Abstract
Objective
Abdominal radical trachelectomy (ART) is one of the fertility-sparing procedures in women with early-stage cervical cancer. The published results of ART, in comparison with vaginal radical trachelectomy, so far are limited.
Materials and Methods
This retrospective study comprises all cases of female patients referred to ART with early-stage cervical cancer from 2 gynecologic oncology centers in Romania.
Results
A total of 29 women were referred for ART, but subsequently, fertility could not be preserved in 3 of them. Eleven women had stage IA2 disease (42.3%), 14 (53.8%) women had stage IB1 disease, and 1 (3.8%) woman had stage IB2 disease. Histologic subtypes were 15 (57.6%) squamous, 8 (30.7%) adenocarcinoma, and 3 (11.5%) adenosquamous. There were no major intraoperative complications in both hospitals. Early postoperative complications were mainly related to the type C parametrectomy—bladder dysfunction for more than 7 days (8 [30.7%] women) and prolonged constipation (6 [23.0%] women). Other complications consisted in symptomatic lymphocele in 2 (7.6%) patients, which were drained. Median follow-up time was 20 months (range, 4–43 months). Up to the present time, there has been 1 (3.8%) recurrence in our series. Most patients did not experience late postoperative complications. Three (11.5%) women are amenorrheic, and 1 (3.8%) woman developed a cervical stenosis. Of the 23 women who have normal menstruation and maintained their fertility, a total of 7 (30.4%) women have attempted pregnancy, and 3 (42.8%) of them achieved pregnancy spontaneously. These pregnancies ended in 2 first trimester miscarriages and 1 live birth at term by cesarean delivery.
Conclusions
Our results demonstrate that ART preserves fertility and maintains excellent oncological outcomes with low complication rates.
Key Words: Cervical cancer, Fertility-sparing procedure, Abdominal radical trachelectomy, Outcomes
Invasive cervical cancer is one of the most common cancers, with 500,000 new cases diagnosed annually. Approximately 15% of all cervical cancers and 45% of surgically treated stage IB cervical cancers occur in women younger than 40 years.1 The excellent prognosis of early-stage cervical cancer (the 5-year survival rate for patients with disease confined to the cervix is 80% to 93%) combined with many patients’ young age has led to a focus on maintaining both the survival prognosis and fertility after treatment. Many young women with decades of survivorship ahead of them consider preservation of fertility a priority and a key element to their quality of life.2
Abdominal radical trachelectomy (ART) is one of the fertility-sparing procedures used in the treatment of early-stage cervical cancer. This technique, invented and described for the first time by the Romanian gynecologist E. Aburel3 in 1956, was almost forgotten for 4 decades and “rediscovered” by the team of Smith et al4 and Ungár et al5 in the 1990s. Together with thex vaginal radical trachelectomy with laparoscopic pelvic lymphadenectomy described in 1994 by Dargent et al,6 it represents a real option for women with cervical cancer stages IA2 to IB2 (and maybe also for IIA) who deserve to preserve their fertility.
After analyzing a few hundred of published cases and comparing with vaginal technique, the abdominal trachelectomy has a shorter learning curve and a higher oncological radicality compared with the vaginal technique.2,5 Another advantage consists of the feasibility to perform it for bulky cervical tumors—2 to 4 cm stage IB1 or IB2 disease.7,8 Its main disadvantage is a less favorable obstetric outcome.2,5 The first successful pregnancy and term delivery subsequent to ART was described in 2001.9
The aim of this study was to present our experiences related to ART in patient selection, surgical complications, and oncological and obstetric results.
MATERIALS AND METHODS
In this retrospective study, all women referred for ART for early-stage cervical cancer in 2 gynecologic oncology centers, the First Clinic of Obstetrics and Gynecology in Târgu Mureş, Romania, and the Regional Institute of Oncology in Iasi, Romania, during May 2010 and June 2013 were enrolled. The criteria for ART were as follows and as recommended10: histologic diagnosis of invasive cervical cancer (squamous cell carcinoma, adenocarcinoma, or adenosquamous carcinoma), fertile age, a desire for future fertility and no history of infertility, stage IA2 to IB2 disease, and estimated length of the remaining cervix of more than 1 cm. Because of similar survival and oncological results of ART compared with radical hysterectomy,11 the Iasi team also considered an acceptable criterion that is the patients’ desire to preserve their menstrual function. The size of the tumor, its location, and the state of lymph nodes were assessed in all patients by a combination of clinical examination, transvaginal ultrasound, and magnetic resonance or computed tomographic scanning.
