Abstract
Background: The challenge of identifying and recruiting U.S. women at elevated risk for HIV acquisition impedes prevention studies and services. HIV Prevention Trials Network (HPTN) 064 was a U.S. multisite, longitudinal cohort study designed to estimate HIV incidence among women living in communities with prevalent HIV and poverty. Venue-based sampling (VBS) methodologies and participant and venue characteristics are described.
Methods: Eligible women were recruited from 10 U.S. communities with prevalent HIV and poverty using VBS. Participant eligibility criteria included age 18–44 years, residing in a designated census tract/zip code, and self-report of at least one high-risk personal and/or male sexual partner characteristic associated with HIV acquisition (e.g., incarceration history). Ethnography was conducted to finalize recruitment areas and venues.
Results: Eight thousand twenty-nine women were screened and 2,099 women were enrolled (88% black, median age 29 years) over 14 months. The majority of participants were recruited from outdoor venues (58%), retail spaces (18%), and social service organizations (13%). The proportion of women recruited per venue category varied by site. Most participants (73%) had both individual and partner characteristics that qualified them for the study; 14% were eligible based on partner risk only.
Conclusion: VBS is a feasible and effective approach to rapidly recruit a population of women at enhanced risk for HIV in the United States. Such a recruitment approach is needed in order to engage women most at risk and requires strong community engagement.
Introduction
The burden of acquired immune deficiency syndrome (AIDS) in women in the United States has grown substantially over the past 30 years, rising from 8% of all newly diagnosed AIDS cases in 1983 to more than 23% in 2010.1,2 In 2010, one in five new human immunodeficiency virus (HIV) infections in the United States were among women; 84% of those infections were acquired through heterosexual transmission.2 Significant racial disparities exist for newly reported cases among women. In 2010, the rate of new HIV infections (per 100,000 for the general female adult and adolescent population) among black/African American women was nearly 20 times as high as white females and approximately four times as high as the rate for Hispanic/Latino females.3
Identifying women at greatest risk of HIV acquisition in the United States has been a challenge, particularly when targeting such women for HIV clinical trials,4 as well as prevention research requiring HIV endpoints.5–7 Women most at risk for HIV in the United States may be less likely to enroll in research, due in part to restrictive eligibility criteria, researcher bias that certain individuals may be more difficult to retain, cultural and language barriers, childcare responsibilities, a lack of trust on the part of the potential study participants, or structural barriers such as access to transportation.4,8–14
Specific individual-level behaviors, such as substance misuse and sex exchange, have been associated with sexually transmitted infections (STIs) and HIV.15–18 As a result, many studies have focused on individual-level behaviors when defining study eligibility criteria. There is a growing appreciation, however, that larger social and structural factors, including neighborhood environment, shape HIV risk. Place characteristics, such as rates of poverty, violent crime, incarceration, and male to female sex ratios are thought to be powerful drivers of sexual behaviors and HIV/STI risk, particularly among U.S. black adults.19–25
Past studies have used a variety of approaches to recruiting high risk women into prospective HIV cohort studies in the United States, such as peer referrals, self-referrals (e.g., flyers), and clinic-based recruitment.6,9,26–29 Methodologies that recruit participants from community settings may be a particularly promising approach to finding women at elevated risk of HIV and to engage them in the research process. One such approach is venue-based sampling (VBS). VBS is a sampling strategy used to find hard-to-reach populations and has been used to sample persons who attend venues within locally defined geographic areas.30 Based on the application of time-space sampling, VBS has been used previously to obtain large, diverse samples from previously underrepresented populations.30–34 The most notable use of venue-based sampling of women in the United States context was the Centers for Disease Control and Prevention National HIV Behavioral Surveillance Heterosexual Cycle (NHBS-HET) pilot study from 2006–2007, which was designed to identify the behavioral and social factors which place heterosexuals at risk for HIV; half of the sites were randomized to VBS recruitment.33,35
Although a number of studies have used venue-based recruitment, little is known about which venues are most fruitful for identifying and recruiting women at high-risk of HIV in the United States. Studies that have described demographic and behavioral characteristics of adults by enrollment venue were heavily weighted toward locales that may not be as relevant for studies recruiting women only, such as sex establishments, bars and clubs, and men's shelters.36,37 A comparison of recruitment venues for at risk adolescent girls and young men who have sex with men (YMSM) determined that young women were more likely to be recruited from neighborhood-based or commercial venues than YMSM.38 Thus, recruitment efforts of women at elevated risk of HIV in the United States may be enhanced by an understanding of what venue types yield the most participants and the behavioral attributes of these participants.
The HIV Prevention Trials Network (HPTN 064) identified women at increased risk for HIV acquisition using VBS as a recruitment strategy. We describe the recruitment process used in HPTN 064 and explore associations between venue category and participant attributes of women enrolled.
Materials and Methods
Study communities
HPTN 064 was a multisite, longitudinal cohort study designed to estimate the HIV incidence among women living in communities with prevalent HIV and poverty and to determine the feasibility of recruiting women using venue-based sampling based on predefined eligibility criteria for location, individual, and partner characteristics associated with high risk for HIV acquisition. The targeted sample size for each site was 200 women. This target could be exceeded by up to 5%. Although the original recruitment target period was 6 months from approval for the initiation of site recruitment activities, a subsequent Scientific Review Committee recommendation and protocol amendment increased the length of recruitment at some sites.17 Participants were enrolled between May 2009 and August 2010 from one of 10 study communities, across six geographic areas. These communities included The Bronx and Harlem (New York City, New York), North and South Newark (Newark, New Jersey), Washington (District of Columbia), Baltimore (Maryland), Durham and Raleigh (North Carolina), and Atlanta and Atlanta/Decatur (Georgia). A certificate of confidentiality was obtained for the study and research sites obtained local institutional review board (IRB) approval before initiation of study activities. Women were followed for 6 or 12 months, depending on date of enrollment, and were compensated for in-person visits (i.e., enrollment and follow-up) and phone locator update calls. The amount of compensation varied by site and was approved by local IRBs (ranging from 35 to 50 dollars for in-person study visits and 10 to 15 dollars for locator-update phone calls). The study design has been described in detail elsewhere.17,39
Recruitment areas: study census tract/zip code selection
Recruitment areas were defined by census tracts (and for New York only, zip codes) with high prevalences of both HIV and poverty. Census tracts on average contain 4,000 persons and are typically homogeneous with respect to population characteristics, economic status, and living conditions.40 In 2000, zip codes in New York City contained an average of 8,785 persons aged 18 and older. A list of eligible census tracts (zip codes for New York City) for study inclusion was generated between November 2008 and August 2009. Eligible study census tracts/zip codes were areas with high prevalence of HIV and poverty as defined based on the NHBS-HET pilot methodology, which in 2006–2007 combined U.S. Census poverty data with state health department HIV prevalence data using a standardized algorithm,33 within reasonable travel time of clinical research site (e.g., within 2 hours), and had sufficient population density to facilitate rapid recruitment. HIV prevalence was generated from the most recently available data, which in 2008–2009 was from 2007 HIV cases rates (2006 for North and South Newark); percent living below poverty was established using 2000 U.S. Census data on population size and poverty rate (2005 estimates for Georgia). Census tracts in the top 30th percentile of poverty and with more than 25% of inhabitants living below the U.S. federal poverty threshold were assigned a combined “score.” Higher ranked scores denoted tracts with greater levels of HIV and poverty relative to the surrounding tracts.
