Abstract
Background:
Cardiovascular diseases (CVDs) remain the most common cause of sudden death. Hence, appropriate drug therapy in intensive cardiac care unit (ICCU) is crucial in managing cardiovascular emergencies and to decrease morbidity and mortality.
Objective:
To evaluate prescribing pattern of drugs and direct cost of therapy in patients admitted in ICCU.
Materials and Methods:
Patients admitted in ICCU of a tertiary care teaching hospital were enrolled. Demographic data, clinical history, and complete drug therapy received during their stay in ICCU were noted. Data were analyzed for drug utilization pattern and direct cost of treatment calculated using patient's hospital and pharmacy bills. Rationality of therapy was evaluated based on American College of Cardiology/American Heart Association (ACC/AHA) guidelines.
Result:
Data of 170 patients were collected over 2 months. Mean age of patients was 54.67 ± 13.42 years. Male to female ratio was 2.33:1. Most common comorbid condition was hypertension 76 (44.7%). Most common diagnosis was acute coronary syndrome (ACS) 49.4%. Mean stay in ICCU was 4.42 ± 1.9 days. Mean number of drugs prescribed per patient was 11.43 ± 2.85. Antiplatelet drugs were the most frequently prescribed drug group (86.5%). Mean cost of pharmacotherapy per patient was ‘2701.24 ± 3111.94. Mean direct cost of treatment per patient was ‘10564.74 ± 14968.70. Parenteral drugs constituted 42% of total drugs and 90% of total cost of pharmacotherapy. Cost of pharmacotherapy was positively correlated with number of drugs (P = 0.000) and duration of stay (P = 0.027).
Conclusion:
Antiplatelet drugs were the most frequently prescribed drug group. Mean number of drugs per encounter were high, which contributed to the higher cost of pharmacotherapy. ACC/AHA guidelines were followed in majority of the cases.
Keywords: Acute coronary syndrome, direct treatment cost, drug utilization, intensive cardiac care unit
Introduction
Industrialization, urbanization, and associated lifestyle changes lead to increase prevalence of obesity, type-2 diabetes mellitus, and metabolic syndrome, which are important risk factors for atherosclerosis and also for cardiovascular diseases (CVDs). There is a global rise in CVDs in the 20th and 21st centuries among all races, ethnic groups, and cultures. CVDs are highly prevalent diseases, diagnosed in 80 million adults, i.e., one-third of the adult population. CVDs remain the most common cause of death, accounting for 35% of all deaths, i.e. almost one million deaths each year. Approximately one-fourth of these deaths are sudden.[1,2] More than 80% of the deaths occurred in low and middle income countries. In India, CVDs are the largest cause of mortality, accounting for around one-fourth of all deaths in 2008. A more worrying fact is that the incidences of CVDs have gone up significantly to 24.8% for productive age group between the 25 and 69 years. Among CVDs, 95% of prevalence and 85% of all CVDs-related deaths are contributed by coronary heart diseases (CHDs) in 2004.[3] Indians have genetic predisposition for higher and earlier risk of CHDs than different races all over the world.[4,5] In addition, rapid socioeconomic growth in developing countries like India increases exposure to risk factors for developing CHDs like diabetes, dyslipidemia, hypertension, and smoking.[6,7]
Acute coronary syndromes (ACS) and acute myocardial infarction, acute decompensated heart failure (HF), arrhythmias, and various other cardiac conditions are emergencies that require specialized equipped intensive cardiac care unit (ICCU) setup to perform lifesaving emergency interventions like fibrinolysis, primary percutaneous coronary intervention (PCI), and defibrillation. Certain drugs like antiplatelet, anticoagulants, and fibrinolytics are needed to be administered at the earliest to these critical patients. There are many drugs prescribed in a single patient simultaneously in ICCU with the aim of maximizing efficacy in a particular condition.[8] Prescribing rationally in ICCU is important to minimize chances of drug interactions, adverse drug reactions, and unduly high cost of treatment. Rationality of drug prescriptions can be analyzed based on recent American Heart Association/American College of Cardiology (AHA/ACC) guidelines in various cardiovascular morbidities.[9,10,11]
Pharmacoepidemiology may be drug-oriented, emphasizing the safety and effectiveness of individual drugs or groups of drugs, or utilization-oriented, aiming to improve the quality of drug therapy through pedagogic intervention. Drug utilization study is an essential part of pharmacoepidemiology, and it provides insight into prescribing pattern, prescription quality, determinants, and outcomes of drug use.[12]
To our knowledge, there are limited numbers of studies from India in this direction.[13,14] Hence, this study was aimed to evaluate prescribing pattern and direct cost of therapy in patients admitted in ICCU.
