Abstract
Pharmacotherapy still seems to play a major role in the treatment of patients suffering from borderline personality disorder (BPD). However, little is known about psychiatrists’ detailed perspective on indication and significance of medication. A total of 233 psychiatrists in the city of Munich and in Upper Bavaria were asked by questionnaire about their treatment habits in the medical treatment of patients with BPD. One hundred and forty-one psychiatrists answered the questionnaire (60.5%). In total, 94% of BPD patients were treated with psychotropic medication. Psychiatrists predominantly saw an indication to prescribe antidepressants (98%), followed by antipsychotics, mood stabilizers, and benzodiazepines. Citalopram/escitalopram and quetiapine were mentioned most frequently. The results are discussed in conjunction with the international guidelines for the treatment of BPD.
Keywords: borderline personality disorder, pharmacological treatment, questionnaire, treatment guidelines
Introduction
In the treatment of patients suffering from borderline personality disorder (BPD), long-term and disorder-specific psychotherapy is commonly accepted as the most successful approach (Stoffers et al., 2012). There is no strong evidence for pharmacotherapy, since randomized controlled trials (RCT) are rare and mostly have small sample sizes. Lieb et al. (2010) identified only 27 RCTs between 1979 and 2008 that reached the quality criteria to be included in a systematic Cochrane analysis. The sample size varied from 16 to 341 participants, involving 1714 BPD patients in total (Lieb et al., 2010). To illustrate the contrast to other fields of psychopharmacological research, a Cochrane analysis comparing the effectiveness of one second-generation antipsychotic with several others found 50 studies with 9476 participants (Komossa et al., 2010). Despite the small evidence base, pharmacological treatment is widely used in BPD therapy. According to Mercer et al. (2009), up to 70% of all BPD patients are taking psychotropic medication on a regular basis. All prescriptions given are in fact ‘off-label use’, because specific pharmacotherapy does not exist; rather, drugs have to be given for different indications, for example, for the treatment of a comorbid depressive disorder. The picture becomes more complex when considering study data on the treatment of depression in BPD, which suggest a very limited benefit of the ‘standard’ group of medication, the selective serotonine reuptake inhibitor (SSRI). To date, no study has found significant effects (Lieb et al., 2010). Little is known about the extent to which these study results have an influence on clinicians’ treatment habits in daily routine. Clinicians are faced with an even more complicated situation as different treatment guidelines make dissimilar recommendations. For example, the most important guidelines published in the UK [National Institute for Health and Clinical Excellence (NICE), 2009] and the USA (APA, 2001) suggest quite contrary treatment strategies, with almost no pharmacological treatment by NICE and a more symptom-oriented approach by the APA (Tyrer and Silk, 2010). In the present study, a survey was conducted with psychiatrists in the city of Munich and the rural region of Upper Bavaria by questionnaire about their treatment habits in the medical treatment of BPD patients.
Materials and methods
A questionnaire was sent to all psychiatrists in private practices in the city of Munich and the region of upper Bavaria in May 2010. The sample was identified by the ‘Kassenärztliche Vereinigung Upper Bavaria’, an organization every physician of the region has to be a member of. We found 235 practices: 233 were reached by mail and two had given up their practice. Two further psychiatrists were not eligible, due to a very specialized service offered (e.g. substitution therapy for addicted patients only).
The questionnaire consisted of three sections. First, characteristics of a typical patient suffering from BPD were presented, to ensure that the physicians surveyed understood correctly the patient population they were being asked about. In the second part, psychiatrists were asked to provide information regarding their age, years in profession, training experience, predominant method of working, utilization of supervision, and advanced training. In addition, we asked about the amount of experience with BPD patients, their attitude toward BPD treatment, and willingness to treat BPD patients. In the third part we asked about treatment habits concerning BPD patients in the fields of antidepressants (ADs), antipsychotics (AP), mood stabilizers, benzodiazepines, and other medication (e.g. stimulants). We finally asked about the individual’s experience in the treatment of the last four BPD patients (how many substance groups were used, the anticipation of treatment outcome, and which further support could possibly be of help in the treatment of BPD patients).
