Abstract
We present a case of brain abscess due to Gemella haemolysans and Bacteroides species in a 60-year-old-immunocompetent man who underwent dental procedures. The patient completely recovered following intravenous therapy with ampicillin and metronidazole for 6 weeks.
CASE REPORT
A 60-year-old man without a remarkable medical history except for repeated periodontal manipulations was hospitalized for right hemiparesis. One month prior to admission, he had been treated for periodontitis and dental caries in a primary dental clinic. The patient had been well until 10 days before he was hospitalized, when headache and dizziness developed. Three days before hospitalization, the weakness in his right extremities became worse, and he was unable to rise or walk. A computed tomographic (CT) scan of his head revealed a left-sided hypodense parietal lesion (3 by 2.7 cm) with cystic, contrast ring enhancement and perilesional edema exerting a significant mass effect (Fig. 1A). He was referred to our hospital and was admitted to a neurosurgical ward. On admission, he remained afebrile and had not experienced weight loss. Dental examination showed cervical abrasion of his first premolar and the root rest of his second premolar on the right submandibular area. His blood pressure was 140/70 mmHg; and he had a respiration rate of 20 breaths per min, a heart rate of 72 beats per min, and a body temperature of 36.6°C. He was conscious and alert. Neurologic examination revealed no evidence of neck stiffness, Kernig's sign, or Brudzinski's sign. Loss of strength was grade 3/5 in his right leg muscle and 4/5 in his right forearm muscle. The sensation of a light touch was preserved. Laboratory data included a peripheral white blood cell count of 3.46 × 109/liter with 56% segment neutrophils, a hemoglobin level of 13.3 g/dl, a platelet count of 169 × 109/liter, an erythrocyte sedimentation rate of 5 mm/h, and a C-reactive protein level of 0.13 mg/liter. His aspartate aminotransferase, alanine aminotransferase, alkaline phosphatase (ALK), creatinine, blood glucose, plasma sodium, and plasma potassium levels were within normal limits. Signs and symptoms of possible infection were negative.
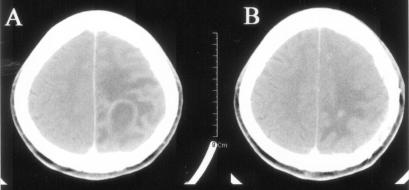
FIG. 1.
CT scans of the head of the case patient before treatment and after 7 weeks. (A) Rim-enhancing lesion with surrounding edema at the left parietal lobe; (B) disappearance of cavity and remarkable decrease of brain edema.
Considering the results of the patient's physical examination and laboratory data, a cystic brain tumor was suspected as the likely diagnosis. He was treated with supportive care, including mannitol and dexamethasone for the control of his brain edema. However, he continued to complain of headache and nausea. On his 10th day in hospital, he complained of severe headache, and his mental state abruptly became worse, with the onset of confusion. An emergency left-sided osteoplastic craniotomy was performed, with a biopsy and aspiration of an encapsulated mass containing white-yellowish pus. The pathological diagnosis was a brain abscess. From that day, he was treated with ceftriaxone (2 g every 12 h intravenously [i.v.]) and metronidazole (500 mg every 6 h i.v.). The day after surgery, the patient's mental state returned to nearly normal, and he no longer complained of headache. The weakness in his right extremities, however, remained similar to that prior to surgery. Echocardiography performed to evaluate the possibility of endocarditis showed neither vegetation nor valvular heart disease.
The pus samples aspirated from the patient's brain abscess were cultured on 5% sheep blood agar at 37°C in air with 5% CO2. Colonies grew slowly and were weakly alpha-hemolytic. Gram stain of the cultures showed gram-variable cocci. The strain was catalase negative, bile-esculin reaction negative, and NO2 reduction positive and failed to grow in broth containing 6.5% NaCl. The pus was also cultured under anaerobic conditions, and gram-negative rods were shown. On the patient's 17th day in hospital, the organism in the pus cultures was identified as Gemella haemolysans, as determined with API 20NE test strips (BioMérieux, Marcy l'Etoile, France), and as Bacteroides species, as determined with ANI test strips (BioMérieux). The characteristics of G. haemolysans on the API 20 NE test strips were leucine aminopeptidase (LAP) negative and ALK positive. The G. haemolysans strain was found by the disk diffusion method to be susceptible to penicillin, ampicillin, amoxicillin-clavulanic acid, cefotaxime, imipenem, and ciprofloxacin but resistant to gentamicin and tobramycin.
