Abstract
Purpose
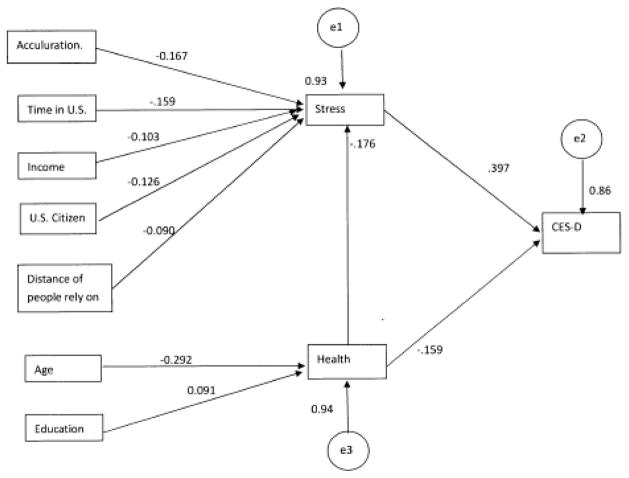
This study documents the indirect effects of social and environmental variables as mediated by immigrant stress and physical health.
Methods
Using data from a large dual frame sample of first generation mandarin speaking Chinese immigrants in metropolitan Los Angeles counties with the largest groups of Chinese immigrants, this study uses a path analytic approach to trace how predictors are related to depressive symptoms and to measure direct and indirect influences of variables.
Results
Although bivariate analyses suggested that many predictors were associated with depressive symptoms, multivariate path analysis revealed a more complex structure of mediated associations. In the multivariate path analysis only reports of physical health and immigrant stress were directly related to depressive symptoms (P<.05), while acculturation, time in the U.S., income, U.S. citizenship, and distance of persons on whom one could rely were related to stress (but not to physical health status) and only to depressive symptoms as mediated by stress. Age and educational attainment were related to health status (and to stress as mediated by physical health) and to depressive symptoms as mediated by both health and stress. These variables were also unrelated directly to health status and to depressive symptoms. Associations were evaluated using statistical significance, P<.05.
Conclusions
This study demonstrates the significance of stress and health as mediators of variables in the larger context of the physical environment and suggests that the mechanisms linking ecological characteristics of immigrants to depressive symptoms may be stress and physical health among immigrants.
Keywords: Depressive symptoms, Immigrant Depression, Stress, Ecological Factors
Introduction
Immigration is intrinsically a stressful process, which places individuals into a foreign social environment that must be accommodated rapidly in order to survive (1). Migration to the U.S. from Asia increased dramatically after the American reform of immigration laws in the 1960’s (2). More than 3.5 million Chinese constituted 24% of all Asians in the U.S., and 63% of these were foreign born (3). About 42% of these Chinese reported limited English proficiency (4).
The prevalence of major depressive symptoms among Chinese Americans is higher than among Chinese residing in mainland of China or Taiwan (2,5). Stress influences mental health among older Chinese immigrants (6) as well as well among other Chinese (7–10). Immigration-related stressors have been associated with mental disorders among Asian Americans (11), including depressive symptoms (12). Life stress, especially stress associated with poor medical health, was reported to be the strongest predictor of depressive symptoms among Asian immigrant elders (6,13) and the effects were reported to be greatest among Chinese American adults (5). Individual stress among immigrants stems from the multitude of difficulties related to low acculturation, especially to language problems (14–16), physical health (6), racism (17) (18), experiencing negative life events and social conflict (11), lack of funds, and unemployment (7,11,19). All of these enhance stress and have been reported to contribute to depressive symptoms (7,10,11,20,21).
Understanding the factors associated with immigrant depressive symptoms will help mental health providers identify vulnerable subgroups and promote adequate mental health services. But the association between environmental variables and depressive symptoms among Asian Americans are complex. More specifically, studies that have examined groups by country or special group of population suggested that the association is not universal across immigrant ethnicity and sub-groups. For example, the pattern that nativity and other social contributors associated with depressive symptoms among women was different from that among men (22,23), moreover, women were reported to be more vulnerable to depressive symptoms in the context of chronic conditions (24) and gender may have interaction with other risk factors (25); first generation immigrants were more likely to have mental health symptoms with the increasing of acculturative stress compare to second and third generations (22), however previous literature does not provide an in-depth understanding of depression etiologies among first-generation immigrants. Furthermore, studies also found that Asian immigrants are not a homogenous group in the context of differences of depression experienced. Depression rates varied across countries among Asian immigrants (22,26), for example, one study revealed that Filipino and Korean immigrant elders had the lowest rate of depression compared to other Asian immigrant including Chinese (6). The influence of acculturation on mood disorders also varied among groups from different country or region due to different culture value and beliefs (27,28), for instance, it was reported that both the amount and sources of perceived stress of elderly Chinese immigrants were different from those of elderly Americans (29). For these reasons, it is useful to investigate the influences of environmental factors among discrete groups of immigrants.
Based on her theory of segmented assimilation, Min Zhou (2009) reports that upward mobility and success by American standards is prevalent among Chinese and other immigrants who bring resources (education, language, money and social linkages) with them (30).
Understanding the factors associated with immigrant depressive symptoms will help mental health providers identify vulnerable subgroups and promote adequate mental health services. However, current understanding of the relationship between acculturative stress and health status and depression is relatively limited, especially among first generation Chinese immigrants. Therefore, it is useful to re-examine the influence of acculturation, stress and social support on mental health among a first-generation Chinese immigrants and compare the difference of patterns between genders in influence of social environmental factors on depressive symptoms.