Materials and Methods
A prospective observational study was carried out in ICCU of a tertiary teaching care hospital after obtaining approval from institutional ethics committee. Study was carried out over a period of 2 months-1st August to 30th September, 2012. All the patients (including moribund patients) admitted in the ICCU during this period were enrolled in the study after obtaining a written informed consent of patient or relative. Demographic data like name, age, sex, address, socioeconomic class were recorded on the case record form. Patients′ clinical data including diagnosis, detailed history of illness, past history, family history were noted. The details of drug therapy including the drug prescribed, dose, frequency, and duration of the treatment were noted in the case record form.
Prescribed drugs were analyzed for inclusion in National List of Essential Medicines (NLEM), India, 2011 and Essential Drug List (EDL) of World Health Organization (WHO), 2011.[15,16] Rationality of therapy was evaluated based on class of recommendation by referring to ACC/AHA guidelines.[9,10,11] Direct cost of treatment was calculated using patient's hospital and pharmacy bills. The cost of drugs was obtained from commercial publications like Indian Drug Review 2012 and current index of medical specialities (CIMS) online.[17,18]
Statistical analysis
All the data were recorded in Microsoft Excel 2010 spread sheet® . Analyses were done using Statistical Package for the Social Sciences (SPSS) version 21.0® . A P < 0.05 was considered statistically significant. We used unpaired t-test to compare between ACS with complications and without complications. We used Pearson's coefficient to correlate between number of drugs, stay in days, and cost of pharmacotherapy.
Results
Demographic and clinical characteristics
A total of 170 patients were included over duration of 2 months. Mean age of patients was 54.67 ± 13.42 years. Most of the patients were male 119 (70%). Majority of the patients belonged to age group of 51-70 years, which comprised around 60% of the total patients.
Hypertension 76 (44.7%), ischemic heart disease 75 (44.1%), and type-2 diabetes mellitus 49 (28.82%) constitute majority of the comorbid conditions. Most of the patients presented with chest pain 70.6% and breathlessness 87 (51.2%). Most common addiction was smoking in 78 (45.9%) patients. Mean stay in ICCU was 4.42 ± 1.9 days (range 1-12).
Morbidity pattern
Distribution of morbidity pattern is shown in Figure 1. Most common diagnosis was ACS in 84 (49.4%) patients with mean age of 55.80 ± 11.22 years. Of 84 ACS patients, 22 (26.2%) developed complications like acute decompensated HF, complete heart block, partial atrioventricular block (AV)-block, atrial fibrillation, and so forth. Majority of the complications were seen in ST elevation myocardial infarction (STEMI) patients, i.e. 20 (37.7%) of 53 STEMI patients. Rest two patients with complications were of unstable angina. Table 1 shows comparison of variables in complicated and uncomplicated ACS patients (n = 84).
Figure 1.
