“Which antidiabetic therapy is administered by the ear?”
Inspired by a similar query in Abraham Verghese’ fictional work Cutting for Stone, this question is pivotal to the praxis of diabetology.
“Compassion is the radicalism of our time.”
-Dalai Lama XIV
Just as the diabetes pandemic has widened, so has our response to this chronic condition. Improved understanding of the pathophysiology of the syndrome has led to advances in diagnosis and management. Newer drugs and devices are now available to combat hyperglycemia and related complications. An increasing maturity in planning strategies to achieve desired therapeutic targets is also evident. With all these innovations and inventions, the current atmosphere of enhanced focus on modern therapeutic tools and targets is understandable. However, our focus on newer drugs alone puts us at risk of forgetting traditional clinical wisdom.
Though not always accompanied by statistical power of significant “P” values, the inherent power of traditional wisdom has served preceding generations of physicians (and their patients) fairly well. This is especially true of nonpharmacological management and is particularly relevant for management of diabetes.
THERAPEUTIC PATIENT EDUCATION
One such treatment for diabetes is patient education. This is now termed as therapeutic patient education (TPE), in view of its proven efficacy as a treatment modality. The evidence supporting TPE as an effective diabetes care modality is older than the landmark studies which provided proof of efficacy of pharmacological therapy in type 1 and type 2 diabetes. The Diabetes Control and Complications Trial (DCCT) and United Kingdom Prospective Diabetes Study (UKPDS) reported their results in 1993 and 1998,[1,2] much after evidence regarding the benefits of TPE was published. Equally important for diabetes care, the seminal work by Mazzuca et al.,[3,4] showed that provision of TPE reduces HbA1c levels in persons with type 2 diabetes. Today, there is ample evidence to support the efficacy of TPE as an essential part of diabetes care.
While TPE can be administered through visual aids and written literature, the predominant method of TPE “administration” is by the ear.
Just as guidelines and framework and frameworks are available for appropriate and rational use of drugs, similar guidance has been developed for TPE. Curricula for training in TPE have been developed by International Diabetes Federation. Various organizations run online and contact programs for diabetes educators, who are now recognized as a distinct profession, both within and outside India.
TPE encompasses various strategies, such as face-to-face counseling and group education. These strategies are utilized to convey messages of varying importance, which can be grouped as primary, secondary, or tertiary education. In a more formal manner, TPE is “administered” as formal structured programs, like Diabetes Education and Self Management for Ongoing and Newly Diagnosed (DESMOND) and DAFNE in the United Kingdom. A patient-centered approach, tempered by awareness of available human and physical resources, helps decide which TPE approach is suitable for a particular clinical setting. The utility of these interventions can be measured by validated instruments (knowledge questionnaires) as well as by improvement in biological (HbA1c) and quantity of life parameters. In all these aspects, TPE is similar to the antidiabetic drugs that we use today.
WORDS OF COMFORT
It may seem a little surreal to write about “words of comfort” to readers of a journal, who (like us, the authors ourselves), are used to celebrating exciting pathophysiological mechanisms and excellently conducted randomized controlled trials. Yet, given the paucity of endocrinologists, when juxtaposed with the sheer magnitude of the diabetes pandemic-it is likely that busy specialists sometimes forget or even deny the power of a compassionate word. This is yet another important antidiabetic therapy, which can be administered by the ear. These are “words of comfort.” Simple, straightforward words, spoken in an empathic, understanding manner, delivered in a friendly, relaxed environment, these messages of reassurance do much to calm the person with diabetes and her or his family. In situations where anxiety is a predominant cause or comorbid condition of uncontrolled hyperglycemia, words of comfort have a major role to play.
