Abstract
Objective
To determine patient satisfaction with care provided at a family medicine teaching clinic.
Design
Mailed survey.
Setting
Victoria Family Medical Centre in London, Ont.
Participants
Stratified random sample of 600 regular patients of the clinic aged 18 years or older; 301 responses were received.
Main outcome measures
Patient satisfaction with overall care, wait times for appointments, contact with physicians, and associated demographic factors. Logistic regression analysis and
 analysis were used to determine the significance of factors associated with satisfaction.
analysis were used to determine the significance of factors associated with satisfaction.
Results
The response rate was 50%. Overall, 88% of respondents were fairly, very, or completely satisfied with care. Older patients tended to be more satisfied. Patients who were less satisfied had longer wait times for appointments (P < .001) and reduced continuity with specific doctors (P = .004). More satisfied patients also felt connected through other members of the health care team.
Conclusion
Patients were generally satisfied with the care provided at the family medicine teaching clinic. Older patients tended to be more satisfied than younger patients. Points of dissatisfaction were related to wait times for appointments and continuity with patients’ usual doctors. These findings support the adoption of practices that reduce wait times and facilitate continuity with patients’ usual doctors and other regular members of the health care team.
Résumé
Objectif
Évaluer le niveau de satisfaction des patients à l’égard des soins reçus à une clinique de médecine familiale.
Type d’étude
Enquête postale.
Contexte
Le Victoria Family Medical Centre à London, Ontario.
Participants
Un échantillon aléatoire stratifié de 600 patients réguliers âgés de 18 ans ou plus ; 301 réponses ont été obtenues.
Principaux paramètres à l’étude
Le niveau de satisfaction des patients concernant l’ensemble des soins, le délai d’obtention d’un rendez-vous et le contact avec les médecins, ainsi que les caractéristiques démographiques associées. On s’est servi d’une analyse de régression logistique et du test des
 pour établir la signification des facteurs associés au niveau de satisfaction.
pour établir la signification des facteurs associés au niveau de satisfaction.
Résultats
Le taux de réponse était de 50 %. Dans l’ensemble, 88 % des répondants étaient plutôt, très ou entièrement satisfaits des soins reçus. Les plus âgés avaient tendance à être plus satisfaits que les jeunes. Les moins satisfaits avaient eu de longues attentes pour des rendez-vous (P < ,001) ou une moins bonne continuité avec certains médecins (P = ,004). Les patients les plus satisfaits croyaient aussi avoir un bon contact avec les autres membres de l’équipe de soins.
Conclusion
En général, les patients étaient satisfaits des soins reçus à cette clinique universitaire de médecine familiale. Les plus âgés avaient tendance à être plus satisfaits que les plus jeunes. Les causes d’insatisfaction avaient rapport aux longs délais pour obtenir un rendez-vous et à la continuité des soins avec le médecin habituel. Selon ces résultats, on devrait adopter des mesures pour réduire le temps d’attente et pour favoriser la continuité avec le médecin habituel du patient et avec les autres membres réguliers de l’équipe de soins.
The Victoria Family Medical Centre (VFMC) in London, Ont, is one of the academic family medical centres affiliated with the Department of Family Medicine at the University of Western Ontario. There are 4 family practices at VFMC, which are multidisciplinary in nature and offer social work, access to a public health nurse, and family practice nurses, as well as laboratory services and a shared mental health care program. Although each patient is under the care of one of the full-time staff family doctors (SFDs) of the VFMC, patients are often seen by family medicine residents, who share the responsibility for care with the SFDs.
Continuity of care is well established as an important determinant of quality of care in family practice.1–3 Haggerty et al point out that the relational continuity in ongoing therapeutic relationships between patients and 1 or more providers is particularly important in primary care.4 Hjortdahl and Laerum showed that a personal patient-doctor relationship increased the odds of patient satisfaction 7-fold.5 Furthermore, the greater the continuity of care, or the longer the patient-doctor relationship, the greater the likelihood of better health indicators.6 Maintaining relational continuity of care can be a challenge in the context of a team-based approach, especially with the addition of new team members within the patients’ circle of care—particularly the addition of learners such as family medicine residents and clinical clerks.
The purpose of this study was to identify the satisfaction levels of patients at the VFMC receiving care from a multidisciplinary team that included multiple learners. Additionally, we were particularly interested to know whether patients were satisfied with access and continuity of care in this type of medical setting.
