Abstract
Objectives: Unplanned pregnancy is a public health problem in the United States, including in rural areas. Primary care physicians are the main providers of health care to women in rural areas and are uniquely positioned to help reduce unplanned pregnancy in rural women. This study documents provision of contraception by rural primary care physicians, focusing on the most effective, long acting methods, intrauterine devices (IUDs) and contraceptive implants.
Methods: We surveyed all primary care physicians practicing in rural areas of Illinois and Wisconsin. Bivariate analysis was performed using chi squared and Fisher's exact test, and multivariable analysis was performed with logistic regression to determine factors associated with provision.
Results: The response rate was 862 out of 2312 physicians (37%). Nine percent of respondents place implants and 35% place IUDs. Eighty-seven percent of physicians had not had training in implant placement, and 41% had not had training in IUD placement. In multivariable analysis, factors associated with placement of long acting contraception include provision of maternity care, and female gender of the physician. The most common reasons for not providing the methods were lack of training and perceived low demand from patients.
Conclusions: Many rural primary care providers do not place long acting contraceptive devices due to lack of training. Female physicians and those providing maternity care are the most likely to place these devices. Increased training for primary care physicians both during and after residency would help increase access to these options for women in rural areas.
Introduction
Women living in rural areas of the United States face health disparities compared with urban and suburban women.1 These disparities include low rates of health screening, and poor reproductive health outcomes, including high teen pregnancy rates.2 Most national data about unplanned pregnancies and contraceptive use are not analyzed by geographic location. However, because women in rural areas have high poverty rates, low levels of education and are less likely to have insurance compared to urban women, all of which are associated with unplanned pregnancy,1 they may also be likely to have high rates of unplanned pregnancy and low rates of effective contraceptive use.3
Highly effective, long acting methods of contraception such as intrauterine devices (IUDs) and contraceptive implants have the lowest failure rates of reversible methods, and the highest user satisfaction.4 However, only a small number of U.S. women use these methods.5 Increased use of these methods could help to reduce the number of unplanned pregnancies experienced by U.S. women.
The majority of rural physicians specialize in family medicine and general internal medicine. These primary care physicians are the main providers of preventative health services and family medicine physicians provide the majority of maternity care to women in rural areas.6 Rural women rely on their primary care physicians for contraception and reproductive health care.
In a survey of rural physicians practicing in Idaho in 1994, 67% of family physicians placed the contraceptive implant, and 50% placed IUDs.7 In a more recent national survey of family physicians, only 24% of the respondents had placed an IUD in the last year.8 Other evidence suggests that rural providers may be less likely than urban providers to recommend the long acting methods: a study of publicly funded Title X family planning clinics in Texas found that rural family planning providers were less likely to have training in placement of the long acting methods and had less favorable attitudes towards these methods compared to providers in urban family planning clinics.9
The objective of this study is to describe current provision of long acting contraceptive methods and barriers to placing these devices for primary care physicians in rural Illinois and Wisconsin, in addition to understanding referral patterns for physicians who do not place these contraceptive devices.
Materials and Methods
Survey development
The survey was developed based on prior surveys of rural physicians and provision of IUDs by family physicians7,8 and in consultation with survey researchers at the University of Illinois Survey Research Lab and the Wisconsin Research and Education Network. Five rural physicians were interviewed to aid in survey and question design. The survey assessed the following: (1) contraceptive provision, with an emphasis on contraceptive implant and intrauterine device placement, (2) provision of maternity care, (3) procedural gynecological care such as performance of endometrial biopsies, (4) reasons for not placing the long acting contraceptive devices, and (5) physicians' perceptions of barriers to device placement.
Sample
The sample consisted of all primary care physicians including family medicine and internal medicine physicians, general practitioners and medicine/pediatrician specialists practicing in rural Illinois and Wisconsin. Both of these states have large rural populations and rural medicine physician training programs within their state medical schools. Physicians were identified from state licensing data. In Wisconsin licensing data, the specialty of the physician was available. For the Illinois physicians, this information was not available in state licensing data, and was obtained using internet searches of publically available practice information. Rural location was defined by a code of four or higher in the rural-urban commuting area (RUCA) zip code approximation. RUCA codes are a classification of rural location developed and maintained by the University of Washington Rural Health Research Center.1 Exclusion criteria were resident physicians in training, not practicing primary care, not practicing in a rural area, not currently in clinical practice or not treating any reproductive age women.