The term “words of comfort,” though commonplace in lay and religious literature, is uncommon in medical research. Even when encountered, it is often placed in the context of good nursing care or optimal terminal care.[5,6,7] This concept, however, is too important to be left to just the terminal part of life, where its importance stems out of TINA (there is no alternative). Rather, it must be positioned strategically in chronic care model where its usefulness makes it a deserving candidate of TIVA (there is a viable alternative). Suffice to say, this is too expansive a tool to be practiced by just one group of health care professionals.
“Words of comfort” differ from, yet encompass, psychotherapy. Not all mental health professionals administer words of comfort, yet the necessity to do so is a common refrain by opinion leaders of the specialty.[8] Psychotherapy is a formal means of treatment, administered by professionals in a planned manner, upon request. Words of comfort, on the contrary, are offered spontaneously, informally, from the heart, by the diabetes care provider. One does not need to be specifically asked to deliver this antidiabetic therapy. Neither does one need to inform the person with diabetes, or take an informed consent, prior to sharing comforting words.
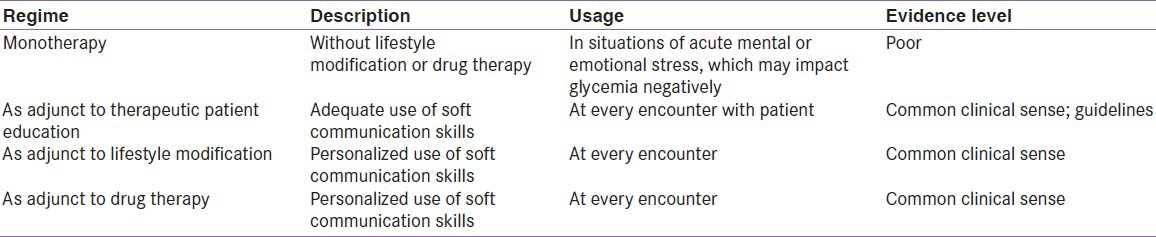
Though words of comfort can, and may, be used as “monotherapy,” they are often used as adjunctive therapy [Table 1]. Words of comfort need to be accompanied by appropriate lifestyle advice and drug therapy. While such words may not be sufficient to control glycemia on their own, they do help in achieving strong patient-provider bonding. This in turn favorably influences adherence to the suggested therapy and ensures concordance in achieving preset targets and goals. Thus, words of comfort can be recognized as a distinct therapeutic intervention in diabetes.
Table 1.
Usage of words of comfort in diabetology
Limitations
There is, however, a flipside to these words of comfort, which come from the heart. Anything that comes from the emotive component of a physician's mind comes at the cost to the physician's mental strength. At all costs, while encouraging the word of comfort-the excess giving away of the word of comfort may well draw upon the limited emotional resources of physicians themselves. This can lead to compassion fatigue[9] to put it simply-do we always talk to the last patient of the day in the same, refreshing, compassionate, relaxed, have-all-the-time-in-the-world-to-listen-to-you tone as the patient we see first in the morning ? This is an important point for physicians to remember, as excessive words of comfort can draw on our own emotional reservoirs-bringing emptiness to other relationships-both within and outside our professional lives. “A fine balance” as they say is essential. Nevertheless, we must learn to energize ourselves to help our patients’ better-at the same time maintain or own equipoise. As endocrinologists helping people with diabetes, this is in the interest of our patients, and ultimately, of our own self-actualization processes.
Words of comfort, if delivered with exclusion of appropriate biological therapy, have the potential to cause harm. Administering words of comfort with oral antidiabetic drugs, to a person with secondary oral hypoglycemic failure, and life-threatening or organ-threatening illness, can not be justified. In such a scenario, words of comfort should be used to encourage acceptance of appropriate insulin therapy, rather than replace it.