This study was approved by the local ethics committee (Ethikkommission der TU Muenchen, 2683/10). The statistical analyses were carried out with SPSS for Windows (version 18.0; IBM, Deutschland, Ehningen, Germany). All data are presented descriptively as means and SDs; group differences on categorical data were examined by χ2-tests.
Results
Of 233 psychiatrists, 141 answered our questionnaire, equivalent to a return rate of 60.5%.
Sample characteristics
The psychiatrists were on average 51.77 years of age (range: 32–68 years), 58% male, 41% female (two answers missing). Eighty-seven percent had additional training in psychotherapy and 13% did not. Of those colleagues trained in psychotherapy, 84% completed training in psychoanalysis or psychodynamic therapy, 39% in cognitive behavioral therapy, and 13% in further methods (e.g. humanistic psychotherapy, dialectic behavioral therapy, transference-focused psychotherapy, trauma therapy). As their predominant method of working, 29% reported prescribing medication only, 41% had a psychotherapeutic focus, and 20% a combination of medical and psychotherapeutic practice. Twenty-six percent offered methods beyond academic medicine (e.g. homeopathy, relaxation techniques, traditional Chinese medicine). Psychiatrists attended between 10 and 220 h of continued medical education per year, on average 56 h. Thirty-seven percent attended no case supervision and the remainder received an average of 15.1 h of supervision per year (range 10–200 h/year).
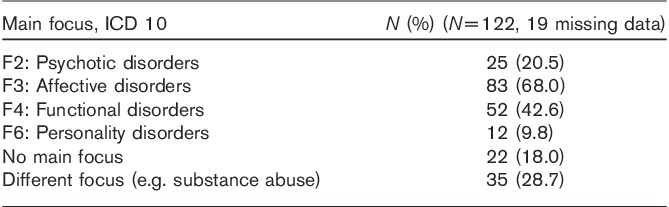
The primary diagnoses of the patients treated by our psychiatrists are shown in Table 1.
Table 1.
Main focus in daily work
Borderline personality disorder treatment in psychiatric practices
Only 2.9% of the sample answered that they were not treating patients with the characteristic symptoms given in the preamble to the questionnaire. Forty-one percent answered that they treated up to five BPD patients per quarter (calendar year divided into four 3-month sections), 26% up to 10, and 30% more than 10 BPD patients per quarter.
Concerning their willingness to treat BPD, 59% of the sample stated that they did not have any objections to caring for BPD patients; 61% answered that they do support patients in finding a psychotherapist. In contrast, 13% said they never accepted BPD patients or that they would do this ‘under extraordinary circumstances’ only. Another 18% tried to ‘first refer patients to a colleague’ and 10% would accept only a limited number of BPD patients per quarter (on average four per quarter).
Pharmacological treatment strategies
The psychiatrists weighted the value of pharmacotherapy versus psychotherapy in BPD treatment with a slight predominance for psychotherapy on a 10-point visual rating scale (mean: 4.8 medication vs. 6.2 psychotherapy).
With regard to the pattern of treatment habits, no statistically significant differences were found when comparing younger (<51 years) versus older (>51 years), male versus female colleagues, and with versus without psychotherapeutic training.
In their last four BPD treatments, psychiatrists had prescribed one or two psychotropic substances to 81% of their patients, 13% of the patients were treated with up to 5 different substances, and 6% were not treated with medication.
