Abstract
Adults caring for children in HIV-endemic communities are at risk for poor psychological outcomes. However, we still have a limited understanding of how various HIV impacts—including caregiver's own HIV illness, responsibilities of caring for a child orphaned by AIDS, or both—affect psychological outcomes among caregivers. Furthermore, few studies have explored the relationship between stigma, HIV, and psychological outcomes among caregivers of children in HIV-endemic communities. A cross-sectional survey conducted from 2009 to 2010 assessed anxiety among 2477 caregivers of children in HIV-endemic South Africa. Chi-square tested differences in anxiety among caregivers living with HIV, caregivers of a child orphaned by AIDS, and caregivers affected with both conditions. Multivariate logistic regressions identified whether the relationship between HIV impacts and anxiety remained after controlling for socio-demographic co-factors. Mediation analysis tested the relationship between stigma, HIV, and anxiety. The odds of meeting threshold criteria for clinically relevant anxiety symptoms were two and a half times greater among caregivers living with HIV compared to nonaffected caregivers. The odds of meeting threshold criteria for clinically relevant anxiety symptoms were greatest among caregivers living with HIV and caring for a child orphaned by AIDS. Exposure to AIDS-related stigma partially mediated the relationship between HIV and anxiety. Interventions are needed to address caregiver psychological health, particularly among caregivers affected with both conditions of living with HIV and caring for a child orphaned by AIDS.
Introduction
Sub-Saharan Africa confronts the challenge of providing long-term care and support for over 14 million children who have been orphaned and made vulnerable by HIV.1 In HIV-endemic communities, adults caring for these children face financial, social, and educational costs associated with care provision.2–4 Caregivers also report poor health outcomes,4–6 including poor psychological outcomes.7–13
However, we do not fully understand how different types of HIV impacts—including how living with HIV while caring for a child orphaned by AIDS—might predict psychological outcomes among caregivers. Studies suggest that becoming a caregiver of a child orphaned by AIDS can elevate risks for poor psychological outcomes,14,15 possibly due to a number of challenges associated with the increased responsibility of caring for additional children within the household.16 Other studies indicate individuals living with HIV17–20 and adults providing care to individuals living with HIV are at increased risk for poor psychological outcomes.21–25 While these studies are with related populations, rather than caregivers of children in HIV-endemic communities, findings identify an important relationship between HIV illness and poor psychological health.
There is a paucity of literature examining the psychological outcomes related to living with HIV while simultaneously caring for orphaned and vulnerable children. One study in the USA examined the impacts of living with HIV while caring for children affected by HIV, but was qualitative and did not probe specifically for psychological outcomes.26 Another study assessed psychological outcomes among caregivers living with HIV while caring for orphaned and vulnerable children but had a small sample (N=13), and took place in Cuba, making it difficult to generalize to sub-Saharan Africa.24 A third study indicated poor psychological outcomes among HIV-infected caregivers of orphaned and vulnerable children in Haiti, but was a clinical sample.25 None of these studies used comparison groups.
If we are to understand the needs of HIV-affected communities, it is essential that we recognize that people can experience multiple simultaneous exposures to the impacts of HIV. Many primary caregivers of orphaned and vulnerable children are HIV-positive themselves, but the identification of whether there are differential psychological outcomes related to these experiences requires large-scale, community-based research. Detangling whether various types of HIV impacts (e.g., living with HIV vs. caring for a child orphaned by AIDS) pose differential risk for poor psychological health, and whether there is a cumulative effect among caregivers affected with both conditions (e.g., living with HIV while simultaneously caring for a child orphaned by AIDS) can provide a deeper understanding of how to formulate policies and programs to support the psychological wellbeing of caregivers in highly affected communities.
There is also a need to understand how HIV-related stigma might affect psychological outcomes among caregivers of children in HIV-endemic communities. HIV-positive people are likely to experience stigma27 as well as orphaned and vulnerable children.28–30 The few studies that examine stigma and psychological outcomes among caregivers living with HIV in HIV-endemic communities suggest that stigma may play an important role in psychological outcomes among caregivers,31,32 possibly due to maladaptive coping mechanisms33 such as disengagement34,35 and social isolation.36 Exploring whether stigma mediates the relationship between HIV and poor psychological outcomes would further our understanding of the role of stigma in psychological outcomes of caregivers affected by HIV.
This article reports on data from a cross-sectional survey of families in HIV-endemic South Africa. Our primary aim was to examine the relationship between differential HIV impacts and caregiver anxiety including: (a) living with HIV but not caring for a child orphaned by AIDS, (b) caring for a child orphaned by AIDS but not living with HIV, (c) and dual HIV effects, defined as caregivers living with HIV while caring for a child orphaned by AIDS, compared to nonaffected caregivers. We chose to focus on anxiety because other psychological studies with this population have examined depression14,15,31 and stress.7,37 Our secondary aim was to explore whether stigma mediated the relationship between HIV and anxiety given that stigma may be a salient variable for caregivers experiencing double stigma due to living with HIV and caring for a child orphaned by AIDS.
Methods
Data collection took place in South Africa from 2009 to 2010, the country with the largest number of people living with HIV.38 Our study took place in one urban and one rural community in KwaZulu-Natal Province, selected based on their high antenatal HIV prevalence (≥30%).39
Population and procedures
Geographical Information Systems (GIS) was used to map the target community. Random sampling of geographical areas representing the smallest political boundary was conducted, and each household in the area was visited to determine household eligibility. Eligible households were invited to participate in a cross-sectional survey. In each household, one adult and one child were interviewed. Adults were primary caregivers, 18 years or older. A primary caregiver was defined as an individual who takes on primary childcare duties; he/she could therefore be a biological or foster (relative or nonrelative) parent. One child under their care, 10–17 years of age, was also selected. Because the study's main purpose was to identify families affected by HIV, including families where caregivers were living with HIV, ill caregivers were purposively sampled within households that had more than one primary caregiver using an illness screening questionnaire. Our community-based sampling did not identify children in institutional care. This may be because the number of children living in institutional settings remains relatively low compared to children living in households, although the exact prevalence of children residing in institutional care is difficult to ascertain due to the proliferation of nonregistered residential care facilities in South Africa.40
Caregivers provided voluntary informed consent for their own participation and voluntary informed consent for child participation. The child interviewed provided voluntary informed assent. Study procedures were approved by Institutional Review Boards at the University of Oxford and University of KwaZulu-Natal. Furthermore, ethical approval was obtained from KwaZulu-Natal's Provincial Departments of Health and Education.
