Abstract
Objective
To describe the associations between the socioeconomic status of emergency department (ED) users and age, sex, and acuity of medical conditions to better understand users’ common characteristics, and to better meet primary and ambulatory health care needs.
Design
A retrospective, observational, population-based analysis. A rigorous proxy of socioeconomic status was applied using census-based methods to calculate a relative deprivation index.
Setting
Ontario.
Participants
All Ontario ED visits for the fiscal year April 1, 2008, to March 31, 2009, from the National Ambulatory Care Reporting System data set.
Main outcome measures
Emergency department visits were ranked into deprivation quintiles, and associations between deprivation and age, sex, acuity at triage, and association with a primary care physician were investigated.
Results
More than 25% of ED visits in Ontario were from the most deprived population; almost half of those (12.3%) were for conditions of low acuity. Age profiles indicated that a large contribution to low-acuity ED visits was made by young adults (aged 20 to 30 years) from the most deprived population. For the highest-volume ED in Ontario, 94 of the 499 ED visits per day were for low-acuity patients from the most deprived population. Most of the highest volume EDs in Ontario (more than 200 ED visits per day) follow this trend.
Conclusion
Overall input into EDs might be reduced by providing accessible and appropriate primary health care resources in catchment areas of EDs with high rates of low-acuity ED visits, particularly for young adults from the most deprived segment of the population.
Résumé
Objectif
Déterminer s’il existe des associations entre le statut socioéconomique des personnes qui visitent les départements d’urgence (DU) et leur âge, leur sexe et la sévérité de leur condition médicale, et ce, afin de mieux comprendre leurs caractéristiques communes et pour mieux répondre aux soins ambulatoires dont ils ont besoin.
Type d’étude
Analyse observationnelle rétrospective basée sur une population. Une mesure rigoureuse du statut socioéconomique à partir des données du recensement a servi à calculer un indice relatif de dépossession.
Contexte
L ‘Ontario.
Participants
Toutes les visites effectuées aux DU de l’Ontario au cours de l’année fiscale 2008 (1er avril au 31 mars), selon les données du Système national d’information sur les soins ambulatoires.
Principaux paramètres à l’étude
On a classé les visites aux DU en quintiles de dépossession et recherché les associations entre la dépossession et l’âge, le sexe, l’urgence au triage ainsi que le fait d’avoir un médecin de première ligne.
Résultats
Plus de 25 % des visites aux DU en Ontario provenaient de la population la moins favorisée; près de la moitié de ces visites (12,3 %) étaient pour des conditions peu urgentes. Le profil des âges montrait qu’une importante proportion de ces visites provenait de jeunes adultes (entre 20 et 30 ans) appartenant à la population la moins favorisée. Dans le cas du DU ayant le plus de visites en Ontario, 94 des 499 visites par jour étaient faites par des patients nécessitant des soins peu urgents qui appartenaient au groupe le moins favorisé. On observait la même tendance dans la plupart des DU ayant le plus de visites en Ontario (plus de 200 visites par jour).
Conclusion
On pourrait réduire le nombre de visites à l’urgence en fournissant des ressources accessibles et appropriées pour des soins de première ligne dans des régions sanitaires où des DU ont un taux élevé de visites peu urgentes, provenant surtout de jeunes adultes appartenant au segment de la population le moins favorisé.
Social and economic inequalities underpin the health of Canadians: despite access to universal health care, Canadians of low socioeconomic status (SES) continue to have poorer overall health and poorer health outcomes than more advantaged citizens.1,2 In particular, people of low SES use medical services such as emergency departments (EDs) more frequently.3–5 One focus of current health care reform is to reduce wait times in EDs; lengthy wait times are influenced by crowded EDs and have multifactorial causes.6 One component of solving these problems is to reduce the overall input of patients to EDs. To do so, we must understand the social and economic conditions of the patients accessing ED services. We have shown previously that, in general, the most socially and materially deprived Ontarians use the ED more than the least deprived, and specifically they use the ED more for medical conditions of low acuity.7 In the current study, we present all Ontario ED visits for 2008, and apply a rigorous proxy of SES allowing an accurate description of the populations accessing ED services, and in particular those patients presenting with medical conditions of low acuity. This research could spearhead informed decisions regarding placement of primary health care resources that could ultimately reduce patient input to Ontario EDs.
Crowded EDs lead to myriad problems in our health care system, such as increased wait times,6,8 increased suffering, increased risk of in-hospital mortality,9 and reduced satisfaction for health care workers.6 The causes of crowding are complex and contentious. Some research suggests that ED crowding is symptomatic of overall hospital inefficiencies, with a lack of upstream access to acute care beds.10,11 Others propose that the use of the ED for health conditions of low acuity is excessive and might exacerbate crowding; diverting these patients to their primary care physicians (PCPs) or to other appropriate medical services would reduce patient input, and might reduce ED wait times.12–14 Most research supports the view that reducing the presentation of low-acuity patients at EDs would only minimally affect wait times, as patients of low acuity do not generally require acute care beds or extensive time for diagnosis and treatment.15,16 However, it is still important to understand who is accessing the ED for reasons of low acuity, as these patients represent nearly half of all ED visits7 and might take up to 30% of ED physician time for treatment at some facilities.17 Focusing primary health care resources on populations using the ED for medical conditions of low acuity might help to alleviate overall ED input and staff workload, as well as improve overall health for populations of demonstrated need.