THEORETICAL FRAMEWORK
To examine factors that may contribute to depressive symptoms of Chinese immigrants living in LA, we used stress-coping model of Maes, Leventhal & De Ridder (1996) (31). The model illustrated the roles of and interrelationships among three major constructs: stressors, mediators or coping resources, and distress or health outcome. The paradigm also theorized that the available coping resources, such as financial and social supports, could affect the stress and then affect mental health status. Our study examined disease related stress (health perception), acculturative stress, and acculturative stressors (those resulting from the acculturation process), demographic characteristics (education, age and gender etc.) and the external supporting resources (distance from people rely on).
We used the definitions from Folkman & Lazarus, which defined stress as a “transaction (or relationship) between individuals and their environment. Such transactions include harm, threats, or challenges” (32). Coping resources are defined as the “primarily properties of the person, including health and energy (a physical resource), positive beliefs (a psychological resource), and problem-solving and social skills (competencies)” (33), it usually include spiritual, financial, and social supports (33,34). We assumed that these immigrants’ coping resources influenced functioning and overall quality of life and, consequently, depressive symptoms. First, acculturative stress was described as the divergence a racial/ethnic minority person experiences when exposed to a dissimilar culture (35). Such as acculturative stress is linked to mental disorders, especially depression (36).
Acculturation has been defined as a dynamic process involving multiple aspects in which individuals gradually adjust to a new environment (37). The acculturation process could result in the development of stress from diverse factors and resources available to immigrants, such as income, education, and language proficiency (13) and to immigrants being unable to receive the social support from their family members after they move to the United States (38). However, when demographic and socioeconomic states variables were controlled, acculturation had no effect on the level of depression (39).
Income was reported to affect mental health independently. Individuals with a lower family income reported a higher level of depressive symptoms (40). Thus, we examined how education, income, and acculturation had influence on depressive reaction independently.
A number of studies found that social support was associated with depression directly. Depression has been reported to occur more frequently among elderly Asian immigrants with few resources for dealing with losses associated with the immigrant experience, such as social networks (13).
Finally, health status has been recognized as an important contributor to depression (6,41), although it also has a profound influence on the individual’s mental functioning. Studies found that self-rated poor health strongly was strongly related to depression among Chinese and Korean elder immigrants (6,40,42). However, poor health may also be a consequence of acculturative stress (43) so that self-rated health was included in our model to better understand the relationships between acculturation and depression.
The purpose of this study is to specify how immigrant stress and physical health may be linked to depressive symptoms and how stress and health may mediate the link between environmental and situational variables and depressive symptoms. The approach is based on the following hypotheses:
H1: Health status and immigrant stress directly influence depressive symptoms among immigrants.
H2: Health status and immigrant stress mediate the influences of depressive symptoms and situational variables such as age, education, income, citizenship, social support, and acculturation.
Method
Data for this study were drawn from a larger study of health concerns among first generation Chinese immigrants residing in three counties of Chinese concentration in the metropolitan Los Angeles area (44). All procedures were approved by the San Diego State University Institutional Review Board. The authors know of no conflicts of interest, and all certify responsibility for the present manuscript.
The Sample
Data were drawn from a larger study of health risks among Chinese immigrants 21years and older who spoke either English or Mandarin and who had been born in mainland China or Taiwan and resided in three counties in the Los Angeles Metropolitan Statistical Area. A dual frame (45–48) sampling approach (N=1199) was used. The first frame of the sample (N=776), randomly selected telephone numbers associated with adults who had one of 300 Anglicized Chinese surnames that appeared in land line telephone directories. The person in the household with the most recent birthday was interviewed (46–49). The 300 name list encompassed over 85% of Han names (by far the most common group in China) according to Lauderdale and Kestenbaum (2000: 290–295). Lauderdale and Kestenbaum estimated that over 90% of Chinese tend to marry within ethnicity, and that the majority of Chinese can still be identified by surname (2002). Recent data, however, suggest that intermarriage among Asians and other groups is increasing (50).
The universe of names encompassed between 80% and 90% of names linked to Chinese persons in the United States, and was the basis for sampling Chinese who resided in Los Angeles, Orange, and San Bernardino counties. The three counties included a large majority of all Chinese who resided in the Los Angeles metropolitan area. These data constituted a probability sample of eligible persons who could be reached by land line telephone, although initial data demonstrated a strong age bias despite stratification by age and age was related to health risks and participating by cell phone.
A second frame (N=423) was based on nonprobability procedures to correct for age biases in the first frame. Random digit dialing (RDD) procedures, which could have captured cell phones, proved cost ineffective since no telephone exchanges in the three counties were populated densely by Chinese at the time of fieldwork. Population and varying mixes of nationality and ethnic migration produced extremely heterogeneous exchanges on which to base RDD sampling (30). Alternative approaches to recruiting included recruitment involving language schools, radio, ethnic fairs, recreational facilities, educational institutions, Asian stores and shops frequented by Chinese. Referrals from would-be survey participants who fell outside the age stratum were also included. While nonprobability procedures do not permit estimating population parameters accurately, the data do permit testing hypotheses. Testing between the subsamples indicated no major structural differences in unstandardized regression coefficients between the subsamples although descriptive data presented significant age differences from the two frames.
The Questionnaire
Survey items were written initially in English and translated into Mandarin by bilingual and monolingual native-born speakers. The items were then subjected to back translation, modifications to translations made, and a process of fore and back translation repeated until native Mandarin speakers were satisfied that the meaning of concepts was clear.
Interviewing
Interviews were conducted using a bilingual team of closely supervised professional interviewers who had been trained and vetted for the survey using role playing and other pedagogical procedures. The cooperation rate (percent of eligible persons who completed interviews) was 55.0%
Measurement
Depressive Symptoms
Depressive symptomatology (rather than a clinical diagnosis of depression) was measured by items from the CESD, developed by Radloff (51), shortened to the form reported by Cole and co-analysts (52). Items were first standardized (mean=0, SD=1) to correct for different variances, items five and eight (the negative measures of depression) reflected, and then items were summed to form the depressive symptoms scale. Reliability for the 10 items was α=0.77 (See Appendix Tables 1 for item wording, and statistics).