Participant recruitment
Physicians received a letter in the mail inviting them to participate in an online survey. They also received a $2 bill incentive in the initial mailing. Physicians who did not respond to the first mailing were sent a second letter asking them to participate in the web survey. Physicians who did not respond to either the first or the second mailing were sent a third letter with the paper version of the survey and a stamped return envelope. Physicians were offered a $20 gift card after completion of the survey. The survey was conducted from November 2011 to April 2012.
Statistical analysis
We analyzed the data using SAS (version 9.2, SAS Institute Inc.). Bivariate analysis using the chi squared test or Fisher's exact test was used to compare demographic and other characteristics of the physicians. We performed multivariable logistic regression modeling to determine the associations between physician characteristics and placement of the contraceptive devices.
The University of Illinois Hospital and Health Sciences Institutional Review Board approved this research.
Results
Survey response
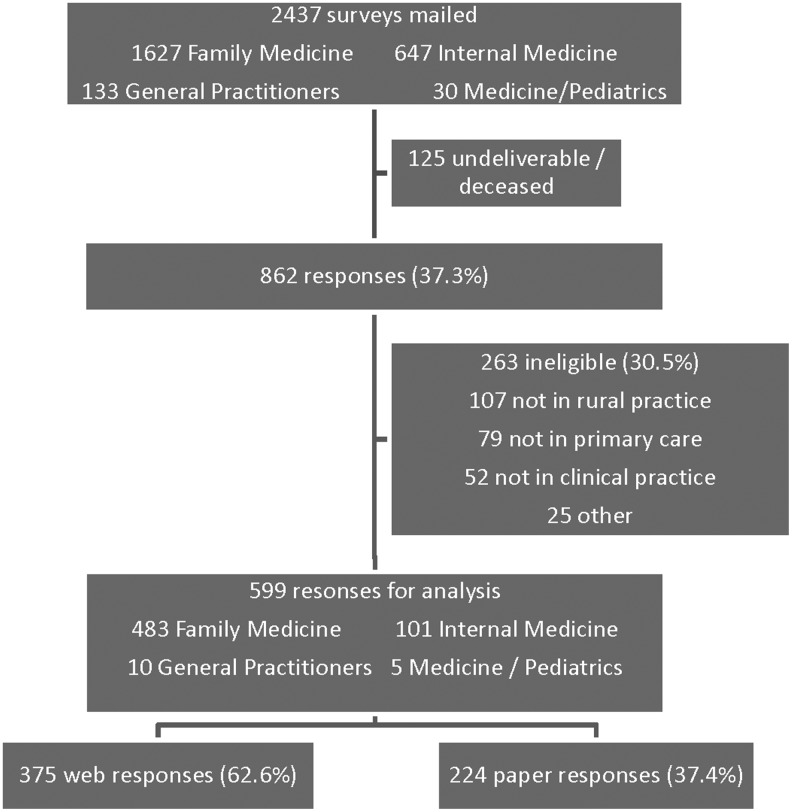
Surveys were mailed to 2,437 physicians (Figure 1). One hundred twenty-five letters were returned undeliverable. A total of 862 physicians responded, for a response rate of 37.3%. Of those that responded, 30.5% were ineligible. The most common reasons for ineligibility were zip code of practice not in a rural area, not in a primary care practice, or no longer in clinical practice. A total of 599 responses were appropriate for analysis. Of the physicians who responded, 62.6% completed the survey by web, and 37.4% completed the paper survey.
FIG. 1.
Survey distribution and response rates.
Response rates varied by specialty and state. The survey was mailed to 1627 family medicine physicians, 647 internal medicine physicians, 133 general practitioners, and 30 medicine/pediatrics physicians. Of the responses included in analysis, 483 were from family physicians (29.7% eligible response rate) and 101 were from internal medicine physicians (20.9% eligible response rate) (p<0.001). Ten general practitioners and five specialists in medicine/pediatrics returned eligible surveys, and their responses were included in the analysis as well. In Wisconsin, eligible responses were received from 401 of 1,359 physicians (29.5%), while the response from Illinois physicians was 198 out of 1,078 (18.4%) (p<0.0001).
