Abstract
Background
Standard-volume polyethylene glycol (PEG) gut lavage solutions are safe and effective, but they require the consumption of large volumes of fluid. A new lower-volume solution of PEG plus ascorbic acid has been used recently as a preparation for colonoscopy.
Aim
A meta-analysis was performed to compare the performance of low-volume PEG plus ascorbic acid with standard-volume PEG as bowel preparation for colonoscopy.
Study
Electronic and manual searches were performed to identify randomized controlled trials (RCTs) that compared the performance of low-volume PEG plus ascorbic acid with standard-volume PEG as bowel preparation for colonoscopy. After a methodological quality assessment and data extraction, the pooled estimates of bowel preparation efficacy during bowel cleansing, compliance with preparation, willingness to repeat the same preparation, and the side effects were calculated. We calculated pooled estimates of odds ratios (OR) by fixed- and/or random-effects models. We also assessed heterogeneity among studies and the publication bias.
Results
Eleven RCTs were identified for analysis. The pooled OR for preparation efficacy during bowel cleansing and for compliance with preparation for low-volume PEG plus ascorbic acid were 1.08 (95% CI = 0.98–1.28, P = 0.34) and 2.23 (95% CI = 1.67–2.98, P<0.00001), respectively, compared with those for standard-volume PEG. The side effects of vomiting and nausea for low-volume PEG plus ascorbic acid were reduced relative to standard-volume PEG. There was no significant publication bias, according to a funnel plot.
Conclusions
Low-volume PEG plus ascorbic acid gut lavage achieved non-inferior efficacy for bowel cleansing, is more acceptable to patients, and has fewer side effects than standard-volume PEG as a bowel preparation method for colonoscopy.
Introduction
Colorectal cancer, a major cause of cancer-associated morbidity and mortality, is one of the most common cancers [1]. Colonoscopy has become the standard procedure for the diagnosis of colorectal cancer, and widespread colorectal cancer screening and surveillance have resulted in an increased demand for colonoscopy [2], [3]. Screening is crucial for the early detection and removal of premalignant adenomas or localized cancers in order to reduce morbidity and mortality associated with colorectal cancer [4], [5]. A clean colon without solids or residual brown liquid, which could mask a potential lesion, ensures adequate visualization of the colonic mucosa.
Thus, the level of bowel cleansing, to a large extent, determines the success of colonoscopy [6]. Moreover, the bowel preparation process is the single greatest deterrent to subsequent screening [7]. Some studies had reported that poor bowel preparation is associated with lower rates of adenoma detection, incomplete colonoscopy, and greater procedural technical difficulty [8]–[10]. In particular, inadequate bowel preparation may lead to failure to detect lesions in the right colon [11].
The quality of bowel preparation is dependent on patient compliance, the type of bowel preparation, and the timing of ingestion [12]. Furthermore, for adequate compliance in asymptomatic individuals, an effective screening procedure must ensure high sensitivity and prove to be both safe and tolerable [13].
Sodium phosphate solution (SPS) has been used since the 1990s [14]. Despite the advantage of being more acceptable to patients, SPS may cause greater osmotic effects, drawing plasma water into the gastrointestinal tract [15]. Furthermore, because of its potential risk for clinically significant alterations in serum electrolyte levels and hemodynamic stability, SPS is generally not recommended for patients with renal failure, congestive heart failure, uncontrolled hypertension, or ascites [16]–[19].
An alternative preparation of polyethylene glycol (PEG)-based gut lavage, which was introduced in 1980 [20], is an iso-osmotic solution that passes through the bowel, without absorption or secretion. The standard-volume PEG-based solution has been confirmed as safe and efficacious in colonoscopy [21], even in patients with serum electrolyte imbalances, advanced hepatic dysfunction, acute and chronic renal failure, and congestive heart failure [6]. However, in clinical practice, patients experience problems completing the preparation due to the large volume (4 L) and salty taste of the solution, and they tend to drink less than the full amount, resulting in suboptimal efficacy [22].
Recently, combining ascorbic acid, a laxative, with PEG showed potential to reduce the volume necessary for effective colonic cleansing, while possibly improving tolerance. The absorption of ascorbic acid reaches saturation at high doses [23], [24]. Thus, excess ascorbic acid, which cannot be absorbed, remains in the bowel, where it exerts an osmotic effect, acting synergistically with PEG. The addition of ascorbic acid also appears to improve the taste of the PEG preparation. Therefore, by adding ascorbic acid, the standard volume of PEG (4 L) can be halved to 2 L, and the solution tastes better. Furthermore, some randomized controlled trials have confirmed that this low-volume PEG plus ascorbic acid preparation was as effective as the standard-volume PEG preparation and improved patient satisfaction and compliance [25]–[27].
In the present study, we performed a systematic review and meta-analysis to qualitatively and quantitatively summarize previous high-quality RCTs that compared low-volume PEG plus ascorbic acid with standard-volume PEG preparation in terms of bowel preparation quality. We also sought to statistically summarize secondary outcomes, such as compliance with the preparation, the willingness of the patient to repeat the same bowel preparation, and side effects.
