Abstract
Background: Primary thyroid lymphoma (PTL) develops mostly in middle-aged and older females. However, the optimal treatment for elderly patients with diffuse large B-cell lymphoma (DLBCL), which accounts for most PTL cases, is unclear. Rituximab is a promising drug that, in combination with traditional combination therapy, has demonstrated an increased antitumor effect without a substantial increase in toxicity. In this study, treatment outcomes of elderly patients with thyroid DLBCL who underwent rituximab-including combination therapy were analyzed.
Method: Between January 2005 and December 2011, 43 patients 60 years of age or older (median 71 years, range 60–80 years) were diagnosed as having stage IE (n=12) or stage IIE (n=31) DLBCL, and three courses of R-CHOP therapy (rituximab 375 mg/m2, cyclophosphamide 750 mg/m2, adriamycin 40 mg/m2, vincristine 1.4 mg/m2, and prednisolone 100 mg/body) and involved field irradiation were planned. Treatment outcomes of these patients were retrospectively reviewed.
Results: Two patients terminated the treatment because of interstitial pneumonia during R-CHOP therapy. Only one patient showed treatment resistance and the regimen was changed; 42 patients (98%) responded to the treatment. Five-year overall survival and event-free survival were 87% (95% confidence interval [95% CI], 64–96%) and 74% (95% CI, 50–89%), respectively.
Conclusion: The results of the present study indicate that rituximab-including combination therapy was effective for elderly patients with thyroid DLBCL. A multicenter, long-term observational study is needed to confirm this, and additional refinement of the treatment protocol is required to optimize the antitumor effect.
Introduction
Primary thyroid lymphoma (PTL) is a rare disease that accounts for approximately 1–2% of all extranodal malignant lymphomas (1). It usually develops in older females (2,3); the median age is 66 years (4). Approximately 90% of patients present with stage IE or IIE disease at diagnosis (2,4). Approximately 90% of these tumors are classified as B-cell lymphoma, which include mucosa-associated-lymphoid tissue (MALT; 10% of total PTL) lymphoma and diffuse large B-cell lymphoma (DLBCL; 69% of total PTL) in large-scale case series (4).
In the past, treatment for thyroid lymphoma centered on surgical resection (5). In recent years, however, a number of groups including our own have reported improved outcomes with the introduction of combined modality therapy (CMT) using the standard treatment for malignant lymphoma in the localized stage, and actual 5-year survival rates of over 80% can be expected (4,6,7). At the same time, recurrence is a major problem. More than 10% of patients in our study had recurrences, which were an obstacle to improved treatment outcomes (6). To overcome this problem, modified treatments to increase the antitumor effect need to be introduced. However, especially in thyroid lymphoma, which primarily afflicts the elderly, there is concern about an increase in adverse events as a result of increased treatment intensity. Balancing the two is difficult, and it remains unclear what kind of treatment strategy should be adopted with these patients. The same applies to nodal malignant lymphomas (8,9).
Rituximab is a promising drug that can be used in elderly people without major adverse effects; it has been shown that an antitumor effect can be expected without an increase in adverse events even in elderly people (10). At Ito Hospital, a major treatment center for thyroid diseases, we have used rituximab-including CMT to treat elderly patients with malignant lymphoma of the thyroid since 2005 (11). With this regimen, a decrease in the recurrence rate is expected without increasing adverse events. This study reviewed those results.
Patients and Methods
Treatment for PTL
In general, all patients with stage IE or stage IIE aggressive B-cell PTL including DLBCL and DLBCL with MALT lymphoma have received rituximab-including CMT at Ito Hospital since 2005. Radiation therapy (RT) encompassed the whole of the neck and the upper mediastinum. CMT usually included RT and three courses of R-CHOP (rituximab 375 mg/m2, cyclophosphamide 750 mg/m2, adriamycin 40 mg/m2, vincristine 1.4 mg/m2, and prednisolone 100 mg/body)-based chemotherapy. As premedication for rituximab, 400 mg of acetaminophen and 30 mg of diphenhydramine hydrochloride were administered. The dosage of adriamycin was modified to 50 mg/m2 since 2012. Patients with Eastern Cooperative Oncology Group performance status 2 or more or with severe comorbidities were excluded.
