Abstract
Thrombocytopenia is one of the most common hematologic disorders, characterized by an abnormally low number of platelets from multiple causes. The normal count of thrombocytes (platelets) is between 150,000 and 450,000 per microliter. The clinical expression of thrombocytopenia has broad variation from asymptomatic to life-threatening bleeding. Various syndromes and diseases are associated with thrombocytopenia. Thrombocytopenia is sometimes a first sign of hematologic malignancies, infectious diseases, thrombotic microangiopathies, and autoimmune disorders, and is also a common side effect of many medications. There are more than 200 diseases that include low number of platelets among their symptoms. A brief discussion of the most common etiologies and management of them is provided in this review.
Introduction
Thrombocytopenia is defined as a platelet count below the 150 × 109/L, the 2.5th lower percentile of the normal platelet count distribution [1]. Typically, platelet counts higher than 50 × 109/L do not lead to clinical problems unless platelet dysfunction coexists with the low count; rather, they are picked up on a routine complete blood count. Medical help is usually sought by a patient with platelet counts less than 30 × 109/L, suffering from spontaneous bruising and purpura or with continuous/relatively long-lasting bleeding from injuries and wounds. Clinically significant spontaneous bleeding does not usually occur until the platelet count is less than 10 × 109/L.
Another aspect of low platelet counts is the concomitant use of medications interfering with platelet function and/or coagulation in a constantly-growing population of patients with cardiovascular and thromboembolic disorders. Otherwise adequate platelet counts in this group of patients can precipitate serious bleeding, for example in patients treated with non-steroidal anti-inflammatory drugs (NSAIDs), especially aspirin, the most common inhibitor of platelet function. Aspirin inhibits platelet cyclo-oxygenase and blocks thromboxane A2 release, an important contributor to platelet aggregation [2]. The list of medications interfering with platelet function includes beta-lactam antibiotics, nitrates, beta-blockers, tricyclic antidepressants, selective serotonin reuptake inhibitors (SSRIs) and others, most of them only in vitro, having unclear clinical significance [3].
Thrombocytes are small (1-3 μm) anucleate cells produced in bone marrow, along with red and white blood cells, that adhere to damaged blood vessels and affect primary hemostasis. Normally, circulating thrombocytes are two thirds of all thrombocytes produced by the bone marrow, and one third is stored (sequestered) in the spleen.
Thrombocytopenia arises from three main causes: ineffective production of platelets by bone marrow, accelerated destruction of platelets, or platelet splenic sequestration (Table 1). Typical examples of the ineffective production of thrombocytes are found in the bone marrow failure syndromes (e.g. aplastic anemia, myelodysplastic syndrome) or processes occupying bone marrow (e.g. lymphoma, leukemia, multiple myeloma, metastases and bone marrow granulomas), whereas increased destruction is seen in conditions such as thrombotic microangiopathies, disseminated intravascular coagulation (DIC) and immune thrombocytopenia (ITP). Platelet sequestration is seen in congestive splenomegaly due to portal hypertension that may be caused by cardiac failure, hepatic vein thrombosis or vena cava thrombosis (Budd-Chiari syndrome), cirrhosis (e.g. due to chronic viral hepatitis or alcoholic liver disease) and, rarely, arteriovenous malformation of the splenic vessels. Platelet sequestration is characterized by redistribution of platelets from those circulating to the splenic pool [4].
Table 1. Classification of thrombocytopenia by mechanism.
| Decreased production | Increased destruction | Splenic sequestration |
|---|---|---|
| Aplastic anemia | DIC | Portal hypertension with splenomegaly |
| MDS | TTP | Cirrhosis with congestive splenomegaly |
| Leukemia | HIT | Gaucher disease |
| DITP | DITP | Myelofibrosis with myeloid metaplasia and splenomegaly |
| ITP | ITP | Viral infections with splenomegaly |
Typical examples are given for each mechanism. In ITP and DITP two mechanisms are involved.
Abbreviations: DIC, disseminated intravascular coagulation; DITP, drug-induced immune thrombocytopenia; HIT, heparin-induced thrombocytopenia; ITP, immune thrombocytopenia; MDS, myelodysplastic syndrome; TTP, thrombotic thrombocytopenia purpura.
Multiple mechanisms (increased destruction and decreased production) are involved in ITP, drug-induced thrombocytopenia and hepatitis C virus (HCV) and human immunodeficiency virus (HIV)-induced thrombocytopenia [5].
When evaluating a patient with thrombocytopenia, it is important to exclude pseudothrombocytopenia, a falsely low platelet count, caused by in vitro agglutination of platelets occurring in approximately 2% of patients with thrombocytopenia, when the blood is collected in ethylenediaminetetra-acetic acid (EDTA) containing tubes. If true thrombocytopenia exists, stepwise evaluation is needed. In clinical practice, physicians are frequently faced by a patient presenting with a new onset severe thrombocytopenia, the cause of which is occult. The most challenging issue is to find the cause in the shortest time and to treat the patient accordingly. Ideally, the adequate treatment should be given in respect to etiology, but in the real world, especially if a patient presents with bleeding, it is not possible to gather all the necessary information that would allow the clinician to weigh all the pros and cons of different treatments, since treatment should be given immediately. In those cases, treatment that has a rapid onset of effect and is minimally harmful is reasonable. Thus, the treatments given in emergency situations, for example platelet transfusion, usually are not long-term therapeutic options. On the other hand, platelet transfusions may not be helpful in certain etiologies, for example in ITP, heparin-induced thrombocytopenia and thrombotic thrombocytopenic purpura (TTP). Therefore, it is very important to recognize the signs and symptoms of these entities. In this review we attempt to provide an algorithm through which the cause(s) of thrombocytopenia can be assessed.
