Bheddah S, Koeppen H, Gogineni A, Ross S, Polakis P, Mallet W. Armed antibodies targeting the mucin repeats of the ovarian cancer antigen, MUC16, are highly efficacious in animal tumor models. Cancer Res. 2007;67:4924–4932. doi: 10.1158/0008-5472.CAN-06-4512. [DOI] [PubMed] [Google Scholar]
- Dharma Rao T, Park KJ, Smith-Jones P, Iasonos A, Linkov I, Soslow RA, Spriggs DR. Novel monoclonal antibodies against the proximal (carboxy-terminal) portions of MUC16. Appl Immunohistochem Mol Morphol. 2010;18:462–472. doi: 10.1097/PAI.0b013e3181dbfcd2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kerschner JE. Mucin gene expression in human middle ear epithelium. Laryngoscope. 2007;117:1666–1676. doi: 10.1097/MLG.0b013e31806db531. [DOI] [PubMed] [Google Scholar]
- Davies JR, Kirkham S, Svitacheva N, Thornton DJ, Carlstedt I. MUC16 is produced in tracheal surface epithelium and submucosal glands and is present in secretions from normal human airway and cultured bronchial epithelial cells. Int J Biochem Cell Biol. 2007;39:1943–1954. doi: 10.1016/j.biocel.2007.05.013. [DOI] [PubMed] [Google Scholar]
- Blalock TD, Spurr-Michaud SJ, Tisdale AS, Heimer SR, Gilmore MS, Ramesh V, Gipson IK. Functions of MUC16 in corneal epithelial cells. Invest Ophthalmol Vis Sci. 2007;48:4509–4518. doi: 10.1167/iovs.07-0430. [DOI] [PubMed] [Google Scholar]
- Hori Y, Spurr-Michaud SJ, Russo CL, Argueso P, Gipson IK. Effect of retinoic acid on gene expression in human conjunctival epithelium: secretory phospholipase A2 mediates retinoic acid induction of MUC16. Invest Ophthalmol Vis Sci. 2005;46:4050–4061. doi: 10.1167/iovs.05-0627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Argueso P, Spurr-Michaud S, Russo CL, Tisdale A, Gipson IK. MUC16 mucin is expressed by the human ocular surface epithelia and carries the H185 carbohydrate epitope. Invest Ophthalmol Vis Sci. 2003;44:2487–2495. doi: 10.1167/iovs.02-0862. [DOI] [PubMed] [Google Scholar]
- Govindarajan B, Gipson IK. Membrane-tethered mucins have multiple functions on the ocular surface. Exp Eye Res. 2010;90:655–663. doi: 10.1016/j.exer.2010.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duraisamy S, Ramasamy S, Kharbanda S, Kufe D. Distinct evolution of the human carcinoma-associated transmembrane mucins, MUC1, MUC4 AND MUC16. Gene. 2006;373:28–34. doi: 10.1016/j.gene.2005.12.021. [DOI] [PubMed] [Google Scholar]
- Govindarajan B, Menon BB, Spurr-Michaud S, Rastogi K, Gilmore MS, Argueso P, Gipson IK. A metalloproteinase secreted by Streptococcus pneumoniae removes membrane mucin MUC16 from the epithelial glycocalyx barrier. PLoS One. 2012;7:e32418. doi: 10.1371/journal.pone.0032418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blalock TD, Spurr-Michaud SJ, Tisdale AS, Gipson IK. Release of membrane-associated mucins from ocular surface epithelia. Invest Ophthalmol Vis Sci. 2008;49:1864–1871. doi: 10.1167/iovs.07-1081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Govindarajan B, Gipson IK. Membrane-tethered mucins have multiple functions on the ocular surface. Exp Eye Res. 2010;90:655–663. doi: 10.1016/j.exer.2010.