Both oncology centers used the typical ART technique with ligation of uterine arteries, preservation of ovarian vessels, and a bilateral parametrectomy corresponding to type C radical hysterectomy in the classification published recently by Querleu and Morrow.12 A careful pelvic peritonization was performed at the end of the procedure, as described elsewhere.13 Neither permanent cerclage during trachelectomy nor cerclage at the beginning of pregnancy was placed in any of the patients.
After surgery, all women were followed up at 3-month intervals with clinical examination, transvaginal ultrasound, Papanicolaou test, and squamous cell carcinoma antigen. The patients were advised to wait a minimum of 6 months after the procedure, with at least 2 consecutive normal cytology samples before trying to conceive.
RESULTS
During the described period, a total of 29 female patients were referred for ART, but fertility could not be preserved in 3 (10.7%) women; they underwent immediate completion of radical hysterectomy because of a positive cranial surgical margin (2 patients) and positive lymph nodes on frozen section (1 patient).
The procedure was performed in a total of 26 patients. The median age was 32 years (range, 24–40 years). Only 4 (15.3%) women had offspring from previous pregnancies.
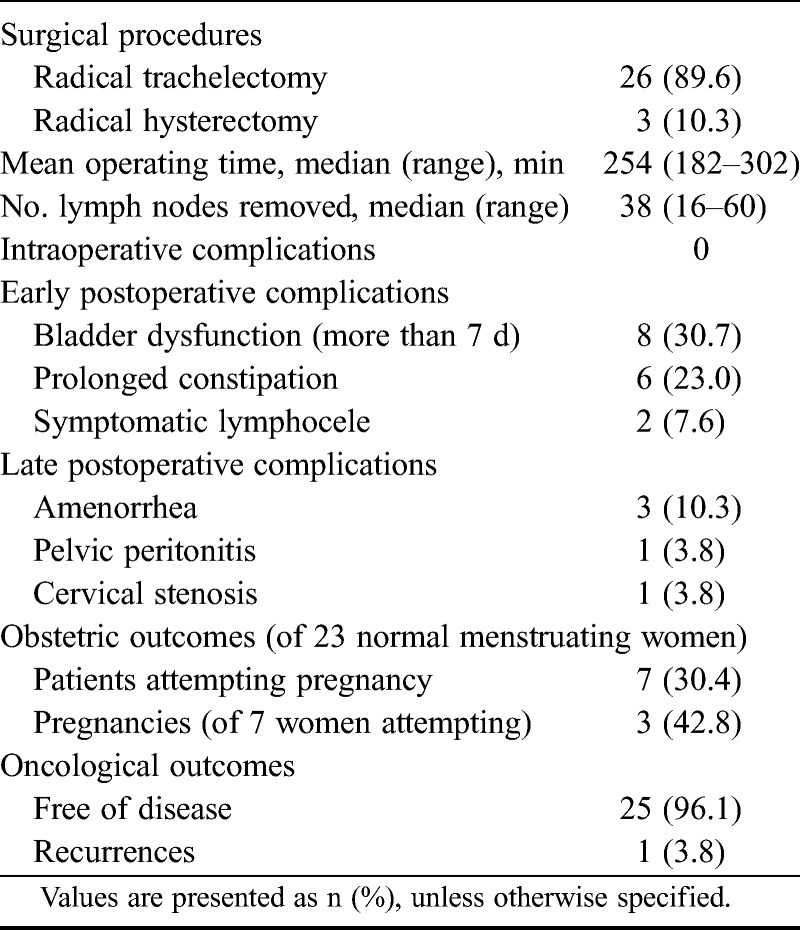
Based on the International Federation of Gynecology and Obstetrics clinical staging system, 11 (42.3%) women had stage IA2 disease, 14 (53.8%) women had stage IB1 disease, and 1 (3.8%) woman had stage IB2 disease. The median tumor size was 1.8 cm (range, 0.3–4.2 cm). Histologic subtypes were 15 (57.6%) squamous carcinoma, 8 (30.7%) adenocarcinoma, and 3 (11.5%) adenosquamous. In the entire study population, the mean operating time was 254 minutes (between 182 and 302 minutes), and the mean number of removed lymph nodes were 38 (between 16 and 60).
