Abstract
Few studies have focused on injuries from the World Trade Center disaster on September 11, 2001. Severe injury has health consequences, including an increased mortality risk 10 years after injury and the risk of mental health problems, such as posttraumatic stress disorder (PTSD). The World Trade Center Health Registry identified 14,087 persons with none of a selected group of preexisting chronic conditions before 2002 who were present during and soon after the World Trade Center attacks, 1,980 of whom reported sustaining 1 or more types of injury (e.g., a broken bone or burn). Survey data obtained during 2003−2004 and 2006−2007 were used to assess the odds of reporting a diagnosis of chronic conditions (heart disease, respiratory disease, diabetes, cancer) up to 5–6 years after the attacks. Number of injury types and probable PTSD were significantly associated with having any chronic conditions diagnosed in 2002–2007. Persons with multiple injuries and PTSD had a 3-fold higher risk of heart disease than did those with no injury and no PTSD, and persons with multiple injuries and with no PTSD had a 2-fold higher risk of respiratory diseases. The present study shows that injured persons with or without comorbid PTSD have a higher risk of developing chronic diseases. Clinicians should be aware of the heightened risk of chronic heart and respiratory conditions among injured persons.
Keywords: chronic conditions, disasters, injury, posttraumatic stress disorder, 9/11 World Trade Center attacks
The terrorist attacks on the World Trade Center (WTC) in New York City on September 11, 2001 (hereafter referred to as 9/11) left more than 2,700 people dead and thousands injured. The collapse of the 2 WTC towers and resulting destruction of/damage to dozens of nearby buildings created a massive cloud of dust and debris that was a source of immediate injury to evacuees and led to a large burden of disaster-related illnesses. In the ensuing decade, numerous studies of survivors and rescue workers have reported increased exposure-related risks of asthma and other respiratory diseases, gastroesophageal reflux disease symptoms, sarcoidosis, and other physical health outcomes, as well as posttraumatic stress disorder (PTSD) and depression that persisted at least 6 years after the event (1–4). Recent reports of increased cardiovascular disease incidence (5) and related deaths (6), as well as those of observed increased rates of prostate and thyroid cancer and multiple myeloma among rescue/recovery workers (7), have raised concerns about the possible emergence of 9/11-related chronic diseases as the exposed population ages, although surveillance and detection biases may underlie some of these findings.
Although chronic disease studies have focused on exposures to toxic elements in the initial dust cloud (e.g., silica, polycyclic aromatic hydrocarbons, heavy metals (8)), as well as other recovery- and cleanup-related exposures (9), a growing body of literature on the potential long-term impact of injuries on chronic diseases and general health (10–15) and on the large number of injuries reported by building evacuees (16) and other survivors (17) motivated us to examine 9/11-related injuries as possible predictors of subsequent chronic disease.
Studies of injuries, including those resulting from disasters, primarily examine injury as an outcome (18–20). For example, factors identified as causes of injury among survivors of the 1995 bombing of a federal building in Oklahoma City included flying glass and window blinds (20). Studies of some disasters have found that injury was a risk factor for the later development of mental health conditions. For instance, among survivors of the Oklahoma City bombing, persons with injuries had a significantly higher rate of PTSD than did those without injuries (21), and in a sample of survivors of the 1998 US embassy bombings in East Africa, injury was the only factor significantly associated with posttraumatic stress reactions (22). With regard to physical health, one study suggested that there was an association between injury and medically unexplained symptoms among survivors of an explosion at a fireworks depot in Enschede, Netherlands (23).
Outside of disaster literature, decrements in health reported among severely injured persons have included elevated mortality rate (11), poor self-rated health (14), higher levels of functional limitations (13), and absenteeism (12). Most data on long-term effects of serious injury on health are based on psychometric (e.g., SF-36) or preference (e.g., Quality of Well-being) measures of health (24, 25). Researchers have also shown that up to 30% of severely injured patients develop PTSD or clinical depression within the first year after injury (26). In addition, in persons who experience multiple injury events over a period of time, the number of prior injury events was significantly associated with self-reported depression up to 10 years after the last injury (14).
Two recent studies found that potentially traumatic events or childhood psychosocial adversities were significant risk factors for adverse physical health and that these associations occurred in the absence of mental health disorders, including PTSD (10, 15). This is in contrast to the interpretation of evidence that traumatic events such as injury increase the risk of adverse physical outcomes only when PTSD develops as a result of the traumatic event (27). In one study, lifetime adult traumatic events, including injuries, had a significant association with osteoarthritis independent of PTSD (15), and in another, childhood adversities, including physical abuse and family violence, were associated with a range of diagnosed adult physical conditions, including heart disease, asthma, diabetes, osteoarthritis, chronic spinal pain, and severe headaches. In both studies, the level of risk was also a function of the number of adversities experienced.
The World Trade Center Health Registry, a longitudinal cohort of survivors of the September 11 disaster, provides an opportunity to assess whether there is a possible relationship between 9/11-related injury and emerging chronic health conditions and to what extent PTSD contributes to any association. We hypothesized that the likelihood of post-9/11 chronic health conditions increased as a function of injury severity, regardless of the magnitude of PTSD symptoms, and that injury amplified the impact of comorbid PTSD on post-9/11 conditions.
METHODS
The Registry monitors the short- and long-term physical and mental health of persons exposed to the WTC attacks on September 11 (1, 17). The sampling frame is the estimated 409,000 persons potentially exposed to the WTC disaster (28), including rescue/recovery workers at the WTC site, the Staten Island landfill, or the debris transport barge; residents of lower Manhattan; area workers; passersby on streets or subways; and students and staff of nearby schools from kindergarten to 12th grade. Registry participants were originally recruited through lists of potentially exposed persons provided by employers or other entities (list-identified), as well as through media and other outreach attempts and a toll-free number (self-identified). The Centers for Disease Control and Prevention and the New York City Health Department institutional review boards approved the Registry protocol.