Appendix Table 1.
Depression Scale Item Wording and Statistics.a
| Item | Never | Monthly/less | 2–4 per Month | 5–7 per Week | Mean | SD | N |
|---|---|---|---|---|---|---|---|
| Score: | 0 | 1 | 2 | 3 | |||
| I was bothered by things that usually don’t bother me | 68.9% | 22.0 | 5.3 | 3.8 | 0.4 | 0.6 | 1198 |
| I had trouble keeping my mind on what I was doing | 77.7% | 16.9 | 2.3 | 2.2 | 0.3 | 0.6 | 1197 |
| I felt depressed | 67.2% | 28.0 | 3.8 | 1.0 | 0.4 | 0.6 | 1198 |
| I felt everything I did was an effort | 80.4% | 16.6 | 1.8 | 1.2 | 0.2 | 0.5 | 1198 |
| I felt hopeful about the future* | 4.9% | 13.5 | 29.7 | 51.9 | 2.3 | 0.9 | 1194 |
| I felt fearful | 78.7% | 18.2 | 2.3 | 0.8 | 0.2 | 0.5 | 1197 |
| My sleep was restless | 67.7% | 17.4 | 7.6 | 7.3 | 0.5 | 0.9 | 1198 |
| I was happy* | 2.4% | 14.9 | 31.2 | 51.6 | 2.3 | 0.8 | 1197 |
| I felt lonely | 68.6% | 26.4 | 3.3 | 1.7 | 0.4 | 0.6 | 1198 |
| I could not get “going” | 61.0% | 35.2 | 2.7 | 1.2 | 0.4 | 0.6 | 1194 |
Respondents were asked: “Now I will read a list of the ways you might have felt or behaved. Please tell me how often you have felt this way during the past week, rarely of none of the time, a little of the time (1–2 days), a moderate amount of the time (3–4days), or most or all of the time (5–7 days).” Numbers in cells are the scores assigned to each response, the percentages who gave each response, the means and standard deviations of the scores, and the number of participants responding to each item.
The “*” indicates that the items were reflected prior to scoring. Scales scores were computed by
Immigrant Stress
Immigrant stress was measured by responses to 11 of the original 20 items (14) from a subset found to be internally consistent (53) in a psychometric study of the original scale among Korean immigrants residing in California. Items were first standardized (mean=0, SD=1) and then summed to form the scale which was reflected so that high scores indicate high stress (Cronbach’s α=0.74). Items focused on missing original country, difficulties in facing new situations and with language, work credentials, poor treatment and lack of respect, and not feeling at home (See Appendix Tables 2. for item wording, and statistics).
Appendix Table 2.
Stress Scale Item Wording and Statistics.a
| Item | Agree Strongly | Agree | Dis-agree | Dis-agree Strongly | Mean | SD | N |
|---|---|---|---|---|---|---|---|
| Score: | 1 | 2 | 3 | 4 | |||
| When I think of my original country, I get teary | 0.8% | 9.7 | 82.4 | 7.1 | 3.0 | 0.4 | 1195 |
| I get sad when I think of special places back home | 1.3% | 22.9 | 70.2 | 5.6 | 2.8 | 0.5 | 1195 |
| I am always facing new situations and circumstances | 2.5% | 37.2 | 58.5 | 1.8 | 2.6 | 0.6 | 1188 |
| I have to depend on other people to show or teach me how things are done | 0.4% | 12.3 | 81.9 | 5.4 | 2.9 | 0.4 | 1192 |
| My work status is lower than it used to be | 2.0% | 27.0 | 65.3 | 5.7 | 2.8 | 0.6 | 897 |
| The work credential I had in my original country are not accepted | 0.7% | 30.1 | 63.1 | 6.1 | 2.8 | 0.6 | 880 |
| Americans have a hard time understanding my accent | 3.5% | 30.4 | 63.1 | 2.9 | 2.6 | 0.6 | 1166 |
| As an immigrant, I am treated as a second class citizen | 2.0% | 30.0 | 65.5 | 2.4 | 2.7 | 0.5 | 1184 |
| People with foreign accents are treated with less respect | 1.2% | 33.9 | 63.4 | 1.5 | 2.6 | 0.5 | 1174 |
| I do not feel at home | 1.3% | 28.0 | 68.0 | 2.8 | 2.7 | 0.5 | 1183 |
Originally names the “Demands of Immigration Scale,” this set of items has been used as markers to major stressors immigrants often encounter. Respondents were asked: “As I read each of the following things regarding how some people feel about living in the U.S., please just tell me if you agree strongly, agree, disagree, or disagree strongly.” Numbers in cells are the scores assigned to each response, the percentages who gave each response, the means and standard deviations of the scores, and the number of participants responding to each item.
Health Status
Health status was measured from responses to “In general, how would you describe your health? Very good, good, poor, or very poor?” scored 4-1. The measure has been found to predict morbidity and mortality (54).
Acculturation
Acculturation was measured using the Suinn-Lew scale adapted for telephone interviews (55,56) and scored so that higher scores indicated greater acculturation. Items were designed to measure aspects of cultural preferences involving language, music, food, and self-identification including how the self is identified, father’s identification, and social linkages including ethnicity of peers and preferred associations. Analysis revealed that the scale was unidimensional. Item scores were first standardized (mean=0, SD=1) to equalize item variance and then summed to form a composite (Cronbach’s α=0.75). The scale was then transformed using the natural logarithm to constrain skewness.
Social Support
Social support was measured from responses to “About how far from where you live are people on whom you can rely on in case of emergencies? Within 1 mile, within 5 miles, within 50 miles, within 500 miles, further, or none in the U.S.?” Categories were scored using the midpoints of distance respectively, so that the higher the score the greater the distance and the lower access to support.
