Abstract
Valproic acid and the antidepressants doxepin and venlafaxine are frequently used psychotropic drugs. In the literature, an influence of valproic acid on serum levels of antidepressants has been described, although studies have focused on amitriptyline. The authors assessed their therapeutic drug monitoring (TDM) database for patients receiving a combination of doxepin or venlafaxine and valproic acid and compared these samples with matched controls without valproic acid comedication in terms of the serum concentration of antidepressants. The mean dose-corrected serum concentration of doxepin+N-doxepin in 16 patients who received valproic acid comedication was higher (2.171±1.482 ng/ml/mg) than that in the matched controls (0.971±0.857 ng/ml/mg, P<0.003). We also found a significant correlation between valproic acid serum level and dose-corrected doxepin+N-doxepin serum level (Spearman’s ρ r=0.602, P<0.014). The mean dose-corrected serum level of venlafaxine+O-desmethylvenlafaxine in 41 patients who received valproic acid comedication did not differ significantly from that of the matched controls (P<0.089), but there was a significant difference between both groups in the dose-corrected serum level of O-desmethylvenlafaxine (1.403±0.665 vs. 1.102±0.444, P<0.017). As a consequence, if a combination of valproic acid with doxepin or venlafaxine is administered, cautious dosing is advisable and TDM should be performed.
Keywords: antidepressants, doxepin, interaction, valproic acid, venlafaxine
Introduction
The mood stabilizer and anticonvulsant drug valproic acid and the antidepressants doxepin and venlafaxine are well-established psychotropic drugs that are used widely. Valproic acid is one of the most important antiepileptic agents (Stephen, 2003; Angalakuditi and Angalakuditi, 2011) applicable in antiepileptic maintenance treatment as well as in epileptic emergency cases such as acute seizures or status epilepticus (Wasterlain et al., 2011). Moreover, it is an established mood stabilizer used in the treatment of bipolar affective disorders (Dietrich and Emrich, 1998; Bowden, 2003), and additionally in nonpsychiatric indications such as vestibular migraine (Bisdorff, 2011) or painful diabetic neuropathy (Bril et al., 2011).
The risk of a possible switch from depression to mania under treatment with antidepressants has led to a long debate on the use of these drugs in patients with bipolar disorder (Koszewska and Rybakowski, 2009) in whom especially tricyclic antidepressants and venlafaxine could trigger a particular switch risk. Even if valproic acid monotherapy has been suggested to be efficacious (Bond et al., 2010) at least in Europe it is not unusual to treat severe depressive episodes in bipolar disorder with tricyclic antidepressants or venlafaxine (Amsterdam and Brunswick, 2003), although not supported by evidence from randomized-controlled trials. In addition, many patients with epilepsy show depressive symptoms during the course of their illness (Miller et al., 2008), which, in some cases of severe depressive episodes, could be the reason for administration of a combination of a tricyclic antidepressant and valproic acid.
The occurrence of severe adverse events during combined treatment with valproic acid and antidepressant drugs has been described in case reports on a recurrence of absence seizures after starting comedication with low-dosed amitriptyline (Avoni et al., 1996), and for status epilepticus after adding clomipramine to valproic acid (DeToledo et al., 1997). In experimental studies, a significant increase in the plasma concentration of amitriptyline and nortriptyline after the addition of valproic acid has been reported (Vandel et al., 1988; Wong et al., 1996). An increase in nortriptyline serum levels in association with valproic acid comedication was also observed in two cases (Fu et al., 1994). Finally, we have previously published a drug–drug interaction study that showed a marked increase in amitriptyline and nortriptyline serum levels in combination with valproic acid (Unterecker et al., 2013).
Even though an influence of valproic acid on serum concentrations of tricyclic antidepressants such as amitriptyline, nortriptyline, and clomipramine has been reported repeatedly in the literature (DeToledo et al., 1997; Fehr et al., 2000; Spina and Perucca, 2002; Patsalos and Perucca, 2003; Perucca, 2005), to date, no studies have examined potential interactions between valproic acid and the tricyclic antidepressant doxepin or the dual selective antidepressant venlafaxine.