The present analysis is based on a subset of adult enrollees who completed the Registry's wave 1 (n = 68,674) and wave 2 (n = 46,602; 68% response rate) surveys. Wave 1 was conducted from September 2003 to November 2004 and wave 2 from November 2006 to January 2008. Most (95%) participants in wave 1 were interviewed via computer-assisted telephone interviewing, with the remainder assessed via in-person interviews; wave 2 used 2 self-administered modes (via the Internet and mail) in addition to computer-assisted telephone interviewing. To limit this analysis to persons who were the most at risk for a 9/11-related injury, we excluded persons who were not present south of Chambers Street in lower Manhattan on the morning of September 11 (n = 18,823). We also excluded persons who were older than 64 years of age on September 11, 2001, to simplify the interpretation of findings related to the emergence of chronic conditions in an older population (n = 808). Persons who reported a diagnosis of a physical or mental health condition before 2002 in the wave 2 survey were excluded. After exclusions, 14,087 enrollees were available for analysis.
Study variables
Wave 1 respondents specified whether they sustained 1 or more of the following types of injury on September 11: cut, abrasion, or puncture wound; sprain or strain; burn; broken bone (fracture) or dislocation; and concussion/head injury/knocked out by being hit on the head. In the present analysis, “number of injury types” is the count of the number of different types of 9/11-related injuries reported by the enrollee at wave 1. We consider this measure to be a crude surrogate for severity. Having a second or third injury increases the severity of the overall injury (29), and persons with multiple injuries have longer hospital stays and more intensive care (30).
Reporting of diagnosis and year during which physical and mental health conditions were diagnosed was based on the following wave 2 questions: “Have you ever been told by a doctor or other health professional that you had any of these conditions?” and “What year were you first told by a doctor or other health professional that you had this condition?” Self-reported diagnosed physical conditions in the study population during 2002–2007 included respiratory conditions (asthma (6.0%), chronic bronchitis (4.7%), emphysema (0.6%), reactive airway disease (1.3%), and other lung conditions (1.8%)), heart disease (angina (0.6%), heart attack (0.6%), and other heart conditions (2.6%)), and other conditions (stroke (0.1%), diabetes (2.9%), sarcoidosis (0.3%), and cancer (2.8%)). We chose to examine this set of conditions because they underlie self-rated poor health (31) and because of the association between self-rated health and mortality risk (32). We separately examined respiratory and heart diseases because heart diseases are the most common chronic conditions in the United States and respiratory diseases are the most prevalent 9/11-related conditions (6).
Exposure to the dust/debris cloud was classified as intense or some/none. Intense exposure was defined as being caught in the dust/debris cloud on September 11 and reporting having at least 1 of 5 experiences: being unable to see more than a couple of feet; having trouble walking or finding the way; finding shelter, such as under a car; being covered head to toe with dust; or not being able to hear.
We included the presence or absence of probable PTSD at wave 1 as a risk factor for having a chronic condition diagnosed during 2002–2007. Probable PTSD was assessed at wave 1 using a 17-item 9/11-specific PTSD checklist (33). Instructions also specified 9/11 as the index event. Each stressor-specific item, such as “feeling very upset when something reminded you of the events of 9/11,” was scored on a 5-point scale for experience of the symptom during the past 30 days. A PTSD checklist score of 44 or greater is indicative of probable PTSD, with a reported sensitivity of 0.78 and a specificity of 0.97 (34).
Data analysis
Descriptive analysis was done for any injury and types of injury by demographic characteristics, dust/debris cloud exposure, smoking status, PTSD at wave 1, and chronic conditions reportedly diagnosed during 2002–2007. Unconditional logistic regression models were used to estimate odds ratios and their 95% confidence intervals for the associations with factors by which the prevalence of diagnosed chronic conditions during 2002–2007 vary, including sociodemographic characteristics (sex, age, educational level, race/ethnicity), smoking (current, former, never), history of hypertension (before and after 2002), and WTC disaster–related characteristics, such as whether an enrollee was a rescue/recovery worker or had dust/debris cloud exposure. Associations of number of injury types and probable PTSD with chronic conditions were assessed via 3 separate multivariable models using: 1) injury and PTSD as separate variables; 2) a single composite variable for number of injury types with and without PTSD; and 3) a pooled model that tested for multiplicative interaction between number of injury types and PTSD. All analyses were conducted using SAS software, version 9.1.3 (SAS Institute, Inc., Cary, North Carolina).
RESULTS
Of the 14,087 enrollees in the analysis sample, 1,980 (14%) reported at least 1 type of injury on September 11 (Table 1). Compared with subjects who reported having no injury, those who reported any injury were more likely to be male (69% vs. 59%) and a rescue or recovery worker (49% vs. 21%). They were also more likely to have experienced an intense dust cloud exposure (69% vs. 38%) and to have had PTSD at wave 1 (22% vs. 10%). Half again as many reported a chronic condition diagnosed during 2002–2007 (25% of those with any injury vs. 16% of those with no injury).
Table 1.