Methods
Search Strategy
A computerized search was performed by two independent investigators (W-L.W. and Q-S.X.) in PubMed/Medline, EMBASE, the Cochrane Library, and Google Scholar to identify relevant articles published between 2000 and 2013. We scanned publishers’ databases and conducted manual searches among surgical endoscopy and other interventional techniques, gastrointestinal endoscopy, endoscopy, digestive endoscopy and diseases of the colon and rectum. The abstracts submitted to the Digestive Disease Week and the ACG national meeting, were also manually searched for accuracy and completeness of data retrieval. The literature search was performed using the following terms: 2L or low-volume polyethylene glycol plus ascorbic acid and 4 L or standard-volume polyethylene glycol and colonoscopy.
Selection Criteria
Two reviewers (W-L.W. and Q-S.X.) read the titles and abstracts of original articles that compared the performance of low-volume PEG plus ascorbic acid with standard-volume PEG as the preparation method for colonoscopy to select potentially relevant articles. All of the selected articles were collected and reviewed independently by the same reviewers to determine their eligibility for detailed analysis. The inclusion criteria were: (i) randomized controlled trials (RCTs), (ii) adult patients undergoing elective colonoscopy, and (iii) using 2 L PEG plus ascorbic acid and 4 L PEG preparations. Exclusion criteria were duplicate publications (based on the same primary study) and a lack of categorical data on preparation quality or adherence. Review articles, editorials, letters to the editor, and articles enrolling patients younger than 18 years old were also excluded. Disagreements between the two reviewers regarding study selection were resolved by consensus after a face-to-face discussion. If data were missing from a study, the investigator was contacted to provide the missing data if possible. Each study was evaluated by a Jada score [28] and criteria based on Jüni et al [29] to assess the quality of the study.
Outcomes
The primary outcome was bowel preparation efficacy. This was prespecified as an Ottawa score less than 5, or an excellent or good bowel preparation designation on the Aronchik scale or other non-validated 3-, 4-, or 5-point scales (excellent, good, fair, poor, very poor). As an assessment of bowel preparation tolerability and side effects, a patient’s subjective evaluation of their level of satisfaction and acceptability of the bowel preparation was recorded by studies that administered a periprocedural non-standardized questionnaire to the patient. Data for the secondary outcomes were extracted from the results of these questionnaires. Compliance with bowel preparation was defined as adherence to the bowel preparation prescribed or consumption of at least 75% of the prescribed bowel preparation. The additional secondary outcomes of willingness to repeat the same bowel preparation and side effects, including abdominal cramping/pain, abdominal bloating, vomiting, and nausea, represented affirmative responses to the relevant question from the questionnaires.
Statistical Analysis
A meta-analysis was performed comparing low-volume PEG plus ascorbic acid solution with standard-volume PEG solution as bowel preparation for colonoscopy by calculating pooled estimates of the quality of the bowel preparation, compliance with the preparation, willingness to repeat the same preparation, and side effects using the odds ratio (OR) with fixed- or random-effects models. Publication bias was assessed using funnel plots. Heterogeneity among studies was assessed by calculating the I 2 measure of inconsistency, which was considered significant if I 2>50%. The RevMan 5.2 software from the Cochrane Collaboration was used for the statistical analysis.
Results
Study Characteristics
Figure 1 shows the flow of our search results. In total, 230 studies were identified using electronic searches. Excluding duplicates, 86 abstracts were assessed, of which 19 appeared relevant, and the full studies were assessed. Ultimately, eight investigations were identified for inclusion [27], [30]–[36]. And three RCTs [37]–[39] were included by manual searches between publisher’s database and the abstracts submitted to the Digestive Disease Week and the ACG national meeting (Table 1).
Figure 1. Flowchart of the studies identified for the meta-analysis.
Table 1. Summary of studies comparing treatment of 2L PEG plus ascorbic acid with 4L PEG solution as bowel preparation for colonoscopy.
| Study | Year | Type of study | Blinding | Location | N | Male (%) | Age | Bowel preparation scale | Preparation and dose used | Jadad score |
| Clark L δ | 2007 | RCT | Single | NR | 294 | NR | NR | NR | 2L PEG+ascorbic acid VS 4L PEG | 1 |
| Ell, C. | 2008 | RCT | Single | German | 308 | 48.7 | 58.8±15.4ξ | Non-validated 5-point scale | 2L PEG+ascorbic acid VS 4L PEG | 3 |
| Lee BC δ | 2008 | RCT | Single | NR | 56 | 50.0 | 57.9ξ | NR | 2L PEG+ascorbic acid VS 4L PEG | 1 |
| Corporaal, S. | 2010 | RCT | Single | Netherlands | 307 | 48.2 | 20–87ζ | Non-validated 5-point scale | 2L PEG+ascorbic acid VS 4L PEG | 2 |
| Marmo, R | 2010 | RCT | Single | Italy | 433 | 57.5 | 58.3±14.8ξ | Inverted Ottawa scale | 2L PEG+ascorbic acid VS 4L PEG | 3 |
| González-Méndez Y δ | 2011 | RCT | Single | Spain | 681 | NR | NR | Non-validated 5-point scale | 2L PEG+ascorbic acid+Bisacodyl VS 4L PEG+Bisacodyl | 1 |
| Pontone, S. | 2011 | RCT | Single | Italy | 142 | 52.7 | 20–84ζ | Aronchick scale | 2L PEG+ascorbic acid VS 4L PEG+simethicone | 3 |
| Jansen, Sita V | 2011 | RCT | Single | Netherlands | 370 | 41.9 | 18–92ζ | Non-validated 3-point scale | 2L PEG+ascorbic acid VS 4L PEG | 2 |
| Valiante, F. | 2012 | RCT | Single | Italy | 332 | 53 | 36–85ζ | Aronchick Scale | 2L PEG+ascorbic acid VS 4L PEG | 3 |
| Gentile, M. | 2013 | RCT | Single | Italy | 120 | 52.5 | 20–87ζ | Aronchick scale | 2L PEG+ascorbic acid VS 4L PEG+simethicone | 3 |
| Ponchon, Thierry | 2013 | RCT | Single | France | 400 | 53 | 55.5±12.3ξ | Harefield Cleansing scale | 2L PEG+ascorbic acid VS 4L PEG | 2 |
The reference marked by symbol of δ presented in abstract form; ξ values represent mean±standard difference, ζ values represent range of age. PEG, polyethylene.