The objectives of this study are to describe the demographic characteristics of patients accessing medical care at Ontario EDs for conditions of low acuity. We examined data from 2008 describing patient flow into Ontario EDs for patients with medical conditions of low acuity according to SES, sex, age, and attachment to a PCP. Socioeconomic status is approximated using an ecologic deprivation index developed by Pampalon and co-workers18 and defined using the 2006 Canadian census. Observed trends in demographic characteristics are discussed in relation to primary health care policy measures that could reduce ED patient input and wait times.
METHODS
This study is a retrospective, observational, population-based analysis of all Ontario ED visits for the fiscal year April 1, 2008, to March 31, 2009. Ethics approval was obtained from the Queen’s University Health Sciences and Affiliated Teaching Hospitals Research Ethics Board. Ontario ED data were extracted from the National Ambulatory Care Reporting System (NACRS) data set. Data elements used in this study included year of visit, postal code, triage acuity, sex, age, and attachment to a PCP. Data quality, including accuracy and comparability, is described in yearly executive summaries for the NACRS data set and, in general, the data sets are complete for 2008, with low incidence of duplication of records and non-submission of data.19
The relative urgency, or acuity, of medical conditions is estimated using the Canadian Triage and Acuity Scale (CTAS). The CTAS provides a standardized guideline to determine the urgency of care for each patient in relation to the presenting case mix.20 Scores range from CTAS I for patients requiring immediate medical attention, to CTAS V for patients presenting with medical conditions that were considered nonurgent and who might safely experience a delay in medical care. For the purposes of this study, CTAS IV (less urgent) and CTAS V (nonurgent) are collectively considered cases of low acuity.15,21 Scores of CTAS I, II, and III represent cases assessed as resuscitation, emergent, and urgent, respectively, and were collectively considered cases of high acuity.
Approximation of SES was made using a combined material and social deprivation index according to the method described by Pampalon et al.18 Briefly, this method uses social and material elements derived from the 2006 Canadian census that best reflect a dissemination area’s average SES. Dissemination areas correspond to distinct postal codes with 400 to 700 residents each. The relevant census elements are the proportions of adults living alone with marital statuses of separated, divorced, or widowed, and single-parent families (social factors); and education, employment, and income (material factors). These data are used to rank postal codes into quintiles of relative deprivation, with the lowest quintile (Q1) corresponding to the population with the least social and material deprivation, and the highest quintile (Q5) having the most social and material deprivation. A patient’s postal code is then used to define the patient’s SES according to conditions observed at the neighbourhood level. All data extracted from the NACRS data set were located using postal codes, and ED visits were then ranked by deprivation quintile. Emergency department visits were further analyzed according to triage acuity, sex, age, and PCP status. Primary care physician status is recorded in the NACRS data set as a patient self-reporting having a PCP or not having a PCP, and does not give any information regarding the details of those associations. Data compilation and analysis were made using R software, version 2.14.2.
RESULTS
In 2008, the population of Ontario was 12 934 499 and 5 337 956 unique visits were made to the ED (Table 1).22 The rate of use was 413 ED visits per 1000 population, with 51.8% of ED visits made by female patients. The percentage of ED visits among Q2, Q3, and Q4 individuals ranged between 17.8% and 18.8%. The percentage of ED visits for Q1 was 13.3% and for Q5 was 25.4%. Medical conditions of low acuity (CTAS IV and V combined) accounted for 47.3% of all ED visits.
Table 1.
Ontario population, number of ED visits, percentage from each deprivation quintile (Q1 is the least deprived, Q5 is the most deprived), and number of low-acuity (CTAS IV and CTAS V) ED visits
| CHARACTERISTIC | VALUE |
|---|---|
| Ontario population as of July 1, 2008* | 12 934 499 |
| No. of ED visits | 5 337 956 |
| No. of ED visits per 1000 population | 413 |
| ED visits from female patients, % | 51.8 |
| ED visits from each deprivation quintile,† % | |
| • Q1 | 13.3 |
| • Q2 | 17.8 |
| • Q3 | 18.0 |
| • Q4 | 18.8 |
| • Q5 | 25.4 |
| CTAS IV | |
| • No. of ED visits | 2 074 586 |
| • Proportion of total ED visits | 38.9 |
| CTAS V | |
| • No. of ED visits | 450 068 |
| • Proportion of total ED visits | 8.4 |
CTAS—Canadian Triage and Acuity Scale, ED—emergency department.
Ontario population from Statistics Canada.22
Total is not 100% owing to omission of postal code data in 6.7% of patient records.
The number of CTAS IV ED visits from Q1 represents 5.2% of all ED visits, or 21 ED visits per 1000 population (Table 2). Only 0.8% of Q1 patients were ranked as CTAS V (3 ED visits per 1000 population). For Q5, CTAS IV visits represented 9.9% of all ED visits (41 per 1000 population), and CTAS V visits represented 2.4% of all ED visits (10 per 1000 population). The relative number of Q5 to Q1 ED visits was 1.90 for CTAS IV visits, and 3.18 for CTAS V visits.
Table 2.
