Abstract
Background
The relationship between childhood internalizing problems and early adolescent alcohol use has been infrequently explored and remains unclear.
Methods
We employed growth mixture modeling of internalizing symptoms for a large, population-based sample of UK children (the ALSPAC cohort) to identify trajectories of childhood internalizing symptoms from age 4 through age 11.5. We then examined the relationship between membership in each trajectory and alcohol use in early adolescence (reported at age 13.8).
Results
Overall, children experiencing elevated levels of internalizing symptoms were less likely to use alcohol in early adolescence. This finding held true across all internalizing trajectories; i.e., those exhibiting increasing levels of internalizing symptoms over time, and those whose symptoms desisted over time, were both less likely to use alcohol than their peers who did not exhibit internalizing problems.
Conclusions
We conclude that childhood internalizing symptoms, unlike adolescent symptoms, are negatively associated with early adolescent alcohol experimentation. Additional studies are warranted to follow up on our preliminary evidence that symptoms of phobia and separation anxiety drive this effect.
Keywords: childhood internalizing symptoms, adolescent alcohol use, growth mixture, modeling, ALSPAC
Introduction
Alcohol misuse and internalizing problems are common, contribute substantially to the global mental health burden, and frequently co-occur. Alcohol experimentation typically begins during adolescence, with over 20% of US students reporting having had a drink by age 13 (Centers for Disease Control and Prevention, 2012); “early-onset drinking” is defined differently across studies, ranging from age 12 and earlier to age 15 and earlier (Donovan and Molina, 2011). Internalizing problems can begin in early childhood, with 10–15% of children or early adolescents experiencing some symptoms of depression (Smucker et al., 1986), though the prevalence of clinical depression in children is low (<5%, Birmaher et al., 1996; Fleming et al., 1989). Anxiety disorders are relatively common, with a prevalence approaching 10–20% in very young children, older children, and adolescents (Costello, 1989; Pine, 1997). Despite abundant research on both childhood internalizing symptoms and adolescent alcohol use, questions remain about their relationship. Does the unfolding of internalizing symptoms during childhood have an impact on adolescent alcohol use, or are the two unrelated?
Many studies have explored the relationship between internalizing symptoms and alcohol use during adolescence and into adulthood, with most reporting a positive association (Goodwin et al., 2004; Marmorstein, 2009; Marmorstein, 2010; McCarty et al., 2012; Needham, 2007). However, there are relatively fewer reports on the association between childhood internalizing symptoms and adolescent alcohol outcomes. Some evidence from prospective studies suggests that individuals who experience internalizing symptoms during childhood and/or early adolescence are at an increased risk of early alcohol use (Crum et al., 2008a; Kaplow et al., 2001; King et al., 2004; Marmorstein et al., 2010b). However, others have reported a negative association between childhood internalizing symptoms and alcohol use (Maggs et al., 2008), or no association (Englund et al., 2008). Relationships could differ across the sexes, and across alcohol outcomes (Crum et al., 2008b). Thus, the predictive value of childhood internalizing symptoms with respect to alcohol use in early adolescence is not well established. The relative paucity of studies on the relation between these phenotypes, particularly in large representative samples, impedes our understanding of factors contributing to early alcohol use.
Aside from the basic question of whether childhood internalizing symptoms are positively or negatively associated with adolescent alcohol use, the question remains whether the course of such symptoms is relevant to alcohol outcomes. Failure to account for symptom course could contribute to conflicting findings. That variation exists in the progression of internalizing symptoms has been well established (Fanti and Henrich, 2010; Feng et al., 2008; Marmorstein et al., 2010a; Reinke et al., 2012; Wanner et al., 2012), with some studies reporting courses related to severity (e.g, Fanti and Henrich, 2010), and others finding evidence of within-class change (e.g., high to low symptoms over time; Feng et al., 2008). Notably, the sample sizes in many of these studies are limited, and in some cases selected (rather than representative) samples were used. Still, few studies have derived trajectories of internalizing symptoms and explored their relationships with alcohol outcomes, and the samples’ age ranges differ across studies and from the age range in the current study. In a study of adolescents and young adults, Marmorstein (2009) examined trajectories of high vs. low depressive symptoms and found that the high class was more likely to have alcohol problems. In a sample of girls, classes exhibiting worse depressive symptoms were more strongly associated with alcohol initiation than other classes; no association was observed for trajectories of generalized anxiety symptoms; and courses of social anxiety symptoms exhibited conflicting associations with alcohol use onset (Marmorstein et al., 2010a). In boys, membership in the “high” class of generalized anxiety symptoms conferred higher risk of alcohol use initiation (Marmorstein et al., 2010b); the “high” class of social anxiety symptoms also exhibited a trend toward higher risk. Fleming and colleagues (2008) found that changes in adolescent depressive symptoms were modestly positively associated with changes in alcohol use, though that study did not identify individual classes of depressive symptoms. Not all studies support a relationship between growth in depressive symptoms and alcohol use (Hooshmand et al., 2012).
Adolescent drinking habits can lay the foundation for future problems with alcohol (Chartier et al., 2010; Englund et al., 2008). Therefore, it is critical for prevention and intervention efforts that the ability to identify individuals at risk for later alcohol problems be improved. Children who experience internalizing symptoms could vary in their risk of later alcohol use or problems as a function of the course of their symptoms, in which case education, prevention, and intervention efforts could be tailored accordingly.
In the current study, we aim to clarify the relationship between trajectories of childhood internalizing symptoms with early adolescent alcohol use, using a large, population-based sample of children in the UK. The goals of our analyses are to identify distinct trajectories of childhood internalizing symptoms in this sample, and to determine whether these trajectories are differentially associated with risk of alcohol use early in adolescence, when individuals typically begin experimenting with alcohol. We examine whether the data provide support for the hypothesis that the relationship between childhood internalizing symptoms and adolescent alcohol use varies as a function of symptom course. For example, are individuals whose internalizing symptoms have not yet remitted by late childhood less likely to experiment with alcohol at 13.8 than their peers? The null hypothesis is that individuals who experience different courses of internalizing symptoms as children do not differ from peers on adolescent drinking outcomes.
