Abstract
U.S. prisons have a court-affirmed mandate to provide health care to prisoners. Given this mandate, we sought to determine whether use of prison health care was equitable across race using a nationally-representative sample of Black and White male state prisoners. We first examined the prevalence of health conditions by race. Then, across all health conditions and for each of 15 conditions, we compared the proportion of Black and White male prisoners with the condition who received health care. For most conditions including cancer, heart disease, and liver-related disorders, the age-adjusted prevalence of disease among Blacks was lower than among Whites (p<.05). Blacks were also modestly more likely than Whites to use health care for existing conditions (p<.05), particularly hypertension, cerebral vascular accident/brain injury, cirrhosis, flu-like illness, and injury. The observed racial disparities in health and health care use are different from those among non-incarcerated populations.
Keywords: Prisoners, health disparities, access to health care, health care systems
Remarkably, the incarceration rate among U.S. adults now exceeds one in 100, and 1.6 million adults are currently serving sentences in state or federal prisons.1,2 Many of these prisoners have engaged in illicit and non-illicit behaviors that can be harmful to health. For example, in national surveys, 57% of state prisoners reported drug use in the month prior to their offense,3 and 50% of prisoners report being current smokers.4 Additionally, before imprisonment many inmates resided in impoverished communities and had diminished access to health care.5–7 Several reports suggest that prison populations have a high burden of disease,3,4,8–11 and as correctional populations grow—and age—a wider spectrum of medical and mental health conditions will become increasingly prevalent within U.S. prisons.12
Confronted with the growing health care needs of the prison population, prisons have a court-affirmed mandate to provide health care. In the 1976 case Estelle v. Gamble, the U.S. Supreme Court ruled that the Eighth Amendment (which prohibits cruel and unusual punishment of prisoners) requires that prisoners be provided with medical care. However, the two legal tests for care—that medical need is “serious” and that prison officials are not “deliberately indifferent” to that need—provide little guidance about the actual provision of care.13 Since the Estelle ruling, recommendations for prison health care have been developed by, among others, the World Health Organization,14 the American Correctional Association,15 and the National Commission on Correctional Health Care (NCCHC).16 The ability and willingness of state and federal prison systems to address these growing and often costly health care needs remains undetermined, and in the 35 years since Estelle, there have been few published assessments of health care services available in prison or prisoners’ use of health care.17
While we are unaware of any broad quantitative assessment of prison health care services, in a 2004 article B. Jaye Anno, cofounder of NCCHC, provided a general sketch of health care services available in correctional settings. According to Anno, prisoners are first admitted to a reception and diagnostic facility where they generally receive an interview regarding their medical history and health needs and are screened for tuberculosis, all within the first few hours. In the next week or two, prisoners receive more thorough medical examinations and are screened for mental illness, substance abuse, and intellectual deficiencies. Following the two-week period, prisoners are transfer to their prison of assignment. Prisons typically use a written request for inmates to access health services for their routine health care needs, and prisons have automated systems for follow-up appointments, medications reviews, and periodic health exams. Most prisons provide on-site ambulatory health care and have standing arrangements either with another prison in its system or with community providers to provide additional care.17
Despite the dearth of information about the availability of health care resources in prison, a nationally representative survey of state prisoners conducted by the U.S. Census Bureau and Bureau of Justice Statistics has provided some insights into prisoners’ disease burden and use of care.18 Analyzing this data, Wilper et al. found that 38% of state prisoners reported a persistent medical condition, but of these, 20% reported that the condition was not examined by medical personnel.19
While results of the Wilper et al. analyses were not disaggregated by health conditions, gender, or race, there is some suggestion that the racial disparities in health and health care observed among non-incarcerated populations may narrow in prison. Examining prisoner mortality data from 29 U.S. states, Patterson found that the age-specific death rates among Black and White male prisoners were similar and each equivalent to those of White non-incarcerated men.20 Other studies of single state prison systems have found similar results21,22 although in the latter study the effect may have been an artifact of the compassionate release program, which sanctioned the release of terminally ill prisoners. Nevertheless, mortality rates from these studies are in contrast to those of the general population, where the age-adjusted mortality rate of Black men is about 40% higher than that of White men.23
It is not completely clear why mortality rates among Black men in prison are lower than those of Black men in the community. A portion of the mortality reduction among male Black prisoners likely reflects the protective effect of prisons, which may shield young men from high levels of accidents and violence in their communities.22,24 However, Patterson demonstrated that age-specific mortality rates among Black male prisoners remained lower than those of Black men in the general population, even after the general population mortality rate was adjusted to exclude two of the most common causes of traumatic deaths among non-institutionalized Black men, motor vehicle and firearm deaths. Consequently, Patterson hypothesized that beyond the apparently protective effect of incarceration to reduce accidental and violent deaths, prison health care may have had an impact in diminishing mortality rates among Black prisoners.20
Indeed, mortality rates are likely to be affected by both prison health care and prisoners’ burden of disease, but these have not been well-delineated by race within a national sample of prisoners. Disease prevalence has been examined by race among prisoners in the Texas Department of Criminal Justice, one of the largest U.S. prison systems. Results from these analyses are mixed. Harzke et al. found that age-adjusted prevalence of chronic medical conditions among Blacks was greater than that of Whites for hypertension, asthma, and diabetes but lower for ischemic heart disease.25 In an earlier study from the Texas prison system with unadjusted disease rates, White men were shown to have lower rates of tuberculosis and HIV than Black men, but higher rates of viral hepatitis.26 Further, in an analysis by Binswanger et al. focusing on comparing disease prevalence among prisoners and non-prisoners using nationally-representative surveys, it was noted that incarceration was generally associated with a higher prevalence of chronic disease among non-Hispanic Whites than among non-Hispanic Blacks and Hispanics; however, the only conditions for which rates of disease were contrasted between Black and White prisoners were hepatitis (higher in Whites) and hypertension (higher in Blacks).4
In the context of the court-affirmed mandate to provide prisoners with health care and the observed reduction in mortality among Black male prisoners compared with their community counterparts, we sought to examine whether use of prison health care differed by race. To do so, we used a nationally representative sample of prisoners to estimate and compare disease prevalence and use of health care among Black and White prisoners. To determine whether our findings were biased by differences in disease detection, we also tested for racial differences in the proportion of prisoners assessed for disease upon prison admission. The findings from these analyses not only provide some context for the previously observed patterns of mortality, but they also build upon our growing understanding of health and health care in our nation’s state prison systems.4,19
Methods
Data source
Data for these analyses come from a public use dataset of The 2004 Survey of Inmates in State Correctional Facilities, which was conducted by the U.S. Census Bureau on behalf of the Bureau of Justice Statistics.18 The survey was administered to a nationally representative sample of state prisoners and is one of a series of surveys that has been conducted about every six years since 1974. Note that this survey is one of several surveys utilized in analyses by Wilper et al.19 and Binswanger et al.,4 which were cited in the introduction.