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Argueso P, Tisdale A, Spurr-Michaud S, Sumiyoshi M, Gipson IK. Mucin characteristics of human corneal-limbal epithelial cells that exclude the rose bengal anionic dye. Invest Ophthalmol Vis Sci. 2006;47:113–119. doi: 10.1167/iovs.05-0735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Argueso P, Guzman-Aranguez A, Mantelli F, Cao Z, Ricciuto J, Panjwani N. Association of cell surface mucins with galectin-3 contributes to the ocular surface epithelial barrier. J Biol Chem. 2009;284:23037–23045. doi: 10.1074/jbc.M109.033332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheon DJ, Wang Y, Deng JM, Lu Z, Xiao L, Chen CM, Bast RC, Behringer RR. CA125/MUC16 is dispensable for mouse development and reproduction. PLoS One. 2009;4:e4675. doi: 10.1371/journal.pone.0004675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y, Cheon DJ, Lu Z, Cunningham SL, Chen CM, Luo RZ, Xing D, Orsulic S, Bast RC Jr, Behringer RR. MUC16 expression during embryogenesis, in adult tissues, and ovarian cancer in the mouse. Differentiation. 2008;76:1081–1092. doi: 10.1111/j.1432-0436.2008.00295.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gubbels JA, Felder M, Horibata S, Belisle JA, Kapur A, Holden H, Petrie S, Migneault M, Rancourt C, Connor JP, Patankar MS. MUC16 provides immune protection by inhibiting synapse formation between NK and ovarian tumor cells. Mol Cancer. 2010;9:11. doi: 10.1186/1476-4598-9-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis DM, Chiu I, Fassett M, Cohen GB, Mandelboim O, Strominger JL. The human natural killer cell immune synapse. Proc Natl Acad Sci U S A. 1999;96:15062–15067. doi: 10.1073/pnas.96.26.15062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orange JS. The lytic NK cell immunological synapse and sequential steps in its formation. Adv Exp Med Biol. 2007;601:225–233. doi: 10.1007/978-0-387-72005-0_23. [DOI] [PubMed] [Google Scholar]
- Mace EM, Orange JS. New views of the human NK cell immunological synapse: recent advances enabled by super- and high-resolution imaging techniques. Front Immunol. 2012;3:421. doi: 10.3389/fimmu.2012.00421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jentoft N. Why are proteins O-glycosylated? Trends Biochem Sci. 1990;15:291–294. doi: 10.1016/0968-0004(90)90014-3. [DOI] [PubMed] [Google Scholar]
- Komatsu M, Yee L, Carraway KL. Overexpression of sialomucin complex, a rat homologue of MUC4, inhibits tumor killing by lymphokine-activated killer cells. Cancer Res. 1999;59:2229–2236. [PubMed] [Google Scholar]
- Belisle JA, Horibata S, Gubbels JA, Petrie S, Kapur A, Andre S, Gabius HJ, Rancourt C, Connor J, Paulson JC, Patankar MS. Identification of Siglec-9 as the receptor for MUC16 on human NK cells, B cells, and monocytes. Mol Cancer. 2010;9:118. doi: 10.1186/1476-4598-9-118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lanier LL. Up on the tightrope: natural killer cell activation and inhibition. Nat Immunol. 2008;9:495–502. doi: 10.1038/ni1581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crocker PR, Clark EA, Filbin M, Gordon S, Jones Y, Kehrl JH, Kelm S, Le Douarin N, Powell L, Roder J, Schnaar RL, Sgroi DC, Stamenkovic K, Schauer R, Schachner M, van den Berg TK, van der Merwe PA, Watt SM, Varki A. Siglecs: a family of sialic-acid binding lectins [letter] Glycobiology. 1998;8:v. doi: 10.1093/oxfordjournals.glycob.a018832. [DOI] [PubMed] [Google Scholar]
- Angata T, Varki A. Siglec-7: a sialic acid-binding lectin of the immunoglobulin superfamily. Glycobiology. 2000;10:431–438. doi: 10.1093/glycob/10.4.431. [DOI] [PubMed] [Google Scholar]
- Zhang JQ, Nicoll G, Jones C, Crocker PR. Siglec-9, a novel sialic acid binding member of the immunoglobulin superfamily expressed broadly on human blood leukocytes. J Biol Chem. 2000;275:22121–22126. doi: 10.1074/jbc.M002788200. [DOI] [PubMed] [Google Scholar]