Study staff conducted an ethnographic review of the top 30th percentile of the ranked census tracts/zip codes generated using the standardized algorithm described above to confirm the ranked tracts were high poverty areas, to determine whether the study areas had experienced notable changes in community characteristics since the 2000 census (e.g., gentrification, consisted of primarily commercial nonresidential areas), and to identify recruitment venues. Each site developed a tailored approach to conducting ethnography based on consultation with local experts and community advisory boards (CABs). Ethnographic data collection activities included, walking and driving through potential tracts (e.g., “windshield tours”), informal communication with community partners, advisory boards, residents, and business owners, and in some cases, brief interviews and focus groups with women and other key informants. Census tracts determined to be largely nonresidential or visibly gentrified were removed from the eligible census tract/zip code list. Through this process, each site generated a final list of census tracts/zip codes that was then used to determine residence eligibility for participants (residential sampling frame). Women residing in a census tract outside of the sampling frame were considered ineligible for the study. A range of 8% to 30% of tracts in each community were ultimately classified as eligible census tracts.
Participant eligibility criteria
Study participants were self-identified women aged 18–44 years who reported unprotected vaginal or anal sex with a man in the past 6 months and who resided within the study census tracts/zip codes as described above, and who reported at least one additional personal risk (e.g., substance use) and/or male partner characteristic (e.g., history of incarceration) associated with greater risk of HIV acquisition, as outlined in Table 1. Women were excluded from participating if they reported a history of previous positive results on an HIV test, current HIV prevention trial enrollment, current or past participation in an HIV vaccine trial, or anticipated absence for more than two consecutive months during follow-up. Eligibility criteria were collected through staff-administered questionnaires. Subsequent behavioral measures (e.g., anal sex, concurrency) were collected at baseline and follow-up using an audio computer-assisted survey instrument (ACASI).17
Table 1.
Study Eligibility Criteria
| All eligible women met the following criteria: |
|---|
| • Self-identify as a woman (transgendered women eligible) |
| • 18 to 44 years of age, inclusive on the date of screening |
| • Willing to receive HIV test results |
| • Reside in designated census tract or, for New York City only, zip code |
| • Unprotected (e.g., without a condom) vaginal and/or anal sex with a man during the prior 6 months |
| AND at least one of the following reported by participant: |
|---|
| Personal history of any of the following in the prior 6 months:a |
| • Illicit injected and/or noninjected drug use (e.g., heroin, cocaine, crack cocaine, methamphetamine, and/or prescription drugs used outside the oversight of a medical professional)b |
| • Alcohol dependencec |
| • Binge drinkingd |
| • Incarceration for more than 24 hours (jail or prison)a |
| • Gonorrhea, chlamydia, trichomonas, or syphilis |
| • Exchange of sex for commodities (e.g., drugs, money, shelter, or other commodities) |
| Male sexual partner with any of the following in the prior 6 months:a |
| • Self-reported use of illicit injected or noninjected drugs (e.g., heroin, cocaine, crack cocaine, methamphetamine, and/or prescription drugs used outside the oversight of a medical professional)b |
| • Incarceration for more than 24 hours (jail or prison)a |
| • Gonorrhea, chlamydia, trichomonas, or syphilis |
| • HIV seropositive diagnosis (ever) |
| • Binge drinkingd |
| • Alcohol dependencec |
| Exclusion criteria |
|---|
| Women were excluded from participating if they reported any of the following: |
| • A history of previous positive results on an HIV test |
| • Current HIV prevention trial enrollment |
| • Current or past participation in an HIV vaccine trial |
| • Anticipated absence for more than two consecutive months during follow-up |
Within the prior 6 months, with the exception of incarceration, which was within the prior 5 years.
Participants whose only illicit drug use is marijuana did not meet the illicit drug use eligibility criteria.
Defined as a CAGE56 score ≥2.
Defined as four or more drinks at one time (e.g., during the morning, afternoon, or evening) for women and five or more drinks for men.
CAGE, cut down, annoyed, guilty, eye-opener.
Venue identification
Participants were recruited using VBS. Eligible venues were located in the highest ranking census tracts/zip codes as defined above or within proximity of the identified census tracts/zip codes and deemed likely to be frequented by women living in the eligible census tracts. Research staff used ethnography (as described above) and community consultation to enumerate a list of all potential venues (e.g., beauty salons, library, grocery, and liquor stores) in or near the study tracts and to assess the age range, gender, and number of individuals typically attending the venue. Venues were determined to be inappropriate for recruitment if (1) they were frequented predominantly by men; (2) a minority of women not meeting the age eligibility criteria were likely to attend the venue (e.g., majority under 18); (3) it would be impossible logistically to screen potential participants for confidentiality or safety reasons; or (4) venue owner(s) refused to allow the project staff access to venue attendees.
For each eligible venue, site ethnographers documented the high traffic days and times (e.g., weekdays from 1–5 pm). Each venue daytime period (VDT) was enumerated and collectively made up the list of potential recruitment venue time slots (e.g., each VDT had a distinct enumeration). A total of 13 venue categories and corresponding definitions were included on the study enrollment form. These categories were based on existing NHBS-HET cycle categories.
Recruitment
Random-number generators were used to select VDTs from the enumerated venue list and to construct monthly sampling frames. Alternative venues for each primary recruitment venue were also randomly selected to ensure that backup venues were available in the event that the primary venue proved unsuccessful (e.g., inclement weather, lack of participants for screening).
A systematic process was used at each venue to recruit potential participants. Prior to initiation of screening activities, study staff identified a catchment area within the venue with high pedestrian traffic; any woman crossing into this region was approached either sequentially or systematically (e.g., every fourth woman) for screening in the order in which they “crossed the line” into the catchment area. This decision was made a priori based on the availability of staff and the amount of foot traffic at the venue. All staff were knowledgeable of the boundaries of this region; however, in an attempt to avoid participant self-selection, this region was “invisible” to potential study participants. Study screening and enrollment activities took place at locations that assured adequate confidentiality, such as a mobile van, nearby community location, or the study clinical site. Other day appointments were scheduled in cases where women were unable to complete screening and enrollment activities at the time of the initial encounter.