There were no major intraoperative complications in both hospitals. Early postoperative complications were mainly related to the type C parametrectomy—bladder dysfunction for more than 7 days (8 [30.7%] patients) and prolonged constipation (6 [23.0%] patients). Other complications consisted in symptomatic lymphocele in 2 (7.6%) patients, which were drained.
Median follow-up time was 20 months (range, 4–43 months). Up to the present time, there has been 1 recurrence in our series, in a 34-year-old nullipara, discovered on the superior part of the vagina 5 months after an ART performed for a stage IA2 grade 3 squamous carcinoma with negative margins and negative lymph nodes in the final pathologic report. She underwent hysterectomy and partial colpectomy, and now, she receives adjuvant chemoradiotherapy.
Most patients did not experience late postoperative complications. Three (11.5%) women are amenorrheic; 1 patient is postmenopausal now at the age of 40 years, 1 patient decided to receive adjuvant radiotherapy for 3 positive lymph nodes (micrometastases) on final pathologic report, and the last 1 patient became amenorrheic, probably as a consequence of diminished blood flow to the endometrium. One patient developed pelvic peritonitis 1 year after the surgery and had a unilateral adnexectomy, but it is difficult to take into consideration a direct causal effect regarding ART. Another patient experienced cervical stenosis, which was solved with dilation of the cervical canal.
Except the 3 patients with amenorrhea, of the total 23 women who had normal menstruation and maintained their fertility, 7 (30.4%) women have attempted pregnancy. Because of the shortness of the follow-up period so far, 3 (42.8%) of our patients achieved spontaneous pregnancy of the previously mentioned 7 women. These pregnancies ended in 2 first trimester miscarriages and 1 live birth at term by cesarean delivery.
All these data are summarized in Tables 1 and 2.
TABLE 1.
Patient characteristics
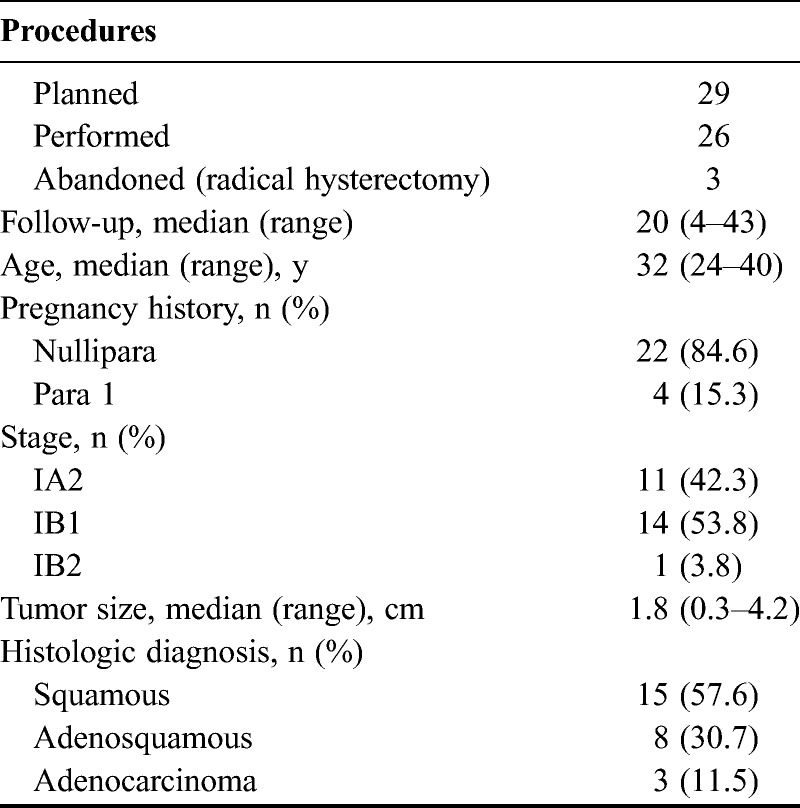
TABLE 2.