Measures
The AIDS-illness status of the caregiver and the child's AIDS-orphan status were identified using self-report and a verbal autopsy (VA) approach. The VA is used for identifying HIV illness or AIDS-related cause of death in settings with high HIV incidence but poor comprehensive vital registration, medical records, and health systems utilization.41,42 The VA questionnaire used in our study was originally validated in Zimbabwe, showing a sensitivity of 83% and specificity of 75% for AIDS death.43 Orphanhood used the United Nations definition of the loss of one or both biological parents.44 Orphaned and vulnerable children were defined as children affected by HIV illness or AIDS-related death.45
Anxiety was measured using the Beck Anxiety Inventory (BAI).46 This 21-item instrument assesses anxiety symptoms over the past month, with responses ranging from ‘Not at all’ (0) to ‘Severely’ (3). The BAI has been widely used in various settings, including South Africa,47–50 has high internal consistency (α=0.90 to 0.94) and a test-retest reliability of 0.75 46,50,51 Scores range from 0 to 63. Scores between 0–7 indicate low/normal anxiety, 8–15 indicate mild anxiety, 16–35 indicate moderate anxiety, and ≥26 indicate high anxiety.46
We also gathered information on socio-demographic and household variables that might function as important covariates. Age, gender, education, and household characteristics including assets and food security were collected using items from the South African National Census,52 General Household Survey,53 Demographic and Health Survey,54 and the KwaZulu-Natal Income Dynamics Study (KIDS) questionnaire.55 Age,56–61 education,62 gender, and economic status have all been identified as potentially important predictors of psychological health more generally, and among HIV-positive individuals and caregivers specifically.63–71 Food security was measured with a question from the Demographic and Health Survey,54 and asked whether the household experienced hunger ranging from ‘never’, to ‘often’. We also assessed enacted stigma. At the time of study planning, we were only able to identify one validated scale for stigma, but it was specific to people living with HIV72 rather than those affected by caring for orphaned and vulnerable children. Thus, we used a 17-item stigma scale drawn from a USAID report that measures enacted stigma by probing for stigma related experiences, including for example, exclusion from social gatherings.73 The stigma scale was scored by tallying the number of affirmative responses.
Data analysis
Data were analyzed using SPSS version 20. Our primary aim was to compare the prevalence of clinically relevant anxiety symptoms among caregivers affected by various types of HIV with those not affected by HIV. Descriptive statistics were used to summarize caregiver socio-demographics, the prevalence of HIV-affected households, and percentage of caregivers meeting clinically relevant criteria for anxiety. Chi-square tests explored whether caregivers living with HIV illness were more likely to meet criteria for anxiety compared to caregivers not living with HIV. Chi-square tests also explored differences in anxiety among caregivers affected only with HIV illness, only with caring for a child orphaned by AIDS, or with both conditions. For these chi-square tests, we re-coded anxiety symptoms into a binary variable, with clinically significant anxiety symptoms ≥8 on the BAI coded as ‘1’, and nonclinically relevant anxiety symptoms coded as ‘0’. Multivariate logistic hierarchical regressions tested whether the relationship between anxiety as a binary outcome and HIV impacts persisted after adjusting for potentially significant co-factors such as socio-demographic differences, household location, poverty, food security, and stigma. In logistic regressions, we coded each type of HIV impact as a binary variable, with each HIV impact (affected with both conditions, only living with HIV, only caring for a child orphaned by AIDS) defined as 1; each category was mutually exclusive. We examined whether stigma directly or indirectly mediated the relationship between HIV and anxiety based on the four step process described by Baron and Kenny,74 but adapted for logistic regressions75 and using a Sobel test.76,77
Results
Nearly all participants identified as Black African (99.8%) with isiZulu as their primary language (95.9%). The majority of caregivers were female (88.9%). The mean caregiver age was 44.2 years (range 18–92 years). Less than a fifth of caregivers had completed high school (18.1%). Approximately half of the children were female (53.9%) with an average age of 13.6 years (range 10–17 years). Approximately half of the households were located in the urban site (48.4%). Only 35.7% of households had a steady source of household income, and 40.4% reported food insecurity. Nearly a third of households (32.2%) were comprised of caregivers living with HIV and/or caring for a child orphaned by AIDS. Nearly half of caregivers (49.4%) reported clinically relevant anxiety symptoms (Table 1).
Table 1.
