This case-control study showed that there are differences at the initial visit between a nonprogressive and a progressive group of patients with adolescent idiopathic scoliosis (AIS). Progressive AIS presented hypokyphosis, higher values for rotational parameters (plane of maximal curvature, torsion, and apical intervertebral rotation) and lower values for local and regional slenderness.
Keywords: adolescent idiopathic scoliosis, 3D morphological parameters, progression, prediction, torsion, hypokyphosis, slenderness, axial rotation, plane of maximum curvature
Abstract
Study Design.
This is a prospective case-control study.
Objective.
The objective of this study was to compare 3-dimensional (3D) morphological parameters of the spine at the first visit between a nonprogressive (NP) and a progressive (P) group of immature adolescent idiopathic scoliosis (AIS).
Summary of Background Data.
Prediction of curve progression remains challenging in AIS at the first visit. Prediction of progression is based on curve type, curve magnitude, and skeletal or chronological age.
Methods.
A prospective cohort of 133 AIS was followed from skeletal immaturity to maturity (mean, 37 mo). The first group was made up of patients with AIS with a minimum 6-degree progression of the major curve between the first and last follow-up (P) (n = 53) and the second group was composed of patients with NP who reached maturity with less than 6-degree progression (n = 81). Computerized measurements were taken on reconstructed 3-dimensional (3D) spine radiographs of the first visit. There were 6 categories of measurements: angle of plane of maximum curvature, Cobb angles (kyphosis, lordosis), 3D wedging (apical vertebra, apical disks), rotation (upper and lower junctional vertebra, apical vertebra, and thoracolumbar junction), torsion, and slenderness (height/width ratio). t tests were also conducted.
Results.
There was no statistical difference between the 2 groups for age and initial Cobb angle. P presented significant hypokyphosis, and parameters related to rotation presented significant statistical differences between NP and P (plane of maximal curvature, torsion, and apical axial rotation). Depth slenderness also presented statistical differences.
Conclusion.
This study confirms that even at the initial visit, 3D morphological differences exist between P and NP AIS. It supports the use of 3D reconstructions of the spine in the initial evaluation of AIS to help predict outcome.
Level of Evidence: 3
Adolescent idiopathic scoliosis (AIS) is a 3-dimensional spinal deformity. The prevalence of AIS in children between the ages 6 and 17 years is 1.34% for a Cobb angle of 10° or more.1 A meta-analysis showed that 38% (95% CI, 23.8%–52.13%) of children screened at school and referred to an orthopedic surgeon actually have an AIS.1 A major challenge with AIS is the difficulty to predict curve progression at the initial presentation for patients diagnosed with the disease.
The main risk factors used to predict curve progression are (1) maturity (chronological age, skeletal age from Risser sign and Tanner-Whitehouse, menarchal status), (2) curve magnitude, and (3) curve location.2,3 Treatment and follow-up intervals are actually oriented using these risk factors. Unfortunately, these factors give an imprecise prediction of the final deformation. A nomogram made to assess incidences of progression for a specific curve was developed by Lonstein and Carlson.3 However, they suggest not using the nomogram to determine treatment, but only as a guide to advise family on the chance of progression. This uncertainty in curve progression and outcome can create anxiety for families and patients with scoliosis, and unnecessary psychosocial stresses associated with brace treatment. Consequences of that incertitude might include delay in treatment, unnecessary treatment, more aggressive treatment, unnecessary radiographs, and unnecessary medical visits.
Genetics tests to predict the outcome of a specific curve are available. It is good to detect the nonprogressive or the rapid progressive curves. An independent study showed that ScoliScore could provide a better risk stratification than traditional Lonstein and Carlson criteria.4 But it still needs to be validated on long-term cohort study.
Previous data suggest that the 3-dimensional (3D) morphology of the spine can help in predicting the progression of AIS. A recent retrospective study showed that various 3D morphological parameters were different at the first visit between a nonprogressive (NP) group and a progressive (P) group.5 Unfortunately, the retrospective nature of that study precludes any strong conclusion about the clinical relevance of using 3D spinal morphology to detect progressive AIS, highlighting the importance to perform a prospective study.
The objective of this prospective study was to evaluate the differences in 3D morphological spine parameters between a P AIS group and a NP AIS group at the first visit.
