Abstract
Objectives
Healthy diet, physical activity and appropriate weight gain during pregnancy contribute to healthy birth outcomes. The Institute of Medicine recommends that women receive counseling about diet and exercise during preconception, pregnancy and postpartum periods. We sought to determine how often healthcare providers report counseling women of childbearing age about diet or exercise and if such rates vary by pregnancy, overweight/obesity status or physician specialty.
Methods
We combined the 2005-2010 National Ambulatory Medical Care Survey (NAMCS) and the National Hospital Ambulatory Medical Care Survey (NHAMCS) to obtain nationally representative estimates of outpatient preventive care visits for women of child-bearing age (15-44 years). Accounting for survey design, we compared proportions of preventive visits that included diet/exercise counseling for pregnant women vs. non-pregnant women and performed multivariable logistic regression models to estimate odds ratios.
Results
Providers reported counseling pregnant women about diet/exercise during 17.9% of preventive care visits compared to 22.6% of visits for non-pregnant women (P<0.01, adj. OR 0.8, 95% CI: 0.7, 1.0). Overweight/obese pregnant (vs. non-pregnant) women were significantly less likely to receive diet/exercise counseling (adj. OR 0.7, CI: 0.5, 0.9) as were women seen by OB/GYNs vs. non-OB/GYNs (adj. OR 0.4, CI: 0.3, 0.5).
Conclusions
Our findings suggest that provider-reported diet/exercise counseling rates during preventive care visits for women of childbearing age vary by overweight/obesity and pregnancy statuses, as well as by provider specialty. Our data suggest that there may be missed opportunities to provide diet/exercise counseling and that increasing rates of counseling could result in improved maternal and infant health outcomes.
Keywords: diet, physical activity, nutrition, counseling, pregnancy, provider practices, physician specialty
Objectives
The 2009 Institute of Medicine (IOM) developed guidelines for weight gain during pregnancy due to increased awareness of the adverse maternal and child health outcomes with excessive gestational weight gain and in response to changing demographics and epidemiologic profiles of the US women of child-bearing age [1]. Particularly, prepregnancy body mass index (BMI) and gestational weight gain (GWG) of women have increased while the proportion of pregnant women of advanced maternal age with chronic conditions has increased since the 1990 guidelines were instituted. The new recommendations emphasize healthy pregnancy outcomes for both the mother and the infant [1].
In order to implement these guidelines, the IOM recommends overweight and obese women receive dietary and physical activity counseling before conception and that all women receive counseling regarding diet and physical activity during pregnancy and postpartum periods [1]. According to one study analyzing the Behavior Risk Surveillance System (BRFSS), self-reported physical activity increased from 1994-2004, but nearly a quarter of women ages 30-49 and a mere fifth of women ages 19-29 reported physical activity in 2004 [2]. In the same study, pregnant women failed to achieve minimum activity recommendations more often (84.2%) than non-pregnant women (73.9%) [2]. Furthermore, observational studies have revealed that most women of child-bearing age do not meet recommended fruit and vegetable consumption [3,4].
In addition to prepregnancy BMI and GWG increasing over time, other health states associated with excessive weight gain have been on the rise since 1990 including depression [5,6], gestational diabetes [7], preeclampsia [8], gestational hypertension [8], cesarean deliveries [9-11], maternal and infant mortality [1,12], low birth weight/very low birth weight [13], small for gestational age births [1], large for gestational age births [1], preterm birth [13,14], and offspring childhood obesity [15].
Using data from the 2005-2010 National Ambulatory Medical Care Survey (NAMCS) and the National Hospital Ambulatory Medical Care Survey (NHAMCS), we sought to investigate how often providers reported providing diet/exercise counseling to women of childbearing age (15-44) during preventive care visits and whether these patterns differed by pregnancy status. Secondarily, we examined whether counseling rates differed by overweight/obesity status or by provider specialty.
Methods
Survey Design
The NAMCS and the NHAMCS are national probability sample surveys administered by the Centers for Disease Control and Prevention in outpatient ambulatory medical care settings [16]. NAMCS collects data on outpatient office-based clinics and community health centers whereas NHAMCS data is collected from hospital outpatient departments and emergency departments. These surveys are completed by non-federally employed physicians involved in direct patient care. In NAMCS, physicians are randomly assigned a 1 week reporting period during the year, in which the physician records data for a random sample of visits. In NHAMCS, a random sample of hospital visits is recorded by hospital staff during 1 of the 16 four-week randomly assigned reporting periods. Both surveys utilize a multi-stage, clustered probability design that involves probability samples of primary sampling units, physician practices within these units and patient visits within these practices. In order to produce unbiased national estimates, each patient visit was assigned an inflation factor, or the patient visit weight, based on the probability of selection and response. This approach allowed us to obtain national estimates of outpatient preventive care visits when appropriate weights were applied. The primary units of analysis were preventive health care visits for women of childbearing age. We combined the two data sources because outpatient office settings as well as hospital-based clinics provide most of preventive care visits in the United States. Visits to emergency departments (a subset of NHAMCS) were excluded from the analysis. To obtain a sample size with adequate power we combined the data for 2005-2010. Estimates were considered to be reliable when relative standard errors were 30 percent or less, and any estimates based on 30 or fewer observations were considered to be unreliable by the National Center for Health Statistics (NCHS) [17-20]. The current CDC data for both NAMCS and NHAMCS is available up until 2010 and 2005 was the first year that height and weight data were collected.