Socio-Demographic Characteristics (N=2477 Caregivers, N=2477 Children)
| Variables | Total sample (n=2477) |
|---|---|
| Caregiver socio-demographic variables | |
| Female (%) | 88.9 |
| Age (mean, SD) | 44.2 (13.9) |
| Completed high school (%) | 18.1 |
| Child socio-demographic variables | |
| Female (%) | 53.9 |
| Age (mean, SD) | 13.6 (2.2) |
| Type of orphanhood | |
| Maternal | 15.6 |
| Paternal | 23.6 |
| Double | 5.6 |
| HIV-affected households (%) | 32.2 |
| Caregiver is living with HIV but children are not orphaned by AIDS (%) | 24.8 |
| Caregiver of a child orphaned by AIDS but not living with HIV (%) | 4.6 |
| Caregiver is living with HIV and children are orphaned by AIDS (%) | 2.8 |
| Household characteristics | |
| Urban (%) | 48.4 |
| Steady source of household income with salaried income (%) | 35.7 |
| Food insecurity (%) | 40.4 |
| Some experience of stigma (%) | 35.3 |
| Caregiver anxiety | 49.4% |
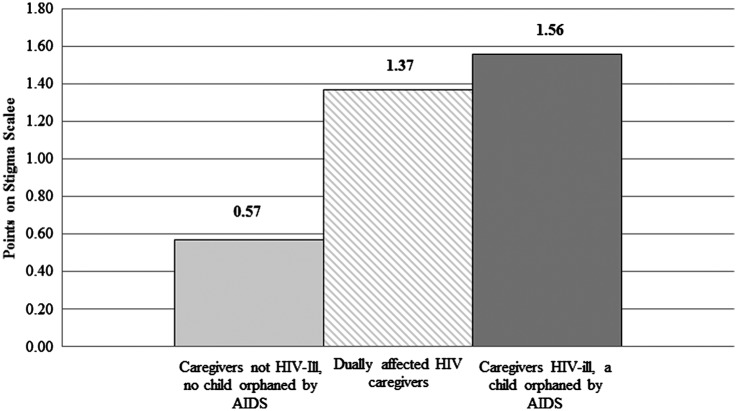
Caregivers living with HIV were significantly more likely to be classified as meeting threshold criteria for clinically relevant anxiety symptoms (66.0%) than caregivers not living with HIV (43.1%) (χ2=104.0, p<0.001). Similarly, caregivers of a child orphaned by AIDS were significantly more likely to be classified as meeting the threshold criteria for clinically relevant anxiety symptoms (58.7%) than caregivers not caring for a child orphaned by AIDS (48.7%) (χ2=6.85, p<0.009). We conducted further analyses on the percentage of caregivers who met threshold criteria for anxiety by disaggregating various HIV impacts including: (1) caregivers of a child orphaned by AIDS but not living with HIV, (2) caregivers living with HIV but not caring for a child orphaned by AIDS, and (3) caregivers affected with both conditions. Caregivers affected with both conditions were the most likely to meet threshold criteria for clinically relevant anxiety symptoms at 75.7%, followed by those caring for a child orphaned by AIDS but not living with HIV at 64.9%, followed by those living with HIV but not caring for a child orphaned by AIDS at 48.2% (χ2=108.26, p<0.001) (Fig. 1).
FIG. 1.
Risk for anxiety among caregivers dually affected by HIV illness and caring for a child orphaned by AIDS (N=2477). Chi square level of significance at p<0.001***.
Multivariate hierarchical logistic regressions are summarized in Table 2. Each model was significant (p<0.001). In Model 1, we examine various types of HIV impacts on caregiver anxiety. Living with HIV increased risk for anxiety, above and beyond caring for a child orphaned by AIDS (Model 1, OR=2.48, 95% CI=2.04–2.99, p<0.001). Importantly, we also identified the cumulative risk for anxiety among caregivers affected with both conditions; the odds of meeting threshold criteria for anxiety was four times greater among caregivers affected with both conditions (Model 1, OR=4.18, 95% CI=2.39–7.28, p<0.001) compared to nonaffected caregivers. The relationship between caring for a child orphaned by AIDS and anxiety was not significant (Model 1, OR=1.25, 95% CI=0.86–1.83, p<0.25). In subsequent models, even after adjusting for differences in caregiver and child age, gender, and education as well as household poverty, urban/rural location, and food security, caregivers affected with both conditions (Model 3, OR=5.29, 95% CI=1.91–14.63, p<0.001) and caregiver HIV illness (Model 3, OR=2.74, 95% CI=2.01–3.73, p<0.001) still predicted anxiety. The final model identified older age (Model 4, OR=1.62, 95% CI=1.24–2.12, p<0.001) and being female (Model 4, OR=1.74, 95% CI=1.18–2.57, p<0.005) as risk factors for anxiety, whereas caregiver education (Model 4, OR=0.50, 95% CI=0.38–0.65, p<0.001) served as a protective factor. The final model also identified stigma as an important risk factor, with caregivers who reported some experience of stigma more likely to meet threshold criteria for clinically relevant anxiety symptoms, by nearly a factor and a half (Model 4, OR=1.44, 95% CI=1.09–1.89, p<0.01) (Table 2).
Table 2.
Multivariate Logistic Regressions Testing Various HIV Impacts on Caregiver Anxiety (N=2477)
| Variables | Model 1 OR [95% CI] | Model 2 OR [95% CI] | Model 3 OR [95% CI] | Model 4 OR [95% CI] |
|---|---|---|---|---|
| Caregivers dually affected | 4.18*** [2.39–7.28] | 5.68*** [2.06–15.64] | 5.29*** [1.91–14.63] | 4.79** [1.72–13.28] |
| Caregivers living with HIV only | 2.48*** [2.04–2.99] | 2.82*** [2.09–3.82] | 2.74*** [2.01–3.73] | 2.59*** [1.90–3.54] |
| Caring for a child orphaned by AIDS only | 1.25 [0.86–1.83] | 1.01 [0.58–1.77] | 1.00 [0.57–1.75] | 1.02 [0.58–1.79] |
| Socio-demographic variables | ||||
| Caregiver agea | 1.53*** [1.19–1.96] | 1.65*** [1.27–2.15] | 1.62*** [1.24–2.12] | |
| Caregiver genderb | 1.78** [1.21–2.61] | 1.75** [1.19–2.58] | 1.74** [1.18–2.57] | |
| Caregiver educationc | 0.49*** [0.38–0.63] | 0.50*** [0.38–0.66] | 0.50*** [0.38–0.65] | |
| Child agea | 1.21 [0.87–1.69] | 1.17 [0.84–1.64] | 1.18 [0.84–1.66] | |
| Child genderb | 1.18 [0.93–1.50] | 1.13 [0.89–1.44] | 1.14 [0.89–1.45] | |
| Child educationc | 0.95 [0.89–1.02] | 0.97 [0.90–1.04] | 0.96 [0.90–1.03] | |
| Household characteristics | ||||
| Povertyd | 0.83 [0.61–1.11] | 0.87 [0.65–1.17] | ||
| Location of householde | 1.13 [0.82–1.56] | 1.07 [0.77–1.48] | ||
| Food securityf | 1.24 [0.90–1.73] | 1.19 [0.86–1.66] | ||
| Stigmag | 1.44** [1.09–1.89] | |||
Significance at p<0.001 level; **Significance at p<0.01 level; *Significance at p<0.05 level.