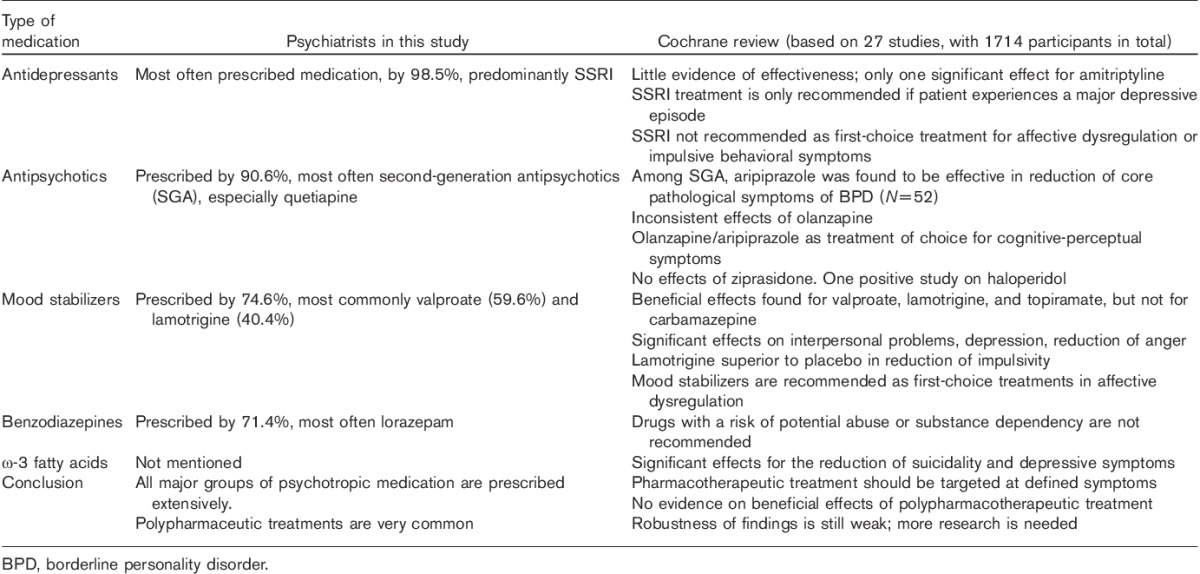
In total, 98.5% of the psychiatrists typically prescribe ADs to BPD patients; predominantly SSRI (86.8%) and serotonin–noradrenaline reuptake inhibitors (42.6%) were mentioned. Citalopram and escitalopram were the most commonly named (58.9% of the AD prescribers). A total of 16.3% of the AD prescribers apply tricyclic antidepressants, and only 1.5% of all psychiatrists did not feel that the prescription of AD was indicated.
With regard to AP, 90.6% of all psychiatrists reported using medication out of this class, and 9.4% stated that these drugs are not indicated in the treatment of BPD. Among the AP-prescribing psychiatrists, 92.2% use second-generation medication, most often quetiapine (70.1% of all AP prescribers), followed by olanzapine (18.7%). A total of 25.9% also think that the use of low-potency first-generation antipsychotics such as levomepromazine or promethazine can be indicated; only 3.4% would use high-potency first-generation antipsychotics such as haloperidol.
A total of 74.6% psychiatrists prescribe mood stabilizers, most commonly valproate (59.6%), followed by lamotrigine (40.4%), lithium (22.3%), and carbamazepine (20.2%).
Benzodiazepines are prescribed by 71.4% physicians, whereas 28.6% see no indication in this diagnosis. There was a preference for benzodiazepines with mainly anxiety-reducing properties, for example, lorazepam was used by 60% of these colleagues. Sixteen percent mentioned benzodiazepines with a short half-life (e.g. lormetazepam).
Treatment habits of this sample of psychiatrists are contrasted with the Cochrane review’s recommendations in Table 2.
Table 2.
Medication in borderline personality disorder treatment: group of psychiatrists in this study vs. Cochrane systematic review (Lieb et al., 2010)
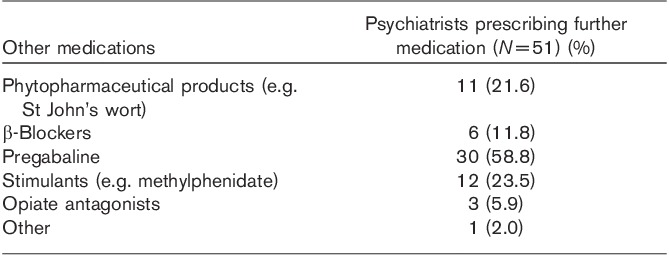
Other types of medication were prescribed by 51 psychiatrists for the treatment of BPD, details of which are summarized in Table 3.