Variable Selection
Our primary outcome of interest was provider reported diet/exercise counseling. We derived this dichotomous variable from a combination of the checked indicator box of health education that included ‘diet/nutrition’, ‘exercise’ or ‘weight reduction’, ICD-9 diagnostic code for exercise counseling (V6541), exercise surveillance counseling (V653-) or a reason for visit code for diet and nutritional counseling (460.00). Visits were identified as ‘preventive care’ if the major reason for visit was recorded as preventive care or reason for visit codes, created by the NCHS for NAMCS/NHAMCS [17-20], were recorded as general medical exam (310.00), unconfirmed pregnancy (320.00), prenatal exam (320.50), gynecological exam (322.50), family planning (350.00), diet and nutritional counseling (460.00), counseling and examination for pregnancy (351.50), or progress visits (480.00). We included visits for women of child-bearing age (15-45 years of age), if they were classified as ‘preventive care’ and, for NAMCS, if the physician specialty was recorded as general/ family practitioner, obstetrician/gynecologist (OB/GYN), internal medicine, or pediatrician. For NAMCS, we only included visits for pregnant women if they were with a general/family medicine or OB/GYN provider. Women were classified as ‘pregnant’ if they had an ICD-9 diagnostic code for routine pregnancy visit (V22), reason for visit code for routine prenatal examination (320.50), pregnancy checkbox was marked (2005 & 2006 only), or if they had an ICD-9 code for complications of pregnancy (164.0 – 167.0).
Since we were interested in whether counseling rates differed by overweight/obesity status, we ascertained maternal BMI in the following ways. For non-pregnant women, we identified overweight and obese women through a combination of a BMI variable generated by the survey if height and weight data were available, ICD-9 diagnostic codes (‘27800’, ‘27801’, and ‘27802’) for overweight and obesity, a marked obesity diagnosis checkbox under the section “Regardless of the diagnoses written in 5a, does the patient now have obesity?” Initially, we intended to solely use the obesity checkmark to identify obese patients’ visits; however, some patients classified as obese had a BMI in the overweight range (25-29.9 kg/m2) and other patients identified with BMI’s > 30 kg/m2 did not have this checkbox marked.
Among pregnant women, BMI is not computed by the surveys; however, we calculated BMI if visits had height and weight data available. Since we were uncertain about which trimester in which the visit occurred and had no access to the woman’s prepregnancy BMI, we used a conservative estimate, subtracting the maximum allowable weight gain during pregnancy stated in the 2009 IOM report (40 lbs for an underweight women) from the current weight to calculate BMI. This provides a conservative proxy for prepregnancy maternal BMI. The same diagnostic codes and obesity checkbox marks in addition to the modified BMI were used to identify overweight and obese pregnant women. We combined visits for overweight and obese women into one category. For purposes of brevity, overweight and obese were referred to as ‘overweight.’ Provider specialty information was only available in the NAMCS data; thus, analyses including provider specialty were restricted to NAMCS only.
Multiple covariates were considered to be potential confounders. Age was divided into 5 categories (15-19; 20-24; 25-29; 30-34; 35-45) as done in a similar study [21] with slight modifications in order to address the issue of cells having less than 30 observations. We obtained race/ethnicity information based on categorizations indicated on the survey. The individual completing the survey recorded the perceived race/ethnicity of the patient based on observation, medical records, or via multiple choice checkboxes on the survey instrument. However, using finer subgroups of race created cells that violated NCHS’ reliability criteria [17,18]; thus, race/ethnicity was re-grouped into non-Hispanic white, non-Hispanic black, Hispanic, or Other (Asian, Native Hawaiian/Other Pacific Islander, American Indian/Alaskan Native, multiple races). We used insurance status as a proxy for socioeconomic status categorized into ‘Private’, ‘Medicaid’ and ‘Other’. Other variables we included were survey instrument (NAMCS vs. NHAMCS), geographic region (Northeast, Midwest, South, and West) and provider type (physician (MD) only, MD and other non-MD provider (nurse practitioner (NP), physician’s assistant (PA) or registered nurse (RN)), and non-MD provider only)). Because the IOM updated its guidelines regarding weight gain in pregnancy in 2009, we compared counseling rates before 2009 with the most recent 2010 data.
Statistical Analysis
Univariate analyses were conducted to obtain estimates of the number of preventive care visits annually in the US for women of child-bearing age. We performed bivariate analyses to obtain estimates of provider-reported counseling according to patient characteristics and provider characteristics. Multivariable logistic regression was utilized to identify predictors from a list of covariates and obtain relative odds of provider-reported counseling. We included covariates in the adjusted models based on clinical and/or statistical significance. The average of the 2005-2010 combined patient weights were used in the PROC SURVEYFREQ/PROC SURVEYLOGISTIC procedures to account for the complex study design.
Provider specialty information was only available in the NAMCS data; thus, analyses including provider specialty were restricted to NAMCS only. Because approximately 50% of visits had no data on overweight status, we compared our multivariable models comparing visits for pregnant vs. non pregnant women as well as the model for OB/GYN vs. non-OB/GYN using all visits to models visits with overweight status included. All analyses were performed using SAS version 9.2 (SAS Institute, Inc., Cary, North Carolina). The Beth Israel Deaconess Medical Center Institutional Review Board (IRB) Committee exempted this analysis from IRB review since it fulfilled criteria set forth in federal regulations at 45 CFR 46.101(b)(4).