Materials and methods
As treatment with the antidepressants doxepin and venlafaxine as well as with the mood stabilizer valproic acid is routinely monitored by therapeutic drug monitoring (TDM) in the Department of Psychiatry, Psychosomatics and Psychotherapy of the University Hospital of Würzburg, we could retrospectively assess this TDM database for the time period January 2008 to December 2011 to identify all cases in which valproic acid in combination with doxepin or venlafaxine was administered. In cases of multiple serum-level determinations of the same drug, only the last determination was considered for evaluation to avoid multiple inclusion of the same individual. In a second step, we included a control group of patients receiving doxepin or venlafaxine without valproic acid comedication. This sample was matched with the patients in the valproic acid group with respect to sex, age, and dose of the respective antidepressant as well as number of comedications. The comedication was registered in detail on the request form. Patients with potential drug–drug interactions because of comedication with drugs that could induce or inhibit the metabolism of doxepin or venlafaxine according to a review of Hiemke et al. (2011) were identified and excluded. We then compared the respective groups with or without valproic acid in terms of dose-corrected serum levels (ng/ml per applied mg of daily dose) of the antidepressants as well as the ratio of the metabolite/parent compound by the Mann–Whitney U-test. Spearman’s ρ correlation coefficients were calculated to analyze the association between valproic acid and antidepressants’ serum levels.
Serum levels were determined in the TDM laboratory of the Psychiatric University Hospital of Würzburg using an isocratic reversed-phase high-performance liquid chromatography method (doxepin, venlafaxine) and a spectrophotometric immunoassay (valproic acid), respectively. Internal and external (Cardiff Bioanalytical Services, The Cardiff Medic Center, Cardiff, UK) quality control programs were operated regularly without rejection.
Results