Data for the 2004 survey were collected during face-to-face interviews conducted from October 2003 through May 2004. Interviews, which lasted about an hour, were conducted using computer-assisted personal interviewing (CAPI), in which a computer program prompts the interviewer with questions, and provides follow-up questions based on the respondent’s answer. All data for the study presented here, with the exception of prison medical expenditures, are based on prisoners’ self-report.
Below, we summarize the U.S. Census Bureau’s sampling scheme and estimation of sample weights. We also describe the survey items included in this analysis and, when appropriate, their coding. A complete description of the sampling procedure and survey items is provided in the survey codebook which, along with the data, is accessible online via the Inter-University Consortium of Political and Social Research website (www.icpsr.umich.edu).18
Our own preliminary analyses suggested that this dataset was not well-suited to examine disease prevalence or use of health care among female prisoners or Hispanic prisoners (both males and females) because, after stratifying by race and condition, the number of prisoners in each category was generally small, resulting in estimates that were too imprecise to make meaningful comparisons. We therefore limited the focus of these analyses to non-Hispanic Black and non-Hispanic White male prisoners, who constituted approximately 70% of all state prisoners in 2004.
Sampling
The sample was selected using a two-stage design. Prisons were selected in the first stage, and inmates within selected prisons were sampled in the second stage. A sampling frame was created based on all state prisons incarcerating men; this included prisons that incarcerated both men and women.
Based on the 2000 Census of State and Federal Correctional Facilities, the universe of state prisons incarcerating men included a total of 1,401 prisons (Appendix Figure 1). An additional 34 prisons, which opened between 2000 and 2003, were also included (for a total of 1,435 prisons). Prisons with more than 6,445 prisoners were selected with certainty as were other large prisons (more than 1,500 prisoners) that also reported medical, mental health, or geriatric care functions. As a result, the 14 largest prisons for men were selected with certainty. The remaining prisons were divided into eight geographic strata. The number of prisons selected within each stratum was determined by multiplying the total number of non-certainty prisons to be sampled, 217, by the proportion of male prisoners in the stratum among the total number of male prisoners across all strata. Within each stratum, facilities were ordered by size and selected with probability proportional to size. Of the selected 231 prisons for men (217 non-certainty prisons + 14 certainty prisons), six prisons were not included because they resulted in “non-interviews or were out of scope,” resulting in a total of 225 prisons. The total number of prisons included in the analysis was ostensibly based on the projected number of participants needed to estimate proportions and differences with adequate precision, but an explicit discussion was not provided in the documentation accompanying the data18 nor is it addressed in other studies that have utilized these survey data.4,19
In the second stage, prisoners were randomly selected for interview from a daily census of the population for each prison. Of the selected prisoners eligible for inclusion, 88.3% (11,569/13,098) of the men were successfully interviewed.18
Sample weights
A basic sample weight was estimated for each prisoner based on his inverse probability of selection. A final weight was estimated after applying a series of adjustment factors to the basic weight to account for 1) discrepancies between the actual and projected number of prisoners in a facility, 2) prisoner non-participation, and 3) the final counts of prisoners in each geographic stratum as of Dec. 31, 2003.18
Study measures
Our outcome measures included health assessment at admission, current medical conditions, and use of medical care for existing health problems. In addition to Race, study variables were chosen from the available data using as a guide the Aday version of Anderson’s Model of Behavioral Health Services Use.27,28 Variables corresponding to the Population Characteristics domains of the model included age, high school graduation, pre-arrest employment status, homelessness, marriage status, whether the respondent was a parent, and veteran status. Other constructs in the model such as health beliefs, consumer satisfaction, purpose of care, and health care need could not be addressed with the available data, although our analysis is based on the conceptual assumption that all prisoners with an existing health condition had a need to see a provider for that condition. We represented the model’s health care system domain using a measure of prison system health resources. Below we describe the coding for the variables used to define our study outcomes (health assessment at admission, health condition, and health care use), our main exposure (race), and our measure of health system resources.
Health assessments during prison admission
Respondents were asked about the health assessments conducted during their admission to prison. Survey items queried if prisoners were: 1) checked for illness, injury, or intoxication; 2) questioned about suicidal thoughts or past attempts; and 3) questioned about their health or medical history. Additionally, respondents were asked if, in their time “since admission,” they had received a 4) medical examination, 5) an HIV test, and 6) a tuberculosis (TB) test. Because medical exams and screening tests for HIV and TB typically occur within the first two weeks of incarceration, we considered them to be part of the prisoners’ initial medical assessment. In addition to these questions, respondents were asked if they were taking prescription medications at the time of their admission.
Health conditions and health care use
We included for analysis the following 16 health conditions: tuberculosis, human immunodeficiency virus (HIV), a sexually transmitted disease (STD) other than HIV, hypertension, diabetes, heart problems, cerebral vascular accident (CVA)/brain injury, kidney problems, asthma, arthritis, hepatitis, cirrhosis, cancer, illness such as a cold, virus, or the flu, (which we refer to as a flu-like illness), accidental injury, and fight-related injury.
For 11 of these 16 conditions, the health condition and use of health care were assessed with a series of three items. Here we provide a generic version of the items: “Have you ever had [condition]?”; “Do you still have [condition]?”; and “Have you seen a doctor, nurse, or other health care person for this since your admission?” For each condition of interest, prisoners responding affirmatively to the second item were coded for the condition; prisoners responding affirmatively to the third item were coded as using health care; those responding negatively were coded as not receiving health care. Accidental and fight-related injuries and flu-like illness were each assessed with only two items, which were specific to occurrences since admission and subsequent health care. Prisoners were coded as TB-positive if they received a positive result on a TB test since admission; they were coded as having used medical care if they reported receiving anti-TB medications. Prisoners were coded as HIV-positive if they reported ever receiving a positive result on an HIV test. Unfortunately, neither health care use for HIV nor receipt of HIV medications was queried in the survey.
Race
Race was coded using an existing survey variable that combined prisoners’ responses to questions about ethnicity and race. We limited our analyses to White non-Hispanics and Black non-Hispanics, whom we refer to as Whites and Blacks.