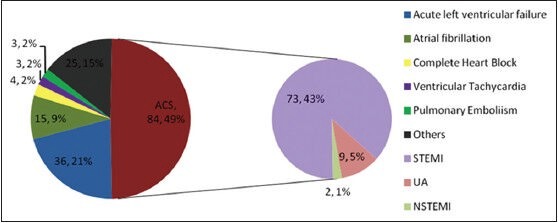
Morbidity pattern in ICCU (n = 170), ICCU: Intensive cardiac care unit; ACS: Acute coronary syndrome; STEMI: ST elevation myocardial infarction; UA: Unstable angina; NSTEMI: Non-ST elevation myocardial infarction
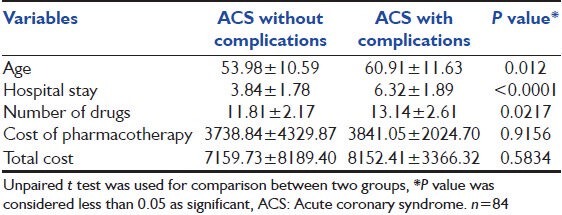
Table 1.
Comparison of variables in complicated and noncomplicated ACS patients
Second most common diagnosis was acute decompensated left ventricular failure (LVF) in 36 (21.2%) patients. Atrial fibrillation 15 (8.8%) was the third most commonly diagnosed CVD.
Prescribing pattern
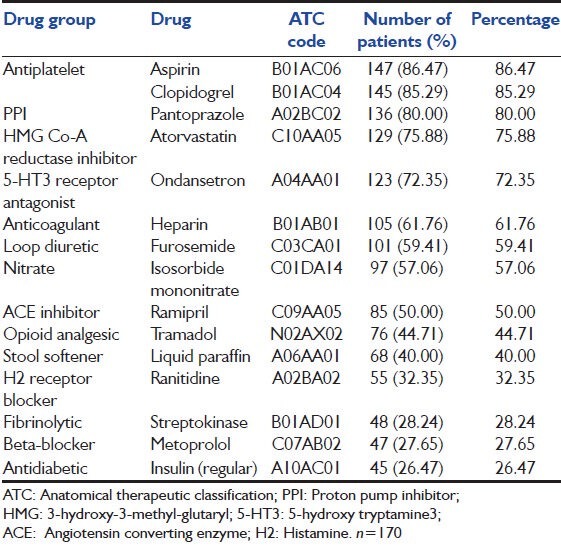
A total of 1943 drugs were prescribed to 170 patients. Mean number of drugs prescribed per patient was 11.43 ± 2.85 (range 3-20). Antiplatelet drugs were the most frequently prescribed drug group in 86.5% of the patients. Aspirin 147 (86.5%) was most frequently prescribed drug followed by clopidogrel 145 (85.3%). Table 2 shows frequently prescribed drugs (n = 170).
Table 2.
Most frequently prescribed drugs
Drug use in acute coronary syndrome
Aspirin and clopidogrel were prescribed to all 84 patients suffering from ACS. Streptokinase was used for thrombolysis in more than two-third patients (67.1%) of STEMI. Unfractionated heparin (UFH) was used in 85.7% ACS patients, and low molecular weight heparin (LMWH) was used in 4.8% ACS patients. Dopamine and dobutamine were used in 16 (19.1%) and nine (10.7%) ACS patients, respectively. Glycoprotein IIb/IIIa receptor antagonists were not used in any ACS patients. Tramadol was used in 76 (44.7%) of the total patients and 63 (75%) patients of ACS.
Figures 2 and 3 show use of drugs in STEMI and unstable angina/non-STEMI UA/NSTEMI patients, respectively, using class of recommendation given by ACC/AHA guidelines.[9,10,11] Apart from use of calcium channel blockers in four patients and intravenous labetolol in one patient, which belonged to class 2a recommendations, all the other prescribed drugs were according to class 1 recommendations of ACC/AHA guidelines.[9,10,11] All the patients with STEMI received tramadol for analgesia instead of morphine, although it is a class 1 recommended drug as per ACC/AHA guideline,[9,10,11] which was a major deviation. In 24 (32.87%) patients, STEMI patients with late presentation (after 12 h of onset), fibrinolytic therapy was not given (class 2a recommendation), which is another deviation according to ACC/AHA guidelines.[9,10,11] In UA/NSTEMI patients (n = 11), all the drugs prescribed were as per AHA/ACC guidelines[9,10,11] [Figure 3].