Methods
Sample
The Avon Longitudinal Study of Parents and Children (ALSPAC) cohort has been described previously (Boyd et al., 2012; Fraser et al., 2012). Briefly, pregnant women in the Avon area of Southwest England with expected delivery dates between April 1, 1991 and December 31, 1992 were eligible to enroll in the study. The initial number of pregnancies enrolled, and for which the mother returned at least one questionnaire or attended a “Children in Focus” clinic, was 14,541. Additional participants have been added as recruitment efforts continue. ALSPAC parents and children have been followed longitudinally, with mothers, mothers’ partners, and children providing data through postal questionnaires and clinic visits. Ethical approval for the study was obtained from the ALSPAC Law and Ethics committee and the Local Research Ethics Committees. Additional details are available at www.alspac.bristol.ac.uk.
The current analyses were limited to the portion of the sample for which partial or complete data were available for maternal reports of offspring internalizing symptoms using the Strengths and Difficulties Questionnaire (SDQ, Goodman et al., 2000); additional details below). The resulting sample size is N=11,157 (51.4% male).
Measures
Childhood internalizing symptoms
Child internalizing symptoms were assessed using maternal reports on the SDQ, a questionnaire designed for children and adolescents. The “emotional symptoms” scale consists of 5 items aimed at measuring symptoms of depression, anxiety, phobia, separation anxiety, and somatic complaints, using questions such as, “[has] many worries, or often seems worried” and “nervous or clingy in new situations, easily loses confidence.” A comparison of the SDQ and the Child Behavior Checklist (Achenbach, 1991) suggested that the instruments are equally valid and successful at identifying psychological problems (Goodman and Scott, 1999). The current report utilizes maternal reports of child behavior at average ages 47 months (3.9 years), 81 months (6.8 years), 97 months (8.1 years), 114 months (9.5 years), and 140 months (11.7 years). Response options are “not true”, “somewhat true”, and “certainly true”, which were coded for the current analyses as 0, 1, and 2, respectively, for each of the 5 items. These were summed together at each age. Where 3 or more items were missing, the sum score for that age was not calculated; if 1 or 2 items were missing, the available items were pro-rated. Skewness for sum scores ranged from 1.24–1.48; kurtosis ranged from 1.30–2.29; Cronbach’s alpha ranged from 0.75–0.82.
Adolescent alcohol use
At 13 years 10 months of age (13.8 years; SD=2.5 months), adolescents participated in clinic visits that involved interviews with researchers, where they were asked questions about their current and past alcohol use. Of the available questions, four separate alcohol-related outcomes were utilized in the current analyses: 1) having had a full drink in the past 6 months; 2) having drunk alcohol without parental permission in the past 6 months; 3) maximum drinks in a 24-hour period (which was dichotomized such that those who reported having 3 or more drinks were classified as “binge” drinkers, as in Melotti et al. (2011); and 4) number of whole drinks consumed in the past 6 months. These outcomes were explored individually rather than combined into a composite risk score or factor score because previous reports have suggested that the relationships observed between internalizing symptoms and alcohol use/problems might differ as a function of the outcome of the outcome being examined (Crum et al., 2008b; Marmorstein et al., 2010b). By considering each alcohol-related outcome individually, we avoid obscuring outcome-specific relationships.
Maternal depression
At 12 weeks gestation, mothers’ questionnaires included an item asking whether they had ever had severe depression. Responses endorsing current or past depression were scored as 1; a response of “no, never” was scored 0. This binary variable was included as a covariate in secondary analyses in order to control for the potential effects of rater bias (Fergusson et al., 1993; Najman et al., 2001).
Family income
When the children were 33 months of age (2.8 years), mothers were asked to report their disposable family income. Responses were coded into quintiles, accounting for family size and composition and estimated housing benefits. This variable was used as a covariate in secondary analyses due to previously reported associations between income and alcohol outcomes in this sample (Melotti et al., 2011).
Item level analyses
As described previously, the emotional symptoms scale of the SDQ consists of 5 items, relating to different manifestations of internalizing. For each item, we created a binary variable that was coded 0 if an individual’s mother had always reported that her child had never exhibited that symptom/behavior, or 1 if the child had ever exhibited that symptom/behavior (e.g., “somewhat true” or “certainly true” in at least one assessment). We then examined whether these binary variables were associated with alcohol use at age 13.8, in the context of a single-stage model including all 5 item-level binary variables, along with sex, maternal depression, and income as covariates.
Statistical Analyses
Mixture modeling
Growth mixture modeling was conducted in Mplus 5.21 (Muthen and Muthen, 1998–2007), using the five internalizing sum scores described above as manifest variables, and estimating an intercept (I), slope (S), and non-linear (quadratic, Q) growth term for each class. Growth mixture models were conducted with the sexes combined, as previous studies have found that sex differences in internalizing typically do not emerge until after the onset of puberty (e.g., Angold et al., 1998; Ge et al., 1994). However, in an effort to account for potential sex differences, sex was used as a covariate in subsequent analyses. As the goal of the mixture modeling was to characterize early internalizing problems, the last age for which data were included is 11.5 years, at which point the majority of the sample was prepubescent (Joinson et al., 2011). Fit and feasibility were assessed using Akaike’s Information Criterion (AIC), Bayesian Information Criterion (BIC), entropy, the Lo-Mendell-Rubin adjusted likelihood ratio test, and general interpretability (see Results). Due to difficulties with model convergence in conditional models, trajectory identification and subsequent analyses were conducted separately, as opposed to in a single stage analysis, within Mplus.
Modeling associations between internalizing classes and alcohol outcomes
After determining the most appropriate number of classes (see Results), we explored the predictive relationship between class membership and alcohol use outcomes via a series of contrast-coded predictors wherein an individual alcohol outcome was regressed onto the contrast and the covariates described above (maternal depression, income, and sex). As preliminary analyses indicated that some covariates were correlated (e.g., maternal depression and income), we employed a modeling framework that allowed for correlations among predictive variables. In each model, each class with elevated levels of internalizing symptoms was compared to the class with the lowest average internalizing score over time (see Results).
Attrition
Individuals present in the originally ascertained sample but missing sufficient data for inclusion in the current analyses were more likely to have a maternal history of depression (χ2=31.03, p<0.0001). They also fell into lower income quintiles that those included in these analyses (χ2=51.42, p<0.0001).
Results
Descriptive Statistics
Mean internalizing sum scores for each wave are provided in Table 1. Internalizing scores were higher for children of mothers with a history of depression (t-statistics ranging from 5.99 to 8.02, p<0.0001). Internalizing scores and family income were inversely related (F-statistics ranging from 10.35 to 12.38, df=4, p<0.0001). Details on alcohol use are provided in Table 2; note that only binge drinking and past 6 month alcohol use variables were included in subsequent analyses. Correlations between binary alcohol use outcomes (excluding the stem item “Have you ever had a full drink?”) ranged from 0.42–0.85. Age at initiation was modestly inversely correlated (−0.07 – −0.03) with the other alcohol outcomes.