Table 3.
Further medication in borderline personality disorder treatment
With regard to the treatment outcome, 17% of the psychiatrists answered that they expected a negative result, 2% a very negative treatment result, 55% saw two of the four patients significantly improving, and 26% were optimistic or very optimistic (answering on a five-point Likert scale).
Discussion
This study has two main results. First, pharmacological treatment plays a major role in the treatment of BPD in the field. It appears that the psychiatrists in our sample do not feel confident with the choice of psychological treatment over medication, as suggested by the literature (e.g. NICE, 2009). Second, and most surprising, although evidence is weak and guidelines are contradictory, the vast majority of the studied psychiatrists applied a similar pattern of prescription. ADs were more often prescribed than AP, and the latter more often than mood stabilizers. In the analysis of the individual substances, citalopram/escitalopram and quetiapine were widely accepted, although there is no RCT supporting this choice. In contrast to BPD psychotherapists, 37% of this sample of psychiatrists did not engage in regular case supervision of their treatments, and another 30% attended supervision less than 10 h/year (c.f. Jobst et al., 2010). This may explain the fact that about 30% of psychiatrists in this study apparently avoid BPD treatments.
Our finding of treatment habits that widely prescribe all major groups of psychotropic substances for the treatment of BPD may also reflect a pronounced ambiguity. On one hand, the psychiatrists used all types of medication for nearly every patient, but on the other they stated that they expected a definite improvement only in a quarter of the treated patients. In addition, they stated that psychotherapy was slightly more important than medication for the treatment of BPD. Both of these findings may hint at a lack of adequate treatment options, with medication as a kind of fill-in coping strategy. The large numbers of BPD patients seeking treatment per quarter reported by the majority of our sample seem to be in line with the percentages of BPD diagnoses in outpatient treatments calculated by Bohus (2002).
Comparing our results to the literature, it is striking that our sample describes a conservative way of treating BPD patients, with SSRI still playing a major role in pharmacotherapy. In pharmacological research these substances have been outdated by mood stabilizers and atypical AP (Abraham and Calabrese, 2008; Feurino and Silk, 2011). It is possible that a future survey will reflect the current trends of pharmacological research, because our study just gives a snapshot of present day-to-day practice. The quite frequent use of pregabalin (c.f. Table 2) may be a result of a temporary trend in treating anxiety disorders, commonly co-occurring with BPD. During mid-2010, when the questionnaire was conducted, only the first articles concerning the potential abuse of pregabalin were published (e.g. Filipetto et al., 2010), whereas by now more detailed objections especially in the treatment of patients with a history of drug abuse or BPD are available (Gahr et al., 2013a, 2013b).
In addition, the international literature indicates different treatment strategies in different countries. For example, while British authors such as Haw and Stubbs (2011) or Vohra (2010) emphasize the value of clozapine in the treatment of BPD patients, none of the psychiatrists in our sample even mentioned this substance.
