A systematic review and meta-analysis were performed to evaluate the impact of resident duty hours (RDH) on clinical and educational outcomes in surgery. A total of 135 articles met inclusion criteria. In surgery, recent RDH changes are not consistently associated with improved resident well-being and may have negative impacts on patient outcomes and education.
Keywords: burnout, patient outcomes, patient safety, postgraduate surgical training, residents, resident duty hours, resident wellness, surgical education
Abstract
Background:
In 2003, the Accreditation Council for Graduate Medical Education (ACGME) mandated 80-hour resident duty limits. In 2011 the ACGME mandated 16-hour duty maximums for PGY1 (post graduate year) residents. The stated goals were to improve patient safety, resident well-being, and education. A systematic review and meta-analysis were performed to evaluate the impact of resident duty hours (RDH) on clinical and educational outcomes in surgery.
Methods:
A systematic review (1980–2013) was executed on CINAHL, Cochrane Database, Embase, Medline, and Scopus. Quality of articles was assessed using the GRADE guidelines. Sixteen-hour shifts and night float systems were analyzed separately. Articles that examined mortality data were combined in a random-effects meta-analysis to evaluate the impact of RDH on patient mortality.
Results:
A total of 135 articles met the inclusion criteria. Among these, 42% (N = 57) were considered moderate-high quality. There was no overall improvement in patient outcomes as a result of RDH; however, some studies suggest increased complication rates in high-acuity patients. There was no improvement in education related to RDH restrictions, and performance on certification examinations has declined in some specialties. Survey studies revealed a perception of worsened education and patient safety. There were improvements in resident wellness after the 80-hour workweek, but there was little improvement or negative effects on wellness after 16-hour duty maximums were implemented.
Conclusions:
Recent RDH changes are not consistently associated with improvements in resident well-being, and have negative impacts on patient outcomes and performance on certification examinations. Greater flexibility to accommodate resident training needs is required. Further erosion of training time should be considered with great caution.
After the tragic death of a young woman named Libby Zion in a New York Hospital, resident duty hour (RDH) restrictions were introduced in this state. An investigation ruled that lack of supervision, the resident's lack of familiarity with this woman's complex diagnosis and resident fatigue were contributing factors in the tragic outcome. In July 2003, the Accreditation Council for Graduate Medical Education (ACGME) mandated an 80-hour duty limit on residents, averaged over a 4-week period. In 2011, the ACGME mandated 16-hour duty periods for first year residents whereas the province of Quebec instituted 16-hour periods for all in-house residents in 2012. The stated goals of duty hour limitations were to improve patient safety, resident well-being, and education.1 Surgical disciplines have expressed concern with the contraction of duty hours stating that the impact on training time could have a negative effect on educational and patient outcomes.2 Specifically, the American College of Surgeons, Division of Education, has stated that mastery in surgery requires extensive and immersive experiences.3 A “one-size fits all” approach to RDHs may not be appropriate given the variation in training needs, diversity of practice patterns, and various competencies required among disciplines.4,5
In March 2012, the Royal College of Physicians and Surgeons of Canada undertook a project to develop a pan-Canadian consensus on issues related to RDH. A national steering committee was struck and this committee further created 6 expert working groups. Recognizing that surgical training is unique in many aspects and that there have been significant obstacles related to the implementation of RDH in surgery, a specific working group entitled Special Considerations for Procedural and Surgical Disciplines was created. The National Steering Committee's full report is published elsewhere (www.residentdutyhours.ca).5 As part of this process, the Procedural/Surgical discipline working group performed a systematic review and meta-analysis to evaluate the association between RDH and clinical and educational outcomes in surgery.
METHODS
Study Selection
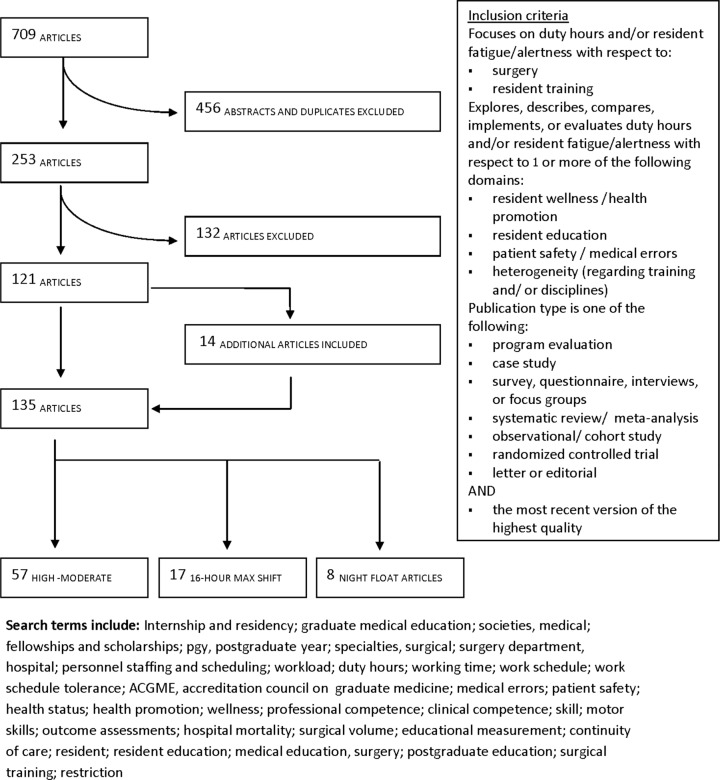
A systematic review (1980–2013) was executed using indexed databases CINAHL, Cochrane Databases, Embase, Medline, and Scopus to identify pertinent articles relating to RDH restrictions with a focus on identifying articles that addressed the 2011 ACGME regulation and Quebec arbitration. Search terms were developed and revised by experts in surgical education. Predetermined eligibility criteria were used to eliminate articles beyond the scope of this review. Articles were included if the research focus was related to the impact of RDH restrictions on surgical resident well-being, education, and/or patient safety. Articles were also included if they addressed heterogeneity across different residency training programs and the varying impacts of RDH on different fields of health care. All abstracts and titles were reviewed by 2 members of the research team for inclusion in review (K.D. and I.K.). To ensure the comprehensive inclusion of high-quality literature on this topic, additional articles identified from hand searching of references and recommendations from content experts were added (Fig. 1).
FIGURE 1.
Study selection and inclusion criteria.
Data Abstraction and Analysis
Quantitative and qualitative data extractions were performed independently by 2 members of the research team for all studies meeting the inclusion criteria. If consensus could not be reached, disputes were resolved by a third member of the research team (N.A.). The quality of the articles was assessed using the GRADE guidelines.6 Each article was rated on a 4-point scale from high to very low, based on the level of confidence in the effect estimate. Attributions for consideration of high quality included multicentre designs, high volume of participants (>100), and control groups and that of low quality included unvalidated surveys and single institutional studies.
Extracted data were tabulated and examined for interpretation. Articles identified as moderate and high quality were analyzed separately. Articles graded as low or very low quality were not included in our overall analysis to maintain the integrity of the results. All articles examining 16-hour and night float shifts were analyzed and reported separately to determine the effects of more recent changes. Major findings for patient safety, resident well-being, and education were divided into actual and perceived impact. The term “unclear” was used to categorize studies that reported contradictory results or when the abstractors were unable to draw firm conclusions from the article.
Qualitative analysis was completed using the grounded theory approach. Open and axial coding was executed to capture themes from articles relevant to the 3 areas identified as sensitive to RDH restrictions: patient safety, resident well-being, and education. Themes were tabulated and refined. Qualitative themes are reported to add context to the quantitative data. Detailed results of the qualitative review will be reported separately.
Statistical Analysis
Articles that examined mortality data were combined in a random-effects meta-analysis to evaluate the impact of RDH on patient outcomes. The analysis was conducted in the statistical program R using the metafor package.7,8 An odds ratio greater than 1 means a higher risk of death for Pre-RDH, relative to Post-RDH and odds ratio less than 1 means a lower risk of death for Pre-RDH relative to Post-RDH. A random-effects model was fit using the restricted maximum likelihood estimator.
RESULTS
A total of 709 articles were identified from indexed sources (CINAHL: 50, Cochrane Databases: 4, Embase: 203, Medline: 301, Scopus: 151). After the review of abstracts, full articles, suggested papers from content experts, and hand searching of references 135 articles were identified as eligible for data analysis (Fig. 1).
Study Characteristics
Ninety-five percent (128) of the studies were conducted in the United States or Canada, with 53% of these being multicentre (Table 1). General surgery was the most commonly studied discipline, comprising half of all studies. The primary study designs were surveys (61, 45%), interventional studies, with the intervention being the implementation of RDH restrictions (52, 39%) and observational studies (8, 6%). Only 1 article used a randomized controlled trial to examine the impact of duty hour restrictions (1%). Overall study objectives were to evaluate the impact of duty hour restrictions on resident education (101, 75%), patient safety (79, 59%), and resident wellness (48, 36%). Nine articles (7%) specifically compared the effect of RDH on training in various specialties. Fifty-eight percent of articles were graded as low or very low quality (N = 78) and 42% of studies were graded as moderate or high quality (N = 57).
TABLE 1.