American Citizenship
Citizenship was measured by responses to “Are you an American citizen?” and coded 1=yes and 0=no.
Demographics
Income, education, time in the U.S., and age were measured by self-report. Both years of education in China/Taiwan and in the U.S. were summed and the redundant years in the sending and receiving nations subtracted.
Analysis
STATA (version 13.0) was employed in all analyses, with the structural equation modeling (SEM) procedure used to compute path analysis. The criterion for statistical significance was set at P≤ 0.05. The logic of analysis assumed that immigrant stress had a major influence on depression, that physical health status influenced both stress and depression, and that age and education would influence health. Income, acculturation, years in the U.S., American citizenship, and social support were assumed to indicate life opportunities and would influence immigrant stress inversely. Gender was unrelated to depression, immigrant stress, and health (P>.05) and was dropped from the analysis.
Results
The Sample
Mean CES-D depressive symptoms for the sample was 6.00 (SD=3.81), stress was −.039 (SD=0.59), and 6.6% rated their health as very poor or poor, while 36.0% rated their health as very good and 57.4% rated their health as good. About 66.7% were American citizens, 52.2% male, and 56.7% were born in mainland China. Mean acculturation (employing the natural logarithm) was 2.29 (SD=0.50), age 43.88 (SD=43.88), family income $26.649 (SD=$24,375), years in the U.S. 15.6 years (10.18), social support 1.8 (SD=1.0) indicating mean distance between one and five miles, and education was 15.27 (SD=3.21) years.
Bivariate correlations between depressive symptoms and each of the predictors are presented in Table 1. Good health status, family income, years in the U.S., education, and American citizenship were all negatively, and immigrant stress positively, associated with depressive symptoms P<0.001. Acculturation and social support were also associated negatively (P<0.01) to depressive symptoms. Years lived in mainland China or Taiwan, gender, and language of interview were not related statistically significantly to depressive symptoms and were dropped from further analysis. Although age was not associated directly to depressive symptoms, subsequent analysis demonstrated that age was related significantly albeit indirectly to depressive symptoms through the mediation of health status. Since language also loaded heavily on the acculturation measure, and gender and years in mainland China or Taiwan failed to be significantly related directly or indirectly to depressive symptoms, they were also dropped from further consideration.
Table 1.
Characteristics of First Generation Mandarin Speaking Chinese Immigrants in Greater Los Angeles, California, 2010–2011.a
| Predictor | Mean/% | SD | N | Bivariate rb |
|---|---|---|---|---|
| CES-D | 6.00 | 3.81 | 1131 | |
| Health status | 2.40 | 0.59 | 1130 | ***−0.24 |
| Immigrant Stress | −0.39 | 3.95 | 1131 | ***0.43 |
| Acculturation | 2.29 | 0.50 | 1131 | **−0.10 |
| Age | 43.88 | 14.04 | 1132 | −0.04 |
| Family income | $26,649 | $24,375 | 946 | ***−0.06 |
| Time in U.S. | 15.60 | 10.18 | 1132 | ***−0.10 |
| Social Support | 1.73 | 0.96 | 1117 | **−.09 |
| Total Years of education | 15.27 | 3.21 | 1125 | ***−.10 |
| American citizen | 66.7% | 1115 | ***−.11 |
Numbers in cells are means, standard deviations, or percentages and numbers of cases among first generation Chinese immigrants. Acculturation was transformed to constrain skewness using a natural logarithm. The total N interviewed was 1199 and the above N’s vary due to missing data being deleted.
Bivariate product moment correlations between depressive symptoms and predictors with
P<.001,
P<.011, and
P<.050.
Remaining correlations P>.050
The probability subsample reported a lower mean depressive symptom score than the non-probability subsample (P<0.006), lower stress (P<0.004), were older (P<0.001), had been in the U.S. longer (P<0.001), reported less education (years) (0.02), and were more likely to be citizens (P<0.001). The probability and non-probability samples were not significantly different on health status, acculturation, social support, and income (P>0.05).
Path Analysis
Path analysis requires simplifying assumptions concerning the temporal order of variables. The initial assumption was that immigrant stress, physical health, and acculturation would directly influence depressive symptoms, and the rest of the variables would be exogenous. The analysis supported our hypothesis that only health and stress served as mediators between other variables, including acculturation.
Figure 1 presents the structure of associations. It became clear that statistically significant direct effects between predictors and depressive symptoms were present in the structural equation model only for immigrant stress and health status once other variables were controlled. Older persons reported poorer health and more years of education, better health, but age and education were unrelated directly to depressive symptoms or to immigrant stress. Acculturation, time in the U.S., income, and American citizenship were related negatively to immigrant stress, and social support was related positively to immigrant stress. These variables were also unrelated directly to health status.
Figure 1.
Path model of Chinese First Generation Immigrants’ depression
The exogenous variables were all related indirectly through the mediation of immigrant stress and health status, as portrayed in Table 2. Once the indirect and direct effects of each variable were computed, it was clear that immigrant stress increased and good health status decreased depressive symptoms substantially, supporting our more general hypothesis. Health status influenced depressive symptoms both directly and indirectly as mediated by immigrant stress on depressive symptoms. Time in the U.S., education, income, and age had relatively small, but theoretical meaningful, indirect and total effects on depressive symptoms, while social support (higher scores indicate lower support), citizenship, acculturation appear to reduce depressive symptoms substantially, and immigrant stress to increase depressive symptoms substantially. Gender was unrelated to depression, stress, and health in bivariate and multivariate analyses and dropped from the model. Model fit met acceptable criteria with χ2(14)=42.41, P<0.001, RMSEA=0.041, and CFI=0.957.
Table 2.