Details for low-acuity (CTAS IV and V) ED visits for the Q1 (least deprived) and Q5 (most deprived) populations
| ACUITY | Q1 | Q5 | RELATIVE NO. OF Q5 VISITS TO Q1 VISITS |
|---|---|---|---|
| CTAS IV | 1.90 | ||
| • No. of ED visits | 277 169 | 527 813 | |
| • ED visits, % | 5.2 | 9.9 | |
| • No. of ED visits per 1000 population | 21 | 41 | |
| • ED visits by female patients, % | 48.6 | 52.2 | |
| CTAS V | 3.18 | ||
| • No. of ED visits | 40 797 | 129 901 | |
| • ED visits, % | 0.8 | 2.4 | |
| • No. of ED visits per 1000 population | 3 | 10 | |
| • ED visits by female patients, % | 47.6 | 50.5 |
CTAS—Canadian Triage and Acuity Scale, ED—emergency department, Q1—quintile 1, Q5—quintile 5.
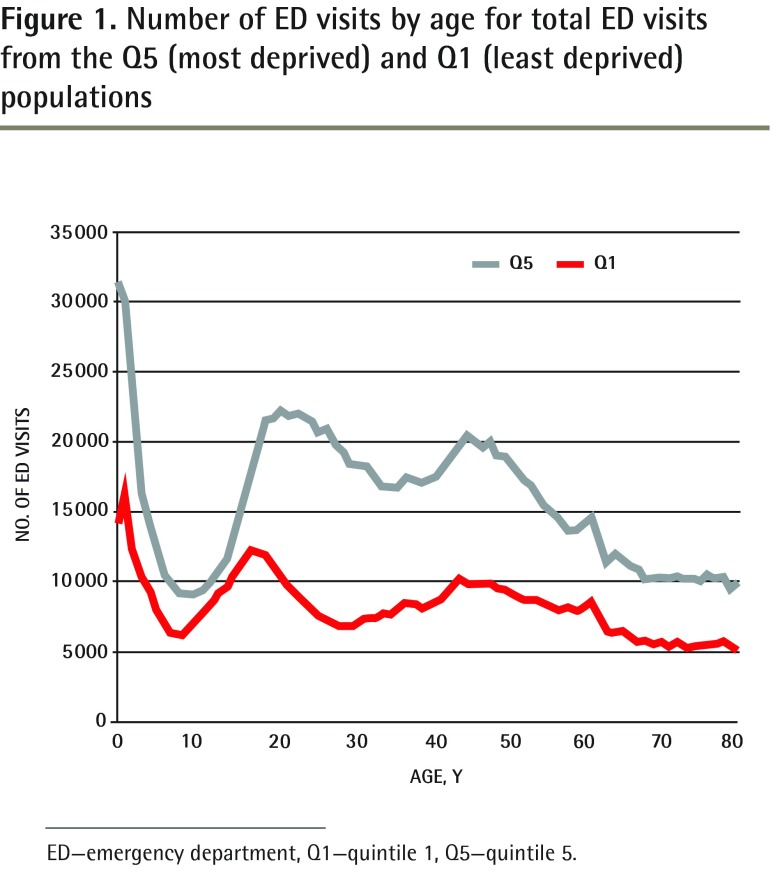
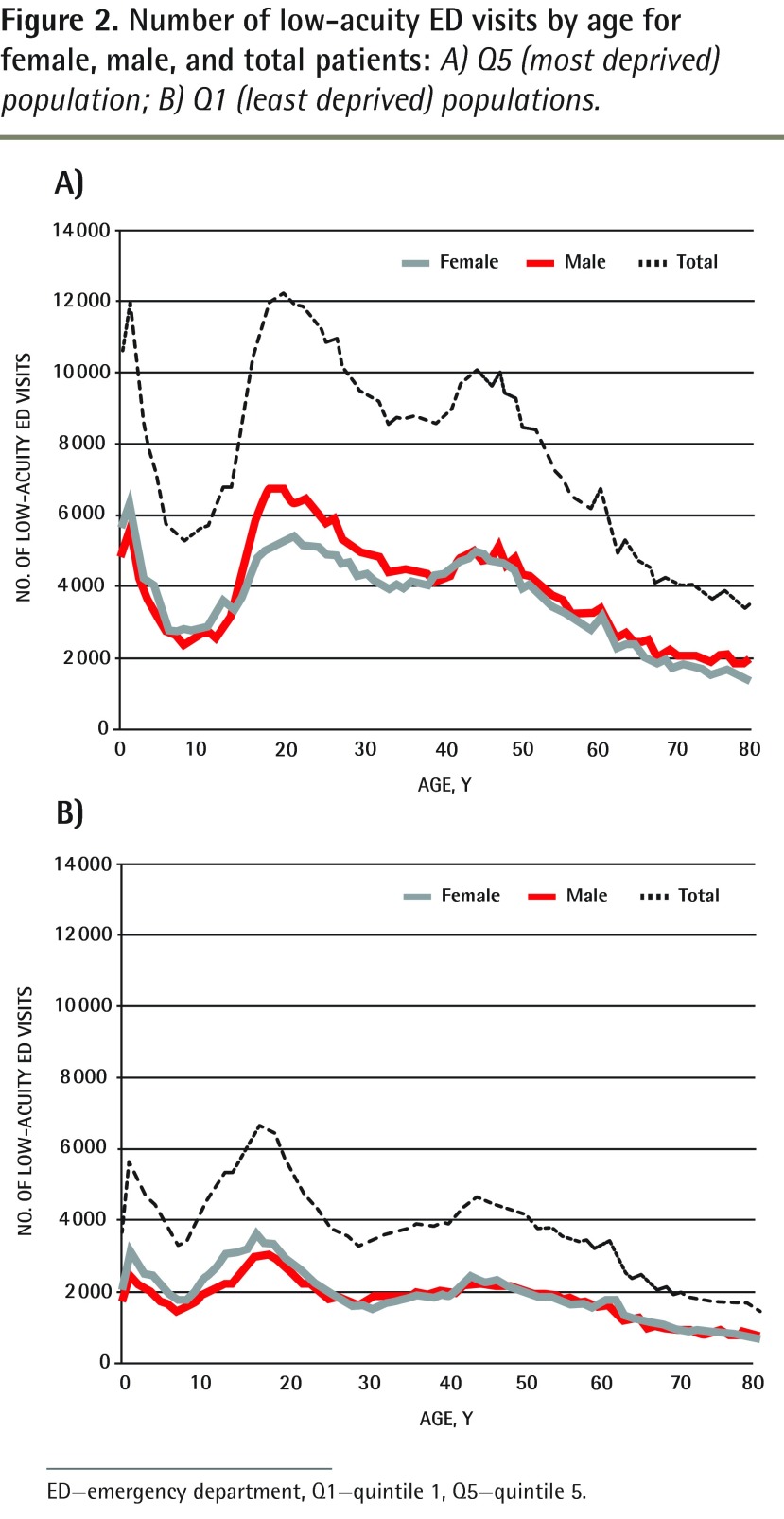
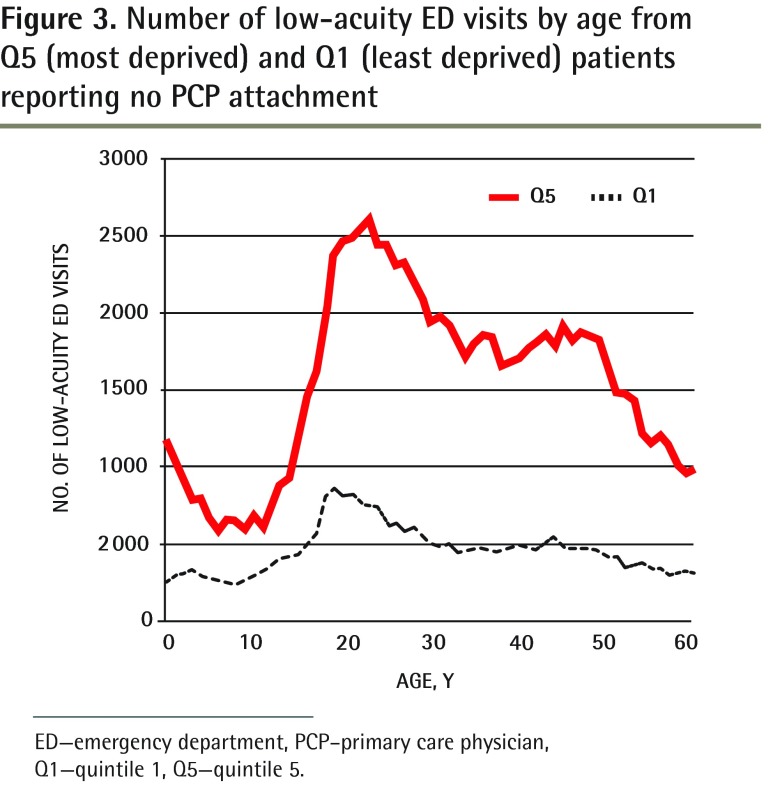
The age profiles for the number of ED visits for both Q1 and Q5 are shown in Figure 1. Quintile 5 represents more than 30% of all ED visits between the ages of 21 and 30. The age profiles for low-acuity ED patients from the Q5 and Q1 populations are shown in Figures 2A and 2B, respectively, for both males and females. The greatest difference in low-acuity ED visits between the sexes is observed for those in their late teens and early 20s. Finally, in Figure 3, the age profiles of Q5 patients who reported not having PCPs and who presented to the ED with low-acuity medical conditions are shown for both Q1 and Q5. Beyond the age of 19, a Q5 individual without a PCP is at least 3 times more likely to use the ED for low-acuity medical conditions.
Figure 1.
Number of ED visits by age for total ED visits from the Q5 (most deprived) and Q1 (least deprived) populations
ED—emergency department, Q1—quintile 1, Q5—quintile 5.
Figure 2.
Number of low-acuity ED visits by age for female, male, and total patients: A) Q5 (most deprived) population; B) Q1 (least deprived) populations.
ED—emergency department, Q1—quintile 1, Q5—quintile 5.
Figure 3.
Number of low-acuity ED visits by age from Q5 (most deprived) and Q1 (least deprived) patients reporting no PCP attachment
ED—emergency department, PCP–primary care physician, Q1—quintile 1, Q5—quintile 5.