METHODS
After a thorough literature review, the General Practice Assessment Survey,7 the Primary Care Assessment Tool,8 and the SF-12 (12-item Short-Form Health Survey)9 were chosen as the measures most easily adaptable to our Canadian primary health care setting. Additional modifications to portions of the General Practice Assessment Survey and Primary Care Assessment Tool instruments were made to better adapt it to the VFMC patient population. As a result of the modifications to these previously validated tools, a small pilot study was undertaken to ensure clarity and validity of the survey. Further revision to the survey instrument was undertaken based on the responses and feedback from the pilot study. The biggest change to the survey was providing clearer definitions of types of physicians. Staff family doctors were identified as those who oversaw the team, and resident family physicians were identified as learners in the practice.
The VFMC Patient Satisfaction Survey was distributed to a stratified random sample of 600 patients of the VFMC. The sample was chosen from the total number of patients at the VFMC stratified to include an equal number from each practice. Exclusion criteria for patients included being younger than 18 years, not understanding written English, and participation in the pilot study.
Questionnaires, personalized information letters, and self-addressed stamped envelopes were distributed to participants according to a modified Dillman method.10 One week after the initial survey mailing a reminder thank-you card was sent to all patients. After 3 weeks a complete survey package was mailed to all nonresponders. Questionnaires were returned to the VFMC in confidence; however, each survey contained a unique code in order to eliminate duplicate mailings and to link patients with physician teams.
The survey data were entered and analyzed using SPSS, version 16.
Ethics approval
This research received ethical approval from the Health Sciences Research Ethics Board at the University of Western Ontario.
RESULTS
Six hundred surveys, stratified by practice, were distributed to patients of the VFMC, and 301 usable responses were returned for a response rate of 50%. Demographic characteristics of the respondents are summarized in Table 1. Respondents were predominantly white (91%), born in Canada (83%), educated to the level of college diploma or higher (56%), and employed full time (55%). Figure 1 indicates the overall satisfaction levels with care at the VFMC. Patients were indeed more satisfied than dissatisfied. Median satisfaction on a scale of 1 to 7 was 6 or “very satisfied.” Satisfaction levels were not significantly different between clinic practices (P = .325). Given the small number of patients in the neutral group or any of the dissatisfied groups, these 4 satisfaction groups were combined into a single “unsatisfied” group for all subsequent analyses. Overall, 88% of patients were fairly, very, or completely satisfied, and 12% were neutral, fairly, very, or completely dissatisfied with care.
Table 1.
Selected demographic characteristics of patients responding to the VFMC Patient Satisfaction Survey
| CHARACTERISTIC | VALUE, N (%) |
|---|---|
| Sex (n = 298) | |
| • Female | 200 (67.1) |
| • Male | 98 (32.9) |
| Age, y (n = 287) | |
| • ≤ 38 | 53 (18.5) |
| • 39–45 | 49 (17.1) |
| • 46–51 | 46 (16.0) |
| • 52–56 | 45 (15.7) |
| • 57–66 | 47 (16.4) |
| • ≥ 67 | 47 (16.4) |
| Marital status (n = 299) | |
| • Single | 44 (14.7) |
| • Married | 169 (56.5) |
| • Common law | 34 (11.4) |
| • Divorced | 33 (11.0) |
| • Separated | 10 (3.3) |
| • Widowed | 9 (3.0) |
| Highest level of education (n = 296) | |
| • High school diploma | 128 (43.2) |
| • College or technical diploma | 96 (32.4) |
| • University degree | 71 (24.0) |
| • Other | 1 (0.3) |
| Income level, $ (n = 283) | |
| • ≤ 20 000 | 53 (18.7) |
| • 20 001–36 000 | 50 (17.7) |
| • 36 001–59 000 | 58 (20.5) |
| • 59 001–72 756 | 40 (14.1) |
| • ≥ 72 757 | 82 (29.0) |
| Length of time as a patient of the VFMC, y (n = 297) | |
| • ≤ 5 | 83 (27.9) |
| • 6–10 | 67 (22.6) |
| • 11–20 | 72 (24.2) |
| • > 20 | 75 (25.3) |
| Diagnosis (n = 248) | |
| • Long-term physical condition | 167 (67.3) |
| • Long-term mental or psychological condition | 81 (28.3) |
VFMC—Victoria Family Medical Centre.
Figure 1.