Patient selection and clinical records
Between January 2005 and December 2011, 56 patients 60 or more years of age were diagnosed as having stage IE or stage IIE aggressive B-cell PTL at Ito Hospital. Of these, 9 patients were transferred to other hospitals. Three patients aged 80 years or older who underwent local irradiation alone and 1 patient with severe diabetes who underwent bendamustine rituximab therapy were excluded. Subsequently, 43 patients were planned to receive rituximab-including CMT at Ito Hospital and JR Tokyo General Hospital, which is a collaborating hospital of Ito Hospital, and the medical records of these patients were retrospectively reviewed. To screen for infectious diseases, hepatitis B surface antigen, hepatitis C virus antibody, and human immunodeficiency virus antibody were checked in all patients. If a patient had a high-risk history of hepatitis B virus infection, hepatitis B core and surface antibodies were also checked. According to the Japanese guidelines, preemptive therapy for hepatitis B virus reactivation was planned (12). Human T-cell leukemia virus type I antibody was not routinely examined unless the patient had a high-risk history.
Definitions and statistical analysis
PTL is defined as a lymphoma developing in the thyroid gland with or without involvement of regional lymph nodes or other visceral tissues (2). The inclusion criteria were histologically proven, aggressive B-cell lymphoma of the thyroid gland, localized disease, and age ≥60 years. Only patients with lymphoma primarily involving the thyroid gland were included (13). The role of surgery was mainly focused on diagnostic biopsies; excision biopsy was performed in all 43 patients. All patients were diagnosed based on histologic examination of thyroid tissue specimens. The clinical stage was evaluated by ultrasonography (n=43), computed tomography (n=43), 67Ga-citrate-scintigraphy (n=43), and bone marrow aspiration biopsy (n=40), using the following criteria. Namely, stage IE applies to disease localized within the thyroid; stage IIE applies to disease confined to the thyroid and regional lymph nodes; stage IIIE applies to disease that involves the thyroid, the lymph nodes on both sides of the diaphragm, and/or the spleen; and stage IVE is used for disseminated disease (5,14). Pathologic diagnosis was based on WHO classifications (15).
Follow-up data were calculated from the time of initial surgery on the thyroid gland to the last follow-up. The clinical follow-up was obtained from patient records, oral communication with the patients and their families, and communication with the referring physicians. This study was approved by the Institutional Review Board of Ito Hospital.
A relapse of PTL was defined as the involvement of new sites, recurrence in originally involved sites, or a greater than 25% increase in the size of the original tumor masses. A complete response was defined as the disappearance of all documented disease. A partial response was defined as a reduction of at least 50% in the largest diameter of every measurable lesion (16).
The data were analyzed as of October 2012. Overall survival (OS) and event-free survival (EFS) were estimated by the Kaplan-Meier method. OS was calculated from the time of initial surgery on the thyroid gland to death from any cause, and EFS was defined as the time from initial surgery on the thyroid gland to the absence of at least a partial response on the intermediate evaluation, relapse, or death in remission. For analysis of OS, data on patients who were alive at the last follow-up contact were censored. For the analysis of EFS, data on patients who were alive without any progression of the primary disease at the last follow-up were censored. JMP version 10.0.2 (SAS Institute Inc., Cary, NC) was used for all statistical analyses.
Results
Patients' characteristics
The characteristics of the 43 patients are shown in Table 1. CMT was planned in these 43 patients, but radiation could not be performed in 3 patients after R-CHOP, so they only received chemotherapy. In 2 of these, it was because of the development of interstitial pneumonia after R-CHOP, and in 1 because of sudden tumor enlargement seen on day 16 of R-CHOP course 2, judged to be a rapid progression of disease. The treatment regimen was changed from the third course onward. Of the 43 patients, 27 were older than 70 years of age. No patient was positive on the routine tests for infectious diseases, including human immunodeficiency virus and hepatitis B and C viruses. No patient received preemptive therapy. The characteristics of these patients aged above 70 years are also shown in Table 1.