The patient was transferred to the Division of Infectious Diseases and was treated with ampicillin (2 g every 4 h i.v.) and metronidazole (500 mg every 6 h i.v.) for 6 weeks. Follow-up CT scan of his head 7 weeks after surgery showed complete resolution of his brain abscess lesion (Fig. 1B). He was discharged in stable condition without any neurologic deficit after68 days in hospital. He is being monitored at the outpatient clinic, and 4 months later, he shows no recurrence of the brain abscess and no recurrence of neurologic signs or symptoms.
Discussion.
Gemella species are facultative, anaerobic, gram-positive cocci which are generally thought to be normal inhabitants of the human oral cavity and the upper respiratory tract (13). These organisms were first isolated in 1917 from the throat, nose, and eyes of patients with measles (15). The members of this genus have been classified as G. haemolysans, G. morbillorum, G. bergeri, G. sanguinis, G. palaticanis, and G. cuniculi on the basis of DNA hybridization and comparative 16S rRNA gene sequencing (11). Infections due to G. haemolysans have been observed infrequently, although the close resemblance of this bacterium to viridans group streptococci may have caused misidentification in the past (11, 12).
It is not easy to differentiate G. haemolysans from viridans group streptococci and Gemella strains not of the species G. haemolysans by the routine identification procedures. G. haemolysans is easily decolorized in the Gram stain and appears to be gram negative, although some cells do not decolorize and appear to be gram positive. The colonies from our patient were gram-variable cocci in pairs or tetrads. The cultures were grown under aerobic conditions and were NO2 reduction positive. The organisms were LAP negative and ALK positive and grouped to G. haemolysans at a similarity of 97.2% on API 20NE test strips, whose sensitivity and specificity for the detection of G. haemolysans have not yet been reported. Viridans group streptococci are gram-positive organisms in chains and are LAP positive. G. morbillorum, which is the most common among the Gemella species, is anaerobic, LAP positive, ALK negative, and NO2 reduction negative (7).
The few infections caused by G. haemolysans reported to date include endocarditis, meningitis, endophthalmitis, pharyngeal abscess, thorax empyema, and spondylodiscitis (2, 3, 5, 8, 10, 12, 14, 16). To our knowledge, this is the first report of a brain abscess caused by G. haemolysans. Gemella species are often a component of dental plaque. In the majority of cases, a dental contamination point has been identified (2, 6, 8). Among the cases of dental origin, G. haemolysans endocarditis was succeeded by bacteremia or cirrhosis (8); and the development of acute postneurosurgical meningitis after a dental procedure has been reported (2). Brain abscesses due to G. morbillorum and Eikenella corrodens, both of which are normal flora of the oral cavity, have been reported after repeated periodontal and dental manipulations (1, 13). Apical venous drainage is connected with the cavernous sinus, and a septic embolus could move by reverse flow, which occurs during yawning and mastication (1, 6). This, in turn, may lead to brain abscesses caused by oral anaerobes present in tooth infections.
Generally, human infections caused by Gemella species are associated with underlying conditions, including an immunocompromised state, cancer, heart disease, sinusitis, or poor dental condition, as well as with previous invasive medical procedures (5, 8, 14). Some cases have been reported in immunocompetent patients and have even caused life-threatening conditions in previously healthy people (12, 13). In our case, the patient was immunocompetent. He had no underlying chronic disease, and his medical history was unremarkable except for previous dental procedures. He presented, however, with a severe neurologic disability expressed as “sudden stroke-like” onset due to a brain abscess (9). At first, his condition was misdiagnosed as a brain tumor, but his rapidly progressing disease led to an emergency craniotomy, and a brain abscess was confirmed from pathological findings and cultures of aspirated specimens.
Brain abscesses are often polymicrobial infections. The predominant anaerobes are anaerobic gram-positive cocci, Bacteroides species, Fusobacterium species, and Prevotella species (4). In our case, the pathogens were G. haemolysans and Bacteroides species, although the latter organism was not further identified. The microbial complexity of this brain abscess suggests that it is necessary to target antimicrobial therapy against polymicrobial pathogens (4, 9). G. haemolysans appears to be highly susceptible to penicillin G and ampicillin (5, 12). Our patient was treated with ampicillin and metronidazole for 6 weeks. He was ultimately cured by means of this combined medical, surgical, and imaging approach. However, his nonspecific medical history and good general condition are likely to have played some role in the favorable outcome of his illness.
In summary, we have described a patient with a history of dental procedures who developed a sudden right hemiparesis due to a brain abscess caused by G. haemolysans and Bacteroides species. G. haemolysans is a rare pathogen, but the prevalence of this infection is underdiagnosed due to difficulties with the positive identification of this organism, which grows slowly and which has characteristics similar to those of viridans group streptococci. Our findings suggest that patients who develop a brain abscess and who have a previous history of periodontal manipulations may be infected with G. haemolysans.
