Abstract
A case of massive right pleural effusion in a postoperative patient of percutaneous nephrolithotomy leading to severe respiratory distress is reported. A high degree of clinical suspicion and prompt intervention by insertion of an intercostal drainage tube prevented the patient from going in to respiratory failure. The development of arrhythmias confused the picture increasing the morbidity of the patient. However, the patient was managed in an intensive care unit with intercostal chest tube insertion and antiarrhythmic agents. After correction of the specific cause of the effusion the intercostal tube was removed on the 4th day without further recurrence of the effusion.
Keywords: Percutaneous nephrolithotomy, pleural effusion, urinothorax
Introduction
The retroperitoneal leakage of urine resulting from a disruption/obstruction of the urinary tract is known as urinoma. The resultant retroperitoneal or intraperitoneal collection of urine finds a way across transdiaphragmatic barrier due to persistent high pressure. Therefore, a concomitant ipsilateral or bilateral pleural effusion should raise suspicion of urinothorax. Thoracocentesis followed by measurement of creatinine in the pleural fluid is a procedure to establish the true diagnosis.[1] Initially, it was described by Corriere et al. in 1968 in their studies on ureteral obstruction in dogs.[2] Nowadays, cases of urinothorax have been described in human patients. Increased awareness of this entity coupled with the availability of advanced imaging and scintigraphic techniques have resulted in the early diagnosis of urinothorax cases.[3]
Case Report
A 65-year-old female patient developed chest pain and respiratory distress on the 2nd day of a percutaneous nephrolithotomy (PCNL) done for lithiasic ureteral obstruction. Since, the patient had evident left bundle branch block in the preoperatory electrocardiogram (ECG), was in evident respiratory distress and chest discomfort, a 12 lead ECG was done, which showed a paroxysmal supraventricular tachycardia. It was treated with amiodarone 5 mg/kg given through slow intravenous infusion and later with diltiazem 30 mg 3 times in a day. The troponin-T and creatine phosphokinase-MB were negative. On physical examination, there were markedly decreased breath sounds on the right side of chest with crepitations. The respiratory rate was 35/min, pulse 142/min and blood pressure 110/82 mm of Hg. Arterial blood gas analysis showed a type I respiratory failure with PO2-50 mm Hg, PCO2-33.3 mm Hg, pH-7.5, HCO3-22.2 mmol/L, O2 saturation 86%. The chest radiograph, as shown in Figure 1, revealed a large fluid collection with a collapsed right lung. Chest ultrasonography confirmed a pleural effusion. The patient was transferred to the intensive care unit for further management.
Figure 1.
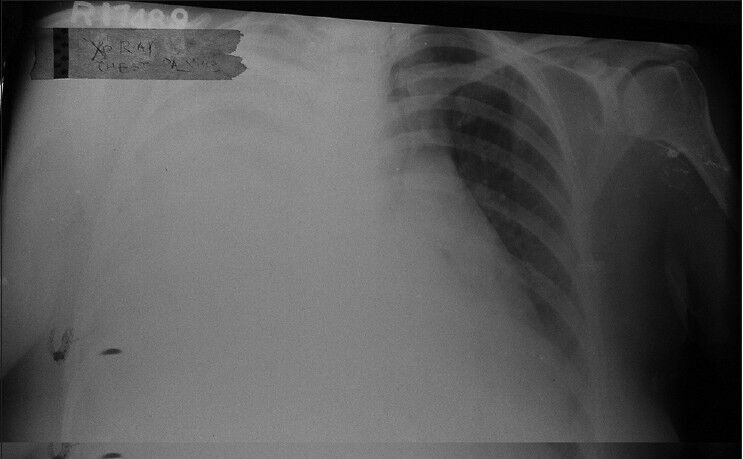
Right side massive pleural effusion
Thoracocentesis was performed which yielded 1.5 L of straw colored fluid with distinctive smell of urine. Fluid analysis revealed a total protein of 0.9 g/dL, pH 7.13, lactate dehydrogenase (LDH) 868 U/L, glucose 28 mg/dL, creatinine 11 mg/dL and urea of 115 mg/dL with a cellularity of 2800/mm3. The bacteriological examination of the fluid revealed no micro-organism in Gram's stain and no acid fast bacilli in Ziehl-Nielsen stain. The fluid culture was negative. The serum LDH levels were 439 U/L, blood urea 115 mg/dL and serum creatinine of 3.4 mg/dL. The routine examination of urine was normal, but the microscopy revealed plenty of red blood cells and pus cells. The urine culture was negative. The electrolytes showed no disarrangements. Ultrasonography revealed a persistent effusion and an intercostal chest tube (ICD) was inserted allowing