Table 1.
Patients' Characteristics and the Treatment of Primary Thyroid Lymphoma
| Variables | Patients aged above 60 years Number (%) | Patients aged above 70 years Number (%) |
|---|---|---|
| No. of patients | 43 | 26 |
| Age (median [range]) (years) | 71 [60–86] | 75 [70–86] |
| Sex (male/female) | 14/29 (33/67) | 9/17 (35/65) |
| Hashimoto's disease | 37 (86) | 23 (88) |
| Pathologic diagnosis | ||
| DLBCL | 32 (74) | 22 (85) |
| DLBCL with MALT lymphoma | 11 (26) | 4 (15) |
| Laboratory tests at diagnosis | ||
| Elevated LDH | 16 (41) | 11 (48) |
| ESR (median [range]) (mm) | 26 [2–82] | 27 [3–75] |
| Free T3 (median [range]) (pg/mL) | 2.8 [2.3–3.5]a | 2.8 [2.3–3.3]a |
| Free T4 (median [range]) (ng/dL) | 1.1 [0.5–1.7]a | 1.1 [0.5–1.7]a |
| TSH (median [range]) (μIU/mL) | 4.2 [0.1–97]a | 5.4 [0.1–97]a |
| TSH (decreased/normal range/elevated) | 1/14/14 (3.4/48.3/48.3)a | 1/7/18 (4/27/69)a |
| sIL-2R (median [range]) (U/mL) | 639 [234–2850] | 716 [298–2850] |
| Clinical stage (IE/IIE) | 12/31 (28/ 72) | 7 19 (27/ 73) |
| Treatment | ||
| Chemotherapy (alone/with irradiation) | 4/39 (9/ 91) | 4/22 (15/ 85) |
| R-CHOP (1–3/4–6 courses) | 41/2 (95/5) | 25/1b (96/4) |
| Doses of irradiation (median [range]) (gray) | 36 [30–40] | 36 [30–40] |
| Dosage of R-CHOP therapy (median [range]) | ||
| R/BSA (mg/m2){%}c | 375 [273–392] {100 [73–104]} | 375 [273–392] {100 [73–105]} |
| CPA/BSA (mg/m2){%} | 750 [413–758] {100 [55–101]} | 736 [413–758] {98 [55–101]} |
| VCR/BSA (mg/m2){%} | 1.2 [0.6–1.4] {87 [45–100]} | 1.1 [0.6–1.4] {80 [45–100]} |
| ADM/BSA(mg/m2){%} | 40 [26–49] {79 [52–98]} | 39 [26–40] {79 [52–81]} |
| PSL/body (mg/body) | 100 [0–100] | 100 [0–100] |
Patients with thyroid hormone replacement therapy were excluded.
For one patient, after six courses of R-CHOP therapy and irradiation, rituximab was added four times monthly.
A percentage of the conventional dose.
DLBCL, diffuse large B-cell lymphoma; MALT, mucosa-associated lymphoid tissue; LDH, lactase dehydrogenase; ESR, erythrocyte sedimentation rate; T3, triiodothyronine; T4, thyroxine; TSH, thyrotropin; R, rituximab; CPA, cyclophosphamide; VCR, vincristine; ADM, adriamycin; PSL, prednisolone; BSA, body surface area.
Treatment response
Treatment response was defined as a reduction of 50% or more in the largest diameter of every measurable lesion (i.e., a partial response or better). Treatment was successful in 42 of the 43 patients (98%). In the remaining patient (2%), the tumor grew rapidly in the second course and was judged to be progression of disease.