- Crocker PR, Varki A. Siglecs in the immune system. Immunology. 2001;103:137–145. doi: 10.1046/j.0019-2805.2001.01241.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Varki A, Angata T. Siglecs–the major subfamily of I-type lectins. Glycobiology. 2006;16:1R–27R. doi: 10.1093/glycob/cwj126. [DOI] [PubMed] [Google Scholar]
- Crocker PR, Paulson JC, Varki A. Siglecs and their roles in the immune system. Nat Rev Immunol. 2007;7:255–266. doi: 10.1038/nri2056. [DOI] [PubMed] [Google Scholar]
- Yamaji T, Teranishi T, Alphey MS, Crocker PR, Hashimoto Y. A small region of the natural killer cell receptor, Siglec-7, is responsible for its preferred binding to alpha2,8-disialyl and branched alpha2,6-sialyl residues: a comparison with Siglec-9. J Biol Chem. 2001;10:6324–6332. doi: 10.1074/jbc.M110146200. [DOI] [PubMed] [Google Scholar]
- Avril T, Floyd H, Lopez F, Vivier E, Crocker PR. The membrane-proximal immunoreceptor tyrosine-based inhibitory motif is critical for the inhibitory signaling mediated by Siglecs-7 and -9, CD33-related Siglecs expressed on human monocytes and NK cells. J Immunol. 2004;173:6841–6849. doi: 10.4049/jimmunol.173.11.6841. [DOI] [PubMed] [Google Scholar]
- Madsen CB, Lavrsen K, Steentoft C, Vester-Christensen MB, Clausen H, Wandall HH, Pedersen AE. Glycan elongation beyond the mucin associated tn antigen protects tumor cells from immune-mediated killing. PLoS One. 2013;8:e72413. doi: 10.1371/journal.pone.0072413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunn GP, Bruce AT, Ikeda H, Old LJ, Schreiber RD. Cancer immunoediting: from immunosurveillance to tumor escape. Nat Immunol. 2002;3:991–998. doi: 10.1038/ni1102-991. [DOI] [PubMed] [Google Scholar]
- Dunn GP, Old LJ, Schreiber RD. The immunobiology of cancer immunosurveillance and immunoediting. Immunity. 2004;21:137–148. doi: 10.1016/j.immuni.2004.07.017. [DOI] [PubMed] [Google Scholar]
- Dunn GP, Old LJ, Schreiber RD. The three Es of cancer immunoediting. Annu Rev Immunol. 2004;22:329–360. doi: 10.1146/annurev.immunol.22.012703.104803. [DOI] [PubMed] [Google Scholar]
- Tang Z, Qian M, Ho M. The role of mesothelin in tumor progression and targeted therapy. Anticancer Agents Med Chem. 2013;13:276–280. doi: 10.2174/1871520611313020014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen SH, Hung WC, Wang P, Paul C, Konstantopoulos K. Mesothelin binding to CA125/MUC16 promotes pancreatic cancer cell motility and invasion via MMP-7 activation. Sci Rep. 2013;3:1870. doi: 10.1038/srep01870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shimizu A, Hirono S, Tani M, Kawai M, Okada K, Miyazawa M, Kitahata Y, Nakamura Y, Noda T, Yokoyama S, Yamaue H. Coexpression of MUC16 and mesothelin is related to the invasion process in pancreatic ductal adenocarcinoma. Cancer Sci. 2012;103:739–746. doi: 10.1111/j.1349-7006.2012.02214.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higashi M, Yamada N, Yokoyama S, Kitamoto S, Tabata K, Koriyama C, Batra SK, Yonezawa S. Pathobiological implications of MUC16/CA125 expression in intrahepatic cholangiocarcinoma-mass forming type. Pathobiology. 2012;79:101–106. doi: 10.1159/000335164. [DOI] [PubMed] [Google Scholar]