Approach to the patient with thrombocytopenia
Family history, medical history and concomitant medications
A detailed history can provide important information regarding the etiology of thrombocytopenia and facilitate diagnosis. The most important aspects that should be investigated include the following: the presence of a family history of thrombocytopenia (it is surprisingly common to diagnose congenital thrombocytopenia not only in children but even in adults – see Figure 1); disease history, paying special attention to recent viral and bacterial infections; vaccinations [6]; malignancies; possibility of pregnancy; recent travels (e.g. exposure to malaria, rickettsiosis, dengue fever); recent transfusions; ingestion of alcohol; dietary habits; and risk factors for HIV and viral hepatitis [5,7]. Particular points of interest are medications taken by the patients, especially those started 1-2 weeks prior to the development of thrombocytopenia. There are two types of drug-induced thrombocytopenia caused by different mechanisms: the first is by direct myelosuppressive effect (e.g. chemotherapy-induced thrombocytopenia) and the second by immune-mediated destruction of platelets due to an idiosyncratic drug reaction (drug-induced immune thrombocytopenia [DITP]) [7,8]. DITP may be caused by classic drug-dependent platelet antibodies (e.g. quinine), haptens (e.g. penicillin), glycoprotein IIb/IIIa receptor antagonists (e.g. tirofiban) [9], stimulation of autoantibody formation (e.g. gold) and immune complex formation (e.g. heparin) [10]. Alcohol, some herbal preparations and even certain foods and beverages can be implicated in the pathogenesis of drug-induced thrombocytopenia [7].
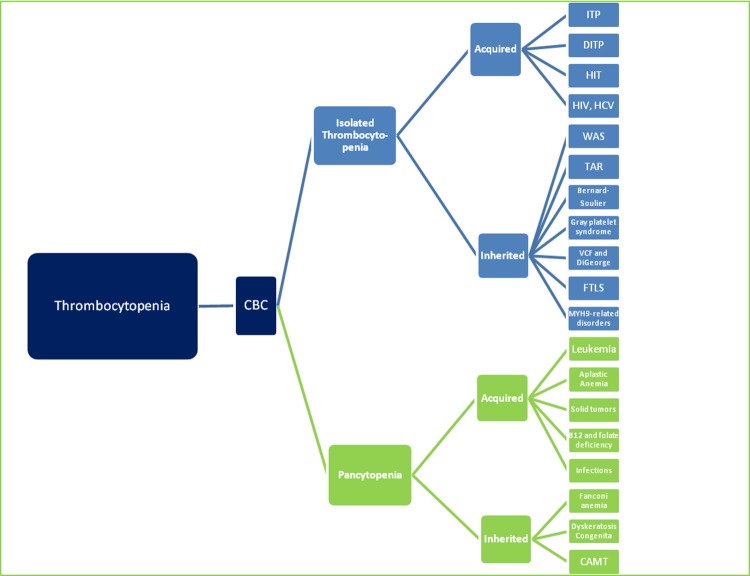
Figure 1. Thrombocytopenia: diagnostic algorithm starting with the complete blood count (CBC).
Abbreviations: CAMT, congenital amegakaryocytic thrombocytopenia; CBC, complete blood count; DITP, drug-induced immune thrombocytopenia; FTLS, familial thrombocytopenia-leukemia syndrome; HIT, heparin-induced thrombocytopenia; HIV, human immunodeficiency virus; HCV, hepatitis C virus; ITP, immune thrombocytopenia; TAR, thrombocytopenia-absent radii syndrome; VCF, velocardiofacial syndrome; WAS, Wiskott-Aldrich syndrome.
Vaccinations can also be associated with thrombocytopenia, the pathogenesis of this type of thrombocytopenia being immune-complex formation. Many types of vaccinations have been implicated in the pathogenesis of thrombocytopenia. The best studied of these is measles-mumps-rubella (MMR). There is also documentation of acute thrombocytopenia developing after vaccination against pneumococcus, Haemophilus influenzae, hepatitis B virus, and varicella-zoster virus, although the incidence is very low [6,7].
Special attention should be paid to recent exposure to heparin (and low-molecular weight heparin), as potential causes of severe, sometimes life-threatening thrombocytopenia [10]. Typically thrombocytopenia will occur between 5 and 14 days of the first heparin dose, but if heparin was given in the previous 100 days, the decrease in platelet count can sometimes occur within hours of exposure. Similar to ITP, heparin-induced thrombocytopenia (HIT) is an immune-mediated disorder, but characterized by consumption and thrombosis, the features that distinguish heparin-induced thrombocytopenia from ITP.
Physical examination
Important clues to diagnosis of thrombocytopenia can be obtained during systematic physical examination. First, general physical examination by inspection, palpation and auscultation can inform one on the general health of the patient e.g. the presence of comorbidities. Second, examination of the skeletal system can shed light on potential causes of thrombocytopenia as indicated below.
Special attention should be paid to:
Bleeding: Some patients have bleeding tendency, independently of etiology. Usually those with platelet counts less than 20 × 109/L present with petechiae, purpura and ecchymoses. Petechiae are the hallmark of platelet-related bleeding.