Adverse effects
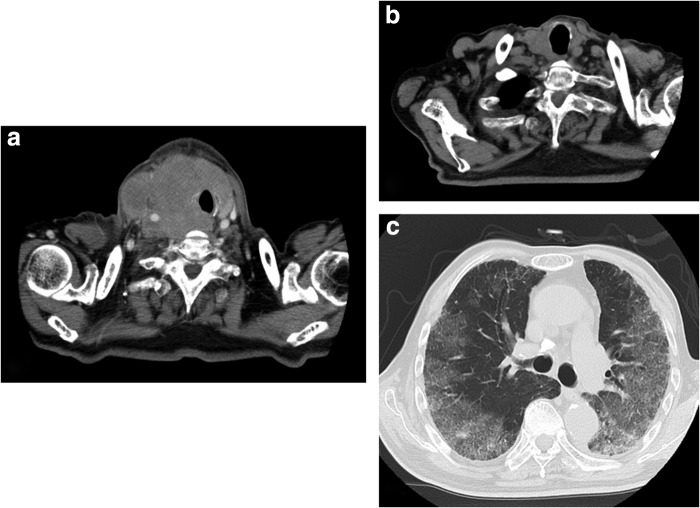
Adverse effects related to treatment are shown in Table 2. Two patients developed interstitial pneumonia, and one patient died. The patient who died was an 86 year-old man with malignant lymphoma, diffuse large B-cell type, stage IIE. He had airway constriction caused by compression by the tumor, and he was given rituximab on the first day after admission. This relieved the airway constriction. From day 19, the first course of R-CHOP was conducted with 70% of the conventional dose of vincristine and adriamycin. The second course was started from hospital day 41 at the same dose, but respiratory discomfort occurred early in the morning of hospital day 52 (day 12 of the second course of R-CHOP), and hypoxemia was seen. On computed tomography (CT), both lung fields showed diffuse ground-glass opacities (Fig. 1). Oxygen was administered, and steroid pulse therapy was started, but oxygenation was poor and he was transferred to another hospital for intensive care. Soon after the transfer, he was intubated, and steroid pulse therapy was performed three times, but his respiratory status deteriorated every time the steroid dose was decreased. Pneumothorax also occurred, and he died on day 93. No evidence indicating infection, including Pneumocystis (carinii) jirovecii, was seen on microscopic examination, culture, and polymerase chain reaction of bronchoalveolar lavage fluid collected soon after the transfer. Another patient developed interstitial pneumonia after three courses of R-CHOP. Steroid administration was successful, but the patient's performance status decreased, and RT was not performed. In these two patients, the serum β-D-glucan level was not elevated. The possibility of Pneumocystis (carinii) jirovecii pneumonia was clinically ruled out based on the course of the interstitial pneumonia.
Table 2.
Adverse Events of R-CHOP Therapy
| Patients aged above 60 years (n=43) any AE/AE ≥grade 3 | Patients aged above 70 years (n=26) any AE/AE ≥grade 3 | |
|---|---|---|
| Adverse events (n, %) | ||
| Infusion reaction | 6/0 (14/0) | 3/0 (12/0) |
| Neutropenia | 42/42 (98/98) | 25/25 (96/96) |
| Neuropathy | 13/0 (30/0) | 8/0 (31/0) |
| Nausea | 13/0 (30/0) | 6/0 (23/0) |
| Vomiting | 5/0 (12/0) | 2/0 (8/0) |
| Pneumonia | 17/2 (37/4) | 10/2 (31/8) |
| Esophagitis | 28/0 (64/0) | 15/0 (58/0) |
| Mucositis, oral | 6/0 (14/0) | 4/0 (15/0) |
| Dry mouth | 5/0 (12/0) | 3/0 (12/0) |
| Skin disorders | 7/0 (16/0) | 3/0 (12/0) |
Adverse events were graded based on Common Terminology Criteria for Adverse Events version 4.0.
FIG. 1.