glycol; RCT, randomized controlled trial; NR, not report.
Table 1 summarizes the characteristics of the eleven studies involving 3431 patients. Regarding bowel preparation scales, non-validated 5-point scales were used in three studies [27], [29], [39], the Aronchick scale in four [31], [33]–[35], the Ottawa scale in one [30], and a non-validated 3-point scale in the final study [32]. Two [31], [34] of the eleven studies compared low-volume PEG plus ascorbic acid with standard-volume PEG plus simethicone as bowel preparations for colonoscopy.
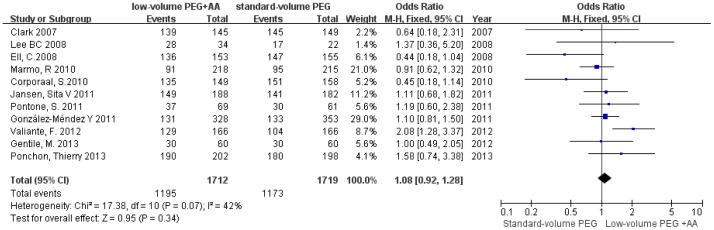
Primary Outcome: Bowel Preparation Efficacy
The forest plot in Figure 2 shows the results of bowel preparation efficacy for the individual studies and for the aggregated studies. Six of the eleven studies reported that low-volume PEG plus ascorbic acid had a higher proportion of patients with excellent or good bowel preparations compared with that of standard-volume PEG. The two studies comparing low-volume PEG plus ascorbic acid with standard-volume PEG plus simethicone showed the same outcome. However, three of the eleven studies found the opposite result. The summary statistic for comparison of low-volume PEG plus ascorbic acid with standard-volume PEG in the eleven studies was an OR of 1.08 (95% CI = 0.92–1.28, P = 0.34, I 2 = 42%), showing no statistically significant difference, indicating that low-volume PEG plus ascorbic acid solution achieved equal bowel preparation efficacy compared with standard-volume PEG.
Figure 2. Forest plot showing equal bowel preparation efficacy of low-volume PEG plus ascorbic acid and standard-volume PEG as bowel preparations for colonoscopy.
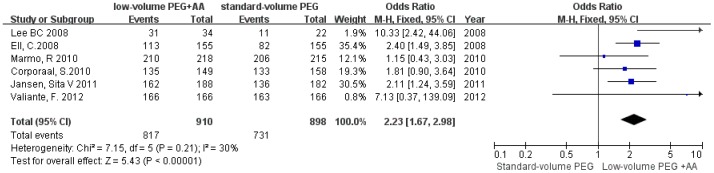
Secondary Outcomes
Six [27], [29], [30], [32], [33], [38] of the eleven studies reported compliance with the preparation, and the pooled OR of compliance with preparation for low-volume PEG plus ascorbic acid was 2.23 (95% CI = 1.67–2.98, P<0.00001, I 2 = 30%), compared with standard-volume PEG (Fig. 3), suggesting that low-volume PEG plus ascorbic acid had significantly better compliance than did standard-volume PEG, without heterogeneity.
Figure 3. Forest plot depicting better compliance with low-volume PEG plus ascorbic acid than with standard-volume PEG as bowel preparations for colonoscopy.
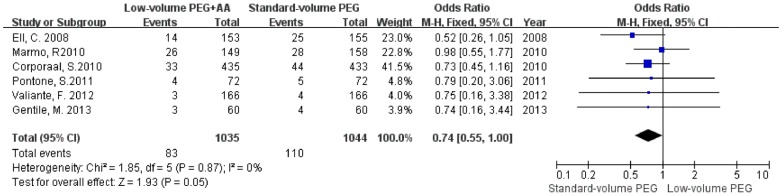
The pooled OR of overall adverse events, willingness to repeat the same bowel preparation, abdominal cramping/pain, abdominal bloating, vomiting, and nausea were 0.73 (95% CI = 0.53–1, P = 0.05, I 2 = 0%), 0.82 (95% CI = 0.56–1.19, P = 0.29, I 2 = 0%), 1.10 (95% CI = 0.83–1.45, P = 0.52, I 2 = 0%), 1.00 (95% CI = 0.73–1.38, P = 0.98, I 2 = 0%), 0.74 (95% CI = 0.55–1.00, P = 0.05, I 2 = 0%), and 0.80 (95% CI = 0.65–0.99, P = 0.04, I 2 = 33%), compared with standard-volume PEG, respectively (Table 2). Thus, low-volume PEG plus ascorbic acid showed significantly fewer overall adverse events and less vomiting and nausea than did standard-volume PEG (Fig. 4–6).