From January 2008 to December 2011, 16 patients were identified in whom serum levels of doxepin and valproic acid were determined and 41 patients in whom serum levels of venlafaxine and valproic acid were measured. From the same time period, a sample of control patients receiving doxepin and venlafaxine without valproic acid was obtained and matched for sex, age, and dose of the antidepressant agent (Table 1).
Table 1.
Comparison of the sample with combined doxepin or venlafaxine and valproic acid treatment and the matched control samples of antidepressants without valproic acid in terms of matching variables and serum levels of antidepressants (Mann–Whitney U-test)
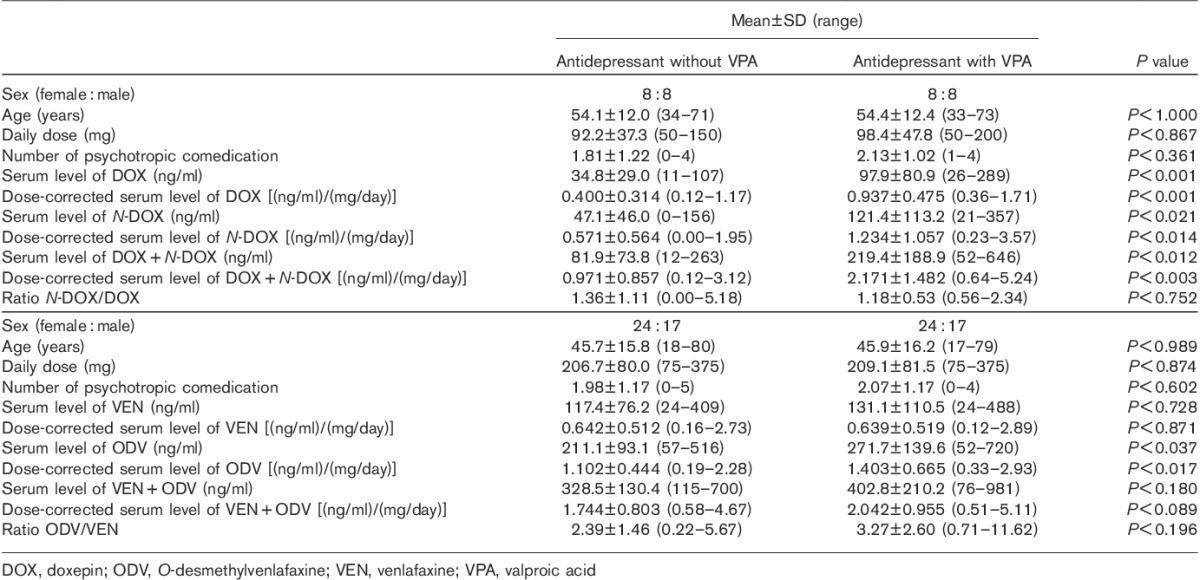
Patients receiving valproic acid and doxepin had higher mean dose-corrected serum levels of doxepin, N-doxepin, and doxepin+N-doxepin in comparison with patients treated with the antidepressant alone. Whereas four of 16 patients in the doxepin plus valproic acid sample showed a total serum level of doxepin+N-doxepin above the alert level of 300 ng/ml (Hiemke et al., 2011), in the control group, this was not the case in any of the 16 patients (χ2 P<0.05). In patients receiving venlafaxine and valproic acid, the mean serum concentration of O-desmethylvenlafaxine was higher than that in patients treated with venlafaxine alone. For dose-corrected serum levels of venlafaxine+O-desmethylvenlafaxine, there only was a trend for a difference (0.05<P<0.10, Table 1) whereas the parent compound showed no difference. In the total serum concentration of venlafaxine+O-desmethylvenlafaxine, two of 41 patients in the valproic acid comedication sample exceeded the alert level (800 ng/ml; Hiemke et al., 2011) whereas none in the group receiving venlafaxine without valproic acid exceeded this level. However, this difference was not statistically significant.
The serum concentrations of the respective antidepressant and its metabolite in relation to the daily dose of the antidepressants in patients with and without valproic acid comedication are shown in Figs 1 and 2. The ratio of the metabolite to parent compound did not differ between patients with or without valproic acid for both drugs (Table 1).
Fig. 1.
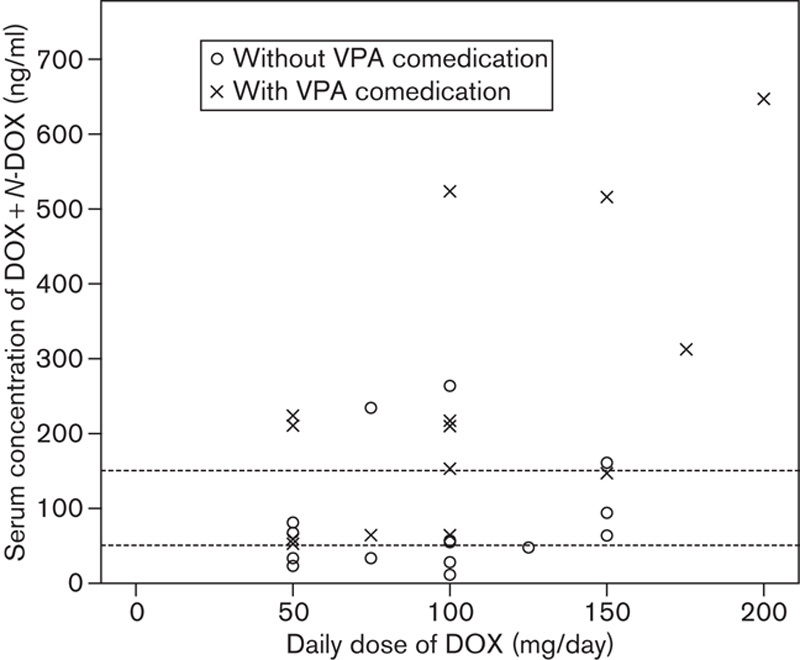
Serum level of doxepin (DOX)+N-DOX (ng/ml) as a function of DOX dose in patients with and without valproic acid (VPA) comedication (dashed lines: lower and upper limit of the therapeutic range).
Fig. 2.
