Abstract
Sheehan's syndrome (SS) presents with hypopituitarism after parturition, usually preceded by postpartum hemorrhage. The first symptom of the disorder is lactation failure because of lactotroph cell necrosis. Recovery of lactotroph function after initial insult has not been reported in the literature. We describe the evaluation of a case of SS in whom lactotroph function recovered after the second pregnancy. A young woman delivered her first child at the age of 25 years; delivery was followed by severe postpartum hemorrhage and required blood transfusion. Sheehan's syndrome was diagnosed because of lactotroph, corticotroph, thyrotroph and somatotroph failure and empty sella on MRI. She conceived twice spontaneously and had normal lactation after the second delivery; investigations confirmed the normal basal and stimulable prolactin levels. We presume that recovery of lactotroph function after the second pregnancy in a patient with SS is possibly because of stimulatory effect of estrogen and progesterone on residual lactotroph cells.
Keywords: Prolactin function recovery, Sheehan's syndrome, lactotroph
INTRODUCTION
Sheehan's syndrome (SS) is development of partial or complete hypopituitarism following parturition, preceded in most of the cases by severe postpartum hemorrhage.[1] The disease continues to be common in some developing countries.[2,3,4] Some of the anterior pituitary functions like those of gonadotroph and corticotroph may be preserved in these women.[5] Lactotroph function is lost early in most of the women resulting in lactation failure. In fact, prolactin (PRL) response to thyrotropin-releasing hormone (TRH) is considered as the most important screening test to diagnose the syndrome.[6] Recovery of lactation function after initial failure has not been previously reported in these women. We present the long-term follow-up of a woman in whom lactotroph deficiency developed as a part of SS after first pregnancy and subsequently recovered after the second spontaneous pregnancy.
CASE REPORT
A 42-year-old woman delivered her first child in 1994 at the age of 25 years. She had prolonged labor, and delivery was complicated by retained placenta; she went into shock after profuse vaginal bleeding and received two blood transfusions at a city hospital. The child died after the 5th day due to birth asphyxia. She had lactation failure and did not resume menstrual cycles after lactation amenorrhea. She also had cold intolerance, constipation and fatigue. She was investigated in July 1996. Investigations revealed central hypothyroidism, growth hormone (GH), PRL and cortisol deficiency on insulin tolerance test [Table 1]. She was put on treatment in the form of prednisolone 7.5 mg/day, thyroxine 0.75 mg/day and cyclic estrogen/progesterone combination. In October 1996, she complained of polyuria and polydipsia and was investigated for possible diabetes insipidus, which was ruled out on water deprivation test. In October 2002, she noticed three episodes of spontaneous bleeding and was again evaluated. In addition to estimation of basal anterior pituitary hormones, she was subjected to insulin tolerance test to assess GH, cortisol, and PRL reserve; metoclopramide test to assess PRL reserve and gonadotropin-releasing hormone (GnRH) test for gonadotroph reserve. These tests again confirmed GH, cortisol and PRL deficiency. The method and results of these dynamic tests are given below. While she was stable on replacement of thyroxine, prednisolone and intermittent low-dose estrogen/progesterone combination, she came to the hospital with pregnancy of 12 weeks’ duration, confirmed on ultrasound. She was continued on thyroxine 0.1 mg/day and prednisolone 7.5 mg/day. In addition, she was put on progesterone support for 3 months. She delivered in December 2003, had a mild postpartum hemorrhage and received one blood transfusion. After the present delivery, she lactated normally. She resumed infrequent cycles after the lactation amenorrhea. In 2007, incidentally she was again found to have pregnancy of 20 weeks while going for a routine ultrasound; she delivered after a cesarean section and again lactated normally. She continues to have normal lactation at present. She was recently evaluated to test for PRL function again. Metoclopramide test revealed normal stimulable PRL [Table 1]. Magnetic resonance imaging (MRI) of pituitary revealed evidence of empty sella [Figure 1].
Table 1.
Hormonal parameters before and after lactotroph recovery
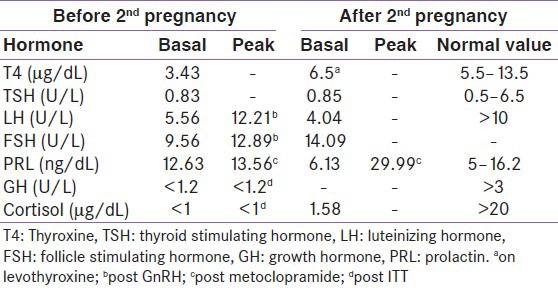
Figure 1.