Figure 2.
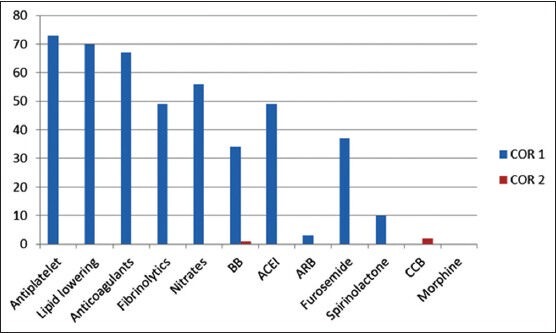
Use of drugs based on ACC/ACS guideline—class of recommendation in STEMI patients (n = 73). ACC: American College of Cardiology; ACS: Acute coronary syndrome; STEMI: ST elevation myocardial infarction; COR: Class of recommendation
Figure 3.
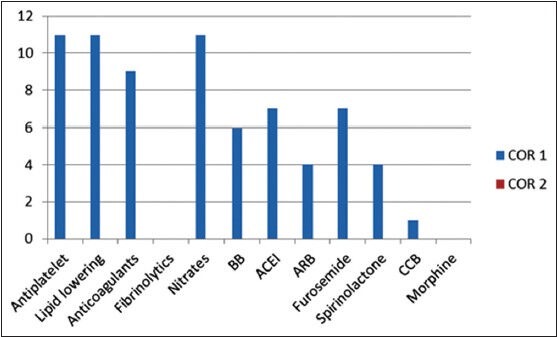
Use of drugs based on ACC/ACS guideline–class of recommendation in NSTEMI/UA patients. n = 11; ACC: American College of Cardiology; ACS: Acute coronary syndrome; UA: Unstable angina; NSTEMI: Non-ST elevation myocardial infarction; COR: Class of recommendation
Drug use in heart failure
Inotropic agents like digoxin, dobutamine, and dopamine were used in 22 (61.1%), 12 (33.3%), and in seven (19.4%) HF patients, respectively. Other drugs like beta-blockers and nitroglycerin were used in 19 (52.8%) and eight (22.2%) patients of 36 patients of acute decompensated HF.
Pantoprazole was coprescribed with clopidogrel in 121 (71.2%) patients. Total 95 (4.9%) antimicrobial drugs were used. Amongst antimicrobials, most commonly prescribed drug was ceftriaxone 36 (37.9%).
Only 19.5% drugs were prescribed by generic name. Numbers of fixed dose drug combinations (FDCs) were 131 (6.7%). Most commonly used FDCs were levosalbutamol + ipratropiumbromide 24 (18.3%) followed by furosemide + spironolactone 15 (11.5%), and aspirin + clopidogrel 13 (9.9%).
Of 1943 drugs, 1470 (75.7%) belong to NLEM, India 2011 and 901 (46.4%) belong to EDL of WHO, 2011.
Direct cost of treatment in ICCU
Mean cost of hospital stay per patient was ₹1425.88 ± 982.11. Mean cost of all investigations per patient was ₹1114.09 ± 212.36. Mean cost of pharmacotherapy per patient was ₹2701.24 ± 3111.94. Mean total cost of hospitalization incurred per patient was ₹10564.74 ± 14968.70.
Of all drugs prescribed, around 42% drugs were administered parenterally and they were responsible for 90% cost burden of total cost of pharmacotherapy. Among all drugs prescribed, only 2.68% were antibiotics used parenterally. The contribution of antibiotics to total cost of pharmacotherapy was 8.07%. Fibrinolytics contributed 44.3% of total cost of pharmacotherapy. Gastrointestinal drugs contributed around 14% of total cost of pharmacotherapy–pantoprazole and ondansetron being the major drugs.
