Abstract
An epidemiologic (cross-sectional study) survey on 462 inhabitants in Corail, Haiti showed that 16.5% were infected with Mansonella ozzardi. This finding was determined from a single 20-μL sample of finger prick blood from each person. Among children, < 2% had a detectable microfilaremia. In persons > 15 years of age, the prevalence of infection for males and females was 23% and 21%, respectively. In general, the microfilaremias were low and 70% of positive persons had < 10 microfilariae per 20 μL of blood; only 5% had > 50 microfilariae. This study shows that persons living near mangrove marshes that are breeding sites for Culicoides furens and C. barbosai biting midges, which are recognized vectors of M. ozzardi in Haiti, are consequently more frequently infected than those living in downtown area of Corail or inland.
Mansonella ozzardi, which is found strictly in the Western Hemisphere, is present in the subtropical, tropical, and temperate regions of Central and South America, and in the Caribbean. Adults live in the subcutaneous tissue, and juvenile stages require development in a dipteran host, namely biting midges of the genus Culicoides or black flies of the genus Simulium.
In Haiti, M. ozzardi is found in limited coastal foci.1 Epidemiologic surveys conducted in the 1970s in Bayeux in northern Haiti reported that 16% of inhabitants had M. ozzardi microfilariae in peripheral blood.2 In this area, Culicoides furens serves as an efficient intermediate host.3 Experimental studies showed that the biting midge Leptoconops bequaerti is also capable of supporting the complete development of M. ozzardi but only on a very limited scale.4 Studies in the southern peninsula of Haiti in the 1980s showed that another biting midge, C. barbosai, a species breeding exclusively in the mangrove marshes, may also support the development of M. ozzardi to the infective stage.5 More than thirty years after these first studies on this neglected tropical disease, this report presents the results of an epidemiologic survey performed in Corail, Haiti.
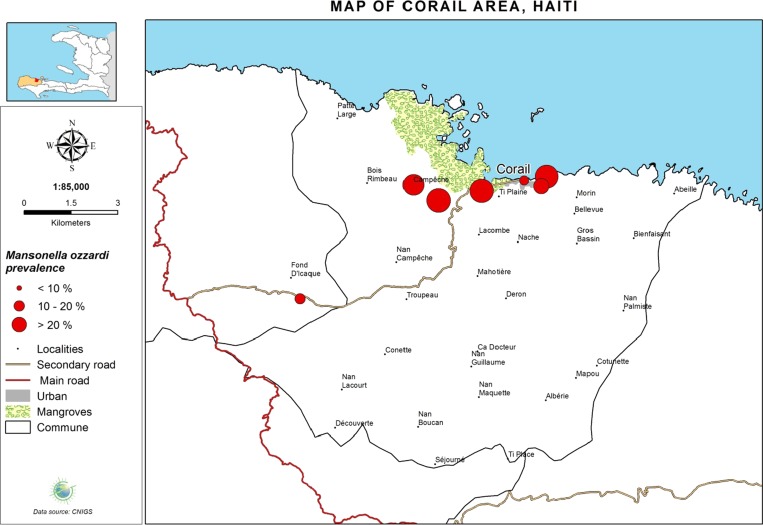
The commune of Corail is located on the northern coastal area of the Grande Anse region between the communes of Roseaux, and Pestel (Figure 1). This commune, which has an area of 108 km2, consists of three municipal sections: Champy, Fond d'Icaque, and Duquillon. The main city in this district is also named Corail. The total estimated population in 2009 was 17,793 inhabitants. This population is engaged in fishing, agriculture, coffee and charcoal production, and production of small livestock. This area is mountainous and isolated because of poor access by roads. Corail is located near a bay colonized by mangrove marshes. An epidemiologic study was performed in June–July 2013 in Corail and its surroundings, Campêche (coastal marshes), and Fond d'Icaque (inland location, altitude = 164 meters above sea level) to characterize the endemic profile of M. ozzardi in these areas.
Figure 1.
Surveyed localities in the commune of Corail, Grande Anse, Haiti, with prevalence rates for microfilariae of Mansonella ozzardi.
Blood films were collected as part of ongoing epidemiologic surveillance by the National Laboratory of Public Health. After the objectives of the study were explained to the community in each location, a sample of volunteers for testing for M. ozzardi microfilaremia was selected on the basis of consent of each participant. A written informed consent was signed by each participant, and a parent or guardian had to provide consent for children. A thick blood smear (20 μL of blood obtained by finger prick) was prepared for each patient, dehemoglobinized and stained with Giemsa.