Characteristicsa of Study Sample and Persons Reporting Any Injury on September 11, 2001, World Trade Center Health Registry, 2003–2007
| Characteristic | All |
Any Injuryb |
No Injury |
|||
|---|---|---|---|---|---|---|
| No. | % | No. | % | No. | % | |
| Wave 1 mode of recruitment | 14,087 | 100.0 | 1,980 | 100.0 | 12,107 | 100.0 |
| List identified | 2,810 | 19.9 | 296 | 14.9 | 2,514 | 20.8 |
| Self identified | 11,277 | 80.1 | 1,684 | 85.1 | 9,593 | 79.2 |
| Wave 2 survey mode | ||||||
| 5,516 | 39.2 | 838 | 42.3 | 4,678 | 38.6 | |
| CATI | 1,835 | 13.0 | 235 | 11.9 | 1,600 | 13.2 |
| Web | 6,736 | 47.8 | 907 | 45.8 | 5,829 | 48.1 |
| Sex | ||||||
| Female | 5,637 | 40.0 | 617 | 31.2 | 5,020 | 41.5 |
| Male | 8,450 | 60.0 | 1,363 | 68.8 | 7,087 | 58.5 |
| Age at wave 1 interview, years | ||||||
| 18–24 | 348 | 2.5 | 13 | 0.7 | 335 | 2.8 |
| 25–44 | 6,605 | 46.9 | 950 | 48.0 | 5,655 | 46.7 |
| 45–54 | 4,410 | 31.3 | 698 | 35.3 | 3,712 | 30.7 |
| ≥55 | 2,724 | 19.3 | 319 | 16.1 | 2,405 | 19.9 |
| Race/ethnic group | ||||||
| Non-Hispanic black | 1,726 | 12.3 | 219 | 11.1 | 1,507 | 12.4 |
| Hispanic | 1,509 | 10.7 | 251 | 12.7 | 1,258 | 10.4 |
| Asian | 972 | 6.9 | 97 | 4.9 | 875 | 7.2 |
| Other | 388 | 2.8 | 60 | 3.0 | 328 | 2.7 |
| Non-Hispanic white | 9,492 | 67.4 | 1,353 | 68.3 | 8,139 | 67.2 |
| Educational attainment | ||||||
| Less than high school or high school | 2,313 | 16.4 | 384 | 19.4 | 1,929 | 15.9 |
| Some college | 3,155 | 22.4 | 603 | 30.5 | 2,552 | 21.1 |
| College/postgraduate | 8,536 | 60.6 | 979 | 49.4 | 7,557 | 62.4 |
| Rescue/recovery worker | ||||||
| Yes | 3,471 | 24.6 | 975 | 49.2 | 2,496 | 20.6 |
| No | 10,616 | 75.4 | 1,005 | 50.8 | 9,611 | 79.4 |
| Smoking status at wave 1 or wave 2 | ||||||
| Former smoker | 3,777 | 26.8 | 512 | 25.9 | 3,265 | 27.0 |
| Current smoker | 1,768 | 12.6 | 289 | 14.6 | 1,479 | 12.2 |
| Never smoker | 8,449 | 60.0 | 1,165 | 58.8 | 7,284 | 60.2 |
| Dust/debris cloud exposure on 9/11 | ||||||
| Intense dust cloud | 5,987 | 42.5 | 1,363 | 68.8 | 4,624 | 38.2 |
| Some/none | 7,597 | 53.9 | 555 | 28.0 | 7,042 | 58.2 |
| Number of injury types | ||||||
| 1 | 1,468 | 10.4 | 1,468 | 74.1 | 0 | 0.0 |
| 2 | 421 | 3.0 | 421 | 21.3 | 0 | 0.0 |
| ≥3 | 91 | 0.6 | 91 | 4.6 | 0 | 0.0 |
| No injuries | 12,107 | 85.9 | 0 | 0.0 | 12,107 | 100.0 |
| Probable PTSD at wave 1 | ||||||
| Yes | 1,586 | 11.3 | 426 | 21.5 | 1,160 | 9.6 |
| No | 12,124 | 86.1 | 1,507 | 76.1 | 10,617 | 87.7 |
| ≥1 chronic physical conditions diagnosed in 2002–2007c | ||||||
| Yes | 2,474 | 17.6 | 495 | 25.0 | 1,979 | 16.3 |
| No | 11,613 | 82.4 | 1,485 | 75.0 | 10,128 | 83.7 |
Abbreviations: CATI, computer-assisted telephone interviewing; PTSD, posttraumatic stress disorder.
a Denominator for percent includes persons with missing data.
b Any injury includes cut, abrasion, or puncture wound; sprain or strain; burn; broken bone (fracture) or dislocation; and concussion/head injury/knocked out by being hit on the head.
c Chronic physical conditions include: angina, heart attack, other heart conditions, stroke, asthma, chronic bronchitis, emphysema, reactive airway disease syndrome, other lung conditions, diabetes, and cancer.
Table 2 displays the number of injury types by selected factors and is organized by frequency of reported injuries as follows: cut/abrasion (n = 1,098), sprain/strain injuries (n = 1,019), burns (n = 211), broken bones (n = 81), and head injuries (n = 69) (Table 2). Having multiple types of injury was most common among those with a broken bone/fracture (81%) or head injury, including concussion (86%). Probable PTSD was also most common among persons with a broken bone or head injury (38% for broken bone/fracture and 41% for head injury). Intense dust cloud exposure was most common among those with a head injury (83%) compared with other types of injuries.
Table 2.
Categories of Type of Injury Sustained on September 11, 2001, by Selected Factors, World Trade Center Health Registry, 2003–2007
| Factora | Type of Injury |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Cut, Abrasion, or Puncture Wound |
Sprain/Strain |
Burn |
Broken Bone (Fracture) or Dislocation |
Concussion/Head Injury/Knocked Out by Being Hit on the Head |
||||||
| No. of Cases | % | No. of Cases | % | No. of Cases | % | No. of Cases | % | No. of Cases | % | |
| All | 1,098 | 100.0 | 1,019 | 100.0 | 211 | 100.0 | 81 | 100.0 | 69 | 100.0 |
| Number of injury types reported | ||||||||||
| 1 | 667 | 60.7 | 611 | 60.0 | 79 | 37.4 | 15 | 18.5 | 10 | 14.5 |
| 2 | 346 | 31.5 | 324 | 31.8 | 83 | 39.3 | 30 | 37.0 | 19 | 27.5 |
| ≥3 | 85 | 7.7 | 84 | 8.2 | 49 | 23.2 | 36 | 44.4 | 40 | 58.0 |
| PTSD at wave 1 | ||||||||||
| Yes | 214 | 19.5 | 258 | 25.3 | 61 | 28.9 | 31 | 38.3 | 28 | 40.6 |
| No | 884 | 80.5 | 761 | 74.7 | 150 | 71.1 | 50 | 61.7 | 41 | 59.4 |
| Dust/debris cloud exposure on 9/11 | ||||||||||
| Intense dust cloud | 852 | 77.6 | 689 | 67.6 | 166 | 78.7 | 65 | 80.2 | 57 | 82.6 |
| Some/none | 246 | 22.4 | 330 | 32.4 | 45 | 21.3 | 16 | 19.8 | 12 | 17.4 |
Abbreviation: PTSD, posttraumatic stress disorder.
a Denominator for percent includes persons with missing data.
Table 3 shows the results of multivariable logistic regression for any chronic conditions during 2002–2007. After adjustment, being female, 45–54 years of age, a rescue/recovery worker, and a former smoker and having less than a college education, reporting diagnosed hypertension, and having intense dust/debris cloud exposure were significantly associated with reporting 1 or more chronic conditions.