Characteristics of Articles (N = 135)
| Country | Study design | ||
|---|---|---|---|
| United States | 121 (90) | Survey | 61 (46) |
| Canada | 7 (5) | Interventional (≥2 groups) | 52 (39) |
| Europe | 6 (4) | Observational | 8 (6) |
| New Zealand | 1 (1) | Systematic review | 6 (4) |
| Type of center | Other | 5 (4) | |
| Academic | 86 (64) | Program evaluation | 2 (1) |
| Community | 20 (15) | Randomized controlled trial | 1 (1) |
| Multicentre | 71 (53) | ||
| Surgical subspecialty | Study objectives | ||
| General surgery | 67 (50) | Education | 101 (75) |
| Orthopedic | 15 (11) | Patient safety | 79 (59) |
| Gynecology | 13 (10) | Wellness | 48 (36) |
| Multi-specialty (including surgery) | 12 (9) | Heterogeneity | 9 (7) |
| All surgical specialties | 12 (9) | Study quality* | |
| Trauma | 10 (7) | High | 21 (15) |
| Other† | 10 (7) | Moderate | 36 (27) |
| ENT | 8 (6) | Low | 51 (38) |
| Pediatrics | 8 (6) | Very low | 27 (20) |
| Cardiac | 8 (6) | Type of surgery | |
| Neurosurgery | 6 (4) | Emergency | 95 (70) |
| Vascular | 5 (4) | Elective | 88 (65) |
| Thoracic | 5 (4) | Not described | 38 (28) |
| Urology | 3 (2) | ||
| Plastic | 3 (2) | ||
| Not described | 12 (9) |
All the values indicate n (%).
*Graded moderate-high quality as per Balshem et al.6
†Other categories include nonsurgical disciplines reported in combination with surgical subspecialties and infrequently reported surgical specialties (ophthalmology, transplant, and critical care).
Major findings of articles with respect to the impact of duty hour restrictions on patient safety, resident well-being, and education can be listed as follows (Table 2).
TABLE 2.
Summary of Effect of RDH Restrictions on Patient Safety and Educational Outcomes for Studies Graded as Moderate-High Quality, and for Studies Focusing on 16-Hour Duty Maximum and/or Night Float Systems
| Improved | Worsened | No Change | Unclear† | Total | |||||
|---|---|---|---|---|---|---|---|---|---|
| Effect of RDH Restrictions* | N | % | N | % | N | % | N | % | N |
| Section 1–-Moderate-high quality articles (N = 57)‡ | |||||||||
| Patient safety | 5 | 19 | 8 | 30 | 13 | 48 | 1 | 4 | 27 |
| Wellness | 5 | 71 | 0 | 0 | 2 | 29 | 0 | 0 | 7 |
| Education | 1 | 4 | 13 | 48 | 11 | 41 | 2 | 7 | 27 |
| Perception of wellness (survey) | 4 | 57 | 0 | 0 | 3 | 43 | 0 | 0 | 7 |
| Perception of education (survey) | 1 | 9 | 4 | 36 | 4 | 36 | 2 | 18 | 11 |
| Perception of patient safety (survey) | 0 | 0 | 6 | 67 | 2 | 22 | 1 | 11 | 9 |
| Section 2—16-h duty maximums (N = 17) | |||||||||
| Patient safety | 0 | 0 | 0 | 0 | 1 | 50 | 1 | 50 | 2 |
| Wellness | 0 | 0 | 0 | 0 | 2 | 100 | 0 | 0 | 2 |
| Education | 0 | 0 | 2 | 100 | 0 | 0 | 0 | 0 | 2 |
| Perception of wellness (survey) | 3 | 38 | 1 | 13 | 1 | 13 | 3 | 38 | 8 |
| Perception of education (survey) | 0 | 0 | 12 | 86 | 2 | 14 | 0 | 0 | 14 |
| Perception of patient safety (survey) | 0 | 0 | 11 | 79 | 2 | 14 | 1 | 7 | 14 |
| Section 3–-Night float systems (N = 8) | |||||||||
| Patient safety | 0 | 0 | 0 | 0 | 1 | 50 | 1 | 50 | 2 |
| Wellness | 1 | 100 | 0 | 0 | 0 | 0 | 0 | 0 | 1 |
| Education | 0 | 0 | 1 | 50 | 0 | 0 | 1 | 50 | 2 |
| Perception of wellness (survey) | 3 | 100 | 0 | 0 | 0 | 0 | 0 | 0 | 3 |
| Perception of education (survey) | 1 | 25 | 1 | 25 | 0 | 0 | 2 | 50 | 4 |
| Perception of patient safety (survey) | 1 | 33 | 2 | 67 | 0 | 0 | 0 | 0 | 3 |
| Section 4–-Both 16-h duty maximums and night float systems (N = 24) | |||||||||
| Patient safety | 0 | 0 | 0 | 0 | 2 | 67 | 1 | 33 | 3 |
| Wellness | 1 | 33 | 0 | 0 | 2 | 67 | 0 | 0 | 3 |
| Education | 0 | 0 | 2 | 67 | 0 | 0 | 1 | 33 | 3 |
| Perception of wellness (survey) | 6 | 55 | 1 | 9 | 1 | 9 | 3 | 27 | 11 |
| Perception of education (survey) | 1 | 6 | 12 | 71 | 2 | 12 | 2 | 12 | 17 |
| Perception of patient safety (survey) | 1 | 6 | 12 | 75 | 2 | 13 | 1 | 6 | 16 |
*RDH restrictions including 2003, 2008 ACGME guidelines and European working time directive guidelines. Four articles in this review assessed the impact on nonsurgical residents and surgical residents, 3 were included in the high quality review,20,34,43 3 were included in the review of the 16-hour max shift,34,70,72 and 1 was included in the review of the night float system.43
†Contradictory results or unable to draw firm conclusions from findings.
‡Graded moderate-high quality as per Balshem et al. (2011).6
Section 1: Effect of RDH Restrictions Including 2003, 2011 ACGME Restrictions and the European Working Time Directive, From 57 Moderate to High Quality Studies
Patient Safety. Thirty-five (61%) articles, graded moderate to high quality, examined patient safety; 8 (30%) of these reported worsened patient safety outcomes (morbidity and mortality) as a result of duty hour restrictions.9–16 Five (19%) reported an improvement17–21 and 13 (48%) reported no change.22–34 Of the 9 articles evaluating perceptions of RDH impact on patient safety, 6 (67%) reported a decrease in quality of care,35–40 and 2 (22%) reported no change.41,42 Thus, the current impact on patient safety is inconclusive, but perceptions of health care professionals suggest negative outcomes.
Resident Well-being. Of the 57 articles considered moderate to high quality, 9 (16%) examined resident wellness. Five (71%) reported that duty hour restrictions had improved resident wellness20,24,43–45 and 2 (29%) reported no change,34,37 as measured by validated tools such as Maslach Burnout Inventory. Of the 7 articles evaluating perception of wellness, 4 (57%) reported improvement after RDH24,42,44 and 3 (43%) reported no change.37,39,45 Overall, the majority of articles reported improved resident wellness.
Resident Education. Thirty-three (58%) articles graded as moderate to high quality examined resident education. Thirteen (48%) of these reported that educational outcomes were worsened after the implementation of RDH38,40,46–56 and 11 (41%) reported no change,22,24,26,32,45,57–62 using measures such as examination scores including American Board of Surgery certification data. Only 1 (4%) study showed an improvement in educational outcomes; the balance of studies showed worsened or no significant effects of RDH restrictions.44 Of the 11 articles evaluating self-reported perceptions of RDH impact on education, 4 (36%) reported a decrease in quality of the educational environment after RDH36,38–40 and 4 (36%) reported no change.35,37,42,61 Only 1 article (9%) reported a perceived improvement in education.43 Therefore, on the basis of objective tools of measurement and perceived impacts, findings suggest resident education has either worsened or remained unchanged after duty hour restrictions.
Section 2: Effect of the 16-Hour Duty Maximums on Patient Safety, Resident Well-being and Educational Outcomes From 17 Articles
Seventeen studies evaluated the impact of 16-hour duty maximums; 11 studies were low quality, 6 were moderate to high quality (Table 2).
Patient Safety. Fifteen articles examined the impact of the 16-hour duty maximum restrictions on patient safety. Two articles objectively analyzed the impact (eg, examined morbidity and mortality rates), 1 study had unclear results38 and the other reported no change.34 Of the 14 articles that evaluated the residents' perceptions of the impact of 16-hour duty maximum on patient safety, 11 (79%) reported that patient safety has declined,4,36–38,63–69 2 (14%) suggested there has been no effect,70,71 and 1 (7%) was inconclusive.72 Thus, the objective impact on patient safety is inconclusive, but the perceived impact suggests patient safety has declined. Decreased continuity of care and increased number of handovers were themes identified from the qualitative review as causes for a decline in patient outcomes after duty hour restrictions.