Sample characteristics
Compared with internal medicine physicians, family physicians were younger (mean age 47.7 vs. 51.8 years, p<0.05), more likely to be female (36.4% vs. 23.8%, p<0.05), and had larger proportions of reproductive aged women in their practices (Table 1). Family physicians had a higher mean RUCA code for their practices (6.6 vs. 5.9, p<0.05), indicating they are located in more rural areas than are internal medicine physicians. In this sample, 34.9% of the family physicians practice obstetrics, while only 2% of internal medicine physicians do (p<0.05), as expected based on differences in residency training and scope of practice between the two specialties. More family physicians reported performing endometrial biopsies (51.7% compared with 5.0% of internal medicine physicians, p<0.05).
Table 1.
Characteristics of Family Medicine and Internal Medicine Respondents by Specialty*
| Family medicine (n=483) | Internal medicine (n=101) | p value | |
|---|---|---|---|
| Age, mean±SD | 47.7±10.9 | 51.8±10.5 | 0.0005 |
| Gender, n (%) | |||
| Female | 176 (36.4) | 24 (23.8) | 0.0146 |
| Male | 307 (63.6) | 77 (76.2) | |
| Percentage of reproductive aged female | |||
| patients in practice, n (%) | |||
| <25% | 114 (23.7) | 64 (63.4) | <0.0001 |
| 25%–49% | 267 (55.4) | 24 (23.8) | |
| 50%–74% | 87 (18.1) | 13 (12.9) | |
| 75&–100% | 14 (2.9) | 0 (0) | |
| Rural urban commuting area code, mean±SD | 6.6±2.1 | 5.9±2.3 | 0.0031 |
| Practice Obstetrics, n (%) | 168 (34.9) | 2 (2.0) | <0.0001 |
| Perform endometrial biopsies,n (%) | 250 (51.7) | 5 (5.0) | <0.0001 |
| Prescribe oral contraceptives, n (%) | 450 (93.4) | 60 (59.4) | <0.0001 |
| Place IUDs,n (%) | 205 (42.2) | 2 (1.8) | <0.0001 |
| Place implants, n (%) | 50 (10.3) | 1 (0.9) | <0.0001 |
| IUD training, n (%) | |||
| Residency | 291 (60.4) | 9 (8.9) | <0.0001 |
| After | 48 (10.0) | 1 (1.0) | |
| None | 143 (29.7) | 91 (90.0) | |
| Implant training, n (%) | |||
| Residency | 20 (4.2) | 2 (2.0) | 0.0028 |
| After | 54 (11.2) | 1 (1.0) | |
| None | 408 (84.7) | 98 (97.0) | |
Responses indicate current clinical practice.
IUD, intrauterine device; SD, standard deviation.
Family physicians were much more likely to have received training in placement of IUDs (70.4% vs. 9.9%, p<0.05) or implants (15.4% vs. 3%, p<0.05). Among physicians who did have training in IUD placement, the majority did so during residency (85.8% of family physicians and 90% of internal medicine physicians). For implants, however, the majority of family physicians with training did so post-residency (73.0% of those trained). Only three internal medicine physicians who responded to the survey had training in implant placement, two during residency. Forty-two percent of family physicians reported placing IUDs in their current practice, while only two internal medicine doctors did. Similarly, 10% of family physicians in the study place the contraceptive implant, while only one internist reported placing the implant. Fewer internal medicine physicians prescribe oral contraceptive pills (59% vs. 93%, p<0.05).