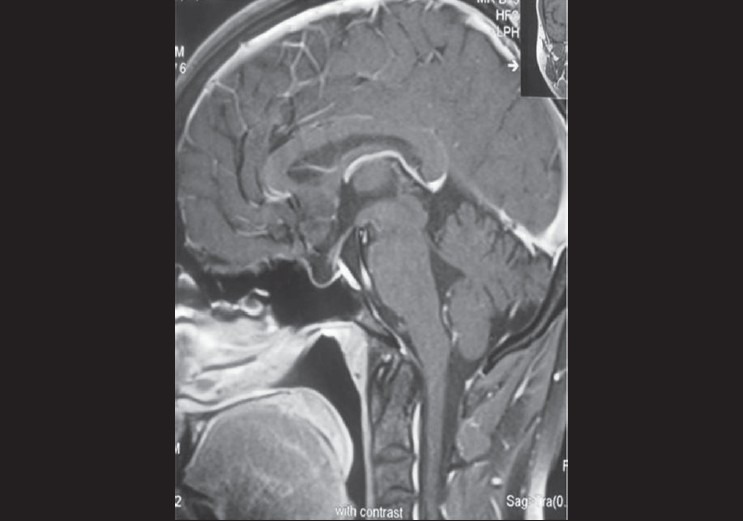
MRI pituitary sagittal view showing pituitary fossa filled with cerebrospinal fluid and stalk touching the base of pituitary floor; features suggestive of empty sella
DYNAMIC TESTS AND METHODS OF HORMONE ASSAYS
Insulin tolerance test was done in fasting state by injecting 0.1U/Kg of regular insulin intravenously. Blood sample was taken for estimation of glucose, GH, cortisol and PRL at 0, 30, 60, 90 and 120 minutes.[7] Metoclopramide test was done to test for PRL reserve. Metoclopramide 10 mg was given intravenous; blood samples for PRL were collected at 0, 30, 60 and 120 minutes after.[8] GnRH test was done to assess the pituitary gonadotroph reserve. GnRH 100 μg was given intravenous and blood samples for luteinizing hormone (LH) and follicle stimulating hormone (FSH) were collected at 30, 60, 90, and 120 minutes after.[9] Serum concentration of thyroxine (T4), thyroid stimulating hormone (TSH), LH, FSH, PRL and GH were measured by immuno-radiometric assay using commercially available kits (Siemens Medical Solutions, Los Angeles, CA 90045-6900, USA); serum cortisol was measured by radio immunoassay using commercially available kits (Diasorin, Stillwater, Minnesota 55082-0285, USA). An informed written consent was obtained from the woman for possible publication of the case.
DISCUSSION
We are presenting the long-term follow-up of a woman who developed SS at the age of 25 years, evidenced by severe postpartum hemorrhage, lactation failure and secondary amenorrhea. Investigations revealed evidence of secondary hypothyroidism, GH, PRL and cortisol deficiency and empty sella on MRI. This woman conceived twice spontaneously. After the second and third delivery, she continued to lactate normally. Results of the dynamic tests after the second delivery confirmed normalization of PRL response. SS is development of partial or complete hypopituitarism following delivery. The disease follows severe postpartum hemorrhage.[1,4] The disease is very infrequently reported from the developed countries because of good obstetric care available to most of the people.[10,11] In developing nations like India, it continues to be a common cause of adult hypopituitarism.[2] Classical as well as some “non-endocrine” features in these women have been reported in areas where the disorder is common.[12,13,14] A significant number of these women present with anemia and other cytopenias, which respond to hormone replacement.[15,16] The two important hormone lines universally lost in these women include lactotroph and somatotroph, because of their location in the lower and lateral parts of pituitary and subsequent susceptibility to infarction.[4] Among anterior pituitary cells, gonadotroph and corticotroph cells are most frequently spared, although uncommonly.[5] Lactotroph failure is considered to be cardinal manifestation of SS, although lactation failure could be because of other disorders and, rarely, hyperprolactinemia may be associated with SS.[8,17] In the present case after the first delivery, she failed to lactate and was documented to have lactotroph failure in addition to somatotroph, corticotroph and thyrotroph failure. She then conceived twice and lactated normally after the second delivery. On subsequent evaluation, she was found to have normal lactotroph function, confirmed by normal response of PRL to metoclopramide test. We believe that possibly insufficient number of lactotrophs was left, causing lactation failure after the first delivery. During subsequent pregnancy, hyperplasia of residual though