Table 3.
Prevalence, Crude, and Adjusted Odds Ratios for Having 1 or More Diagnosed Chronic Conditionsa, World Trade Center Health Registry, 2003–2007
| Characteristicb | No. | % | cOR | 95% CI | aORc | 95% CI |
|---|---|---|---|---|---|---|
| All | 2,474 | 100.0 | ||||
| Sex | ||||||
| Female | 980 | 39.6 | 1.0 | 0.9, 1.1 | 1.2 | 1.1, 1.4 |
| Male | 1,494 | 60.4 | 1.0 | Referent | 1.0 | Referent |
| Age at wave 1 interview, years | ||||||
| 18–24 | 29 | 1.2 | 0.6 | 0.4, 0.8 | 0.5 | Referent |
| 25–44 | 929 | 37.6 | 1.0 | Referent | 1.0 | |
| 45–54 | 890 | 36.0 | 1.5 | 1.4, 1.7 | 1.4 | 1.3, 1.6 |
| ≥55 | 626 | 25.3 | 1.8 | 1.6, 2.1 | 1.7 | 1.5, 2.0 |
| Race/ethnicity group | ||||||
| Non-Hispanic black | 340 | 13.7 | 1.2 | 1.1, 1.4 | 1.0 | 0.8, 1.1 |
| Hispanic | 315 | 12.7 | 1.3 | 1.1, 1.5 | 1.1 | 1.0, 1.3 |
| Asian | 150 | 6.1 | 0.9 | 0.8, 1.1 | 1.1 | 0.9, 1.4 |
| Other | 76 | 3.1 | 1.2 | 0.9, 1.6 | 1.2 | 0.9, 1.6 |
| Non-Hispanic white | 1,593 | 64.4 | 1.0 | Referent | 1.0 | Referent |
| Educational attainment | ||||||
| Less than high school or high school | 474 | 19.2 | 1.5 | 1.3, 1.7 | 1.2 | 1.0, 1.3 |
| Some college | 717 | 29.0 | 1.7 | 1.5, 1.9 | 1.4 | 1.2, 1.5 |
| College/postgraduate | 1,267 | 51.2 | 1.0 | Referent | 1.0 | Referent |
| Rescue/recovery worker | ||||||
| Yes | 845 | 34.2 | 1.8 | 1.6, 2.0 | 1.7 | 1.5, 1.9 |
| No | 1,629 | 65.8 | 1.0 | Referent | 1.0 | Referent |
| Smoking status at wave 1 or wave 2 | ||||||
| Former smoker | 724 | 29.3 | 1.2 | 1.1, 1.3 | 1.1 | 1.0, 1.2 |
| Current smoker | 349 | 14.1 | 1.3 | 1.1, 1.4 | 1.1 | 0.9, 1.3 |
| Never smoker | 1,383 | 55.9 | 1.0 | Referent | 1.0 | Referent |
| Hypertension | ||||||
| Yes | 899 | 36.3 | 2.1 | 1.9, 2.3 | 1.8 | 1.6, 1.9 |
| No | 1,575 | 63.7 | 1.0 | Referent | 1.0 | Referent |
| Dust/debris cloud exposure on 9/11 | ||||||
| Intense dust cloud | 1,288 | 52.1 | 1.7 | 1.5, 1.8 | 1.4 | 1.2, 1.5 |
| Some/none | 1,081 | 43.7 | 1.0 | Referent | 1.0 | Referent |
| Number of injury types | ||||||
| 1 | 343 | 13.9 | 1.6 | 1.4, 1.8 | 1.2 | 1.0, 1.3 |
| 2 | 122 | 4.9 | 2.1 | 1.7, 2.6 | 1.3 | 1.0, 1.6 |
| ≥3 | 30 | 1.2 | 2.5 | 1.6, 3.9 | 1.6 | 1.0, 2.5 |
| Number of injury types | 1,979 | 80.0 | 1.0 | Referent | 1.0 | Referent |
| PTSD at wave 1 | ||||||
| Yes | 464 | 18.8 | 2.2 | 1.9, 2.4 | 1.7 | 1.5, 2.0 |
| No | 1,939 | 78.4 | 1.0 | Referent | 1.0 | Referent |
Abbreviations: aOR, adjusted odds ratio; CI, confidence interval; cOR, crude odds ratio; PTSD, posttraumatic stress disorder.
a Includes angina, heart attack, other heart conditions, stroke, asthma, chronic bronchitis, emphysema, reactive airway disease syndrome, other lung conditions, diabetes, and cancer.
b Denominator for percent includes persons with missing data.
c Multivariable model includes all the variables in the table.
Injury categories including 1 injury type (adjusted odds ratio (aOR) = 1.2, 95% confidence interval (CI): 1.0, 1.3), 2 injury types (aOR = 1.3, 95% CI: 1.0, 1.6), and 3 or more injury types (aOR = 1.6, 95% CI: 1.0, 2.5) (Table 3) were significantly associated with having chronic conditions diagnosed during 2002–2007 relative to no injuries, with a significant trend (P = 0.0043). After adjustment, probable PTSD at wave 1 was also significantly associated with having 9/11-related chronic conditions diagnosed (aOR = 1.7, 95% CI: 1.5, 2.0). In a separate multivariable pooled analysis with a cross-product of number of types of injuries and PTSD, there was a significant multiplicative interaction between number of types of injuries and probable PTSD (P = 0.04).