Community engagement
Study sites used a combination of techniques to develop community partnerships and gain trust within each community. A study-wide community working group (HPTN 064 CWG) with representatives from each study site and local community advisory boards (CABs) were established early in study development. The HPTN 064 CWG and CABs were consulted on a regular basis and provided feedback to the protocol team and study site staff on community engagement plans, community education and recruitment materials, ethnographic assessments, and venue identification procedures.
A study logo and associated branding was developed through a community-based logo contest and selected through collaboration between the study protocol, study sites, and the HPTN 064 CWG. Study staff developed ongoing partnerships with local community organizations and key community gatekeepers (e.g., community advocates, respected neighborhood members). Site staff maintained an active presence at community events and in day-to-day activities by frequenting community businesses and volunteering at community events.
Staffing considerations
Study recruiters were predominantly women of color. A minimum of two staff members were required for all recruitment activities to ensure the safety of study staff and to ensure that there was an adequate number of staff to approach and recruit potential participants.
Retention
Although the focus of this manuscript is study recruitment, it should be noted that a variety of strategies were used to ensure retention of enrolled participants. Retention strategies included: community engagement; interpersonal relationship building (e.g., phone calls and personalized mailings); reduction of external barriers (e.g., study visits outside of traditional business hours, clinical and community visit sites); staff capacity building (e.g., ongoing training); and external tracing (e.g., prison and jail database searches). These strategies are discussed in detail elsewhere.39
Measures and data analysis
Descriptive statistics were obtained using SAS version 9.2 (SAS Inc.). Continuous variables were summarized using medians and interquartile ranges. Categorical variables were tabulated. Screen to enrollment ratio was defined as the number of women screened divided by the number of women enrolled and was generated using site tracking logs and enrollment reports.
For purpose of analysis, study venues categories were grouped into one of seven categories: (1) retail space, (2) outdoor venue (e.g., park, street), (3) social service organization, (4) public housing, (5) special event (e.g., any one-time event such as a community event or concert), (6) other public space (e.g., public transportation, library, church), and (7) space that serves alcohol (e.g., bar, club). These groupings were informed by descriptions of venue categories in available literature and through consultation with team members with expertise in this area (Table 2).36–38,41
Table 2.
Venue Categories
| Venue category | Category listed on study enrollment forma |
|---|---|
| (1) Retail Space (n=388) | Restaurant/caféb (n=40) Retail (n=348) |
| (2) Outdoor location (n=1,215) | Streetc (n=1,108) |
| Parkc (n=107) | |
| (3) Social service organization (n=268) | Social service organizationc (e.g., WIC) (n=268) |
| (4) Public housingd (n=80) | Generated from “other” category, includes participants where a specific public housing complex was listed as the recruitment venue category |
| (5) Special eventd (n=66) | Generated from “other” category, includes participants recruited from a one-time event such as fair |
| (6) Other public space (n=65) | Public transportd (n=18) |
| Churchd (n=12) | |
| Social groupc,e (n=5) | |
| Libraryd (n=14) | |
| Courtd (n=15) | |
| Gymc (n=1) | |
| (7) Spaces that serve alcohol (n=13) | Barc (n=5) |
| Dance clubc (n=1) | |
| Sex establishmentc (n=2) | |
| House partyc (n=5) |
“Rave or similar event” was included on the study enrollment form; however, no participants were enrolled from this venue type and it is not included in the categories above.
Majority of restaurants/cafés are fast food restaurants.
Pre-specified enrollment form category.
Developed based on “other” category.
Church group.
Exploratory analyses of participant characteristics by venue were conducted using exact logistic regression (SAS version 9.2) in order to assess associations between venue type, participant self-reported eligibility (as described in Table 1), laboratory-confirmed HIV infection (recent and newly diagnosed prevalent), and baseline behaviors associated with increased risk of HIV acquisition (any anal sex in the prior six months (yes/no) and concurrency (sexual partnerships overlapping in time in the prior 6 months). Both direct concurrency (participant report of nonmonogamous partnerships that overlap in time [yes/no]) and indirect concurrency (participant self-report of being in a sexual partnership where her male partner had one or more additional sexual partners, [yes/no]) were explored. Exploratory analyses modeled venue category as the independent variable and participant characteristics as the dependent variable. Self-reported eligibility criteria modeled included personal characteristics only, partner characteristics only, personal and partner characteristics, specific criteria met (e.g., alcohol misuse [dependence and/or binge]; substance use; history of STI; exchange of sex for drugs, money, shelter, or other commodities; and incarceration).
Of note, as described in Table 1, all eligibility captured behaviors/characteristics within the prior six months, with the exception of incarceration history, which included at least 24 hours in jail or prison within the prior five years.
Results
Screening
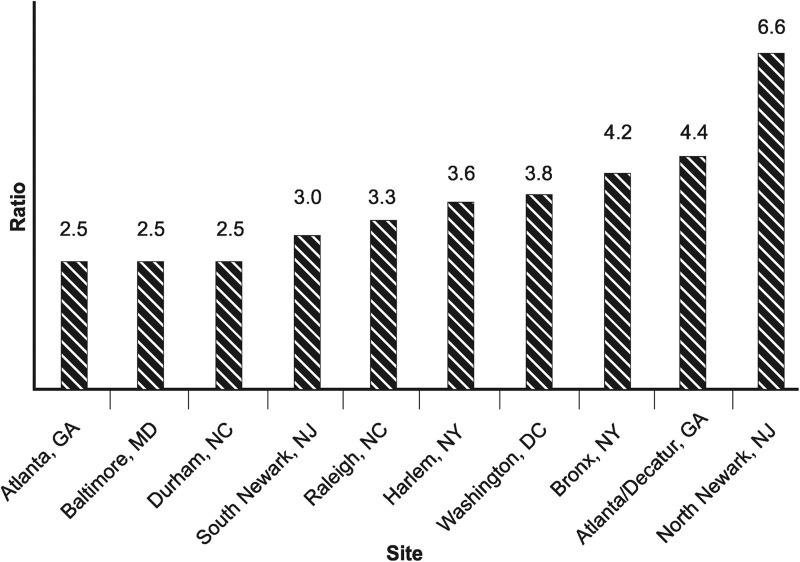
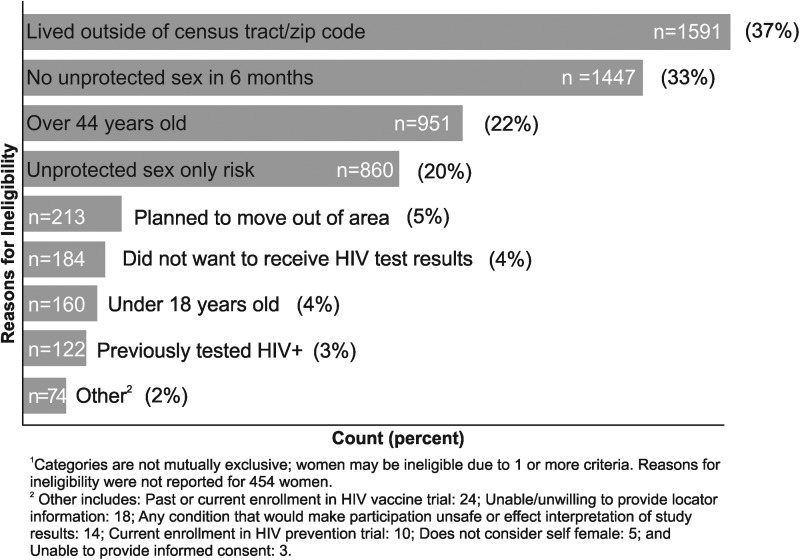
A total of 8,029 women were screened between May 2009 and August 2010. Screen to enrollment ratios by site ranged from ranged from 2.5 to 6.6, with an average of 3.5 women screened per woman enrolled (Fig. 1). Sixty percent of women screened (n=4,796) did not meet study eligibility criteria. Reasons for ineligibility are available for 4,342 women (Fig. 2). Reasons for ineligibility are not mutually exclusive; women could screen out of the study for more than one reason. The four most common reasons for ineligibility were: (1) lived outside of the eligible census tract-sampling frame (n=1591, 37%); (2) no unprotected sex with a man in the prior 6 months (n=1447, 33%); (3) over 44 years of age (n=951, 22%); and (4) unprotected sex only reported risk (n=860, 20%). A total of 3,233 (40%) of women screened were eligible for enrollment. Of those eligible, 1,134 (35%) did not enroll; the majority of these women did not return to the clinical research site for the scheduled enrollment visit (69%).