MATERIALS AND METHODS
A study based on a prospective cohort was performed. A prospective cohort was recruited in a single center from January 2006 to May 2010. The inclusion criteria were (1) first visit with an orthopedic surgeon for AIS, (2) Cobb angle between 11° and 40°, and (3) Risser sign of 0 or 1. The exclusion criteria were (1) congenital, (2) neuromuscular, or (3) syndromic scoliosis. This research was approved by the ethics institutional review board (Research Center, Sainte-Justine University Hospital Center), and all subjects (and/or legal guardians) signed an informed consent to participate in the study.
At the first and all subsequent visits, each patient had lateral and posteroanterior spine radiographs. Patients were followed by 1 of 4 spine surgeons, with intervals of follow-up chosen by the treating surgeon. The follow-up concluded at skeletal maturity (at least Risser 4) or with a surgery (for the study). Brace treatments were permitted according to the treating physician, but braces had to be removed the night before the appointment.
All patients of the cohort were included, but divided in 2 groups according to the magnitude of their last Cobb angle at skeletal maturity (Risser 4) or before surgery. The first group was a progressive (P) group defined by a progression of 6° between the first and last visits. The second group was a nonprogressive (NP) group defined by a progression of less than 6° between the first and last visits. A 6-degree cutoff was chosen as it represents the measurement error on radiographs.6
All patients underwent a 3D spinal reconstruction of the radiographs at the first visit (posteroanterior and lateral views). Radiographs were done either with EOS system (EOS Imaging, Paris, France) or standard Fuji system (Fujifilm, Tokyo, Japan). Reconstructions were completed with 2 software programs Spine 3D (LIS3D; Montreal, Canada) and IdefX (LIO; Montreal, Canada), by one research assistant considered an expert in the technique. Two programs were used because radiographs obtained from the Fuji system could only be reconstructed with Spine 3D. Spine 3D software uses algorithms based on direct linear transformation combined with the nonstereo corresponding points algorithm7,8; this is based on the identification of corresponding anatomical landmarks on vertebrae from stereoradiographs. IdefX software uses a semiautomated method based on a priori knowledge.8 Pomero et al9 showed that there is no difference in terms of mean errors between 3D vertebral models issued from stereoradiography (nonstereo corresponding points algorithm and semiautomated) and computed tomographic–scan reconstructions. The precision of these reconstructions has previously been shown to be very satisfactory with mean point-to-surface errors of less than 1.5 mm and less than 2° for angular measurements when compared with conventional computed tomographic–scan reconstructions.8,10 Therefore, both software generated 3D reconstructions of comparable precision.
All measurements were computerized 3D radiological measurements completed with the same custom software IdefX (LIO) for all reconstructions.
The calculated parameters were divided into 6 categories. Each category refers to global (whole spine), regional (scoliotic segment), and local (vertebra) descriptors. Vertebra centroid is understood as the halfway point between the centers of the 2 endplates of the vertebra. The local vertebra axis system is defined by the SRS 3D terminology group as follows:
the origin is at the centroid of the vertebral body (half way between the centers of the 2 endplates), the local z-axis passes through the centers of the upper and lower endplates, and y-axis is parallel to a line joining similar landmarks on the bases of the right and left pedicles.
-
Cobb angles:
Cobb angles defined as the angle between the upper and lower endplate of the respective end vertebrae of a curve. Cobb angle was measured in the frontal plane, in the plane of maximal deformation in 3D, and in the sagittal plane for thoracic kyphosis (T4–T12) and lumbar lordosis (L1–L5).
-
Plane of maximal deformation:
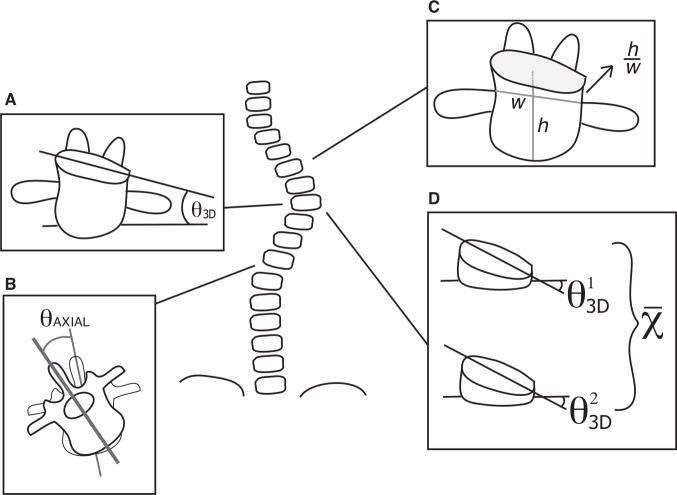
Axial angle of the plane in which the Cobb angle is maximal (Figure 1).