Duration of ICCU stay was positively correlated with number of drugs (Pearson's correlation r = 0.494, P = 0.000) and with cost of pharmacotherapy (Pearson's coefficient r = 0.169, P = 0.027). Number of drugs is positively correlated with cost of pharmacotherapy (Pearson's coefficient r = 0.310, P = 0.000). As the stay in days was increased, number of drugs prescribed per patient and cost of pharmacotherapy both were increased.
Discussion
This study was carried out with the aim to analyze prescribing pattern, the rationality of treatment, and to estimate direct treatment cost in ICCU. Mean age of patients in our study was comparable with Indian study by Patel et al.[13] But mean age of patients in our study is lower as compared with other two other foreign studies that reported 60.45 ± 12.45 and 64 years.[19,20] The possible explanation to this fact could be the lower age in Indian population for CVDs.[5] Other demographic and morbidity pattern in our study was comparable with earlier studies.[13,14,19] The majority of the patients in our study were males which is comparable to similar to earlier Indian and foreign studies.[13,14,19,21]
In our study, prevalence of hypertension and type-2 diabetes is generally high; however, in our study prevalence of these comorbid conditions was lower than that of an Indian study performed in a cardiac unit.[14] The pattern of comorbid conditions may vary with the study population.
Mean stay in ICCU was higher as compared with an Indian study in ICCU that reported 3.07 ± 1.39 days.[13] The possible reason may be due to difference in practicing policies in different hospital ICCUs. Most common diagnosis was ACS, which is comparable with earlier Indian study[13] and a study from Malayasia.[19] Majority of the ACS patients was presented in the age range of 51-60 years, which was also observed by Manurung et al.[21] In our study, incidence of STEMI patients was higher as compared with earlier study.[22] The possible reason of this difference might be due to lifestyle changes and added stress in recent decade. Second major diagnosis in our study was acute LVF, which was higher in our study as compared with an Indian study in ICCU (10.75%).[13]
In Indian studies,[13,23] mean number of drugs was more than 10, which was also seen in our study, in contrast to a foreign study that reported less than 10 drugs.[19] This can be due to difference in morbidity pattern and the different prescribing practices in different countries. Majority (80.5%) of the drugs were prescribed by brand name in our study, which was significantly higher than that of an Indian study of ICCU (65.54%)[13] and that of another study performed in CCU (54.8%).[19] This shows inappropriate prescribing behavior, as the drugs should be prescribed by generic name so as to decrease cost and prescription errors.[24] Hospital stay in days is positively correlated with number of drugs (Pearson's correlation r = 0.494, P = 0.000), which is a known fact.[25]
As per ACC/AHA guidelines, there are three classes of recommendations. Class 1 drugs are those having highest benefit risk ratio and recommended. Class 2 drugs are those with somewhat less benefit risk ratio compared with class 1 and are probably recommended. Class 3 drugs are those that are not recommended or potentially harmful. In our study, considering the rationality based on ACC/AHA guidelines for ACS, in all UA/NSTEMI patients, guidelines were adhered to. As far as drug therapy for STEMI is concerned, majority of prescriptions adhered to the guidelines in form of class 1 and class 2 recommendations. None of the drugs belonging to class 3 were prescribed. However, we detected major deviation in the form of tramadol substituting morphine, which is a class 1 recommended drug for analgesia in all STEMI patients.
Use of aspirin, clopidogrel, UFH, fibrinolytics, and beta-blockers were according to standard ACC/AHA guidelines.[9,10] Antiplatelet drugs were the most frequently prescribed; this finding was similar to other Indian studies.[13,14] In our study, none of the patients received glycoprotein IIb/IIIa receptor antagonists. Abciximab is a first-line glycoprotein IIb/IIIa inhibitor for patients undergoing primary PCI, who have not received fibrinolytics.[9,10] Only two ACS patients underwent PCI, none of them received glycoprotein IIb/IIIa receptor antagonist due to its prohibitive cost.