In 2008, the ED with the largest patient volume in Ontario treated approximately 499 patients per day, or a total of 182 273 per year (Table 3). Of these, 221 ED visits per day were of low acuity, and 94 of these were from the Q5 population. Most of the other 17 Ontario EDs with more than 200 visits per day had more than 25% of visits from Q5 patients (Table 4). The number of low-acuity Q1 patients ranged from 4 to 36 patients per day, and low-acuity Q5 patients ranged from 6 to 66 patients per day.
Table 3.
Number of ED visits per day, number of low-acuity ED visits per day, and percentage of low-acuity visits by deprivation quintile (Q1 is the least deprived, Q5 is the most deprived) for the Ontario ED with the highest patient volume
| QUINTILE | NO. OF ED VISITS | NO. OF ED VISITS PER DAY | NO. OF LOW-ACUITY VISITS PER DAY | LOW-ACUITY ED VISITS, % OF ED VISITS PER DAY |
|---|---|---|---|---|
| Q1 | 17 933 | 49 | 21 | 4.2 |
| Q2 | 23 747 | 65 | 28 | 5.6 |
| Q3 | 28 538 | 78 | 33 | 6.6 |
| Q4 | 36 171 | 99 | 45 | 9.0 |
| Q5 | 75 884 | 208 | 94 | 18.8 |
| Total | 182 273 | 499 | 221 | 44.2 |
ED—emergency department.
Table 4.
Demographic characteristics for Q1 and Q5 (Q1 is the least deprived, Q5 is the most deprived) quintiles for EDs in Ontario with input rates greater than 200 visits per day in 2008
| ED | NO. ED VISITS PER DAY |
TOTAL ED VISITS, %
|
NO. OF LOW-ACUITY ED VISITS PER DAY
|
||
|---|---|---|---|---|---|
| Q1 | Q5 | Q1 | Q5, N (%) OF TOTAL ED VISITS | ||
| 1* | 499 | 9.8 | 41.6 | 21 | 94 (18.8) |
| 2 | 382 | 10.6 | 17.0 | 10 | 14 (3.7) |
| 3 | 366 | 16.8 | 30.9 | 29 | 54 (14.8) |
| 4 | 344 | 16.8 | 22.8 | 23 | 28 (8.1) |
| 5 | 321 | 17.8 | 15.4 | 25 | 19 (5.9) |
| 6 | 293 | 38.1 | 7.9 | 35 | 6 (2.0) |
| 7 | 287 | 20.8 | 22.0 | 13 | 16 (5.6) |
| 8 | 269 | 15.4 | 36.3 | 12 | 32 (11.9) |
| 9 | 269 | 22.1 | 13.0 | 25 | 13 (4.8) |
| 10 | 263 | 11.1 | 37.6 | 20 | 66 (25.1) |
| 11 | 258 | 11.2 | 32.6 | 17 | 47 (18.2) |
| 12 | 254 | 9.7 | 29.6 | 13 | 35 (13.8) |
| 13 | 249 | 5.9 | 31.4 | 6 | 31 (12.4) |
| 14 | 247 | 6.2 | 39.1 | 5 | 27 (10.9) |
| 15 | 242 | 18.2 | 18.1 | 18 | 16 (6.6) |
| 16 | 234 | 6.6 | 42.6 | 4 | 25 (10.7) |
| 17 | 216 | 9.0 | 35.3 | 4 | 17 (7.9) |
| 18 | 206 | 27.4 | 25.8 | 36 | 31 (15.0) |
ED—emergency department.
Details for this ED are shown in Table 3.
DISCUSSION
In 2008, approximately 413 ED visits per 1000 population were made to Ontario EDs. The average rate for the years 2003 through 2009 was previously calculated to be 415 per 1000 population and was observed to be fairly stable during this period.7 It was also observed that the relative proportion of patients from each deprivation quintile was relatively constant between 2003 and 2009, with similar average proportions to those observed for 2008.7 Each deprivation quintile represents 20% of the population, and the proportions for Q2, Q3, and Q4 approach 20%: they were 17.8%, 18.0%, and 18.8%, respectively. However, the least deprived group, Q1, is underrepresented at the ED with only 13.3%, and the most deprived group, Q5, is overrepresented at the ED with 25.4%. The greater representation of patients of low SES at the ED correlates well with results from other studies and generally reflects the increased health care needs of the most vulnerable population and their associated poorer health status.1,3
For many of our subsequent analyses, observations were made for the extreme deprivation quintiles (Q1 and Q5), as we believed that a comparison of these populations would give the most information regarding the social demographic characteristics of those accessing the ED the most and the least often. Furthermore, it is of interest to characterize the patients that are seeking medical treatment at the ED for medical conditions of low acuity (CTAS IV and V), as the volume of these cases might be reduced by targeting health care resources to improve access to primary care.23 Nearly half of all ED visits were for low-acuity conditions (47.3% in 2008). Nearly twice as many patients in Q5 than in Q1 were triaged as CTAS IV: 9.9% and 5.2% of all ED visits, respectively. Patients triaged as CTAS V represented a small proportion of both populations, with 0.8% of all ED visits from Q1 and 2.4% from Q5. Although these are relatively low volumes of CTAS V patients, it is important to note that the Q5 patients are overrepresented for this triage acuity score.