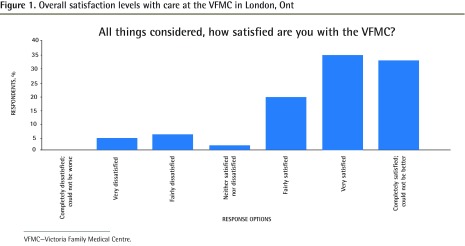
Overall satisfaction levels with care at the VFMC in London, Ont
VFMC—Victoria Family Medical Centre.
There was no difference between groups (satisfied vs unsatisfied) in the length of time the respondents had been patients at the VFMC or patients of particular physicians. There was no difference in satisfaction level between patients who had been diagnosed with physical conditions and those diagnosed with psychological conditions.
A logistic regression analysis of 4 independent demographic factors—sex, age, birth in Canada, and length of time as a VFMC patient—revealed that the 4 factors, taken together, were significantly associated with patient satisfaction (
 6,278 = 13.75, P = .032). Of those factors, age made the most significant contribution to the model (P = .035).
6,278 = 13.75, P = .032). Of those factors, age made the most significant contribution to the model (P = .035).
Access to care
Access to care was explored through a number of themes. One thematic area centred on clinic hours and how patients felt about their ability to access the physicians at the clinic. Most patients (59%) believed that the clinic hours were very good or excellent, although 40% of patients would have liked to see the clinic hours extended into the evening (26%) or weekend (14%). Less satisfied patients were also less satisfied with clinic hours (P < .001), with more dissatisfied patients more likely to prefer clinic hours extended into the early morning or over the lunch hour.
When patients booked appointments with any doctors, the median wait time was 2 working days; when patients requested specific doctors, the median wait time was increased by 1 day (Figure 2).
Figure 2.
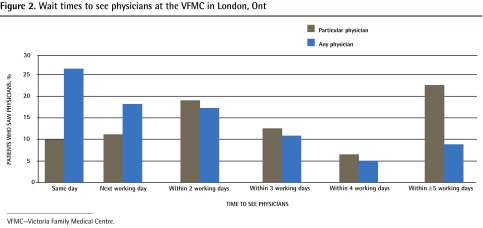
Wait times to see physicians at the VFMC in London, Ont
VFMC—Victoria Family Medical Centre.
There was a relationship between overall patient satisfaction with wait times and satisfaction with which doctor they saw. Less satisfied patients were less satisfied with wait times (P < .001) and believed they had longer wait times when booking appointments with any (P < .001) or specific (P = .004) doctors. While most patients were able to see doctors when they had urgent needs, completely satisfied patients made up the largest proportion (39%) of those patients who were able to get in (68% overall), while fairly satisfied patients made up the largest proportion (38%) of those patients who believed that they were unable to get in when they had urgent needs (6% overall).
Continuity of care
Sixty-four percent of respondents indicated that their usual doctors were SFDs, while 36% indicated their usual doctors were family medicine residents. There was no difference in satisfaction level between patients who considered their usual doctors to be SFDs and patients who considered their usual doctors to be residents. There was a breakdown in satisfaction when patients believed that they saw their usual doctors less often: 13% of unsatisfied patients responded that they saw their usual doctors never or almost never, while 60% of completely satisfied patients responded that they saw their usual doctors always, almost always, or a lot of the time (P = .001). Sixty percent of unsatisfied patients rated the frequency of their interactions with their usual doctors as poor, while more than 70% of completely satisfied patients rated the frequency of their interactions as excellent or very good (P < .001).
Patients in the satisfied group were more likely to feel connected to the VFMC through relationships with other staff members (P < .001), most often with the family practice nurse (approximately 60%) and the receptionist (approximately 20%).
DISCUSSION
This study of patient satisfaction at a family medicine teaching clinic found that satisfaction was not independently related to sex, income, employment, diagnosis, or treatment, but was more related to service components such as access to care and continuity of care with the patients’ usual doctors. The respondents in this survey were predominantly white, so one would not anticipate race to be a significant factor in interpreting our analysis. In fact, the literature does not support race as a substantial factor affecting patient satisfaction.11
There was no difference in satisfaction between patients who considered their usual doctors to be residents and those who considered their usual doctors to be SFDs. This is particularly important and comforting for family medicine training programs, in which both SFDs and residents provide care.
One would expect that a longer relationship with a physician would lead to more patient satisfaction, as has been suggested in the literature.1–5 This was not found in our study, perhaps because the unsatisfied group was so small in number. An additional possibility could be that patients established relationships with doctors earlier and developed them quickly because of the frequent turnover of physicians in the teaching practice. Furthermore, residents might have been viewed as extensions of the SFDs and, therefore, seeing residents was less likely to affect patient satisfaction.