Results
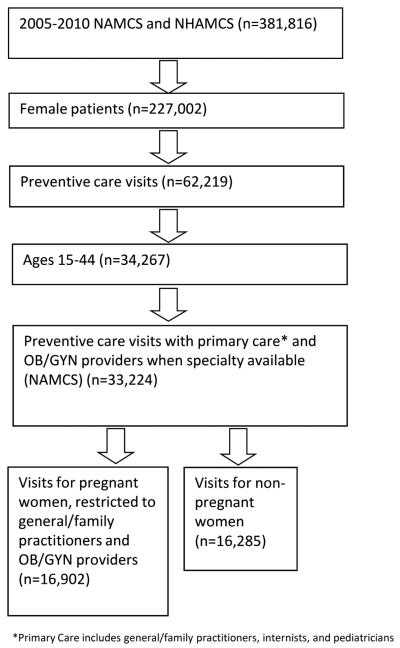
From 2005-2010 NAMCS and NHAMCS, a total of 33,187 preventive care visits for women of childbearing age were sampled, representing approximately 67.9 million visits annually (Figure 1). Providers reported providing diet/exercise counseling during 20.5% of these visits (95% CI: 18.2, 22.8). Forty-one percent of all of these visits were for pregnant women. Overall, preventive care visits for pregnant (vs. non-pregnant) women and for non-overweight (vs. overweight) women had lower rates of provider reported diet/exercise counseling. Only 17.9% of visits for pregnant women included counseling compared to 22.6% of the visits for non-pregnant women (P < 0.01). This association persisted after adjustment for age, race/ethnicity, insurance status, survey type (NAMCS vs. NHAMCS), region of the country, and provider type (adjusted OR 0.8, 95% CI: 0.7, 1.0). In addition, race, insurance status and provider type did not predict receipt of counseling (Table 1). Rates of counseling before (18.0%) and after (17.5%) the 2009 IOM updated pregnancy weight gain recommendations did not differ for pregnant women (P = 0.89). In the multivariable adjusted model, women ages 25-29 compared to younger (< 20 years) and older (≥ 35 years) age categories, women who were seen in outpatient ambulatory clinics compared to outpatient hospital departments and women who were seen in the Midwestern, Southern and Western regions of the US compared to the Northeastern region were less likely to receive counseling (Table 2). Among preventive care visits in which overweight status could be ascertained (49.2%), lean pregnant and non-pregnant women received less counseling than their overweight counterparts (20.0% vs. 26.0% (P = 0.05) and 19.4% vs. 36.2% (P < 0.0001), respectively). While visits for non-Hispanic White women were less likely to be coded as overweight (47.2 %) compared to non-Hispanic Black (58.0%) and Hispanic (50.0%) women, counseling rates were almost equivalent (25.4%, 26.0% and 28.2% respectively, P = 0.4). In an analysis analogous to the multivariable model above but restricted to visits in which overweight status could be obtained, we found that pregnant women were similarly less likely to receive diet/exercise counseling compared to non-pregnant women (adj. OR 0.8, CI: 0.6, 1.0). When we adjusted further for overweight status in this model, pregnancy continued to confer lower but non-significant and attenuated odds of a visit including counseling (adj. OR 0.9, CI: 0.7, 1.2). Among visits for overweight women, pregnant women were less likely to receive diet/exercise counseling than non-pregnant women (26.0% vs. 36.2%, P < 0.002, unadjusted OR 0.6, CI: 0.5, 0.8). After adjustment for age, race, insurance status, survey instrument, region and provider type, this association persisted (OR 0.7, CI: 0.5, 0.9). In an additional analysis treating those missing overweight status as its own category, we found that rates of counseling both pregnant (14.4%, CI: 10.9-17.9) and non-pregnant women (13.0%, CI: 10.9, 15.2) were low. Visits for those missing overweight status had a lower odds of receiving counseling compared to visits for overweight individuals (adj. OR 0.3, CI: 0.3, 0.4) and surprisingly lower odds compared to visits for non-overweight individuals (adj. OR 0.7, CI: 0.5, 0.8).
Figure 1.
Outpatient Visit Selection
Table 1.
Characteristics of preventative care visits for women of childbearing age (15-44 years), NAMCS, NHAMCS, 2005-2010.