the drainage of 3 L of fluid. A central venous cannulation was done to guide fluid therapy. The patient had a single functional kidney in which PCNL was done. The blood urea and serum creatinine levels started rising and the patient developed oliguria. A decision was made to put a Double J (DJ) stent and change the ureteric catheter to correct oliguria. In the operation theater, it was found that the ureteric catheter had slipped from its position which was the cause for obstruction and recurrent collection. The respiratory distress subsided and arrhythmias secondary to the hypoxemia were controlled after DJ stenting. The ICD was removed on the 4th day when there was a full expansion of lung as shown in theFigure 2. The patient was transferred to the ward and was discharged home on the 10th day.
Figure 2.
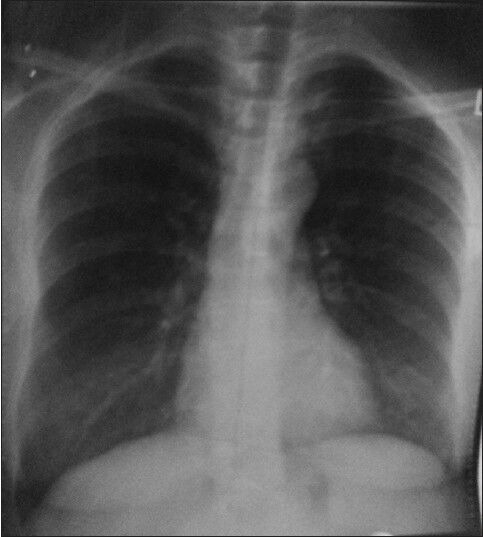
Full expansion of lung
Discussion
Urinothorax can be divided into two categories. (1) Obstructive urinothorax due to bilateral obstructive uropathy and (2) traumatic urinothorax due to unilateral traumatic injury of the urinary system, mostly iatrogenic.[4] It is a rare cause of transudative pleural effusion secondary to obstructive uropathy. There are two theories under debate concerning the mechanisms responsible for the transdiaphragmatic evasion of urine. (1) Urine may travel through lymphatic drainage into pleural space or (2) retroperitoneal urine firstly enters the peritoneal cavity and afterwards travels through direct transdiaphragmatic passage into the pleural cavity.[5] In general, the patient with urinothorax have low pH and high LDH levels, resulting in misinterpretation of the effusion being exudative. The average pleural fluid-to-serum creatinine ratio is in the range of 1.09-19.8.[6] Pleural effusion can occur due to infections, malignancies, and congestive heart failure. Urinothorax is clearly an uncommon cause of pleural effusion.[7]
Our patient presented with severe respiratory distress after undergoing PCNL. The chest radiograph revealed a massive pleural effusion and thoracocentesis led to high suspicion of urinothorax due to a distinctive urine smell. An ICD was put under ultrasonographic guidance due to recurrent effusion. The distinctive urine smell and its subsequent biochemical analysis-with characteristic of transudate except for the high LDH levels-and the pleural fluid-to-serum creatinine ratio of 3.2 confirmed the diagnosis of urinothorax. Renal scintigraphy with technetium-99 m DTPA, technetium 99 m ethylene dicysteine or with technetium 99 m mercaptoacetyltryglycerine-3 can demonstrate any extravasation of urine from the region of the kidney or ureter.[5,8] Due to hemodynamic instability our patient could not be subjected to further investigation. The fluid in urinothorax is usually straw-colored with a distinctive ammoniacal smell. In the majority of cases, the fluid is transudative according to Light's criteria, with biochemical features of low glucose, low protein, and low pH, but elevated LDH levels.[9,10] The most important biochemical parameter is the pleural fluid creatinine-to-serum creatinine ratio which is >1 and mostly >10.[3] Urinothorax should be included in the differential diagnosis of pleural effusion in patients with a recent urinary tract disorder even with features of pleural exudate.[11] The correction of the underlying cause usually leads to resolution of urinothorax; however, in the present case, despite the pleural drainage with a thoracostomy tube, repeated collection occurred due to the unnoticed slippage of the ureteric catheter that lead to oliguria and rise in blood urea and serum creatinine levels. Insertion of a DJ stent allowed the resolution of the problem and complete lung reexpansion.