Standardized Direct, Indirect and Total Effects on CES-D Among Chinese First Generation Immigrants in Greater Los Angeles.a
| Predictor | Direct | Indirect | Total |
|---|---|---|---|
| Immigrant stress | .383 | - | .383 |
| Ln acculturation | - | −.505 | −.505 |
| Time in U.S. | - | −.023 | −.023 |
| Age | - | .018 | .018 |
| Health Status | −1.018 | −.447 | −1.466 |
| Family Income | - | −.063 | −.063 |
| American Citizen | - | −.403 | −.403 |
| Social Support | - | .141 | .141 |
| Education | - | −.024 | −.024 |
Numbers in cells are direct, indirect, and total effects based on path analysis. The model improved fit significantly, χ2 (14)=42.41, P<.001, RMSEA=.041, CFI=.957, TLI=.926. “Ln” indicates the natural logarithm of acculturation was used to constrain skewness.
The analyses were replicated first, with the probability sample, and second, with the non-probability sample. The probability sample results generally mirrored those for both groups combined. While coefficients were similar among the non-probability sample, some differences in coefficients were revealed, most likely due to age and differing concerns in the life cycle. Age had a greater association with health and education but a lower association (P>0.05) with health among the non-probability group. Although the directions of associations were the same, neither citizenship nor social support was related statistically significantly (P>0.05) to immigrant stress. The same was true of the association between income and stress, albeit borderline (P=0.051).
Discussion
This study demonstrates that stress and health status are associated with depressive symptoms among a sample of first generation immigrants from China or Taiwan. It also clarifies that ecological and situational variables have important influences on depressive symptoms primarily through the mediation of immigrant stress and physical health status. Poor health and acculturative stress play a direct role in increasing risk for depression. The findings support those reported in a number of other studies, but also specify that situational variables likely influence depression through mediation rather than being associated with depression directly. In contrast to several studies, gender was not associated with depression in our data.
Our data support the view, also reported in other studies, that situations and problems that immigrants are likely to face in coming to a new society, be they physical health, language problems, low levels of social support, and diminished social status, may increase stress which in turn leads to depressive symptoms. This demonstrates the significance of the ecological and situational variables in counseling and treating immigrants for depression since these variables are associated with direct causes of depressive symptoms.
Our results showed that the effects of acculturation on depressive symptoms was indirect, which is generally consistent with those observed among Chinese immigrants (6–8,23) as well as among Korean Americans (9,10), these studies also found that acculturation affects the severity of depressive symptoms via indirect pathway mediated by stress, and acculturative stress is key risk factors for immigrants’ depression (11,22,23). However, we found that the effects of acculturation on mental health were primarily positive, which is inconsistent with other observations (11,57).
Several reasons may contribute to the inconsistency. First, the average age of participants in this study were relative older (43.88 ± 14.04 years old) than the Hwang’s study (38.38 ± 12.65 years old) and Shen’s study (38.67 ± 9.52 years old), and it was suggested that acculturation was associated with depression positively among young adults and negatively among older adults (57). Second, all of the participants in this study were foreign born and, although a few have been in the U.S. for more than 60 years, the mean years in the U.S. was only 15.6 years. This suggests that this group of immigrants was more vulnerable to stress others who had been in the U.S. longer. Also, English is taught in both mainland China and Taiwan and is usually regarded as the most important component of acculturation so that the negative association with stress is to be expected. This suggests that immigrants may benefit special instruction that conveys better command of English.
This study also suggests that reported health status has both direct and positive effects on depression; people with better health are less likely to report depressive symptoms. However, the association of depression with poor health is complex. Although previous studies have documented that health status, number of medical conditions, and the numbers of stressful events were associated with depressive symptoms (58), it is difficult to determinate the direction of association. Poor self-rated health has been found to be a risk for depression in longitudinal analyses (6), and poor physical health may be a consequence of depression (59), Given the cross-sectional study design, we cannot discern the direction of association between health status and depression nor the direction of association among other variables. However, our assumptions agree with those in many studies.
Our model also demonstrated that income level was more strongly related to acculturative stress than health status, and that education only influenced depressive symptoms when mediated by health status, but that income was not directly associated with stress. However, Shen’s analysis supported the conclusion that SES (a composite combing education and income) was related to health status (57).
Based on these findings, we can draw some implications about the development of depression among Chinese immigrants. First, acculturative stress and reported health status are two main contributors to depressive symptoms and act partially independently, which supports the first hypothesis. Second, acculturation is primarily indirectly and negatively related to depressive symptoms. Third, higher income is related to less acculturative stress, and constitutes a major confounding factor in evaluating the association between acculturation and depression. Fourth, availability of people on whom one can rely (social support) may reduce the severity of depression. Lastly, meditative processes are important components in thinking about interventions in reducing depression.
Strengths
This study has several contributions to the existing literature. First, it explored the role of acculturation and health status and its association with depressive symptoms and used particularly rigorous statistical procedures to demonstrate moderation. It was based on two sampling frames, one with a representative sample of the community and the other a non-probability sample that, on testing, demonstrated general agreement in structural equations. The results indicated that the effect of acculturation on depressive symptoms is primarily indirect, which is consistent with previous studies (57), and it also indicated that higher acculturation was associated with less depressive symptoms among older and first-generation Chinese immigrants. Second, this study also disentangled the effect of confounding factors such as education and income on associations between stress, health status and depressive symptoms. Our results implied that income level was only associated with acculturative stress, while education mainly had effect on health status, thus clarifying that separate components of SES may have different pathways on influence of depressive symptoms.