- Gubbels JA, Belisle J, Onda M, Rancourt C, Migneault M, Ho M, Bera TK, Connor J, Sathyanarayana BK, Lee B, Pastan I, Patankar MS. Mesothelin-MUC16 binding is a high affinit: N-glycan dependent interaction that facilitates peritoneal metastasis of ovarian tumors. Mol Cancer. 2006;5:50. doi: 10.1186/1476-4598-5-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scholler N, Garvik B, Hayden-Ledbetter M, Kline T, Urban N. Development of a CA125-mesothelin cell adhesion assay as a screening tool for biologics discovery. Cancer Lett. 2006;247:130–136. doi: 10.1016/j.canlet.2006.03.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sathyanarayana BK, Hahn Y, Patankar MS, Pastan I, Lee B. Mesothelin, Stereocilin, and Otoancorin are predicted to have superhelical structures with ARM-type repeats. BMC Struct Biol. 2009;9:1. doi: 10.1186/1472-6807-9-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hassan R, Schweizer C, Lu KF, Schuler B, Remaley AT, Weil SC, Pastan I. Inhibition of mesothelin-CA-125 interaction in patients with mesothelioma by the anti-mesothelin monoclonal antibody MORAb-009: Implications for cancer therapy. Lung Cancer. 2010;68:455–459. doi: 10.1016/j.lungcan.2009.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chopra A. Molecular Imaging and Contrast Agent Database (MICAD) MD: Bethesda; 2004. 111In-Labeled CHX-A''-DTPA-conjugated MORAb-009, a chimeric monoclonal antibody directed against mesothelin. [PubMed] [Google Scholar]
- Hassan R, Cohen SJ, Phillips M, Pastan I, Sharon E, Kelly RJ, Schweizer C, Weil S, Laheru D. Phase I clinical trial of the chimeric anti-mesothelin monoclonal antibody MORAb-009 in patients with mesothelin-expressing cancers. Clin Cancer Res. 2010;16:6132–6138. doi: 10.1158/1078-0432.CCR-10-2275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hassan R, Ho M. Mesothelin targeted cancer immunotherapy. Eur J Cancer. 2008;44:46–53. doi: 10.1016/j.ejca.2007.08.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaneko O, Gong L, Zhang J, Hansen JK, Hassan R, Lee B, Ho M. A binding domain on mesothelin for CA125/MUC16. J Biol Chem. 2009;284:3739–3749. doi: 10.1074/jbc.M806776200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiang X, Feng M, Felder M, Connor JP, Man YG, Patankar MS, Ho M. HN125: A Novel Immunoadhesin Targeting MUC16 with Potential for Cancer Therapy. J Cancer Educ. 2011;2:280–291. doi: 10.7150/jca.2.280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen SH, Dallas MR, Balzer EM, Konstantopoulos K. Mucin 16 is a functional selectin ligand on pancreatic cancer cells. FASEB J. 2012;26:1349–1359. doi: 10.1096/fj.11-195669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ligtenberg MJ, Kruijshaar L, Buijs F, van Meijer M, Litvinov SV, Hilkens J. Cell-associated episialin is a complex containing two proteins derived from a common precursor. J Biol Chem. 1992;267:6171–6177. [PubMed] [Google Scholar]
- Hilkens J, Buijs F. Biosynthesis of MAM-6, an epithelial sialomucin. Evidence for involvement of a rare proteolytic cleavage step in the endoplasmic reticulum. J Biol Chem. 1988;263:4215–4222. [PubMed] [Google Scholar]
- Komatsu M, Arango ME, Carraway KL. Synthesis and secretion of Muc4/sialomucin complex: implication of intracellular proteolysis. Biochem J. 2002;368:41–48. doi: 10.1042/BJ20020862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Albrecht H, Carraway KL 3rd. MUC1 and MUC4: switching the emphasis from large to small. Cancer Biother Radiopharm. 2011;26:261–271. doi: 10.1089/cbr.2011.1017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Senapati S, Das S, Batra SK. Mucin-interacting proteins: from function to therapeutics. Trends Biochem Sci. 2010;35:236–245. doi: 10.1016/j.tibs.2009.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Y, Ren J, Yu W, Li Q, Kuwahara H, Yin L, Carraway KL 3rd, Kufe D. The epidermal growth factor receptor regulates interaction of the human DF3/MUC1 carcinoma antigen with c-Src and beta-catenin. J Biol Chem. 2001;276:35239–35242. doi: 10.1074/jbc.C100359200. [DOI] [PubMed] [Google Scholar]