-
Three-dimensional wedging of vertebral body and disk:
Wedging of the apical vertebral body in the plane of maximal deformation (3D plane) and mean maximal 3D wedging of the 2 apical intervertebral disks (Figure 2A–D). Maximal 3D wedging represents the wedging measured in the plane, wherein the wedging value is maximal around the vertical axis.10 If apex was a disk, then the mean of the 3D wedging of both apical vertebral bodies was calculated and only the 3D wedging of the apical disk was documented. Three-dimensional disk wedging was analyzed for all levels of the spine (from T1–T2 to L4–L5).
-
Axial intervertebral rotation of the apex, upper, and lower junctional level and thoracolumbar level:
Rotation between 2 adjacent vertebrae at upper, apical, and lower curve levels and thoracolumbar junction (T12–L1) in the axial plane according to the inferior local vertebrae reference (Figure 2B).
-
Torsion:
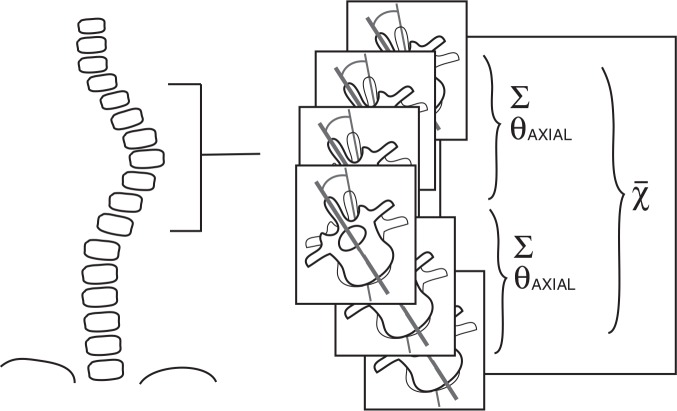
Mean of the sum of intervertebral axial rotation (measured according to the local referential of the inferior vertebrae) of the 2 hemicurvatures of the curve (between upper end vertebra and apex and between lower end vertebra and apex) (Figure 3).
-
Slenderness (local T6, T12, and L4 and regional T1–L5):
Ratio between the height (distance between the superior and inferior endplates at the center of the vertebrae) and the width (measured at the center of the vertebrae using a line perpendicular to the height line in mediolateral direction) of the vertebral body for T6, T12, and L4 vertebrae (Figure 2C). Ratio between the length of the spine from T1 to L5 and the mean of the width of vertebral bodies of T6–T12 and L4. The same measurement was made by replacing the width by the depth (a line perpendicular to the height line at the center of the vertebra in an anteroposterior direction). This is the height-depth ratio.
Figure 1.
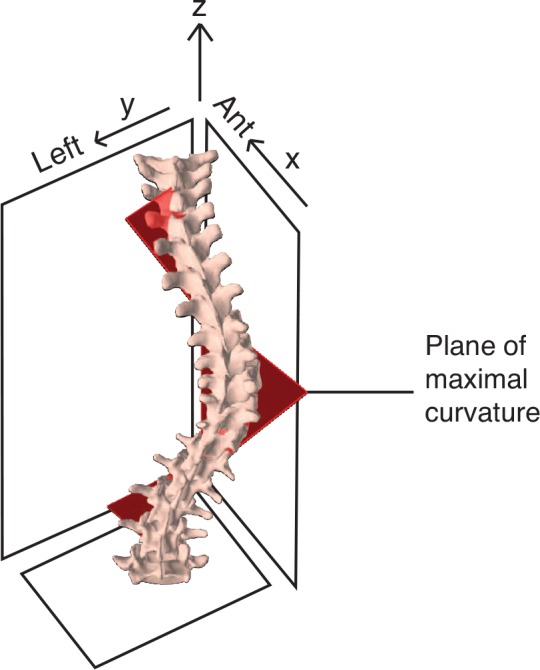
Plane of maximal curvature.
Figure 2.
A, Three-dimensional wedging of vertebral body. B, Axial intervertebral rotation at inferior junctional level. C, Slenderness (height/width ratio illustrated). D, Mean of apical disc 3D wedging. 3D indicates 3-dimensional.