Lymphadenopathy: Lymphoma, acute or chronic leukemia (T-cell acute lymphoblastic leukemia, chronic lymphocytic leukemia), viral infections (Epstein-Barr Virus (EBV), cytomegalovirus (CMV), HIV, tuberculosis, sarcoidosis, autoimmune lymphoproliferative (Canale-Smith) syndrome.
Splenomegaly: Gaucher disease, portal hypertension, cirrhosis, certain types of lymphoma and leukemia (eg. CLL), myelofibrosis with extramedullar hematopoiesis, infections (e.g. malaria), EBV and CMV infections.
Hepatomegaly: chronic hepatitis, hepatosplenic lymphoma.
Skeletal abnormalities: short stature, malformations of the thumbs and forearms seen in Fanconi anemia patients, thrombocytopenia-absent radii (TAR-syndrome) characterized by bilateral shortened or absent radii, thumb abnormalities [11].
Multiple abnormalities are common in inherited syndromes: facial dysmorphology (velocardiofacial [VCF] syndrome, Jacobsen syndrome), cleft palate (DiGeorge syndrome); eyes, kidneys and urinary tract, ears (MYH9-related disorders [May-Hegglin anomaly associated with MYH9 gene]), heart, gastrointestinal system, central nervous system abnormalities, signs of hypogonadism (Fanconi anemia) [11].
Skin abnormalities: abnormal skin pigmentation in Fanconi anemia, necrotic skin lesions in HIT patients, eczema in Wiskott-Aldrich syndrome (WAS), “lacy” skin pigmentation associated with abnormal growth and shape of nails in dyskeratosis congenita.
Complete blood count (CBC)
The following issues must be taken into account:
Isolated thrombocytopenia is typically associated with immune-mediated disorders [12] (e.g. ITP, DITP) and inherited disorders (e.g. Bernard-Soulier, TAR syndrome), but is uncommon in malignant processes involving bone marrow.
Thrombocytopenia associated with anemia and leucopenia (pancytopenia) can be caused by bone marrow suppression by various medications (commonly chemotherapy, rarely antihypertensive medications and antibiotics e.g. chloramphenicol); viral infections (HIV); bacterial infections (e.g. leishmaniasis); severe folate and B12 deficiency; paroxismal nocturnal hemoglobinuria; systemic lupus erythematosus (SLE); inherited disorders (e.g. dyskeratosis congenita, Fanconi anemia); malignancy (metastatic disease, leukemia, lymphoma with bone marrow involvement, multiple myeloma, rarely solid tumors) or bone marrow failure (e.g. aplastic anemia, myelodysplastic syndrome).
If thrombocytopenia is associated with neutrophilia, infection should be considered or, rarely, chronic myeloid leukemia, usually associated with “left shift” — an increased percentage of immature neutrophils (bands, metamyelocytes and myelocytes). Thrombocytopenia can be accompanied by lymphocytosis suggestive of lymphoid malignancies (e.g. chronic lymphocytic leukemia [CLL], pertussis, or viral infections).
Blood smear
Blood smear has inestimable value in the diagnosis of thrombocytopenia. Firstly, as discussed, pseudothrombocytopenia should be excluded. Secondly, in cases of true thrombocytopenia, blood cell morphology should be investigated thoroughly. Giant platelets can be found with different types of hereditary thrombocytopenia (Paris-Trousseau thrombocytopenia, gray platelet syndrome, Bernard-Soulier) and these can result in falsely low platelet counts if the giant platelets are not counted as platelets. Microthrombocytes are typically seen in WAS or X-linked thrombocytopenia [13] and TORCH infections (toxoplasmosis, others [such as syphilis, varicella-zoster, parvovirus B19], rubella, cytomegalovirus, and herpes infections). Neutrophils with toxic granulation occur in blood smears of patients with sepsis, and Döhle-like bodies in the cytoplasm of neutrophils are seen in the MYH9-related disorders (May-Hegglin anomaly associated with MYH9 gene). Neutrophils with bilobed nuclei suggest Pelger-Huèt anomaly. Atypical lymphocytes are seen in many viral infections in children but Epstein-Barr virus is the one classically associated with type II atypical lymphocytes or Downey cells. Acute leukemia should be considered if there are blasts on blood smear; in this case special blood tests (especially bone marrow aspiration and biopsy) are the next steps of diagnostic evaluation. Red blood cell fragments (schistocytes) are common in microangiopathic hemolytic anemias (such as TTP and DIC). Appearance of dacrocytes (“teardrop” erythrocytes) and nucleated erythrocytes should lead to further bone marrow investigation, since these findings are indicative of primary myelofibrosis and myelodysplastic syndrome.
Additional investigations
Elevated blood lactate dehydrogenase (LDH) and indirect bilirubin, combined with low haptoglobin level and a positive direct antiglobulin test (direct Coombs test), are common in patients with Evans syndrome, a disorder presenting with autoimmune hemolytic anemia and thrombocytopenia (both processes may occur at the same time, or, more commonly, different times) as a consequence of anti-platelet and anti-erythrocyte antibodies. Elevated LDH combined with renal function impairment may indicate TTP or hemolytic uremic syndrome (HUS).
Blood coagulation tests disturbance: prolonged prothrombin time (PT), low fibrinogen and elevated D-dimers are typical for DIC.