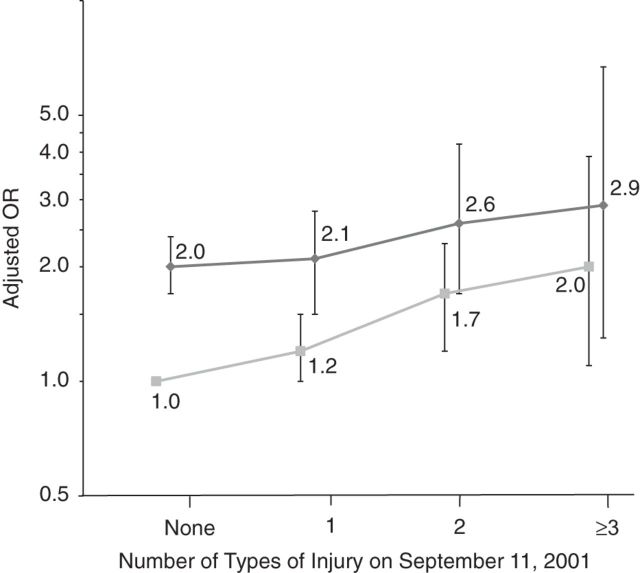
For respiratory disease, we found a dose-response relationship between number of injury types and occurrence of chronic conditions regardless of PTSD status (Table 4 and Figure 1). For instance, there was a significant trend for number of injury types without PTSD (P = 0.0026), with adjusted odds ratios ranging from 1.2 (95% CI: 1.0, 1.5) for 1 injury to 2.0 (95% CI: 1.1, 3.9) for 3 injuries relative to no injury and no PTSD. Among those with PTSD, the adjusted odds ratios ranged from 2.0 (95% CI: 1.7, 2.4) for no injury to 2.9 (95% CI: 1.3, 6.7) for 3 or more types of injuries, but the trend was not significant.
Table 4.
Association of Number of Types of Injury Sustained on September 11, 2001, Posttraumatic Stress Disorder, and Dust/Debris Cloud With Respiratory and Heart Diseases Diagnosed in 2002–2007, World Trade Center Health, 2003–2007
| Risk Factor | Respiratory Disease (Asthma, Chronic Bronchitis, Emphysema, Other Lung Problems, Reactive Airway Disease Syndrome) |
Heart Disease (Angina, Heart Attack, Other Heart Disease) |
||||
|---|---|---|---|---|---|---|
| No. of Cases | aOR | 95% CI | No. of Cases | aOR | 95% CI | |
| PTSD status | ||||||
| With PTSD | ||||||
| No injuries | 200 | 2.0 | 1.7, 2.4 | 79 | 2.4 | 1.8, 3.2 |
| 1 | 54 | 2.1 | 1.5, 2.8 | 17 | 2.2 | 1.3, 3.8 |
| 2 | 32 | 2.6 | 1.7, 4.2 | 10 | 3.3 | 1.6, 6.8 |
| ≥3 | 9 | 2.9 | 1.3, 6.7 | 3 | 2.9 | 0.8, 10.2 |
| Without PTSD | ||||||
| No injuries | 897 | 1.0 | Referent | 270 | 1.0 | Referent |
| 1 | 158 | 1.2 | 1.0, 1.5 | 51 | 1.6 | 1.2, 2.3 |
| 2 | 62 | 1.7 | 1.2, 2.3 | 15 | 1.5 | 0.8, 2.8 |
| ≥3 | 13 | 2.0 | 1.1, 3.9 | 3 | 1.8 | 0.5, 5.9 |
| Dust/debris exposure | ||||||
| Intense dust cloud | 805 | 1.5 | 1.3, 1.7 | 238 | 1.3 | 1.05, 1.6 |
| Some/none | 589 | 1.0 | Referent | 203 | 1.0 | Referent |
Abbreviations: aOR, adjusted odds ratio; CI, confidence interval; PTSD, posttraumatic stress disorder.
Figure 1.
Adjusted odds ratios (ORs) for the association of posttraumatic stress disorder (PTSD) and number of types of injury sustained on September 11, 2001, with diagnosed respiratory conditions in 2002–2007, World Trade Center Health Registry. Dark lines with diamonds indicate the presence of PTSD; gray lines with squares indicate the absence of PTSD. The reference category is no injury or PTSD. Bars, 95% confidence intervals.
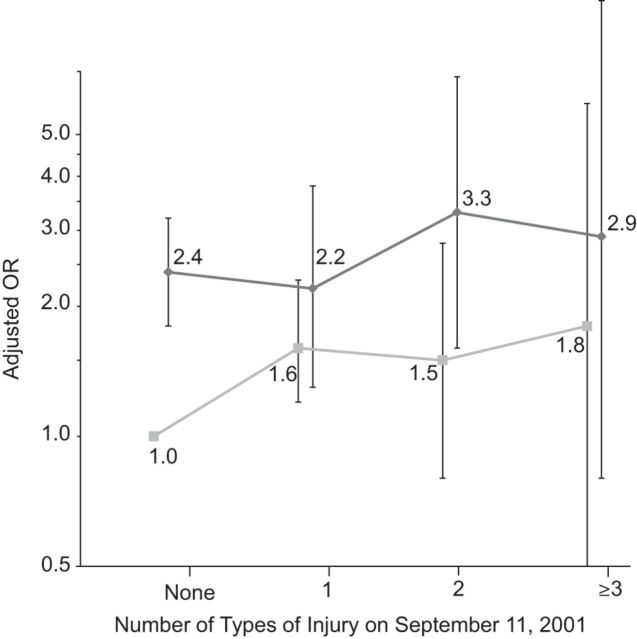
For heart disease, the number of injury types clearly had more impact in the presence of PTSD, with adjusted odds ratios ranging from 2.4 (95% CI: 1.8, 3.2) for PTSD and no injuries to 3.3 (95% CI: 1.6, 6.8) for 2 injury types relative to no injuries and no PTSD (Table 4 and Figure 2). Probably because of the small number of cases, only the adjusted odds ratio for 1 injury type without PTSD was significant (aOR = 1.6, 95% CI: 1.2, 2.3).
Figure 2.
Adjusted odds ratios (OR) for the association of posttraumatic stress disorder (PTSD) and number of types of injury sustained on September 11, 2001, with diagnosed heart diseases in 2002–2007, World Trade Center Health Registry. Dark lines with diamonds indicate the presence of PTSD; gray lines with squares indicate the absence of PTSD. The reference category is no injury or PTSD. Bars, 95% confidence intervals.