insufficient lactotrophs could result in recovery of lactotroph function and subsequent normal lactation. Although there have been some rare reports of normal lactation in women with SS even with documented lactotroph failure,[18] in the present case, normal lactation after the second delivery was associated with normal prolactin dynamics. In normal human pituitary, lactotrophs comprise about 15–30% of the total number of cells. During pregnancy there is considerable lactotroph hyperplasia, presumably due to stimulatory effect of estrogen and progesterone. This stimulatory effect also holds true for prolactinomas where there is significant pregnancy-induced tumor enlargement. The reverse hemolytic plaque assay reveals that in normal pituitary cells secreting both GH and PRL, about one-third secrete GH alone, one-third secrete PRL alone and one-third secrete both.[19] Estradiol treatment causes some somatotroph cells to secrete PRL also, i.e., they are converted from somatotroph to mamotroph cells.[20] It may be hypothesized that some of the cells secreting GH and PRL must be left after the first delivery and the stimulatory effect of estrogen and progesterone in pregnancy and the ability of cell population to shift between GH and PRL may be responsible for recovery of PRL function.[20] It is also known that estrogen and progesterone produced from the placenta stimulate PRL synthesis. This is because of stimulation of lactotroph DNA synthesis and mRNA levels.[21,22] Whether in the present case pregnancy resulted in recovery of lactotroph function because of the above mechanisms can only be postulated. There are no reports of recovery of lactotroph function in the literature in women with SS. This could be because the disease is no longer seen in the western world and long-term follow-up is required to suspect such a phenomenon. In the present case, such a phenomenon was thought of 15 years after she initially developed SS.
In summary, long-term follow-up of a woman with SS is presented in whom lactotroph recovery occurred after spontaneous pregnancy following an initial PRL deficiency.
ACKNOWLEDGMENT
The authors would like to thank Professor H. Fahrettin Kelestimur, Professor, Department of Endocrinology, Erciyes University Medical School, Kayseri, Turkey, for his valuable suggestions on the manuscript.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Sheehan HL. Postpartum necrosis of the anterior pituitary. J Pathol Bact. 1937;45:189–214. [Google Scholar]
- 2.Zargar AH, Singh B, Laway BA, Masoodi SR, Wani AI, Bashir MI, et al. Epidemiological aspects of postpartum pituitary hypofunction (Sheehan's syndrome) Fertil Steril. 2005;84:523–8. doi: 10.1016/j.fertnstert.2005.02.022. [DOI] [PubMed] [Google Scholar]
- 3.Dokmetas HS, Kilicli F, Korkmaz S, Yonem O. Characteristic features of 20 patients with Sheehan's syndrome. Gynecol Endocrinol. 2006;22:279–83. doi: 10.1080/09513590600630504. [DOI] [PubMed] [Google Scholar]
- 4.Kelestimur F. Sheehan's syndrome. Pituitary. 2003;6:181–8. doi: 10.1023/b:pitu.0000023425.20854.8e. [DOI] [PubMed] [Google Scholar]
- 5.Laway BA, Mir SA, Gojwari T, Shah TR, Zargar AH. Selective preservation of anterior pituitary functions in patients with Sheehan's syndrome. Indian J Endocrinol Metab. 2011;15(Suppl 3):S238–41. doi: 10.4103/2230-8210.84874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shahmanesh M, Ali Z, Pourmand M, Nourmand I. Pituitary function tests in Sheehan's syndrome. Clin Endocrinol (Oxf) 1980;12:303–11. doi: 10.1111/j.1365-2265.1980.tb02714.x. [DOI] [PubMed] [Google Scholar]