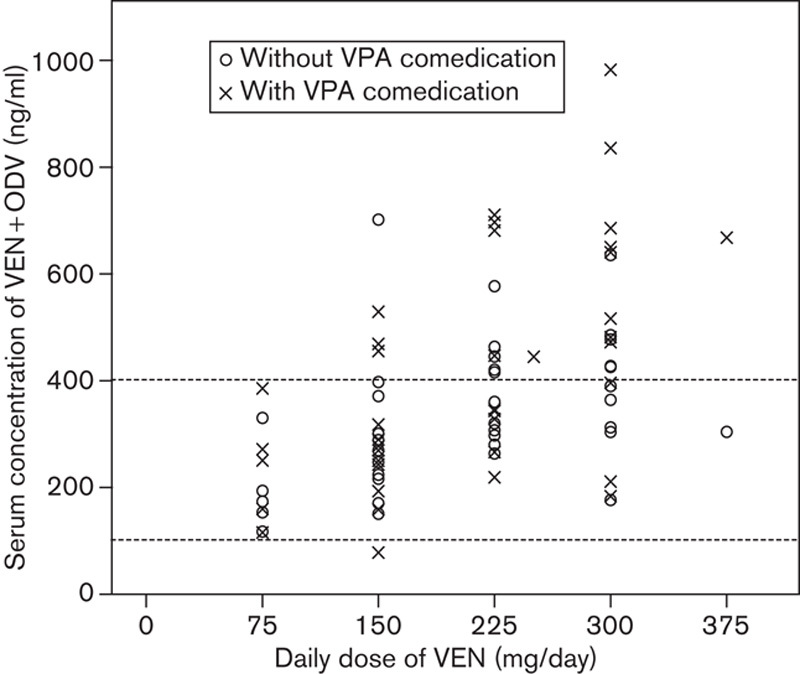
Serum level of venlafaxine (VEN)+O-desmethylvenlafaxine (ODV) (ng/ml) as a function of VEN dose in patients with and without valproic acid (VPA) comedication (dashed lines: lower and upper limit of the therapeutic range).
On examining a potential association between the serum level of valproic acid and the dose-corrected serum levels of the respective antidepressants and their metabolites, a significant correlation (Spearman’s ρ) was found between valproic acid and doxepin+N-doxepin serum levels (Fig. 3). In terms of dose-corrected serum levels of venlafaxine+O-desmethylvenlafaxine (r=0.191, P=0.231, n=41), there was no significant correlation with the valproic acid serum concentration.
Fig. 3.
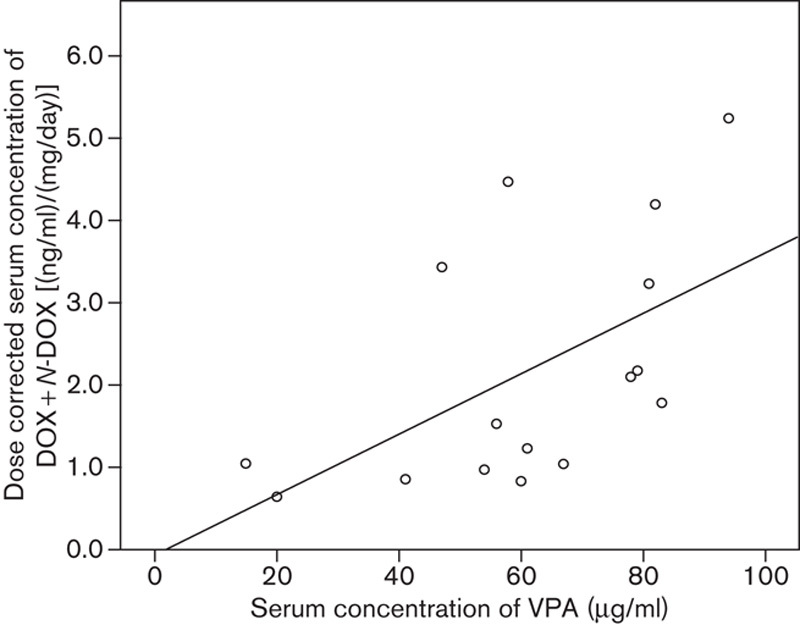
Scatterplot of dose-corrected serum level of doxepin (DOX)+N-DOX [(ng/ml)/(mg/day)] and serum level of valproic acid (VPA) (Spearman’s ρ r=0.602, P<0.014, n=16).