Table 1.
Descriptive statistics for internalizing sum scores.
| Age in Months (SD) | |||||
|---|---|---|---|---|---|
| 47 (9.24) | 81 (9.15) | 97 (3.08) | 114 (1.57) | 140 (1.64) | |
| Mean (SE) | 1.45 (0.02) | 1.51 (0.02 | 1.69 (0.02) | 1.52 (0.02) | 1.47 (0.02) |
Table 2.
Descriptive statistics for alcohol use variables. Note that not all participants provided responses to every question. Items in italics were included as outcome variables.
| Alcohol use variable | % (N) of total sample |
|---|---|
| Ever had 1 full alcoholic drink | 52.6 (3119) |
| Had full drink within past 6 months | 41.0 (2428) |
| Ever drank without parental permission | 26.1 (1550) |
| Drank without parental permission, past 6 months | 24.1 (1426) |
| Had 3+ drinks on single occasion | 20.7 (1210) |
| Mean (SD) | |
| Age at first drink | 12.0 (1.1) |
| Number of whole drinks, past 6 months | 2.1 (5.5) |
Growth Mixture Modeling
Models with 2–6 classes were fit. To facilitate model convergence and identification, the variance of the quadratic term was fixed to 0 within each class for all models. A 5-class solution was selected for additional analyses: Although a 6-class solution provided minor improvements in AIC and BIC, the likelihood ratio test indicated that it did not provide a significantly better fit (Table 3). Furthermore, the sixth class reflected a difference in severity, but not shape, from another class. We did not pursue additional refinement of parameter estimates and variances, as our aim was to explore differences in alcohol outcomes across classes rather than to examine whether within-class variation differentially predicted alcohol outcomes. The variances of the intercept and slope terms were estimated to be different from 0 (p<0.001).
Table 3.
Growth mixture modeling fit statistics.
| # of Classes | AIC | BIC | Entropy | LMR Adjusted LRT p-value1 |
|---|---|---|---|---|
| 2 | 146,757.138 | 146,866.936 | 0.820 | <0.0000 |
| 3 | 145,504.964 | 145,644.041 | 0.803 | <0.0000 |
| 4 | 144,519.283 | 144,687.639 | 0.791 | <0.0000 |
| 5 | 143,900.295 | 144,097.930 | 0.777 | 0.0174 |
| 6 | 143,309.166 | 143,536.080 | 0.776 | 0.1560 |
A significant p-value indicates that a solution with n classes is significantly better than one with n−1 classes.
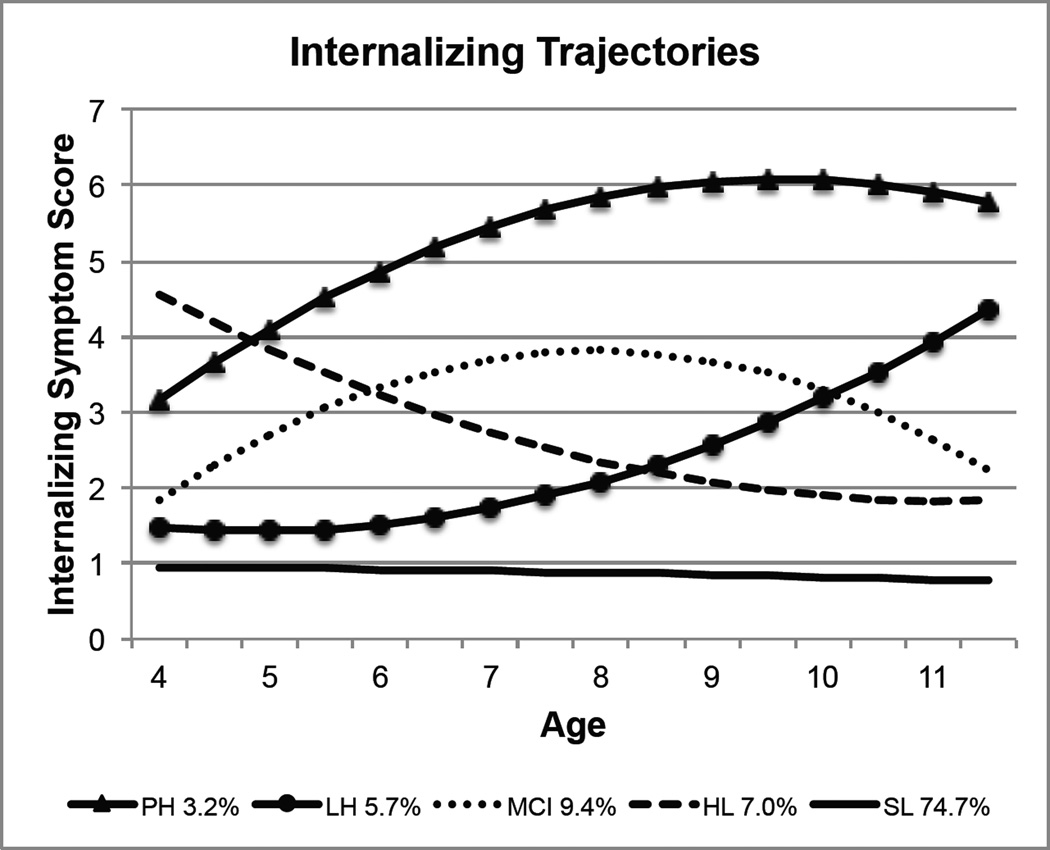
Description of the 5-Class Trajectory Solution
The five trajectories resulting from the model fitting process are depicted in Figure 1. Estimated mean growth parameters for each class are provided in Supplementary Table 1. For subsequent analyses, individuals were assigned to the class in which they had the highest posterior probability of membership; Supplementary Table 2 provides mean posterior probabilities of class membership for individuals assigned to each class. Class 1 (N=362, 3.2% of the sample; persistently high [PH]) is characterized by the second-highest initial level of internalizing symptoms, which increases for several years before stabilizing. Class 2 (N=631, 5.7%; low-to-high [LH]) has relatively low initial levels of internalizing symptoms, but these increase beginning at age 7. Class 3 (N=1048, 9.4%; mid-childhood increase [MCI]) exhibits increasing internalizing symptoms until approximately age 8, after which symptoms decrease. Class 4 (N=785, 7.0%; high-to-low [HL]) begins with the highest levels of problems, which decrease through age 9 and stabilize thereafter. Individuals in Class 5 (N=8331, 74.7%; stable low [SL]) exhibit consistently low levels of internalizing symptoms. The SL class was the reference class in subsequent analyses. Relationships between each class and demographic variables are described in Table 4.