Computed tomography images of a 86-year-old man with malignant lymphoma, diffuse large B-cell type, stage IIE, developing interstitial pneumonia on therapy with R-CHOP. Day 1 (a), day 19 (b), and day 58 (c).
Of the 43 patients, 6 developed infusion reactions, including a skin eruption (n=3) and fever (n=3). These were successfully resolved in all 6 patients with the addition of antihistamine (n=3) or without any medication (n=3).
Survival
OS and EFS of the 43 patients are shown in Figure 2. Five-year OS and EFS were 87% (95% confidence interval [95% CI], 64–96%) and 74% (95% CI, 50–89%), respectively.
FIG. 2.
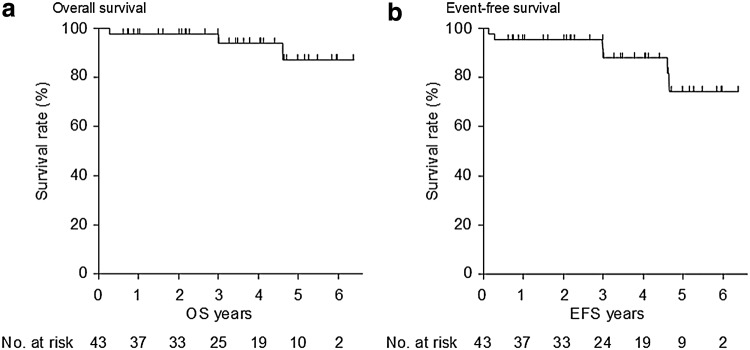
Overall (a) and event-free (b) survivals.
Relapse occurred in 2 patients after the completion of therapy. Relapse was seen in the thyroid 4.5 years after treatment in 1 patient, and in the thyroid, right hilar region, and tracheal bifurcation lymph node 3.0 years after treatment in 1 patient. In both cases, recurrence was in the radiation exposure fields. Causes of death included pneumonia (n=2) and lung cancer (n=1). The median follow-up of the surviving patients was 42 months (range, 1–78 months). OS and EFS of patients older than 70 years of age were 77% (95% CI, 43–94%) and 69% (95% CI, 40–88%), respectively.
Discussion
There have been no reported studies focusing on the treatment of elderly patients with PTL, and several important findings were revealed for the first time in this study.
First, it was shown that rituximab-including CMT is effective even in elderly patients with aggressive PTL. Chemotherapy resistance was seen in one patient in this study, and scheduled radiotherapy could not be performed, but the treatment was successful in all of the remaining patients. The response rate was 98%. There are few reports on treatment outcomes for malignant lymphoma of the thyroid in the localized stage limited to elderly patients, but it is comparable to the response rate in our hospital (91%) from 1990 to 2004 before the introduction of rituximab.
Interestingly, there was considerable improvement in OS. Before the introduction of rituximab, the 5-year survival rate for patients of the same age group in the localized stage who were treated with CMT at our hospital was 71%, but after the introduction of rituximab, it improved to 90%. This was likely due mainly to a decrease in the percentage of patients with relapse, from 21% to 7%. The dose of cytotoxic agents was the same as before, suggesting an add-on effect of rituximab. Rituximab has been reported to effectively lower the recurrence rate after remission is achieved even in elderly patients with nodal aggressive lymphoma (17), and the same result can be expected in elderly PTL patients.
Inability to control the primary disease is an issue in some patients. One patient showed treatment resistance, and in two patients there was localized recurrence. The finding in a previous study that nearly all posttreatment recurrences in localized stage patients were at distant sites is in contrast to the results of the present study. Although no definitive conclusion can be reached because of the small number of patients, it may be that the present treatment regimen did not have a sufficient local antitumor effect on the periphery of the primary tumor. Relapse occurred in the irradiation field in all relapse cases, but the doses of irradiation (Table 1) in this study cannot be considered small in comparison to widely used radiotherapy treatments (18); thus, increasing the intensity of radiation therapy to prevent local recurrence is probably not realistic. Intensifying chemotherapy to enhance the antitumor effect could also be considered, but there is the problem of the greater likelihood of adverse effects in elderly people than in young people, and it is not known whether that approach could be adopted for PTL.