Availability of health services for each state prison system
Data describing the availability of health services in each respondent’s prison were desirable for analysis, but these data were not collected with the survey. However, one measure of health services, the average expenditure on medical care per inmate for each state prison system, was available for the year 2001.29 We used these values to determine the upper and lower bounds for each of five medical expenditure quintiles, and coded each of the 50 U.S. state prison systems based on the quintile corresponding to its medical expenditure. Although the state prison system in which each respondent was housed at the time of survey was not available, we created a proxy for this variable based on prisoners’ state of arrest. Our preliminary analysis demonstrated that more than 85% of prisoners were arrested in their home states. Since less than 1% of all state prisoners are housed in prison systems outside their state of conviction,30 we used state of arrest as a proxy for respondents’ state prison system. Respondents were then assigned a medical expenditure quintile based on their (proxy) state prison system.
Analysis
To adjust for the correlation induced by the complex sampling design, all point estimates and their corresponding 95% confidence intervals (95% CIs) were estimated after applying the jackknife weighting using the replicate weights included in the dataset.
We first estimated the proportions of Black and White prisoners across a wide range of characteristics to describe the surveyed populations and the prison systems in which they were incarcerated. Then, as both a measure of health care use and as a method to determine if disease prevalence was biased by disease detection, we estimated race-stratified proportions of prisoners who reported not receiving each of six health assessments or tests traditionally provided at intake. We also assessed the race-stratified proportion of respondents reporting use of prescription medications at the time of admission.
Next, for each of the 16 medical conditions of interest, we estimated the race-stratified proportions of prisoners with each health condition of interest. We then estimated the median number of conditions per inmate across each race and the race-stratified proportion of prisoners with any medical condition. In preliminary analyses, we noted that approximately 60% of participants reported flu-like illness (which includes “colds”), a proportion about three times as great as that of the next most prevalent condition. In response, we excluded flu-like illness from all subsequent analyses in which conditions were aggregated together (i.e., when we examined prevalence of “any condition”) so that this one common set of conditions, which included colds, would not unduly influence our overall results.
We constructed binomial log-linear regression models to estimate the relative risk (RR) and 95% CIs, comparing the prevalence of disease among Whites to the prevalence among Blacks (referent). A model was created for “any condition” which aggregated together all of the health conditions except for flu-like illness, and then models were created for each of the 16 health conditions of interest. We adjusted our estimates by age to enhance the comparability. Most conditions were adjusted by age using a three-level age variable (16–24, 25–44, and 45+ years), but among Blacks and Whites there were fewer than five cases of HIV, cancer, and cirrhosis in the youngest age groups, so model-based estimates for these conditions were limited to prisoners in the older two groups.
Among prisoners reporting any medical condition, we estimated the proportion reporting having been seen by a health care provider, which we call use of health care. We then repeated this estimation for each of the 15 conditions for which we had data (data were not collected for HIV). For example, among prisoners who reported currently having hypertension, we estimated the proportion who reported using health care services for hypertension during their incarceration.
We then constructed a binomial log-linear regression model to assess the effect of confounders on the relationship between prisoner race and health care use, among prisoners reporting any medical condition, again excluding flu-like illness. In constructing our model, we proceeded in a step-wise fashion, estimating the effect of race after including a single potential confounder in the model. All potential confounders resulting in a 10% or greater change from the unadjusted point estimate for race were to be retained in our final multivariable model.31 Potential confounders included age, employment status at arrest, homelessness, veteran status, marriage status, fatherhood status, educational achievement, and state prison system medical expenditures. However, using our a priori criteria of a 10% or greater change, none of the potential confounders were retained in the model.
Therefore, for each individual condition, we report the unadjusted point estimate (i.e., RR) for race because it provides an efficient means to compare the proportions of Whites and Blacks who used health care, among those reporting a health condition.
All analyses were conducted using STATA 10.0.32
Results
The sample included 8,795 White and Black male respondents representing a total of 862,978 state prisoners (Table 1). A little over half of prisoners were Black (54%) and about two-thirds (63%) were between the ages of 25 and 44 years, with the median age of Blacks two years younger than that of Whites (34 years vs. 36 years). The proportion of Black prisoners who had not graduated from high school or earned a GED was almost twice that of Whites (41% vs. 23%, p<.05). More than two-thirds of prisoners were employed or had a job prior to their arrest. Fifteen percent of respondents were married and 43% had at least one child. Whites were more likely than Blacks to have been homeless (9.2% vs. 6.8%, p<.05) and twice as likely to have been a veteran (17.2% vs. 8.6%, p<.05).
Table 1.
CHARACTERISTICS OF WHITE AND BLACK MALE STATE PRISONERS, 2004
| White n=393,950a |
Black n=469,029a |
|||
|---|---|---|---|---|
| % | (95% Ci) | % | (95% Ci) | |
| Age (years) | ||||
| 16–24 | 14.2 | (12.5, 16.1) | 18.1 | (16.1, 20.4) |
| 25–44 | 61.6 | (59.8, 63.5) | 64.6 | (62.5, 66.7) |
| 45+ | 24.2 | (22.3, 26.1) | 17.2 | (15.9, 18.7) |
| Region | ||||
| Northeast | 10.5 | (8.8, 12.4) | 15.5 | (13.9, 17.2) |
| Midwest | 25.5 | (22.9, 28.2) | 22.1 | (19.8, 24.7) |
| South | 38.7 | (35.9, 41.6) | 50.7 | (48.1, 53.4) |
| West | 24.5 | (22.6, 26.5) | 10.5 | (9.4, 11.8) |
| Missing | 0.8 | (0.5, 1.3) | 1.1 | (0.7, 1.8) |
| Less than HS education and no GED | 22.8 | (21.2, 24.4) | 41.4 | (39.6, 43.2) |
| Employed at time of arrest | 75.7 | (74.2, 77.1) | 65.8 | (64.3, 67.4) |
| Homeless ever | 9.2 | (8.4, 10.2) | 6.8 | (6.1, 7.7) |
| Married at time of arrest | 15.8 | (14.6, 17.0) | 13.8 | (12.8, 14.9) |
| Children (any) | 39.2 | (37.7, 40.8) | 45.8 | (44.3, 47.3) |
| Veteran | 17.2 | (15.8, 18.7) | 8.6 | (7.8, 9.5) |
| Medical Expenditure per Prisonerb | ||||
| Quintile (Q) 1 (lowest) | 20.4 | (15.8, 25.9) | 23.2 | (18.1, 29.3) |
| Quintile (Q) 2 | 21.6 | (17.2, 26.8) | 17.3 | (14.2, 20.9) |
| Quintile (Q) 3 | 15.4 | (11.3, 20.7) | 16.0 | (12.2, 20.6) |
| Quintile (Q) 4 | 9.0 | (6.8, 11.8) | 11.6 | (9.2, 14.5) |
| Quintile (Q) 5 (highest) | 19.7 | (16.7, 23.1) | 15.6 | (13.3, 18.2) |
| Missing | 13.9 | (9.9, 19.1) | 16.4 | (11.8, 22.2) |
weighted population
$1,705 (Q1)
$1,706–2,062 (Q2)
$2,603–3,260 (Q3)
$3,261–3,620 (Q4)
>$3,620 (Q5)
HS = High School
GED = Graduate Equivalency Degree
Q = Quintile
The proportion of male prisoners in prison systems from each medical expenditure quintile ranged from about 9% (Q4) to 23% (Q1), but there were no statistically significant differences in expenditure quintile by race.