Dichotomous variable calculated based on median value; higher values reflect higher age; b1, female; 0, male; cDichotomous variable calculated based on mean value; higher values reflect more education; dDichotomous variable calculated based on mean value; higher values reflect more household assets; 1=high, 0=low; e1=rural, 0=urban; fDichotomous variable calculated where answers of the household is sometimes and always hungry were coded as 1=yes, and the household was rarely or never hungry were coded as 0=no; gDichotomous variable calculated based on any report of stigma was coded as 1=yes, and no experience of stigma coded as 0=no.
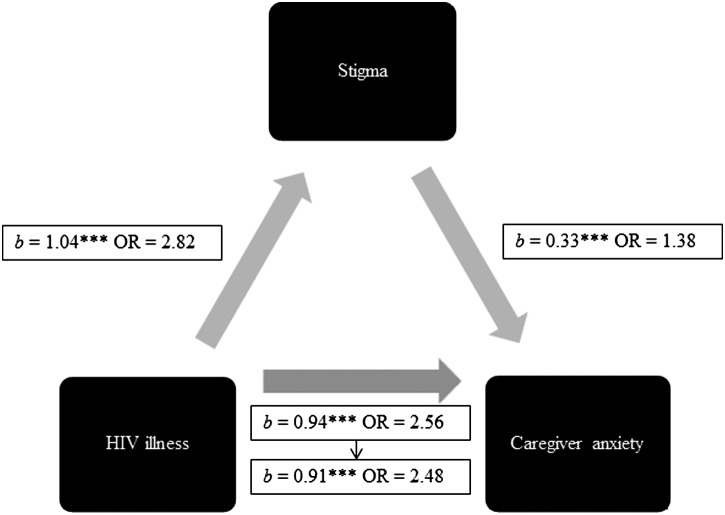
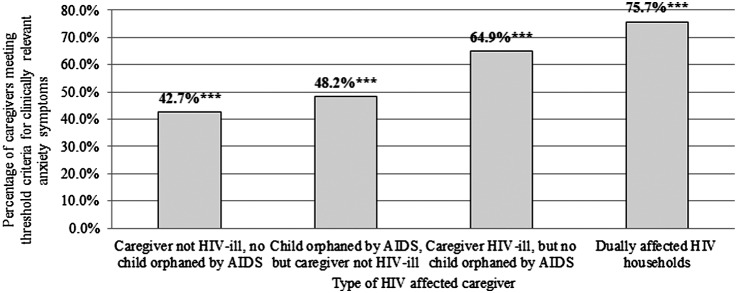
Finally, we analyzed whether stigma mediated HIV and caregiver anxiety. First, we checked that caregivers affected with both conditions (M=1.37, SD=2.18) and those living with HIV (M=1.56, SD=2.29) reported significantly higher stigma scores than nonaffected caregivers (M=0.57, SD=1.23), F (2, 2359)=89.72, p<0.001 (Fig. 2). Second, we assessed whether stigma mediated the relationship between HIV illness and caregiver anxiety. When both HIV illness and stigma were regressed simultaneously onto caregiver anxiety, we found the stigma partially mediated the effect between HIV and anxiety with a decrease in the relationship between HIV illness and caregiver anxiety from b=0.94, OR=2.56, p<0.001 to b=0.91, OR=2.48, p<0.001. An additional Sobel's test of the indirect effect confirmed the significance of the mediator (z=7.21, p<0.001) (Fig. 3).
FIG. 2.
Caregivers dually affected by HIV or living with HIV are likely to report higher levels of stigma (N=2477). F test of significance at p<0.001***.
FIG. 3.
Stigma mediates the relationship between HIV and caregiver anxiety.
Discussion
This study adds to our understanding of how HIV illness alone, responsibility of caring for a child orphaned by AIDS alone, or the combined effects of HIV illness with caring for a child orphaned by AIDS are related to caregiver psychological outcomes. Different types of HIV impacts pose varying risks for anxiety among adults caring for children in HIV-endemic South African communities. Findings indicate caregivers are at high risk for anxiety and psychological disparities, consistent with previous studies among caregivers of children orphaned and vulnerable children in South Africa13,78 and elsewhere.11,79 However, our study offers a more nuanced understanding of the varied psychological risks posed by differential types of HIV impacts. Our findings suggest that it was not caring for a child orphaned by AIDS per se that increased risk for anxiety. Rather, it was the combination of caring for a child orphaned by AIDS while simultaneously coping with one's own HIV illness that placed caregivers at heightened risk for anxiety. Particularly striking is the finding that dually affected HIV caregivers—those living with HIV while caring for a child orphaned by AIDS—faced a cumulative risk for anxiety.
This study also identified that women and older caregivers were at increased risk for anxiety, consistent with the broader psychological literature. Women may be at risk for anxiety,80–82 possibly due to approaches to managing negative affect, coping responses to stress,83,84 and etiological differences.85 Age may increase risk for anxiety due to an increase in chronic health conditions86,87 and neurological changes.88 Our findings also identify education as an important protective factor for anxiety which may be linked to protective health behaviours.62,89
Stigma increased risk for anxiety. Other studies have shown that individuals report elevated risk for poor psychological outcomes due to internalized stigma17 or secondary stigma derived from caring for family infected or affected by HIV.90 While the relationship between stigma and poor outcomes among HIV-infected populations is not surprising, this relationship has not been examined in depth in relation to the psychological outcomes of adults caring for children in HIV-endemic communities. We found that stigma partially mediated the relationship between HIV and anxiety, suggesting that strategies to identify and target caregivers for psychosocial interventions need to be designed carefully to limit further stigmatization of HIV-affected caregivers who need psychological support.