Fig. 1.
Ratio of Women Screened to Women Enrolled, by Site (n=8029).
Fig. 2.
Reasons for Enrollment Ineligibility1 (n=4342).
Participant characteristics
A total of 2,099 women were ultimately enrolled (approximately 210 per site). Overall study retention was 92%. Overall, 1 in 300 women in this cohort were identified with newly acquired HIV infection.17,42 Select baseline characteristics are presented in Table 3. The majority of participants were black (86%). The median age was 29 years. Thirty-seven percent had less than a high school education and 44% percent reported an annual income of $10,000 or less. Baseline binge drinking and illicit substance use in the last 6 months was high; 62% reported binge drinking and 35% reported illicit substance use (excluding cannabis). Condom use at last sex was low (18%). Thirty-eight percent of women reported anal sex, 37% reported direct concurrency (i.e., non-monogamous partnerships that overlap in time), and 36% reported suspected partner concurrency (i.e., being in a sexual partnership where her male partner had one or more additional sexual partners).
Table 3.
Select Participant Baseline Characteristics (in Previous Six Months)
| Variable | n=2,099 |
|---|---|
| Median age (interquartile range) | 29 (23–38) |
| Black race | 1802 (86%) |
| Less than high school education | 777 (37%) |
| Condom use at last vaginal sex | 376 (18%) |
| Concurrent sexual partners | |
| Direct (Self-report of non-monogamous partnerships that overlap in time) | 776 (37%) |
| Indirect (Sexual partner with ≥1 additional sexual partner[s]) | 763 (36%) |
| Mental health | |
| Symptoms indicative of depressiona | 692 (33%) |
| Symptoms indicative of PTSDb | 600 (29%) |
| Abuse history | |
| Physical, emotional, sexual or feeling unsafe | 811 (39%) |
| Childhood abuse (ever) | 934 (44%) |
| Illicit non-alcohol drug usec | 726 (35%) |
| Binge drinkingd | 1300 (62%) |
| Homelesse | 182 (9%) |
| Number of children financially responsible for | |
| 0 or NA | 990 (47%) |
| 1 | 465 (22%) |
| ≥2 | 644 (31%) |
| Reported food insecurity | 971 (46%) |
Symptoms of depression was defined as a score of 7 or greater on a shortened CES-D scale used by DiClemente et al.57
Symptoms of post-traumatic stress disorder (PTSD) was defined as a score of 3 or greater on the primary care PTSD screener.58
Excludes cannabis.
Defined as four or more drinks at one time (e.g., during the morning, afternoon, or evening).
Baseline housing is not available for 30 participants.
CES-D, Center for Epidemiologic Studies Depression Scale.
Most participants met both personal and partner eligibility criteria (73%). However, 14% of participants were eligible based on partner characteristics only, and 13% of participants were eligible based on personal characteristics alone (Table 4). Sixty percent of participants met alcohol misuse (dependence and/or binge) criteria, 12% met the substance use criterion, 14% met criteria for self-reported history of STI, 27% met the criterion for sex exchange, and 40% met the incarceration eligibility criterion.
Table 4.
Participant Self-Reported Eligibility Characteristics (n=2,099)
| Venue category | ||||||||
|---|---|---|---|---|---|---|---|---|
| Self-reported characteristics | Retail space (n=388) | Outdoor venue (n=1215) | Social service organization (n=268) | Public housing (n=80) | Special event (n=66) | Other public space (n=66) | Space that serves alcohol (n=13) | TotalOverall (n=2,099) |
| Personal and partner eligibility criteria meta | ||||||||
| Personal characteristic only | 39 (10%) | 175 (14%) | 28 (10%) | 9 (11%) | 9 (14%) | 6 (9%) | 1 (7%) | 267 (13%) |
| Sexual partner characteristic only | 60 (21%) | 168 (14%) | 33 (12%) | 13 (16%) | 17 (26%) | 11 (17%) | 2 (15%) | 304 (14%) |
| Both personal and partner | 289 (74%) | 872 (72%) | 207 (77%) | 58 (73%) | 40 (61%) | 52 (79%) | 10 (77%) | 1528 (73%) |
| Behavioral eligibility criteria meta | ||||||||
| Alcohol misuse (binge and/or dependence) | 233 (60%) | 726 (60%) | 167 (62%) | 48 (60%) | 26 (39%) | 45 (68%) | 10 (77%) | 1255 (60%) |
| Non-alcoholic substance use | 30 (8%) | 183 (15%) | 28 (10%) | 5 (6%) | 5 (8%) | 2 (3%) | 1 (7%) | 254 (12%) |
| STI | 78 (20%) | 144 (12%) | 37 (14%) | 16 (2%) | 12 (18%) | 14 (21%) | 3 (23%) | 304 (14%) |
| Sex exchange | 108 (38%) | 324 (27%) | 84 (31%) | 11 (14%) | 10 (15%) | 22 (33%) | 4 (31%) | 566 (27%) |
| Past incarceration | 151 (39%) | 495 (41%) | 120 (45%) | 27 (34%) | 20 (30%) | 29 (44%) | 6 (46%) | 848 (40%) |
| Select baseline behaviorsb | ||||||||
| Anal sex | 135 (35%) | 483 (40%) | 111 (41%) | 15 (19%) | 24 (36%) | 25 (38%) | 3 (23%) | 796 (38%)d |
| Direct concurrency | 126 (32%) | 449 (37%) | 102 (38%) | 32 (40%) | 28 (42%) | 33 (50%) | 6 (46%) | 776 (37%)e |
| Indirect concurrency | 145 (37%) | 422 (35%) | 99 (37%) | 33 (41%) | 30 (45%) | 28 (42%) | 6 (46%) | 763 (36%) |
| HIV infectionc | 8 (2%) | 25 (2%) | 3 (1%) | 1 (1%) | 1 (2%) | 0 (0%) | 0 (0%) | 38 (2%) |
Participant characteristics by venue
In the exploratory analyses conducted to determine if participant characteristics were associated with venue category (Table 4), there were no statistically significant relationships between venue type, participant self-reported eligibility, laboratory-confirmed HIV infection (recent and newly diagnosed prevalent), and baseline behaviors associated with higher risk of HIV acquisition (anal sex, participant concurrency, and partner concurrency). Odd ratios, confidence intervals, and associated p-values are not presented.