Procedures details, complications, and outcomes
DISCUSSION
The management of fertility-sparing surgery must include a good selection of patients and complete information about this technique. They need to be informed about the possibility of late complications and especially the oncological and obstetric outcomes related to the surgery as well as the alternative approaches. There is no guarantee of fertility after a radical trachelectomy, and the standard treatment of early-stage cervical carcinoma is still radical hysterectomy. In addition, the indication for ART regarding the preservation of uterine corpus and subsequently the menstrual function is debatable. Anyway, in the largest literature review,14 only around one third (38%) of these patients attempted to get pregnant. As a fertility-sparing procedure aimed to treat an oncological disease, the ART must find an appropriate balance among oncological radicality, obstetric outcome, and the desire to preserve the menstrual function. Thus, detailed informed consent is essential.15–17
The outcomes of 485 cases of ART have been published up to date,14 but there are still many unanswered questions regarding this technique.
A proper selection of patients proposed for ART is very important. Together with clinical examination, all patients underwent a transvaginal ultrasound examination with power Doppler to assess as precisely as possible the local extension of the tumor. At the same time, we performed a pelvic and abdominal computed tomography scan or magnetic resonance imaging to exclude advanced-stage disease, parametrial invasion, or lymph node metastases. To assess more precisely the cervical tumor regarding the length of the cervix and for a more reliable prediction of the distance from the tumor to the endocervical margin, a transvaginal ultrasound elastography has been performed, and our first results will be ready soon. The sentinel node biopsy technique has not been used in our series, but all intraoperative suspicious lymph nodes were sent for frozen section and the procedure abandoned if this proved to be positive (in 1 patient). In our series, there were found positive cranial margins of the uterine cervix or isthmus in 2 patients, but in some situations, it is quite difficult to asses and to respect intraoperatively the exact estimated length of the remaining cervix of more than 1 cm. A pathologic review of the complete surgical specimen will identify those patients who underwent an attempt at ART but in whom fertility preservation is not appropriate and ensured oncological outcomes are maintained. Currently, the therapeutic options for advanced-stage disease include hysterectomy and/or adjuvant chemoradiation. It remains to be seen whether adjuvant chemotherapy alone or focal surgical procedures, such as the laterally extended parametrectomy for positive lymph nodes, are sufficient as adjuvant therapy that would further increase the percentage of patients who are able to maintain their fertility.
Both our teams did not consider the necessity to perform a cerclage, recommended only by some authors during abdominal trachelectomy.18 As described by Aburel,3 the scary tissue resulted on the uterine isthmus; vaginal anastomosis would be sufficient for a future pregnancy. This may be the reason for the reduced incidence of cervical stenosis in our series (3.9%) compared with other reports (9.5%–12%).2,14 As a fertility-preserving technique and to offer more chances for a spontaneous conception, it is important to perform a careful pelvic peritonization at the end of the procedure.13 In addition, the prophylactic cerclage during the pregnancy is debatable and sometimes technically demanding by vaginal route. So far, there is no evidence regarding a better obstetric outcome.
There are fewer reported pregnancies after ART, which are lower than after vaginal radical trachelectomy, even if correlated to the number of performed procedures. These results are likely or at least partially caused by the selection of patients for both types of procedure.17,19–21 Of the total of 113 patients who attempted to get pregnant, 67 (59.3%) of them were able to conceive.14 But in another study,20 the pregnancy rate among patients who wished to conceive was much lower (36.2% [25/69 patients]). Among the 31 pregnancies in 25 patients, 4 patients had first trimester miscarriage and 1 patient had second trimester miscarriage. Four patients had preterm birth in the second trimester, and 17 patients delivered in the third trimester. Of the 17 pregnancies that reached the third trimester, 2 (11.8%) were preterm births between 29 and 32 weeks, 11 (64.7%) were delivered between 32 and 37 weeks, and 4 (23.5%) were delivered at 37 and above weeks of gestation. In smaller series, the pregnancy rate varied between 10% and 74% of the women who attempted to conceive2,21–24; in our group, this was 42%.
A further challenge for performing ART is the preservation of the uterine arteries, or at least one, to ensure a better blood supply for a subsequent pregnancy. Initial description of the procedure involved the sacrifice of the uterine artery bilaterally. There were concerns that this may lead to uterine atrophy and amenorrhea and subsequently have negative impact on fertility (cervical/isthmic stenosis) and obstetric outcomes (prematurity, low birth weight, etc). Reports about preserving uterine arteries are isolated,25–27 and the main concern could be represented by the possibility to perform a similar type C parametrectomy for oncological safety when preserving the uterine arteries, which is technically more difficult.