Limitations
First, in the absence of variables enabling clear identification of the equations required to estimate feedback, a simpler recursive path model was assumed in this cross sectional data set so that evidence of causality is weaker than it would be in a longitudinal or experimental study. Second, the sampling procedure proved particularly difficult to execute since the Chinese population in greater Los Angeles, while numerically large, constitutes a relatively a small proportion of the total population in any telephone exchange. This necessitated a dual sampling frame using surname probability sampling of listed numbers and a second frame involving non-probability sampling of others (45), a procedure that limits estimation of population parameters. Replicating the analyses among the participants in each of the two frames, however, supported the general conclusions. This study, moreover, focused on testing hypotheses rather than estimating population parameters. Finally, our secondary analysis of data collected for other purposes did not include direct measures of other stressors, such as hassles of daily life. However, the measure of stress was designed specifically to tap a variety of stressors that affect immigrants directly. Conclusions. In order to reduce depression among Chinese immigrants, community-based intervention should target less acculturated, lower income, persons without social support, those with physical infirmities, and elder populations.
Data in this study suggest that health practitioners should focus attention not only on pharmaceutical interventions but also on the environmental situations in which immigrants find themselves (60,61). Clearly, success in America as indicated by education, money, language, citizenship, and other variables making life easier are expected to reduce stress and, consequently, diminish depressive symptoms. So too does time, but time is also related to aging and the infirmities of age are often non-manipulatable within the current health care delivery system. Attention should be paid to involving other social agencies in rectifying problems that immigrants confront, including economic problems, social isolation, citizenship uncertainty, lack of social support, and physical health in order to reduce depressive symptoms.
Comparative studies involving different groups of immigrants living under varying social conditions will expand understanding of the situations associated with depressive symptoms among immigrants from different cultures, situations, and immediate problems of life, as Iris Chang and Min Zhou describes in her studies of Chinese immigration to America (17,30). It is likely that immigrant stress and ill health are common denominators of depression, but attention should be directed at the manipulatable correlates of such stress and possible types of intervention to address these factors to greatly improve the ability to improve immigrant health.
Acknowledgments
This project was supported by a grant to C. Richard Hofstetter, 1RC1AA018970-01, from NIH/NIAAA 09/28/09 – 08/31/11 and extramural support from the Center for Behavioral Epidemiology and Community Health. We would like to thank David Strong, Department of Family and Preventive Medicine, University of California at San Diego, for helpful comments on the mss. Statistical tables and a path diagram are available from the second author on request.
Footnotes
Conflicts of interest: None.
All procedures and translations were approved by the San Diego State University Institutional Review Board.
Contributor Information
Yueling Li, Center for Behavioral Epidemiology and Community Health, 9245 Sky Park Ct, Ste 230, San Diego, CA 92123-4388 (858) 505-4770.
C. Richard Hofstetter, Center for Behavioral Epidemiology and Community Health, 9245 Sky Park Ct, Ste 230, San Diego, CA 92123-4388 (858) 505-4770.
Veronica Irving, Center for Behavioral Epidemiology and Community Health, 9245 Sky Park Ct, Ste 230, San Diego, CA 92123-4388 (858) 505-4770.
Doug Chhay, Center for Behavioral Epidemiology and Community Health, 9245 Sky Park Ct, Ste 230, San Diego, CA 92123-4388 (858) 505-4770.
Melbourne F. Hovell, Center for Behavioral Epidemiology and Community Health, 9245 Sky Park Ct, Ste 230, San Diego, CA 92123-4388 (858) 505-4770
References
- 1.Dalla RL, DeFrain J, Johnson JM, Abbott DA. Strengths and challenges of new immigrant families: implications for research, education, policy, and service. Rowman & Littlefield; 2009. [Google Scholar]
- 2.Nations U. Statistics Division, D. o. E. a. S. A., United Nations, editor. United Nations demographic yearbook review: National reporting of international migration data. New York, NY: 2004. [Google Scholar]
- 3.MPI Data Hub. 2010. Migration Facts, Stats, And Maps. Foreign-Born Population and Foreign Born as Percentage of the Total US Population, 1850 to 2009. [Google Scholar]
- 4.Chen EWC. Encyclopedia of Asian American Issues Today. Greenwood Pub Group; 2010. [Google Scholar]
- 5.Hwang WC, Myers HF, Takeuchi DT. Psychosocial predictors of first-onset depression in Chinese Americans. Soc Psychiatry Psychiatr Epidemiol. 2000;35:133–145. doi: 10.1007/s001270050196. [DOI] [PubMed] [Google Scholar]
- 6.Mui AC, Kang SY. Acculturation stress and depression among Asian immigrant elders. Soc Work. 2006;51:243–255. doi: 10.1093/sw/51.3.243. [DOI] [PubMed] [Google Scholar]
- 7.Beiser M, Hamilton H, Rummens JA, Oxman-Martinez J, Ogilvie L, Humphrey C, Armstrong R. Predictors of emotional problems and physical aggression among children of Hong Kong Chinese, Mainland Chinese and Filipino immigrants to Canada. Soc Psychiatry Psychiatr Epidemiol. 2010;45:1011–1021. doi: 10.1007/s00127-009-0140-3. [DOI] [PubMed] [Google Scholar]