Figure 3.
Torsion.
RESULTS
At the time of the analysis 133 patients, made up of 117 females and 16 males, could be included in the study.
The mean age was 12.6 years at the first visit with a mean Cobb angle of 22.1° ± 8.4°. There were 32 right thoracic curves, 48 double curves (22 main thoracic, and 26 main left lumbar), 7 triple curves, 36 left thoracolumbar curves, and 10 either right lumbar or left thoracic curves. In total, 58 patients had their first-visit radiographs obtained with the Fuji system and 75 with the EOS system. All descriptive statistics are presented in Table 1.
TABLE 1. Descriptive Parameters.
| Cohort | NP | P | |
|---|---|---|---|
| n | 133 | 80 | 53 |
| Age (yr) | 12.6 ± 1.2 | 12.6 ± 1.2 | 12.6 ± 1.2 |
| Sex | |||
| Male | 16 | 7 | 9 |
| Female | 117 | 73 | 44 |
| Risser | |||
| 0 and TR open | 48 | 22 | 26 |
| 0 and TR closed | 47 | 30 | 17 |
| 1 | 38 | 28 | 10 |
| Cobb angle (°) | 22.1 ± 8.4 | 21.3 ± 8.3 | 23.4 ± 8.6 |
| Follow-up (mo) | 36.7 ± 13.6 | 35.1 ± 14.2 | 38.9 ± 12.3 |
| Type | |||
| RT | 35 | 22 | 13 |
| RT-LL | 22 | 10 | 12 |
| LL-RT | 26 | 18 | 8 |
| Triple | 7 | 1 | 6 |
| LTL | 36 | 26 | 10 |
| Other | 7 | 3 | 4 |
| Treatment | |||
| Observation | 51 | 44 | 7 |
| Brace | 67 | 36 | 31 |
| Surgery | 15 | 0 | 15 |
NP indicates nonprogressive; P, progressive; n, sample size; TR, triradiate cartilage; RT, right thoracic; RT-LL, right thoracic-left lumbar; LL-RT, left lumbar-right thoracic; LTL, left thoracolumbar; other, left thoracic, right lumbar.
Although 15 patients underwent surgery as final treatment, 67 patients underwent brace treatment. The mean follow-up was 36.7 months (range, 12–67 mo).
Between the last and first visits, 80 patients with AIS had a Cobb angle difference of less than 6° and 53 had a difference of 6° or more. There was no significant difference between the 2 groups in regard to age (12.6 yr, P = 0.8 for both groups) and Cobb angle (21.3° NP and 23.4°P = 0.7) at the first visit.
In total, 10 parameters showed significant differences at the first visit. All results are presented in Table 2.
TABLE 2. Values of the Different Parameters Measured at the First Visit and Their P Values.
| Parameters | Nonprogressive | Progressive | P |
|---|---|---|---|
| Kyphosis | 25 | 20.6 | 0.02 |
| Lordosis | 47.1 | 45.6 | 0.45 |
| 2D Cobb angle | 21.3 | 23.4 | 0.2 |
| 3D Cobb angle | 30 | 27.8 | 0.2 |
| Angle of plane of maximal curvature | 51.4 | 63.5 | 0.001 |
| Apical vertebral body wedging | 2.5 | 2.5 | 0.9 |
| Apical disk wedging | 5.8 | 6 | 0.6 |
| Upper curve disk wedging | 3.5 | 4 | 0.2 |
| Lower curve disk wedging | 6.5 | 6.1 | 0.6 |
| Apical intervertebral rotation | 5.7 | 8.1 | 0.006 |
| Upper curve intervertebral rotation | 2.4 | 2.8 | 0.2 |
| Lower curve intervertebral rotation | 1.6 | 1.9 | 0.3 |
| T12–L1 intervertebral rotation | 2.1 | 1.9 | 0.6 |
| Torsion | 3.1 | 4.5 | 0.02 |
| T6 width slenderness | 56.9 | 55.3 | 0.09 |
| T6 depth slenderness | 67 | 65 | 0.05 |
| T12 width slenderness | 54.3 | 52.5 | 0.1 |
| T12 depth slenderness | 70.3 | 67.2 | 0.03 |
| L4 width slenderness | 52.1 | 50.3 | 0.009 |
| L4 depth slenderness | 76.5 | 73.5 | 0.007 |
| T1–L5 width slenderness | 11.5 | 11.3 | 0.05 |
| T1–L5 depth slenderness | 15.3 | 14.9 | 0.005 |
3D indicates 3-dimensional; 2D, 2-dimensional.