Health assessments conducted at admission
Whites were less likely than Blacks to report being checked for illness, injury, or intoxication (71.7% vs. 74.1%). Although the absolute difference in proportions was less than three percentiles, the relative difference of not being checked was statistically significant (RR: 1.09, 95% CI: 1.01, 1.18). There was no statistically significant difference between Whites and Blacks for assessments of suicidality or medical history. About 84% of both Whites and Blacks reported receiving a medical exam, and about 94% of both Whites and Blacks reported receipt of a TB test, with no statistical differences by race for either. Whites were more likely than Blacks to report that they did not receive an HIV test (RR: 1.12, 95% CI: 1.04, 1.21). A greater proportion of White than Black men (26.2% vs. 18.2%, p<.05) reported taking prescription medications at admission, even after adjusting for age (RR: 1.37, 95% CI: 1.27, 1.49).
Medical conditions
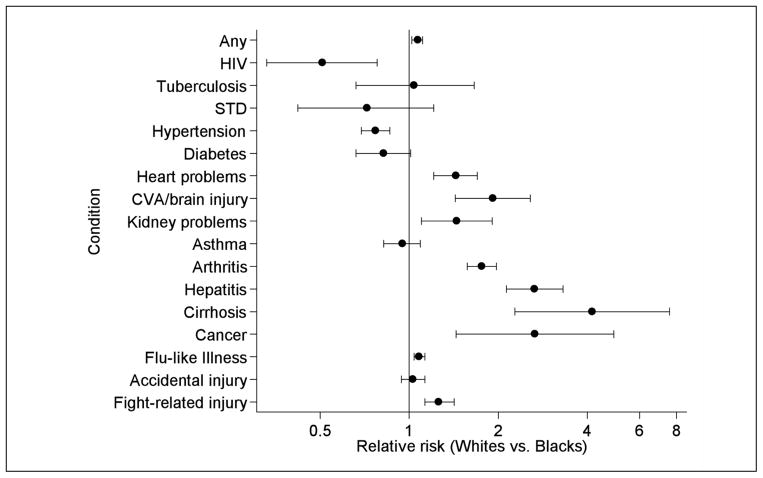
Eighty-two percent of Whites and 77% of Blacks reported having at least one of the 16 medical conditions of interest; excluding the most commonly reported condition, flu-like illnesses, the prevalence of “any condition” was 62% among Whites and 56% among Blacks. After adjusting for age, Whites were 7% more likely to report a condition than Blacks (RR: 1.07, 95% CI: 1.02, 1.11) (Figure 1). The mean number of conditions was lower among Black men than among White men (1.2 vs. 1.4, p<.05). Of the 16 conditions, the top five conditions most frequently self-reported by Black and White men included flu-like illness, accidental injury, fight-related injury, arthritis and hypertension (Table 2). For nine conditions, the age-adjusted prevalence among Whites was greater than that of Blacks (p<.05). These conditions were heart problems, CVA/brain injury, kidney problems, arthritis, hepatitis, cirrhosis, cancer, flu-like illness, and fight-related injury (Figure 1). For two conditions, HIV and hypertension, the prevalence was greater among Blacks than Whites (p< .05).
Figure 1.
Age-adjusted associations between race and selected health conditions among a nationally representative sample of male state prisoners in 2004. Blacks are the referent. Black circles represent point estimates; bars and caps represent 95% CIs. Estimates are plotted on the x-axis using log scaling. “Any” does not include flu-like illness.
HIV = Human Immunodeficiency Virus
STD = Sexually Transmitted Disease
CVA = Cerebral Vascular Accident
CIs = Confidence Intervals
Table 2.