Our study has several strengths, including our rigorous sampling approach, use of a large community sample, use of comparison groups, and distinguishing the differential risks posed by different types of HIV impacts. However, we also recognize the limitations of our study. For example, using biomarkers to identify HIV illness would ensure further validation of caregiver HIV status, and can be used in future studies. Moreover, we did not gather qualitative data, which could have provided a deeper understanding of how the process of HIV illness and day-to-day responsibilities of caring for children impact psychological outcomes. Our cross-sectional data limited our ability to examine the temporal effects of HIV impacts on caregiver anxiety.
Regardless of these limitations, we feel that this study offers new insights to our approaches to support the wellbeing of families in HIV-endemic communities. Findings reveal an important family dynamic underlying caregivers' psychological outcomes. It is the unique combination of caregiver HIV illness with the responsibility of caring for a child orphaned by AIDS that considerably increased vulnerability to poor psychological outcomes. Among adults caring for orphaned and vulnerable children, those living with HIV may be an ideal target group for policies and programs that help HIV positive caregivers access treatment, support disclosure, and address psychological wellbeing. There are a growing number of community-based interventions in South Africa supporting access to HIV testing and counselling and treatment that could be explored for this target population.91,92 Given the important role of stigma in mediating the relationship between HIV and anxiety, interventions supporting disclosure may also be needed for the target population but remains a major challenge for parents and other caregivers in South Africa93,94 and elsewhere.95 Disclosure interventions have been tested in South Africa96 and elsewhere97 that could be tested for use among caregivers. Caregivers affected with both conditions are most vulnerable; it follows that development of psychological interventions to support these caregivers may need to incorporate a family-level approach. However, few family-based interventions that simultaneously address HIV and psychological needs of families in HIV endemic South Africa exist,98 and this remains a major gap in the scientific evidence base. Findings also reveal the important role of stigma in the HIV-anxiety relationship, but more work needs to be done to detangle whether stigma is related to living with HIV or caring for a child orphaned by AIDS or both. Regardless of type of stigma, our findings suggest that we need to pair psychological interventions with community-level policies and programs that diminish stigma and address discrimination.
Acknowledgments
The authors would like to gratefully acknowledge the families and communities who participated in the study. We would also like to thank our community partner, Tholulwazi Uzivikele. The authors would also like to thank the fieldwork teams. This study was generously funded by the Health Economics and AIDS Research Division (HEARD) at the University of KwaZulu-Natal, the Economic and Social Research Council (UK), the National Research Foundation (SA), the National Department of Social Development (South Africa), the Claude Leon Foundation, and the John Fell Fund. Additional support for publication was provided to CK by the National Institute for Mental Health grants (K01 MH096646, L30 MH098313, R24 HD077976).
Author Disclosure Statement
The authors have no conflict of financial interests to report.
References
- 1.UNAIDS. UN Report on the Global AIDS Epidemic. Geneva: UNAIDS, 2010 [Google Scholar]
- 2.Heymann J, Earle A, Rajaraman D, Miller C, Bogen K. Extended family caring for children orphaned by AIDS: Balancing essential work and caregiving in a high HIV prevalence nations. AIDS Care 2007;19:337–345 [DOI] [PubMed] [Google Scholar]
- 3.Heymann J, Kidman R. HIV/AIDS, declining family resources and the community safety net. AIDS Care 2009;21:34–42 [DOI] [PubMed] [Google Scholar]
- 4.Ssengonzi R. The impact of HIV/AIDS on the living arrangements and well-being of elderly caregivers in rural Uganda. AIDS Care 2009;21:309–314 [DOI] [PubMed] [Google Scholar]
- 5.Ice G, Yogo J, Heh V, Juma E. The impact of caregiving on the health and well-being of Kenyan Luo grandparents. Res Aging 2010;32:40–66 [Google Scholar]
- 6.Howard B, Phillips C, Matinhure N, Goodman K, McCurdy S, Johnson C. Barriers and incentives to orphan care in a time of AIDS and economic crisis: A cross-sectional survey of caregivers in Rural Zimbabwe. BMC Public Health 2006;6:1–11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Oburu PO, Palmerus K. Parenting stress and self-reported discipline strategies of Kenyan caregiving grandmothers. Intl J Behav Develop 2003;27:505–512 [Google Scholar]
- 8.Rotheram-Borus M, Leonard N, Lightfood M, Franzke L, Tottenham N, Lee S. Picking up the pieces: Caregivers of adolescents bereaved by parental AIDS. Clin Child Psychol Psychiatr 2002;7:115–124 [Google Scholar]
- 9.Hansell P, Hughes C, Caliandro G, et al. . Stress and social support in older caregivers of children with HIV/AIDS: An intervention model. In: Joslin D, ed. Invisible Caregivers: Older Adults Raising Children in the Wake of HIV/AIDS. New York: Columbia University Press; 2002, pp. 113–130 [Google Scholar]
- 10.Strug D, Burr C. Service needs of male caretakers of HIV-infected and affected children: Policy and practice implications. Social Work Health Care 2003;38:73–92 [DOI] [PubMed] [Google Scholar]
- 11.Ssengonzi R. The plight of older persons as caregivers to people infected/affected by HIV/AIDS: Evidence from Uganda. J Cross-Cultural Gerontol 2007;22:339–353 [DOI] [PubMed] [Google Scholar]