Our findings also lead to the question as to the extent to which guidelines and RCTs have an impact on daily treatment in clinical practice. On one hand, RCTs contribute strongly to the development of treatment guidelines and on the other, documented differences between the patient population of RCTs and ‘real-life’ conditions raise doubts about the generalizability of RCT results. Eligible nonparticipants of an RCT on borderline treatment were found to have a lower level of functioning (general assessment of functioning score), were more frequently living alone, and showed comorbid affective and anxiety disorders more often. Moreover, nonparticipants showed a higher number of discontinued psychotherapeutic treatment approaches (Rentrop et al., 2010). British authors found that pharmacotherapy of BPD is still common in the UK, even after the NICE guidelines asserted that ‘drug treatment should not be used specifically for BPD or for the individual symptoms or behavior associated with the disorder’ (NICE, 2009). In the survey by Haw and Stubbs (2011), 80% of the BPD patients received medication, 48% two or more psychotropic substances. Our results suggest an even higher rate of pharmacological treatment, with 94% of BPD patients treated with medication and 13% with three to five different substances at once. Rogers and Acton (2012) suggested in a qualitative interview study that various medications had been applied instead of psychological treatment in the past and the implementation of the NICE guideline led to a broader offer given by specialist BPD psychotherapists. This result suggests that the problems in the long-term care of BPD patients are quite similar in the UK and Germany, in that German patients also do not regularly receive BPD-specific psychotherapy (Jobst et al., 2010). McMain et al. (2009, 2012) introduced, through the ‘general psychiatric management program’, an approach that goes beyond a dichotomous distribution of borderline therapy in psychotherapy versus medication. The group of psychiatrists studied in our questionnaire most likely applied supportive psychotherapeutic counseling in addition to the prescribing of medication, but most certainly not in a structured or manualized form. Programs like the one studied by McMain would be of great interest for German psychiatrists, especially as the majority of colleagues have the prerequisites for an advanced training in specialized borderline treatment, given their basic education in psychotherapy. Above all, our questionnaire suggests a need for intensified continuing education for psychiatrists. We did not gather information on the participation in quality circles, which exist in the Munich region, and which also may help decrease the gap between treatment recommendations and habits of daily routine.
This study has some limitations. First, information was gathered with a nonstandardized instrument, and second, only physicians from a relatively small region were surveyed, with just one city and the surrounding rural region. However, the return rate of 60% implies that the results are generalizable for outpatient psychiatrists both in this major city and the rural surroundings.
Conclusion
We have shown that pharmacological treatment still plays a major role in the treatment of patients suffering from BPD. As recommendations in drug treatment of BPD are weak (Schwerthöffer et al., 2013), we suggest conducting more studies exploring accepted customs. Our results emphasize the need for further studies, in particular on quetiapine and citalopram/escitalopram. In addition, more studies are needed that explore the rationale of the differences found here, with psychotherapy being recommended by psychiatrists on one hand, and an obvious preference for prescribing medication in daily routine on the other.
Acknowledgements
Conflicts of interest
Michael Rentrop has received lecture honoraria from Janssen Cilag (Johnson & Johnson), EliLilly, Pfizer, AstraZeneca, and EssexPharma. Stefan Leucht has received in the last 3 years honoraria for lectures from AstraZeneca, BristolMyersSquibb, ICON, EliLilly, Janssen, Johnson & Johnson, Roche, SanofiAventis, Lundbeck, and Pfizer, and for consulting/advisory boards from Roche, EliLilly, Medavante, BristolMyersSquibb, Alkermes, Janssen, Johnson & Johnson, and Lundbeck. EliLilly has provided medication for a study with SL as primary investigator. For the remaining authors there are no conflicts of interest.