DISCUSSION
In a cohort of persons directly exposed to the WTC disaster, we confirmed the hypothesized associations among injury sustained on September 11, PTSD, and subsequent chronic disease. There was, for instance, a dose-response relationship between number of types of injury and diagnosed chronic conditions, including respiratory diseases. Importantly, the association between injury and adverse physical health was observed in the absence of probable PTSD, although the likelihood of post-2001 physical conditions increased multiplicatively among persons with probable PTSD with each additional type of injury. These results are consistent with recent reports in which adverse events (e.g., physical abuse) in either childhood or adulthood predicted diagnosed physical health conditions later in life independent of mental disorders, including PTSD (10, 15). The apparent indirect association between injury and physical chronic disease is consistent with studies of nondisaster injuries that have reported both direct and indirect adverse relationships between serious injury and self-rated poor health (14), functional limitations affecting life and work (35), and diminished quality of life (24) up to 10 years after the injury.
Sustaining an injury during a disaster like 9/11 would considerably heighten the life-threatening traumatic exposure, which could lead to PTSD. Biological stress reactions associated with PTSD can lead to an increased risk of disease, especially cardiovascular disease (36). After controlling for depression, Kubzansky et al. (37) reported a 30% increase in fatal heart disease among veterans who had a combat-related PTSD score that was 1 standard deviation higher than the norm. Earlier Registry analyses reported significant associations between PTSD and heart disease (5, 38).
In a sensitivity analysis, injury was significantly associated with post-9/11 chronic disease, even when the total PTSD checklist score was as low as 25 (for 3 or more types of injuries, aOR = 3.0, 95% CI: 1.0, 8.6). The finding of an association between injury and adverse physical health in the absence of probable PTSD is important because the indirect connection between injury and disease would be expected to be dependent on the presence of a stress-related disorder. For instance, there is a well-established relationship between PTSD and chronic heart disease, for which biologically plausible mechanisms have been proposed (36, 37). It is not so clear, however, how injury without higher levels of psychopathology of PTSD, for instance, could cause elevated adverse physical health effects. Nonetheless, it could be posited that prolonged stress symptoms associated with an injury, apart from PTSD, create a state of allostatic load, which is defined as a chronic chemical imbalance in the hormonal and neurotransmitter mediators of the stress response (39, 40).
The combination of evidence from studies on long-term effects of serious injuries on overall health (either self-rated health or mortality risk) (11, 14) and 2 recent studies reporting adverse physical health effects from childhood or adult adverse events (e.g., physical abuse) in the absence of mental disorders (10, 15) provides further support for an injury-induced adverse physical health effect. In the context of the present study, the studies by Keyes et al. (15) and Scott et al. (10) are especially relevant because they also included questions about physical health based on the Health Interview Survey (41). They found that the likelihood of an adverse physical health effect increased with the number of traumatic or adverse events after controlling for mental health disorders. However, they used a broad range of traumatic events that included physical injury and assaults, and on average there was a much longer period of time (decades in some instances) between the event and onset of illness.
In the present study, there was a dose-response relationship between injury and respiratory diseases regardless of probable PTSD. The strong association between injury and respiratory diseases may be the result of the joint impact of being injured on September 11 and experiencing 9/11 environmental exposures associated with lung problems, especially being in the vicinity of the WTC towers when they collapsed and being caught in the dust/debris cloud (16). Environmental pollutants in the dust/debris cloud, including combustion products, probably led to the development of acute and chronic respiratory conditions such as asthma (1). Although intense dust cloud exposure was statistically independent from the association of number of types of injury and PTSD on respiratory diseases after 2001, the 2 exposures are intertwined because at least 70% of persons with 1 of the 5 types of injury experienced an intense dust cloud. Both being caught in a dust/debris cloud and being injured on September 11 represent a likely intensified environmental exposure.
Being injured could also result in behavioral lifestyle changes and increased health-care utilization. Lifestyle changes can include starting smoking, increasing medication use (e.g., pain medication), and not exercising, which are themselves risk factors for some chronic diseases (24). We did find that a slightly higher proportion of persons injured on September 11 were current smokers compared with noninjured persons (15% vs. 12%). With regard to health-care utilization, injured and noninjured enrollees had similar frequencies of doctor visits for a routine checkup in the past year (68% vs. 65%), which suggests that surveillance bias is not a major factor for chronic disease diagnosis in the present study.
Strengths and limitations
An important strength of this study is that the Registry's sample size is sufficient to allow us to assess multiple types of injury and categories of chronic conditions. It also has a noninjured comparison group, which other studies of long-term health effects of injury typically do not have (26, 35, 42).
A study limitation is having incomplete information about injuries on September 11; we had no data on the body part injured, the severity of injury, whether the injury was treated in an emergency department or hospital, or the circumstances of the injury itself. In present analysis, we used number of types of injury as a surrogate for injury severity, assuming that a person with more than 1 type of injury (e.g., a laceration and burn) also has a more severe injury than did another with only a laceration or burn. This approach is supported by evidence that multiple injuries (more than 1 type of injury or injuries to different areas of the body) results in an increased risk of death and a longer hospital stay (30).
Second, key measures such as dust/debris cloud exposure, PTSD symptoms, and diagnosed chronic conditions were based on self-report, which is subject to various sources of bias (e.g., recall bias). Our confidence in self-reporting is strengthened by the agreement between Registry findings regarding the association between PTSD and heart disease based on self-report (5) and those based on hospitalization discharge (38) and mortality measures (6). Additionally, we did not observe an excess of diabetes or cancer cases with increased number of injuries independent of PTSD, which suggests that there was no general over-reporting of conditions by injured persons.
A third limitation is our lack of information on risk factors other than smoking for the chronic diseases used as outcomes in this analysis, such as weight and height (which could be used to compute body mass index) and family medical history. However, residual confounding applies to these risk factors as well as to 9/11 exposures, including dust cloud and rescue and recovery work.
Conclusion
The present study provides evidence to suggest that injury in itself is associated with long-term physical health outcomes independent of PTSD and that comorbid injury and PTSD have a potentially profound association with the development of heart disease. An important implication of this finding is that a significantly large group of survivors injured on September 11 may be vulnerable to subsequent chronic physical illness that is separate from the direct impact of being injured. Clinicians should be aware of the heightened risk of chronic heart and respiratory conditions among persons injured on September 11, 2001.