The oncological outcomes of 485 patients after ART14 are extremely promising; there were 3.8% disease recurrences and 0.4% deaths because of the disease. Other studies reported recurrence rates between 0% and 10%,2,10,24 similar with those reported after radical hysterectomy for the same stages. For larger cervical tumors (2–4 cm), the recurrence rate ranged between 0% and 38%.8 Currently, there was only 1 (3.8%) recurrence in our series, but the follow-up period is short for many of our patients.
These data demonstrate that ART preserves fertility and maintains excellent oncological outcomes. It is similar to the abdominal radical hysterectomy procedure that most gynecologic oncologists are familiar with. The learning curve is clearly shorter and requires minimal additional training. Therefore, this approach has gained considerable popularity worldwide. Indications and advantages of the abdominal approach include patients with distorted vaginal anatomy, bulky exophytic lesions, and the need for increased radicality. Most women attempting pregnancy after ART are able to achieve pregnancy and deliver in the third trimester. Gynecologic oncologists trained in radical abdominal hysterectomy should consider offering this procedure to eligible patients.
Footnotes
The authors report disclosure of funding received for this work from any of the following organizations: National Institutes of Health, Wellcome Trust, Howard Hughes Medical Institute, and other(s).
REFERENCES
- 1. Noyes N, Knopman JM, Long K, et al. Fertility considerations in the management of gynecologic malignancies. Gynecol Oncol. 2011; 120: 326– 333 [DOI] [PubMed] [Google Scholar]
- 2. Wethington SL, Cibula D, Duska LR, et al. An international series on abdominal radical trachelectomy: 101 patients and 28 pregnancies. Int J Gynecol Cancer. 2012; 22: 1251– 1257 [DOI] [PubMed] [Google Scholar]
- 3. Aburel E. Colpohisterectomia lărgită subfundică. In: Sîrbu P, Chiricută I, Pandele A, Setlacec D, eds. Chirurgia Ginecologică. Ed Medicală, Bucureşti; 1981: 714– 722 [Google Scholar]
- 4. Smith JR, Boyle D, Corless DJ, et al. Abdominal radical trachelectomy: a new surgical technique for the conservative management of cervical carcinoma. BJOG. 1997; 104: 1196– 1200 [DOI] [PubMed] [Google Scholar]
- 5. Ungár L, Pálfalvi L, Hogg R, et al. Abdominal radical trachelectomy: a fertility-preserving option for women with early cervical cancer. BJOG. 2005; 112: 366– 369 [DOI] [PubMed] [Google Scholar]
- 6. Dargent D, Brun JL, Roy M, et al. La trachelectomie elargie (TE) une alternative a l’hysterectomie radicale dans le traitement des cancers infiltrants developes sur la face externe du col uterin. J Obstet Gynaecol. 1994; 2: 285– 292 [Google Scholar]
- 7. Lintner B, Saso S, Tarnai L, et al. Use of abdominal radical trachelectomy to treat cervical cancer greater than 2 cm in diameter. Int J Gynecol Cancer. 2013; 23: 1065– 1070 [DOI] [PubMed] [Google Scholar]
- 8. Wethington SL, Sonoda Y, Park KJ, et al. Expanding the indications for radical trachelectomy: a report on 29 patients with stage IB1 tumors measuring 2 to 4 centimeters. Int J Gynecol Cancer. 2013; 23: 1092– 1098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Palfalvi L, Ungar L, Boyle D, et al. Announcement of healthy baby boy born following abdominal radical trachelectomy. Int J Gynecol Cancer. 2003; 13: 249. [DOI] [PubMed] [Google Scholar]
- 10. Schneider A, Erdemoglu E, Chiantera V, et al. Clinical recommendation radical trachelectomy for fertility preservation in patients with early-stage cervical cancer. Int J Gynecol Cancer. 2012; 22: 659– 666 [DOI] [PubMed] [Google Scholar]