Elevated liver enzymes with or without elevated bilirubin, LDH and alkaline phosphatase should lead to the investigation of hepatic disease (viral hepatitis, drug-induced or toxic hepatitis), cirrhosis, and viral infection such as cytomegalovirus (usually only liver enzymes and LDH are elevated).
Serological tests for viruses, blood cultures, anti-platelet antibodies, bone marrow biopsy and many other diagnostic tests can be performed at the discretion of the physician according to the presenting signs and course of the disease.
Treatment of thrombocytopenia
One treatment approach is to direct treatment to the etiology of thrombocytopenia (e.g. discontinuation of the drug that caused thrombocytopenia, treatment of the underlying infection, immunoglobulin G (IgG) replacement, chemotherapy directed at CLL). Unfortunately, only in a minority of cases is the etiology of thrombocytopenia clear and the cause found. In addition, in some cases “curing” the underlying medical cause of the ITP may not change the platelet count.
In a case of severe bleeding, if the etiology of thrombocytopenia is unknown, but not thought to be immunologic, platelet transfusion can be used to provide an immediate platelet increase. In contrast, if the underlying cause is immune, the effect from platelet transfusion may be minimal and at best very short-lived, and it should be reserved only for life-threatening bleeding (ideally transfused following intravenous immunoglobulin to “protect” the platelets).
If the cause of thrombocytopenia is unknown and there are no contraindications, such as infections, corticosteroids may be used to increase the platelet count. More specific treatment plans usually depend on the underlying etiology of the thrombocytopenia.
Inherited thrombocytopenia
Patients with inherited thrombocytopenia and their families should be educated about their diagnosis to avoid unnecessary investigations and especially potentially dangerous medical/surgical treatment for ITP. In the past, patients with inherited thrombocytopenia have been treated with platelet transfusions (reserved for cases of bleeding or its prevention, e.g. prior to surgery). While the fear of sensitization has dominated restriction of platelet transfusion, the availability of leukoreduction has greatly decreased this risk. Recently, one of the two thrombopoietin-receptor agonists, eltrombopag, was investigated as a possible treatment option in MYH9-related disorders (May-Hegglin anomaly associated with the MYH9 gene) thrombocytopenia, with at least some success in 12 of 15 patients [14]. Preliminary results have also been obtained in patients with WAS. Fear of induction of malignancy has restricted its use in syndromes in which there is myelodysplastic syndrome or a potential for the development of leukemia, for example congenital amegakaryocytic thrombocytopenia (CAMT), TAR, GATA-1 (globin transcription factor 1)-related X-linked thrombocytopenia, and familial leukemia-thrombocytopenia. The option of allogeneic stem cell transplantation is reserved for inherited thrombocytopenias with a high risk of marrow failure or a high risk of acute leukemia [15,16].
Immune thrombocytopenia (ITP)
According to the Medscape reference library [12], the incidence rates for ITP are as follows: in the US there are 66 adult cases and 50 childhood cases per 1,000,000 per year; in Denmark and England there are 10 to 40 cases per 1,000,000 per year; and in Kuwait there are 125 cases per 1,000,000 per year.
Many cases of ITP can be left untreated, and spontaneous remission in children is common. However, counts of under 50 × 109/L are usually monitored with regular blood tests, and those with counts of under 10-20 × 109/L are usually treated, as the risk of serious spontaneous bleeding, especially intra-cranial hemorrhage, is much higher with lower platelet counts. Any patient experiencing severe bleeding symptoms secondary to thrombocytopenia should also be treated [17,18]. According to the American Society of Hematology 2011 guidelines, treatment initiation is suggested when an adult patient is newly-diagnosed with a platelet count <30 × 109/L (grade 2C evidence) [19], but in clinical practice various factors (e.g. bleeding tendency, age, medical history and concomitant medications) need to be taken into account.
If therapy is required, the first-line treatment option is generally corticosteroids, with the recommended prednisone dose 1 mg/kg/day orally for up to 21-28 days depending upon response, followed by slow tapering. More prominent platelet responses have been reported with repeated pulses of high-dose dexamethasone 40 mg daily for 4 days [20], but no comparative data favoring dexamethasone exists.
Also, intravenous immunoglobulin or intravenous anti-D (Rho[D] immune globulin) can be used as initial treatment with or without steroids [19]. The initial intravenous immunoglobulin dose of either 0.4 g/kg/day for up to 5 days or, alternatively, a short course of high dose intravenous immunoglobulin (1 g/kg for 1-2 days) has been found to be effective [21]. Most adult patients will relapse after initial treatment (or are refractory to first-line therapy) and require second-line therapy.
The most effective second-line treatment option is splenectomy. The initial response rate is perhaps 80-85% with a 5-year response rate of 60-65%. Unfortunately, predictors of response to splenectomy are not well defined yet [22,23]. Additional second-line treatment options with documented evidence of efficacy (allowing postponement of splenectomy) include many agents: azathioprine, cyclosporine, cyclophosphamide, danazol, dexamethasone, vinca alkaloids, mycophenolate mofetil, rituximab, and thrombopoietin-receptor agonists. The pros and cons of the leading agents have been recently summarized [24].
Rituximab, the leading and original anti-CD20 monoclonal antibody (several others exist) is widely used in ITP, in various regimens and combinations with other drugs, for example with dexamethasone. The most commonly used rituximab schedule is intravenous infusion of 375 mg/m2 given once weekly for 4 weeks [25]. Patel et al. [26] recently reported 5-year outcomes of both children and adults. This study specifically selected responders to rituximab in order to assess the duration of response 5 or more years from initial treatment. The 5-year sustained response to rituximab was shown to be 26% for children and 21% for adults [26]. Two studies of one cycle of dexamethasone and rituximab demonstrated the additive if not synergistic effects of the combination, especially in the newly diagnosed and patients with persistent disease [27,28].