Predictors of IUD and implant placement
In the overall sample, 34.6% of respondents place IUDs, while only 8.7% currently place the implant (Table 2). In unadjusted analysis, female physicians, family medicine physicians, those performing endometrial biopsies, and those providing maternity care were more likely to place both methods. In multivariable analysis, controlling for the physician characteristics gender, age, specialty, maternity care, and training, providing maternity care was significantly associated with placing both IUDs (odds ratio [OR] 7.4, 95% confidence interval [CI] 4.3–12.7) and implants (OR 9.7, 95% CI 3.1–10.4), while female gender of the physician was significantly associated with placing IUDs (OR 2.2, 95% CI 1.3–3.7). We also found that physicians who were trained in placement of the methods after residency were more likely to place the methods than those who were trained during residency, in both unadjusted and adjusted analysis. Predictors of performing endometrial biopsies are not presented here as the focus of this analysis is on placement of the contraceptive devices.
Table 2.
Predictors of Placement of Intrauterine Devices and Contraceptive Implants by Rural Primary Care Physicians
| All respondents (n=599) | Place implant (n=52) | Unadjusted OR | Adjusted OR | Place IUDs (n=207) | Unadjusted OR | Adjusted OR | ||
|---|---|---|---|---|---|---|---|---|
| Total,n (%) | 599 (100) | 52 (8.7) | 207 (34.6) | |||||
| Gender, n (%) | ||||||||
| Male | 394 (64.8) | 23 (5.8) | ref | ref | 103 (26.1) | ref | ref | |
| Female | 205 (34.2) | 29 (14.1) | 2.7 (1.5–4.8) | 1.7 (0.5–5.3) | 104 (50.7) | 2.9 (2.0–4.1) | 2.2 (1.3– 3.7) | |
| Age, mean±SD | 48.3±11.0 | 43.7±10.2 | p<0.01 | ns | 45.8±10.6 | p<0.01 | ns | |
| Specialty, n (%)* | ||||||||
| Internal medicine | 101 (16.9) | 1 (0.9) | ref | ref | 2 (1.8) | ref | ref | |
| Family medicine | 483 (80.6) | 50 (10.3) | 11.5 (1.6–84.6) | 2.6 (0.2–34.4) | 205 (42.2) | 36.3 (8.9–149) | 4.0 (0.8–20.1) | |
| Practice obstetrics, n (%) | ||||||||
| No | 428 (71.5) | 18 (4.2) | ref | ref | 83 (19.4) | ref | ref | |
| Yes | 171 (28.5) | 34 (19.9) | 5.7 (3.1–10.4) | 9.7 (2.8–34.2) | 124 (72.5) | 11.1 (7.3–16.8) | 7.4 (4.3–12.7) | |
| Perform endometrial biopsies,n (%) | ||||||||
| No | 343 (57.3) | 15 (4.4) | ref | 36 (10.5) | ref | |||
| Yes | 256 (42.7) | 37 (14.5) | 3.7 (2.0–6.8) | 170 (66.4) | 16.6 (10.8–25.5) | |||
| Training, n (%) | Implant | IUD | ||||||
| During residency | 23 (3.7) | 305 (50.9) | 9 (39.1) | ref | ref | 170 (55.7) | ref | ref |
| After residency | 56 (9.4) | 49 (8.2) | 40 (71.4) | 3.6 (1.3–10.1) | 9.2 (2.0–42.6) | 34 (69.4) | 1.8 (1.0–3.4) | 2.1 (1.0–4.5) |
| None | 520 (86.9) | 245 (40.9) | 3 (0.6) | 3 (1.2) | ||||
Specialty does not total 100% due to inclusion of general practitioners and medicine/pediatrics specialists.
ns, not significant; OR, odds ratio.
Barriers
The most common barrier reported by those who do not place the methods in their practice was lack of training. The majority (87%) of those who responded had not been trained in implant placement, and 41% had not been trained in IUD placement. Lack of demand from patients was the main barrier for many physicians for both the IUD (11.5%) and implant (12.5%), with several physicians writing in comments that there was not enough volume to keep up their skills for placement of the methods. Ten percent of the physicians cited a moral objection to placing IUDs, while only 3% reported this concern for the implant. Six percent of physicians sited cost as the main barrier for both IUDs and implants.