| Pregnant | Non-pregnant | |||||
|---|---|---|---|---|---|---|
|
| ||||||
| Sample visits (n) |
Annual visit estimates in millions (%) |
Percent of visits with provider- reported counseling % (95% CI) |
Sample visits (n) |
Annual visit estimates in millions (%) |
Percent of visits with provider- reported counseling % (95% CI) |
|
| All visits | 16,902 | 29.9 | 17.9 (14.5, 21.3)a | 16,285 | 38.0 | 22.6 (20.4, 24.7) |
| Age categories (years)b | ||||||
| < 20 | 2256 | 3.1 (10.2) | 16.9 (11.6, 22.1) | 2529 | 5.5 (14.5) | 28.1 (24.0, 32.1) |
| 20-24 | 4936 | 7.6 (25.6) | 18.8 (14.6, 23.0) | 2820 | 5.5 (14.5) | 17.3 (14.4, 20.2) |
| 25-29 | 4775 | 9.2 (30.9) | 17.0 (13.3, 20.6) | 2862 | 6.5 (17.0) | 19.9 (16.6, 23.2) |
| 30-34 | 3433 | 7.3 (24.5) | 18.7 (14.4, 23.0) | 2578 | 5.7 (15.1) | 19.6 (16.3, 22.9) |
| ≥ 35 | 1502 | 2.6 (8.8) | 17.8 (13.1, 22.4) | 5496 | 14.8 (38.8) | 24.8 (21.7, 27.9) |
| Race/ ethnicity | ||||||
| Non- Hispanic White |
7004 | 17.2 (57.4) | 15.6 (12.0, 19.1) | 7503 | 23.3 (61.4) | 22.9 (20.2, 25.5) |
| Non- Hispanic Black |
3512 | 4.6 (15.5) | 20.6 (13.4, 27.7) | 3707 | 5.9 (15.6) | 22.1 (18.5, 25.8) |
| Hispanic | 4851 | 6.1 (20.3) | 22.4 (16.1, 28.7) | 3749 | 6.4 (16.8) | 20.7 (17.6, 23.8) |
| Other | 1535 | 2.0 (6.9) | 18.1 (12.2, 24.1) | 1326 | 2.4 (6.3) | 25.7 (19.7, 31.8) |
| Insurance status | ||||||
| Private | 4771 | 16.0 (55.0) | 15.6 (11.9, 19.3) | 6553 | 25.5 (69.5) | 23.1 (20.5, 25.7) |
| Medicaid | 9429 | 10.5 (36.0) | 21.1 (15.8, 26.4) | 5981 | 6.6 (18.0) | 20.3 (16.9, 23.7) |
| Other | 2200 | 2.6 (8.9) | 20.8 (11.4, 30.2) | 3088 | 4.6 (12.5) | 23.5 (18.8, 28.3) |
| Survey Instrumentc | ||||||
| NAMCS | 4197 | 25.5 (85.4) | 16.0 (12.2, 19.8) | 5751 | 33.5 (88.1) | 22.8 (20.4, 25.1) |
| NHAM | ||||||
| CS-OPD | 12705 | 4.4 (14.6) | 29.0 (23.8, 34.3) | 10534 | 4.5 (11.9) | 21.2 (18.5, 23.9) |
| Regionc | ||||||
| Northeast | 4803 | 4.1 (13.9) | 33.0 (22.6, 43.4) | 5666 | 7.9 (20.8) | 27.2 (21.2, 33.1) |
| Midwest | 4532 | 7.2 (24.2) | 10.7 (7.1, 14.2) | 3826 | 8.4 (22.2) | 22.1 (17.6, 26.5) |
| South | 3760 | 11.5 (38.3) | 20.0 (13.3, 26.7) | 3789 | 13.4 (35.4) | 20.3 (17.0, 23.7) |
| West | 3807 | 7.0 (23.6) | 13.0 (7.9, 18.1) | 3004 | 8.2 (21.6) | 22.3 (18.8, 25.7) |
| Provider Type | ||||||
| MD only |
3994 | 13.3 (44.6) | 15.7 (11.4, 20.0) | 5291 | 18.6 (49.2) | 22.0 (19.2, 24.9) |
| MD + | ||||||
| other provider (NP, PA or RN) |
9717 | 14.3 (48.3) | 19.9 (15.0, 24.7) | 7803 | 16.2 (43.0) | 23.8 (20.8, 26.8) |
| Non- MD only (NP, PA or RN) |
3075 | 2.1 (7.1) | 19.6 (13.5, 25.8) | 3039 | 2.9 (7.8) | 19.5 (13.7, 25.3) |
| Physician specialty (NAMCS only)b | ||||||
| OB/GYN | 3636 | 23.4 (91.5) | 16.0 (12.1, 19.9) | 3022 | 18.4 (54.9) | 15.9 (13.2, 18.6) |
| Non- OB/GYNe |
561 | 2.2 (8.5) | 15.9 (9.2, 22.6) | 2729 | 15.1 (45.1) | 31.1 (28.0, 34.3) |
| Overweight statusb,d | ||||||
| Overweight or Obese | 3077 | 5.0 (37.0) | 26.0 (19.9, 32.0) | 5118 | 12.8 (55.7) | 36.2 (32.8, 39.6) |
| Normal BMI/Underweight |
4855 | 8.5 (62.8) | 20.0 (15.5, 24.4) | 3268 | 10.2 (44.3) | 19.4 (16.4, 22.4) |
Abbreviations: MD physician, RN registered nurse, NP nurse practitioner, PA physician’s assistant, OB/GYN obstetrician/gynecologist, NAMCS National Ambulatory Medical Care Survey, NHAMCS-OPD National Hospital Ambulatory Medical Care Survey Outpatient Department
P < 0.01 Chi-Square comparing provider reported counseling for pregnant vs. non-pregnant women.
P < 0.0001 Chi-Square comparing provider reported counseling within covariate group among non-pregnant women.
P < 0.0001 Chi-Square comparing provider reported counseling within covariate group among pregnant women.
P < 0.05 Chi-Square comparing provider reported counseling within covariate group among pregnant women.
In NAMCS, non-OB/GYN visits for pregnant women includes general/family practitioners and for non-pregnant women, includes general/family practitioners, internists and pediatricians.
Table 2.