It is important to understand the current patterns of ED use if primary health care initiatives are to effectively reduce ED workloads and improve overall health status for Ontarians. To understand what health care resources are needed, and in particular where these resources would best serve the Q5 population, it is helpful to examine the demographic characteristics of the Q5 population using ED services. An age profile of all ED visits for Q5 is shown in Figure 1, with Q1 shown for comparison. High rates of ED use are seen for children younger than 2 years for both Q5 and Q1, with twice as many Q5 ED visits, underscoring the association between maternal and infant health and SES. Volumes of ED visits drop sharply for both groups during the childhood years; ED visits approach similar rates for the most and least deprived populations, with the ratio of Q5 to Q1 reaching its lowest value of 1.18 at age 12. Peak volumes for both populations are reached again during the young-adult years, but at much higher rates for Q5. Approximately 30% of all ED visits are for Q5 individuals between the ages of 20 and 30 years, with the ratio of Q5 to Q1 reaching its highest value of 2.79 at age 29. Again, overall poorer health status and poorer health care practices are the main reasons for the over-representation of Q5 for all ages in the ED.
The age profile for low-acuity ED use by the Q5 population shows a similarly shaped profile, with volume peaks at ages 1 year and 20 years (Figure 2A). Proportionally more females than males present to the ED for low-acuity conditions during the peak observed in the early 20s. The reasons for this pattern are not clear and merit further study. In comparison, the age profile for low-acuity ED use by the Q1 population shows a similar pattern, with peak volume at age 17 years with a slightly higher proportion of males (Figure 2B). The reasons that a low-acuity patient chooses treatment at the ED are complex. For example, there might be real or perceived issues regarding PCP availability and accessibility or an overestimate of medical urgency.12,14,24 For people of low SES, the ED is also an important medical and social safety net.25 The high volume of young adults accessing ED services for low-acuity conditions from the Q5 population suggests a need for improved availability and accessibility of appropriate primary health care resources. Indeed, the number of low-acuity ED patients reporting no attachment to PCPs is 3 to 4 times higher for the Q5 population between the ages of 19 and 50 years than for the Q1 population at that age (Figure 3). The percentage of all ED patients who reported not having PCPs is 11.7%, and approximately 20% of these are low-acuity patients from the Q5 population, compared with only 5% from Q1.
The distribution of wealth is not uniform across Ontario, nor are the proportions of individuals from each deprivation quintile accessing each ED. For example, if Q5 patients presented to the ED at similar rates as Q1 patients for conditions of low acuity, nearly 340 000 fewer patients would be seen at Ontario EDs. Considering that there were 176 EDs reporting to NACRS in 2008, this would translate into a decrease of about 5 visits per day for each ED. However, any potential reduction in ED workload would only be experienced at EDs that disproportionately serve the Q5 population. The total number of visits for each ED ranged from 4 to 499 visits per day (mean 104). The ED with the highest rate triaged a total of 182 273 patients, with 41.6% of patients from Q5 and 9.8% from Q1 (Table 3). At this ED, nearly 19% of all visits (94 per day) were from Q5 individuals presenting with low-acuity conditions. Numbers for Q4 were also high for this ED, with another 45 low-acuity visits per day. Reducing these numbers by placing accessible and appropriate primary health care in the areas served by this ED might alleviate the workload experienced at this hospital. Indeed, this is not a typical Ontario ED in terms of throughput, but for the 18 EDs that saw more than 200 visits per day in 2008, all but 7 served a disproportionate number of Q5 patients (ie, greater than 25%) (Table 4). Further, low-acuity Q5 patients represented more than 10% of all ED visits in 10 of these EDs. These represent the EDs most likely to benefit from improved access and availability of primary health care resources for the most deprived populations.
These findings make clear the need to tailor health care resources to the needs of the population: reduction in input volumes at some EDs might be possible with improved and appropriate primary health care placed upstream for specific populations. Of course, not all low-acuity ED visits should be diverted from the ED, as the centralized resources available in the ED might be the most efficient access point for certain conditions. Further study regarding the nature of low-acuity visits to the ED is needed to better understand which upstream primary health care resources should be augmented. Further, geographic maps showing the relative deprivation of an ED’s catchment area can be generated from these data,7 as can the relative volumes of each deprivation quintile accessing ED services. These maps would be useful for targeting local inventions as opposed to relying on provincewide generalized interventions.
Limitations
This study is observational, etiologic, and contextual in nature, and there are associated limitations to any generalizations made about an individual from the characteristics of the population. The deprivation index employed in this study imposes uniformity to an average SES for all individuals in a dissemination area. Obviously there is variability, but this is not expected to affect results owing to the large population size used for this study.18 Several factors affect the trends observed, including the reliability of data reported to NACRS. Data quality is documented in yearly executive reports18; the data undergo a series of quality controls during capture and submission and no important issues were identified for this data set. In particular, it is difficult to estimate the accuracy of the data for attachment to PCPs without cross-referencing Ontario Health Insurance Plan numbers with other databases. Approximately 2.6% of records did not have information on attachment to PCPs; this likely led to underestimation of association between deprivation index and PCP attachment. Finally, consistency and accuracy in assigning triage scores is also assumed between and within EDs: the CTAS is revised and updated on an ongoing basis, with guidelines and implementation of standardized instructional materials, and there is general compliance with guidelines.26
Conclusion
The application of a rigorous measure of SES in this analysis makes clear that the most socially and materially deprived Ontarians, particularly young adults, use the ED disproportionately more than the least deprived do, generally for all medical conditions and particularly for low-acuity conditions. Socioeconomic status remains one of the principal determinants of health, despite decades of universal health care.1 The overrepresentation of young adults from Q5 at the ED for medical conditions of low acuity likely indicates problems with availability, accessibility, and appropriateness of primary health care resources for this population. Services for this age and social group need to be improved, both to increase overall health and to possibly alleviate ED workloads at some facilities, particularly those with a large patient throughput. Qualitative analyses of ED use patterns, including an analysis of diagnostic codes, might lead to greater understanding of the health care needs of this population. This work could improve understanding of issues affecting wait times at EDs and overall system utilization. If we are to make advancements in ED services and primary health care services in general, we need to focus on evidence-based placement of the right care for the right person in the right place.