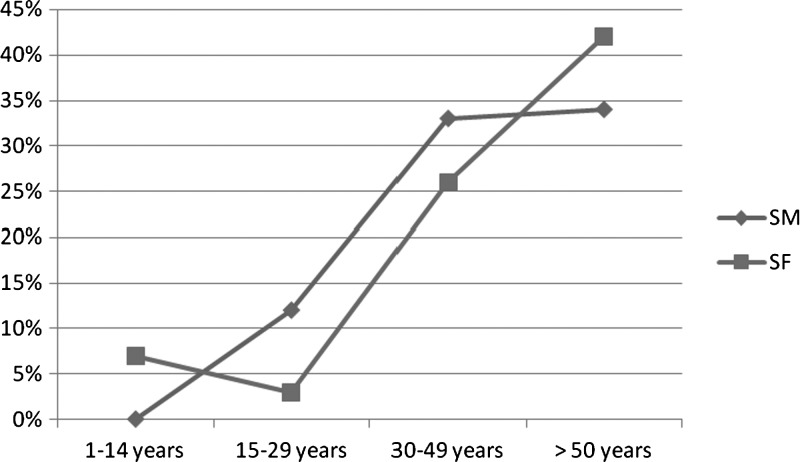
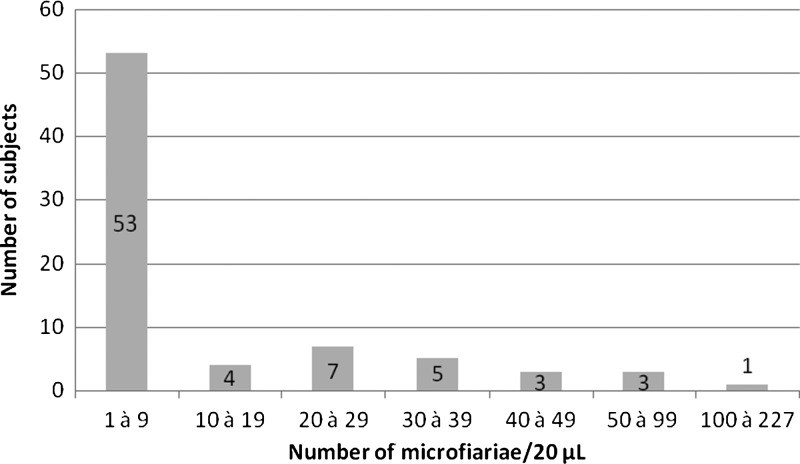
A total of 462 inhabitants were included in the survey and 76 (16.5%) had microfilariae of M. ozzardi in peripheral blood (Table 1). The distribution of microfilariemia by sex and age of participants is shown in Figure 2. Microfilariae were rarely found in children < 15 years of age. Microfilaremia was higher in adults: 23% of men and 21% of women. In 70% of persons tested, the density of microfilariae was < 10 per 20 μL of blood (Figure 3). Two men 42 and 85 years of age and one woman 70 years of age old had 79, 97, and 227 microfilariae/20 μL of blood, respectively.
Table 1.
Prevalence of Mansonella ozzardi microfilariae and density average in surveyed sites of the commune of Corail, Grande Anse, Haiti
| Municipal town/section | No. persons | No. positive persons | Prevalence rate (%) | Average microfilaria/20 μL of blood |
|---|---|---|---|---|
| Corail | ||||
| Cité Balaou | 50 | 2 | 4 | 2.5 |
| Cité Bédard | 56 | 6 | 11 | 9.2 |
| Fond Févry | 75 | 19 | 25 | 8.3 |
| Vinfor | 50 | 13 | 36 | 39.5 |
| Champy | ||||
| Campeche | 101 | 21 | 20 | 12.9 |
| La Combe | 41 | 11 | 27 | 15.5 |
| Fond d'Icaque | 89 | 4 | 5 | 1.5 |
Figure 2.
Distribution by sex and age of the holders of microfilariae Mansonella ozzardi in the population of the commune of Corail, Grande Anse, Haiti. SM = males; SF = females.
Figure 3.
Density distribution of microfilariae of Mansonella ozzardi among 76 persons infected in the commune of Corail, Grande Anse, Haiti.
The epidemiologic characteristics of mansonelliasis in this focus are similar to those observed 35 years ago in Bayeux in northern Haiti2: scarcity of infection in childhood, but a rapid increase in the rate of infection in persons > 20 years of age, which included 34% of the men and 41% of the women ≥ 50 years of age. The prevalence rate was similar in the two foci (16% and 16.5%, respectively, in Bayeux and Corail).
As previously observed in the area of Bayeux, the prevalence rate in the commune of Corail was significantly higher in the areas located near mangroves marshes, such as Vinfort (26%) and Fond Févry (25%), and near swampy areas, such as La Combe (27%) and Campêche (20%). In these areas, the average density of microfilaria in blood of infected inhabitants was high and reached 39.5 microfilariae/20 μL of blood in Vinfort where houses are built on the edge of mangrove marshes. These biotopes are favorable for development of sand flies in Haiti.6,7 Conversely, in downtown (Cité Balaou) and inland (Fond d'Icaque) areas, the prevalence was low (4% and 5%, respectively) and there were low numbers of microfilariae in infected persons (1 or 2 per μL of blood). These results confirm the close correlation between the human type of habitat, its proximity with the breeding sites of sand flies, and the rate of infection by M. ozzardi in Haiti. This correlation explains why foci of mansonelliasis in Haiti are specifically located in coastal areas.