Table 2. Secondary outcomes of low-volume PEG plus ascorbic acid VS standard-volume PEG.
| Outcomes | Studies n | Patients N | Pooled OR | 95%CI | P | I2 |
| Overall adverse events | 3 | 760 | 0.73 | 0.53–1.00 | 0.05 | 0% |
| Willingness to repeat | 3 | 571 | 0.82 | 0.56–1.19 | 0.29 | 0% |
| Abdominal cramping/pain | 7 | 2449 | 1.10 | 0.83–1.45 | 0.52 | 0% |
| Abdominal bloating | 3 | 1483 | 1.00 | 0.73–1.38 | 0.98 | 0% |
| Vomiting | 6 | 2079 | 0.74 | 0.55–1.00 | 0.05 | 0% |
| Nausea | 6 | 2079 | 0.80 | 0.65–0.99 | 0.04 | 33% |
PEG, polyethylene glycol; OR, odds ratios.
Figure 4. Forest plot revealing fewer overall adverse events with low-volume PEG plus ascorbic acid than with standard-volume PEG as bowel preparations for colonoscopy.
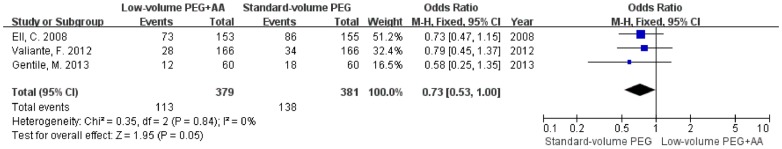
Figure 6. Forest plot showing less nausea with low-volume PEG plus ascorbic acid than with standard-volume PEG as bowel preparations for colonoscopy.
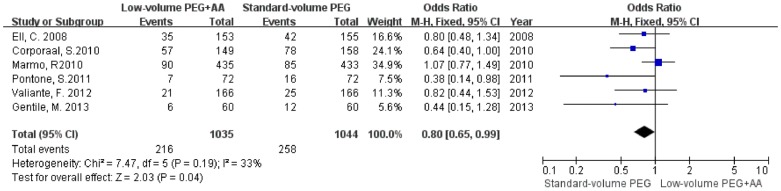
Figure 5. Forest plot showing less vomiting with low-volume PEG plus ascorbic acid than with standard-volume PEG as bowel preparations for colonoscopy.
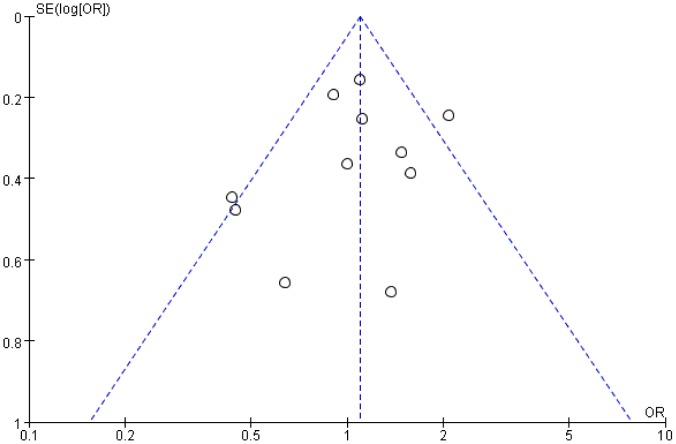
There was no significant publication bias detected for the primary outcome of excellent or good bowel preparation efficacy, as assessed using a funnel plot (Fig. 7).
Figure 7. Funnel plot showing no significant publication bias for the primary outcome.
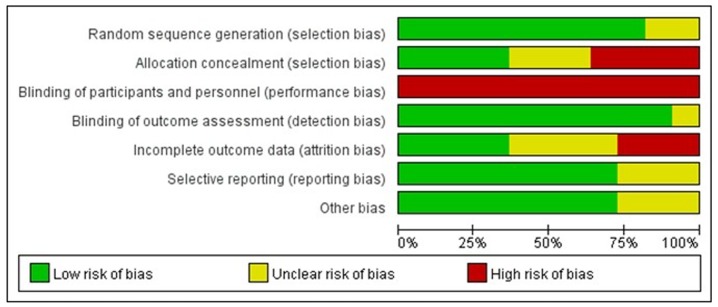
And the risk of bias across all included studies was assessed by using the Cochrane Collaboration’s tool (Fig. 8).
Figure 8. Risk of bias grapy: review author’s judgements about each risk of bias item presented as percentages across all included studies.
Discussion
Sodium phosphate (SP) has similar bowel preparation efficacy to and better tolerability than that of PEG [40]. However, SP has been associated with renal dysfunction and severe disturbances in electrolyte balance [41]–[44]. In addition, a consensus statement recommends that for children, the elderly, and those with renal insufficiency, bowel preparation should be restricted to PEG-based solutions [45]. Thus, standard-volume (4 L) PEG has been regarded as the gold standard for bowel preparation [46]. However, a difficulty of standard-volume PEG is that many patients are unable or unwilling to consume a 4-L preparation [47], [48].