DISCUSSION
Prediction of progression in AIS is predominantly based on skeletal and chronological age as well as on the type and magnitude of the curve. These risk factors are insufficient in predicting precisely the progression of the curve at the first visit. This prospective study identified differences in spine morphology between P and NP AIS, and these findings could significantly increase the precision of the prediction of final deformation.
The first and more important significant parameter was the angle of the plane of maximal curvature, which was 12.1° higher in the P group. In their longitudinal study, Villemure et al10 found a tendency for the plane of maximal curvature to increase with the severity of deformation. This is the first study that showed potential for a 3D parameter for identification of a progressive curve in AIS. A recent study by the Scoliosis Research Society 3D Scoliosis Committee11 showed that for a similar 2-dimensional scoliotic deformity 2 spines can have a totally different 3D morphology and emphasized the importance of a new 3D classification. This study could provide a new parameter for dividing the different geometrics of deformation, increasingly interesting should such a parameter be a risk factor of progression.
The second significant difference between P and NP AIS was the kyphosis being 4.4° less in the P group. This finding is of particular interest because it supports the buckling theory for AIS etiology. Porter12 showed that the spinal canal length was smaller to the anterior vertebral body length in scoliosis and that such a disparity increases with rotational deformity. This asymmetrical growth between anterior and posterior spine leads to buckling of the spine and, eventually, the classical 3D deformity seen in AIS. This is also in accordance with the asymmetrical growth theory published by Guo et al,7 stating that there is an anterior overgrowth of the vertebral body. The difference in kyphosis is small, but all measurements were taken on small curves at the first visit and with no difference in Cobb angle. Therefore, it is a finding with clinical significance as it could be indicative of a new risk factor for progression.
The third significant parameter was the apical intervertebral axial rotation with 2.4° more rotation in the P group. Villemure et al10 showed that, in some cases, axial rotation increased toward convexity of the curve with curve severity. In this study, a significant difference was found for this parameter at the first visit between the P and NP AIS.
The fourth significant parameter was torsion, with 1.4° more torsion in the P group. This is in accordance with results found by Champain,13 who observed that the progressive curve had a torsion more than 5°. The population used in this study had at least a moderate deformation explaining why their values are more significant.
The last group of parameters that presented significant difference was slenderness based on the ratio between height and depth of the vertebral body. The difference was present for the local measurement of T6–T12 and L4 and for the general measurement of the whole spine (T1–L5). This parameter was described by Skogland and Miller14 as the height/width ratio measure on simple radiographs. The authors found a higher ratio for AIS, than control subjects, for T6 and L4 vertebrae. Guo et al7 also found a higher height/depth ratio for T6 in AIS than controls on magnetic resonance images. These findings support the theory of slenderness. This study did not find a higher ratio for P AIS. On the contrary, all height/depth ratios (for T6–T12–L4 and whole spine) were higher for NP AIS, and the height/width of L4. Despite that no real explanation could be found, this is not considered a random finding as all ratios are statistically significant between P and NP AIS.
Villemure et al10 found a concomitant progression between curve severity and 3D vertebral body wedging. This study did not reveal any differences in vertebral wedging for P and NP AIS, likely because the magnitude of the Cobb angle was the same at the initial visit. Additional longitudinal analyses of the cohort could eventually confirm this finding.
A limitation of this study is the small values found for the difference between the 2 groups. Larger differences were not expected because all patients evaluated at the first visit presented with similar Cobb angle curves less than 40°. Consequently, classic parameters such as curve magnitude, curve type, and skeletal maturity would not have been of any help in predicting progression of deformation.
A strength of this study is that it has been designed prospectively, and the 2 groups were equivalent at the first visit and all data were collected in the majority of patients. Subsequently, the sample size is greater possibly contributing to the successful identification of significant differences between P and NP groups.
CONCLUSION
To our knowledge, this is the first study that has evaluated 3D morphological spine parameters at the first visit with positive findings. This could become of crucial importance for the follow-up planning of patients with AIS after their first visit.
Key Points
Progressive AIS is hypokyphotic at the initial visit compared with an equivalent NP group.