Among fibrinolytics, streptokinase was most commonly used agent in 96% of fibrinolytic-treated STEMI patients (65.75% STEMI) in our study due to its affordability (as it is the least expensive option available). Use of streptokinase was higher as compared with other studies.[14,20] This can be due to few primary PCI interventions in this study.
Heparin was used for anticoagulation in majority of the patients of ACS after the fibrinolytic therapy was over. Even the LMWHs have shown equal efficacy and better clinical composite end points in the treatment of STEMI.[1] In our study, LMWHs had a limited usage probably because of the cost.[9,10]
Tramadol was used in 44.71% of total patients and 75% patients of ACS. Tramadol, which is a weak mu agonist and is relatively free from side effects like respiratory depression, has been used in the majority of the patients. However, clinical studies demonstrating effectiveness of tramadol in ACS are lacking. Morphine and pethidine usage is advocated as per the guidelines; none of the patients in this study received morphine or pethidine.[9,10]
Use of inotropes, beta-blockers, and vasodilators in HF patients was according to standard ACC/AHA guidelines for acute HF.[11]
The proton pump inhibitors (PPI) could lead to therapeutic ineffectiveness of clopidogrel because this metabolic enzyme–CYP2C19–is responsible for its bioactivation. So, wide use of PPIs needs a “watchful eye” when coprescribed with other drugs.[26]
Most commonly prescribed antimicrobial drug group was third generation cephalosporin in our study, which was similar to an Indian study.[13] Cardiac interventions are clean surgeries according to Centers for Disease Control and Prevention (CDC) guidelines;[27] cefazolin, which is a first generation cephalosporin having excellent Gram-positive coverage should be used for prophylaxis against the development of surgical site infection. Prescribers in our setup used antibiotics for 3 days, which is irrational according to CDC guidelines.[27] Use of antibiotics for extra days will contribute more to the cost of pharmacotherapy.
Mean cost of pharmacotherapy, hospital stay, investigations per patient constituted 25.57, 13.50, and 10.55% per patient, respectively. Mean cost of pharmacotherapy was higher than that of an Indian study (‘867.84).[13] Among all the drugs, 42% were administered parenterally adding to a significant cost burden to the patient. Pantoprazole, ondansetron, heparin, tramadol, streptokinase, furosemide, dopamine, dobutamine, ceftriaxone, and other constituted most of the parenteral drugs. About 90% of total cost of pharmacotherapy was attributed to these parenteral drugs. This finding was comparable with an Indian study.[13] Our institute is a nonprofit organization. Our institute is a semigovernment institute, although the cost of investigations was subsidized, but they were still higher as compared with government setup. Cost of fibrinolytics is justifiable, but the off-label use of PPI and 5-hydroxy tryptamine3 (5-HT3) antagonists contributed significantly to cost of drugs, which needs attention.[28]
Earlier studies estimated only direct cost of pharmacotherapy, whereas in our study we have analyzed the total cost of treatment. In the present study, we have also analyzed different variables with regard to uncomplicated and complicated ACS, which was lacking in earlier studies. Our study has evaluated rationality of pharmacotherapy in ICCU based on ACC/AHA guidelines[9,10,11] for various CVDs, including ACSs and HF.
Our study had a few limitations. This was a short study with no follow up after discharge from the ICCU. We did not estimate the indirect cost, which includes daily wages loss, transportation cost, and so forth. Focusing on drug therapy in ICCU would be helpful to cardiologists in improving prescribing policies. Future studies can focus on drug use in ICCU and outcomes like adverse drug reactions and actual drug-drug interactions.