Resident Wellness, Fatigue, and Burnout. Nine of the 17 articles examined the impact of 16-hour duty hour restrictions on resident wellness; 2 articles using validated measures (eg, Maslach Burnout Inventory) concluded there has been no significant change. Eight articles examined the perceived impact; 3 (38%) reported improvement,64,70,72 1 (13%) suggested wellness was worse,67 1 (13%) reported no significant change,37 and 3 (38%) had unclear results.4,65,71 Validated tools suggest no significant change after RDH restrictions; findings from the perceived impact are unclear. Thematic review of the data suggests resident training, professional satisfaction, preparedness for more senior roles, and the wellness of more senior trainees has been compromised by the practice of 16-hour duty maximums.71
Resident Education. Fifteen articles evaluated impact of the 16-hour duty maximums on resident education; 2 objectively assessed the impact and concluded education was worse (eg, examination data and/or clinical performance).38,55 Fourteen examined the perceived impact; 12 (86%) articles concluded that education is worse4,36,38,64–72 and 2 (14%) reported no significant change.22,35,37 Overall, both the objective and perceived impact findings support a trend toward worsened outcomes. Thematic data analysis of the literature suggests 16-hour duty maximums result in poorer integration into teams and mentoring of residents, increased patient handover, decreased operative exposure, and increased self-reported medical errors.
Section 3: Effect of Night Float Systems From 8 Studies
Our analysis of the 8 studies examining night float systems showed that there was an improvement in resident wellness reported in 1 study,43 there were 2 studies that reported adverse or unclear effects on resident education,38,43 and 2 studies reported negative impacts on patient safety (Table 2).29,38 No studies of night float systems showed improved patient or resident educational outcomes using objective criteria. Survey data suggested improved resident wellness (N = 3 studies).43,73,74 Two studies reported a perception of worsening patient outcomes38,73 with an inconclusive effect on resident education.43,73
Section 4: Effect of 16-Hour Duty Maximums and Night Float Systems From 24 Studies
When considering the 24 articles examining both 16-hour duty maximums and night float systems, we found that 3 studies examined the effect of these call models on morbidity and mortality (Table 2).29,34,38 No studies showed an improvement or a worsening effect on patient safety as a result of these changes to RDH. Concerning resident wellness, 1 of 3 studies reported an improvement,43 whereas 2 studies reported no change in resident well-being.34,37 With respect to resident education, there were no studies showing improvement. Two studies showed worsened educational outcomes using examination data, access to operating room (OR) times, and clinical performance;38,55 in 1 study, the overall impact could not be determined.43 In more than half of the studies (6, 55%) using self-reported survey data, residents believed that their wellness had improved after 16-hour shift restrictions and/or the implementation of night float systems.43,64,70,72–74 Seventeen surveys queried self-reported educational outcomes and 12 (71%) surveys showed that educational outcomes were believed to have worsened;4,36,38,64–72 only 1 (6%) survey reported improved educational outcomes.73 Sixteen survey studies examined the effects of 16-hour or night float systems on perceptions of patient safety; 12 (75%) reported a perception of worsened patient outcomes,4,35–38,64–69,73 whereas 1 (6%) survey reported improved perceptions of patient safety.74
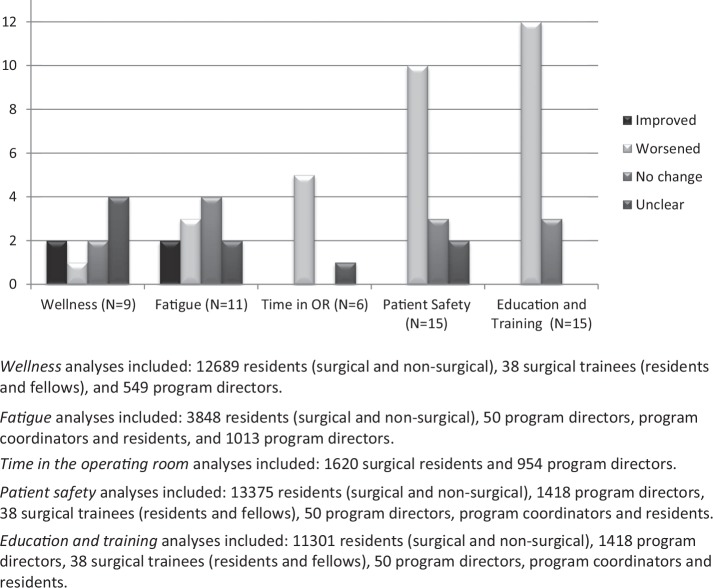
Figure 2 summarizes the findings from the 17 papers related to 16-hour duty maximums; 13 studies were surveys. The results of studies related to resident wellness and fatigue are heterogeneous with a few studies in each category. Six studies examined time in the OR and overall reported that there was decreased time in the OR (N = 5) as a result of RDH restrictions.4,35,37,55,68 Fifteen studies examined the effect on patient safety and found a strong signal toward worsened patient outcomes (N = 10),4,35–37,64–69 with no study reporting improved patient outcomes. Fifteen studies examined education and training; 12 of these showed worsened outcomes4,36,38,55,65–68,70–72 and 3 studies showed no significant change.35,37,69 No studies reported improved educational outcomes.
FIGURE 2.
Impact of 16-hour duty maximums in surgery (N = 17 studies).
Section 5: Effect of RDH Restrictions on Patient Mortality and Morbidity
Mortality. A Forest plot summarizing 13 studies examining the effect of RDH on patient mortality is presented in Figure 3. Two population-based series demonstrate an increase in patient mortality.18,19 Overall, the Random Effects model suggests a trend toward increased mortality in surgical patients in the epoch of time after the implementation of RDH restrictions, compared with the epoch of time before the implementation of RDH restrictions. However, this effect did not reach statistical significance.
FIGURE 3.
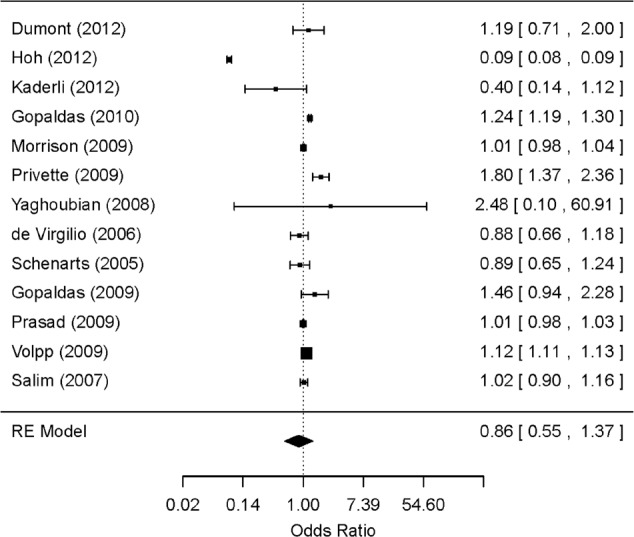
Forest plot describing the effect of RDH restrictions on patient mortality.
TABLE 3.
Effect of RDH Restrictions on Postoperative Morbidity
| Reference | Quality Score | Discipline | Participants | Morbidity Measure | Outcome Values* | Impact of RDH on Morbidity† | |
|---|---|---|---|---|---|---|---|
| Interventional study design | Pre-RDH | Post-RDH | |||||
| Browne et al14 | High | Orthopedic surgery | 48,430 | Perioperative complications | NA | NA | Increased |
| De Virgilio et al22 | Moderate | Trauma surgery | 11,518 | Overall morbidity rate | 38 | 40 | No change |
| Dumont et al10 | Moderate | Neurosurgery | 12,957 | Morbidity rates per 1000 patients | 70 | 89 | Increased |
| Avoidable or possibly preventable morbidity rates per 100 patients | 56 | 76 | Increased | ||||
| Gopaldas et al21 | Moderate | Cardiothoracic surgery | 1562 | Ventilator time >48 h | 60 | 93 | Increased |
| Reoperation for bleeding | 5 | 24 | Increased | ||||
| Gopaldas et al13 | High | Cardiac surgery | 614,177 | In-hospital complications | 78446 | 50390 | Increased |
| Hoh et al11 | High | Neurosurgery | 222,610 | Morbidity rates | 483 | 832 | Increased |
| Kaderli et al12 | Moderate | Surgery | 2686 | Postoperative surgical complications | 32 | 72 | Increased |
| Intraoperative complications | 6 | 8 | No change | ||||
| Morrison et al15 | High | Trauma surgery | 492,173 | Mechanical ventilation | 1.6 d | 1.3 d | Decreased |
| Length of ICU stay | 2.2 | 2.1 | Decreased | ||||
| Length of hospital stay | 5.8 | 5.8 | No change | ||||
| Privette et al18 | Moderate | Trauma surgery; Vascular surgery; General surgery | 14,610 | Total complications | 1688 | 1852 | No change |
| Major complications | 333 | 212 | Decreased | ||||
| Moderate complications | 690 | 768 | No change | ||||
| Minor complications | 663 | 869 | Increased | ||||
| Salim et al9 | Moderate | Trauma surgery | 16,854 | Total number of complications | 504 | 576 | No change |
| Number of preventable complications | 80 | 101 | No change | ||||
| Schenarts et al29 | Moderate | Trauma surgery | 2826 | Respiratory, cardiac, intra-abdominal, and infectious complications | 391 | 401 | No change |
| Length of ICU stay | 5.4 d | 5.4 d | No change | ||||
| Mechanical ventilation | 5.8 d | 5.6 d | No change | ||||
| Length of hospital stay | 6.8 d | 6.4 d | No change | ||||
| Yaghoubian et al19 | Moderate | General surgery | 2470 | Overall morbidity rate | 65 | 24 | Decreased |
| Systematic reviews | |||||||
| Baldwin et al17 | Moderate | Surgery and Medicine | NA | 13 studies assessed morbidity rates: deep surgical infections, disseminated intravascular coagulation, intra-abdominal abscesses, mediastinitis, medication errors, complications attributed to care providers, electrolyte abnormalities, drug-drug interactions, hematomas, transfusions, renal complications, reoperations for bleeding, thromboembolic complications, septicemia, test delays, and systems and patient-related complications. | NA | NA | 5 studies demonstrated decreases in individual complications; 7 studies demonstrated increases in individual complications |
| Fletcher et al20 | High | Surgery‡ | NA | 11 articles assessed morbidity rates; overall complication rates and readmissions to the surgical intensive care unit | NA | NA | 2 studies showed a decrease in overall complications, 2 showed an increase in complication rates, 3 revealed no significant change and the outcomes were not available in 4 studies. |
| Jamal et al25 | High | Surgery | 64,346 | Morbidity rates | 33317 | 31029 | No change |
*If comparison between teaching and nonteaching hospitals, reported values are from teaching hospitals.