Venue characteristics
Approximately half of participants were recruited from outdoor venues (n=1,215, 58%), followed by commercial spaces (n=388, 18%), and social service organizations (n=268, 13%) (Table 4). The proportion of women recruited per venue category varied by site (Table 5). For example, 16% of participants were recruited from outdoor venues at the Durham site, whereas approximately 90% of women were recruited from outdoor venues in South Newark, New Jersey and Harlem, New York. The percentage of women recruited from commercial venues ranged from about 1% in South Newark and Bronx, New York to around 43% in Washington, DC, and Raleigh, North Carolina. All participants recruited from special events were located in North Carolina.
Table 5.
Number of Enrolled Participants by Recruitment Venue (by Site and Overall) (n=2,099)
| Venue category | ||||||||
|---|---|---|---|---|---|---|---|---|
| Site | Retail space | Outdoor venue | Social service organization | Public housing | Special event | Other public space | Space that serves alcohol | Totala |
| Bronx, NY | 4 (2%) | 153 (73%) | 28 (13%) | 6 (3%) | 0 (0%) | 19 (9%) | 0 (0%) | 210 |
| Harlem, NY | 11 (5%) | 188 (90%) | 10 (5%) | 0 (0%) | 0 (0%) | 1 (<1%) | 0 (0%) | 210 |
| North Newark, NJ | 8 (4%) | 145 (69%) | 56 (27%) | 0 (0%) | 0 (0%) | 0 (0%) | 1 (%) | 210 |
| South Newark, NJ | 3 (1%) | 186 (89%) | 21 (10%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 210 |
| Baltimore, MD | 41 (20%) | 141 (68%) | 22 (11%) | 0 (0%) | 0 (0%) | 0 (0%) | 4 (2%) | 208 |
| Washington, DC | 91 (43%) | 106 (50%) | 13 (6%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 210 |
| Durham, NC | 66 (32%) | 34 (16%) | 9 (4%) | 42 (20%) | 40 (19%) | 18 (9%) | 0 (0%) | 209 |
| Raleigh, NC | 93 (44%) | 58 (28%) | 2 (1%) | 32 (15%) | 24 (11%) | 1 (<1%) | 0 (0%) | 210 |
| Atlanta, GA | 26 (12%) | 90 (43%) | 71 (34%) | 0 (0%) | 0 (0%) | 21 (10%) | 3 (1%) | 211 |
| Atlanta/Decatur, GA | 45 (21%) | 114 (54%) | 36 (17%) | 0 (0%) | 2 (1%) | 9 (4%) | 5 (2%) | 211 |
| Total | 388 (18%) | 1,215 (58%) | 268 (13%) | 80 (4%) | 66 (3%) | 69 (3%) | 13 (<1%) | 2,099 |
Protocol target enrollment for each site was 200 participants and could be exceeded up to 5%.
Discussion
This study demonstrated that it is feasible to engage and recruit women using venue-based sampling based on predefined eligibility criteria for location, individual, and partner characteristics associated with high-risk for HIV acquisition. VBS proved a rapid, effective way to recruit a large cohort of predominantly black women from community-based settings, with some sites enrolling over 200 women in less than 3 months. One in 300 women in HPTN 064 acquired HIV, which is substantially higher than estimates of HIV incidence among black women of similar age and comparable to some sub-Saharan African countries.17
Fourteen percent of women reported partner risk characteristics only and would not be included in studies targeting personal risk behavior alone. Women at elevated risk of HIV acquisition in the United States may not perceive themselves at risk, particularly if this risk is due to male sexual partner or network characteristics.43 It is likely that these women would not have been identified through recruitment methods, such as flyers, which require women to self-select for screening. Moreover, 38% of women reported anal sex in the prior 6 months at baseline, which is higher than existing cross-sectional estimates among the general population of women in the United States, with 20% reporting anal sex in last 12 months.44 Anal sex is an HIV risk factor for heterosexual women; however, stigma related to disclosure of anal sex behaviors may be a barrier to recruitment.45 These results suggest that it may be possible to recruit women who engage in anal sex using VBS, without requiring disclosure of anal sex practices at screening.
Community engagement is a critical element of study implementation, and of recruitment and retention in particular.46–50 Community partnerships were necessary, not only to identify study communities and venues, but also to establish and maintain the trust of venue owners, management, and potential participants, and also to reduce other structural barriers, such as access to transportation to clinical research sites. It is likely that the substantial ongoing community collaborations, as evidenced by establishment of local community advisory boards and working groups, frequenting of local businesses, and volunteering at community events, was responsible for rapid recruitment and successful identification of a cohort of women at heightened risk for HIV. Study branding, such as a study-wide logo developed in collaboration with community partners and study t-shirts, facilitated recognition of study staff by community members. Branding has been shown in the past to be an effective way to recruit and retain female study participants.4,51
Notably, only 13 women were recruited from a “space that serves alcohol,” but 60% of women met alcohol misuse eligibility criteria. Women may not visit bars and clubs as frequently as some other groups targeted by VBS, such MSM. Instead, women may be more likely to drink at home or with friends. Off-site alcohol consumption has been associated with higher sexual risk.52,53 Interestingly, reports of personal risk behaviors provided to satisfy eligibility criteria during recruitment were not always consistent with the risk behaviors reported during the subsequent ACASI interview. Although only 12 percent of women reported non-alcohol substance use in the prior 6 months at screening, 35% of women reported some level of substance use in the prior 6 months at the baseline ACASI, suggesting that substance use was underreported at screening. It is possible that some potential participants may be reluctant to report substance use to recruiters, particularly if recruitment takes place at a locale where revealing substance use could result in the loss of benefits (e.g., social service organizations, public housing).