Associations of provider-reported diet/exercise counseling for women of childbearing age by maternal, survey, and provider characteristics (NAMCS, NHAMCS 2005-2010)
| Model 1a | Model 2b | Model 3c | |
|---|---|---|---|
| OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| Pregnant (vs. non-pregnant) | 0.8 (0.7, 1.0) | 0.8 (0.6, 1.0) | 0.9 (0.7, 1.2) |
| Age categories (years) | |||
| < 20 | 1.3 (1.0, 1.6) | 1.6 (1.3, 2.1) | 1.8 (1.4, 2.4) |
| 20-24 | 1.0 (0.8, 1.1) | 1.0 (0.8, 1.2) | 1.0 (0.9, 1.3) |
| 25-29 | reference | reference | reference |
| 30-34 | 1.1 (0.9, 1.3) | 1.1 (0.9, 1.3) | 1.0 (0.8, 1.3) |
| ≥ 35 | 1.3 (1.1, 1.5) | 1.3 (1.1, 1.6) | 1.2 (1.0, 1.5) |
| Race/ ethnicity | |||
| Non-Hispanic White | reference | reference | reference |
| Non-Hispanic Black | 1.0 (0.8, 1.3) | 1.0 (0.7, 1.3) | 0.9 (0.7, 1.2) |
| Hispanic | 1.1 (0.9, 1.4) | 1.2 (1.0, 1.5) | 1.2 (0.9, 1.5) |
| Other | 1.2 (0.9, 1.6) | 1.3 (0.9, 1.9) | 1.5 (1.0, 2.1) |
| Insurance status | |||
| Private | reference | reference | reference |
| Medicaid | 1.0 (0.8, 1.3) | 1.0 (0.8, 1.2) | 0.9 (0.7, 1.1) |
| Other | 1.1 (0.8, 1.5) | 1.1 (0.8, 1.6) | 1.1 (0.7, 1.5) |
| Survey | |||
| NAMCS (vs. NHAMCS) | 0.8 (0.6, 1.0) | 0.8 (0.6, 1.1) | 0.8 (0.6, 1.1) |
| Region | |||
| Northeast | reference | reference | reference |
| Midwest | 0.5 (0.3, 0.8) | 0.6 (0.4, 1.0) | 0.6 (0.4, 0.9) |
| South | 0.7 (0.4, 1.0) | 0.8 (0.5. 1.1) | 0.7 (0.5, 1.1) |
| West | 0.6 (0.4, 0.9) | 0.5 (0.4, 0.8) | 0.5 (0.3, 0.8) |
| Provider Type | |||
| MD only | reference | reference | reference |
| MD + other provider (NP, PA or RN) | 1.1 (0.8, 1.4) | 1.1 (0.9, 1.5) | 1.1 (0.9, 1.5) |
| Non-MD only (NP, PA or RN) | 1.4 (0.9, 2.2) | 1.1 (0.8, 1.7) | 1.1 (0.8, 1.7) |
| Overweight status | |||
| Overweight/obese | N/A | N/A | 2.1 (1.8, 2.5) |
| Non-overweight/obese | N/A | N/A | reference |
NAMCS National Ambulatory Medical Care Survey, NHAMCS National Hospital Ambulatory Medical Care Survey
Model 1 is adjusted for all listed variables except overweight status.
Model 2 = model 1 restricted to visits not missing overweight status.
Model 3 = model 2 further adjusted for overweight status.
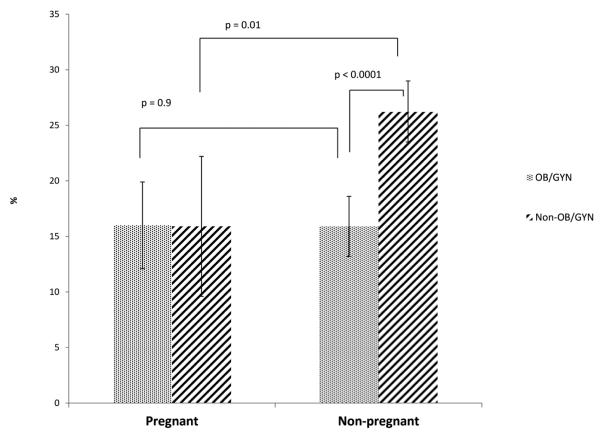
Among preventive care visits for non-pregnant women to office-based physicians (NAMCS), internists, general and family medicine practitioners and pediatricians reported higher rates (31.1%, CI: 28.0, 34.3) of counseling compared to OB/GYNs (15.9%, CI: 13.2, 18.6) (P < 0.0001). There was no difference in counseling rates between OB/GYN vs. non-OB/GYN for visits for pregnant women (Table 1). The interaction term between provider specialty and pregnancy status was significant (P = 0.005). When we further stratified by pregnancy status, it became evident that there was no difference in counseling by overweight status among visits for pregnant women, but that there were vast differences among visits for non-pregnant women (Table 3, Figure 2). In a multivariable regression model restricted to visits for non-pregnant women and adjusting for age, race, insurance type, region and provider type, the association persisted with OB/GYNs reporting counseling less often than their non-OB/GYN counterparts (OR 0.4, CI: 0.3, 0.5). When we compared odds ratios of OB/GYN (vs. non-OB/GYN) reported counseling in models restricted to visits with overweight status before and after adjustment for overweight status, there was no change in adjusted odds ratios (0.4, CI: 0.3, 0.5 and 0.4, CI: 0.3, 0.6 respectively).
Table 3.
Percentage (95 % CI) of NAMCS visits including provider reported diet-exercise counseling by provider specialty and overweight/obesity statusesa
| % counseling | OB/GYN | Non-OB/GYN |
|---|---|---|
| Visits for pregnant women b | 20.1 (14.7, 25.5) | 21.7 (11.4, 32.0) |
| Visits for non-pregnant women c | 19.8 (16.1, 23.6) | 37.0 (33.2, 30.9) |
| Overweight/Obese d | 26.0 (21.6, 30.4) | 45.3 (40.6-49.9) |
| Non-overweight/Obese e | 13.0 (8.7, 17.3) | 26.2 (22.0-30.3) |
NAMCS National Ambulatory Medical Care Survey
Analysis was restricted to those with overweight status ascertained (n = 5377). We did not stratify visits for pregnant women by overweight status since some cells had < 30 observations.