†Studies reporting an increase or decrease in morbidity showed a significant difference in their findings; studies with no change did not find a statistically significant difference before and after the implementation of RDH restrictions.
‡Data from surgical studies only.
NA indicates not available.
Morbidity. Fifteen studies examined the effect of RDH restrictions on postoperative morbidity and are summarized in Table 3. Because of the heterogeneity of the manner in which complications reported, we were unable to conduct a meta-analysis related to these outcomes. Overall, there were 15 studies from which we could extract data; 6 studies reported increased patient-level morbidity as a result of RDH.10–14,21 The systematic review conducted by Jamal et al25 reported no overall change, but their results suggested an increase in complications in patients undergoing emergency surgery. Two systematic reviews had heterogeneous results and did not report a conclusive impact of RDH restrictions on surgical patient morbidity.17,20 Two studies reported decreased complication rates,15,19 and 3 studies reported no significant change in patient complications as a result of RDH restrictions.5,22,29 Privette et al showed decreased rates for major complications after RDH restrictions but increased rates for minor complications, and no significant change for total and moderate complications after RDH restrictions.18 More recent studies and those studies examining acutely ill patients reported increased complication rates post duty hour regulations.10–13,21
DISCUSSION
We have completed a comprehensive review of the relevant literature related to RDH restrictions in surgery. This study has several limitations. These limitations are related to the heterogeneous nature of the studies, the various RDH restrictions imposed over varying time intervals, the clinical contexts in which they were conducted, and that for the vast majority of studies, randomization was not possible owing to the regulated nature of duty hours in most jurisdictions. In addition, although there are many areas of debate with respect to the impact of duty hour restrictions, this article focused on patient safety, resident wellness, and resident education. Unfortunately, other topics such as professionalism, impact on surgical faculty and costs associated with mitigating the impact of RDH restrictions was deemed outside the scope of this review. The large number of articles examining perceptions of RDH impact using unvalidated surveys reduces the validity of the findings; to mitigate this, the perceived impacts were reported separately. Most of these papers were categorized as low quality and therefore not included in our final results. Finally, it proved impossible to conduct a meaningful meta-analysis of the literature related to surgical complications because of the manner in which these data were collected and reported across studies. The authors instead chose to report their findings in tabular format.
Patient Safety
One of the stated goals of RDH restrictions was to protect patients from the deleterious effects of physician fatigue. Although evidence demonstrating deficits in attention and hand-eye coordination after sleep deprivation suggest that physician fatigue could compromise patient safety, particularly for the surgical population, this contention has not been demonstrated to date.16,22,25–27,33,75–79 Careful review of the literature over the last decade fails to demonstrate improved patient safety after the implementation of RDH restrictions. A recently published, high-level meta-analysis surveying the surgical literatures shows convincingly that there has been no improvement in patient safety as a result of RDH restrictions.25 Our study confirmed that overall there was no reduction in mortality in the RDH epoch (Fig. 2). More recently, there is increasingly strong evidence that RDH restrictions could be associated with harm to patients.11,75 Recent, larger studies demonstrated increased morbidity and mortality, specifically in high-acuity patient populations as a result of restrictions in RDH.10–12 Specifically, studies in neurosurgery, cardiac surgery, and critical care show that patient-level complications have increased after the implementation of restricted RDH.10,11,13 The largest study suggesting that RDH restrictions have increased patient morbidity was performed by Poulose et al.16 An interrupted time series analysis was performed between 1995 and 2001. Approximately 2.6 million patient discharges from New York area hospitals were reviewed annually over that time period. The authors demonstrated increased incidence of thrombotic/embolic complications and accidental lacerations and punctures after the institution of RDH restrictions. In 2012, Hoh et al11 analyzed the Nationwide Inpatient Sample database of more than 107,000 neurotrauma patients. They compared teaching hospital versus nonteaching hospitals for a 3-year period before and after the 2003 ACGME Work Duty Hours restrictions. The complication rates did not change in nonteaching hospitals (OR = 0.98; 95% CI: 0.787–1.22; P = 0.86) but did change significantly in teaching hospitals (OR = 1.23; 95% CI: 1.00–1.50; P < 0.05). There were no differences in mortality rates between the hospitals across these time points. The increased complications were attributed to the increased handovers. The notion that increasing the frequency of handovers has negative impacts on patient safety has been substantiated by a number of other studies.63,76,80 A recent study published by Dumont et al in the Journal of Neurosurgery also suggested an increase in complications. The authors studied a prospectively collected divisional Morbidity and Mortality database. They showed that the morbidity rate increased from 70 to 89 per 1000 patients treated after institution of work-hour restrictions (P = 0.001). The morbidities that were deemed avoidable or possibly preventable increased from 56 to 66 per 1000 patients treated (P = 0.017).10 These same authors queried the Nationwide Inpatient Sample for all patients admitted for elective craniotomy for meningioma from 1998 to 2008, excluding 2003. The complication rate was compared for 5-year epochs at teaching and nonteaching hospitals before (1998–2002) and after (2004–2008) the ACGME work hour restrictions. They identified 21,177 patients who met the inclusion criteria. They found a statistically significant increase in complication rates from 14% to 16% in teaching hospitals in contrast to a stable 15% complication rate in nonteaching hospitals. This effect remained significant in a multivariate analysis including age and existing comorbidities. Aligned with previous research related to the 2003 ACGME regulations, there is no demonstrable improvement in patient safety after the 2011 ACGME 16-hour duty limitations. More recent evidence studying the effect of 2011 ACGME regulations suggests a decrease in patient safety related to increased numbers of handovers and work compression.34 Similar results of increased complications as a result of RDH restrictions have been documented in a large series of intensive care unit (ICU) patients.81 Surgical diseases, complication, and outcomes may differ qualitatively from other fields of medicine, as surgical practice is tied to large inpatient units with patients whose clinical course can evolve significantly over hours. The observed worsening of outcomes in surgery as a result of RDH restrictions may be related to an increased frequency of handovers, which cause fragmented care and loss of crucial information. Frequent shift changes, as experienced with some restrictive RDH stipulations, may impede residents' ability to observe the natural course of disease and recognize deviations from an expected trajectory and complications of surgery. It is imperative that surgeons are trained to recognize the early signs of postoperative problems and institute appropriate interventions. The development of surgical acumen and the management of complications of surgery require repeated exposures so that subtle variations in clinical presentations can be mastered.
Resident Wellness, Fatigue, and Burnout
Review of the literature pertaining to the change in RDH restrictions in surgery shows an improvement in resident well-being, fatigue, and burnout after the implementation of the 80-hour workweek and coincident with the 2003 ACGME regulations. However, the anticipated improvements in resident wellness, physical or occupational health, have not been consistently realized from subsequent regulations, such as the 2011 ACGME stipulations of 16-hour in-house duty maximums for first-year residents. A longitudinal cohort study undertaken by Sen et al34 showed that the decrease of working hours under the 2011 ACGME standards have resulted in an “unanticipated increase in self-reported medical errors” and has not shown an improvement in well-being or depressive symptoms, nor has it prompted an increase in hours of sleep. Drolet et al in a large national survey of residents from all specialties showed that 48% of respondents disapprove of 16-hour call maximums and only 22% of respondents supported the move to 16-hour duty in-house call maximums. The restrictions were perceived as detrimental to resident quality of life, education, and engagement with their supervisor. The residents' survey responses suggest an improved quality of life for interns; however, quality of life for senior residents seems to suffer in the new paradigm. Interns also reported a decreased sense of readiness for more senior roles, raising a concern that 2011 duty hour reforms could result in prolongation of an already lengthy training.71,72 Antiel and colleagues conducted a longitudinal survey of US PGY1 (post graduate year) surgery residents training under the 16-hour duty maximum regulations. Participants reported a significant negative effect on quality of life in their first year of training, a lack of continuity of care, exposure to supervisors and operative cases.37 A prospective longitudinal cohort multicentre study of 2323 PGY1 trainees (58% response rate) showed that although there was a small decrease in duty hours worked per week, there was no significant change in hours slept, depressive symptoms, or well-being (measured using a validated tool).34 A smaller, single-center study showed that surgical residents experienced a paradoxical increased sense of fatigue and felt that their education was compromised as a result of 16-hour duty maximums. In addition to residents reporting feeling more fatigued, they also reported that they could not master surgical skills and perceived a decline in the quality of patient care they provided. Seventy percent of residents reported feeling disconnected from their service and that their mentoring relationship with faculty was compromised. Sixteen hour in house call maximums resulted in increased rates of burnout, isolation, as well as reduced morale among surgical trainees.67
Night, evening, rotating, and irregular shifts may also be associated with an elevated risk of workplace injuries and elevated rates of burnout. Shift work in general is associated with increased preterm labor, depression, weight gain, increased rates of injury and burnout and has been classified as a class I carcinogen by the World Health Organization.82 Studies show increased rates of needle stick injury among surgical residents training under traditional 24-hour call models.83 However, the incidence of needle stick injuries is correlated with the level of the learner more so than with sleep deprivation.84 These findings suggest that implementation of early education could decrease this specific occupational risk. Continuous wakefulness for prolonged periods (24 hours) should be avoided, especially if this pattern is frequently repeated. The period of duty for residents may not necessarily have to equate with continuous wakefulness. Rest periods and protected sleep time that respects circadian physiology could improve resident fatigue and professional satisfaction, whereas preserving their access to educational opportunities and preserving patient safety. Night float systems alternate at weekly intervals as per the ACGME guidelines, causing not only a disruption in one's internal balance but creating a cycle where a resident may not have sufficient time to recover from the disruption before being exposed again to a 12-hour shift. Residents who adhere to traditional 24-hours call schedules may be more likely overall to experience relatively normal sleep patterns with deep sleep occurring at night. Thus far, it seems the recent trend toward night float and shift work has not yielded the desired result of more rested and professionally satisfied surgical residents.