Conclusion
Antiplatelet drugs were the most frequently prescribed drug group in ICCU. Mean number of drugs per encounter is high, which contributes more to the cost of pharmacotherapy. Most of the drugs belonged to NLEM. ACC/AHA guidelines were followed for all prescriptions except for use of tramadol in place of morphine for analgesia in all STEMI patients.
Acknowledgement
Our sincere thanks to the Dean of the college Dr. Pankaj R. Patel.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Gaziano TA, Gaziano JM. Epidemiology of cardiovascular diseases. In: Longo DL, Fauci AS, Kasper DL, Hauser SL, Jameson JL, Loscalzo J, editors. Harrison's Principles of Internal Medicine. 18th ed. McGraw Hill: 2012. pp. 1811–6. [Google Scholar]
- 2.Epidemiology of Cardiovascular Disease. Promoting Cardiovascular Health in the Developing World: A Critical Challenge to Achieve Global Health. Epidemiology of Cardiovascular Disease. [Last cited on 2013 Aug 13]. Available from: http://www.ncbi.nlm.nih.gov/books/NBK45688/
- 3.Cardiovascular diseases in India-Challenges and way ahead. [Last cited on 2013 Aug 13]. Available from: http://www.deloitte.com/assets/Dcom.India/Local%20Assets/Documents/Cardiovascular_diseases_in_India.pdf .
- 4.Rissam HS, Kishore SN. Trehan coronary artery disease in young Indians - The missing link. J Indian Acad Clin Med. 2001;3:128–32. [Google Scholar]
- 5.Bahl VK, Prabhakaran D, Karthikeyan G. Coronary artery disease in Indians. Indian Heart J. 2001;53:707–13. [PubMed] [Google Scholar]
- 6.Okrainec K, Banerjee DK, Eisenberg MJ. Coronary artery disease in the developing world. Am Heart J. 2004;148:7–15. doi: 10.1016/j.ahj.2003.11.027. [DOI] [PubMed] [Google Scholar]
- 7.Reddy KS, Yusuf S. Emerging epidemic of cardiovascular disease in developing countries. Circulation. 1998;97:596–601. doi: 10.1161/01.cir.97.6.596. [DOI] [PubMed] [Google Scholar]
- 8.Kutz JN, Becker RC. Evolution of the Coronary Care Unit: Past, Present, and Future. In: Jeremias A, Brown DL, editors. Cardiac Intensive Care. 2nd ed. Philadelphia: Elsevier Publication; 2010. pp. 1–8. [Google Scholar]
- 9.O′Gara PT, Kushner FG, Ascheim DD, Casey DE, Jr, Chung MK, de Lemos JA, et al. CF/AHA Task Force.2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: Executive summary: A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2013;127:529–55. doi: 10.1161/CIR.0b013e3182742c84. [DOI] [PubMed] [Google Scholar]
- 10.O′Connor RE, Brady W, Brooks SC, Diercks D, Egan J, Ghaemmaghami C, et al. Part 10: Acute coronary syndromes: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2010;122:S787–817. doi: 10.1161/CIRCULATIONAHA.110.971028. [DOI] [PubMed] [Google Scholar]
- 11.Weintraub NL, Collins SP, Pang PS, Levy PD, Anderson AS, Arslanian-Engoren C, et al. American Heart Association Council on Clinical Cardiology and Council on Cardiopulmonary, Critical Care, Perioperative and Resuscitation. Acute heart failure syndromes: Emergency department presentation, treatment, and disposition: Current approaches and future aims: A scientific statement from the American Heart Association. Circulation. 2010;122:1975–96. doi: 10.1161/CIR.0b013e3181f9a223. [DOI] [PubMed] [Google Scholar]
- 12.Introduction to Drug Utilization Research. [Last cited on 2013 Aug 13]. Available from: http://apps.who.int/medicinedocs/en/d/Js4876e/
- 13.Patel BJ, Patel KH, Trivedi HR. Drug utilization study in intensive coronary care unit of a tertiary care teaching hospital. NJIRM. 2012;3:28–33. [Google Scholar]
- 14.Wal P, Wal A, Nair VR, Rai AK, Pandey U. Management of coronary artery disease in a Tertiary Care Hospital. J Basic Clin Pharm. 2013;4:31–5. doi: 10.4103/0976-0105.113605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.National List of Essential Medicines of India. [Last cited on 2013 Aug 13]. Available from: http://www.cdsco.nic.in/NationalListofEssentialMedicine.finalcopy.pdf .