- Raina D, Ahmad R, Chen D, Kumar S, Kharbanda S, Kufe D. MUC1 oncoprotein suppresses activation of the ARF-MDM2-p53 pathway. Cancer Biol Ther. 2008;7:1959–1967. doi: 10.4161/cbt.7.12.6956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boivin M, Lane D, Piche A, Rancourt C. CA125 (MUC16) tumor antigen selectively modulates the sensitivity of ovarian cancer cells to genotoxic drug-induced apoptosis. Gynecol Oncol. 2009;115:407–413. doi: 10.1016/j.ygyno.2009.08.007. [DOI] [PubMed] [Google Scholar]
- Theriault C, Pinard M, Comamala M, Migneault M, Beaudin J, Matte I, Boivin M, Piche A, Rancourt C. MUC16 (CA125) regulates epithelial ovarian cancer cell growth, tumorigenesis and metastasis. Gynecol Oncol. 2011;121:434–443. doi: 10.1016/j.ygyno.2011.02.020. [DOI] [PubMed] [Google Scholar]
- Lakshmanan I, Ponnusamy MP, Das S, Chakraborty S, Haridas D, Mukhopadhyay P, Lele SM, Batra SK. MUC16 induced rapid G2/M transition via interactions with JAK2 for increased proliferation and anti-apoptosis in breast cancer cells. Oncogene. 2012;31:805–817. doi: 10.1038/onc.2011.297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reinartz S, Failer S, Schuell T, Wagner U. CA125 (MUC16) gene silencing suppresses growth properties of ovarian and breast cancer cells. Eur J Cancer. 2011;48:1558–1569. doi: 10.1016/j.ejca.2011.07.004. [DOI] [PubMed] [Google Scholar]
- Schmalfeldt B, Prechtel D, Harting K, Spathe K, Rutke S, Konik E, Fridman R, Berger U, Schmitt M, Kuhn W, Lengyel E. Increased expression of matrix metalloproteinases (MMP)-2, MMP-9, and the urokinase-type plasminogen activator is associated with progression from benign to advanced ovarian cancer. Clin Cancer Res. 2001;7:2396–2404. [PubMed] [Google Scholar]
- Kenny HA, Kaur S, Coussens LM, Lengyel E. The initial steps of ovarian cancer cell metastasis are mediated by MMP-2 cleavage of vitronectin and fibronectin. J Clin Invest. 2008;118:1367–1379. doi: 10.1172/JCI33775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Akita K, Tanaka M, Tanida S, Mori Y, Toda M, Nakada H. CA125/MUC16 interacts with Src family kinases, and over-expression of its C-terminal fragment in human epithelial cancer cells reduces cell-cell adhesion. Eur J Cell Biol. 2013;92:257–263. doi: 10.1016/j.ejcb.2013.10.005. [DOI] [PubMed] [Google Scholar]
- Cancer Genome Atlas Research N. Integrated genomic analyses of ovarian carcinoma. Nature. 2011;474:609–615. doi: 10.1038/nature10166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radhakrishnan P, Mohr AM, Grandgenett PM, Steele MM, Batra SK, Hollingsworth MA. MicroRNA-200c modulates the expression of MUC4 and MUC16 by directly targeting their coding sequences in human pancreatic cancer. PLoS One. 2013;8:e73356. doi: 10.1371/journal.pone.0073356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baum RP, Hertel A, Baew-Christow T, Noujaim AA, Hor G. In: Nuclear Medicine. Schmidt HAE, Stuttgart RH, editor. New York: Schattuer; 1992. A novel Tc-99m labeled monoclonal antibody against CA125 (B43.13) for radioimmunodetection pf ovarian cancer-initial results; pp. 670–672. [Google Scholar]