Conclusion
The physicians should include urinothorax in the differential diagnosis of pleural effusions, particularly in patients that underwent kidney or ureteral surgical procedures such as extracorporeal shock wave lithotripsy, PCNL, or ureterorenoscopy. As most of the cases can be managed only with therapeutic thoracocentesis and resolution of the underlying problem, aggressive chest tube drainage of voluminous effusion with respiratory failure is only rarely needed.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Gurtner B. Urine in the wrong place: Urothorax. Schweiz Rundsch Med Prax. 1994;83:30–5. [PubMed] [Google Scholar]
- 2.Corriere JN, Jr, Miller WT, Murphy JJ. Hydronephrosis as a cause of pleural effusion. Radiology. 1968;90:79–84. doi: 10.1148/90.1.79. [DOI] [PubMed] [Google Scholar]
- 3.Handa A, Agarwal R, Aggarwal AN. Urinothorax: An unusual cause of pleural effusion. Singapore Med J. 2007;48:e289–92. [PubMed] [Google Scholar]
- 4.Garcia-Pachon E, Romero S. Urinothorax: A new approach. Curr Opin Pulm Med. 2006;12:259–63. doi: 10.1097/01.mcp.0000230628.65515.86. [DOI] [PubMed] [Google Scholar]
- 5.Bhattacharya A, Venkataramarao SH, Kumar S, Mittal BR. Urinothorax demonstrated on 99mTc ethylene dicysteine renal scintigraphy. Nephrol Dial Transplant. 2007;22:1782–3. doi: 10.1093/ndt/gfm105. [DOI] [PubMed] [Google Scholar]
- 6.Garcia-Pachon E, Padilla-Navas I. Urinothorax: Case report and review of the literature with emphasis on biochemical diagnosis. Respiration. 2004;71:533–6. doi: 10.1159/000080642. [DOI] [PubMed] [Google Scholar]
- 7.Doerr CH, Miller DL, Ryu JH. Chylothorax. Semin Respir Crit Care Med. 2001;22:617–26. doi: 10.1055/s-2001-18797. [DOI] [PubMed] [Google Scholar]
- 8.Jelic S, Sampogna RV. Detection of unrecognized urinothorax with renal scintigraphy. Kidney Int. 2009;76:353. doi: 10.1038/ki.2009.149. [DOI] [PubMed] [Google Scholar]
- 9.Tortora A, Casciani E, Kharrub Z, Gualdi G. Urinothorax: An unexpected cause of severe dyspnea. Emerg Radiol. 2006;12:189–91. doi: 10.1007/s10140-006-0468-x. [DOI] [PubMed] [Google Scholar]
- 10.Light RW, Macgregor MI, Luchsinger PC, Ball WC., Jr Pleural effusions: The diagnostic separation of transudates and exudates. Ann Intern Med. 1972;77:507–13. doi: 10.7326/0003-4819-77-4-507. [DOI] [PubMed] [Google Scholar]
- 11.Mora RB, Silvente CM, Nieto JM, Cuervo MA. Urinothorax: Presentation of a new case as pleural exudate. South Med J. 2010;103:931–3. doi: 10.1097/SMJ.0b013e3181e9a38a. [DOI] [PubMed] [Google Scholar]