As described earlier, there are limited data available on the basis for grouping venue categories and the association of venue category to participant attributes. To our knowledge, this is one of the first studies to characterize participant HIV risk characteristics by venue for U.S. women exclusively. For this analysis, study venue categories were created using existing literature to the extent that it applied to a female-only study population but also include unique categories not previously described in the literature. Retail venues, outdoor venues, public spaces, special events, and spaces that serve alcohol have been previously described in VBS literature targeting U.S. adult populations.36,37 Social service organizations and public housing have not to our knowledge been identified as distinct VBS categories in other HIV cohort or prevention studies enrolling women. These categories were developed using the rationale that each represents a specific venue type and may be frequented by women with different demographics or life circumstances (e.g., social service organizations may represent women who are able to identify and access services).
The proportion of women recruited from each venue category varied across study site, which reflects both the geographic diversity of the sites and of the participant population. VBS allows for the development of a sampling frame based on local ethnography, and as such, this is to be expected. Roughly half of the cohort was recruited from outdoor venues. The success of this approach was in part due to the heavy foot traffic in many of the urban sites and the popularity of parks as “hang-out” areas in warmer months across several sites. Of note, a smaller proportion of women were recruited from outdoor venues in the periurban sites: 16% of women were recruited from outdoor venues in Durham, NC, as compared with 90% in Harlem, NY. Applications of VBS to different settings should consider population density, venue types, weather, and expected foot traffic and tailor strategies and timelines accordingly.
In addition, women were recruited from a number of venues not previously anticipated during the development of study forms (e.g., library, church, public housing). This highlights the need for thorough ethnography prior to initiation of recruitment activities, so as to ensure that the initial sample frame reflects the attributes of the study communities. People and places change over time; the recruitment universe was reviewed on a regular basis by study staff members to determine whether venues should be added or removed based on site staff experience or additional information obtained from the community. For example, hair and nail salons were initially included in the venue universe but were later removed by the majority of sites due to challenges with participant confidentiality and the low number of women attending the venue during a given recruitment block. In addition, seasonal, temporal, and safety considerations (e.g., gang activity) also influenced hours present at the and monthly venue productivity.
Exploratory analyses of the associations between venue category and participant characteristics, such as reasons for eligibility, HIV infection, and sexual risk were not statistically significant in exact logistic models. As described, eligible venues were frequented by women living in discrete census tracts. It is possible that the lack of statistical association is reflective of generalized risk among women living in “hot spot” geographic areas with high combined prevalence of HIV and poverty,54 and as such, sociodemographic characteristics of venue locations, rather than the type of venue may be most critical. However, it is possible that the nonsignificant result is due to small cell sizes and resulting low power. Additional research could further define venue characteristics and help to clarify their association with recruitment of specific populations.
Moving forward, studies using geospatial administrative data sources, such as the U.S. Census, to determine eligibility should be mindful of the timing of collection of these data relative to study activities. Sites initiated ethnographic assessments in 2008, eight years after the collection of the 2000 U.S. Census data. Some sites, such as those in Atlanta, GA, experienced significant gentrification during this time.55 Early ethnographic assessment in Atlanta revealed that the ranked census tracts generated using 2000 census data did not reflect current socioeconomic characteristics of the tracts, which necessitated the purchase of updated census data for the year 2005 and additional ethnographic assessment, including significant input from community partners. The intricate steps associated with ethnography combined with strong community partnerships can help ensure that the study team is knowledgeable of phenomena such as gentrification or out-migration of communities that would justify the use of updated Census data.
The findings in this manuscript are subject to limitations. Venue-based sampling methods are used to produce estimates for hard-to-reach populations when sampling frames of the individual members of those populations do not exist or are difficult to construct. However, the data in this manuscript are not weighted to account for variations in venue attendance or likelihood of being selected to participate in the survey and do not account for women who do not attend those venues. In addition, the study did not systematically collect data on screening refusals, and as a result, response rates cannot be calculated. Study eligibility criteria were assessed using self-report; socially undesirable behaviors (e.g., drug use) might have been underreported at the time of eligibility determination. Furthermore, partner's risk behaviors may be underreported, since many women may not be aware of their partner's risk. Finally, since high-risk personal or male sex partner behaviors were included as eligibility criteria, the proportions of high-risk behavior are not representative of all women living in these communities. Findings from this study might not be generalizable to other U.S. states or cities.
Conclusion
In summary, we demonstrated the feasibility and effectiveness of rapid recruitment of a population of women at elevated risk for HIV infection from a range of community-based settings using a venue-based sampling methodology and a combination of geographic, personal, and partner eligibility criteria. Such recruitment approaches require strong community engagement and substantial commitment by study funders and research sites, but are needed to engage women most at risk for targeted HIV prevention research and programs.
Acknowledgments
The authors thank the study participants, community stakeholders, and staff from each study site. In particular, they acknowledge Alexis Amsterdam, Nirupama Sista, Kathy Hinson, Lisa Diane White, Waheedah Shabaaz-El, Carlos del Rio, Quarraisha Abdool-Karim, Sten Vermund, Karen Quick, LeTanya Johnson-Lewis, Edward E. Telzak, Rita Sondengam, Cheryl Guity, Avelino Loquere, Jr., Carolyna Torres, Marta Paez-Quinde, Christopher Chauncey Watson, Manya Magnus, Illene Wiggins, Tracey Chambers Thomas, Makisha Ruffin, Genda Dockery, Oluwakemi Amola, Christin Root, and Valarie Hunter.
Funding for this study provided through grants from the National Institute of Allergy and Infectious Diseases, National Institute on Drug Abuse, and National Institute of Mental Health (UM1 AI068619, U01-AI068613, and UM1-AI068613); Centers for Innovative Research to Control AIDS, Mailman School of Public Health, Columbia University (5U1Al069466); University of North Carolina Clinical Trials Unit (AI069423); University of North Carolina Clinical Trials Research Center of the Clinical and Translational Science Award (RR 025747); University of North Carolina Center for AIDS Research (AI050410); Emory University HIV/AIDS Clinical Trials Unit (5UO1AI069418), Center for AIDS Research (P30 AI050409), and Clinical and Translational Science Award (UL1 RR025008); The Terry Beirn Community Programs for Clinical Research on AIDS Clinical Trials Unit(5 UM1 AI069503-07); The Johns Hopkins Adult AIDS Clinical Trial Unit (AI069465); The Johns Hopkins Clinical and Translational Science Award (UL1 RR 25005); and the HPTN Scholars Program funded by the National Institute of Allergy and Infectious Disease and the National Institute of Mental Health. The primary author's time has been supported in part by the Emory University Laney Graduate School Robert W. Woodruff Pre-Doctoral Fellowship.