Education and Training
Overall, of the 15 studies examining the effect of 16-hour duty maximums, none showed improvements in educational outcomes after the implementation of RDH restrictions. The majority of studies showed worsening of outcomes, whereas a few studies showed no change. Studies related to RDH restriction in education showed that overall the total numbers of operations performed during residency have decreased slightly. However, there has been a proportionately greater decrease in the volume of emergency surgical procedures performed. Furthermore, the residents' role in the OR has changed over the last decade, with a significant decline in the numbers of cases reported as first assistant and as teaching assistant.51 This trend is worrisome, as first assistant cases represent an opportunity for trainees to learn surgical anatomy, steps of the procedure and receive mentorship in the OR, and the teaching assistant role allows residents to develop and demonstrate surgical mastery.51 These findings are consistent with recent studies related to resident time in the OR after the implementation of the 16-hour duty maximums, with 5 of 6 studies demonstrating decreased time in the OR; no studies demonstrated a neutral effect or increased time in the OR. Most recently, in a study of 249 surgical residents, Schwartz et al55 showed a 25% decrease in PGY1-level operative cases subsequent to the implementation of 16-hour duty maximums, compared to the 4 previous years.
The mastery of procedural components of surgery requires time on task in a mentored environment and with graduated responsibility. Specifically, achieving mastery of complex technical tasks requires deliberate practice. Some authors suggest that 10,000 hours of deliberate practice may be required.85,86 Teaching of technical expertise and surgical judgement requires that mentors spend longitudinal time with trainees to appreciate their strengths and weaknesses. Coaching in the OR specifically requires that mentors observe progress, provide feedback, and then look for progress at the next opportunity. In teaching programs, surgical faculty voice a growing concern that they have insufficient exposure to individual residents to identify deficiencies, address weaknesses, or provide meaningful evaluation. This observation is especially true for night-float rotations where exposure to teaching faculty can be extremely variable, random, and often brief.87 This phenomenon may delay the maturation of surgical competence in the OR and result in prolongation of training. This unintended consequences of shift work and night float systems was described in a nationwide survey of US PGY1 residents as they are feeling less prepared to assume the PGY2 role.71
Simulation has emerged as an important adjunct to training for specific types of skills. It can prepare learners for laparoscopic, endoscopic, and endovascular procedures through use of geometric exercises, which can accustom them to the 2 dimensional environment, thus improving hand eye coordination and instrument handling. Well-designed simulation curricula for these types of procedures result in greater ease with routine parts of the operation and can decrease time to achieve competence and entry into practice.88 Simulation training also has an emerging role in teaching crisis resource management skills, such as leadership and communication;89 however, its impact on patient outcomes remains unknown. Simulation for open surgery is useful to assist residents to learn the repetitive parts of operations (eg, practicing a stapled bowel anastomosis using porcine material). These motor skills then become more “automatic,” allowing learners to focus on anatomy, pathology, and judgment when they are in the OR. However, relying on simulation to learn clinical reasoning, intraoperative decision-making, or refining sophisticated surgical techniques, especially for open surgery, is not feasible. Simulation models lack fidelity to human anatomy and tissues and are ill equipped to accommodate for variation, unexpected findings, and abnormal or diseased anatomy. Simulation training is best thought of as preparatory for residents' participation in the OR, as skills beyond the fundamental level in open surgery and accommodation to the 2 dimensional environment for laparoscopic procedures are better learned in the OR under the guidance and coaching of an experienced mentor.
Perhaps most concerning is the trend toward increased failure rates on the oral component of the various surgical board examinations. Although correlation does not imply causation, as many factors are involved in the outcome of board examinations, the American Board of Thoracic Surgery reported that over the last decade there has been a nearly linear increase in the failure rate of candidates, with 35% of trainees being unsuccessful in 2012, compared with 12% in 2003.53 In General Surgery, the American Board failure rate has nearly doubled from 15% to 25% over 10 years, with a peak failure rate of 28% in 2011–2012.52 Interestingly, the results on written examination have remained static. Whereas performance on the written examination reflects knowledge and synthesis of information, performance on the oral examination tests judgement and candidates' real world experience with complex surgical issues. The American Board of Neurologic Surgeons has increased the length of residency training from 6 to 7 years, suggesting that ongoing RDH restrictions may affect the duration of training and time to achieve competence for independent practice. A survey conducted by the Fellowship Council of 145 subspecialty General Surgery program directors showed that they found starting fellows to be inadequately prepared for the OR; 38% demonstrated a lack of patient ownership, 30% could not independently perform a laparoscopic cholecystectomy, 66% were deemed unable to operate for 30 minutes unsupervised on a major procedure, and one-quarter were unable to recognize the early signs of complications.90
Trainees' involvement in emergency operations is important for the development of surgical judgement and competence. Residents learn from their integral involvement in patient care about the evolution of surgical diagnoses; when to operate, how much diagnostic accuracy is sufficient, and perhaps most importantly, to recognize and manage surgical complications. Major surgical complications are relatively infrequent, but they are serious. Rare presentations and infrequent complications of surgery require greater flexibility in resident scheduling, so that residents may benefit from these exposures, as expertise in these areas remains tied to experiences nested in the clinical environment. These aspects of surgical acumen are an essential part of professional maturation and require time on task. As emphasized in a recent commentary in the New England Journal of Medicine by Kesselheim et al. education and service are inextricably linked and the current focus on “duty hours” as an isolated consideration may undermine the overarching objective of postgraduate medical training.77 Our findings as well as others', emphasize that surgery perhaps more than other disciplines, requires immersion in the clinical environment, and that to a significant degree the training of a surgeon is well suited to the apprenticeship model.
2011 ACGME Restrictions—16-Hour Duty Shift Maximums for Surgical Residents
Review of the 17 studies that focused on assessing the impact of the 16-hour duty maximums showed a trend toward an overall negative impact in surgical training. Fargen et al65 showed in a survey of neurosurgical residents across the United States and Puerto Rico that 83% of respondents disagreed with, or strongly disagreed with 16-hour duty maximums for PGY1 residents. De Martino et al64 reported a similar concern among vascular surgery trainees. Recently, a national survey of 549 US program directors from Internal Medicine, Pediatrics and General Surgery programs revealed that 72% did not approve the 16-hour shift limit for interns. Although they generally did agree with other ACGME duty hour restrictions, they felt that currently, there were simply too many restrictions and that these restrictions resulted in negative effects on resident education, preparedness for senior roles, and no tangible benefits to resident wellness.70 These authors support greater flexibility with program and specialty specific tailoring of the educational environment for trainees. Our findings, and those of other authors, do not support 16-hour duty maximums for surgical residents at this time. Implementation of these RDH restrictions should be anticipated to result in prolongation of an already lengthy training duration and potential risk to patients, without tangible benefits to resident wellness.
Solutions to Improve Resident Wellness
Streamlining Resident Workflow and Investment in Wellness Resources
Residency systems have created expectations in teaching centers that the “doctor (aka resident) is always around.” This phenomenon dates back to the origins of the term “Resident.” Perhaps it is time to step back and reconsider the current role and purpose of surgical residency. Residents are present in teaching hospitals to learn about and deliver patient care. Their time and energy should be preserved to participate in patient evaluations, decision making, and operating. Surgical training needs to be more efficient. Other members of the health care team, such as physician assistants, nurse practitioners, respiratory therapists, pharmacists, phlebotomists, physiotherapists, and social workers, if correctly deployed could alleviate some of the “nonphysician” functions that currently distract residents from focusing their time in OR, management of ill patients, ambulatory clinics, academic rounds, and structured curricula.11,91 This approach would improve residents' professional satisfaction and sense of wellness. Additional strategies to alleviate fatigue and prevent burnout include improved opportunities for sleep while on call as was recommended in the 2009 Institute of Medicine report. These solutions more readily respect circadian physiology than the current trend toward shift work and night float systems.92,93 Improved handover tools, innovations such as electronic rounding reports, and polices to escalate care to more senior residents and faculty, when appropriate, would alleviate resident workload and improve patient safety.94
Expansion of OR resources and acute care surgery teams may be necessary in certain settings to better ensure urgent operative cases are completed during daytime hours when feasible, leaving overnight OR resources for patients who present during the evening and night with life, limb, or vision threatening surgical diagnoses.95,96 There will remain a subset of patients who require urgent operative intervention after midnight. Resident participation in these patients' preoperative and operative care is essential for residents' professionalization.