- 16.WHO Model Lists of Essential Medicines-2011. [Last cited on 2013 Aug 13]. Available from: http://whqlibdoc.who.int/hq/2011/a95053_eng.pdf .
- 17.Malik A, Malik S. Indian drug review compendium. 1st ed. New Delhi: Mediworld Publications; 2012. [Google Scholar]
- 18.CIMS Asia. [Last cited on 2013 Aug 13]. Available from: http://www.cimsasia.com/
- 19.Al-Junid SM, Ezat WP, Surianti S. Prescribing patterns and drug cost among cardiovascular patients in Hospital Universiti Kebangsaan Malaysia. Med J Malaysia. 2007;62:59–65. [PubMed] [Google Scholar]
- 20.Hod H, Gotlieb S, Green M, Hammerman H, Zahger D, Hasdai D, et al. Trends in management, morbidity and mortality of patients with acute myocardial infarction hospitalized in the last decade. Harefuah. 2006;145:326–31, 400. [PubMed] [Google Scholar]
- 21.Manurung D. Lipid profiles of acute coronary syndrome patients hospitalized in ICCU of Cipto Mangunkusumo Hospital. Acta Med Indones. 2006;38:196–201. [PubMed] [Google Scholar]
- 22.Valente S, Lazzeri C, Sori A, Giglioli C, Bernardo P, Gensini GF. The recent evolution of coronary care units into intensive cardiac care units: The experience of a tertiary center in Florence. J Cardiovasc Med (Hagerstown) 2007;8:181–7. doi: 10.2459/JCM.0b013e32801261e3. [DOI] [PubMed] [Google Scholar]
- 23.Patel VK, Acharya LD, Rajakannan T, Surulivelrajan M, Guddattu V, Padmakumar R. Potential drug interactions in patients admitted to cardiology wards of a south Indian teaching hospital. Australas Med J. 2011;4:9–14. doi: 10.4066/AMJ.2011.450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Richard FG. The ongoing regulation of generic drugs. N Engl J Med. 2007;357:1993–6. doi: 10.1056/NEJMp078193. [DOI] [PubMed] [Google Scholar]
- 25.Shankar R, Partha P, Shenoy N. Prescribing Patterns of drugs among patients admitted with cardiovascular disorders in the internal medicine ward: Prescribing patterns in inpatients. [Last cited on 2013 Aug 13];Internet J Pharmacol. 2001 1 Available from: http://www.ispub.com/IJIM/3/1/3481 . [Google Scholar]
- 26.Drug Interactions Checker from Drugs.com. [Last cited on 2013 Aug 13]. Available from: http://www.Drug.com .
- 27.Mangram AJ, Horan TC, Pearson ML, Silver LC, Jarvis WR. Guideline for prevention for of surgical site infection; 1999. Centers for Disease Control and Prevention (CDC) Hospital Infection Control Practices Advisory Committee. [Last cited on 2013 Aug 13];Am J Infect Controla. 1999 27:97–132. Available from: http://www.cdc.gov/hicpac/pdf/guidelines/SSI 1999.pdf . [PubMed] [Google Scholar]
- 28.Singh H, Houy TL, Singh N, Sekhon S. Gastrointestinal prophylaxis in critically ill patients. Crit Care Nurs Q. 2008;31:291–301. doi: 10.1097/01.CNQ.0000336814.04548.ec. [DOI] [PubMed] [Google Scholar]