Discussion
Our results indicate a clinically relevant increase in the serum concentrations of doxepin and O-desmethylvenlafaxine if a comedication with valproic acid is administered. In patients receiving doxepin and valproic acid, there was also a significant positive correlation between the serum levels of valproic acid and dose-corrected serum level of the antidepressant.
An obvious limitation is the retrospective nature of the study, which, in principle, cannot determine any causal relationship. Thus, the results of this study are of an explorative nature and have to be confirmed by prospective investigations. Furthermore, our study did not take into account the fact that both doxepin and venlafaxine are formulated as a mixture of trans-stereoisomers and cis-stereoisomers (Haritos et al., 2000). Even if a potential pharmacokinetic influence of psychiatric and somatic comedication was controlled for by excluding patients who received a comedication with drugs known for their inducing or inhibiting properties in terms of the metabolic activity of cytochrome P450 enzymes, the possibility of an undetected drug–drug interaction cannot be ruled out completely. Therefore, the polypharmacy that was observed in all the patients studied in both naturalistic samples might have compromised the analysis. In terms of the number of simultaneously administered psychotropic drugs, there was no significant difference between patients with and without valproic acid for any of the antidepressant drugs evaluated. Moreover, both groups did not differ with respect to sex, age, or dose of the antidepressant agent.
In terms of valproic acid and clomipramine, DeToledo et al. (1997) reported the case of a patient with status epilepticus associated with a combination of valproic acid and clomipramine. They found elevated serum levels of clomipramine despite applying a relatively small dose (75 mg), which was also observed by Fehr et al. (2000). In a patient who received a comedication with valproic acid, elevated serum levels of amitriptyline and nortriptyline resulting in a severe cardiac adverse effect (Brugada syndrome) were described by Roberts-Thomson et al. (2007). However, the authors did not discuss a possible causal role of an interaction between amitriptyline and valproic acid, which shows the importance of a further clarification of the interaction potential of a combination of valproic acid and tricyclic antidepressants. In contrast, an increase in the serum level of another tricyclic antidepressant, desipramine, after discontinuation of valproic acid has been described (Joseph and Wroblewski, 1993), suggesting that potential interactions between valproic acid and antidepressants could result in different effects on serum levels of the antidepressants.
According to the results of the present study, there is not only a significant influence of valproic acid on the serum level of doxepin but also a significant correlation between dose-corrected serum level of doxepin+N-doxepin and valproic acid serum level. As a significant influence of amitriptyline on the plasma half-life of valproic acid has been described (Pisani et al., 1986) according to our results, a change in valproic acid metabolism by doxepin might also be assumed.
However, the mechanism of the influence of valproic acid on doxepin and venlafaxine metabolism still remains unclear. Both doxepin and venlafaxine are metabolized mainly by CYP2D6 and CYP2C19. To a minor degree, doxepin is metabolized by CYP2C9 and venlafaxine by CYP3A4 (Hiemke et al., 2011). According to Wen et al. (2001) valproic acid in vitro inhibited CYP2C19 as well as CYP3A4 slightly, and CYP2C9 to a larger extent. The latter might be the main reason for the considerable increase in doxepin+N-doxepin in combination with valproic acid. Therefore, the addition of valproic acid in patients treated with substrates of CYP2C9 might be problematic as a considerable increase in the serum level of the respective drug might occur, even if alternative metabolic pathways exist. Whereas CYP2C19 contributes considerably toward N-demethylation of doxepin, CYP2C9 seems to play only a minor role in the metabolism of doxepin (Härtter et al., 2002). Nevertheless, an inhibition of its metabolic activity of CYP2C9 might be followed by an increase in doxepin serum concentrations (Kirchheiner et al., 2002). In addition to an influence of valproic acid by inhibition of CYP2C9, the influence of saturated pathways must be considered as valproic acid is also metabolized by CYP2C9.