Because the ideal bowel cleanser is effective, safe for all patient groups, and acceptable to patients, the combined use of low-volume (2 L) PEG and ascorbic acid was recently introduced into clinical practice. However, several investigators have argued that low-volume PEG provides inadequate cleansing of the upper colon and significantly worse bowel preparation than either standard-volume PEG or SP [49]–[51]. Recently, Godfrey [52] reported that there was no significant difference between the two bowel lavage solutions.
Compared to Godfrey’s study, in the present study, we included 2 more RCTs and confirmed by meta-analysis that low-volume PEG plus ascorbic acid solution achieved the same bowel preparation efficacy as did standard-volume PEG (OR = 1.08, P = 0.34, I 2 = 42%). The two studies comparing low-volume PEG plus ascorbic acid with standard-volume PEG plus simethicone also reported similar bowel preparation quality. This non-inferior efficacy in bowel cleansing benefited substantially from the synergistic osmotic effect achieved with low-volume PEG [23], [24].
Several factors may contribute to heterogeneity among trials. First, variation in timing of bowel preparation may affect preparation quality. The time at which the bowel preparation was started was not uniform among the trials, ranging from 12–48 h before the scheduled procedure. Second, variation in the dosage schedule may also impact bowel preparation efficacy. The dosage schedule included a non-split-dosage schedule, which involved consuming the entire dose the evening prior to the day of the planned colonoscopy, and a split-dosage schedule, which involved drinking half the dose the afternoon prior and the other half the morning of the the procedure. Third, variation in dietary instructions prior to and during the preparation may have contributed to the heterogeneity. Among the trials included, the dietary instructions were not uniform, ranging from a regular diet to a clear liquid diet for lunch and a clear liquid diet in the evening. Fourth, the diverse use of bowel preparation scales potentially led to heterogeneity. We found that the eight studies used differing preparation scales, such as the Aronchick scale, the Ottawa scale, and non-validated 3-, 4-, and 5-point scales. Finally, the use of different adjuvants probably resulted in heterogeneity. Two studies [32], [35] used ascorbic acid and simethicone, but the other studies used ascorbic acid only.
Colonoscopy is increasingly being used to screen healthy patients (or those with relatively minor symptoms) for bowel cancer [53]. Inability to consume the complete preparation may reduce screening efficacy [49]. Physicians favor preparations associated with best patient compliance to achieve optimal results. Patients favor preparations that are low in volume, palatable, and in easy-to-complete regimens [45]. Given its desirability to physicians and patients, a new low-volume preparation has been developed using ascorbic acid added to a 2-L PEG solution. Godfrey’s study [52] presented a very valuable data on satisfactory bowel preparation of the two bowel lavage solution, however, it was a pity for no investigation of compliance with the two bowel lavage solutions. The present study confirmed that low-volume PEG plus ascorbic acid has significantly better compliance than standard-volume PEG without heterogeneity (OR = 2.23, P<0.00001, I 2 = 30%). The individual studies [27], [29], [30], [32], [33] included in the analysis consistently reported that a larger proportion of patients in the low-volume preparation group consumed at least 75% of the prescribed bowel preparation than did patients enrolled in the standard-volume preparation group. The better compliance may result from the consumption of a smaller volume of liquid and the more palatable ascorbic acid. Better compliance, combined with the laxative effect of ascorbic acid, may account for the similar bowel preparation efficacies between the lower- and standard-volume preparations. The low-volume preparation was especially applicable to outpatients who conducted their intake independently.
In the present study, we also compared overall adverse events, abdominal cramping/pain and bloating, vomiting, and nausea between the low-volume PEG plus ascorbic acid and the standard-volume PEG groups. We found that there was no significant difference in abdominal cramping/pain or bloating between the groups. However, we did see that the low-volume group had significantly fewer overall adverse events and less vomiting and nausea than did the standard-volume group. This significant difference may result from the safety of ascorbic acid, even at high doses [54], [55], and the lower volume of PEG, reducing any PEG-based electrolyte or volume alterations [34].
In summary, optimal bowel cleansing should be not only effective but also safe for all patients. With non-inferior bowel preparation efficacy and the advantages of fewer adverse events and better compliance, the low-volume PEG plus ascorbic acid solution was clearly more applicable to bowel preparation for colonoscopy.
Supporting Information
PRISMA checklist.
(DOC)
Acknowledgments
This manuscript was edited and proofread by Textcheck. A certificate can be obtained from the following link: http://www.textcheck.com/login.
Funding Statement
This work was supported by grants from the National Natural Science Foundation of China (No. 81172315/H1617), the research Special Fund For public welfare industry of health and the translational research of early diagnosis and comprehensive treatment in pancreatic cancer (201202007). The funders had a role in preparation of the manuscript and publication.