Figure 1.
Five class trajectory solution.
Table 4.
Relationship between internalizing trajectories and demographic variables
| Class | % Girls1 | Family Income1,2 |
% with Maternal Depression History1 |
|---|---|---|---|
| Full sample | 48.6 | 3.4 | 8.5 |
| SL | 47.2a | 3.4a | 7.2a |
| PH | 54.1b,c | 2.9c | 20.1b |
| LH | 56.4c | 3.4a,b | 10.7c |
| MCI | 52.7b,c | 3.3b | 11.4c |
| HL | 49.6a,b | 3.2b | 11.4c |
Classes not identified by the same letter are significantly different from one other. Values for the full sample are provided for reference.
As described in the Methods, income is divided into quintiles. Here, the mean quintile is provided.
Relationship Between Internalizing Trajectories and Early Adolescent Alcohol Use
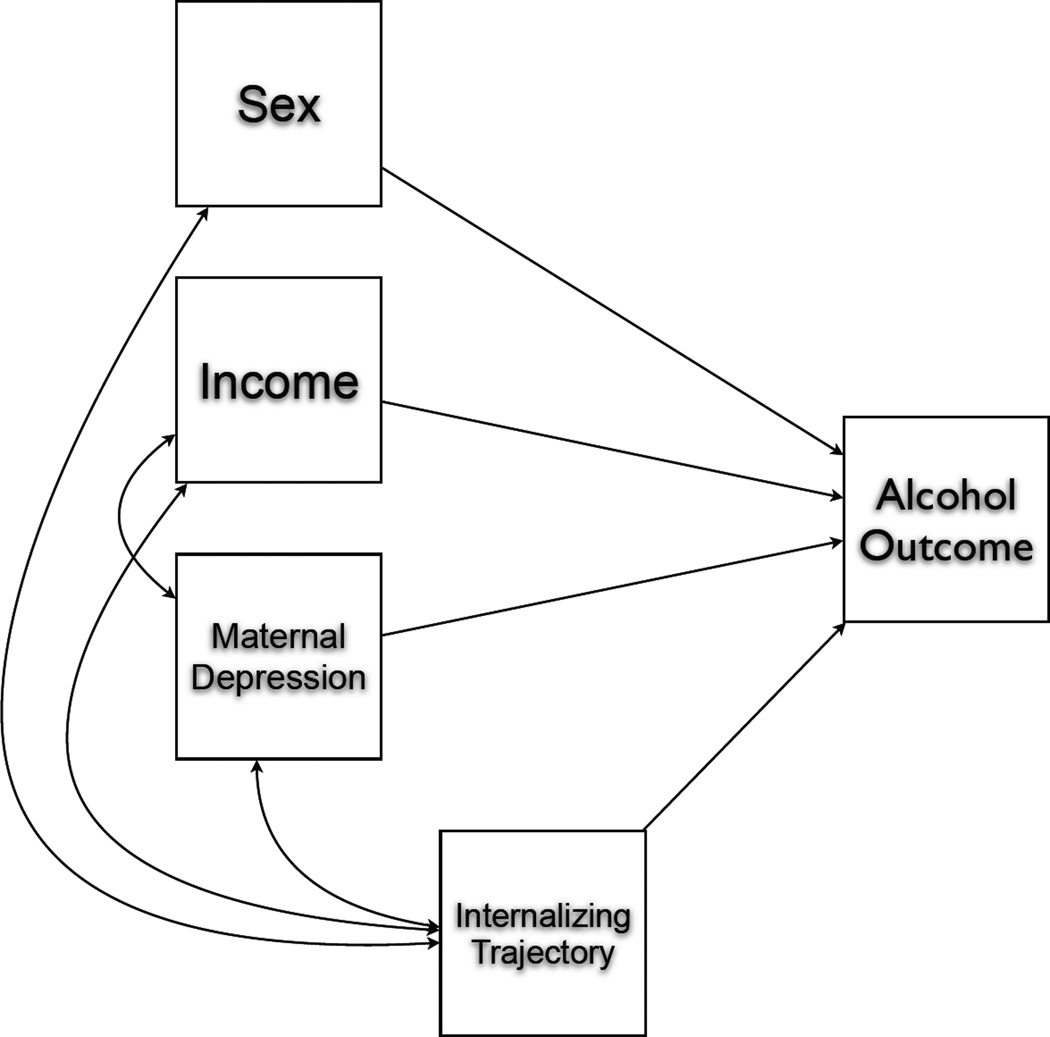
We next tested whether membership in each of the classes with elevated levels of internalizing symptoms – PH, LH, MCI, and HL – was associated with increased or decreased risk of each of the four alcohol outcomes as reported at age 13.8, relative to the SL class (see Figure 2 for a generalized model). The resulting odds ratios/parameter estimates are adjusted for the effects of sex, maternal depression, and income on alcohol outcomes, as well as for correlations among predictive variables. Results are presented in Table 5.
Figure 2.
Generalized structural equation model for assessing association between internalizing trajectory and adolescent alcohol use. Only correlations among covariates with p<0.05 are depicted. The “internalizing trajectory” variable is one of 5 contrasts described in the text.
Table 5.
Odds ratios (95% CI, p-value) for binary alcohol outcomes, and standardized parameter estimate (95% CI) for the continuous outcome (number of drinks), as a function of childhood internalizing trajectory. All estimates are adjusted for the effects of covariates (sex, income, and maternal depression). In each case, the Stable Low trajectory is the reference class.