Similar to the study of Vandel et al. (1988) on unchanged ratios of nortriptyline and amitriptyline before and after the addition of valproic acid, the present study showed no differences in the ratios of the metabolite and the parent compound for doxepin in patients with and without valproic acid comedication. As, according to Kirchheiner et al. (2002), the doxepin as well as the N-doxepin serum level might be elevated by an inhibition of CYP2C9, our result of a lack of influence on the ratio N-doxepin/doxepin is in agreement with these findings. In contrast to the strong inhibitory influence of valproic acid on the metabolism of doxepin, in the venlafaxine sample, only a significant increase in the metabolite O-desmethylvenlafaxine, which is also known as desvenlafaxine, was found. Even if CYP2D6 is dominant, in addition to CYP2C19, CYP2C9 also plays a role in the N-demethylation of venlafaxine. However, inhibitors of CYP2C9 showed no consistent inhibition of O-desmethylvenlafaxine formation (Fogelman et al., 1999). However, CYP2C9, in addition to CYP2C19 and CYP3A, contributes considerably toward the formation of N-desmethylvenlafaxine (Fogelman et al., 1999). Even if some authors disregard an influence of CYP2C9 on the N-demethylation of venlafaxine (Shams et al., 2006; McAlpine et al., 2011), the results of the present study suggest a significant contribution of CYP2C9 because of the higher O-desmethylvenlafaxine serum levels in the valproic acid comedication sample. In particular, the inhibition of valproic acid on the N-demethylation pathway might lead to a stronger O-demethylation and as a consequence to higher serum levels of O-desmethylvenlafaxine. On the basis of this interpretation, it must be assumed that a treatment with desvenlafaxine that is chemically identical to venlafaxine’s major metabolite O-desmethylvenlafaxine and marketed as an original drug is not influenced by valproic acid comedication.
In contrast to previous findings (Unterecker et al., 2013) showing a significant difference in the ratios of nortriptyline/amitriptyline in the samples with and without valproic acid comedication as an indicator of a change in metabolism by valproic acid, the present study found no differences in the ratios of the metabolite and the parent compound for doxepin and venlafaxine in patients with and without valproic acid comedication. Therefore, the first step of biotransformation of doxepin and venlafaxine does not seem to be influenced significantly by valproic acid, but possibly further steps in the metabolic pathways.
According to the results of this naturalistic study, there is a significant influence of valproic acid comedication on the dose-corrected doxepin+N-doxepin serum concentration (mean elevation of 124%) and on the dose-corrected O-desmethylvenlafaxine serum concentration (mean elevation of 27%), but only a trend of an influence on the dose-corrected venlafaxine+O-desmethylvenlafaxine serum concentration (mean elevation 17%). Adverse events were not documented systematically in this study, but case reports in the literature suggest that especially in treatment with tricyclic antidepressants, severe adverse effects can be induced by a considerable increase in serum levels (Avoni et al., 1996; DeToledo et al., 1997; Unterecker et al., 2013). The significant positive correlation between valproic acid serum level and dose-corrected doxepin+N-doxepin serum level indicates that in addition to a careful dosage of doxepin lower valproic acid doses are also advisable. To the best of our knowledge, no report of a significant correlation between the serum levels of an antidepressant and a mood stabilizer has been published thus far; yet, clinicians should be aware of such an interaction. As a consequence, a combination treatment of valproic acid and tricyclic antidepressant drugs such as amitriptyline, nortriptyline, doxepin, or clomipramine should be avoided and other antidepressant drugs with a better safety profile and less interaction potential should be preferred. A comedication of valproic acid and venlafaxine should also be administered with caution. If valproic acid is applied in combination with these antidepressants, for reasons of safety, they should be used with great caution, avoiding high doses completely and administering half of the usual dose. Dose adjustment by TDM will be very helpful and should be used regularly if available.
Acknowledgements
The authors gratefully acknowledge the staff of the TDM laboratory of the Department of Psychiatry, Psychosomatics and Psychotherapy, University Hospital of Würzburg, R. Burger, M. Burger, R. Schreiner, and M. Weyer.