References
- 1. Arditi C, Peytremann-Bridevaux I, Burnand B, Eckardt VF, Bytzer P, et al. (2009) Appropriateness of colonoscopy in Europe (EPAGE II). Screening for colorectal cancer. Endoscopy 41: 200–208. [DOI] [PubMed] [Google Scholar]
- 2. Nelson RS, Thorson AG (2009) Colorectal cancer screening. Curr Oncol Rep 11: 482–489. [DOI] [PubMed] [Google Scholar]
- 3. Tsikitis VL, Malireddy K, Green EA, Christensen B, Whelan R, et al. (2009) Postoperative surveillance recommendations for early stage colon cancer based on results from the clinical outcomes of surgical therapy trial. J Clin Oncol 27: 3671–3676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Rex DK, Johnson DA, Anderson JC, Schoenfeld PS, Burke CA, et al. (2009) American College of Gastroenterology guidelines for colorectal cancer screening 2009 [corrected]. Am J Gastroenterol 104: 739–750. [DOI] [PubMed] [Google Scholar]
- 5. Zauber AG, Winawer SJ, O’Brien MJ, Lansdorp-Vogelaar I, van Ballegooijen M, et al. (2012) Colonoscopic polypectomy and long-term prevention of colorectal-cancer deaths. N Engl J Med 366: 687–696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Lichtenstein G (2009) Bowel preparations for colonoscopy: a review. Am J Health Syst Pharm 66: 27–37. [DOI] [PubMed] [Google Scholar]
- 7. Harewood GC, Wiersema MJ, Melton LJ 3rd (2002) A prospective, controlled assessment of factors influencing acceptance of screening colonoscopy. Am J Gastroenterol 97: 3186–3194. [DOI] [PubMed] [Google Scholar]
- 8. Froehlich F, Wietlisbach V, Gonvers JJ, Burnand B, Vader JP (2005) Impact of colonic cleansing on quality and diagnostic yield of colonoscopy: the European Panel of Appropriateness of Gastrointestinal Endoscopy European multicenter study. Gastrointest Endosc 61: 378–384. [DOI] [PubMed] [Google Scholar]
- 9. Chokshi RV, Hovis CE, Hollander T, Early DS, Wang JS (2012) Prevalence of missed adenomas in patients with inadequate bowel preparation on screening colonoscopy. Gastrointest Endosc 75: 1197–1203. [DOI] [PubMed] [Google Scholar]
- 10. Lebwohl B, Kastrinos F, Glick M, Rosenbaum AJ, Wang T, et al. (2011) The impact of suboptimal bowel preparation on adenoma miss rates and the factors associated with early repeat colonoscopy. Gastrointest Endosc 73: 1207–1214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Brenner H, Chang-Claude J, Seiler CM, Rickert A, Hoffmeister M (2011) Protection from colorectal cancer after colonoscopy: a population-based, case-control study. Ann Intern Med 154: 22–30. [DOI] [PubMed] [Google Scholar]
- 12. Halphen M, Heresbach D, Gruss HJ, Belsey J (2013) Validation of the Harefield Cleansing Scale: a tool for the evaluation of bowel cleansing quality in both research and clinical practice. Gastrointest Endosc 78: 121–131. [DOI] [PubMed] [Google Scholar]
- 13. Bitoun A, Ponchon T, Barthet M, Coffin B, Dugue C, et al. (2006) Results of a prospective randomised multicentre controlled trial comparing a new 2-L ascorbic acid plus polyethylene glycol and electrolyte solution vs. sodium phosphate solution in patients undergoing elective colonoscopy. Aliment Pharmacol Ther 24: 1631–1642. [DOI] [PubMed] [Google Scholar]
- 14. Vanner SJ, MacDonald PH, Paterson WG, Prentice RS, Da Costa LR, et al. (1990) A randomized prospective trial comparing oral sodium phosphate with standard polyethylene glycol-based lavage solution (Golytely) in the preparation of patients for colonoscopy. Am J Gastroenterol 85: 422–427. [PubMed] [Google Scholar]
- 15. Hsu CW, Imperiale TF (1998) Meta-analysis and cost comparison of polyethylene glycol lavage versus sodium phosphate for colonoscopy preparation. Gastrointest Endosc 48: 276–282. [DOI] [PubMed] [Google Scholar]
- 16. Pitcher DE, Ford RS, Nelson MT, Dickinson WE (1997) Fatal hypocalcemic, hyperphosphatemic, metabolic acidosis following sequential sodium phosphate-based enema administration. Gastrointest Endosc 46: 266–268. [DOI] [PubMed] [Google Scholar]
- 17. Shaoul R, Wolff R, Seligmann H, Tal Y, Jaffe M (2001) Symptoms of hyperphosphatemia, hypocalcemia, and hypomagnesemia in an adolescent after the oral administration of sodium phosphate in preparation for a colonoscopy. Gastrointest Endosc 53: 650–652. [DOI] [PubMed] [Google Scholar]
- 18. Lieberman DA, Ghormley J, Flora K (1996) Effect of oral sodium phosphate colon preparation on serum electrolytes in patients with normal serum creatinine. Gastrointest Endosc 43: 467–469. [DOI] [PubMed] [Google Scholar]