Further study is needed with regard to the safety of this treatment in elderly patients. Severe lung damage occurred in two patients, and the scheduled treatment had to be discontinued. Moreover, one of them died. The occurrence of interstitial pneumonia in patients who receive R-CHOP has been previously reported. Although infrequent, it is sometimes severe. The causes are unknown, and methods of prevention have not been established. Good responses with low recurrence are reported with steroid treatment (19–22). Although interstitial pneumonia cannot be considered frequent in elderly patients (21), once it occurs, it tends to become severe patients with low reserve organ capacity. Thus, greater attention should be paid to the possibility of this complication in elderly people than in young people.
In this study, excision biopsy was performed in all 43 patients. All patients were diagnosed based on histologic examination of thyroid tissue specimens. Some researchers have suggested that fine-needle biopsy and core-needle biopsy with flow cytometry are useful and less invasive techniques (5,23). However, the more limited specimen obtained by core biopsy than by surgical excision biopsy is usually not representative of the entire tumor, particularly in the case of coexisting MALT and DLBCL histologies. Thus, surgical excision biopsy continues to play an important role in assessing these aggressive histologies. By contrast, in the treatment for PTL, the role of surgical intervention for thyroid DLBCL is limited. Because of the typically aggressive clinical course, the mainstay of treatment for DLBCL is a combination of chemotherapy and radiotherapy. However, surgical intervention may be required for palliation in the setting of critical airway obstruction in patients with DLBCL due to tumor compression or invasion (24).
Several limitations to this study should be noted. First, it is the possible that more accurate evaluation of clinical stage based on CT due to advances in resolution, particularly the ability to exclude patients with minute distant lesions that tended to be missed in the era before rituximab, has produced improvements in prognosis compared with outcomes before rituximab. Second, fluorine-18-fluorodeoxyglucose positron emission tomography (FDG-PET) scanning was not routinely performed in this study. Recent studies have suggested that FDG-PET has superior accuracy in staging of lymphoma compared to computed tomography or magnetic resonance imaging (25). It may provide more accurate staging in thyroid lymphoma (26,27); therefore, some patients in our study might be diagnosed as having more advanced clinical stage lymphoma. Future studies will allow a proper interpretation. Finally, this study was a small-scale, retrospective study. The effects of an unrecognized bias cannot be ruled out.
In summary, this study demonstrates the utility of the treatment strategy of adding rituximab to CMT chemotherapy in elderly patients with PTL. Confirmation of the utility of this treatment in a future multicenter study with longer follow-up and further refinement of treatment strategies to obtain better antitumor effects are desired.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Freeman C, Berg JW, Cutler SJ.1972Occurrence and prognosis of extranodal lymphomas. Cancer 29:252–260 [DOI] [PubMed] [Google Scholar]