Conflicts of interest
S.U. has received travel and accommodation expenses from Astra Zeneca, Pfizer, and Janssen. A.R. has received speaker’s honoraria from Otsuka and research grants from Astra Zeneca. P.R. has received honorarium from Merz-Pharmaceuticals GmbH. J.D. has received speaker’s honoraria from Janssen, Bristol-Myers Squibb, Wyeth, Lundbeck, Astra Zeneca, and Pfizer and grant support from Medice. B.P. has received speaker’s honoraria from Astra Zeneca, Janssen, and Pfizer. For the remaining authors there are no conflicts of interest.
References
- Amsterdam JD, Brunswick DJ.Antidepressant monotherapy for bipolar type II major depression.Bipolar Disord 2003;5:388–395 [DOI] [PubMed] [Google Scholar]
- Angalakuditi M, Angalakuditi N.A comprehensive review of the literature on epilepsy in selected countries in emerging markets.Neuropsychiatr Dis Treat 2011;7:585–597 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Avoni P, Riva R, Albani F.Recurrence of absence seizures induced by a low dose of amitriptyline: a case report.Eur J Neurol 1996;3:272–274 [DOI] [PubMed] [Google Scholar]
- Bisdorff AR.Management of vestibular migraine.Ther Adv Neurol Disord 2011;4:183–191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bond DJ, Lam RW, Yatham LN.Divalproex sodium versus placebo in the treatment of acute bipolar depression: A systematic review and meta-analysis.J Affect Disord 2010;124:228–234 [DOI] [PubMed] [Google Scholar]
- Bowden CL.Valproate.Bipolar Disord 2003;5:189–202 [DOI] [PubMed] [Google Scholar]
- Bril V, England JD, Franklin GM, Backonja M, Cohen JA, Del Toro DR, et al. Evidence-based guideline: treatment of painful diabetic neuropathy – report of the American association of neuromuscular and electrodiagnostic medicine, the American academy of neurology, and the American academy of physical medicine & rehabilitation.Muscle Nerve 2011;43:910–917 [DOI] [PubMed] [Google Scholar]
- DeToledo JC, Haddad H, Ramsay RE.Status epilepticus associated with the combination of valproic acid and clomipramine.Ther Drug Monit 1997;19:71–73 [DOI] [PubMed] [Google Scholar]
- Dietrich DE, Emrich HM.The use of anticonvulsants to augment antidepressant medication.J Clin Psychiatry 1998;59:51–58 [PubMed] [Google Scholar]
- Fehr C, Gründer G, Hiemke C, Dahmen N.Increase of serum clomipramine concentrations caused by valproate.J Clin Psychopharmacol 2000;20:493–494 [DOI] [PubMed] [Google Scholar]
- Fogelman SM, Schmider J, Venkatakrishnan K, von Moltke LL, Harmatz JS, Shader RI, et al. O- and N-demethylation of venlafaxine in vitro by human liver microsomes and by microsomes from cDNA-transfected cells: effect of metabolic inhibitors and SSRI antidepressants.Neuropsychopharmacology 1999;20:480–490 [DOI] [PubMed] [Google Scholar]
- Fu C, Katzman M, Goldbloom DS.Valproate/nortriptyline interaction.J Clin Psychopharmacol 1994;14:205–206 [DOI] [PubMed] [Google Scholar]
- Haritos VS, Ghabrial H, Ahokas JT, Ching MS.Role of cytochrome P450 2D6 (CYP2D6) in the stereospecific metabolism of E- and Z-doxepin.Pharmacogenetics 2000;10:591–603 [DOI] [PubMed] [Google Scholar]
- Härtter S, Tybring G, Friedberg T, Weigmann H, Hiemke C.The N-demethylation of the doxepin isomers is mainly catalyzed by the polymorphic CYP2C19.Pharm Res 2002;19:1034–1037 [DOI] [PubMed] [Google Scholar]
- Hiemke C, Baumann P, Bergemann N, Conca A, Dietmaier O, Egberts K, et al. AGNP Consensus Guidelines for Therapeutic Drug Monitoring in Psychiatry: Update 2011.Pharmacopsychiatry 2011;44:195–235 [DOI] [PubMed] [Google Scholar]