Non-significant p-value, comparing visits for pregnant women seen by OB/GYN vs. non-OB/GYN, n=1847.
P < 0.0001 chi square, comparing all visits for non-pregnant women seen by OB/GYN vs. non-OB/GYN, n=3810.
P < 0.0001 chi square, comparing visits for obese non-pregnant women seen by OB/GYN vs. non-OB/GYN, n=2215.
P < 0.0003 chi square, comparing visits for non-obese non-pregnant women seen by OB/GYN vs. non-OB/GYN, n=1595.
Figure 2.
Percentage of NAMCS visits including provider-reported diet-exercise counseling by pregnancy status and provider specialty (n=9948).
Discussion
We found that overall, providers reported counseling women of childbearing age about diet/nutrition/exercise during only a fifth of all preventive visits. Visits for pregnant women (vs. non-pregnant), non-overweight (vs. overweight) women and visits with OB/GYN (vs. non-OB/GYN) providers were less likely to include counseling. There were no differences in counseling rates by race/ethnicity despite a higher incidence of overweight among minority women. We did not detect differences in counseling before and after the 2009 IOM pregnancy weight gain guidelines, but we suspect it may be too early to detect any change since 2010 is the most recent data available for analysis.
While non-pregnant women were more likely to receive counseling, rates were still relatively low and there is room for improvement among primary care providers. This is consistent with a recently published study of NAMCS data by Kraschnewski and colleagues [22]. While they studied all primary care visits for adults, not just women of childbearing age, they reported low rates of counseling of 7.8% and 6.2% of the visits in two distinct survey periods (1995-1996 and 2007-2008, respectively). While their study relied on diagnostic coding, their data support our findings that provider report of counseling is uncommon. Another study utilizing the National Health and Nutrition Examination data have found that overweight and obese patients whose physicians have acknowledged their weight status have a greater desire to lose weight or attempt weight loss [23]. These studies provide evidence that preventive care visits may be an underutilized and potentially useful venue to increase diet and exercise counseling for both pregnant and non-pregnant women.
Previous studies have shown that women who receive advice about weight gain during pregnancy are more likely to gain the recommended amount of weight [24]. Despite its importance, a national study surveying US OB/GYNs prevention and management of obesity in pregnancy found that only 63.4% of the physicians used maternal pre-pregnancy BMI to modify their pregnancy weight gain recommendations [25]. In another survey study, most obstetric providers reported advising gestational weight gain ranges that were not in accordance with the IOM guidelines [26]; suggesting not only are there missed chances to counsel but that the content of the counseling sessions may have opportunities to improve. Additionally, in our analysis, we observed that visits for pregnant women in outpatient office-based clinics were less likely to include counseling compared to those in outpatient hospital departments. This is consistent with studies that have demonstrated using national surveys that women of lower socioeconomic status received less or lower quality prenatal and other health-related counseling in private offices compared to outpatient hospital clinics [27,28].
The primary strength of our study is the use of a large, nationally representative sample, with patient weights applied to obtain national estimates. There are several limitations to this study inherent to large surveys. Information biases from survey instruments may lead to exposure and/or outcome misclassification. It is possible that the providers provided counseling without marking a checkmark on the Patient Record Form, thus underestimating the number of visits that included counseling. The forms were completed primarily by either hospital staff or Census field representatives during a specific period; therefore it is probable that the women are receiving counseling during separate visits that are not captured by the record from that day. It is also plausible that another individual with a different role (nutritionist, community health worker) within the healthcare or community setting could be providing counseling that would not be captured in this survey. However, underreporting is most likely to be random based on patient characteristics and was quite low regardless of the individual marking the Patient Record Form. Additionally, the quality of the counseling could not be assessed from these forms.
Pregnancy status could potentially be misclassified since the pregnancy status checkbox was only available for certain years. However, we used a robust method to identify pregnant women through a combination of ICD-9 diagnostic codes, checkbox and reason for visit codes. These codes were carefully examined to be indicative of pregnancy status that would minimize misclassification. Similar methods were used to identify preventive care visits and to keep misclassification to a minimum.
Although we attempted to identify obese/overweight status through methods similar to identifying pregnancy status, approximately 50% of the visits were missing overweight status. This could potentially bias our results substantially. However, comparison of our primary analysis in the overall cohort to the smaller cohort of visits that had BMI data produced similar results. When we subsequently adjusted for overweight status, the association between pregnancy status and receipt of counseling was somewhat attenuated, raising the possibility of confounding by overweight status. However, the association was still in the same direction. Nonetheless it is still very likely that these visits are not missing overweight status at random since the rates of counseling for those missing overweight status was very low for both pregnant and non-pregnant women. We speculate that when overweight was not of clinical concern to the provider or the patient (i.e. leaner, healthier patients), it was omitted from the collection form. Such omission, if included would have likely only strengthened the association between overweight and counseling. We do not believe it would have significantly altered the inverse association between pregnancy status and counseling. Additionally, the obesity/overweight rates among pregnant women is likely to be underestimated since we only considered pregnant women in extreme BMIs to be included in this category. Our overall obesity/overweight rate was 48.9%. According to the CDC data, the prevalence of age-adjusted obese/overweight individuals in the US from 2005-2010 ranged from 66.9-68.8% [29]. Alternatively, it is possible that our estimates may be plausible. According to the Pediatric and Pregnancy Nutrition Surveillance System (PNSS) data from 2005-2010, between 48.5% and 55.0% of all pregnant women were overweight (including obese) and 44.0% to 50.2% of all mothers gained weight that exceeded the ideal weight gain recommended in the 2009 IOM report [30].