| Internalizing Trajectory | |||||
|---|---|---|---|---|---|
| Alcohol Outcome | Persistently High (N=362) |
Low to High (N=631) |
Mid-Childhood Increase (N=1048) |
High to Low (N=785) |
Stable Low (reference) (N=8331) |
| Ever binged | .94 (.65 – 1.35, p=0.72) | .75 (.58 –.99, p=0.04) | .72 (.57 –.91, p<0.01) | .88 (.68 – 1.15, p=0.36) | 1.00 |
| Had whole drink in past 6 months | .83 (.61 – 1.12, p=0.22) | .83(.67 – 1.02, p=0.08) | .87 (.73 – 1.04, p=0.12) | .77 (.62 – .95, p=0.02) | 1.00 |
| Drank without parental permission in past 6 months | .87 (.61 – 1.24, p=0.44) | .86 (.67 – 1.09, p=0.21) | 1.04 (.85 – 1.27, p=0.71) | .75 (.58 –.97, p=0.03) | 1.00 |
| Number of whole drinks in past 6 months | −.92 (−1.04 – −.80, p<0.01) | 1.04 (−.42 – 0.63, p=0.70) | −.66 (−1.01 – −.31, p<0.01) | −.78 (−1.07 – −.48, p<0.01) | 1.00 |
Overall, individuals in any class with increased internalizing symptoms (PH, LH, MCI, and HL) were less likely to have engaged in at least one of the four alcohol-related outcomes. However, evidence for this association was inconsistent across class and outcome: individuals in LH and MCI were less likely to have binged relative to SL, while those in HL were less likely to have drank alcohol (with or without parental permission) in the last 6 months. With the exception of the LH class, all classes with elevated internalizing symptoms consumed fewer drinks in the previous 6 months than the SL class. Subsequent analyses indicated that no significant differences existed among elevated internalizing classes and the four alcohol-related outcomes (e.g., members of the PH class were no less likely to have binged than members of the MCI class; data available upon request).
Item Level Analyses
As a secondary analysis, we examined whether the relation between internalizing symptoms and alcohol use outcomes varied across different manifestations of internalizing symptomatology by conducting an item-level analysis. Because trajectory analyses indicated that the course of internalizing symptoms was not relevant to alcohol outcomes – only whether one had ever experienced elevated symptoms – we did not examine trajectories for each of the specific internalizing items. Rather, binary variables were derived for each (see Methods). Results, provided in Table 6, indicated that items suggestive of phobia and separation anxiety were consistently negatively associated with the four alcohol outcomes, with only one exception. Associations involved the remaining items were much less consistent.
Table 6.
Odds ratios (95% CI, p-value) for binary alcohol outcomes, and standardized parameter estimates (95% CI, p-value) for the continuous outcome (number of drinks), as a function of individual SDQ items. All estimates are adjusted for the effects of covariates (sex, income, and maternal depression).
| SDQ Item | |||||
|---|---|---|---|---|---|
| Alcohol Outcome | Often unhappy, depressed, or tearful |
Many worries or often seems worried |
Many fears, easily scared |
Nervous or clingy in new situations, easily loses confidence |
Complains of headaches, stomach-aches, or sickness |
| Ever binged1 | 1.24 (1.08 – 1.42, p<0.01) | .83 (.72 – .96, p=0.01) | .81 (.71 – .94, p<0.01) | .73 (.64 – .83, p<0.01) | 1.11 (.98 – 1.27, p=0.11) |
| Had whole drink in past 6 months1 | 1.03 (.92 – 1.15, p=0.65) | 1.01 (.90 – 1.13, p=0.86) | .85 (.75 – .95, p<0.01) | .74 (.66 – .82, p<0.01) | 1.07 (.96 – 1.19, p=0.22) |
| Drank without parental permission in past 6 months1 | 1.08 (.95 – 1.23, p=0.25) | 1.00 (.88 – 1.14, p=0.99) | .84 (.74 – .95, p<0.01) | .78 (.69 – .89, p<0.01) | 1.09 (.96 – 1.23, p<0.19) |
| Number of whole drinks in past 6 months2 | .14 (−.09 – .38, p=0.23) | − .17 (−.43 – .09, p=0.21) | .04 (− .23 – .31, p<0.78) | − .40 (− .66 – −.15, p<0.01) | .22 (− .03 – .47, p=0.08) |
Results provided are odds ratios;
Results provided are standardized parameter estimates.
Discussion
The goals of these analyses were to identify trajectories of internalizing symptoms from early childhood to early adolescence and to determine whether internalizing trajectories are associated with differential risk of four alcohol-related outcomes in early adolescence. We focused on this period because alcohol experimentation typically begins in early adolescence. While nearly 75% of the sample had stably low levels of internalizing symptoms, the remainder fell into four qualitatively different internalizing symptom trajectories. In general, individuals with elevated symptoms were less likely to engage in at least one of the four alcohol-related outcomes at age 13.8 relative to individuals in the stable low class. This could be due to a causal relationship, where internalizing symptoms protect against alcohol use. A non-causal explanation is also possible, wherein an unobserved shared factor (e.g., genetics or environmental confounders) influences both internalizing symptoms and liability to alcohol use. These mechanisms are not mutually exclusive.
The majority of the sample falls into the Stable Low trajectory, consistent with previous reports that a minority of children experience internalizing symptoms (Smucker et al., 1986). Among children who do experience problems, there is prior evidence of trajectories similar to those identified in the current study (Fanti and Henrich, 2010; Marmorstein et al., 2010a; McCarty et al., 2012; Wanner et al., 2012). Results vary across studies, possibly as a function of sample size and measurement instrument, but overall are broadly consistent with regards to trajectory shapes and interpretation.
While odds ratios and parameter estimates suggested that any early elevation in internalizing problems is inversely associated with at least one measure of alcohol use (e.g., binge drinking, drinking without parental permission, etc.) at age 13.8, the statistical significance of these estimates is quite modest and is inconsistent across class and the four alcohol-related outcomes. To determine whether the use of a class variable rather than a continuous variable affected our ability to detect relationships, we also conducted analyses using individuals’ posterior probability of class membership rather than assigning each individual to one class, with comparable results. An explanation for the specific patterns of association observed across the different trajectories is not immediately obvious, but the trend is for elevated internalizing symptoms to be negatively associated with alcohol use. These analyses should be replicated in other samples to provide additional information about whether the age at which children experience internalizing symptoms is relevant to their early adolescent alcohol use, or whether any childhood internalizing problems, regardless of course or duration, are associated with a lower risk of alcohol use in early adolescence.
Adolescent internalizing symptoms are frequently associated with higher levels of contemporaneous or later alcohol use (King et al., 2004; Marmorstein, 2009; Marmorstein, 2010; McCarty et al., 2012). However, few studies have examined childhood internalizing symptoms and their relationship with early adolescent alcohol use. The current results indicate that the course of these symptoms – whether persistent or temporally limited – is largely irrelevant to later alcohol outcomes: it is sufficient to have merely experienced elevated internalizing symptoms sometime during childhood.