- Joseph AB, Wroblewski BA.Potentially toxic serum concentrations of desipramine after discontinuation of valproic acid.Brain Inj 1993;7:463–465 [DOI] [PubMed] [Google Scholar]
- Kirchheiner J, Meineke I, Müller G, Roots I, Brockmöller J.Contributions of CYP2D6, CYP2C9 and CYP2C19 to the biotransformation of E- and Z-doxepin in healthy volunteers.Pharmacogenetics 2002;12:571–580 [DOI] [PubMed] [Google Scholar]
- Koszewska I, Rybakowski JK.Antidepressant-induced mood conversions in bipolar disorder: a retrospective study of tricyclic versus non-tricyclic antidepressant drugs.Neuropsychobiology 2009;59:12–16 [DOI] [PubMed] [Google Scholar]
- McAlpine DE, Biernacka JM, Mrazek DA, O’Kane DJ, Stevens SR, Langman LJ, et al. Effect of cytochrome P450 enzyme polymorphisms on pharmacokinetics of venlafaxine.Ther Drug Monit 2011;33:14–20 [DOI] [PubMed] [Google Scholar]
- Miller JM, Kustra RP, Vuong A, Hammer AE, Messenheimer JA.Depressive symptoms in epilepsy: prevalence, impact, aetiology, biological correlates and effect of treatment with antiepileptic drugs.Drugs 2008;68:1493–1509 [DOI] [PubMed] [Google Scholar]
- Patsalos PN, Perucca E.Clinically important drug interactions in epilepsy: interactions between antiepileptic drugs and other drugs.Lancet Neurol 2003;2:473–481 [DOI] [PubMed] [Google Scholar]
- Perucca E.Clinically relevant drug interactions with antiepileptic drugs.Br J Clin Pharmacol 2005;61:246–255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pisani F, Primerano G, Amendola D’Agostino A, Spina E, Fazio A.Valproic acid–amitriptyline interaction in man.Ther Drug Monit 1986;8:382–383 [PubMed] [Google Scholar]
- Roberts-Thomson KC, Teo KS, Young GD.Drug-induced Brugada syndrome with ST-T wave alternans and long QT.Intern Med J 2007;37:199–200 [DOI] [PubMed] [Google Scholar]
- Shams MEE, Arneth B, Hiemke C, Dragicevic A, Müller MJ, Kaiser R, et al. CYP2D6 polymorphism and clinical effect of the antidepressant venlafaxine.J Clin Pharm Ther 2006;31:493–502 [DOI] [PubMed] [Google Scholar]
- Spina E, Perucca E.Clinical significance of pharmacokinetic interactions between antiepileptic and psychotropic drugs.Epilepsia 2002;43:37–44 [DOI] [PubMed] [Google Scholar]
- Stephen LJ.Drug treatment of epilepsy in elderly people: focus on valproic acid.Drugs Aging 2003;20:141–152 [DOI] [PubMed] [Google Scholar]
- Unterecker S, Burger R, Hohage A, Deckert J, Pfuhlmann B.Interaction of valproic acid and amitriptyline – analysis of therapeutic drug monitoring data under naturalistic conditions.J Clin Psychopharmacol 2013;33:561–564 [DOI] [PubMed] [Google Scholar]
- Vandel S, Bertschy G, Jounet JM, Allers G.Valpromide increases the plasma concentrations of amitriptyline and its metabolite nortriptyline in depressive patients.Ther Drug Monit 1988;10:386–389 [PubMed] [Google Scholar]
- Wasterlain CG, Baldwin R, Naylor DE, Thompson KW, Suchomelova L, Niquet J.Rational polytherapy in the treatment of acute seizures and status epilepticus.Epilepsia 2011;52:70–71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wen X, Wang JS, Kivistö KT, Neuvonen PJ, Backman JT.In vitro evaluation of valproic acid as an inhibitor of human cytochrome P450 isoforms: preferential inhibition of cytochrome P450 2C9 (CYP2C9).Br J Clin Pharmacol 2001;52:547–553 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong SL, Cavanaugh J, Shi H, Awni WM, Granneman GR.Effects of divalproex sodium on amitriptyline and nortriptyline pharmacokinetics.Clin Pharmacol Ther 1996;60:48–53 [DOI] [PubMed] [Google Scholar]