- Mobus VJ, Baum RP, Bolle M, Kreienberg R, Noujaim AA, Schultes BC, Nicodemus CF. Immune responses to murine monoclonal antibody-B43.13 correlate with prolonged survival of women with recurrent ovarian cancer. Am J Obstet Gynecol. 2003;189:28–36. doi: 10.1067/mob.2003.347. [DOI] [PubMed] [Google Scholar]
- Noujaim AA, Schultes BC, Baum RP, Madiyalakan R. Induction of CA125-specific B and T cell responses in patients injected with MAb-B43.13–evidence for antibody-mediated antigen-processing and presentation of CA125 in vivo. Cancer Biother Radiopharm. 2001;16:187–203. doi: 10.1089/10849780152389384. [DOI] [PubMed] [Google Scholar]
- Schultes BC, Zhang C, Xue LY, Noujaim AA, Madiyalakan R. Immunotherapy of human ovarian carcinoma with OvaRex MAb-B43.13 in a human-PBL-SCID/BG mouse model. Hybridoma. 1999;18:47–55. doi: 10.1089/hyb.1999.18.47. [DOI] [PubMed] [Google Scholar]
- Schultes BC, Baum RP, Niesen A, Noujaim AA, Madiyalakan R. Anti-idiotype induction therapy: anti-CA125 antibodies (Ab3) mediated tumor killing in patients treated with Ovarex mAb B43.13 (Ab1) Cancer Immunol Immunother. 1998;46:201–212. doi: 10.1007/s002620050479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma J, Samuel J, Kwon GS, Noujaim AA, Madiyalakan R. Induction of anti-idiotypic humoral and cellular immune responses by a murine monoclonal antibody recognizing the ovarian carcinoma antigen CA125 encapsulated in biodegradable microspheres. Cancer Immunol Immunother. 1998;47:13–20. doi: 10.1007/s002620050499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reinsberg J, Krebs D. Are human anti-idiotypic anti-OC125 antibodies formed after immunization with the anti-CA125 antibody B43.13? Hybridoma. 1997;16:59–63. doi: 10.1089/hyb.1997.16.59. [DOI] [PubMed] [Google Scholar]
- Madiyalakan R, Sykes TR, Dharampaul S, Sykes CJ, Baum RP, Hor G, Noujaim AA. Antiidiotype induction therapy: evidence for the induction of immune response through the idiotype network in patients with ovarian cancer after administration of anti-CA125 murine monoclonal antibody B43.13. Hybridoma. 1995;14:199–203. doi: 10.1089/hyb.1995.14.199. [DOI] [PubMed] [Google Scholar]
- Baum RP, Niesen A, Hertel A, Nancy A, Hess H, Donnerstag B, Sykes TR, Sykes CJ, Suresh MR, Noujaim AA, Hor G. Activating anti-idiotypic human anti-mouse antibodies for immunotherapy of ovarian carcinoma. Cancer. 1994;73:1121–1125. doi: 10.1002/1097-0142(19940201)73:3+<1121::AID-CNCR2820731353>3.0.CO;2-Q. [DOI] [PubMed] [Google Scholar]
- Baum RP, Noujaim AA, Nanci A, Moebus V, Hertel A, Niesen A, Donnerstag B, Sykes T, Boniface G, Hor G. Clinical course of ovarian cancer patients under repeated stimulation of HAMA using MAb OC125 and B43.13. Hybridoma. 1993;12:583–589. doi: 10.1089/hyb.1993.12.583. [DOI] [PubMed] [Google Scholar]
- Berek JS. Immunotherapy of ovarian cancer with antibodies: a focus on oregovomab. Expert Opin Biol Ther. 2004;4:1159–1165. doi: 10.1517/14712598.4.7.1159. [DOI] [PubMed] [Google Scholar]
- Berek JS, Taylor PT, Gordon A, Cunningham MJ, Finkler N, Orr J Jr, Rivkin S, Schultes BC, Whiteside TL, Nicodemus CF. Randomized, placebo-controlled study of oregovomab for consolidation of clinical remission in patients with advanced ovarian cancer. J Clin Oncol. 2004;22:3507–3516. doi: 10.1200/JCO.2004.09.016. [DOI] [PubMed] [Google Scholar]