However, our secondary analysis of the individual emotional problems subscale items suggests that these negative associations differ across components of the internalizing spectrum. In particular, items suggestive of phobia (“many fears, easily scared”) and separation anxiety (“nervous or clingy in new situations…”) are more consistently associated with lower alcohol use than are the other items. These findings are consistent with previous studies suggesting that particular manifestations of childhood internalizing problems are differentially associated with alcohol use (Hussong et al., 2011; Kaplow et al., 2001; King et al., 2004; Marmorstein et al., 2010b; Wu et al., 2010), though findings are inconsistent as to whether anxiety or depressive disorders are more problematic. A previous study of the ALSPAC sample found that self-reported depressive symptoms at age 10.5 were positively associated with problematic alcohol use in adolescence (Saraceno et al., 2011); this is consistent with the result for binge drinking reported here. While the limited nature of the SDQ (i.e., one item per manifestation) precluded more nuanced analyses, we do find support for the hypothesis that specific childhood internalizing constructs are differentially related to alcohol outcomes. Additional research is needed with a more comprehensive set of variables.
This study was not designed to identify the specific mechanisms through which childhood internalizing problems and adolescent alcohol use are associated. However, previous studies suggest that early childhood internalizing might be related to behaviorally inhibited temperament (Hussong et al., 2011), which could lead to difficulty interacting with peers later in childhood. This could represent a non-causal negative association, where internalizing symptoms merely index temperament, which itself predicts less alcohol use. As alcohol use in early adolescence occurs largely within the context of peer interactions (Hussong, 2000; Hussong, 2002), individuals whose childhood internalizing problems inhibit their ability to establish strong social contacts might be less likely to find themselves among peers who are experimenting with alcohol later. This represents a potential causal relationship.
It is critical to note that our study focused on very early adolescent alcohol use, as we were particularly interested in this period of early experimentation, and we did not explore whether childhood internalizing trajectories were associated with alcohol outcomes later in adolescence or early adulthood, where different relationships have been observed. To the extent that alcohol becomes more widely available later in adolescence and beyond, one’s childhood internalizing and potential social problems might present less of a “barrier to entry” later in development. Individuals whose internalizing problems desist might then be able to establish peer relationships, exposing them to opportunities for alcohol experimentation through peer groups. Even those who continue to experience internalizing symptoms during adolescence are still likely to experiment with alcohol (though this experimentation might be delayed relative to peers), at which point their experience with internalizing symptoms might lead to problematic drinking behaviors or expectations (Hussong et al., 2011).
In summary, we find that approximately one quarter of children experience elevated levels of internalizing symptoms at some point between ages 4 and 11.5. The course of these problems varies, with few (3.2%) experiencing high and sustained symptoms, others experiencing gradually increasing (5.7%) or decreasing (7.0%) symptoms over time, and yet others (9.4%) experiencing a transient increase in symptoms during mid-childhood. Children in any of these trajectories are slightly less likely to use alcohol at age 13.8. Given relatively modest levels of statistical significance and effect sizes that would not necessary meet significance criteria in smaller samplers, we cannot assert that individuals in a particular trajectory are differentially “protected”, nor can we determine whether the observed associations are due to a causal relationship. Symptoms of phobia and separation anxiety appear to drive the observed negative associations, though additional research is warranted as we were unable to assess whether the temporal course of construct-specific problems is relevant. Likewise, future studies on longitudinally assessed, population-based samples should examine how the relationship between internalizing symptoms and alcohol use changes from childhood into adolescence and young adulthood.
Limitations
These results must be considered in the context of several limitations. First, the measures of internalizing used in these analyses are derived from maternal reports. While this is appropriate for the age range of the sample, it is possible that maternal reports are less accurate than self-reports. In addition, there is some evidence that the observed relationship between internalizing symptoms and alcohol use differs depending on the reporter (McCarty et al., 2012). In addition, we did not explore whether childhood internalizing trajectories were associated with alcohol outcomes later in adolescence or early adulthood.
Second, individuals in all four trajectories of elevated internalizing symptoms were more likely to have a mother with a history of depression than were individuals in the SL class. A relationship between maternal depression and the emotional symptoms scale of the SDQ has been previously reported for this sample (Araya et al., 2009). Reporting bias in these mothers might have resulted in their description of elevated levels of internalizing in their child, though empirical studies of such an effect have produced mixed results (Fergusson et al., 1993; Sawyer et al., 1998). It is also possible that children of mothers with a history of depression actually experience more internalizing problems than their peers. With the current data is it not possible to determine whether either scenario is at work here. In addition, as noted in the Methods, some modest differences exist between the original sample and the sample retained in these analyses. These differences could have lead to slight biases in the results.
We would also underscore that the analyses conducted at the item level (reported in Table 3) should be considered with caution, as they are each based on a single indicator. Similarly, the alcohol-related outcomes were single items, and not based on comprehensive scales; this approach was selected to enable detection of potential distinctions among the different outcomes. We did not adjust significance thresholds to correct for multiple tests, and it is likely that a portion of the results meeting a threshold of p<0.05 would not survive such a correction. Finally, as with all applied statistical methodologies, growth mixture modeling has potential limitations (Bauer, 2007). Most notably, in addition to accurately depicting the developmental realities, GMM might spuriously result in the overextraction of trajectory classes. Specifically, misspecification of the structural model may require additional classes to account for discrepancies in the observed versus model implied means, variances, and covariances. Thus, it is critical that we temper our confidence in the results (Bauer and Curran, 2003). In summary, these analyses provide insight into the complex relationship between the course of internalizing problems and alcohol use, suggesting that, unlike adolescent depression, childhood internalizing problems protect individuals from early alcohol experimentation.
Supplementary Material
Acknowledgments
We are extremely grateful to all the families who took part in this study, the midwives for their help in recruiting them, and the whole ALSPAC team, which includes interviewers, computer and laboratory technicians, clerical workers, research scientists, volunteers, managers, receptionists and nurses. The UK Medical Research Council Grant ref: 74882) the Wellcome Trust (Grant ref: 076467) and the University of Bristol provide core support for ALSPAC. This publication is the work of the authors and the corresponding author will serve as guarantor for the contents of this paper. This research was specifically funded by the National Institutes of Health (K01AA021399 to A.C.E; K01AA020333 to S.J.L.; K02AA018755 to D.M.D.; R01AA018333 to D.M.D. and K.S.K).
Footnotes
Conflicts of Interest: None.