SCREENING, EXAMS, HEALTH CONDITIONS, AND USE OF HEALTHCARE AMONG WHITE AND BLACK MALE STATE PRISONERS, 2004
| Yes/Prevalence
|
Seen by healthcare provider
|
|||
|---|---|---|---|---|
| White N=393,950* % (95% Ci) |
Black N=469,029a % (95% Ci) |
White % (95% Ci) |
Black % (95% Ci) |
|
| Screening assessment | ||||
| Illness, injury, intoxication | 71.7 (69.9, 73.5) | 74.1 (72.3, 75.8) | — | — |
| Suicide risk | 86.4 (85.1, 87.7) | 84.8 (83.1, 86.3) | — | — |
| Medical history | 86.3 (85.0, 87.4) | 87.5 (86.2, 88.8) | — | — |
| Medical exam and tests | ||||
| Medical exam | 84.8 (82.8, 86.5) | 83.7 (81.8, 85.5) | — | — |
| Tuberculosis test | 94.6 (93.5, 95.5) | 94.0 (93.1, 94.7) | — | — |
| HIV test | 64.8 (62.4, 67.2) | 68.7 (66.4, 70.9) | — | — |
| Condition | ||||
| Tuberculosis | 6.5 (5.7, 7.4) | 8.1 (7.1, 9.1) | 83.2 (77.7, 87.6) | 87.3 (83.2, 90.5) |
| HIVb | 0.8 (0.6, 1.2) | 1.6 (1.2, 2.1) | — | — |
| STD | 0.6 (0.4, 0.8) | 0.8 (0.6, 1.1) | 79.0 (56.0, 91.7) | 68.9 (51.7, 82.1) |
| Hypertension | 13.3 (12.0, 14.7) | 15.5 (14.3, 16.7) | 86.8 (82.9, 89.9) | 92.9 (90.7, 94.5) |
| Diabetes | 3.8 (3.2, 4.5) | 3.9 (3.4, 4.5) | 95.0 (89.4, 97.7) | 94.1 (88.8, 97.0) |
| Heart problems | 7.7 (6.7, 8.8) | 4.9 (4.3, 5.5) | 80.2 (75.0, 84.6) | 72.8 (66.2, 78.5) |
| CVA/brain injury | 3.5 (3.0, 4.2) | 1.7 (1.4, 2.2) | 60.4 (51.9, 68.4) | 77.1 (67.3, 84.7) |
| Kidney problems | 3.7 (3.1, 4.4) | 2.3 (1.9, 2.9) | 73.3 (65.2, 80.2) | 71.9 (62.4, 79.7) |
| Asthma | 8.2 (7.3, 9.2) | 8.7 (7.9, 9.6) | 75.9 (70.6, 80.4) | 79.6 (75.6, 83.1) |
| Arthritis | 20.5 (19.0, 22.1) | 10.4 (9.3, 11.4) | 61.3 (57.5, 64.9) | 66.5 (61.9, 70.8) |
| Hepatitis | 7.4 (6.5, 8.3) | 2.4 (2.0, 3.0) | 87.4 (83.1, 90.8) | 89.4 (81.3, 94.2) |
| Cirrhosis | 1.6 (1.2, 2.0) | 0.3 (0.2, 0.5) | 87.5 (75.5, 94.1) | 100.0 — |
| Cancer | 1.3 (0.9, 1.7) | 0.4 (0.2, 0.6) | 91.8 (79.4, 97.0) | 83.3 (56.0, 95.1) |
| Flu-like illness | 63.7 (61.2, 66.1) | 58.1 (55.8, 60.4) | 51.3 (48.7, 53.8) | 58.2 (56.0, 60.5) |
| Accidental injury | 22.8 (21.0, 24.7) | 22.2 (20.5, 24.0) | 82.1 (79.4, 84.4) | 87.0 (84.6, 89.1) |
| Fight-related injury | 17.9 (16.2, 19.7) | 14.4 (13.0, 16.0) | 65.9 (62.0, 69.0) | 72.4 (68.4, 76.0) |
Weighted population
Receipt of HIV care not queried in the survey
HIV = Human Immunodeficiency Virus
CVA = Cerebral Vascular Accident
STD = Sexually Transmitted Disease
The five conditions with the largest percentile differences between White and Black men, in descending order, were arthritis (10.1 percentiles), flu-like illness, hepatitis, fight-related injury, and heart problems (2.8 percentiles).
Health care use
Among prisoners who reported a health condition, the proportion ever seen by a prison health care provider for that condition ranged between 51%, for flu-like illness reported by Whites, and 100%, for cirrhosis reported by Blacks (Table 2).
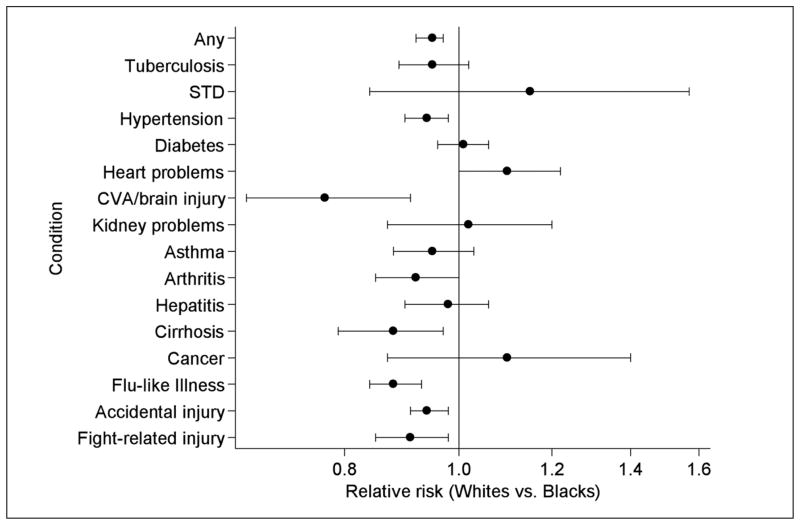
Whites were about 5% less likely than Blacks to use health care for any reported health condition (RR: 0.95, 95% CI: 0.92, 0.97). For 11 of 15 conditions (data were not collected for HIV), a smaller proportion of Whites than Blacks with the condition reported being seen by a health care provider for that condition, with the difference being statistically significant for six of these conditions: hypertension, CVA/brain injury, cirrhosis, flu-like illness, accidental injury, and fight-related injury. For five conditions, Whites were more likely than Blacks to be seen by a provider, but none of these differences were statistically significant (Figure 2). The five conditions for which inmates were least likely to use medical care for Whites and Blacks were flu-like illness, arthritis, fight-related injury, kidney problems, and CVA/brain injury (Whites only) or STDs (Blacks only).
Figure 2.
Associations between race and use of health services among a nationally-representative sample of male prisoners reporting healthcare problems in 2004. Blacks are the referent. Point estimates represented by black circles; 95% CIs represented by bars with caps. Estimates are plotted on the x-axis using log scaling. “Any” does not include flu-like illness or HIV.
STD = Sexually Transmitted Disease
CVA = Cerebral Vascular Accident
CI = Confidence Intervals
In estimating the absolute number of prisoners with an unexamined medical condition (Appendix Table 1), we found that among Whites, the top five conditions with the greatest number of unseen cases were flu-like illness (122,200 unseen cases), arthritis, fight-related injury, accidental injury, and asthma (7,800 unseen cases). Among Blacks, the top five conditions with the greatest number of unseen cases were flu-like illness (113,900 unseen cases), fight-related injury, arthritis, accidental injury, and asthma (8,300 unseen cases).
Appendix Table 1.
Male Prisoners Not Seen by a Healthcare Provider for Reported Health Conditions, 2004
| White | Black | White-Black | |
|---|---|---|---|
| Tuberculosis | 4,300 | 4,800 | −500 |
| STD | 500 | 1,200 | −700 |
| Hypertension | 6,900 | 5,200 | 1,700 |
| Diabetes | 800 | 1,100 | −300 |
| Heart problems | 6,000 | 6,300 | −300 |
| CVA/brain injury | 5,500 | 1,900 | 3,600 |
| Kidney problems | 3,900 | 3,000 | 900 |
| Asthma | 7,800 | 8,300 | −500 |
| Arthritis | 31,300 | 16,400 | 14,900 |
| Hepatitis | 3,700 | 1,200 | 2,500 |
| Cirrhosis | 800 | 0 | 800 |
| Cancer | 400 | 300 | 100 |
| Flu-like illness | 122,200 | 113,900 | 8,300 |
| Accidental injury | 16,100 | 13,500 | 2,600 |
| Fight-related injury | 24,000 | 18,600 | 5,400 |
Weighted population; estimates are rounded to nearest 100
Discussion
Despite limited resources and a morbid population, U.S. prisons have a court-affirmed mandate to provide health care to prisoners. In the context of this mandate and racial inequalities in access to care in non-incarcerated populations, we sought to determine whether use of prison health care was equitable across races.