Although most infected patients are usually asymptomatic or have few signs and symptoms, such as fever, headache, cold legs, or joint pain, M. ozzardi microfilariae could be linked to ophthalmic pathologies. Lesions of cornea, such as nummular or punctuated keratitis, have been reported in populations in Brazil that have a high prevalence of microfilaremia.8–10 A recent study conducted in Coari on the Solimões River in Brazil reported that the prevalence of M. ozzardi was 26.4%, and a positive correlation was found between microfilaremiae and corneal lesions. In some patients with a positive blood smear, the presence of microfilariae were observed in the cornea by using confocal microscopic examination of the eye.11 Because our study reported a high prevalence in the region of Corail, we look will conduct further investigations on a potential positive correlation between microfilaremiae and corneal lesions within this community.
In conclusion, in coastal areas of Haiti where persons live near mangrove marshes, a survey of M. ozzardi infection should be conducted, particularly for adults. This parasite could be considered as a potential eye pathogen, and treatment of heavily infected patients with ivermectin is recommended.
Footnotes
Authors' addresses: Christian P. Raccurt, Laboratoire National de Santé Publique, Parasitologie, Delmas #33, Port-au-Prince, Haïti, E-mail: raccurt@yahoo.fr. Philippe Brasseur, Institut de Recherche pour le Développement, Unités Mixtes de Recherche 98, Dakar, Senegal, E-mail: philippe.brasseur@ird.fr. Micheline Cicéron and Jacques Boncy, Laboratoire National de Santé Publique, Parasitologie, Port-au-Prince, Haiti, E-mails: michecice1012@yahoo.fr and jboncy1001@yahoo.fr.
References
- 1.Ripert C, Raccurt C, Douyon PL. La filariose Mansonella ozzardi en Haïti (Grandes Antilles). Premières données épidémiologiques. Bord Med. 1977;37:689–696. [Google Scholar]
- 2.Raccurt C, Lowrie RC, Jr, McNeeley DF. Mansonella ozzardi in Haiti. I. Epidemiological survey. Am J Trop Med Hyg. 1980;29:803–808. doi: 10.4269/ajtmh.1980.29.803. [DOI] [PubMed] [Google Scholar]
- 3.Lowrie RC, Jr, Raccurt C. Mansonella ozzardi in Haiti. II. Arthropod vector studies. Am J Trop Med Hyg. 1981;30:598–603. doi: 10.4269/ajtmh.1981.30.598. [DOI] [PubMed] [Google Scholar]
- 4.Lowrie RC, Jr, Raccurt CP, Eberhard ML, Katz SP. Assessment of Leptoconops bequaerti as a potential vector of Mansonella ozzardi in Haiti. Am J Trop Med Hyg. 1983;32:1013–1015. doi: 10.4269/ajtmh.1983.32.1013. [DOI] [PubMed] [Google Scholar]
- 5.Lowrie RC, Jr, Raccurt CP. Assessment of Culicoides barbosai as a vector of Mansonella ozzardi in Haiti. Am J Trop Med Hyg. 1984;33:1275–1277. doi: 10.4269/ajtmh.1984.33.1275. [DOI] [PubMed] [Google Scholar]
- 6.Raccurt C, Rebholtz C, Kremer M. Geographical distribution and ecology of Culicoides in Haiti. Mosq News. 1977;37:287. [Google Scholar]
- 7.Raccurt C, Rebholtz C, Kremer M. Gîtes larvaires nouveaux ou atypiques et particularités biologiques de quelques Culicoides en Haïti. Ann Parasitol Hum Comp. 1979;54:258. [Google Scholar]
- 8.Branco BC, Chamon W, Belfort R. Ocular findings in Pauiní (southwest of the Brazilian Amazon) and possible corneal lesions caused by Mansonella. Arq Bras Oftalmol. 1998;61:647–682. [Google Scholar]
- 9.Garrido C, Campos M. First report of presumed parasitic keratitis in Indians from the Brazilian Amazon. Cornea. 2000;19:817–819. doi: 10.1097/00003226-200011000-00011. [DOI] [PubMed] [Google Scholar]
- 10.Cohen JM, Ribeiro JA, Martins M. Ocular manifestations in mansonelliasis. Arq Bras Oftalmol. 2008;71:167–171. doi: 10.1590/s0004-27492008000200007. [DOI] [PubMed] [Google Scholar]
- 11.Vianna LM, Martins M, Cohen MJ, Cohen JM, Belfort R. Mansonella ozzardi corneal lesions in the Amazon: a cross-sectional study. BMJ. 2012;10:1136–1141. doi: 10.1136/bmjopen-2012-001266. [DOI] [PMC free article] [PubMed] [Google Scholar]