References
- Achenbach TM. Manual for the Child Behavior Checklist/4–18 and 1991 Profile. Burlington, VT: University of Vermont; 1991. [Google Scholar]
- Angold A, Costello EJ, Worthman CM. Puberty and depression: the roles of age, pubertal status and pubertal timing. Psychol Med. 1998;28:51–61. doi: 10.1017/s003329179700593x. [DOI] [PubMed] [Google Scholar]
- Araya R, Hu X, Heron J, Enoch MA, Evans J, Lewis G, Nutt D, Goldman D. Effects of stressful life events, maternal depression and 5-HTTLPR genotype on emotional symptoms in pre-adolescent children. Am J Med Genet B Neuropsychiatr Genet. 2009;150B:670–682. doi: 10.1002/ajmg.b.30888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bauer DJ. Observations on the use of growth mixture models in psychological research. Multivariate Behavioral Research. 2007;42:757–786. [Google Scholar]
- Bauer DJ, Curran PJ. Distributional assumptions of growth mixture models: implications for overextraction of latent trajectory classes. Psychol Methods. 2003;8:338–363. doi: 10.1037/1082-989X.8.3.338. [DOI] [PubMed] [Google Scholar]
- Birmaher B, Ryan ND, Williamson DE, Brent DA, Kaufman J, Dahl RE, Perel J, Nelson B. Childhood and adolescent depression: a review of the past 10 years. Part I. J Am Acad Child Adolesc Psychiatry. 1996;35:1427–1439. doi: 10.1097/00004583-199611000-00011. [DOI] [PubMed] [Google Scholar]
- Boyd A, Golding J, Macleod J, Lawlor DA, Fraser A, Henderson J, Molloy L, Ness A, Ring S, Davey Smith G. Cohort Profile: The 'Children of the 90s'--the index offspring of the Avon Longitudinal Study of Parents and Children. Int J Epidemiol. 2012 doi: 10.1093/ije/dys064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. MMWR. Atlanta, GA: 2012. Youth Risk Behavior Surveillance - United States, 2011. [Google Scholar]
- Chartier KG, Hesselbrock MN, Hesselbrock VM. Development and vulnerability factors in adolescent alcohol use. Child Adolesc Psychiatr Clin N Am. 2010;19:493–504. doi: 10.1016/j.chc.2010.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costello EJ. Child psychiatric disorders and their correlates: a primary care pediatric sample. J Am Acad Child Adolesc Psychiatry. 1989;28:851–855. doi: 10.1097/00004583-198911000-00007. [DOI] [PubMed] [Google Scholar]
- Crum RM, Green KM, Storr CL, Chan YF, Ialongo N, Stuart EA, Anthony JC. Depressed mood in childhood and subsequent alcohol use through adolescence and young adulthood. Arch Gen Psychiatry. 2008a;65:702–712. doi: 10.1001/archpsyc.65.6.702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crum RM, Storr CL, Ialongo N, Anthony JC. Is depressed mood in childhood associated with an increased risk for initiation of alcohol use during early adolescence? Addict Behav. 2008b;33:24–40. doi: 10.1016/j.addbeh.2007.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donovan JE, Molina BS. Childhood risk factors for early-onset drinking. J Stud Alcohol Drugs. 2011;72:741–751. doi: 10.15288/jsad.2011.72.741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Englund MM, Egeland B, Oliva EM, Collins WA. Childhood and adolescent predictors of heavy drinking and alcohol use disorders in early adulthood: a longitudinal developmental analysis. Addiction. 2008;103(Suppl 1):23–35. doi: 10.1111/j.1360-0443.2008.02174.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fanti KA, Henrich CC. Trajectories of pure and co-occurring internalizing and externalizing problems from age 2 to age 12: findings from the National Institute of Child Health and Human Development Study of Early Child Care. Dev Psychol. 2010;46:1159–1175. doi: 10.1037/a0020659. [DOI] [PubMed] [Google Scholar]
- Feng X, Shaw DS, Silk JS. Developmental trajectories of anxiety symptoms among boys across early and middle childhood. J Abnorm Psychol. 2008;117:32–47. doi: 10.1037/0021-843X.117.1.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fergusson DM, Lynskey MT, Horwood LJ. The effect of maternal depression on maternal ratings of child behavior. J Abnorm Child Psychol. 1993;21:245–269. doi: 10.1007/BF00917534. [DOI] [PubMed] [Google Scholar]
- Fleming CB, Mason WA, Mazza JJ, Abbott RD, Catalano RF. Latent growth modeling of the relationship between depressive symptoms and substance use during adolescence. Psychol Addict Behav. 2008;22:186–197. doi: 10.1037/0893-164X.22.2.186. [DOI] [PubMed] [Google Scholar]
- Fleming JE, Offord DR, Boyle MH. Prevalence of childhood and adolescent depression in the community. Ontario Child Health Study. Br J Psychiatry. 1989;155:647–654. doi: 10.1192/s0007125000018146. [DOI] [PubMed] [Google Scholar]
- Fraser A, Macdonald-Wallis C, Tilling K, Boyd A, Golding J, Davey Smith G, Henderson J, Macleod J, Molloy L, Ness A, Ring S, Nelson SM, Lawlor DA. Cohort Profile: The Avon Longitudinal Study of Parents and Children: ALSPAC mothers cohort. Int J Epidemiol. 2012 doi: 10.1093/ije/dys066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ge X, Lorenz FO, Conger RD, Elder GH, Simons RL. Trajectories of stressful life events and depressive symptoms during adolescence. Developmental Psychology. 1994;30:467–483. [Google Scholar]
- Goodman R, Ford T, Simmons H, Gatward R, Meltzer H. Using the Strengths and Difficulties Questionnaire (SDQ) to screen for child psychiatric disorders in a community sample. Br J Psychiatry. 2000;177:534–539. doi: 10.1192/bjp.177.6.534. [DOI] [PubMed] [Google Scholar]
- Goodman R, Scott S. Comparing the Strengths and Difficulties Questionnaire and the Child Behavior Checklist: is small beautiful? J Abnorm Child Psychol. 1999;27:17–24. doi: 10.1023/a:1022658222914. [DOI] [PubMed] [Google Scholar]
- Goodwin RD, Fergusson DM, Horwood LJ. Association between anxiety disorders and substance use disorders among young persons: results of a 21-year longitudinal study. J Psychiatr Res. 2004;38:295–304. doi: 10.1016/j.jpsychires.2003.09.002. [DOI] [PubMed] [Google Scholar]