- 12.Smith Fawzi M, Eustache E, Oswald C, et al. . Psychosocial functioning among HIV-affected youth and their caregivers in Haiti: Implications for family-focused service provision in high HIV burden settings. AIDS Patient Care STDs 2010;24:147–158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kuo C, Operario D. Health of adults caring for orphaned children in an HIV endemic community in South Africa. AIDS Care 2010;5:344–352 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kuo C, Operario D, Cluver L. Depression amongst carers of AIDS-orphaned and other-orphaned children in Umlazi Township, South Africa. Global Public Health 2012;7:253–269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lv Y, Zhao Q, Li X, et al. . Depression symptoms among caregivers of children in HIV-affected families in rural China AIDS Care 2010;22:669–676 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Littrell M, Boris NW, Brown L, Hill M, Macintyre K. The influence of orphan care and other household shocks on health status over time: A longitudinal study of children's caregivers in rural Malawi. AIDS Care 2011;23:1551–1561 [DOI] [PubMed] [Google Scholar]
- 17.Simbayi LC, Kalichman S, Strebel A, Cloete A, Henda N, Mqeketo A. Internalized stigma, discrimination, and depression among men and women living with HIV/AIDS in Cape Town, South Africa. Social Sci Med 2007;64:1823–1831 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kagee A. Symptoms of distress and posttraumatic stress among South African former political detainees. Ethnic Health 2005;10:169–179 [DOI] [PubMed] [Google Scholar]
- 19.Marwick KFM, Kaaya SF. Prevalence of depression and anxiety disorders in HIV-positive outpatients in rural Tanzania. AIDS Care 2010;22:415–419 [DOI] [PubMed] [Google Scholar]
- 20.Lawler K, Mosepele M, Seloilwe E, et al. . Depression among HIV-positive individuals in Botswana: A behavioral surveillance. AIDS Behav 2011;15:204–208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lee SJ, Li L, Jiraphongsa C, Rotheram-Borus MJ. Caregiver burden of family members of persons living with HIV in Thailand. Int J Nurs Pract 2010;16:57–63 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kangethe S. Critical coping challenges facing caregivers of persons living with HIV/AIDS and other terminally iII persons: The case of Kanye Care Program, Botswana. Indian J Palliat Care 2009;15:115–121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mitchell MM, Knowlton A. Stigma, disclosure, and depressive symptoms among informal caregivers of people living with HIV/AIDS. AIDS Patient Care STDS 2009;23:611–617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Santiesteban Y, Castro M, Calvo M. Mental health of primary caregivers for children and adolescents with HIV/AIDS in Cuba. MEDICC Rev 2012;14:30–34 [DOI] [PubMed] [Google Scholar]
- 25.Fawzi M, Eustache E, Oswald C, et al. . Psychosocial functioning among HIV-affected youth and their caregivers in Haiti: Implications for family-focused service provision in high HIV burden settings. AIDS Patient Care STDs 2010;24:147–158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hackl KL, Somlai AM, Kelly JA, Kalichman SC. Women living with HIV/AIDS: The dual challenge of being a patient and caregiver. Health Social Work 1997;22:53–62 [DOI] [PubMed] [Google Scholar]
- 27.Lawless S, Kippax S, Crawford J. Dirty, diseased and undeserving: The positioning of HIV positive women. Social Sci Med 1996;43:1371–1377 [DOI] [PubMed] [Google Scholar]
- 28.Nyamukapa CA, Gregson S, Wambe M, et al. . Causes and consequences of psychological distress among orphans in eastern Zimbabwe. AIDS Care 2010;22:988–996 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cluver L, Gardner F. Risk and protective factors for psychological well-being of children orphaned by AIDS in Cape Town: A qualitative study of children and caregivers' perspectives. AIDS Care 2007;19:318–325 [DOI] [PubMed] [Google Scholar]
- 30.Hamra M, Ross MW, Karuri K, Orrs M, D'Agostino A. The relationship between expressed HIV/AIDS-related stigma and beliefs and knowledge about care and support of people living with AIDS in families caring for HIV-infected children in Kenya. AIDS Care 2005;17:911–922 [DOI] [PubMed] [Google Scholar]
- 31.Surkan PJ, Mukherjee JS, Williams DR, et al. . Perceived discrimination and stigma toward children affected by HIV/AIDS and their HIV-positive caregivers in central Haiti. AIDS Care 2010;22:803–815 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Murphy DA, Austin EL, Greenwell L. Correlates of HIV-related stigma among HIV-positive mothers and their uninfected adolescent children. Women Health 2007;44:19–42 [DOI] [PubMed] [Google Scholar]
- 33.Heckman T, Carlson B. A randomized clinical trial of two telephone-delivered, mental health interventions for HIV-infected persons in rural areas of the United States. AIDS Behav 2007;11:5–14 [DOI] [PubMed] [Google Scholar]
- 34.Varni S, Miller C, McCuin T, Solomon S. Disengagement and engagement coping with HIV/AIDS stigma and psychological well-being of people with HIV/AIDS. J Social Clin Psychol 2012;31:123–150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gonzalez A, Solomon S, Zvolensky M, Miller C. Exploration of the relevance of anxiety sensitivity among adults living with HIV/AIDS for understanding anxiety vulnerability. J Health Psychol 2010;15:138–146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Emlet C. Measuring stigma in older and younger adults with HIV/AIDS: An analysis of an HIV stigma scale and initial exploration of subscales. Res Social Work Practice 2005;15:291–300 [Google Scholar]
- 37.Oburu PO, Palmerus K. Stress related factors among primary and part-time caregiving grandmothers of Kenyan grandchildren. Intl J Aging Human Develop 2005;60:273–282 [DOI] [PubMed] [Google Scholar]