While we observed few differences in disease screening by race, we found that Black prisoners were less likely than White prisoners to report existing health problems, but modestly more likely to have existing problems addressed by a prison health care provider. However, statistically significant differences in accessing care were detected only for six conditions. Nevertheless, these results stand in contrast to findings from the U.S. non-institutionalized population, which indicate a higher prevalence of many chronic conditions (e.g., heart disease and cancer)33 and more limited health care access and continuity among Black males than among White males.34 These results are consistent with the hypothesis that Black men may benefit from prison health care, but we caution that these findings are highly exploratory in nature. Moreover, our results do not reflect disease severity, nor do they capture any dimensions of health care quality. Future studies could improve upon our work by capturing disease-specific outcomes over time (e.g., change in glycated hemoglobin among prisoners with diabetes), and general measures of quality such as timeliness of care, physician-patient communication, patient-provider trust, and patient social support. Notably, an expert review panel recently published 79 measures of prison health care quality based on findings from the California prison system.35 Incorporation of these or similar measures into a national survey of prison facilities could provide an important step in furthering our understanding of prison health care. To investigate more fully patterns of prisoner mortality in the future, it will be necessary to obtain comparable morbidity and health care data from populations of both prisoners and non-prisoners.
Across most of the conditions examined in this study (9/16), Blacks had a lower prevalence of disease than Whites; only hypertension and HIV were more prevalent among Blacks than Whites. We found that the prevalence of cancer, heart problems, hepatitis, and cirrhosis were between about 40% and 310% greater among Whites than among Blacks. Data from the Bureau of Justice Statistics indicates that 60% of deaths among all state prisoners were from cancer, heart disease, and liver disease (which include hepatitis and cirrhosis), and for each of these conditions, crude death rates among White prisoners were at least 80% greater than among Black prisoners;36 however, these crude rates were likely confounded by different age distributions across Black and White prisoners.
While Blacks were less likely than Whites to report health problems, they were modestly more likely than Whites to report using health care for existing problems. Using the Aday and Anderson model as a framework, we were unable to identify any covariate that substantially changed the relationship between race and our overall measure of health care use; however, because of the limited availability of data, we were unable to represent all of the constructs in the model.
Conditions for which Whites were less likely to use health care included hypertension, flu-like illness, accidental injury, fight-related injury, CVA/brain injury, and cirrhosis; for these conditions, the relative difference between Whites and Blacks was generally modest in magnitude. Although we are unclear why Whites reported less use of health care for these conditions, it is possible that differences in care are explained in-part by racial differences in health care-seeking attitudes.
For example, qualitative research has found that men in prisons forgo health care for injuries as a demonstration of masculinity.37 This response to injury is posited to be more common among men who feel vulnerable and threatened in prison settings. Our data showed that a greater proportion of Whites than Blacks reported sustaining fight-related injuries. If this is accurate, it is possible that Whites feel more vulnerable in prison, which may discourage them from seeking health care even when medical intervention is warranted. Future studies should explore how strategies for constructing masculinity in prison settings potentiate differences in health care seeking between White and Black males.
In contrast to Whites, it is probable that Black male prisoners experience an improvement in health care use upon entry into prison. Indeed, data suggest that non-institutionalized African American men are 75% less likely than non-institutionalized White males to be insured and are less likely to have a usual source of care or physician.33 Data describing use of health care prior to prisoners’ incarcerations were not collected for our study population, but compared with Whites, Blacks had lower rates of both pre-arrest employment and prescription medication use—both of which may be indicators of impeded access to and use of health care prior to incarceration.
In addition to prisoner’s attitudes and expectations, health care use is likely affected by systemic barriers to care. For example co-payments are sometimes required for sick-call visits, which are non-emergent, prisoner-initiated health care visits. As in community settings, co-payments in prison are used to help offset the cost of care and to create disincentives for the overuse of health care services. In one study, use of co-payments diminished the use of sick-call visits among male prisoners by 35%.38 We are unaware of any recent studies that have assessed use of co-payments across state prison systems, but a 1996 survey found that co-payments were implemented or approved in 29 states, and introduction of legislation for prison co-payment was pending in an additional nine states. In states requiring a co-payment, fees ranged between two and five dollars.39 Even though fees are relatively modest, they may heavily tax prisoners’ small resources, causing concern that co-payments unduly diminish prisoners’ use of care.40 We note that of all conditions, the condition most likely to require a sick-call (flu-like illness) was least likely to result in care.
Other systemic barriers to care unique to correctional settings include the tension between providing care and adequate security, less than complete privacy and confidentiality, and limited medical personnel and resources. Medical expenditure is a useful albeit imperfect surrogate for health care resources. The wide range of per prisoner medical expenditures documented across state prison systems in 2001—from a minimum of $860 in Louisiana to a maximum of $5,601 in Maine29—suggests that medical resources vary greatly by state system. On the other hand, a portion of the variation can likely be attributed to geographic differences in cost rather than a strict representation of resource allocation. Our data were limited in fully addressing these possible systemic barriers to care, and our analyses incorporating medical expenditures found no association between costs and using health care. Nevertheless, we acknowledge that our results could have been biased if Whites were more likely than Blacks to be housed in prison systems with high levels of systemic barriers to care.
In most prison systems, basic health assessments as well as testing for tuberculosis and HIV are conducted soon after inmates enter prison.17 However, our data suggest that the elements of health assessments at intake were not universally provided; the proportion of prisoners who reported not receiving at least one element of screening ranged between about 6% and 30%. It may be that prisoners’ reports of intake health assessments were low because some prisoners did not recognize or remember being screened given the multitude of assessments administered upon prison intake or the length of time between intake and the survey interview. Nevertheless, the provision of health assessments during prison intake represents an important entryway into prison health services, and lapses in these assessments at intake undermine the potential benefits of prison health care.