Referral patterns
Physicians who do not place the methods were asked to what type of providers they refer patients for these devices, and the distance from their office to these providers. Patients were most commonly referred to a gynecologist (63% for IUDs, 52% for implants), another primary care physician (20% for IUDs, 15% for implants) or a nurse practitioner or physician's assistant (7% for IUDs and 12% for implants). Fifty percent of physicians refer to a provider in the same office for IUD placement, and 46% for implant placement. Very few patients are referred greater than 25 miles away for IUD (11%) or implant (15%) placement.
Discussion
The minority of primary care physicians who responded to our survey reported placing IUDs and contraceptive implants in their current practice. Female physicians were more likely to place IUDs, and those providing maternity care are more likely to place both methods. This information is useful to help focus training and other resources for the physicians who are most likely to place these contraceptive methods. There is also a need to recruit and train more of these physicians, as there are fewer women practicing in rural compared with urban areas,10 as well as a shortage of maternity care providers in rural areas.2
A 2008 national survey of family medicine physicians reported that 24% of the respondents had placed an IUD in the last year.8 Of the family medicine physicians who responded to our survey, 42% reported placing IUDs in their practice, although we did not specify a time range. This may indicate that more family physicians in rural areas of Wisconsin and Illinois are placing IUDs compared with family physicians nationally, possibly due to wider scope of practice for rural physicians. Or, this finding may be a reflection of the increasing use of IUDs in the U.S. population over this time period.5
In a recent survey of family medicine residencies in the United States, 78% of chief residents reported receiving some training in hormonal IUD placement, and 20% reported training in in contraceptive implant placement.11 To our knowledge, similar information on IUD and implant training during internal medicine residency is not published. In our study, very few internal medicine physicians reported training for placement of IUDs (10%) or implants (3%) during or after residency, and were unlikely to place either device. However, more than half reported writing prescriptions for oral contraceptive pills. This finding shows that providing contraceptive care is within the scope of their practice, and exposure to contraception provision and management during training is important. The Accreditation Council for Graduate Medical Education does require “opportunities for experience in…office gynecology,” for internal medicine residencies.12 Physicians planning on a rural practice may especially benefit from exposure to placement of long acting contraception in training. While the majority of internal medicine physicians may not place IUDs or implants, increased knowledge of and training in these methods may help them be better able to counsel and refer patients.
Physician training is not the only barrier to provision of these methods. Physicians' perceptions of other barriers included low patient demand or high cost. As popularity of these methods grows in the United States,5 more patients are requesting these devices. Additionally, now that the Affordable Care Act mandates that all contraceptive methods must be covered by insurance without cost sharing, the financial barrier to these methods will be removed for many more women.
It is encouraging that post-residency training is associated with provision of IUDs and implants. This relationship between training post-residency and abortion provision was also noted among family physicians,13 highlighting the importance of availability of procedural training for motivated physicians in practice. This might suggest that physicians are more likely to seek out post-residency training if there is sufficient patient demand and a lack of other barriers. Our survey did not determine how and in what settings the physicians were able to obtain training post-residency; more work is needed in this area to determine the best ways to facilitate post-residency training. Hands-on training post residency can be difficult to obtain, as finding time, a preceptor, and adequate malpractice coverage can be challenging. These issues highlight the importance of increasing this training during residency as well, when these logistical barriers are not present.
A strength of our study is our focus on primary care physicians in rural practice. Physicians practicing in rural areas have important differences from their urban colleagues, with fewer specialists at further distances available for referrals. Our findings suggest that family medicine physicians in rural practice may be more likely to place long acting contraception than the general population of family physicians.8 This information can help inform curriculum development for medical schools and residency programs that focus on training physicians for practice in rural areas.
Limitations of this study include that we assessed provision only by physicians, and that we did not assess care provided by other clinicians such as nurse practitioners or physician assistants. It is likely that there are advanced practice clinicians providing contraception, especially at publicly funded (Title X) family planning clinics, with broader availability of these contraceptive methods in rural areas than our data would suggest.
Another limitation is our survey had a response rate of 37%—this is low but similar to many other published physician survey response rates.14 State licensing information was not current for all physicians, and led to a high number of ineligible responses. We only surveyed physicians in Wisconsin and Illinois; these results may not be generalizable to physicians in other rural areas of the United States.