There is significant difference between nonprogressive and progressive AIS with respect to the plane of maximal curvature, torsion and apical intervertebral rotation at the first visit.
Slenderness based on the depth of the vertebral body is higher, using local and regional measures, for nonprogressive AIS at the first visit.
Footnotes
Acknowledgment date: October 9, 2012. First revision date: February 14, 2013. Acceptance date: February 18, 2013.
The device(s)/drug(s) is/are FDA-approved or approved by corresponding national agency for this indication.
Canadian Institute of Health Research (CIHR), Operating Grant (2007–2012) funds were received to support this work.
Relevant financial activities outside the submitted work: grant, consulting fee or honorarium, board membership, consultancy, grants/grants pending, patents, stock/stock options, travel/accommodations/meeting expenses, royalties, Academic Chair in Pediatric Spinal Deformity of CHU Sainte-Justine, Research Chair in Spinal Trauma at University of Montreal, support for spine fellows at University of Montreal.
References
- 1.Fong DY, Lee CF, Cheung KM, et al. A meta-analysis of the clinical effectiveness of school scoliosis screening. Spine (Phila Pa 1976) 2010;35:1061–71 [DOI] [PubMed] [Google Scholar]
- 2.Bunnell WP. The natural history of idiopathic scoliosis before skeletal maturity. Spine (Phila Pa 1976) 1986;11:773–6 [DOI] [PubMed] [Google Scholar]
- 3.Lonstein JE, Carlson JM. The prediction of curve progression in untreated idiopathic scoliosis during growth. J Bone Joint Surg Am 1984;66:1061–71 [PubMed] [Google Scholar]
- 4.Roye BD, Wright ML, Williams BA, et al. Does ScoliScore provide more information than traditional clinical estimates of curve progression? Spine (Phila Pa 1976) 2012;37:2099–103 [DOI] [PubMed] [Google Scholar]
- 5.Nault ML, Mac-Thiong JM, Roy-Beaudry M, et al. Three-dimensional spine parameters can differentiate between progressive and nonprogressive patients with AIS at the initial visit. J Pediatr Orthop 2013;33:618–23 [DOI] [PubMed] [Google Scholar]
- 6.Pruijs JE, Hageman MA, Keessen W, et al. Variation in Cobb angle measurements in scoliosis. Skeletal Radiol 1994;23:517–20 [DOI] [PubMed] [Google Scholar]
- 7.Guo X, Chau WW, Chan YL, et al. Relative anterior spinal overgrowth in adolescent idiopathic scoliosis. Results of disproportionate endochondral-membranous bone growth. J Bone Joint Surg Br 2003;85:1026–31 [DOI] [PubMed] [Google Scholar]
- 8.Humbert L, De Guise JA, Aubert B, et al. 3D reconstruction of the spine from biplanar x-rays using parametric models based on transversal and longitudinal inferences. Med Eng Phys 2009;31:681–7 [DOI] [PubMed] [Google Scholar]
- 9.Pomero V, Mitton D, Laporte S, et al. Fast accurate stereoradiographic 3D-reconstruction of the spine using a combined geometric and statistic model. Clin Biomech (Bristol, Avon) 2004;19:240–7 [DOI] [PubMed] [Google Scholar]
- 10.Villemure I, Aubin CE, Grimard G, et al. Progression of vertebral and spinal three-dimensional deformities in adolescent idiopathic scoliosis: a longitudinal study. Spine 2001;26:2244–50 [DOI] [PubMed] [Google Scholar]
- 11.Labelle H, Aubin CE, Jackson R, et al. Seeing the spine in 3D: how will it change what we do? J Pediatr Orthop 2011;31:S37–45 [DOI] [PubMed] [Google Scholar]
- 12.Porter RW. Idiopathic scoliosis: the relation between the vertebral canal and the vertebral bodies. Spine (Phila Pa 1976) 2000;25:1360–6 [DOI] [PubMed] [Google Scholar]
- 13.Champain N. Recherche des facteurs biomécanique dans l'aggravation de la scoliose idiopathique. Biomécanique. Paris: École Nationale Supérieure d'Arts et Métiers; 2004 [Google Scholar]
- 14.Skogland LB, Miller JA. The length and proportions of the thoracolumbar spine in children with idiopathic scoliosis. Acta Orthop Scand 1981;52:177–85 [DOI] [PubMed] [Google Scholar]