REFERENCES
- 1.Asensi, V., M. Alvarez, J. A. Carton, M. Lago, J. A. Maradona, J. M. Asensi, and J. M. Arribas. 2002. Eikenella corrodens brain abscess after repeated periodontal manipulations cured with imipenem and neurosurgery. Infection 30:240-242. [DOI] [PubMed] [Google Scholar]
- 2.Aspevall, O., E. Hillebrant, B. Linderoth, and M. Rylander. 1991. Meningitis due to Gemella haemolysans after neurosurgical treatment of trigeminal neuralgia. Scand. J. Infect. Dis. 23:503-505. [DOI] [PubMed] [Google Scholar]
- 3.Berger, U. 1985. Prevalence of Gemella haemolysans on the pharyngeal mucosa of man. Med. Microbiol. Immunol. (Berlin) 174:267-274. [DOI] [PubMed] [Google Scholar]
- 4.Brook, I. 1992. Aerobic and anaerobic bacteriology of intracranial abscesses. Pediatr. Neurol. 8:210-214. [DOI] [PubMed] [Google Scholar]
- 5.Buu-Hoi, A., A. Sapoetra, C. Branger, and J. F. Acar. 1982. Antimicrobial susceptibility of Gemella haemolysans isolated from patients with subacute endocarditis. Eur. J. Clin. Microbiol. 1:102-106. [DOI] [PubMed] [Google Scholar]
- 6.Colombo, A. P., A. D. Haffajee, F. E. Dewhirst, B. J. Paster, C. M. Smith, M. A. Cugini, and S. S. Socransky. 1998. Clinical and microbiological features of refractory periodontitis subjects. J. Clin. Periodontol. 25:169-180. [DOI] [PubMed] [Google Scholar]
- 7.Facklam, R., and J. A. Elliott. 1995. Identification, classification, and clinical relavance of catalase-negative, gram-positive cocci, excluding the streptococci and enterococci. Clin. Microbiol. Rev. 8:479-495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fresard, A., V. P. Michel, X. Rueda, G. Aubert, G. Dorche, and F. Lucht. 1993. Gemella haemolysans endocarditis. Clin. Infect. Dis. 16:586-587. [DOI] [PubMed] [Google Scholar]
- 9.Friedlander, R. M., R. G. Gonzalez, N. A. Afridi, and R. Pfannl. 2003. Case 16—2003. A 58-year-old woman with left-sided weakness and a right frontal brain mass. N. Engl. J. Med. 348:2125-2132. [DOI] [PubMed] [Google Scholar]
- 10.Garcia-Lechuz, J. M., O. Cuevas-Lobato, S. Hernamgomez, A. Hermida, J. Guinea, M. Marin, T. Pelaez, and E. Bouza. 2002. Extra-abdominal infections due to Gemella species. Int. J. Infect. Dis. 6:78-82. [DOI] [PubMed] [Google Scholar]
- 11.Kilpper-Balz, R., and K. H. Schleifer. 1988. Transfer of Streptococcus morbillorum to the genus Gemella as Gemella morbillorum, comb. nov. Int. J. Syst. Bacteriol. 38:442-443.
- 12.Martha, B., M. Duong, M. Buisson, M. Grappin, L. Piroth, P. Chavanet, and H. Portier. 2003. Acute Gemella haemolysans spondylodiscitis in an immunocompetent patient. Presse Med. 32:1273-1275. [PubMed] [Google Scholar]
- 13.Messori, A., F. Bartolucci, M. Dini, A. M. Paggi, R. A. Ricciuti, F. Rychlicki, and U. Salvolini. 2002. Gemella morbillorum deep brain abscess successfully treated with combined stereotactic, medical, and imaging approach. Eur. J. Radiol. 44:143-151. [DOI] [PubMed] [Google Scholar]
- 14.Ritterband, D., M. Shah, M. Kresloff, M. Intal, U. Shabto, and J. Seedor. 2002. Gemella haemolysans keratitis and consecutive endophthalmitis. Am. J. Ophthalmol. 133:268-269. [DOI] [PubMed] [Google Scholar]
- 15.Tunnicliff, R. 1917. The cultivation of a micrococcus from blood in pre-eruptive and eruptive stages of measles. JAMA 68:1028-1030. [Google Scholar]
- 16.Veziris, N., C. Fuhrman, C. Chouaid, E. Marque, B. Housset, J. Lange, and I. Monnet. 1999. Empyema of the thorax due to Gemella haemolysans. J. Infect. 39:245-246. [DOI] [PubMed] [Google Scholar]