- 7.Zargar AH, Masoodi SR, Laway BA, Shah NA. Clinical Spectrum of Sheehan's syndrome. Ann Saudi Med. 1996;16:338–41. doi: 10.5144/0256-4947.1996.338. [DOI] [PubMed] [Google Scholar]
- 8.Zargar AH, Masoodi SR, Laway BA, Shah NA, Salahuddin M. Familial Puerperal alactogenesis - possibility of a genetically transmitted isolated prolactin deficiency. Br J Obstet Gynaecol. 1997;104:629–31. doi: 10.1111/j.1471-0528.1997.tb11548.x. [DOI] [PubMed] [Google Scholar]
- 9.Osher E, Stem N. Protocols for stimulation and suppression tests commonly used in clinical endocrinology. In: Lavin N, editor. Manual of endocrinology and metabolism. 4th ed. London: Lippincott Williams & Wilkins; 2010. pp. 793–816. [Google Scholar]
- 10.Kristjansdottir HL, Bodvarsdottir SP, Sigurjonsdottir HA. Sheehan's syndrome in modern times: A nationwide retrospective study in Iceland. Eur J Endocrinol. 2011;164:349–54. doi: 10.1530/EJE-10-1004. [DOI] [PubMed] [Google Scholar]
- 11.Tessnow AH, Wilson JD. The changing face of Sheehan's syndrome. Am J Med Sci. 2010;340:402–6. doi: 10.1097/MAJ.0b013e3181f8c6df. [DOI] [PubMed] [Google Scholar]
- 12.Laway BA, Mir SA, Dar MI, Zargar AH. Sheehan's syndrome with central diabetes insipidus. Arq Bras Endocrinol Metabol. 2011;55:171–4. doi: 10.1590/S0004-27302011000200010. [DOI] [PubMed] [Google Scholar]
- 13.Laway BA, Ganie MA, Bashir MI, Kotwal SK, Mir SA, Gojwari T. Sheehan's syndrome with hyperprolactinemia. Turk JEM. 2010;14:47–9. [Google Scholar]
- 14.Laway BA, Shah T, Bashir M, Dada A, Zargar AH. Acute onset psychosis following steroid replacement in Sheehan's syndrome. Acta Endocrinologica (Buc) 2010;6:533–8. [Google Scholar]
- 15.Laway BA, Mir SA, Bashir MI, Bhat JR, Samoon J, Zargar AH. Prevalence of hematological abnormalities in patients with Sheehan's syndrome: Response to replacement of glucocorticoids and thyroxine. Pituitary. 2011;14:39–43. doi: 10.1007/s11102-010-0255-2. [DOI] [PubMed] [Google Scholar]
- 16.Laway BA, Bhat JR, Mir SA, Khan RS, Lone MI, Zargar AH. Sheehan's syndrome with pancytopenia—complete recovery after hormone replacement (case series with review) Ann Hematol. 2010;89:305–8. doi: 10.1007/s00277-009-0804-9. [DOI] [PubMed] [Google Scholar]
- 17.Kelestimur F. Hyperprolactinemia in a patient with Sheehan's syndrome. South Med J. 1992;85:1008–10. doi: 10.1097/00007611-199210000-00019. [DOI] [PubMed] [Google Scholar]
- 18.Gei-Guardia O, Soto-Herrera E, Gei-Brealey A, Chen-Ku CH. Sheehan syndrome in Costa Rica: Clinical experience with 60 cases. Endocr Pract. 2011;17:337–44. doi: 10.4158/EP10145.OR. [DOI] [PubMed] [Google Scholar]
- 19.Frawley LS, Boockfor FR, Hoeffler JP. Identification by plaque assays of a pituitary cell type that secretes both growth hormone and prolactin. Endocrinology. 1985;116:734–7. doi: 10.1210/endo-116-2-734. [DOI] [PubMed] [Google Scholar]
- 20.Boockfor FR, Hoeffler JP, Frawley LS. Estradiol induces a shift in cultured cells that release prolactin or growth hormone. Am J Physiol. 1986;250:103–15. doi: 10.1152/ajpendo.1986.250.1.E103. [DOI] [PubMed] [Google Scholar]
- 21.Vician L, Shupnik MA, Gorski J. Effects of estrogen on primary ovine pituitary cell cultures: Stimulation of prolactin secretion, synthesis, and preprolactin messenger ribonucleic acid activity. Endocrinology. 1979;104:736–43. doi: 10.1210/endo-104-3-736. [DOI] [PubMed] [Google Scholar]
- 22.Rakoff JS, Yen SS. Progesterone induced acute release of prolactin in estrogen primed ovariectomized women. J Clin Endocrinol Metab. 1978;47:918–21. doi: 10.1210/jcem-47-4-918. [DOI] [PubMed] [Google Scholar]