We restricted provider specialty for preventive visits for pregnant women to OB/GYN and family and general practitioners. We included internists and pediatricians (in addition to OB/GYN and family and general practitioners) for visits for non-pregnant women. We were only able to do so for NAMCS visits because these data are not available from NHAMCS. Selectively restricting the NAMCS sample to appropriate primary care providers but not for NHAMCS could potentially introduce differential misclassification bias. Visits to non-primary care providers from NHAMCS could be included in our sample. This, however, is unlikely to have an influence on the outcome since the weighted frequency of visits to outpatient office physicians (NAMCS) was 86.9% compared to 13.1% of the total percentage of visits to outpatient hospital departments (NHAMCS). NHAMCS provider misclassification would be expected to a minimal effect on our results. It is possible that internists and pediatricians more routinely counsel about diet and exercise regardless of the patient in their offices. This could partially explain differences in counseling during visits for pregnant vs. non-pregnant patients.
It is also possible that OB/GYN’s report counseling less often because they have many prenatal visits during which they may only provide counseling during a subset (i.e. initial visit). However, this is not likely responsible for our findings given that the main difference in specialty specific counseling rates were among visits for non-pregnant patients. In the multivariable analyses, OB/GYNs still provided less counseling compared to non-OB/GYNs even after controlling for pregnancy and overweight statuses. Still, it is important to note that the “episode” of care is different when comparing visits for pregnant vs. non-pregnant patients because non-pregnant patients are likely to be seen only once a year.
In summary, we found that despite clear recommendations that pregnant women receive counseling regarding diet, exercise and weight gain during pregnancy, that pregnant women are less likely to receive such counseling during the course of preventive care. Our data suggest that there may be many missed opportunities to provide diet/exercise counseling and propose that efforts to increase counseling rates could result in improved maternal and infant health outcomes.
Acknowledgements
The authors would like to thank the CDC and the participating patients and providers who contributed to NAMCS and NHAMCS. The senior author is funded by the Klarman Scholars Program and by NIH/NIEHS K23-ES022242.
References
- 1.(IOM) Institute of Medicine; (NRC) National Research Council, editor. Weight Gain During Pregnancy: Reexamining the Guidelines. The National Academies Press; Washington, DC: Jul 30, 2010. 2009. [PubMed] [Google Scholar]
- 2.Evenson KR, Savitz DA, Huston SL. Leisure-Time Physical Activity among Pregnant Women in the Us. Paediatr Perinat Epidemiol. 2004;18:400–407. doi: 10.1111/j.1365-3016.2004.00595.x. [DOI] [PubMed] [Google Scholar]
- 3.Guenther PM, Dodd KW, Reedy J, Krebs-Smith SM. Most Americans Eat Much Less Than Recommended Amounts of Fruits and Vegetables. J Am Diet Assoc. 2006;106:1371–1379. doi: 10.1016/j.jada.2006.06.002. [DOI] [PubMed] [Google Scholar]
- 4.Serdula MK, Gillespie C, Kettel-Khan L, Farris R, Seymour J, Denny C. Trends in Fruit and Vegetable Consumption among Adults in the United States: Behavioral Risk Factor Surveillance System, 1994-2000. Am J Public Health. 2004;94:1014–1018. doi: 10.2105/ajph.94.6.1014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Compton WM, Conway KP, Stinson FS, Grant BF. Changes in the Prevalence of Major Depression and Comorbid Substance Use Disorders in the United States between 1991-1992 and 2001-2002. Am J Psychiatry. 2006;163:2141–2147. doi: 10.1176/ajp.2006.163.12.2141. [DOI] [PubMed] [Google Scholar]
- 6.Gaynes BN, Gavin N, Meltzer-Brody S, Lohr KN, Swinson T, Gartlehner G, Brody S, Miller WC. Perinatal Depression: Prevalence, Screening Accuracy, and Screening Outcomes. Evid Rep Technol Assess (Summ) 2005:1–8. doi: 10.1037/e439372005-001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Getahun D, Nath C, Ananth CV, Chavez MR, Smulian JC. Gestational Diabetes in the United States: Temporal Trends 1989 through 2004. Am J Obstet Gynecol. 2008;198:525, e521–525. doi: 10.1016/j.ajog.2007.11.017. [DOI] [PubMed] [Google Scholar]
- 8.Wallis AB, Saftlas AF, Hsia J, Atrash HK. Secular Trends in the Rates of Preeclampsia, Eclampsia, and Gestational Hypertension, United States, 1987-2004. Am J Hypertens. 2008;21:521–526. doi: 10.1038/ajh.2008.20. [DOI] [PubMed] [Google Scholar]
- 9.Chu SY, Kim SY, Schmid CH, Dietz PM, Callaghan WM, Lau J, Curtis KM. Maternal Obesity and Risk of Cesarean Delivery: A Meta-Analysis. Obes Rev. 2007;8:385–394. doi: 10.1111/j.1467-789X.2007.00397.x. [DOI] [PubMed] [Google Scholar]
- 10.MacDorman MF, Menacker F, Declercq E. Cesarean Birth in the United States: Epidemiology, Trends, and Outcomes. Clin Perinatol. 2008;35:293–307. v. doi: 10.1016/j.clp.2008.03.007. [DOI] [PubMed] [Google Scholar]
- 11.Menacker F, Declercq E, Macdorman MF. Cesarean Delivery: Background, Trends, and Epidemiology. Semin Perinatol. 2006;30:235–241. doi: 10.1053/j.semperi.2006.07.002. [DOI] [PubMed] [Google Scholar]
- 12.Martin JA, Kung HC, Mathews TJ, Hoyert DL, Strobino DM, Guyer B, Sutton SR. Annual Summary of Vital Statistics: 2006. Pediatrics. 2008;121:788–801. doi: 10.1542/peds.2007-3753. [DOI] [PubMed] [Google Scholar]
- 13.Martin JA, Hamilton BE, Ventura SJ, Osterman MJ, Kirmeyer S, Mathews TJ, Wilson EC. Births: Final Data for 2009. Natl Vital Stat Rep. 60:1–70. [PubMed] [Google Scholar]
- 14.Martin JA, Osterman MJ, Sutton PD. Are Preterm Births on the Decline in the United States? Recent Data from the National Vital Statistics System. NCHS Data Brief. :1–8. [PubMed] [Google Scholar]
- 15.Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of Overweight and Obesity in the United States, 1999-2004. JAMA. 2006;295:1549–1555. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- 16. [Accessed December 4, 2012];Ambulatory Health Care Data. Available at: http://www.cdc.gov/nchs/ahcd.htm.