While length of time as a patient did not seem to affect satisfaction levels in our study, the ability of patients to see their usual doctors was associated with increased satisfaction. Thus, relational continuity in this study was shown to be more important than length of time as a patient in establishing patient satisfaction. This is consistent with the findings of Starfield12 and Gray et al.13
Reduced continuity of care is viewed as a potential drawback to team-based care models such as the Patient’s Medical Home proposed by the College of Family Physicians of Canada.14,15 The findings in this study support reduced continuity of care as a drawback. Multidisciplinary teams should be encouraged to adopt practices that would facilitate patient contact with their usual physicians as often as possible. In this study, continuity with other team members, such as the family practice nurse or receptionist, also enhanced patient satisfaction. This was shown previously in a study of long-term patients attending a family medicine teaching clinic.16 Considering it is neither possible nor necessary that the patient see the same doctor or any doctor at each visit, multidisciplinary teams could enhance patient satisfaction with care by adopting practices that facilitate continuity with other team members, as well as with the doctors, where appropriate. This would help to reinforce the concept of team-based continuity with patients. This is an example of the relational continuity described by Haggerty et al in which, even when ongoing relationships with multiple care providers are challenging, “a consistent core of staff can provide patients with a sense of predictability and coherence.”4
While access to care, or wait times, in this study could be regarded as good, access still had an influence on patient satisfaction. Patients with better access were more satisfied. This finding supports the recommendation for family practices to adopt methods that increase access to care such as the advanced access scheduling systems currently being advocated.17–19
The findings on continuity and access were consistent with other findings in the literature. Morgan et al, in their study on continuity of care, showed that most patients were satisfied to see their preferred doctors, but a subset valued more rapid access over preferred providers.20
Extended hours on evenings and weekends are part of the services provided by patient enrolment models of care in Ontario, including at the VFMC. The findings in this study suggest that patient education about clinic hours and services is essential, and could be improved for the VFMC.
Limitations
Pilot work with the VFMC Patient Satisfaction Survey suggested that patients had difficulty distinguishing between SFDs and family medicine residents. Although the final survey included an explanatory note that explicitly named the SFDs at the VFMC, comments on the returned surveys suggested that a few patients still did not make the distinction between SFDs and residents. This conflation of SFDs and residents might have complicated the interpretation of survey responses about continuity of care; however, the number of respondents that indicated confusion was small.
The response rate was only fair, despite use of the Dillman method. Monetary incentives might have improved the response rate but might have influenced the results. This was a study of patient satisfaction in a family medicine teaching clinic and the results might not be applicable to other family practice settings.
Conclusion
Patients were generally satisfied with the care provided at the VFMC. Older patients tended to be more satisfied than younger patients. Points of dissatisfaction were related to wait times for appointments and continuity with patients’ usual doctors. More satisfied patients also felt connected through other team members including the nurse and receptionist. These findings support the adoption of practices that reduce wait times and facilitate continuity with patients’ usual doctors and other team members.
EDITOR’S KEY POINTS
This study of patient satisfaction at a family medicine teaching clinic found that satisfaction was not independently related to sex, income, diagnosis, or treatment, but was more related to service components such as access to care and continuity of care with the patients’ usual doctors.
There was no difference in satisfaction between patients who considered their usual doctors to be residents and those who considered their usual doctors to be staff family doctors.
While access to care, or wait times, in this study could be regarded as good, access still had an influence on patient satisfaction. Patients with better access were more satisfied. This finding supports the recommendation for family practices to adopt methods that increase access to care.
POINTS DE REPÈRE DU RÉDACTEUR
Cette étude sur la satisfaction des clients d’une clinique universitaire de médecine familiale a montré que leur niveau de satisfaction n’est pas relié de façon indépendante à leur sexe, leur revenu, leur diagnostic ou leur traitement, mais plutôt à certaines composantes des services comme l’accès aux soins et leur continuité avec le médecin habituel du patient.
Les patients qui pensaient que leur médecin habituel était un résident et ceux qui pensaient que c’était un médecin de famille faisant partie du personnel avaient le même niveau de satisfaction.
Même si on peut dire que l’accès aux soins et le temps d’attente étaient satisfaisants dans cette étude, l’accès aux soins avait quand même une influence sur la satisfaction des patients, ceux qui avaient un meilleur accès étant plus satisfaits. D’après ces résultats, les cliniques de médecine familiale auraient avantage à adopter des mesures pour augmenter l’accès aux soins.