The use of thrombopoietin-receptor agonists is an effective and safe second-line treatment strategy. Two thrombopoietin-receptor agonists were approved for the treatment of chronic ITP in adults by the US Food and Drug Administration (FDA) in 2008 and have as of now been used extensively for treatment of chronic ITP (ITP duration ≥ 1 year) in relapsed and refractory patients [29-31]. These were romiplostim, a thrombopoietin mimetic formed from peptides (peptibody) and eltrombopag (a small molecule, non-peptide). Thrombopoietin receptor activation with these agents resulted in megakaryocyte precursor proliferation and also elevation of the platelet count in many but not all cases in a variety of different uses.
Thrombotic thrombocytopenic purpura
TTP is a medical emergency, since the mortality of untreated patients exceeds 80%. The mortality is thought to be caused by disseminated microvascular thrombosis which may provoke ischemic injury and multiple organ failure. Ischemic organ injury can affect all organs, but the brain and heart are typically most affected. Acute kidney injury requiring dialysis and resulting in chronic kidney disease is rare. Central nervous system involvement is often manifested by transient focal neurologic abnormalities resulting from micro-infarcts in the brain, which may cause focal neurologic deficits.
The mainstay of treatment is plasmapheresis with plasma replacement [32,33]. Plasmapheresis works by removing antibodies directed against the von Willebrand factor cleaving protease, ADAMTS-13. The plasma infused as part of the procedure also provides active ADAMTS-13 protease to the patient, further restoring a more physiologic state of von Willebrand factor multimers. Other treatment modalities in non-responders to plasmapheresis include immune-suppression, not limited to high dose steroids, and B-cell depleting agents (e.g. rituximab). Patients with autoantibodies against ADAMTS-13 do not always manifest TTP, and these antibodies alone are not sufficient to demonstrate the impending relapse of the disease. In the case of TTP, it is considered better to avoid platelet transfusion, which should be reserved for patients with clinically significant bleeding, as severe thrombocytopenia itself is not an indication for platelet transfusion. Conversely, platelet transfusion is probably not as dangerous as it was thought to be a decade ago [34].
Drug-induced thrombocytopenia/DITP and heparin-induced thrombocytopenia
In the event of drug-induced thrombocytopenia/DITP, it is universal practice to stop the suspected drug immediately. Platelet counts usually recover within several days to 2 weeks. Platelet transfusions may be required to treat patients with severe thrombocytopenia and bleeding. Other supportive measures include high dose intravenous immunoglobulin, a brief course of corticosteroids, or even plasmapheresis. Drug-dependent platelet antibodies can persist for years; thus, patients with a confirmed diagnosis should be counseled to avoid future exposures to the drug (with the possible exception of heparin). Testing at one of the few experienced laboratories can be very helpful in confirming a diagnosis.
The diagnosis of heparin-induced thrombocytopenia is based on the clinical setting: a platelet count of 200,000 may have decreased enough in a post-op case as to indicate platelet consumption. The management of heparin-induced thrombocytopenia is based on the immediate discontinuation of heparin and the institution of alternative, immediately active anticoagulation [11]. It is extremely important to prevent additional thrombosis and, for this reason, patients are usually treated with an alternative anticoagulant, even if heparin was given only as a prophylactic measure. Options include direct thrombin inhibitors such as lepirudin or argatroban, which are approved by the FDA. Other medications, such as bivalirudin and fondaparinux, can be used in this setting, but are not FDA-approved for the treatment of heparin-induced thrombocytopenia. Coumadin should not be given in the acute setting, as it can provoke thrombotic complications due to protein C depletion during the first days of use. Therefore, coumadin treatment should be postponed until complete normalization of the platelet count. Platelet transfusions are not a routine component of the treatment of heparin-induced thrombocytopenia, since thrombosis, not bleeding, is the primary clinical problem in this illness.
Thrombocytopenia in pregnancy
Causes of thrombocytopenia during pregnancy can be directly related to pregnancy, or be unrelated. Average platelet counts are decreased during pregnancy, especially during the third trimester, and when this decrease is mild and otherwise unexplained it is termed gestational thrombocytopenia, the most common cause of thrombocytopenia during pregnancy. Gestational thrombocytopenia develops due to the combination of hemodilution and platelet consumption. Increased levels of thromboxane A2 can contribute to increased platelet aggregation. Gestational thrombocytopenia usually develops during the late second or third trimester and disappears within months after delivery; there is no risk of fetal/neonatal thrombocytopenia in this condition. Therapy is virtually never given for this condition unless the platelet count is <80−100 × 109/L, the threshold needed for epidural anesthesia.