COMPARISION AND CONTRAST
Both TPE and “words of comfort” are ideal partners for all other lifestyle modification and drug therapy in diabetes. Both deserve (but unfortunately do not receive) mention in all management algorithms. Excluding either of them from a consultation will negatively impact the result of drug therapeutics. While they do not suffice in isolation, they are a necessary spice for the vast patient centred smorgasbord that diabetes drug therapy is today
It is relatively difficult to learn, and to teach, soft skills, as compared with hard skills. Thus, TPE is a concept that is easily understood by diabetes care providers, but “speaking words of comfort” may be difficult to internalize for some. While TPE is a tool designed to achieve a desired therapeutic outcome, “words of comfort” are the appropriate technique to administer TPE. Methods such as the CARES and I See mnemonic[10,11] have been designed to help diabetes care providers grasp the soft skills required to communicate with their patients. While it may come easily to some, it requires continuous, sustained effort for the majority of us, to practice words of comfort, especially in stressful situations.
Words of comfort should be integrated into undergraduate and postgraduate curriculum, along with motivational training to draw upon the immense emotional resources that every budding physician, or for that matter, any human being is endowed with. Bedside teaching is a perfect platform to demonstrate the soft skills required in communicating with patients in our care.
CONCLUSION
“Which antidiabetic therapy is administered by the ear?”
Both TPE and words of comfort are a perfect answer for the question posed at the beginning for this editorial. An even better answer, perhaps, would be one which merges both therapies in one phrase: Educative words of comfort or comforting TPE.
As we continue to fight the diabetes epidemic, using the best resources available, aiming to achieve optimal health for people with diabetes in our care, we should not lose sight of these two simple, yet effective, therapies, both administered by the ear.
ACKNOWLEDGMENT
This editorial is inspired by the book “Cutting for Stone” by Abraham Verghese.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.The Diabetes Control and Complications Trial Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med. 1993;329:977–86. doi: 10.1056/NEJM199309303291401. [DOI] [PubMed] [Google Scholar]
- 2.UK Prospective Diabetes Study (UKPDS) Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33) Lancet. 1998;352:837–53. [PubMed] [Google Scholar]
- 3.Mazzuca SA, Moorman NH, Wheeler ML, Norton JA, Fineberg NS, Vinicor F, et al. The diabetes education study: A controlled trial of the effects of diabetes patient education. Diabetes Care. 1986;9:1–10. doi: 10.2337/diacare.9.1.1. [DOI] [PubMed] [Google Scholar]
- 4.Mazzuca SA. Does patient education in chronic disease have therapeutic value? J Chronic Dis. 1982;35:521–9. doi: 10.1016/0021-9681(82)90071-6. [DOI] [PubMed] [Google Scholar]
- 5.Humphries A. Starting out - A patient derived great comfort from the spiritual care I provided. Nurs Stand. 2013;28:31. doi: 10.7748/ns2013.10.28.7.31.s35. [DOI] [PubMed] [Google Scholar]
- 6.Possner A. Words of comfort. Acad Med. 2013;88:1201. [Google Scholar]
- 7.Minden P. The importance of words: Suggesting comfort rather than pain. Holist Nurs Pract. 2005;19:267–71. doi: 10.1097/00004650-200511000-00007. [DOI] [PubMed] [Google Scholar]
- 8.Wolf ES. The dutiful physician: The central role of empathy in psychoanalysis, psychotherapy, and medical practice. Hillside J Clin Psychiatry. 1980;2:41–56. [Google Scholar]
- 9.Bhutani J, Bhutani S, Balhara YS, Kalra S. Compassion fatigue and burnout amongst clinicians: A medical exploratory study. Indian J Psychol Med. 2012;34:332–7. doi: 10.4103/0253-7176.108206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kalra S, Kalra B. A good diabetes cousellor ‘cares’: Soft skills in diabetes counseling. Int J Health. 2010;11:1. [Google Scholar]
- 11.Baruah MP, Kalra B, Kalra S. Patient centred approach in endocrinology: From introspection to action. Indian J Endocr Metab. 2012;16:679–81. doi: 10.4103/2230-8210.100629. [DOI] [PMC free article] [PubMed] [Google Scholar]