- 19. Barclay RL, Depew WT, Vanner SJ (2002) Carbohydrate-electrolyte rehydration protects against intravascular volume contraction during colonic cleansing with orally administered sodium phosphate. Gastrointest Endosc 56: 633–638. [DOI] [PubMed] [Google Scholar]
- 20. Davis GR, Santa Ana CA, Morawski SG, Fordtran JS (1980) Development of a lavage solution associated with minimal water and electrolyte absorption or secretion. Gastroenterology 78: 991–995. [PubMed] [Google Scholar]
- 21. Toledo TK, DiPalma JA (2001) Review article: colon cleansing preparation for gastrointestinal procedures. Aliment Pharmacol Ther 15: 605–611. [DOI] [PubMed] [Google Scholar]
- 22. Nyberg C, Hendel J, Nielsen OH (2010) The safety of osmotically acting cathartics in colonic cleansing. Nat Rev Gastroenterol Hepatol 7: 557–564. [DOI] [PubMed] [Google Scholar]
- 23. Wilson JX (2005) Regulation of vitamin C transport. Annu Rev Nutr 25: 105–125. [DOI] [PubMed] [Google Scholar]
- 24. Fujita I, Akagi Y, Hirano J, Nakanishi T, Itoh N, et al. (2000) Distinct mechanisms of transport of ascorbic acid and dehydroascorbic acid in intestinal epithelial cells (IEC-6). Res Commun Mol Pathol Pharmacol 107: 219–231. [PubMed] [Google Scholar]
- 25. Sharma VK, Steinberg EN, Vasudeva R, Howden CW (1997) Randomized, controlled study of pretreatment with magnesium citrate on the quality of colonoscopy preparation with polyethylene glycol electrolyte lavage solution. Gastrointest Endosc 46: 541–543. [DOI] [PubMed] [Google Scholar]
- 26. Sharma VK, Chockalingham SK, Ugheoke EA, Kapur A, Ling PH, et al. (1998) Prospective, randomized, controlled comparison of the use of polyethylene glycol electrolyte lavage solution in four-liter versus two-liter volumes and pretreatment with either magnesium citrate or bisacodyl for colonoscopy preparation. Gastrointest Endosc 47: 167–171. [DOI] [PubMed] [Google Scholar]
- 27. Corporaal S, Kleibeuker JH, Koornstra JJ (2010) Low-volume PEG plus ascorbic acid versus high-volume PEG as bowel preparation for colonoscopy. Scand J Gastroenterol 45: 1380–1386. [DOI] [PubMed] [Google Scholar]
- 28. Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, et al. (1996) Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials 17: 1–12. [DOI] [PubMed] [Google Scholar]
- 29. Kilgore TW, Abdinoor AA, Matteson ML, Puli SR, Marshall JB, et al. (2001) Systematic reviews in health care: Assessing the quality of controlled clinical trials. BMJ 323: 42–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Ell C, Fischbach W, Bronisch HJ, Dertinger S, Layer P, et al. (2008) Randomized trial of low-volume PEG solution versus standard PEG+electrolytes for bowel cleansing before colonoscopy. Am J Gastroenterol 103: 883–893. [DOI] [PubMed] [Google Scholar]
- 31. Marmo R, Rotondano G, Riccio G, Marone A, Bianco MA, et al. (2010) Effective bowel cleansing before colonoscopy: a randomized study of split-dosage versus non-split dosage regimens of high-volume versus low-volume polyethylene glycol solutions. Gastrointest Endosc 72: 313–320. [DOI] [PubMed] [Google Scholar]
- 32. Pontone S, Angelini R, Standoli M, Patrizi G, Culasso F, et al. (2011) Low-volume plus ascorbic acid vs high-volume plus simethicone bowel preparation before colonoscopy. World J Gastroenterol 17: 4689–4695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Jansen SV, Goedhard JG, Winkens B, van Deursen CTBM (2011) Preparation before colonoscopy. European Journal of Gastroenterology & Hepatology 23: 897–902. [DOI] [PubMed] [Google Scholar]
- 34. Valiante F, Pontone S, Hassan C, Bellumat A, De Bona M, et al. (2012) A randomized controlled trial evaluating a new 2-L PEG solution plus ascorbic acid vs 4-L PEG for bowel cleansing prior to colonoscopy. Dig Liver Dis 44: 224–227. [DOI] [PubMed] [Google Scholar]
- 35. Gentile M, De Rosa M, Cestaro G, Forestieri P (2013) 2 L PEG plus ascorbic acid versus 4 L PEG plus simethicon for colonoscopy preparation: a randomized single-blind clinical trial. Surg Laparosc Endosc Percutan Tech 23: 276–280. [DOI] [PubMed] [Google Scholar]
- 36. Ponchon T, Boustière C, Heresbach D, Hagege H, Tarrerias A-L, et al. (2013) A low-volume polyethylene glycol plus ascorbate solution for bowel cleansing prior to colonoscopy: The NORMO randomised clinical trial. Digestive and Liver Disease 45: 820–826. [DOI] [PubMed] [Google Scholar]
- 37. Clark L, Gruss HJ, Kloess HR, Dugue C, Geraint M, et al. (2007) Better efficacy of a new 2 litre bowel cleansing preparation in the ascending colon. Gastrointest Endosc 65: AB262. [Google Scholar]