- 11. Diaz JP, Sonoda Y, Leitao MM, et al. Oncologic outcome of fertility-sparing radical trachelectomy versus radical hysterectomy for stage IB1 cervical carcinoma. Gynecol Oncol. 2008; 111: 255– 260 [DOI] [PubMed] [Google Scholar]
- 12. Querleu D, Morrow CP. Classification of radical hysterectomy. Lancet Oncol. 2008; 9: 297– 303 [DOI] [PubMed] [Google Scholar]
- 13. Căpîlna ME, Szabo B, Toma A, et al. Pelvic peritonization after abdominal radical trachelectomy. Int J Gynecol Cancer. 2010; 20 (suppl 2):poster 766 [Google Scholar]
- 14. Pareja R, Rendón GJ, Sanz-Lomana CM, et al. Surgical, oncological, and obstetrical outcomes after abdominal radical trachelectomy—a systematic literature review. Gynecol Oncol. 2013; (Epub ahead of print). [DOI] [PubMed] [Google Scholar]
- 15. Carter J, Sonoda Y, Chi DS, et al. Radical trachelectomy for cervical cancer: postoperative physical and emotional adjustment concerns. Gynecol Oncol. 2008; 111: 151– 157 [DOI] [PubMed] [Google Scholar]
- 16. Carter J, Sonoda Y, Abu-Rustum NR. Reproductive concerns of women treated with radical trachelectomy for cervical cancer. Gynecol Oncol. 2007; 105: 13– 16 [DOI] [PubMed] [Google Scholar]
- 17. Ribeiro Cubal AF, Ferreira Carvalho JI, osta MF, et al. Fertility-sparing surgery for early-stage cervical cancer. Int J Surg Oncol. 2012; 2012: 936534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Lewin SN, Abu-Rustum NR. Fertility-sparing radical abdominal trachelectomy for cervical cancer. In: Levine DA, Barakat RR, Abu-Rustum NR, eds. Atlas of Procedures in Gynecologic Oncology. 2nd ed Informa Healthcare; 2008: 129– 136 [Google Scholar]
- 19. Testa R, Ramirez PT, Ferreyra H, et al. Abdominal radical trachelectomy: a safe and feasible option for fertility preservation in developing countries. J Low Genit Tract Dis. 2013; 17: 378– 384 [DOI] [PubMed] [Google Scholar]
- 20. Nishio H, Fujii T, Sugiyama J, et al. Reproductive and obstetric outcomes after radical abdominal trachelectomy for early-stage cervical cancer in a series of 31 pregnancies. Hum Reprod. 2013; 28: 1793– 1798 [DOI] [PubMed] [Google Scholar]
- 21. Cibula D, Sláma J, Svárovský J, et al. Abdominal radical trachelectomy in fertility-sparing treatment of early-stage cervical cancer. Int J Gynecol Cancer. 2009; 19: 1407– 1411 [DOI] [PubMed] [Google Scholar]
- 22. Li J, Li Z, Wang H, et al. Radical abdominal trachelectomy for cervical malignancies: surgical, oncological and fertility outcomes in 62 patients. Gynecol Oncol. 2011; 121: 565– 570 [DOI] [PubMed] [Google Scholar]
- 23. Muraji M, Sudo T, Nakagawa E, et al. Type II versus type III fertility-sparing abdominal radical trachelectomy for early-stage cervical cancer: a comparison of feasibility of surgical outcomes. Int J Gynecol Cancer. 2012; 22: 479– 483 [DOI] [PubMed] [Google Scholar]
- 24. Plante M. Evolution in fertility-preserving options for early-stage cervical cancer: radical trachelectomy, simple trachelectomy, neoadjuvant chemotherapy. Int J Gynecol Cancer. 2013; 23: 982– 989 [DOI] [PubMed] [Google Scholar]
- 25. Wan XP, Yan Q, Xi XW, et al. Abdominal radical trachelectomy: two new surgical techniques for the conservation of uterine arteries. Int J Gynecol Cancer. 2006; 16: 1698– 1704 [DOI] [PubMed] [Google Scholar]
- 26. Yao T, Mo S, Lin Z. The functional reconstruction of fertility-sparing radical abdominal trachelectomy for early stage cervical carcinoma. Eur J Obstet Gynecol Reprod Biol. 2010; 151: 77– 81 [DOI] [PubMed] [Google Scholar]
- 27. Yoo S, Terai Y, Tanaka T, et al. Role of the two-point pull-up technique for treating the uterine arteries during radical hysterectomy and trachelectomy. Eur J Obstet Gynecol Reprod Biol. 2013; 170: 544– 549 [DOI] [PubMed] [Google Scholar]