- 2.Derringer GA, Thompson LD, Frommelt RA, Bijwaard KE, Heffess CS, Abbondanzo SL.2000Malignant lymphoma of the thyroid gland: a clinicopathologic study of 108 cases. Am J Surg Pathol 24:623–639 [DOI] [PubMed] [Google Scholar]
- 3.Zinzani PL, Magagnoli M, Galieni P, Martelli M, Poletti V, Zaja F, Molica S, Zaccaria A, Cantonetti AM, Gentilini P, Guardigni L, Gherlinzoni F, Ribersani M, Bendandi M, Albertini P, Tura S.1999Nongastrointestinal low-grade mucosa-associated lymphoid tissue lymphoma: analysis of 75 patients. J Clin Oncol 17:1254. [DOI] [PubMed] [Google Scholar]
- 4.Graff-Baker A, Roman SA, Thomas DC, Udelsman R, Sosa JA.2009Prognosis of primary thyroid lymphoma: demographic, clinical, and pathologic predictors of survival in 1,408 cases. Surgery 146:1105–1115 [DOI] [PubMed] [Google Scholar]
- 5.Graff-Baker A, Sosa JA, Roman SA.2010Primary thyroid lymphoma: a review of recent developments in diagnosis and histology-driven treatment. Curr Opin Oncol 22:17–22 [DOI] [PubMed] [Google Scholar]
- 6.Watanabe N, Noh JY, Narimatsu H, Takeuchi K, Yamaguchi T, Kameyama K, Kobayashi K, Kami M, Kubo A, Kunii Y, Shimizu T, Mukasa K, Otsuka F, Miyara A, Minagawa A, Ito K.2011Clinicopathological features of 171 cases of primary thyroid lymphoma: a long-term study involving 24 553 patients with Hashimoto's disease. Br J Haematol 153:236–243 [DOI] [PubMed] [Google Scholar]
- 7.Onal C, Li YX, Miller RC, Poortmans P, Constantinou N, Weber DC, Atasoy BM, Igdem S, Ozsahin M, Ozyar E.2011Treatment results and prognostic factors in primary thyroid lymphoma patients: a rare cancer network study. Ann Oncol 22:156–164 [DOI] [PubMed] [Google Scholar]
- 8.Armitage JO.2007How I treat patients with diffuse large B-cell lymphoma. Blood 110:29–36 [DOI] [PubMed] [Google Scholar]
- 9.Fields PA, Linch DC.2012Treatment of the elderly patient with diffuse large B cell lymphoma. Br J Haematol 157:159–170 [DOI] [PubMed] [Google Scholar]
- 10.Coiffier B, Lepage E, Briere J, Herbrecht R, Tilly H, Bouabdallah R, Morel P, Van Den Neste E, Salles G, Gaulard P, Reyes F, Lederlin P, Gisselbrecht C.2002CHOP chemotherapy plus rituximab compared with CHOP alone in elderly patients with diffuse large-B-cell lymphoma. N Engl J Med 346:235–242 [DOI] [PubMed] [Google Scholar]
- 11.Momotani N, Noh J, Oyanagi H, Ishikawa N, Ito K.1986Antithyroid drug therapy for Graves' disease during pregnancy. Optimal regimen for fetal thyroid status. N Engl J Med 315:24–28 [DOI] [PubMed] [Google Scholar]
- 12.The Japan Society of Hepatology. 2013 Guidelines for the Management of Hepatitis B Virus Infection v1.2 [in Japanese]. www.jsh.or.jp/medical/guidelines/jsh_guidlines/hepatitis_b (Last accessed March7, 2014)
- 13.Bonnet C, Fillet G, Mounier N, Ganem G, Molina TJ, Thieblemont C, Ferme C, Quesnel B, Martin C, Gisselbrecht C, Tilly H, Reyes F.2007CHOP alone compared with CHOP plus radiotherapy for localized aggressive lymphoma in elderly patients: a study by the Groupe d'Etude des Lymphomes de l'Adulte. J Clin Oncol 25:787–792 [DOI] [PubMed] [Google Scholar]
- 14.Lister TA, Crowther D, Sutcliffe SB, Glatstein E, Canellos GP, Young RC, Rosenberg SA, Coltman CA, Tubiana M.1989Report of a committee convened to discuss the evaluation and staging of patients with Hodgkin's disease: Cotswolds meeting. J Clin Oncol 7:1630–1636 [DOI] [PubMed] [Google Scholar]