- 38. Lee BC, Moyes DA, Mcloughlin JC, Lim PL (2008) The efficacy, acceptability and safety of the new 2L polyethylene glycol+electrolytes+ascorbic acid (PEG+E+ASC) VS the 4L polyethylene glycol 3350+ electrolytes (PEG+E) in patients undergoing elective colonoscopies in a UK teaching hospital. Gastrointest Endosc 67: AB290–AB291. [Google Scholar]
- 39. González-Méndez Y, Alarcón-Fernández O, Romero-García R, Adrián-De-Ganzo Z, Alonso-Abreu, et al (2011) Comparison of colon cleansing with two liters of polyethylen glycol-electrolyte: A prospective and randomized study. Gastrointest Endosc 73: AB424. [Google Scholar]
- 40. Belsey J, Epstein O, Heresbach D (2007) Systematic review: oral bowel preparation for colonoscopy. Aliment Pharmacol Ther 25: 373–384. [DOI] [PubMed] [Google Scholar]
- 41. Barkun A, Chiba N, Enns R, Marcon M, Natsheh S, et al. (2006) Commonly used preparations for colonoscopy: efficacy, tolerability, and safety–a Canadian Association of Gastroenterology position paper. Can J Gastroenterol 20: 699–710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Mathus-Vliegen EM, Kemble UM (2006) A prospective randomized blinded comparison of sodium phosphate and polyethylene glycol-electrolyte solution for safe bowel cleansing. Aliment Pharmacol Ther 23: 543–552. [DOI] [PubMed] [Google Scholar]
- 43. Markowitz GS, Stokes MB, Radhakrishnan J, D’Agati VD (2005) Acute phosphate nephropathy following oral sodium phosphate bowel purgative: an underrecognized cause of chronic renal failure. J Am Soc Nephrol 16: 3389–3396. [DOI] [PubMed] [Google Scholar]
- 44. Markowitz GS, Nasr SH, Klein P, Anderson H, Stack JI, et al. (2004) Renal failure due to acute nephrocalcinosis following oral sodium phosphate bowel cleansing. Hum Pathol 35: 675–684. [DOI] [PubMed] [Google Scholar]
- 45. Wexner SD, Beck DE, Baron TH, Fanelli RD, Hyman N, et al. (2006) A consensus document on bowel preparation before colonoscopy: prepared by a task force from the American Society of Colon and Rectal Surgeons (ASCRS), the American Society for Gastrointestinal Endoscopy (ASGE), and the Society of American Gastrointestinal and Endoscopic Surgeons (SAGES). Dis Colon Rectum 49: 792–809. [DOI] [PubMed] [Google Scholar]
- 46. Wexner SD, Beck DE, Baron TH, Fanelli RD, Hyman N, et al. (2006) A consensus document on bowel preparation before colonoscopy: prepared by a task force from the American Society of Colon and Rectal Surgeons (ASCRS), the American Society for Gastrointestinal Endoscopy (ASGE), and the Society of American Gastrointestinal and Endoscopic Surgeons (SAGES). Gastrointest Endosc 63: 894–909. [DOI] [PubMed] [Google Scholar]
- 47. Aronchick CA, Lipshutz WH, Wright SH, Dufrayne F, Bergman G (2000) A novel tableted purgative for colonoscopic preparation: efficacy and safety comparisons with Colyte and Fleet Phospho-Soda. Gastrointest Endosc 52: 346–352. [DOI] [PubMed] [Google Scholar]
- 48. Radaelli F, Meucci G, Imperiali G, Spinzi G, Strocchi E, et al. (2005) High-dose senna compared with conventional PEG-ES lavage as bowel preparation for elective colonoscopy: a prospective, randomized, investigator-blinded trial. Am J Gastroenterol 100: 2674–2680. [DOI] [PubMed] [Google Scholar]
- 49. Di Febo G, Gizzi G, Calo G, Siringo S, Brunetti G (1990) Comparison of a new colon lavage solution (Iso-Giuliani) with a standard preparation for colonoscopy: a randomized study. Endoscopy 22: 214–216. [DOI] [PubMed] [Google Scholar]
- 50. Huppertz-Hauss G, Bretthauer M, Sauar J, Paulsen J, Kjellevold O, et al. (2005) Polyethylene glycol versus sodium phosphate in bowel cleansing for colonoscopy: a randomized trial. Endoscopy 37: 537–541. [DOI] [PubMed] [Google Scholar]
- 51. Young CJ, Simpson RR, King DW, Lubowski DZ (2000) Oral sodium phosphate solution is a superior colonoscopy preparation to polyethylene glycol with bisacodyl. Dis Colon Rectum 43: 1568–1571. [DOI] [PubMed] [Google Scholar]
- 52. Godfrey JD, Clark RE, Choudhary A, Ashrf I, Matteson ML, et al. (2013) Ascorbic acid and low-volume polyethylene glycol for bowel preparation prior to colonoscopy: A meta-analysis. World J Meta-Anal 26: 10–15. [PMC free article] [PubMed] [Google Scholar]
- 53. Bond JH (2006) The case for direct colonoscopy screening for colorectal cancer. Am J Gastroenterol 101: 263–265. [DOI] [PubMed] [Google Scholar]
- 54. Blanchard J, Tozer TN, Rowland M (1997) Pharmacokinetic perspectives on megadoses of ascorbic acid. Am J Clin Nutr 66: 1165–1171. [DOI] [PubMed] [Google Scholar]
- 55. Bendich A, Langseth L (1995) The health effects of vitamin C supplementation: a review. J Am Coll Nutr 14: 124–136. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
PRISMA checklist.
(DOC)