Additionally, all survey research findings may be limited by response bias. Physicians with an interest in contraception were probably more likely to respond to the survey. It is likely that the general population of physicians has a lower percentage of providers of the long acting methods than our survey respondents. Little demographic or practice characteristic information about nonresponders is available from the state licensing information.
Conclusions
While many rural primary care physicians care for reproductive age women and prescribe contraceptives, a minority of these physicians place the most effective forms of contraception, intrauterine devices and contraceptive implants. Primary care physicians who provide maternity care and female physicians are more likely to place these methods. Lack of physician training and low patient demand were the barriers to placement most frequently cited by the physicians. This suggests that additional training opportunities during family medicine and general internal medicine residency and post-residency may increase the availability of these services in rural areas.
Acknowledgments
The authors wish to thank Dr. Marji Gold for her review of an earlier version of the manuscript. This project was funded by a grant from the Society of Family Planning. This project was supported by the University of Wisconsin Institute for Clinical and Translational Research, funded through an NIH Clinical and Translational Science Award, grant number 1 UL1 RR025011.
Disclosure Statement
No competing financial interests exist.
References
- 1.Hart LG, Larson EH, Lishner DM. Rural definitions for health policy and research. Am J Public Health 2005;95:1149–1155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.ACOG Committee Opinion No. 429: Health disparities for rural women. American College of Obstetricians and Gynecologists. Obstet Gynecol 2009;113:762–765 [DOI] [PubMed] [Google Scholar]
- 3.Chandra A, Martinez GM, Mosher WD, Abma JC, Jones J. Fertility, family planning, and reproductive health of U.S. women: Data from the 2002 National Survey of Family Growth. National Center for Health Statistics. Vital Health Stat 2005;23:1–160 [PubMed] [Google Scholar]
- 4.Espey E, Ogburn T. Long-acting reversible contraceptives: intrauterine devices and the contraceptive implant. Obstet Gynecol 2011;117:705–719 [DOI] [PubMed] [Google Scholar]
- 5.Finer LB, Jerman J, Kavanaugh ML. Changes in the use of long-acting contraceptive methods in the United States, 2007–2009. Fertil Steril 2012;98:893–897 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Council on Graduate Medical Education. Eighteenth report: New paradigms for physician training and improving access to health care. Rockville, MD: Council on Graduate Medical Education, 2007 [Google Scholar]
- 7.Rosenblatt R, Mattis R, and Hart LG. Abortions in rural Idaho: physicians' attitudes and practices. Am J Public Health 1995;85:1423–145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rubin SE, Fletcher J, Stein T, Segall-Gutierrez P, Gold M. Determinants of intrauterine contraception provision among US family physicians: a national survey of knowledge, attitudes and practice. Contraception 2011;83:472–478 [DOI] [PubMed] [Google Scholar]
- 9.Vaaler ML, Kalanges LK, Fonseca VP, Castrucci BC. Urban-rural differences in attitudes and practices toward long-acting reversible contraceptives among family planning providers in Texas. Womens Health Issues 2012;22:e157–162 [DOI] [PubMed] [Google Scholar]
- 10.Ellsbury KE, Doescher MP, Hart G. US medical schools and the rural family physician gender gap. Fam Med 2000;32:331–337 [PubMed] [Google Scholar]
- 11.Herbitter C, Greenberg M, Fletcher J, Query C, Dalby J, Gold M. Family planning training in US family medicine residencies. Fam Med 2001;143:574–581 [PubMed] [Google Scholar]
- 12.Accreditation Council for Graduate Medical Education. ACGME Program Requirements for Graduate Medical Education in Internal Medicine. www.acgme.org/acgmeweb/Portals/0/PFAssets/ProgramRequirements/140_internal_medicine_07012009.pdf Accessed November30, 2012
- 13.Greenberg M, Herbitter C, Gawinski BA, Fletcher J, Gold M. Barriers and enablers to becoming abortion providers: The reproductive health program. Fam Med 2011;44:493–500 [PubMed] [Google Scholar]
- 14.Kellerman SE, Herold J. Physician response to surveys; a review of the literature. Am J Prev Med 2001;20:61–67 [DOI] [PubMed] [Google Scholar]