Expansion of Wellness Resources and Implementation of Wellness Programs
Physicians, and perhaps to a greater extent surgeons, have long ignored our own health. This phenomenon in part is related to our professionalization and societal expectations, but it is also connected to the reality that every single one of our patients at any given moment is much worse off than the treating doctor. For the resident on a ward of cancer, trauma, sepsis, or burn patients, prioritizing one's own health is nearly impossible. Structural changes are required to accommodate this reality and enable residents to attend to their own physical and emotional well-being when necessary. One of the key recommendations in the Royal College of Physicians and Surgeons of Canada National Steering Committee report is to move the current discussion away from one that is focused solely on RDH and includes institutional strategies that enable fatigue mitigation and management, rather than relying only on externally imposed RDH limits.5 This strategy, in part, could include wellness programs within residency structures that screen for and are equipped to manage psychological distress and burnout. Wellness programs are defined by a combination of active and passive initiatives targeting the various domains of physical, mental, social, and intellectual wellness and have been shown to be effective, inexpensive, and well received by trainees.97–99
CONCLUSIONS
Systematic review of the literature related to RDH restrictions in surgery shows that there were benefits to resident wellness realized from 2003 ACGME regulations limiting RDH to 80 hours per week. However, there seems to be some concern for increased morbidity and mortality rates in high-acuity patients as a result of the 2003 and to a greater extent the 2011 ACGME regulations.11,12,20 Also concerning is the trend for poorer performance on American Board of Surgery certification examinations over the last decade. Further evaluation of the literature related specifically to the implementation of 16-hour duty maximums for PGY1 residents in the United States and all in-house residents in the province of Quebec showed that there may be little added benefit to residents' wellness.67 Recent evidence suggests that adverse patient outcomes may extend beyond the highest acuity patients in surgery, as residents perceive increased rates of medical errors as a result of 16-hour duty maximums. Equally concerning, we found no evidence for improved educational or training experiences as a result of 16-hour duty maximums. Rather, there seems to be consistent findings across many studies of increased patient handovers, poorer team integration, professional dissatisfaction, concern for maturation of clinical skills, and decreased time in the OR. Philibert et al100 recently published a literature review of high-quality articles with similar conclusions.
Fatigue is potentially harmful, mitigating its effects while ensuring adequate training is essential. Strategies such as less than 24 hour shifts have failed to demonstrate a significant benefit to resident wellness and potentially deleterious consequences for patient and training outcomes.35,38,55 This observation has also been documented in critically ill patients in the ICU setting.81 Training should prepare residents for schedules commonly encountered in the independent practice of that specialty. It is clear that a “one-size fits all” solution to the issue of RDH restrictions is not appropriate for all medical disciplines. A more tailored and discipline specific approach is required such that training objectives and patient outcomes are protected. This view has been supported by a pan-Canadian consensus process related to RDHs, led by the Royal College of Physicians and Surgeons in Canada.5 This report is the first nonsurgical document to support this perspective, one that has been emphasized by many surgical education bodies including the American College of Surgeons, Division of Education and the Royal College of Surgeons of Edinburgh.3,101 The challenge for surgical training programs will be how best to support resident wellness though fatigue mitigation strategies, screening and addressing resident burnout, as well as improving resident workflow to optimize resident sleep, supervision and minimize tasks unrelated to the provision of medically necessary care, and preserving access to key mentorship and high impact learning opportunities. An approach that centers on the training mandate of residencies and allows a degree of flexibility will be necessary if we wish to preserve robust educational and patient-level outcomes without further prolonging an already arduous and lengthy training experience. It is well time to reconsider the direction of RDH as it relates to surgical training, as the recent erosion of resident training time has not achieved the desired results. A broader dialogue beyond duty hours alone will yield a more satisfactory outcome for all stakeholders, and especially for surgical residents.
ACKNOWLEDGMENTS
The authors thank the National Steering Committee on RDHs and the Royal College of Physicians and Surgeons of Canada for their assistance in the completion of this project and especially Lisa Gorman and Sarah Taber. They also thank the following working group members for their inputs: Barbara Guido, Henry Broekhuyse, Joanne Carrier, David Steven, Douglas Hedden, Jefferson Wilson, Jean Francios Chevalier, Joel Werier, Pamela Chu, Piotr Blachut, Ravi Sidhu, Grace Yeung, and Mark Walsh.
Footnotes
Disclosure: This study was supported by Health Canada and the Department of Surgery, University of Toronto, Ontario, Canada. The authors declare that they have no conflict of interest.
REFERENCES
- 1.Nasca TJ. An Open Letter to the GME Community. Chicago, IL: Accreditation Council for Graduate Medical Education; 2010 [Google Scholar]
- 2.Temple J. Time for Training: A Review of the impact of the European Working Time Directive on the Quality of Training. London, UK: Royal College of Surgeons of England; 2010 [Google Scholar]
- 3.American College of Surgeons Task Force. Position of the American College of Surgeons on restrictions on resident work hours. Paper presented at: The Institute of Medicine of the National Academies, Committee on Optimizing Graduate Medical Trainee (Resident) Schedules to Improve Patient Safety; March 4, 2008; Irvine, CA [Google Scholar]
- 4.Drolet B, Sangisetty S, Tracy T, et al. Surgical residents' perceptions of 2011 Accreditation Council for Graduate Medical Education duty hour regulations. JAMA Surg. 2013;148:427–433 [DOI] [PubMed] [Google Scholar]
- 5.National Steering Committee on Resident Duty Hours. Fatigue, Risk, & Excellence: Towards a Pan-Canadian Consensus on Resident Duty Hours. Ottawa, ON: Royal College of Physicians and Surgeons of Canada; 2013 [Google Scholar]
- 6.Balshem H, Helfand M, Schünemann H, et al. GRADE guidelines: 3. Rating the quality of evidence. J Clin Epidemiol. 2011;64:401–406 [DOI] [PubMed] [Google Scholar]
- 7.Viechtbauer W. Conducting meta-analyses in R with the metafor package. J Stat Softw 2010;36:1–48 [Google Scholar]
- 8.R Development Core Team. R: A Language and Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing; 2013 [Google Scholar]
- 9.Salim A, Teixeira P, Chan L, et al. Impact of the 80-hour workweek on patient care at a level I trauma center. Arch Surg. 2007;142:708–712; discussion 712–714. [DOI] [PubMed] [Google Scholar]
- 10.Dumont TM, Rughani AI, Penar PL, et al. Increased rate of complications on a neurological surgery service after implementation of the Accreditation Council for Graduate Medical Education work-hour restriction. J Neurosurg. 2012;116:483–486 [DOI] [PubMed] [Google Scholar]
- 11.Hoh BL, Neal DW, Kleinhenz DT, et al. Higher complications and no improvement in mortality in the ACGME resident duty-hour restriction era: an analysis of more than 107,000 neurosurgical trauma patients in the nationwide inpatient sample database. Neurosurgery. 2012;70:1369–1382 [DOI] [PubMed] [Google Scholar]
- 12.Kaderli R, Businger A, Oesch A, et al. Morbidity in surgery: impact of the 50-hour work-week limitation in Switzerland. Swiss Med Wkly. 2012;142:w13506. [DOI] [PubMed] [Google Scholar]
- 13.Gopaldas RR, Chu D, Dao TK, et al. Impact of ACGME work-hour restrictions on the outcomes of coronary artery bypass grafting in a cohort of 600,000 patients. J Surg Res. 2010;163:201–209 [DOI] [PubMed] [Google Scholar]
- 14.Browne JA, Cook C, Olson SA, et al. Resident duty-hour reform associated with increased morbidity following hip fracture. J Bone Joint Surg Am. 2009;91:79–85 [DOI] [PubMed] [Google Scholar]
- 15.Morrison CA, Wyatt MM, Carrick MM. Impact of the 80-hour work week on mortality and morbidity in trauma patients: an analysis of the National Trauma Data Bank. J Surg Res. 2009;154:157–162 [DOI] [PubMed] [Google Scholar]