EDITOR’S KEY POINTS
The application of a rigorous measure of socioeconomic status in this analysis makes clear that the most socially and materially deprived Ontarians, particularly young adults, use the emergency department (ED) disproportionately more than the least deprived do, particularly for low-acuity conditions.
The overrepresentation of young adults from the most deprived quintile in the ED for medical conditions of low acuity likely indicates problems with availability, accessibility, and appropriateness of primary health care resources for this population.
Services for this age and social group need to be improved, both to increase overall health and to possibly alleviate ED workloads at some facilities, particularly those with a large patient throughput. Qualitative analyses of ED use patterns, including an analysis of diagnostic codes, might lead to greater understanding of the health care needs of this population.
POINTS DE REPÈRE DU RÉDACTEUR
L’utilisation dans cette analyse d’une mesure rigoureuse du statut socioéconomique montre clairement que les Ontariens les moins favorisés sur les plans social et économique, et particulièrement les jeunes adultes, utilisent les départements d’urgence (DU) beaucoup plus souvent que les mieux nantis, particulièrement pour des conditions moins urgentes.
Le fait que des jeunes adultes du quintile le plus défavorisé sont surreprésentés dans les visites aux DU pour des conditions médicales de peu de gravité suggère qu’il existe des problèmes de disponibilité, d’accessibilité et de pertinence des ressources en soins primaires pour cette population.
Il y a lieu d’améliorer les services pour les personnes de cet âge et de ce statut socioéconomique, tant pour améliorer la santé globale que pour éventuellement diminuer la charge de travail des DU à certains endroits, surtout ceux qui sont très achalandés. Une analyse quantitative des modes d’utilisation des DU, incluant une analyse des codes de diagnostic, pourrait favoriser une meilleure compréhension des besoins de santé de cette population.
Footnotes
This article has been peer reviewed.
Cet article a fait l’objet d’une révision par des pairs.
Contributors
Dr VanStone contributed to the main body of work, including data analysis and interpretation. Dr Belanger provided the geocoding of all emergency department (ED) visits by postal code, computation of deprivation quintiles, relative ranking of all ED visits, and the geospatial mapping of ED visits. Drs Moore and Caudle contributed to the conceptual framework, data and statistical interpretation, and revision. All authors have reviewed the final manuscript and have provided their permission to publish the manuscript.
Competing interests
None declared
References
- 1.Alter DA, Stukel T, Chong A, Henry D. Lesson from Canada’s universal care: socially disadvantaged patients use more health services, still have poorer health. Health Aff (Millwood) 2011;30(2):274–83. doi: 10.1377/hlthaff.2009.0669. [DOI] [PubMed] [Google Scholar]
- 2.Raphael D, Curry-Stevens A, Bryant T. Barriers to addressing the social determinants of health: insights from the Canadian experience. Health Policy. 2008;88(2–3):222–35. doi: 10.1016/j.healthpol.2008.03.015. Epub 2008 May 8. [DOI] [PubMed] [Google Scholar]
- 3.Beattie TF, Gorman DR, Walker JJ. The association between deprivation levels, attendance rate and triage category of children attending a children’s accident and emergency department. Emerg Med J. 2001;18(2):110–1. doi: 10.1136/emj.18.2.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Glazier RH, Badley EM, Gilbert JE, Rothman L. The nature of increased hospital use in poor neighbourhoods: findings from a Canadian inner city. Can J Public Health. 2000;91(4):268–73. doi: 10.1007/BF03404286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stewart M, Reutter L, Makwarimba E, Rootman I, Williamson D, Raine K, et al. Determinants of health-service use by low-income people. Can J Nurs Res. 2005;37(3):104–31. [PubMed] [Google Scholar]
- 6.Hoot NR, Aronsky D. Systematic review of emergency department crowding: causes, effects and solutions. Ann Emerg Med. 2008;52(2):126–36. doi: 10.1016/j.annemergmed.2008.03.014. Epub 2008 Apr 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Caudle JM, VanStone NA, Wynn A, Biro S, Williamson T, Belanger P, et al. Trends in emergency department use in Ontario, 2003 to 2009: correlations between determinants of health and Canadian triage acuity scores. Poster presented at: Canadian Association of Emergency Physicians Annual Conference; 2013 Jun 1–5; Vancouver, BC. [Google Scholar]