ACKNOWLEDGMENTS
Author affiliations: World Trade Center Health Registry, Division of Epidemiology, New York City Department of Health and Mental Hygiene, Long Island City, New York (Robert M. Brackbill, James E. Cone, Mark R. Farfel, Steven D. Stellman); and Department of Epidemiology, Mailman School of Public Health, Columbia University, New York, New York (Steven D. Stellman).
The study was supported by cooperative agreement U50/OH009739 from the National Institute for Occupational Safety and Health of the US Centers for Disease Control and Prevention; cooperative agreement U50/ATU272750 from the Agency for Toxic Substances and Disease Registry, which included support from the National Center for Environmental Health; and the New York City Department of Health and Mental Hygiene.
The contents of this article are solely the responsibility of the authors and do not necessarily represent the official views of Centers for Disease Control and Prevention.
Conflict of interest: none declared.
REFERENCES
- 1.Brackbill RM, Hadler JL, DiGrande L, et al. Asthma and posttraumatic stress symptoms 5 to 6 years following exposure to the World Trade Center terrorist attack. JAMA. 2009;302(5):502–516. doi: 10.1001/jama.2009.1121. [DOI] [PubMed] [Google Scholar]
- 2.Li J, Brackbill RM, Stellman SD, et al. Gastroesophageal reflux symptoms and comorbid asthma and posttraumatic stress disorder following the 9/11 terrorist attacks on World Trade Center in New York City. Am J Gastroenterol. 2011;106(11):1933–1941. doi: 10.1038/ajg.2011.300. [DOI] [PubMed] [Google Scholar]
- 3.Jordan HT, Stellman SD, Prezant D, et al. Sarcoidosis diagnosed after September 11, 2001, among adults exposed to the World Trade Center disaster. J Occup Environ Med. 2011;53(9):966–974. doi: 10.1097/JOM.0b013e31822a3596. [DOI] [PubMed] [Google Scholar]
- 4.Stellman JM, Smith RP, Katz CL, et al. Enduring mental health morbidity and social function impairment in world trade center rescue, recovery, and cleanup workers: the psychological dimension of an environmental health disaster. Environ Health Perspect. 2008;116(9):1248–1253. doi: 10.1289/ehp.11164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jordan HT, Miller-Archie SA, Cone JE, et al. Heart disease among adults exposed to the September 11, 2001 World Trade Center disaster: results from the World Trade Center Health Registry. Prev Med. 2011;53(6):370–376. doi: 10.1016/j.ypmed.2011.10.014. [DOI] [PubMed] [Google Scholar]
- 6.Jordan HT, Brackbill RM, Cone JE, et al. Mortality among survivors of the Sept 11, 2001, World Trade Center disaster: results from the World Trade Center Health Registry cohort. Lancet. 2011;378(9794):879–887. doi: 10.1016/S0140-6736(11)60966-5. [DOI] [PubMed] [Google Scholar]
- 7.Li J, Cone JE, Kahn AR, et al. Association between World Trade Center exposure and excess cancer risk. JAMA. 2012;308(23):2479–2488. doi: 10.1001/jama.2012.110980. [DOI] [PubMed] [Google Scholar]
- 8.Lioy PJ, Weisel CP, Millette JR, et al. Characterization of the dust/smoke aerosol that settled east of the World Trade Center (WTC) in lower Manhattan after the collapse of the WTC 11 September 2001. Environ Health Perspect. 2002;110(7):703–714. doi: 10.1289/ehp.02110703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Maslow CB, Friedman SM, Pillai PS, et al. Chronic and acute exposures to the world trade center disaster and lower respiratory symptoms: area residents and workers. Am J Public Health. 2012;102(6):1186–1194. doi: 10.2105/AJPH.2011.300561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Scott KM, Von Korff M, Angermeyer MC, et al. Association of childhood adversities and early-onset mental disorders with adult-onset chronic physical conditions. Arch Gen Psychiatry. 2011;68(8):838–844. doi: 10.1001/archgenpsychiatry.2011.77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cameron CM, Purdie DM, Kliewer EV, et al. Long-term mortality following trauma: 10 year follow-up in a population-based sample of injured adults. J Trauma. 2005;59(3):639–646. [PubMed] [Google Scholar]
- 12.Gillen M, Jewell SA, Faucett JA, et al. Functional limitations and well-being in injured municipal workers: a longitudinal study. J Occup Rehabil. 2004;14(2):89–105. doi: 10.1023/b:joor.0000018326.23090.63. [DOI] [PubMed] [Google Scholar]
- 13.Holtslag HR, Post MW, Lindeman E, et al. Long-term functional health status of severely injured patients. Injury. 2007;38(3):280–289. doi: 10.1016/j.injury.2006.10.026. [DOI] [PubMed] [Google Scholar]
- 14.Toft AM, Møller H, Laursen B. The years after an injury: long-term consequences of injury on self-rated health. J Trauma. 2010;69(1):26–30. doi: 10.1097/TA.0b013e3181d3cbf2. [DOI] [PubMed] [Google Scholar]
- 15.Keyes KM, McLaughlin KA, Demmer RT, et al. Potentially traumatic events and the risk of six physical health conditions in a population-based sample. Depress Anxiety. 2013;30(5):451–460. doi: 10.1002/da.22090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Brackbill RM, Thorpe LE, DiGrande L, et al. Surveillance for World Trade Center disaster health effects among survivors of collapsed and damaged buildings. MMWR Surveill Summ. 2006;55(2):1–18. [PubMed] [Google Scholar]
- 17.Farfel M, DiGrande L, Brackbill R, et al. An overview of 9/11 experiences and respiratory and mental health conditions among World Trade Center Health Registry enrollees. J Urban Health. 2008;85(6):880–909. doi: 10.1007/s11524-008-9317-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Knowles SB, Marshall SW, Bowling MJ, et al. Risk factors for injury among high school football players. Epidemiology. 2009;20(2):302–310. doi: 10.1097/EDE.0b013e318193107c. [DOI] [PubMed] [Google Scholar]