- Reinartz S, Kohler S, Schlebusch H, Krista K, Giffels P, Renke K, Huober J, Mobus V, Kreienberg R, DuBois A, Sabbatini P, Wagner U. Vaccination of patients with advanced ovarian carcinoma with the anti-idiotype ACA125: immunological response and survival (phase Ib/II) Clin Cancer Res. 2004;10:1580–1587. doi: 10.1158/1078-0432.CCR-03-0056. [DOI] [PubMed] [Google Scholar]
- Reinartz S, Hombach A, Kohler S, Schlebusch H, Wallwiener D, Abken H, Wagner U. Interleukin-6 fused to an anti-idiotype antibody in a vaccine increases the specific humoral immune response against CA125+ (MUC-16) ovarian cancer. Cancer Res. 2003;63:3234–3240. [PubMed] [Google Scholar]
- Reinartz S, Wagner U, Giffels P, Gruenn U, Schlebusch H, Wallwiener D. Immunological properties of a single-chain fragment of the anti- idiotypic antibody ACA125. Cancer Immunol Immunother. 2000;49:186–192. doi: 10.1007/s002620000126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reinartz S, Boerner H, Koehler S, Von Ruecker A, Schlebusch H, Wagner U. Evaluation of immunological responses in patients with ovarian cancer treated with the anti-idiotype vaccine ACA125 by determination of intracellular cytokines–a preliminary report. Hybridoma. 1999;18:41–45. doi: 10.1089/hyb.1999.18.41. [DOI] [PubMed] [Google Scholar]
- Wagner U, Schlebusch H, Kohler S, Schmolling J, Grunn U, Krebs D. Immunological responses to the tumor-associated antigen CA125 in patients with advanced ovarian cancer induced by the murine monoclonal anti-idiotype vaccine ACA125. Hybridoma. 1997;16:33–40. doi: 10.1089/hyb.1997.16.33. [DOI] [PubMed] [Google Scholar]
- Sabbatini P, Dupont J, Aghajanian C, Derosa F, Poynor E, Anderson S, Hensley M, Livingston P, Iasonos A, Spriggs D, McGuire W, Reinartz S, Schneider S, Grande C, Lele S, Rodabaugh K, Kepner J, Ferrone S, Odunsi K. Phase I study of abagovomab in patients with epithelial ovarian, fallopian tube, or primary peritoneal cancer. Clin Cancer Res. 2006;12:5503–5510. doi: 10.1158/1078-0432.CCR-05-2670. [DOI] [PubMed] [Google Scholar]
- Sabbatini P, Harter P, Scambia G, Sehouli J, Meier W, Wimberger P, Baumann KH, Kurzeder C, Schmalfeldt B, Cibula D, Bidzinski M, Casado A, Martoni A, Colombo N, Holloway RW, Selvaggi L, Li A, del Campo J, Cwiertka K, Pinter T, Vermorken JB, Pujade-Lauraine E, Scartoni S, Bertolotti M, Simonelli C, Capriati A, Maggi CA, Berek JS, Pfisterer J. Abagovomab as maintenance therapy in patients with epithelial ovarian cancer: a phase III trial of the AGO OVAR, COGI, GINECO, and GEICO–the MIMOSA study. J Clin Oncol. 2013;31:1554–1561. doi: 10.1200/JCO.2012.46.4057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pfisterer J, Harter P, Simonelli C, Peters M, Berek J, Sabbatini P, du Bois A. Abagovomab for ovarian cancer. Expert Opin Biol Ther. 2011;11:395–403. doi: 10.1517/14712598.2011.553598. [DOI] [PubMed] [Google Scholar]
- Grisham RN, Berek J, Pfisterer J, Sabbatini P. Abagovomab: an anti-idiotypic CA-125 targeted immunotherapeutic agent for ovarian cancer. Immunotherapy. 2011;3:153–162. doi: 10.2217/imt.10.100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belisle JA, Gubbels JA, Raphael CA, Migneault M, Rancourt C, Connor JP, Patankar MS. Peritoneal natural killer cells from epithelial ovarian cancer patients show an altered phenotype and bind to the tumour marker MUC16 (CA125) Immunology. 2007;122:418–429. doi: 10.1111/j.1365-2567.2007.02660.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
BLAST analysis showing location of SEA domains in each of the repeat and the C-terminal domain of MUC16.
MUC16 mutations listed in TCGA data on ovarain cancer samples.