- 15.Harris NL, Jaffe ES, Diebold J, Flandrin G, Muller-Hermelink HK, Vardiman J.2000Lymphoma classification—from controversy to consensus: the R.E.A.L. and WHO classification of lymphoid neoplasms. Ann Oncol 11(Suppl 1):3–10 [PubMed] [Google Scholar]
- 16.Cheson BD, Pfistner B, Juweid ME, Gascoyne RD, Specht L, Horning SJ, Coiffier B, Fisher RI, Hagenbeek A, Zucca E, Rosen ST, Stroobants S, Lister TA, Hoppe RT, Dreyling M, Tobinai K, Vose JM, Connors JM, Federico M, Diehl V.2007Revised response criteria for malignant lymphoma. J Clin Oncol 25:579–586 [DOI] [PubMed] [Google Scholar]
- 17.Feugier P, Van Hoof A, Sebban C, Solal-Celigny P, Bouabdallah R, Ferme C, Christian B, Lepage E, Tilly H, Morschhauser F, Gaulard P, Salles G, Bosly A, Gisselbrecht C, Reyes F, Coiffier B.2005Long-term results of the R-CHOP study in the treatment of elderly patients with diffuse large B-cell lymphoma: a study by the Groupe d'Etude des Lymphomes de l'Adulte. J Clin Oncol 23:4117–4126 [DOI] [PubMed] [Google Scholar]
- 18.Harada H, Inoue M, Itasaka S, Hirota K, Morinibu A, Shinomiya K, Zeng L, Ou G, Zhu Y, Yoshimura M, McKenna WG, Muschel RJ, Hiraoka M.2012Cancer cells that survive radiation therapy acquire HIF-1 activity and translocate towards tumour blood vessels. Nat Commun 3:783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zayen A, Rais H, Rifi H, Ouarda M, Afrit M, Cherif A, Mezline A.2011Rituximab-induced interstitial lung disease: case report and literature review. Pharmacology 87:318–320 [DOI] [PubMed] [Google Scholar]
- 20.Katsuya H, Suzumiya J, Sasaki H, Ishitsuka K, Shibata T, Takamatsu Y, Tamura K.2009Addition of rituximab to cyclophosphamide, doxorubicin, vincristine, and prednisolone therapy has a high risk of developing interstitial pneumonia in patients with non-Hodgkin lymphoma. Leuk Lymphoma 50:1818–1823 [DOI] [PubMed] [Google Scholar]
- 21.Wagner SA, Mehta AC, Laber DA.2007Rituximab-induced interstitial lung disease. Am J Hematol 82:916–919 [DOI] [PubMed] [Google Scholar]
- 22.Ennishi D, Terui Y, Yokoyama M, Mishima Y, Takahashi S, Takeuchi K, Ikeda K, Tanimoto M, Hatake K.2008Increased incidence of interstitial pneumonia by CHOP combined with rituximab. Int J Hematol 87:393–397 [DOI] [PubMed] [Google Scholar]
- 23.Novoa E, Gurtler N, Arnoux A, Kraft M.2012Role of ultrasound-guided core-needle biopsy in the assessment of head and neck lesions: a meta-analysis and systematic review of the literature. Head Neck 34:1497–1503 [DOI] [PubMed] [Google Scholar]
- 24.Sippel RS, Gauger PG, Angelos P, Thompson NW, Mack E, Chen H.2002Palliative thyroidectomy for malignant lymphoma of the thyroid. Ann Surg Oncol 9:907–911 [DOI] [PubMed] [Google Scholar]
- 25.Baba S, Abe K, Isoda T, Maruoka Y, Sasaki M, Honda H.2011Impact of FDG-PET/CT in the management of lymphoma. Ann Nucl Med 25:701–716 [DOI] [PubMed] [Google Scholar]
- 26.Treglia G, Del Ciello A, Di Franco D.2013Recurrent lymphoma in the thyroid gland detected by fluorine-18-fluorodeoxyglucose PET/CT. Endocrine 43:242–243 [DOI] [PubMed] [Google Scholar]
- 27.Nakadate M, Yoshida K, Ishii A, Koizumi M, Tochigi N, Suzuki Y, Ryu Y, Nakagawa T, Umehara I, Shibuya H.2013Is 18F-FDG PET/CT useful for distinguishing between primary thyroid lymphoma and chronic thyroiditis? Clin Nucl Med 38:709–714 [DOI] [PubMed] [Google Scholar]