The views expressed herein are those of the authors and do not necessarily represent the views of the National Institute of Allergy and Infectious Diseases, the National Institute of Mental Health, the National Institutes of Health, the Centers for Disease Control and Prevention, the HPTN, or its funders.
Disclosure Statement
Sally Hadder, MD has disclosed that she has received consulting fees from Bristol-Myers Squibb, Gilead Science, GlaxoSmithKline/Viiv, and Janssen; and that her spouse has ownership interest in Merck and Becton Dickinson. For all other authors there are no competing financial interests.
References
- 1.McDavid K, Li J, Lee LM. Racial and ethnic disparities in HIV diagnoses for women in the United States. J Acquir Immune Defic Syndr 2006;42:101–107 [DOI] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. HIV Surveillance Report 2011;23 www.cdc.gov/hiv/topics/surveillance/resources/reports/ Published February2013
- 3.Centers for Disease Control and Prevention. Estimated HIV incidence in the United States, 2007–2010. HIV Surveillance Supplemental Report 2012;17 www.cdc.gov/hiv/topics/surveillance/resources/reports/#supplemental Published December2012
- 4.Falcon R, Bridge DA, Currier J, et al. Recruitment and retention of diverse populations in antiretroviral clinical trials: practical applications from the gender, race and clinical experience study. J Womens Health (Larchmt) 2011;20:1043–1050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Buchbinder SP, Mehrotra DV, Duerr A, et al. Efficacy assessment of a cell-mediated immunity HIV-1 vaccine (the Step Study): a double-blind, randomised, placebo-controlled, test-of-concept trial. Lancet 2008;372:1881–1893 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Seage GR, Holte SE, Metzger D, et al. Are US populations appropriate for trials of human immunodeficiency virus vaccine? The HIVNET Vaccine Preparedness Study. Am J Epidemiol 2001;153:619–627 [DOI] [PubMed] [Google Scholar]
- 7.Flynn NM, Forthal DN, Harro CD, et al. Placebo-controlled phase 3 trial of a recombinant glycoprotein 120 vaccine to prevent HIV-1 infection. J Infect Dis 2005;191:654–665 [DOI] [PubMed] [Google Scholar]
- 8.Hines-Martin V, Speck BJ, Stetson B, Looney SW. Understanding systems and rhythms for minority recruitment in intervention research. Res Nurs Health 2009;32:657–670 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hessol NA, Schneider M, Greenblatt RM, et al. Retention of women enrolled in a prospective study of human immunodeficiency virus infection: impact of race, unstable housing, and use of human immunodeficiency virus therapy. Am J Epidemiol 2001;154:563–573 [DOI] [PubMed] [Google Scholar]
- 10.BeLue R, Taylor-Richardson KD, Lin J, Rivera AT, Grandison D. African Americans and participation in clinical trials: differences in beliefs and attitudes by gender. Contemp Clin Trials 2006;27:498–505 [DOI] [PubMed] [Google Scholar]
- 11.Smith YR, Johnson AM, Newman LA, Greene A, Johnson TR, Rogers JL. Perceptions of clinical research participation among African American women. J Womens Health (Larchmt) 2007;16:423–428 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Humphreys K, Weingardt KR, Harris AH. Influence of subject eligibility criteria on compliance with National Institutes of Health guidelines for inclusion of women, minorities, and children in treatment research. Alcohol Clin Exp Res 2007;31:988–995 [DOI] [PubMed] [Google Scholar]
- 13.Chandra A, Paul DP. African American participation in clinical trials: Recruitment difficulties and potential remedies. Hosp Top 2003;81:33–38 [DOI] [PubMed] [Google Scholar]
- 14.Shaya FT, Gbarayor CM, Huiwen Keri Yang , Agyeman-Duah M, Saunders E. A perspective on African American participation in clinical trials. Contemp Clin Trials 2007;28:213–217 [DOI] [PubMed] [Google Scholar]
- 15.Stein M, Herman DS, Trisvan E, Pirraglia P, Engler P, Anderson BJ. Alcohol use and sexual risk behavior among human immunodeficiency virus-positive persons. Alcohol Clin Exp Res 2005;29:837–843 [DOI] [PubMed] [Google Scholar]
- 16.Seth P, Wingood GM, DiClemente RJ, Robinson LS. Alcohol use as a marker for risky sexual behaviors and biologically confirmed sexually transmitted infections among young adult African-American women. Womens Health Issues 2011;21:130–135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hodder SL, Justman J, Hughes JP, et al. HIV Acquisition among women from selected areas of the United States: A cohort study. Ann Intern Med 2013;158:10–18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sterk CE, Theall KP, Elifson KW. Effectiveness of a risk reduction intervention among African American women who use crack cocaine. AIDS Educ Prev 2003;15:15–32 [DOI] [PubMed] [Google Scholar]
- 19.Adimora AA, Schoenbach VJ, Taylor EM, Khan MR, Schwartz RJ, Miller WC. Sex ratio, poverty, and concurrent partnerships among men and women in the United States: A multilevel analysis. Ann Epidemiol 2013;23:716–719 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rudolph AE, Linton S, Dyer TP, Latkin C. Individual, network, and neighborhood correlates of exchange sex among female non-injection drug users in Baltimore, MD (2005–2007). AIDS Behav 2013;17:598–611 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Green TC, Pouget ER, Harrington M, et al. Limiting options: sex ratios, incarceration rates, and sexual risk behavior among people on probation and parole. Sex Transm Dis 2012;39:424–430 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pouget ER, Kershaw TS, Niccolai LM, Ickovics JR, Blankenship KM. Associations of sex ratios and male incarceration rates with multiple opposite-sex partners: potential social determinants of HIV/STI transmission. Public Health Rep 2010;125Suppl 4:70–80 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ford JL, Browning CR. Neighborhoods and Infectious Disease Risk: Acquisition of Chlamydia during the Transition to Young Adulthood. J Urban Health 2013;91:136–150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jennings JM, Woods SE, Curriero FC. The spatial and temporal association of neighborhood drug markets and rates of sexually transmitted infections in an urban setting. Health Place 2013;23:128–137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jennings JM, Taylor R, Iannacchione VG, et al. The available pool of sex partners and risk for a current bacterial sexually transmitted infection. Ann Epidemiol 2010;20:532–538 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Koblin BA, Metch B, Novak RM, et al. Feasibility of identifying a cohort of US women at high risk for HIV infection for HIV vaccine efficacy trials: Longitudinal results of HVTN 906. J Acquir Immune Defic Syndr 2013;63:239–244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Brown-Peterside P, Chiasson MA, Ren L, Koblin BA. Involving women in HIV vaccine efficacy trials: lessons learned from a vaccine preparedness study in New York City. J Urban Health 2000;77:425–437 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hessol NA, Weber KM, Holman S, et al. Retention