- 8.Yeh C, Inose M. Difficulties and coping strategies of Chinese, Japanese, and Korean immigrant students. Adolescence. 2002;37:69–82. [PubMed] [Google Scholar]
- 9.Shin HS, Han HR, Kim MT. Predictors of psychological well-being amongst Korean immigrants to the United States: a structured interview survey. Int J Nurs Stud. 2007;44:415–426. doi: 10.1016/j.ijnurstu.2006.04.007. [DOI] [PubMed] [Google Scholar]
- 10.Noh S, Kaspar V. Perceived discrimination and depression: moderating effects of coping, acculturation, and ethnic support. Am J Public Health. 2003;93:232–238. doi: 10.2105/ajph.93.2.232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hwang WC, Myers HF. Major depression in Chinese Americans: the roles of stress, vulnerability, and acculturation. Soc Psychiatry Psychiatr Epidemiol. 2007;42:189–197. doi: 10.1007/s00127-006-0152-1. [DOI] [PubMed] [Google Scholar]
- 12.Kuo BCH, Roysircar G. Predictors of Acculturation for Chinese Adolescents in Canada: Age of Arrival, Length of Stay, Social Class, and English Reading Ability. Journal of Multicultural Counseling and Development. 2004;32:12. [Google Scholar]
- 13.Mui AC, Kang SY. Acculturation stress and depression among Asian immigrant elders. Social Work. 2006;51:243–255. doi: 10.1093/sw/51.3.243. [DOI] [PubMed] [Google Scholar]
- 14.Aroian KJ, Norris AE, Tran TV, Schappler-Morris N. Development and psychometric evaluation of the Demands of Immigration Scale. Journal of Nursing Measurement. 1998;6:175–194. [PubMed] [Google Scholar]
- 15.John DD. Strengths and challenges of new immigrant families: implications for research, education, policy, and service. Rowman & Littlefield; 2009. [Google Scholar]
- 16.Miller AM, Chandler PJ. Acculturation, resilience, and depression in midlife women from the former Soviet Union. Nursing Research. 2002;51:26. doi: 10.1097/00006199-200201000-00005. [DOI] [PubMed] [Google Scholar]
- 17.Chang I. The Chinese in America: A narrative history. Penguin Group; USA: 2004. [Google Scholar]
- 18.Gee GC. A multilevel analysis of the relationship between institutional and individual racial discrimination and health status. American Journal of Public Health. 2002;92:615. doi: 10.2105/ajph.92.4.615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kuo BCH, Roysircar G. Predictors of acculturation for Chinese adolescents in Canada: Age of arrival, length of stay, social class, and English reading ability. Journal of Multicultural Counseling and Development. 2004;32:143–154. [Google Scholar]
- 20.Lai DW. Impact of culture on depressive symptoms of elderly Chinese immigrants. Can J Psychiatry. 2004;49:820–827. doi: 10.1177/070674370404901205. [DOI] [PubMed] [Google Scholar]
- 21.Beiser M, Hou F, Hyman I, Tousignant M. Poverty, family process, and the mental health of immigrant children in Canada. Am J Public Health. 2002;92:220–227. doi: 10.2105/ajph.92.2.220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sirin SR, Ryce P, Gupta T, Rogers-Sirin L. The role of acculturative stress on mental health symptoms for immigrant adolescents: a longitudinal investigation. Dev Psychol. 2013;49:736–748. doi: 10.1037/a0028398. [DOI] [PubMed] [Google Scholar]
- 23.Shen BJ, Takeuchi DT. A structural model of acculturation and mental health status among Chinese Americans. Am J Community Psychol. 2001;29:387–418. doi: 10.1023/A:1010338413293. [DOI] [PubMed] [Google Scholar]
- 24.Jang Y, Kim G, Chiriboga DA. Gender differences in depressive symptoms among older Korean American immigrants. Social work in public health. 2011;26:96–109. doi: 10.1080/10911350902987003. [DOI] [PubMed] [Google Scholar]
- 25.Miller AM, Sorokin O, Fogg L. Individual, family, social, and cultural predictors of depressed mood in former soviet immigrant couples. Res Nurs Health. 2013;36:271–283. doi: 10.1002/nur.21535. [DOI] [PubMed] [Google Scholar]
- 26.Miszkurka M, Goulet L, Zunzunegui MV. Contributions of immigration to depressive symptoms among pregnant women in Canada. Canadian journal of public health = Revue canadienne de sante publique. 2010;101:358–364. doi: 10.1007/BF03404853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Alegria M, Canino G, Stinson FS, Grant BF. Nativity and DSM-IV psychiatric disorders among Puerto Ricans, Cuban Americans, and non-Latino Whites in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry. 2006;67:56–65. doi: 10.4088/jcp.v67n0109. [DOI] [PubMed] [Google Scholar]
- 28.Alegria M, Canino G, Shrout PE, Woo M, Duan N, Vila D, Torres M, Chen CN, Meng XL. Prevalence of mental illness in immigrant and non-immigrant U.S. Latino groups. Am J Psychiatry. 2008;165:359–369. doi: 10.1176/appi.ajp.2007.07040704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lee AA, Ellenbecker CH. The perceived life stressors among elderly Chinese immigrants: are they different from those of other elderly Americans? Clinical excellence for nurse practitioners: the international journal of NPACE. 1998;2:96–101. [PubMed] [Google Scholar]
- 30.Zhou M. Contemporary Chinese America: Immigration, ethnicity, and community transformation. Temple University Press; 2009. [Google Scholar]
- 31.Maes S, Leventhal H, de Ridder DTD. Coping with chronic diseases 1996 [Google Scholar]
- 32.Folkman S, Lazarus RS, Dunkel-Schetter C, DeLongis A, Gruen RJ. Dynamics of a stressful encounter: Cognitive appraisal, coping, and encounter outcomes. Journal of Personality and Social Psychology; Journal of Personality and Social Psychology. 1986;50:992. doi: 10.1037//0022-3514.50.5.992. [DOI] [PubMed] [Google Scholar]
- 33.Lazarus RS, Folkman S. Coping and adaptation. The handbook of behavioral medicine. 1984:282–325. [Google Scholar]