- 38.UNAIDS. Global report: UNAIDS report on the global epidemic. Geneva: UNAIDS, 2012 [Google Scholar]
- 39.South African Department of Health. The National HIV and Syphilis Prevalence Survey South Africa: Pretoria: South African Department of Health, 2008 [Google Scholar]
- 40.Meintjes H, Moses S, Berry L, Mampane R. Home Truths: The Phenomenon of Residential Care for Children in a Time of AIDS. Cape Town: Children's Institute, University of Cape Town and Centre for the Study of AIDS, University of Pretoria, 2007 [Google Scholar]
- 41.Hosegood V, Vannestea , Timæus I. Levels and causes of adult mortality in rural South Africa: The impact of AIDS. AIDS 2004;18:663–671 [DOI] [PubMed] [Google Scholar]
- 42.Setel P, Whiting D, Hemed Y, et al. . Validity of verbal autopsy procedures for determining cause of death in Tanzania. Tropic Med Intl Health 2006;11:681–696 [DOI] [PubMed] [Google Scholar]
- 43.Lopman B, Barnabas R, Boerma J, et al. . Creating and validating an algorithm to measure AIDS mortality in the adult population using verbal autopsy. Plos Med 2006;3:e312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.UNAIDS. Children on the Brink 2004: A Joint Report of New Orphan Estimates and a Framework for Action. New York: UNAIDS, 2004 [Google Scholar]
- 45.UNICEF. Africa's Orphaned and Vulnerable Generations: Children Affected by AIDS. Geneva: UNICEF, 2006 [Google Scholar]
- 46.Beck A, Steer R. Manual for the Beck Anxiety Inventory. San Antonio, TX: Psychological Corporation, 1993 [Google Scholar]
- 47.Faure S, Loxton H. Anxiety, depression and self-efficacy levels of women undergoing first trimester abortion. South African J Psychol 2003;33:28–38 [Google Scholar]
- 48.Pillay A, Edwards S, Sargent C. Anxiety among university students in South Africa. Psychol Rep 2001;88:1182–1186 [DOI] [PubMed] [Google Scholar]
- 49.Pillay A, Sargent C. Relationship of age and education with anxiety, depression, and hopelessness in a South African community sample. Percept Motor Skills 1999;89:881–884 [DOI] [PubMed] [Google Scholar]
- 50.Steele G, Edwards D. Development and validation of the Xhosa translations of the Beck Inventories: 2. Item analysis, internal consistency and factor analysis. J Psychol Africa 2008;18:217–226 [Google Scholar]
- 51.Beck A, Epstein N, Brown G, Steer R. An inventory for measuring clinical anxiety: Psychometric properties. J Consult Clin Psychol 1988;56:893–897 [DOI] [PubMed] [Google Scholar]
- 52.Statistics South Africa. Census 2001. http://www.statssa.gov.za/publications/CensusKey/CensusKey2001.pdf Accessed December3, 2009
- 53.Statistics South Africa. General Household Survey 2005. http://www.statssa.gov.za/publications/P0318/P0318July2005.pdf Accessed January2, 2009, 2012
- 54.South African Department of Health. South Africa Demographic and Health Survey 2003. Pretoria: South African Department of Health, 2007 [Google Scholar]
- 55.May J, Carter M, Haddad L, Maluccio J. KwaZulu-Natal Income Dynamics Study (KIDS) 1993–1998: A Longitudinal Household Data Set for South African Policy Analysis. 1999. Located at: Working Paper No. 21. School of Development Studies, University of Kwazulu-Natal Durban [Google Scholar]
- 56.Madhavan S. Fosterage Patterns in the age of AIDS: Continuity and change. Soc Sci Med 2004;58:1443–1454 [DOI] [PubMed] [Google Scholar]
- 57.Kim S, Lee Y, Kim H, Cho I, Lee J, Cho S. Age as a moderator of the association between depressive symptoms and morningness-eveningness. J Psychosomat Res 2009;68:159–164 [DOI] [PubMed] [Google Scholar]
- 58.Knight E, Ofsthun N, Teng M, Lazarus J, Curhan G. The association between mental health, physical function, and hemodialysis mortality. Kidney Intl 2003;63:1843–1851 [DOI] [PubMed] [Google Scholar]
- 59.Mirowsky J, Ross C. Age and depression. J Health Social Behav 1992;33:187–204 [PubMed] [Google Scholar]
- 60.Strawbridge W, Deleger S, Roberts R, Kaplan G. Physical activity reduces the risk of subsequent depression for older adults. Am J Epidemiol 2002;156:328–334 [DOI] [PubMed] [Google Scholar]
- 61.Tyler K. The effects of an acute stressor on depressive symptoms among older adults: The moderating effects of social support and age. Res Aging 2000;22:143–164 [Google Scholar]
- 62.Ross C, Wu C. The links between education and health. Am Sociolog Rev 1995;60:719–745 [Google Scholar]
- 63.Whetten K, Reif S, Whetten R, Murphy-McMillan Trauma, mental health, distrust, and stigma among HIV-positive persons: Implications for effective care. Psychosomat Med 2008;70:531–538 [DOI] [PubMed] [Google Scholar]
- 64.Zinkernagel C, Taffe P, Rickenbach M, et al. . Importance of mental health assessment in HIV-infected outpatients. J Acq Immune Def Syndr 2001;28:240–249 [DOI] [PubMed] [Google Scholar]
- 65.Patel V, Kleinman A. Poverty and common mental disorders in developing countries. Bull World Health 2003;81:609–615 [PMC free article] [PubMed] [Google Scholar]
- 66.Brandt R. Putting mental health on the agenda for HIV+Women: A review of evidence from sub-Saharan Africa. Women Health 2009;49:215–228 [DOI] [PubMed] [Google Scholar]
- 67.World Health Organisation. The World Health Report 2001: Mental Health: New Understanding, New Hope. Geneva: World Health Organization, 2001 [Google Scholar]
- 68.Pinquart M, Sorensen S. Correlates of physical health of informal caregivers: A meta-analysis. J Gerontol Series B, Psycholog Sci Soc Sci 2007;62:126–137 [DOI] [PubMed] [Google Scholar]
- 69.Crosier T, Butterworth P, Rodgers B. Mental health problems among single and partnered mothers: The role of financial hardship and social support. Soc Psychiatr Psychiatr Epidemiol 2007;42:6–13 [DOI] [PubMed] [Google Scholar]