- Hooshmand S, Willoughby T, Good M. Does the direction of effects in the association between depressive symptoms and health-risk behaviors differ by behavior? A longitudinal study across the high school years. J Adolesc Health. 2012;50:140–147. doi: 10.1016/j.jadohealth.2011.05.016. [DOI] [PubMed] [Google Scholar]
- Hussong AM. The settings of adolescent alcohol and drug use. Journal of Youth and Adolescence. 2000;29:107–119. [Google Scholar]
- Hussong AM. Differentiating peer contexts and risk for adolescent substance use. Journal of Youth and Adolescence. 2002;31:207–220. [Google Scholar]
- Hussong AM, Jones DJ, Stein GL, Baucom DH, Boeding S. An internalizing pathway to alcohol use and disorder. Psychol Addict Behav. 2011;25:390–404. doi: 10.1037/a0024519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joinson C, Heron J, Lewis G, Croudace T, Araya R. Timing of menarche and depressive symptoms in adolescent girls from a UK cohort. Br J Psychiatry. 2011;198:17–23. doi: 10.1192/bjp.bp.110.080861. sup 1–2. [DOI] [PubMed] [Google Scholar]
- Kaplow JB, Curran PJ, Angold A, Costello EJ. The prospective relation between dimensions of anxiety and the initiation of adolescent alcohol use. J Clin Child Psychol. 2001;30:316–326. doi: 10.1207/S15374424JCCP3003_4. [DOI] [PubMed] [Google Scholar]
- King SM, Iacono WG, Mcgue M. Childhood externalizing and internalizing psychopathology in the prediction of early substance use. Addiction. 2004;99:1548–1559. doi: 10.1111/j.1360-0443.2004.00893.x. [DOI] [PubMed] [Google Scholar]
- Maggs JL, Patrick ME, Feinstein L. Childhood and adolescent predictors of alcohol use and problems in adolescence and adulthood in the National Child Development Study. Addiction. 2008;103(Suppl 1):7–22. doi: 10.1111/j.1360-0443.2008.02173.x. [DOI] [PubMed] [Google Scholar]
- Marmorstein NR. Longitudinal associations between alcohol problems and depressive symptoms: early adolescence through early adulthood. Alcohol Clin Exp Res. 2009;33:49–59. doi: 10.1111/j.1530-0277.2008.00810.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marmorstein NR. Longitudinal associations between depressive symptoms and alcohol problems: The influence of comorbid delinquent behavior. Addict Behav. 2010;35:564–571. doi: 10.1016/j.addbeh.2010.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marmorstein NR, White H, Chung T, Hipwell A, Stouthamer-Loeber M, Loeber R. Associations between first use of substances and change in internalizing symptoms among girls: differences by symptom trajectory and substance use type. J Clin Child Adolesc Psychol. 2010a;39:545–558. doi: 10.1080/15374416.2010.486325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marmorstein NR, White HR, Loeber R, Stouthamer-Loeber M. Anxiety as a predictor of age at first use of substances and progression to substance use problems among boys. J Abnorm Child Psychol. 2010b;38:211–224. doi: 10.1007/s10802-009-9360-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mccarty CA, Wymbs BT, King KM, Mason WA, Vander Stoep A, Mccauley E, Baer J. Developmental consistency in associations between depressive symptoms and alcohol use in early adolescence. J Stud Alcohol Drugs. 2012;73:444–453. doi: 10.15288/jsad.2012.73.444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melotti R, Heron J, Hickman M, Macleod J, Araya R, Lewis G. Adolescent alcohol and tobacco use and early socioeconomic position: the ALSPAC birth cohort. Pediatrics. 2011;127:e948–e955. doi: 10.1542/peds.2009-3450. [DOI] [PubMed] [Google Scholar]
- Muthen LK, Muthen BO. Mplus User's Guide. Fifth Edition. Los Angeles, CA: Muthen & Muthen; 1998–2007. [Google Scholar]
- Najman JM, Williams GM, Nikles J, Spence S, Bor W, O'callaghan M, Le Brocque R, Andersen MJ, Shuttlewood GJ. Bias influencing maternal reports of child behaviour and emotional state. Soc Psychiatry Psychiatr Epidemiol. 2001;36:186–194. doi: 10.1007/s001270170062. [DOI] [PubMed] [Google Scholar]
- Needham BL. Gender differences in trajectories of depressive symptomatology and substance use during the transition from adolescence to young adulthood. Soc Sci Med. 2007;65:1166–1179. doi: 10.1016/j.socscimed.2007.04.037. [DOI] [PubMed] [Google Scholar]
- Pine DS. Childhood anxiety disorders. Curr Opin Pediatr. 1997;9:329–338. doi: 10.1097/00008480-199708000-00006. [DOI] [PubMed] [Google Scholar]
- Reinke WM, Eddy JM, Dishion TJ, Reid JB. Joint Trajectories of Symptoms of Disruptive Behavior Problems and Depressive Symptoms During Early Adolescence and Adjustment Problems During Emerging Adulthood. J Abnorm Child Psychol. 2012 doi: 10.1007/s10802-012-9630-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saraceno L, Heron J, Munafo M, Craddock N, Van Den Bree MB. The relationship between childhood depressive symptoms and problematic alcohol use in early adolescence: findings from a large longitudinal population-based study. Alcohol problems in depressed boys and girls. Addiction. 2011 doi: 10.1111/j.1360-0443.2011.03662.x. [DOI] [PubMed] [Google Scholar]
- Sawyer MG, Streiner DL, Baghurst P. The influence of distress on mothers' and fathers' reports of childhood emotional and behavioral problems. J Abnorm Child Psychol. 1998;26:407–414. doi: 10.1023/a:1022614800179. [DOI] [PubMed] [Google Scholar]
- Smucker MR, Craighead WE, Craighead LW, Green BJ. Normative and reliability data for the Children's Depression Inventory. J Abnorm Child Psychol. 1986;14:25–39. doi: 10.1007/BF00917219. [DOI] [PubMed] [Google Scholar]
- Wanner B, Vitaro F, Tremblay RE, Turecki G. Childhood trajectories of anxiousness and disruptiveness explain the association between early-life adversity and attempted suicide. Psychol Med. 2012:1–10. doi: 10.1017/S0033291712000438. [DOI] [PubMed] [Google Scholar]
- Wu P, Goodwin RD, Fuller C, Liu X, Comer JS, Cohen P, Hoven CW. The relationship between anxiety disorders and substance use among adolescents in the community: specificity and gender differences. J Youth Adolesc. 2010;39:177–188. doi: 10.1007/s10964-008-9385-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.