Other causes of thrombocytopenia during pregnancy should be differentiated from gestational thrombocytopenia because the approach to these conditions is different. For pregnant women, it is reasonable to define thrombocytopenia as a platelet count below the 2.5th percentile: 116 × 109/L (2.5th percentile in non-pregnant women is 150 × 109/L). The reasonable trigger for further investigation, unless certain findings suggest otherwise, is a platelet count lower than 80 × 109/L [35]. Diagnosis is largely dependent on the time of the onset of thrombocytopenia, its severity and association with other abnormal findings, and whether hemolysis or organ dysfunction are involved. Mild to moderate thrombocytopenia developing in the second or third trimester can be associated with pre-eclampsia. To diagnose pre-eclampsia, new onset hypertension and proteinuria are required, sometimes associated with liver enzyme elevation and mild LDH elevation. More prominent liver enzyme elevation and LDH elevation, associated with microangiopathic hemolytic anemia, suggest HELLP (hemolysis, elevated liver enzymes, low platelet) syndrome. Moderate to severe thrombocytopenia is typical for HELLP syndrome. Pre-eclampsia, associated with HELLP syndrome, is treated symptomatically, but the most effective treatment is the delivery of the fetus, although seizures after delivery have occurred. Sometimes plasmapheresis is needed for HELLP [36].
Another cause of thrombocytopenia during pregnancy (and the second most common cause after gestational thrombocytopenia) is ITP. It is impossible to distinguish this kind of thrombocytopenia from gestational thrombocytopenia, as a diagnostic test for both conditions does not exist. It is reasonable to use a cut-off of 50−70 × 109/L platelets as a lower limit for gestational thrombocytopenia [37]. If ITP is suspected, frequent follow up (every 1-3 weeks) is required, depending upon the count and the time to expected delivery. During the first and second trimester, treatment for ITP is necessary only if a patient is symptomatic, if a procedure is required, for example, an amniocentesis, or the platelet count drops below 20 × 109/L. If the patient is asymptomatic and the platelet count is >20 × 109/L, treatment may be required only during the last part of the third trimester to elevate the platelet count prior to epidural anesthesia or Caesarian section. Low dose (10-20 mg/day) prednisone or intravenous immunoglobulin or both are reasonable options in these situations. Other treatment modalities can be used in symptomatic pregnant ITP patients (e.g. if there is bleeding) or if a platelet count is less than 20 × 109/L. A high dose of steroids can be used, especially in combination with intravenous immunoglobulin and/or intravenous anti-D (if Rhesus positive, direct antiglobulin test-negative and not splenectomized). In a very refractory patient other medications can be used, including azathioprin and/or cyclosporin (if needed). Splenectomy can be performed during the second trimester for severe ITP cases but this option is very rarely pursued. Limited data are available to describe rituximab use during pregnancy but, as an IgG1 monoclonal, it is expected to cross the placenta and thus cannot be recommended for fear of depleting fetal B cells, although a series of lymphoma cases treated during pregnancy have been accumulated demonstrating an apparent absence of serious fetal/neonatal effects [38]. Many other agents, typically used for ITP treatment, cannot be used during pregnancy due to their potential for crossing the placenta and being teratogenic. The effect on the fetus of thrombopoietin-agonists is unknown, and these medications cannot be recommended due to the lack of data and the anticipation that they will cross the placenta and stimulate the fetal marrow in utero.
Other types of thrombocytopenia should be taken into account in pregnant patients. Inherited thrombocytopenia, for example, can be diagnosed occasionally during pregnancy.
Conclusions
An important approach to the successful treatment of thrombocytopenia is the understanding of the underlying pathophysiological processes in the development of the disease. Thrombocytopenia can either be primary or secondary, in that it can accompany a broad spectrum of syndromes and diseases and may be caused by various mechanisms. Prompt investigation and identification may be crucial and sometimes life-saving as in TTP, heparin-induced thrombocytopenia, acute leukemia or even severe ITP. Taking a detailed history and a thorough physical investigation can provide clues regarding possible underlying diseases and medical treatments. Careful examination of the peripheral blood smear is mandatory. When differential diagnosis is problematic, sometimes a short trial of treatment can help to clarify the cause. For example, it may be difficult to distinguish inherited thrombocytopenia (without a family history) from ITP; in this example, intravenous immunoglobulin infusion will likely have no effect in inherited thrombocytopenia, but will usually be helpful in ITP.
Notable progress has been made in recent years in developing new treatment options for thrombocytopenia patients, especially in ITP. In addition to rituximab and the thrombopoietin agents, combinations of different diagnostic and therapeutic modalities and various therapeutic approaches are the main strategies for difficult cases.
A number of issues complicate the differential diagnosis and treatment of thrombocytopenia.
There is no specific diagnostic test for many of the thrombocytopenias, such as ITP. Alternatively if the definitive test of a suspected condition is molecular, it may require months before the results become available. Also, the natural history and prognosis are often unpredictable and the response to treatment is unknown. Another factor is that it may be difficult to choose an effective treatment for a specific patient. For example, in ITP there is no universally accepted specific test currently available to predict response to splenectomy or rituximab.
More targeted therapies and preventative strategies are crucial for the treatment of thrombocytopenia, ideally defining and eliminating etiologic factors. Clinical trials are needed to determine the efficacy and safety of new approaches and to compare different therapeutic modalities. Long-term maintenance treatment options for chronic patients should be investigated, not only in regard to efficacy but also toxicity, and with a special view to potential curative effects.