- 17. [Accessed October 20, 2012];2005 Namcs Micro-Data File Documentation. 2005 Available at: ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Dataset_Documentation/NAMCS/doc05.pdf.
- 18. [Accessed November 4, 2012];2005 Nhamcs Micro-Data File Documentation. 2005 Available at: ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Dataset_Documentation/NHAMCS/doc05.pdf.
- 19. [Accessed November 4, 2012];2010 Nhamcs Micro-Data File Documentation. 2010 Available at: ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Dataset_Documentation/NHAMCS/doc2010.pdf.
- 20. [Accessed November 5, 2012];2010 Namcs Micro-Data File Documentation. 2010 Available at: ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Dataset_Documentation/NAMCS/doc2010.pdf.
- 21.Burris HH, Werler MM. U.S. Provider Reported Folic Acid or Multivitamin Ordering for Non-Pregnant Women of Childbearing Age: Namcs and Nhamcs, 2005-2006. Matern Child Health J. 2010;15:352–359. doi: 10.1007/s10995-010-0587-6. [DOI] [PubMed] [Google Scholar]
- 22.Kraschnewski JL, Sciamanna CN, Stuckey HL, Chuang CH, Lehman EB, Hwang KO, Sherwood LL, Nembhard HB. A Silent Response to the Obesity Epidemic: Decline in Us Physician Weight Counseling. Med Care. 2013;51:186–192. doi: 10.1097/MLR.0b013e3182726c33. [DOI] [PubMed] [Google Scholar]
- 23.Post RE, Mainous AG, 3rd, Gregorie SH, Knoll ME, Diaz VA, Saxena SK. The Influence of Physician Acknowledgment of Patients’ Weight Status on Patient Perceptions of Overweight and Obesity in the United States. Arch Intern Med. 2011;171:316–321. doi: 10.1001/archinternmed.2010.549. [DOI] [PubMed] [Google Scholar]
- 24.Stotland NE, Haas JS, Brawarsky P, Jackson RA, Fuentes-Afflick E, Escobar GJ. Body Mass Index, Provider Advice, and Target Gestational Weight Gain. Obstet Gynecol. 2005;105:633–638. doi: 10.1097/01.AOG.0000152349.84025.35. [DOI] [PubMed] [Google Scholar]
- 25.Power ML, Cogswell ME, Schulkin J. Us Obstetrician-Gynaecologist’s Prevention and Management of Obesity in Pregnancy. J Obstet Gynaecol. 2009;29:373–377. doi: 10.1080/01443610902946911. [DOI] [PubMed] [Google Scholar]
- 26.Herring SJ, Platek DN, Elliott P, Riley LE, Stuebe AM, Oken E. Addressing Obesity in Pregnancy: What Do Obstetric Providers Recommend? J Womens Health (Larchmt) 19:65–70. doi: 10.1089/jwh.2008.1343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kotelchuck M, Kogan MD, Alexander GR, Jack BW. The Influence of Site of Care on the Content of Prenatal Care for Low-Income Women. Matern Child Health J. 1997;1:25–34. doi: 10.1023/a:1026272318642. [DOI] [PubMed] [Google Scholar]
- 28.McCormick MC, Deal LW, Devaney BL, Chu D, Moreno L, Raykovich KT. The Impact on Clients of a Community-Based Infant Mortality Reduction Program: The National Healthy Start Program Survey of Postpartum Women. Am J Public Health. 2001;91:1975–1977. doi: 10.2105/ajph.91.12.1975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Health, United States, 2011 [Accessed December 4, 2012];With Special Feature on Socioeconomic Status and Health. 2012 Available at: http://www.cdc.gov/nchs/data/hus/hus11.pdf#069. [PubMed]
- 30. [Accessed December 15, 2012];2011 Pregnancy Nutrition Surveillance: Summary of Trends in Maternal Health Indicators by Race/Ethnicity. 2011 Available at: http://www.cdc.gov/PEDNSS/pnss_tables/pdf/national_table20.pdf.