- 16.Poulose BK, Ray WA, Arbogast PG, et al. Resident work hour limits and patient safety. Ann Surg. 2005;241:847–860 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Baldwin K, Namdari S, Donegan D, et al. Early effects of resident work-hour restrictions on patient safety: a systematic review and plea for improved studies. J Bone Joint Surg Am. 2011;93:1–9 [DOI] [PubMed] [Google Scholar]
- 18.Privette AR, Shackford SR, Osler T, et al. Implementation of resident work hour restrictions is associated with a reduction in mortality and provider-related complications on the surgical service. Ann Surg. 2009;250:316–321 [DOI] [PubMed] [Google Scholar]
- 19.Yaghoubian A, Saltmarsh G, Rosing DK, et al. Decreased bile duct injury rate during laparoscopic cholecystectomy in the era of the 80-hour resident workweek. Arch Surg. 2008;143:847–851 [DOI] [PubMed] [Google Scholar]
- 20.Fletcher K, Reed D, Arora V. Patient safety, resident education and resident well-being following implementation of the 2003 ACGME duty hour rules. J Gen Intern Med. 2011;26:907–919 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gopaldas RR, Huh J, Bakaeen F, et al. The impact of resident work-hour restrictions on outcomes of cardiac operations. J Surg Res. 2009;157:268–274 [DOI] [PubMed] [Google Scholar]
- 22.De Virgilio C, Yaghoubian A, Lewis RJ, et al. The 80-hour resident workweek does not adversely affect patient outcomes or resident education. Curr Surg. 2006;63:435–439 [DOI] [PubMed] [Google Scholar]
- 23.Helling T, Kaswan S, Boccardo J, et al. The effect of resident duty hour restriction on trauma center outcomes in teaching hospitals in the state of Pennsylvania. J Trauma. 2010;69:607–612 [DOI] [PubMed] [Google Scholar]
- 24.Hutter MM, Kellogg KC, Ferguson CM, et al. The impact of the 80-hour resident workweek on surgical residents and attending surgeons. Ann Surg. 2006;243:864–875 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jamal MH, Doi SAR, Rousseau M, et al. Systematic review and meta-analysis of the effect of North American working hours restrictions on mortality and morbidity in surgical patients. Br J Surg. 2012;99:336–344 [DOI] [PubMed] [Google Scholar]
- 26.Moonesinghe SR, Lowery J, Shahi N, et al. Impact of reduction in working hours for doctors in training on postgraduate medical education and patients' outcomes: systematic review. BMJ. 2011;342:d1580. [DOI] [PubMed] [Google Scholar]
- 27.Prasad M, Iwashyna T, Christie J, et al. Effect of work-hours regulations on intensive care unit mortality in United States teaching hospitals. Crit Care Med. 2009;37:2564–2569 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rosen A, Loveland S, Romano P, et al. Effects of resident duty hour reform on surgical and procedural patient safety indicators among hospitalized Veterans Health Administration and Medicare patients. Med Care. 2009;47:723–731 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Schenarts PJ. The effect of a rotating night float scheme on preventable and potentially preventable morbidity at a level 1 trauma center. Am J Surg. 2005;190:147–152 [DOI] [PubMed] [Google Scholar]
- 30.Schlosser K, Maschuw K, Kupietz E, et al. Call-associated acute fatigue in surgical residents-subjective perception or objective fact? A cross-sectional observational study to examine the influence of fatigue on surgical performance. World J Surg. 2012;36:2276–2287 [DOI] [PubMed] [Google Scholar]
- 31.Shetty KD, Bhattacharya J. Changes in hospital mortality associated with residency work-hour regulations. Ann Intern Med. 2007;147:73–80 [DOI] [PubMed] [Google Scholar]
- 32.Shonka DCJ, Ghanem TA, Hubbard MA, et al. Four years of Accreditation Council of Graduate Medical Education duty hour regulations: have they made a difference? Laryngoscope. 2009;119:635–639 [DOI] [PubMed] [Google Scholar]
- 33.Volpp KG, Rosen AK, Rosenbaum P, et al. Did duty hour reform lead to better outcomes among the highest risk patients? J Gen Intern Med. 2009;24:1149–1155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sen S, Kranzler H, Didwania A, et al. Effects of the 2011 duty hour reforms on interns and their patients: a prospective longitudinal cohort study. JAMA Intern Med. 2013;173:657–662 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Antiel R, Van Arendonk K, Reed D, et al. Surgical training, duty-hour restrictions, and implications for meeting the Accreditation Council for Graduate Medical Education core competencies: views of surgical interns compared with program directors. Arch Surg. 2012;147:536–541 [DOI] [PubMed] [Google Scholar]
- 36.Antiel R, Thompson S, Hafferty F, et al. Duty hour recommendations and implications for meeting the ACGME core competencies: views of residency directors. Mayo Clin Proc. 2011;86:185–191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Antiel RM, Reed DA, Van Arendonk KJ, et al. Effects of duty hour restrictions on core competencies, education, quality of life, and burnout among general surgery interns. JAMA Surg. 2013;148:448–455 [DOI] [PubMed] [Google Scholar]
- 38.Desai S, Feldman L, Brown L, et al. Effect of the 2011 vs 2003 duty hour regulation-compliant models on sleep duration, trainee education, and continuity of patient care among internal medicine house staff: a randomized trial. JAMA Intern Med. 2013;173:649–655 [DOI] [PubMed] [Google Scholar]
- 39.Fitzgibbons SC, Chen J, Jagsi R, et al. Long-term follow-up on the educational impact of ACGME duty hour limits: a pre-post survey study. Ann Surg. 2012;256:1108–1112 [DOI] [PubMed] [Google Scholar]
- 40.Jagannathan J, Vates GE, Pouratian N, et al. Impact of the Accreditation Council for Graduate Medical Education work-hour regulations on neurosurgical resident education and productivity. J Neurosurg. 2009;110:820–827 [DOI] [PubMed] [Google Scholar]
- 41.Biller CK, Antonacci AC, Pelletier S, et al. The 80-hour work guidelines and resident survey perceptions of quality. J Surg Res. 2006;135:275–281 [DOI] [PubMed] [Google Scholar]
- 42.Stamp T, Termuhlen P, Miller S, et al. Before and after resident work hour limitations. Curr Surg. 2005;62:117–121 [DOI] [PubMed] [Google Scholar]
- 43.Fletcher K, Underwood W, III, Davis S, et al. Effects of work hour reduction on residents' lives: a systematic review. JAMA. 2005;294:1088–1100 [DOI] [PubMed] [Google Scholar]
- 44.Jamal MH, Rousseau MC, Hanna WC, et al. Effect of the ACGME duty hours restrictions on surgical residents and faculty: a systematic review. Acad Med. 2011;86:34–42 [DOI] [PubMed] [Google Scholar]
- 45.Zare SM, Galanko JA, Behrns KE, et al. Psychologic well-being of surgery residents after inception of the 80-hour workweek: a multi-institutional study. Surgery. 2005;138:150–157 [DOI] [PubMed] [Google Scholar]
- 46.Carlin AM, Gasevic E, Shepard AD. Effect of the 80-hour work week on resident operative experience in general surgery. Am J Surg. 2007;193:326–330 [DOI] [PubMed] [Google Scholar]
- 47.Connors RC, Doty JR, Bull DA, et al. Effect of work-hour restriction on operative experience in cardiothoracic surgical residency training. J Thorac Cardiovasc Surg. 2009;137:710–714 [DOI] [PubMed] [Google Scholar]
- 48.Damadi A, Davis AT, Saxe A, et al. ACGME duty-hour restrictions decrease resident operative volume: a 5-year comparison at an ACGME-accredited University General Surgery residency. J Surg Educ. 2007;64:256–259 [DOI] [PubMed] [Google Scholar]
- 49.Fairfax LM, Christmas AB, Green JM, et al. Operative experience in the era of duty hour restrictions: is broad-based General Surgery training coming to an end? Am Surg. 2010;76:578–582 [PubMed] [Google Scholar]
- 50.Feany MA, Scott BG, Mattox KL, et al. Impact of the 80-hour work week on resident emergency operative experience. Am J Surg. 2005;190:947–949 [DOI] [PubMed] [Google Scholar]
- 51.Kairys JC, McGuire K, Crawford AG, et al. Cumulative operative experience is decreasing during General Surgery residency: a worrisome trend for surgical trainees? J Am Coll Surg. 2008;206:804–813 [DOI] [PubMed] [Google Scholar]
- 52.Lewis FR, Klingensmith ME. Issues in General Surgery residency training—2012. Ann Surg. 2012;256:553–559 [DOI] [PubMed] [Google Scholar]
- 53.Moffatt-Bruce S, Ross PS, Williams T. American Board of Thoracic Surgery examination: fewer graduates, more failures. Paper presented at: AATS Annual Meeting; May 4–8, 2013; Minneapolis, MN: [DOI] [PubMed] [Google Scholar]
- 54.Sadaba JR, Urso S. Does the introduction of duty-hour restriction in the United States negatively affect the operative volume of surgical trainees? Interact Cardiovasc Thorac Surg. 2011;13:316–319 [DOI] [PubMed] [Google Scholar]
- 55.Schwartz S, Galante J, Kaji A, et al. Effect of the 16-hour work limit on General Surgery intern operative case volume: a multi-institutional study. JAMA Surg. 2013;148:829–833 [DOI] [PubMed] [Google Scholar]
- 56.Watson DR, Flesher TD, Ruiz O, et al. Impact of the 80-hour workweek on surgical case exposure within a general surgery residency program. J Surg Educ. 2010;67:283–289 [DOI] [PubMed] [Google Scholar]
- 57.Bland KI, Stoll DA, Richardson JD, et al. Brief communication of the Residency Review Committee-Surgery (RRC-S) on residents' surgical volume in general surgery. Am J Surg. 2005;190:345–350 [DOI] [PubMed] [Google Scholar]