We found that for most elements of the intake health assessment, there were only modest if any differences in screening across race; the element with the largest absolute difference across race was for HIV, in which 3.9 percentile fewer Whites than Blacks were tested. Unlike other elements of screening, HIV testing in 29 U.S. state prison systems was voluntary at the time of the study,41 meaning that prisoners had a choice about whether or not to be tested. However, we found no evidence that racial differences in testing rates were the result of differences in testing policies across states (data not shown). Our finding that Whites had lower HIV testing rates than Blacks is in contrast with results from other studies, which determined testing status using prison records rather than self-report.42,43 However, these studies have only been conducted in a few states.
This study had several limitations. Foremost, the study was based on prisoner self-report and not administrative or medical records. In comparison with system records, estimates based on self-report likely understate the true burden of disease. However, our prevalence estimates were generally consistent with findings from other studies, which derived estimates from medical records.25,26
Second, items assessing morbidity (e.g., heart problems, asthma) were vague and likely elicited responses representing a wide range of severity. Similarly, our basic measure of using health care, being “seen” by a health care provider, does not reflect the quality of that interaction or the frequency of visits.
Third, we did not have information detailing whether prisoners attempted unsuccessfully to initiate care, or data about systematic barriers to care, as discussed above. To address the later, we created a proxy measure for health care expenditures, but this variable alone did not capture the full range of potential barriers.
Fourth, respondents were interviewed at different times during their incarceration and data describing their time served were not available. Inmates interviewed soon after their imprisonment likely had better recall of their admission experiences than other inmates, while inmates’ opportunities to use health care services increase with their length of stay.
Finally, we did not have information on the frequency of routine medical exams across respondents’ prisons nor can we determine the extent to which these visits confounded responses about receiving medical attention. Despite these limitations, this research provides some new insights into our understanding of prisoners’ health and health care. First, we found that Black prisoners had less morbidity than White prisoners. Second, the mandate to provide health care did not eliminate racial disparities in the use of health care; however, with Black prisoners more likely than White prisoners to use care, these disparities were in the opposite direction of disparities typically observed in non-incarcerated populations. Third, prior research studies examining the burden of disease among prisoners have either been limited to a single state prison system or they failed to stratify by race, gender, or both.4,44 By stratifying our analyses by race and focusing exclusively on males, we improved upon existing prevalence estimates and uncovered previously obscured health and health care disparities among White male prisoners as compared to Black male prisoners. Fourth, while we were unable to determine whether lapses in health care were based on systematic barriers to care or individual factors, our finding that medical assessments upon admission were not universal should prompt prison systems to evaluate these programs in greater detail. Finally, our study points to numerous areas for future research. Among these areas is the need to understand better prisoners’ perceptions of heath and health care throughout their life-course. Further research is needed comparing morbidity and access to care among prisoners and non-prisoners to understand more fully the effect that prison has on morbidity and mortality.
Notes
- 1.West HC, Sabol WJ. Prisoners in 2007 (NCJ 224280) Washington, DC: U.S. Department of Justice/Bureau of Justice Statistics; 2008. Dec, [Google Scholar]
- 2.The Pew Center on the States. One in 100: behind bars in America, 2008. Washington, DC: The Pew Charitable Trust; 2008. Available at: http://www.pewcenteronthestates.org/uploadedFiles/One%20in%20100.pdf. [Google Scholar]
- 3.Mumola CJ. Substance abuse and treatment, state and federal prisoners, 1997 (NCJ 172871) Washington, DC: U.S. Department of Justice/Bureau of Justice Statistics; 1999. Jan, [Google Scholar]
- 4.Binswanger IA, Krueger PM, Steiner JF. Prevalence of chronic medical conditions among jail and prison inmates in the USA compared with the general population. J Epidemiol Community Health. 2009 Nov;63(11):912–9. doi: 10.1136/jech.2009.090662. [DOI] [PubMed] [Google Scholar]
- 5.La Vigne NG, Mamalian C, Travis J, et al. A portrait of prisoner reentry in Illinois. Washington, DC: The Urban Institute; 2003. Available at: http://www.urban.org/uploadedpdf/410662oILPortraitReentry.pdf. [Google Scholar]
- 6.La Vigne NG, Kachnowski V, Travis J, et al. A portrait of prisoner reentry in Maryland. Washington, DC: The Urban Institute; 2003. Available at: http://www.urban.org/uploadedpdf/410655oMDPortraitReentry.pdf. [Google Scholar]
- 7.Conklin TJ, Lincoln T, Tuthill RW. Self-reported health and prior health behaviors of newly admitted correctional inmates. Am J Public Health. 2000 Dec;90(12):1939–41. doi: 10.2105/ajph.90.12.1939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.National Commission on Correctional Health Care. The health status of soon-to-be-released inmates: a report to Congress. Vol. 1. Chicago, IL: National Commission on Correctional Health Care; 2002. Mar, Available at: https://www.ncjrs.gov/pdffiles1/nij/grants/189735.pdf. [Google Scholar]
- 9.Maruschak LM, Beavers R. HIV in prisons, 2007–08 (NCJ 228307) Washington, DC: U.S. Department of Justice/Bureau of Justice Statistics; 2009. Dec, [Google Scholar]
- 10.Maruschak LM. Medical problems of prisoners (NCJ 221740) Washington, DC: U.S. Department of Justice/Bureau of Justice Statistics; 2008. Jul, [Google Scholar]
- 11.Baillargeon J, Wu H, Kelley MJ, et al. Hepatitis C seroprevalence among newly incarcerated inmates in the Texas correctional system. Public Health. 2003 Jan;117(1):43–8. doi: 10.1016/s0033-3506(02)00009-4. [DOI] [PubMed] [Google Scholar]
- 12.Mitka M. Aging prisoners stressing health care system. JAMA. 2004 Jul;292(4):423–4. doi: 10.1001/jama.292.4.423. [DOI] [PubMed] [Google Scholar]