- 70.Howard B, Phillips C, Matinhure N, Goodman K, McCurdy S, Johnson C. Barriers and incentives to orphan care in a time of AIDS and economic crisis: A cross-sectional survey of caregivers in rural Zimbabwe. BMC Public Health 2006;6:27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Lv Y, Zhao Q, Li X, et al. . Depression symptoms among caregivers of children in HIV affected families in rural China. AIDS CARE 2010;22:669–676 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Kalichman SC, Simbayi LC, Jooste S, et al. . Development of a brief scale to measure AIDS-related stigma in South Africa. AIDS Behav 2005;9:135–143 [DOI] [PubMed] [Google Scholar]
- 73.USAID. Can We Measure HIV/AIDS-Related Stigma and Discrimination? Washington, DC: USAID, 2006 [Google Scholar]
- 74.Baron R, Kenny D. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic and statistical considerations. Journal of Personality and Social Psychology. 1986;51:1173–1182 [DOI] [PubMed] [Google Scholar]
- 75.MacKinnon DP, Dwyer JH. Estimating mediated effects in prevention studies. Eval Rev 1993;17:144–158 [Google Scholar]
- 76.Sobel ME, ed. Asymptotic intervals for indirect effects in structural equations models. San Francisco Jossey-Bass, 1982. Leinhart S, ed. Sociological Methodology [Google Scholar]
- 77.Preacher KJ, Hayes AF. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behav Res Meth Instruments Computers 2004;36:717–731 [DOI] [PubMed] [Google Scholar]
- 78.Govender K, Penning S, George G, Quinlan T. Weighing up the burden of care on caregivers of orphan children: The Amajuba District Child Health and Wellbeing Project, South Africa. AIDS Care 2012;24:712–721 [DOI] [PubMed] [Google Scholar]
- 79.Joslin D, Harrison R. The “hidden patient”: Older relatives raising children orphaned by AIDS. J Am Med Women's Assoc 1998;53:65–71, 76 [PubMed] [Google Scholar]
- 80.Bruce S, Yonkers K, Otto M, et al. . Influence of psychiatric comorbidity on recovery and recurrence in generalized anxiety disorder, social phobia, and panic disorder: A 12-year prospective study. Am J Psychiatr 2005;162:1179–1187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Kessler Rc MKAZS, et al. . Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the united states: Results from the national comorbidity survey. Arch Gen Psychiatr 1994;51:8–9 [DOI] [PubMed] [Google Scholar]
- 82.McLean CP, Asnaani A, Litz BT, Hofmann SG. Gender differences in anxiety disorders: Prevalence, course of illness, comorbidity and burden of illness. J Psychiatr Res 2011;45:1027–1035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Rudolph K. Gender differences in emotional responses to interpersonal stress during adolescence. J Adolesc Health 2002;30:3–13 [DOI] [PubMed] [Google Scholar]
- 84.Stewart S, Taylor S, Baker J. Gender differences in dimensions of anxiety sensitivity. J Anxiety Dis 1997;11:179–200 [DOI] [PubMed] [Google Scholar]
- 85.Pigott T. Gender differences in the epidemiology and treatment of anxiety disorders. J Clin Psychiatr 1999;60:4–15 [PubMed] [Google Scholar]
- 86.Schoevers RA, Beekman ATF, Deeg DJH, Jonker C, Tilburg Wv. Comorbidity and risk-patterns of depression, generalised anxiety disorder and mixed anxiety-depression in later life: Results from the AMSTEL study. Intl J Geriatric Psychiatr 2003;18:994–1001 [DOI] [PubMed] [Google Scholar]
- 87.Schoevers R, Deeg D, van Tilburg W, Beekman A. Depression and generalized anxiety disorder: Co-occurrence and longitudinal patterns in elderly patients. Am J Geriatric Psychiatr 2005;13:31–39 [DOI] [PubMed] [Google Scholar]
- 88.Forsell Y, Winblad B. Feelings of anxiety and associated variables in a very elderly population. Intl J Geriatric Psychiatr 1998;13:454–458 [DOI] [PubMed] [Google Scholar]
- 89.Ford E, Merritt R, Heath G, et al. . Physical activity behaviors in lower and higher socioeconomic status populations. Am J Epidemiol 1991;133:1246–1255 [DOI] [PubMed] [Google Scholar]
- 90.Orner P. Psychosocial impacts on caregivers of people living with AIDS. AIDS Care 2006;18:236–240 [DOI] [PubMed] [Google Scholar]
- 91.Duwell MM, Knowlton AR, Nachega JB, et al. . Patient-nominated, community-based HIV treatment supporters: Patient perspectives, feasibility, challenges, and factors for success in HIV-infected South African adults. AIDS Patient Care STDS 2013;27:96–102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Doherty T, Tabana H, Jackson D, et al. . Effect of home based HIV counselling and testing intervention in rural South Africa: Cluster randomised trial. BMJ 2013;346:3481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Madiba S, Letsoalo R. HIV disclosure to partners and family among women enrolled in prevention of mother to child transmission of HIV program: Implications for infant feeding in poor resourced communities in South Africa. Glob J Health Sci. 2013;5:1–13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Palin FL, Armistead L, Clayton A, et al. . Disclosure of maternal HIV-infection in South Africa: Description and relationship to child functioning. AIDS Behav 2009;13:1241–1252 [DOI] [PubMed] [Google Scholar]
- 95.Qiao S, Li X, Zhao G, Zhao J, Stanton B. Secondary disclosure of parental HIV status among children affected by AIDS in Henan, China. AIDS Patient Care STDS 2012;26:546–556 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Rochat TJ, Mkwanazi N, Bland R. Maternal HIV disclosure to HIV-uninfected children in rural South Africa: A pilot study of a family-based intervention. BMC Public Health 2013February18;13:147, doi: 10.1186/1471-2458-13-147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Murphy DA, Armistead L, Marelich WD, Payne DL, Herbeck DM. Pilot trial of a disclosure intervention for HIV+ mothers: The TRACK program. J Consult Clin Psychol 2011;79:203–214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Bhana A, Mellins CA, Petersen I, et al. . The VUKA family program: Piloting a family-based psychosocial intervention to promote health and mental health among HIV infected early adolescents in South Africa. AIDS Care 2014;26:1–11 [DOI] [PMC free article] [PubMed] [Google Scholar]