Footnotes
This article has been peer reviewed.
Cet article a fait l’objet d’une révision par des pairs.
Contributors
All authors contributed to the concept and design of the study; data gathering, analysis, and interpretation; and preparing the manuscript for submission.
Competing interests
None declared
References
- 1.McWhinney IR, editor. A textbook of family medicine. 2nd ed. New York, NY: Oxford University Press; 1997. Principles of family medicine; pp. 18–20. [Google Scholar]
- 2.Hennen BK. Continuity of care in family practice. Part 1: dimensions of continuity. J Fam Pract. 1975;2(5):371–2. [PubMed] [Google Scholar]
- 3.McWhinney IR. Continuity of care in family practice. Part 2: implications of continuity. J Fam Pract. 1975;2(5):373–4. [PubMed] [Google Scholar]
- 4.Haggerty JL, Reid RJ, Freeman GK, Starfield BH, Adair CE, McKendry R. Continuity of care: a multidisciplinary review. BMJ. 2003;327(7425):1219–21. doi: 10.1136/bmj.327.7425.1219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hjortdahl P, Laerum E. Continuity of care in general practice: effect on patient satisfaction. BMJ. 1992;304(6837):1287–90. doi: 10.1136/bmj.304.6837.1287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bower P, Roland M, Campbell J, Mead N. Setting standards based on patients’ views on access and continuity: secondary analysis of data from the general practice assessment survey. BMJ. 2003;326(7383):258. doi: 10.1136/bmj.326.7383.258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ramsay J, Campbell JL, Schroter S, Green J, Roland M. The General Practice Assessment Survey (GPAS): test of data quality and measurement properties. Fam Pract. 2000;17(5):372–9. doi: 10.1093/fampra/17.5.372. [DOI] [PubMed] [Google Scholar]
- 8.Shi L, Starfield B, Xu J. Validating the adult Primary Care Assessment Tool. J Fam Pract. 2001;50(2):161w–75w. [Google Scholar]
- 9.Ware J, Jr, Kosinski M, Keller SD. A 12-item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34(3):220–33. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 10.Dillman DA. Mail and Internet surveys: the tailored design method. 2nd ed. New York, NY: Wiley; 2000. [Google Scholar]
- 11.Barr DA. Race/ethnicity and patient satisfaction. Using the appropriate method to test for perceived differences in care. J Gen Intern Med. 2004;19(9):937–43. doi: 10.1111/j.1525-1497.2004.30415.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Starfield B. Is patient-centered care the same as person-focused care? Perm J. 2011;15(2):63–9. doi: 10.7812/tpp/10-148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gray DP, Evans P, Sweeney K, Lings P, Seamark D, Seamark C, et al. Towards a theory of continuity of care. J R Soc Med. 2003;96(4):160–6. doi: 10.1258/jrsm.96.4.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.College of Family Physicians of Canada . A vision for Canada. Family practice: the patient’s medical home. Mississauga, ON: College of Family Physicians of Canada; 2011. Available from: www.cfpc.ca/uploadedFiles/Resources/Resource_Items/PMH_A_Vision_for_Canada.pdf. Accessed 2014 Mar 13. [Google Scholar]
- 15.Rosser WW, Colwill JM, Kasperski J, Wilson L. Progress of Ontario’s Family Health Team model: a patient-centered medical home. Ann Fam Med. 2011;9(2):165–71. doi: 10.1370/afm.1228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Brown JB, Dickie I, Brown L, Biehn J. Long-term attendance at a family practice teaching unit. Qualitative study of patients’ views. Can Fam Physician. 1997;43:901–6. [PMC free article] [PubMed] [Google Scholar]
- 17.Soloway B, Swartz J. Advanced access scheduling. Fam Med. 2009;41(7):462–4. [PubMed] [Google Scholar]
- 18.Baxley EG, Weir S. Advanced access in academic settings: definitional challenges. Ann Fam Med. 2009;7(1):90–1. doi: 10.1370/afm.953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mitchell V. Same-day booking. Success in a Canadian family practice. Can Fam Physician. 2008;54:379–83. [PMC free article] [PubMed] [Google Scholar]
- 20.Morgan ED, Pasquarella M, Holman JR. Continuity of care and patient satisfaction in a family practice clinic. J Am Board Fam Pract. 2004;17(5):341–6. doi: 10.3122/jabfm.17.5.341. [DOI] [PubMed] [Google Scholar]