- 13.Posner MJ. The Estelle medical professional judgement standard: the right of those in state custody to receive high-cost medical treatments. Am J Law Med. 1992;18(4):347–68. [PubMed] [Google Scholar]
- 14.Møller L, Stöver H, Jürgens R, et al., editors. Health in prisons: a WHO guide to the essentials in prison health. Copenhagen, Denmark: World Health Organization, Europe; 2007. Available at: http://www.who.int/hiv/topics/idu/prisons/e90174.pdf. [Google Scholar]
- 15.Commission on Accreditation for Corrections. Performance-based standards for correctional health care for adult correctional institutions. Alexandria, VA: American Correctional Association; 2002. [Google Scholar]
- 16.National Commission on Correctional Health Care. Standards for health services in prisons. 4. Chicago, IL: National Commission on Correctional Health Care; 1997. [Google Scholar]
- 17.Anno BJ. Prison health services: an overview. J Correct Health Care. 2004 Apr;10(3):287–301. [Google Scholar]
- 18.U.S. Department of Justice/Bureau of Justice Statistics. Survey of inmates in state correctional facilities, 2004. Washington, DC: U.S. Department of Justice/Bureau of Justice Statistics; 2004. Available at: http://www.icpsr.umich.edu/icpsrweb/ICPSR/studies/4572?archive=ICPSR&q=ICPSR+4572. [Google Scholar]
- 19.Wilper AP, Woolhandler S, Boyd JW, et al. The health and health care of U.S. prisoners: results of a nationwide survey. Am J Public Health. 2009 Apr;99(4):666–72. doi: 10.2105/AJPH.2008.144279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Patterson EJ. Incarcerating death: mortality in U.S. state correctional facilities, 1985–1998. Demography. 2010 Aug;47(3):587–607. doi: 10.1353/dem.0.0123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rosen DL, Wohl DA, Schoenbach VJ. All-cause and cause-specific mortality among Black and White North Carolina state prisoners, 1995–2005. Ann Epidemiol. 2011 Oct;21(10):719–26. doi: 10.1016/j.annepidem.2011.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Spaulding AC, Seals RM, McCallum VA, et al. Prisoner survival inside and outside of the institution: implications for health-care planning. Am J Epidemiol. 2011 Mar;173(5):479–87. doi: 10.1093/aje/kwq422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Centers for Disease Control and Prevention/National Center for Health Statistics. Compressed Mortality File 1999–2007. Hyattsville, MD: Centers for Disease Control and Prevention/National Center for Health Statistics; 2008. Available at: http://wonder.cdc.gov/cmf-icd10.html. [Google Scholar]
- 24.The Henry J. Kaiser Family Foundation. Race, ethnicity and health care: young African American men in the United States. Washington, DC: The Henry J. Kaiser Family Foundation; 2006. Jul, Available at: http://www.kff.org/minorityhealth/upload/7541.pdf. [Google Scholar]
- 25.Harzke AJ, Baillargeon JG, Pruitt SL, et al. Prevalence of chronic medical conditions among inmates in the Texas prison system. J Urban Health. 2010 May;87(3):486–503. doi: 10.1007/s11524-010-9448-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Baillargeon J, Black SA, Pulvino J, et al. The disease profile of Texas prison inmates. Ann Epidemiol. 2000 Feb;10(2):74–80. doi: 10.1016/s1047-2797(99)00033-2. [DOI] [PubMed] [Google Scholar]
- 27.Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav. 1995 Mar;36(1):1–10. [PubMed] [Google Scholar]
- 28.Aday LA, Andersen R. A framework for the study of access to medical care. Health Serv Res. 1974 Fall;9(3):208–20. [PMC free article] [PubMed] [Google Scholar]
- 29.Stephan JJ. State prison expenditures, 2001 (NCJ 202949) Washington, DC: U.S. Department of Justice/Bureau of Justice Statistics; 2004. Jun, [Google Scholar]
- 30.U.S. Department of Justice/Bureau of Justice Statistics. Prison and jail inmates at midyear 2001 (NCJ 191702) Washington, DC: U.S. Department of Justice/Bureau of Justice Statistics; 2002. Apr, [Google Scholar]
- 31.Mickey RM, Greenland S. The impact of confounder selection criteria on effect estimation. Am J Epidemiol. 1989 Jan;129(1):125–37. doi: 10.1093/oxfordjournals.aje.a115101. [DOI] [PubMed] [Google Scholar]
- 32.StataCorp. Stata statistical software: release 10. College Station, TX: StataCorp LP; 2009. [Google Scholar]
- 33.Rosamond W, Flegal K, Furie K, et al. Heart disease and stroke statistics—2008 update: a report from the American Heart Association statistics committee and stroke statistics subcommittee. Circulation. 2008 Jan;117(4):e25–146. doi: 10.1161/CIRCULATIONAHA.107.187998. [DOI] [PubMed] [Google Scholar]
- 34.Agency for Health Care Research and Quality. Quality tool: national health care disparities report, 2004. Rockville, MD: Agency for Health Care Research and Quality; 2008. [Google Scholar]
- 35.Asch SM, Damberg CD, Hiatt L, et al. Selecting performance indicators for prison health care. J Correct Health Care. 2011 Apr;17(2):138–49. doi: 10.1177/1078345810397712. [DOI] [PubMed] [Google Scholar]
- 36.Mumola CJ. Medical causes of death in state prisons, 2001–2004 (NCJ 216340) Washington, DC: U.S. Department of Justice/Bureau of Justice Statistics; 2007. Jan, [Google Scholar]
- 37.Sabo D, Kupers T, London W, editors. Prison masculinities. Philadelphia, PA: Temple University Press; 2001. [Google Scholar]
- 38.Hyde R, Brumfield B. Effect of co-payment on the use of medical services by male and female prisoners. J Correct Health Care. 2003 Jan;9(4):371–80. [Google Scholar]
- 39.Gipson FT, Pierce EA. Current trends in state inmate user fee programs for health services. J Correct Health Care. 1996 Oct;3(2):159–78. [Google Scholar]
- 40.Harrison BP. In the matter of correctional facilities charging prisoners for health services. J Correct Health Care. 1996 Oct;3(2):109–27. [Google Scholar]
- 41.Maruschak LM. HIV in prisons, 2004 (NCJ 213897) Washington, DC: U.S. Department of Justice/Bureau of Justice Statistics; 2006. Nov, [Google Scholar]
- 42.Behrendt C, Kendig N, Dambita C, et al. Voluntary testing for human immunodeficiency virus (HIV) in a prison population with a high prevalence of HIV. Am J Epidemiol. 1994 May;139(9):918–26. doi: 10.1093/oxfordjournals.aje.a117098. [DOI] [PubMed] [Google Scholar]
- 43.Rosen DL, Schoenbach VJ, Wohl DA, et al. An evaluation of HIV testing among inmates in the North Carolina prison system. Am J Public Health. 2009 Oct;99( Suppl 2):S452–9. doi: 10.2105/AJPH.2007.133124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Williams BA, McGuire J, Lindsay RG, et al. Coming home: health status and homelessness risk of older pre-release prisoners. J Gen Intern Med. 2010 Oct;25(10):1038–44. doi: 10.1007/s11606-010-1416-8. [DOI] [PMC free article] [PubMed] [Google Scholar]