Abbreviations
- CAMT
congenital amegakaryocytic thrombocytopenia
- CBC
complete blood count
- DIC
disseminated intravascular coagulation
- DITP
drug-induced immune thrombocytopenia
- EBV
Epstein-Barr virus
- FDA
US Food and Drug Administration
- HELLP
hemolysis elevated liver enzymes, low platelet
- HIT
heparin-induced thrombocytopenia
- HIV
human immunodeficiency virus
- IgG
immunoglobulin G
- ITP
immune thrombocytopenia
- LDH
lactate dehydrogenase
- MYH9-RD
May-Hegglin-related disorders associated with the MYH9 gene
- TAR
thrombocytopenia-absent radii syndrome
- TTP
thrombotic thrombocytopenia purpura
- WAS
Wiskott-Aldrich syndrome
Disclosures
Jim Bussel and relatives own stock in both Amgen and GlaxoSmithKline (less than USD 50,000), and Jim has served on multiple advisory boards for Amgen, GlaxoSmithKline, Eisai, Cangene, Baxter, and Sysmex and has received research funding from these entities. Marina Izak declares that she has no disclosures.
The electronic version of this article is the complete one and can be found at: http://f1000.com/prime/reports/m/6/45
References:
- 1.Lab Tests online UK Platelet count aka thrombocyte count. http://www.labtestsonline.org.uk/understanding/analytes/platelet/tab/test [Google Scholar]
- 2.Patrono C, Rocca B. Aspirin and Other COX-1 inhibitors. Handb Exp Pharmacol. 2012:137–64. doi: 10.1007/978-3-642-29423-5_6. [DOI] [PubMed] [Google Scholar]
- 3.Konkle BA. Acquired disorders of platelet function. Hematology Am Soc Hematol Educ Program. 2011;2011:391–6. doi: 10.1182/asheducation-2011.1.391. [DOI] [PubMed] [Google Scholar]
- 4.Aster RH. Pooling of platelets in the spleen: role in the pathogenesis of “hypersplenic” thrombocytopenia. J Clin Invest. 1966;45:645–57. doi: 10.1172/JCI105380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Provan D, Stasi R, Newland AC, Blanchette VS, Bolton-Maggs P, Bussel JB, Chong BH, Cines DB, Gernsheimer TB, Godeau B, Grainger J, Greer I, Hunt BJ, Imbach PA, Lyons G, McMillan R, Rodeghiero F, Sanz MA, Tarantino M, Watson S, Young J, Kuter DJ. International consensus report on the investigation and management of primary immune thrombocytopenia. Blood. 2010;115:168–86. doi: 10.1182/blood-2009-06-225565. [DOI] [PubMed] [Google Scholar]
- 6.Grimaldi-Bensouda L, Michel M, Aubrun E, Leighton P, Viallard J, Adoue D, Magy-Bertrand N, Tisserand G, Khellaf M, Durand J, Quittet P, Fain O, Bonnotte B, Morin AS, Limal N, Costedoat-Chalumeau N, Morel N, Pan-Petesch B, Decaux O, Mahevas M, Ruel M, Sacre K, Lefrere F, Abenhaim L, Godeau B. A case-control study to assess the risk of immune thrombocytopenia associated with vaccines. Blood. 2012;120:4938–44. doi: 10.1182/blood-2012-05-431098. [DOI] [PubMed] [Google Scholar]; http://f1000.com/prime/717971065
- 7.Cines DB, Liebman H, Stasi R. Pathobiology of secondary immune thrombocytopenia. Semin Hematol. 2009;46:S2–14. doi: 10.1053/j.seminhematol.2008.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Arnold DM, Nazi I, Warkentin TE, Smith JW, Toltl LJ, George JN, Kelton JG. Approach to the diagnosis and management of drug-induced immune thrombocytopenia. Transfus Med Rev. 2013;27:137–45. doi: 10.1016/j.tmrv.2013.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Huxtable LM, Tafreshi MJ, Rakkar ANS. Frequency and management of thrombocytopenia with the glycoprotein IIb/IIIa receptor antagonists. Am J Cardiol. 2006;97:426–9. doi: 10.1016/j.amjcard.2005.08.066. [DOI] [PubMed] [Google Scholar]
- 10.Linkins L, Dans AL, Moores LK, Bona R, Davidson BL, Schulman S, Crowther M. Treatment and prevention of heparin-induced thrombocytopenia: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed.: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141:e495S–530S. doi: 10.1378/chest.11-2303. [DOI] [PMC free article] [PubMed] [Google Scholar]; http://f1000.com/prime/718390768
- 11.Drachman JG. Inherited thrombocytopenia: when a low platelet count does not mean ITP. Blood. 2004;103:390–8. doi: 10.1182/blood-2003-05-1742. [DOI] [PubMed] [Google Scholar]
- 12.Medscape reference library. http://www.medscape.com/
- 13.Patel PD, Samanich JM, Mitchell WB, Manwani D. A unique presentation of Wiskott-Aldrich syndrome in relation to platelet size. Pediatr Blood Cancer. 2011;56:1127–9. doi: 10.1002/pbc.22920. [DOI] [PubMed] [Google Scholar]; http://f1000.com/prime/718390785
- 14.Pecci A, Gresele P, Klersy C, Savoia A, Noris P, Fierro T, Bozzi V, Mezzasoma AM, Melazzini F, Balduini CL. Eltrombopag for the treatment of the inherited thrombocytopenia deriving from MYH9 mutations. Blood. 2010;116:5832–7. doi: 10.1182/blood-2010-08-304725. [DOI] [PubMed] [Google Scholar]; http://f1000.com/prime/718390786