and attendance of women enrolled in a large prospective study of HIV-1 in the United States. J Womens Health (Larchmt) 2009;18:1627–1637 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bacon MC, von Wyl V, Alden C, et al. The Women's Interagency HIV Study: An observational cohort brings clinical sciences to the bench. Clin Diagn Lab Immunol 2005;12:1013–1019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Muhib FB, Lin LS, Stueve A, et al. A venue-based method for sampling hard-to-reach populations. Public Health Rep 2001;116:216–222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lansky A, Sullivan PS, Gallagher KM, Fleming PL. HIV behavioral surveillance in the U.S.: a conceptual framework. Public Health Rep 2007;122:16–23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.MacKellar DA, Gallagher KM, Finlayson T, Sanchez T, Lansky A, Sullivan PS. Surveillance of HIV risk and prevention behaviors of men who have sex with men–a national application of venue-based, time-space sampling. Public Health Rep 2007;122:39–47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Dinenno EA, Oster AM, Sionean C, Denning P, Lansky A. Piloting a system for behavioral surveillance among heterosexuals at increased risk of HIV in the United States. Open AIDS J 2012;6:169–176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Polk S, Ellen JM, Fichtenberg C, Huettner S, Jennings JM. HIV Prevalence overall and among high-HIV-risk behaviorally defined subgroups among heterosexuals at community-based venues in a mid-Atlantic, US City. J Urban Health 2012;90:747–757 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gallagher KM, Sullivan PS, Lansky A, Onorato IM. Behavioral surveillance among people at risk for HIV infection in the U.S.: the National HIV Behavioral Surveillance System. Public Health Rep 2007;1221:32–38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wohl DA, Khan MR, Tisdale C, et al. Locating the places people meet new sexual partners in a southern US city to inform HIV/STI prevention and testing efforts. AIDS Behav 2011;15:283–291 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Voetsch AC, Lansky A, Drake AJ, et al. Comparison of demographic and behavioral characteristics of men who have sex with men by enrollment venue type in the National HIV Behavioral Surveillance System. Sex Transm Dis 2012;39:229–235 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chutuape KS, Ziff M, Auerswald C, et al. Examining differences in types and location of recruitment venues for young males and females from urban neighborhoods: findings from a multi-site HIV prevention study. J Urban Health 2009;86:31–42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Haley DF, Lucas J, Golin CE, et al. Retention strategies and factors associated with missed visits among low income women at increased risk of HIV acquisition in the US (HPTN 064). AIDS Patient Care STDS. 2014;28(4):206–217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Krieger N, Waterman PD, Chen JT, Soobader MJ, Subramanian SV. Monitoring socioeconomic inequalities in sexually transmitted infections, tuberculosis, and violence: Geocoding and choice of area-based socioeconomic measures—the public health disparities geocoding project (US). Public Health Rep 2003;118:240–260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Weir S, Tate J, Hileman S, et al. Priorities for Local AIDS Control Efforts: A Manual for Implementing the PLACE Method. Chapel Hill, NC: MEASURE Evaluation, 2005 [Google Scholar]
- 42.Eshleman SH, Hughes JP, Laeyendecker O, et al. Use of a multifaceted approach to analyze HIV incidence in a cohort study of women in the United States: HIV Prevention Trials Network 064 Study. J Infect Dis 2013;207:223–231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hodder SL, Justman J, Haley DF, et al. Challenges of a hidden epidemic: HIV prevention among women in the United States. J Acquir Immune Defic Syndr 2010;55:S69–73 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Herbenick D, Reece M, Schick V, Sanders SA, Dodge B, Fortenberry JD. Sexual behavior in the United States: results from a national probability sample of men and women ages 14–94. J Sex Med 2010;7:255–265 [DOI] [PubMed] [Google Scholar]
- 45.Adimora AA, Ramirez C, Auerbach JD, et al. Preventing HIV infection in women. J Acquir Immune Defic Syndr 2013;63:S168–173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Corbie-Smith G, Moody-Ayers S, Thrasher AD. Closing the circle between minority inclusion in research and health disparities. Arch Intern Med 2004;164:1362–1364 [DOI] [PubMed] [Google Scholar]
- 47.Gilliss CL, Lee KA, Gutierrez Y, et al. Recruitment and retention of healthy minority women into community-based longitudinal research. J Womens Health Gend Based Med 2001;10:77–85 [DOI] [PubMed] [Google Scholar]
- 48.Morin SF, Maiorana A, Koester KA, Sheon NM, Richards TA. Community consultation in HIV prevention research: a study of community advisory boards at 6 research sites. J Acquir Immune Defic Syndr 2003;33:513–520 [DOI] [PubMed] [Google Scholar]
- 49.Leonard NR, Lester P, Rotheram-Borus MJ, Mattes K, Gwadz M, Ferns B. Successful recruitment and retention of participants in longitudinal behavioral research. AIDS Educ Prev 2003;15:269–281 [DOI] [PubMed] [Google Scholar]
- 50.Frew PM, Hou SI, Davis M, et al. The likelihood of participation in clinical trials can be measured: The Clinical Research Involvement Scales. J Clin Epidemiol 2010;63:1110–1117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Frew PM, Macias W, Chan K, Harding AC. In “Step” with HIV vaccines? A content analysis of local recruitment campaigns for an international HIV vaccine study. J Health Mass Commun 2009;1:11–39 [PMC free article] [PubMed] [Google Scholar]
- 52.Theall KP, Scribner R, Ghosh-Dastidar B, Cohen D, Mason K, Simonsen N. Neighbourhood alcohol availability and gonorrhea rates: impact of social capital. Geospat Health 2009;3:241–255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Theall KP, Lancaster BP, Lynch S, et al. The neighborhood alcohol environment and at-risk drinking among African-Americans. Alcohol Clin Exp Res 2011;35:996–1003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.El-Sadr WM, Mayer KH, Hodder SL. AIDS in America–forgotten but not gone. N Engl J Med 2010;362:967–970 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Cooper HL, Bonney LE, Ross Z, et al. The aftermath of public housing relocation: Relationship to substance misuse. Drug Alcohol Depend 2013;33:37–44 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Ewing JA. Detecting alcoholism. The CAGE questionnaire. JAMA 1984;252:1905–1907 [DOI] [PubMed] [Google Scholar]
- 57.DiClemente RJ, Wingood GM, Crosby RA, et al. A prospective study of psychological distress and sexual risk behavior among black adolescent females. Pediatrics 2001;108:E85. [DOI] [PubMed] [Google Scholar]
- 58.Prins A, Ouimette P, Kimerling RP, et al. The primary care PTSD screen (PC-PTSD): Development and operating characteristics. Primary Care Psychiatry 2003;9:9–14 [Google Scholar]