- 58.Ferguson CM, Kellogg KC, Hutter MM, et al. Effect of work-hour reforms on operative case volume of surgical residents. Curr Surg. 2005;62:535–538 [DOI] [PubMed] [Google Scholar]
- 59.Simien C, Holt KD, Richter TH, et al. Resident operative experience in General Surgery, Plastic Surgery, and Urology 5 years after implementation of the ACGME duty hour policy. Ann Surg. 2010;252:383–389 [DOI] [PubMed] [Google Scholar]
- 60.Smith RP. Resident technical experience in obstetrics and gynecology before and after implementation of work-hour rules. Obstet Gynecol. 2012;115:1166–1171 [DOI] [PubMed] [Google Scholar]
- 61.Spencer AU, Teitelbaum DH. Impact of work-hour restrictions on residents' operative volume on a subspecialty surgical service. J Am Coll Surg. 2005;200:670–676 [DOI] [PubMed] [Google Scholar]
- 62.Occhino J, Hannigan T, Baggish M, et al. Resident duty-hour restrictions and their effect on operative experience in obstetrics and gynecology. Gynecol Obstet Invest. 2011;72:73–78 [DOI] [PubMed] [Google Scholar]
- 63.Babu MA, Nahed BV, Heary RF. Investigating the scope of resident patient care handoffs within neurosurgery. PLoS One. 2012;7:e41810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.De Martino RR, Brewster LP, Kokkosis AA, et al. The perspective of the vascular surgery trainee on new ACGME regulations, fatigue, resident training and patient safety. Vasc Endovascular Surg. 2011;45:697–702 [DOI] [PubMed] [Google Scholar]
- 65.Fargen KM, Chakraborty A, Friedman WA. Results of a national neurosurgery resident survey on duty hour regulations. Neurosurgery. 2011;69:1162–1170 [DOI] [PubMed] [Google Scholar]
- 66.Lee DY, Myers EA, Rehmani SS, et al. Surgical residents' perception of the 16-hour work day restriction: concern for negative impact on resident education and patient care. J Am Coll Surg. 2012;215:868–877 [DOI] [PubMed] [Google Scholar]
- 67.Hamadani F, Deckelbaum D, Sauve A, et al. Abolishment of 24-hour continuous medical call duty in Quebec: a quality of life survey of general surgical residents following implementation of the new work-hour restrictions. J Surg Educ. 2013;70:296–303 [DOI] [PubMed] [Google Scholar]
- 68.Shea J, Willett L, Borman K, et al. Anticipated consequences of the 2011 duty hours standards: views of internal medicine and surgery program directors. Acad Med. 2012;87:895–903 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Tan P, Hogle NJ, Widmann WD. Limiting PGY1 residents to 16 hours of duty: review and report of a workshop. J Surg Educ. 2012;69:355–359 [DOI] [PubMed] [Google Scholar]
- 70.Drolet B, Khokhar M, Fischer S. The 2011 duty-hour requirements—a survey of residency program directors. N Engl J Med. 2013;368:694–697 [DOI] [PubMed] [Google Scholar]
- 71.Drolet BC, Christopher DA, Fischer SA. Residents' response to duty-hour regulations: a follow-up national survey. N Engl J Med. 2012;366:e35. [DOI] [PubMed] [Google Scholar]
- 72.Drolet BC, Spalluto LB, Fischer SA. Residents' perspectives on ACGME regulation of supervision and duty hours: a national survey. N Engl J Med. 2010;363:e34. [DOI] [PubMed] [Google Scholar]
- 73.Abraham T, Freitas M, Frangos S, et al. Are resident work-hour limitations beneficial to the trauma profession? Am Surg. 2006;72:35–41 [PubMed] [Google Scholar]
- 74.Goldstein MJ, Kim E, Widmann WD, et al. A 360° evaluation of a night-float system for General Surgery: a response to mandated work-hours reduction. Curr Surg. 2004;61:445–451 [DOI] [PubMed] [Google Scholar]
- 75.Businger AP, Laffer U, Kaderli R. Resident work hour restrictions do not improve patient safety in surgery: a critical appraisal based on 7 years of experience in Switzerland. Patient Saf Surg. 2012;6:17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Mueller S, Call S, McDonald F, et al. Impact of resident workload and handoff training on patient outcomes. Am J Med. 2012;125:104–110 [DOI] [PubMed] [Google Scholar]
- 77.Kesselheim J, Cassel C. Service: an essential component of graduate medical education. New Engl J Med. 2013;368:500–501 [DOI] [PubMed] [Google Scholar]
- 78.Volpp KG, Rosen AK, Rosenbaum P, et al. Mortality among hospitalized Medicare beneficiaries in the first 2 years following ACGME resident duty hour reform. JAMA. 2007;298:975–983 [DOI] [PubMed] [Google Scholar]
- 79.Afessa B, Kennedy C, Klarich K, et al. Introduction of a 14-hour work shift model for house staff in the medical ICU. Chest. 2005;128:3910–3915 [DOI] [PubMed] [Google Scholar]
- 80.Moseley BD, Smith JH, Diaz-Medina GE, et al. Standardized sign-out improves completeness and perceived accuracy of inpatient neurology handoffs. Neurology. 2012;79:1060–1064 [DOI] [PubMed] [Google Scholar]
- 81.Bollschweiler E, Krings A, Fuchs K, et al. Alternative shift models and the quality of patient care. An empirical study in surgical intensive care units. Langenbecks Arch Surg. 2001;386:104–109 [DOI] [PubMed] [Google Scholar]
- 82.International Agency for Research on Cancer. Agents Classified by the IARC Monographs. Lyon, France: International Agency for Research on Cancer, World Health Organization; 2013 [Google Scholar]
- 83.Makary M, Al-Attar A, Holzmueller C, et al. Needlestick injuries among surgeons in training. N Engl J Med. 2007;356:2693–2699 [DOI] [PubMed] [Google Scholar]
- 84.Brasel K, Mol C, Kolker A, et al. Needlesticks and surgical residents: who is most at risk? J Surg Educ. 2007;64:395–398 [DOI] [PubMed] [Google Scholar]
- 85.Anders Ericsson K, Krampe R, Tesch-Romer C. The role of deliberate practice in the acquisition of expert performance. Psychol Rev. 1993;100:363–406 [Google Scholar]
- 86.Gladwell M. Outliers: The Story of Success. New York, NY: Little, Brown and Company; 2008 [Google Scholar]
- 87.Lefrak S, Miller S, Schirmer B, et al. The night float system: ensuring educational benefit. Am J Surg. 2005;189:639–642 [DOI] [PubMed] [Google Scholar]
- 88.Grantcharov TP, Bardram L, Funch-Jensen P, et al. Laparoscopic performance after one night on call in a surgical department: prospective study. BMJ. 2001;323:1222–1223 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Doumouras AG, Keshet I, Nathens A, et al. A crisis of faith? A review of simulation in teaching team-based, crisis management skills to surgical trainees. J Surg Educ. 2012;69:274–281 [DOI] [PubMed] [Google Scholar]
- 90.Mattar S, Alseidi A, Jones D, et al. General Surgery residency inadequately prepares trainees for fellowship: results of a survey of fellowship Program Directors. Ann Surg. 2013;258:440–449 [DOI] [PubMed] [Google Scholar]
- 91.Kamath AE, Baldwin K, Meade LK, et al. The increased financial burden of further proposed orthopaedic resident work-hour reductions. J Bone Joint Surg Am. 2012;93:e31. [DOI] [PubMed] [Google Scholar]
- 92.Volpp K, Shea J, Small D, et al. Effect of a protected sleep period on hours slept during extended overnight in-hospital duty hours among medical interns: a randomized trial. JAMA. 2012;308:2208–2217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.National Research Council. Resident Duty Hours: Enhancing Sleep, Supervision, and Safety. Washington, DC: The National Academies Press; 2009 [PubMed] [Google Scholar]
- 94.DeRienzo CM, Frush K, Barfield ME, et al. Handoffs in the era of duty hours reform: a focused review and strategy to address changes in the Accreditation Council for Graduate Medical Education common program requirements. Acad Med. 2012;87:403–410 [DOI] [PubMed] [Google Scholar]
- 95.Faryniuk AM, Hochman DJ. Effect of an acute care surgical service on the timeliness of care. Can J Surg. 2013;56:187–191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Wood L, Buczkowski A, Panton OMN, et al. Effects of implementation of an urgent surgical care service on subspecialty general surgery training. Can J Surg. 2010;53:119–125 [PMC free article] [PubMed] [Google Scholar]
- 97.Eckleberry-Hunt J, Vean Dyke A, Lick D, et al. Changing the conversation from burnout to wellness: physician well-being in residency training programs. J Grad Med Educ. 2009;1:225–230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Saadat H, Snow D, Ottenheimer S, et al. Wellness program for anesthesiology residents: a randomized, controlled trial. Acta Anaesthesiol Scand. 2012;56:1130–1138 [DOI] [PubMed] [Google Scholar]
- 99.Edwards S, Verma S, Zulla R. Developing a program for resident wellness at the postgraduate medical education office, University of Toronto. Clin Invest Med. 2007;30:S63. [Google Scholar]
- 100.Philibert I, Nasca TJ, Brigham T, et al. Duty-hour limits and patient care and resident outcomes: can high-quality studies offer insight into complex relationships? Ann Rev Med. 2013;64:467–483 [DOI] [PubMed] [Google Scholar]
- 101.MacFie J. Challenges for the Future of Surgical Training: A Discussion Document. The Surgical Forum of Great Britain and Ireland. London, UK: Federation of Surgical Speciality Association; 2013 [Google Scholar]