- 19.Graafmans WC, Ooms ME, Hofstee HM, et al. Falls in the elderly: a prospective study of risk factors and risk profiles. Am J Epidemiol. 1996;143(11):1129–1136. doi: 10.1093/oxfordjournals.aje.a008690. [DOI] [PubMed] [Google Scholar]
- 20.Glenshaw MT, Vernick JS, Li G, et al. Factors associated with injury severity in Oklahoma City bombing survivors. J Trauma. 2009;66(2):508–515. doi: 10.1097/TA.0b013e31815d9b72. [DOI] [PubMed] [Google Scholar]
- 21.North CS, Nixon SJ, Shariat S, et al. Psychiatric disorders among survivors of the Oklahoma City bombing. JAMA. 1999;282(8):755–762. doi: 10.1001/jama.282.8.755. [DOI] [PubMed] [Google Scholar]
- 22.Pfefferbaum B, North CS, Flynn BW. The emotional impact of injury following an international terrorist incident. Public Health Rev. 2001;29(2-4):271–280. [PubMed] [Google Scholar]
- 23.van den Berg B, Yzermans CJ, van der Velden PG, et al. Risk factors for unexplained symptoms after a disaster: a five-year longitudinal study in general practice. Psychosomatics. 2009;50(1):69–77. doi: 10.1176/appi.psy.50.1.69. [DOI] [PubMed] [Google Scholar]
- 24.Polinder S, Haagsma JA, Belt E, et al. A systematic review of studies measuring health-related quality of life of general injury populations. BMC Public Health. 2010;10:783. doi: 10.1186/1471-2458-10-783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Segui-Gomez M, MacKenzie EJ. Measuring the public health impact of injuries. Epidemiol Rev. 2003;25:3–19. doi: 10.1093/epirev/mxg007. [DOI] [PubMed] [Google Scholar]
- 26.Zatzick D, Jurkovich GJ, Rivara FP, et al. A national US study of posttraumatic stress disorder, depression, and work and functional outcomes after hospitalization for traumatic injury. Ann Surg. 2008;248(3):429–437. doi: 10.1097/SLA.0b013e318185a6b8. [DOI] [PubMed] [Google Scholar]
- 27.Kubzansky LD, Koenen KC. Is posttraumatic stress disorder related to development of heart disease? An update. Cleve Clin J Med. 2009;76(suppl 2):S60–S65. doi: 10.3949/ccjm.76.s2.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Murphy J, Brackbill RM, Thalji L, et al. Measuring and maximizing coverage in the World Trade Center Health Registry. Stat Med. 2007;26(8):1688–1701. doi: 10.1002/sim.2806. [DOI] [PubMed] [Google Scholar]
- 29.Baker SP, O'Neill B, Haddon W, Jr, et al. The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma. 1974;14(3):187–196. [PubMed] [Google Scholar]
- 30.Aharonson-Daniel L, Boyko V, Ziv A, et al. A new approach to the analysis of multiple injuries using data from a national trauma registry. Inj Prev. 2003;9(2):156–162. doi: 10.1136/ip.9.2.156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Møller L, Kristensen TS, Hollnagel H. Self rated health as a predictor of coronary heart disease in Copenhagen, Denmark. J Epidemiol Community Health. 1996;50(4):423–428. doi: 10.1136/jech.50.4.423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Idler EL, Angel RJ. Self-rated health and mortality in the NHANES-I Epidemiologic Follow-up Study. Am J Public Health. 1990;80(4):446–452. doi: 10.2105/ajph.80.4.446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.McDonald SD, Calhoun PS. The diagnostic accuracy of the PTSD Checklist: a critical review. Clin Psychol Rev. 2010;30(8):976–987. doi: 10.1016/j.cpr.2010.06.012. [DOI] [PubMed] [Google Scholar]
- 34.Ruggiero KJ, Del Ben K, Scotti JR, et al. Psychometric properties of the PTSD Checklist-Civilian Version. J Trauma Stress. 2003;16(5):495–502. doi: 10.1023/A:1025714729117. [DOI] [PubMed] [Google Scholar]
- 35.Soberg HL, Bautz-Holter E, Roise O, et al. Long-term multidimensional functional consequences of severe multiple injuries two years after trauma: a prospective longitudinal cohort study. J Trauma. 2007;62(2):461–470. doi: 10.1097/01.ta.0000222916.30253.ea. [DOI] [PubMed] [Google Scholar]
- 36.Boscarino JA. Posttraumatic stress disorder and physical illness: results from clinical and epidemiologic studies. Ann N Y Acad Sci. 2004;1032:141–153. doi: 10.1196/annals.1314.011. [DOI] [PubMed] [Google Scholar]
- 37.Kubzansky LD, Koenen KC, Spiro A, 3rd, et al. Prospective study of posttraumatic stress disorder symptoms and coronary heart disease in the Normative Aging Study. Arch Gen Psychiatry. 2007;64(1):109–116. doi: 10.1001/archpsyc.64.1.109. [DOI] [PubMed] [Google Scholar]
- 38.Jordan HT, Stellman SD, Morabia A, et al. Cardiovascular disease hospitalizations in relation to exposure to the September 11, 2001 World Trade Center disaster and posttraumatic stress disorder. J Am Heart Assoc. 2013;2(5):e000431. doi: 10.1161/JAHA.113.000431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Maestripieri D, Hoffman CL. Chronic stress, allostatic load, and aging in nonhuman primates. Dev Psychopathol. 2011;23(4):1187–1195. doi: 10.1017/S0954579411000551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Carpenter LL, Carvalho JP, Tyrka AR, et al. Decreased adrenocorticotropic hormone and cortisol responses to stress in healthy adults reporting significant childhood maltreatment. Biol Psychiatry. 2007;62(10):1080–1087. doi: 10.1016/j.biopsych.2007.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Beckett M, Weinstein M, Goldman N, et al. Do health interview surveys yield reliable data on chronic illness among older respondents? Am J Epidemiol. 2000;151(3):315–323. doi: 10.1093/oxfordjournals.aje.a010208. [DOI] [PubMed] [Google Scholar]
- 42.Holtslag HR, van Beeck EF, Lindeman E, et al. Determinants of long-term functional consequences after major trauma. J Trauma. 2007;62(4):919–927. doi: 10.1097/01.ta.0000224124.47646.62. [DOI] [PubMed] [Google Scholar]