- 34.Mui AC, Burnette JD. A comparative profile of frail elderly persons living alone and those living with others. Journal of Gerontological Social Work. 1994;21:5–26. [Google Scholar]
- 35.Berry JW. Acculturation as varieties of adaptation. Acculturation: Theory, models and some new findings. 1980:9–25. [Google Scholar]
- 36.Gonidakis F, Korakakis P, Ploumpidis D, Karapavlou DA, Rogakou E, Madianos MG. The relationship between acculturation factors and symptoms of depression: A cross-sectional study with immigrants living in Athens. Transcultural psychiatry. 2011;48:437–454. doi: 10.1177/1363461511408493. [DOI] [PubMed] [Google Scholar]
- 37.Berry JW. Psychology of acculturation. 1990 [PubMed] [Google Scholar]
- 38.Hooyman NR, Kiyak HA. Social gerontology: A multidisciplinary perspective. Allyn & Bacon; 2008. [Google Scholar]
- 39.Golding JM, Burnam MA. Immigration, stress, and depressive symptoms in a Mexican-American community. Journal of Nervous and Mental Disease. 1990;178:161–171. doi: 10.1097/00005053-199003000-00003. [DOI] [PubMed] [Google Scholar]
- 40.Lee HY, Moon A, Knight BG. Depression among elderly Korean immigrants. Journal of Ethnic and Cultural Diversity in Social Work. 2005;13:1–26. [Google Scholar]
- 41.Stein M, Miller AH, Trestman RL. Depression, the immune system, and health and illness: findings in search of meaning. Archives of General Psychiatry. 1991;48:71. doi: 10.1001/archpsyc.1991.01810260079012. [DOI] [PubMed] [Google Scholar]
- 42.Mui AC. Depression among elderly Chinese immigrants: an exploratory study. Soc Work. 1996;41:633–645. [PubMed] [Google Scholar]
- 43.John DA, de Castro AB, Martin DP, Duran B, Takeuchi DT. Does an immigrant health paradox exist among Asian Americans? Associations of nativity and occupational class with self-rated health and mental disorders. Social science & medicine. 2012;75:2085–2098. doi: 10.1016/j.socscimed.2012.01.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hofstetter CR. Understanding Networking and Alcohol Consumption among Recent Immigrants. NIAAA; San Diego: 2009–2011. [Google Scholar]
- 45.Hu SS, Balluz L, Battaglia MP, Frankel MR. Improving public health surveillance using a dual-frame survey of landline and cell phone numbers. American journal of epidemiology. 2011;173:703. doi: 10.1093/aje/kwq442. [DOI] [PubMed] [Google Scholar]
- 46.Sasao T. Using surname - based telephone survey methodology in Asian - American communities: Practical issues and caveats. Journal of Community Psychology. 1994;22:283–295. [Google Scholar]
- 47.Choi BCK, Hanley J, Holowaty EJ, Dale D. Use of surnames to identify individuals of Chinese ancestry. American journal of epidemiology. 1993;138:723–734. doi: 10.1093/oxfordjournals.aje.a116910. [DOI] [PubMed] [Google Scholar]
- 48.Tjam EY. How to find Chinese research participants: use of a phonologically based surname search method. Canadian journal of public health. Revue canadienne de sante publique. 2001;92:138. doi: 10.1007/BF03404948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Rosenwaike I. Surname analysis as a means of estimating minority elderly. Research on Aging. 1994;16:212–227. [Google Scholar]
- 50.Wang W. The Rise of Intermarriage. Rates, Characteristics Vary by Race and Gender. Washington, DC: Pew Social & Demographic Trends; 2012. Feb, http://www.pewsocialtrends.org/2012/02/16/the-rise-of-intermarriage. [Google Scholar]
- 51.Radloff LS. the Ces-D scale. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- 52.Cole JC, Rabin AS, Smith TL, Kaufman AS. Development and validation of a Rasch-derived CES-D short form. Psychological Assessment. 2004;16:360. doi: 10.1037/1040-3590.16.4.360. [DOI] [PubMed] [Google Scholar]
- 53.Ding D, Hofstetter CR, Norman GJ, Irvin VL, Chhay D, Hovell MF. Measuring immigration stress of first-generation female Korean immigrants in California: psychometric evaluation of Demand of Immigration Scale. Ethnicity & Health. 2011;16:11–24. doi: 10.1080/13557858.2010.523107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Baum A, Posluszny DM. Health psychology: mapping biobehavioral contributions to health and illness. Annual Review of Psychology. 1999;50:137–163. doi: 10.1146/annurev.psych.50.1.137. [DOI] [PubMed] [Google Scholar]
- 55.Suinn RM, Knoo G, Ahuna C. The Suinn-Lew Asian Self-Identify Acculturation Scale: Cross-cultural information. Journal of Multicultural Counseling and Development 1995 [Google Scholar]
- 56.Suinn RM, Rickard-Figueroa K, Lew S, Vigil P. The Suinn-Lew Asian Self-Identity Acculturation Scale (SL-ASIA) Educational and Psychological Measurement. 1987;47:401–407. [Google Scholar]
- 57.Shen BJ, Takeuchi DT. A structural model of acculturation and mental health status among Chinese Americans. American Journal of Community Psychology. 2001;29:387–418. doi: 10.1023/A:1010338413293. [DOI] [PubMed] [Google Scholar]
- 58.Mui AC, Domanski MD. A community needs assessment among Asian American elders. Journal of Cross-Cultural Gerontology. 1999;14:77–90. doi: 10.1023/a:1006652809763. [DOI] [PubMed] [Google Scholar]
- 59.Han B. Depressive symptoms and self-rated health in community-dwelling older adults: a longitudinal study. J Am Geriatr Soc. 2002;50:1549–1556. doi: 10.1046/j.1532-5415.2002.50411.x. [DOI] [PubMed] [Google Scholar]
- 60.Hovell M, Wahlgren D, Adams M. The logical and empirical basis for the behavioral ecological model. Emerging theories in health promotion practice and research. 2009:2. [Google Scholar]
- 61.Glass TA, McAtee MJ. Behavioral science at the crossroads in public health: extending horizons, envisioning the future. Social science & medicine. 2006;62:1650–1671. doi: 10.1016/j.socscimed.2005.08.044. [DOI] [PubMed] [Google Scholar]