- 8.Pines JM, Hilton JA, Weber EJ, Alkemade AJ, Al Shabanah H, Anderson PD, et al. International perspectives on emergency department crowding. Acad Emerg Med. 2011;18(12):1358–70. doi: 10.1111/j.1553-2712.2011.01235.x. [DOI] [PubMed] [Google Scholar]
- 9.Bernstein SL, Aronsky D, Duseja R, Epstein S, Handel D, Hwang U, et al. The effect of emergency department crowding on clinically oriented outcomes. Acad Emerg Med. 2009;16(1):1–10. doi: 10.1111/j.1553-2712.2008.00295.x. Epub 2008 Nov 8. [DOI] [PubMed] [Google Scholar]
- 10.Canadian Association of Emergency Physicians . Position statement on emergency department overcrowding. Ottawa, ON: Canadian Association of Emergency Physicians; 2009. [Google Scholar]
- 11.Rowe B, Bond K, Ospina M, Blitz S, Afilalo M, Campbell SG, et al. Frequency, determinants, and impact of overcrowding in emergency departments in Canada: a national survey of emergency department directors [Technology report no. 67.3] Ottawa, ON: Canadian Agency for Drugs and Technologies in Health; 2006. [Google Scholar]
- 12.Redstone P, Vancura JL, Barry D, Kutner JS. Nonurgent use of the emergency department. J Ambul Care Manage. 2008;31(4):370–6. doi: 10.1097/01.JAC.0000336555.54460.fe. [DOI] [PubMed] [Google Scholar]
- 13.Han A, Ospina MB, Blitz S, Strome T, Rowe BH. Patients presenting to the emergency department: the use of other health care services and reasons for presentation. CJEM. 2007;9(6):428–34. doi: 10.1017/s1481803500015451. [DOI] [PubMed] [Google Scholar]
- 14.Field S, Lantz A. Emergency department use by CTAS levels IV and V patients. CJEM. 2006;8(5):317–22. doi: 10.1017/s1481803500013968. [DOI] [PubMed] [Google Scholar]
- 15.Vertesi L. Does the Canadian Emergency Department Triage and Acuity Scale identify non-urgent patients who can be triaged away from the emergency department? CJEM. 2004;6(5):337–42. doi: 10.1017/s1481803500009611. [DOI] [PubMed] [Google Scholar]
- 16.Schull MJ, Kiss A, Szalai JP. The effect of low-complexity patients on emergency department waiting times. Ann Emerg Med. 2007;49(3):257–64. doi: 10.1016/j.annemergmed.2006.06.027. e1. Epub 2006 Aug 25. [DOI] [PubMed] [Google Scholar]
- 17.Office of the Auditor General of Ontario . 2010 annual report. Toronto, ON: Queen’s Printer for Ontario; 2010. [Google Scholar]
- 18.Pampalon R, Hamel D, Gamache P, Raymond G. A deprivation index for health planning in Canada. Chronic Dis Can. 2009;29(4):178–91. [PubMed] [Google Scholar]
- 19.Canadian Institute for Health Information . Database background and general data limitations documentation. National Ambulatory Care Reporting System (NACRS). 2008–2009. Executive summary. Ottawa, ON: Canadian Institute for Health Information; 2009. [Google Scholar]
- 20.Canadian Association of Emergency Physicians [website] Implementation guidelines. Ottawa, ON: Canadian Association of Emergency Physicians; 2012. Available from: http://caep.ca/resources/ctas/implementation-guidelines. Accessed 2012 Nov 1. [Google Scholar]
- 21.Steele S, Anstett D, Milne WK. Rural emergency department use by CTAS IV and V patients. CJEM. 2008;10(3):209–14. doi: 10.1017/s1481803500010125. [DOI] [PubMed] [Google Scholar]
- 22.Statistics Canada [website] Table 3.6-1. Ontario census divisions—annual population estimates at July 1. Ottawa, ON: Statistics Canada; 2013. Available from: www.statcan.gc.ca/pub/91-214-x/2010000/t043-eng.htm. Accessed 2014 Mar 5. [Google Scholar]
- 23.Glazier RH, Zagorski BM, Rayner J. Comparison of primary care models in Ontario by demographics, case mix and emergency department use, 2008/09 to 2009/10. Toronto, ON: Institute for Clinical Evaluative Sciences; 2012. [Google Scholar]
- 24.Wong WB, Edgar G, Liddy C, Vaillancourt C. Can after-hours family medicine clinics represent an alternative to emergency departments? Survey of ambulatory patients seeking after-hours care. Can Fam Physician. 2009;55:1106–7. e1–4. Available from: www.cfp.ca/content/55/11/1106.full.pdf+html. Accessed 2014 Mar 5. [PMC free article] [PubMed] [Google Scholar]
- 25.Browne AJ, Smye VL, Rodney P, Tang SY, Mussell B, O’Neil J. Access to primary care from the perspective of aboriginal patients at an urban emergency department. Qual Health Res. 2011;21(3):333–48. doi: 10.1177/1049732310385824. Epub 2010 Nov 12. [DOI] [PubMed] [Google Scholar]
- 26.Bullard MJ, Unger B, Spence J, Grafstein E, CTAS National Working Group Revisions to the Canadian Emergency Department Triage and Acuity Scale (CTAS) adult guidelines. CJEM. 2008;10(2):136–51. doi: 10.1017/s1481803500009854. [DOI] [PubMed] [Google Scholar]