References
- Abraham PF, Calabrese JR.Evidenced-based pharmacologic treatment of borderline personality disorder: a shift from SSRIs to anticonvulsants and atypical antipsychotics?J Affect Disord 2008;111:21–30 [DOI] [PubMed] [Google Scholar]
- APA Practice guidelines for the treatment of patients with borderline personality disorder 2001Washington, DC, USA:APA [Google Scholar]
- Bohus M.Borderline-Störung 2002Göttingen:Hogrefe [Google Scholar]
- Feurino L, Silk KR.State of the art in the pharmacologic treatment of borderline personality disorder.Curr Psychiatry Res 2011;13:69–75 [DOI] [PubMed] [Google Scholar]
- Filipetto FA, zipp CP, Coren JS.Potential for pregabalin abuse or diversion after past drug-seeking behavior.J Am Osteopath Assoc 2010;110:605–607 [PubMed] [Google Scholar]
- Gahr M, Franke B, Freudenmann RW, Kölle MA, Schönfeldt-Lecuona C.Concerns about pregabalin: further experience with its potential of causing addictive behaviors.J Addict Med 2013a;7:147–149 [DOI] [PubMed] [Google Scholar]
- Gahr M, Freudenmann RW, Hiemke C, Kölle MA, Schönfeldt-Lecuona C.Pregabalin abuse and dependence in Germany: results from a database query.Eur J Clin Pharmacol 2013b;69:1335–1342 [DOI] [PubMed] [Google Scholar]
- Haw C, Stubbs J.Medication for borderline personality disorder: a survey at a secure hospital.Int J Psychiatry Clin Pract 2011;15:280–285 [DOI] [PubMed] [Google Scholar]
- Jobst A, Hörz S, Birkhofer A, Martius P, Rentrop M.Psychotherapists' attitudes towards the treatment of patients with borderline personality disorder. [in German].Psychother Psychosom Med Psychol 2010;60:126–131 [DOI] [PubMed] [Google Scholar]
- Komossa K, Rummel-Kluge C, Hunger H, Schmid F, Schwarz S, Duggan L, et al. Olanzapine versus other atypical antipsychotics for schizophrenia.Cochrane Database Syst Rev 2010;17:CD006654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lieb K, Völlm B, Rücker G, Timmer A, Stoffers J.Pharmacotherapy for borderline personality disorder: Cochrane systematic review of randomised trials.Br J Psychiatry 2010;196:4–12 [DOI] [PubMed] [Google Scholar]
- McMain SF, Links PS, Gnam WH, Guimond T, Cardish RJ, Korman L, Streiner DL.A randomized trial of dialectical behavior therapy versus general psychiatric management for borderline personality disorder.Am J Psychiatry 2009;166:1365–1374 [DOI] [PubMed] [Google Scholar]
- McMain SF, Guimond T, Streiner DL, Cardish RJ, Links PS.Dialectical behavior therapy compared with general psychiatric management for borderline personality disorder: clinical outcomes and functioning over a 2-year follow-up.Am J Psychiatry 2012;169:650–661 [DOI] [PubMed] [Google Scholar]
- Mercer D, Douglass AB, Links PS.Meta-analysis of mood-stabilizers, antidepressants and antipsychotics in the treatment of borderline personality disorder: effectiveness for depression and anger symptoms.J Pers Disord 2009;23:156–174 [DOI] [PubMed] [Google Scholar]
- National Institute for Health and Clinical Excellence (NICE) NICE clinical guideline 78 Borderline personality disorder: treatment and management 2009London:NICE; [PubMed] [Google Scholar]
- Rentrop M, Martius P, Bäuml J, Buchheim P, Doering S, Hörz S.Patients with borderline personality disorder not participating in an RCT: are they different?Psychopathology 2010;43:369–372 [DOI] [PubMed] [Google Scholar]
- Rogers B, Acton T.‘I think we’re all guinea pigs really’: a qualitative study of medication and borderline personality disorder.J Psychiatr Ment Health Nurs 2012;19:341–347 [DOI] [PubMed] [Google Scholar]
- Schwerthöffer D, Bäuml J, Rentrop M.Pharmacological treatment for patients with borderline personality disorder: practice and study results. [in German].Fortschr Neurol Psychiatr 2013;81:437–443 [DOI] [PubMed] [Google Scholar]
- Stoffers JM, Völlm BA, Rücker G, Timmer A, Huband N, Lieb K, The Cochrane Collaboration Psychological therapies for people with borderline personality disorder [review] 2012New York:Wiley; [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tyrer P, Silk KR.A comparison of UK and US guideline for drug treatment in borderline personality disorder.Int Rev Psychiatry 2010;23:388–394 [DOI] [PubMed] [Google Scholar]
- Vohra AK.Treatment of severe borderline personality disorder with clozapine.Indian J Psychiatry 2010;52:267–269 [DOI] [PMC free article] [PubMed] [Google Scholar]