- 15.Al-Ahmari A, Ayas M, Al-Jefri A, Al-Mahr M, Rifai S, El-Solh H. Allogeneic stem cell transplantation for patients with congenital amegakaryocytic thrombocytopenia (CAT) Bone Marrow Transplant. 2004;33:829–31. doi: 10.1038/sj.bmt.1704445. [DOI] [PubMed] [Google Scholar]; http://f1000.com/prime/718390787
- 16.Bizzetto R, Bonfim C, Rocha V, Socié G, Locatelli F, Chan K, Ramirez O, Stein J, Nabhan S, Miranda E, Passweg J, Souza CA de, Gluckman E. Outcomes after related and unrelated umbilical cord blood transplantation for hereditary bone marrow failure syndromes other than Fanconi anemia. Haematologica. 2011;96:134–41. doi: 10.3324/haematol.2010.027839. [DOI] [PMC free article] [PubMed] [Google Scholar]; http://f1000.com/prime/718390788
- 17.Page LK, Psaila B, Provan D, Michael Hamilton J, Jenkins JM, Elish AS, Lesser ML, Bussel JB. The immune thrombocytopenic purpura (ITP) bleeding score: assessment of bleeding in patients with ITP. Br J Haematol. 2007;138:245–8. doi: 10.1111/j.1365-2141.2007.06635.x. [DOI] [PubMed] [Google Scholar]
- 18.Cines DB, Bussel JB, Liebman HA, Luning Prak ET. The ITP syndrome: pathogenic and clinical diversity. Blood. 2009;113:6511–21. doi: 10.1182/blood-2009-01-129155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Neunert C, Lim W, Crowther M, Cohen A, Solberg L, Crowther MA. The American Society of Hematology 2011 evidence-based practice guideline for immune thrombocytopenia. Blood. 2011;117:4190–207. doi: 10.1182/blood-2010-08-302984. [DOI] [PubMed] [Google Scholar]; http://f1000.com/prime/718390789
- 20.Mazzucconi MG, Fazi P, Bernasconi S, Rossi G de, Leone G, Gugliotta L, Vianelli N, Avvisati G, Rodeghiero F, Amendola A, Baronci C, Carbone C, Quattrin S, Fioritoni G, D'Alfonso G, Mandelli F. Therapy with high-dose dexamethasone (HD-DXM) in previously untreated patients affected by idiopathic thrombocytopenic purpura: a GIMEMA experience. Blood. 2007;109:1401–7. doi: 10.1182/blood-2005-12-015222. [DOI] [PubMed] [Google Scholar]
- 21.Godeau B, Chevret S, Varet B, Lefrère F, Zini JM, Bassompierre F, Chèze S, Legouffe E, Hulin C, Grange MJ, Fain O, Bierling P. Intravenous immunoglobulin or high-dose methylprednisolone, with or without oral prednisone, for adults with untreated severe autoimmune thrombocytopenic purpura: a randomised, multicentre trial. Lancet. 2002;359:23–9. doi: 10.1016/S0140-6736(02)07275-6. [DOI] [PubMed] [Google Scholar]; http://f1000.com/prime/718390790
- 22.Bussel JB, Kaufmann CP, Ware RE, Woloski BM. Do the acute platelet responses of patients with immune thrombocytopenic purpura (ITP) to IV anti-D and to IV gammaglobulin predict response to subsequent splenectomy? Am J Hematol. 2001;67:27–33. doi: 10.1002/ajh.1072. [DOI] [PubMed] [Google Scholar]
- 23.Wood JH, Partrick DA, Hays T, Ziegler MM. Predicting response to splenectomy in children with immune thrombocytopenic purpura. J Pediatr Surg. 2010;45:140–4. doi: 10.1016/j.jpedsurg.2009.10.026. discussion 144. [DOI] [PubMed] [Google Scholar]
- 24.Ghanima W, Godeau B, Cines DB, Bussel JB. How I treat immune thrombocytopenia: the choice between splenectomy or a medical therapy as a second-line treatment. Blood. 2012;120:960–9. doi: 10.1182/blood-2011-12-309153. [DOI] [PubMed] [Google Scholar]
- 25.Godeau B, Porcher R, Fain O, Lefrère F, Fenaux P, Cheze S, Vekhoff A, Chauveheid M, Stirnemann J, Galicier L, Bourgeois E, Haiat S, Varet B, Leporrier M, Papo T, Khellaf M, Michel M, Bierling P. Rituximab efficacy and safety in adult splenectomy candidates with chronic immune thrombocytopenic purpura: results of a prospective multicenter phase 2 study. Blood. 2008;112:999–1004. doi: 10.1182/blood-2008-01-131029. [DOI] [PubMed] [Google Scholar]; http://f1000.com/prime/718390800
- 26.Patel VL, Mahévas M, Lee SY, Stasi R, Cunningham-Rundles S, Godeau B, Kanter J, Neufeld E, Taube T, Ramenghi U, Shenoy S, Ward MJ, Mihatov N, Patel VL, Bierling P, Lesser M, Cooper N, Bussel JB. Outcomes 5 years after response to rituximab therapy in children and adults with immune thrombocytopenia. Blood. 2012;119:5989–95. doi: 10.1182/blood-2011-11-393975. [DOI] [PMC free article] [PubMed] [Google Scholar]; http://f1000.com/prime/717965659
- 27.Zaja F, Baccarani M, Mazza P, Bocchia M, Gugliotta L, Zaccaria A, Vianelli N, Defina M, Tieghi A, Amadori S, Campagna S, Ferrara F, Angelucci E, Usala E, Cantoni S, Visani G, Fornaro A, Rizzi R, Stefano V de, Casulli F, Battista ML, Isola M, Soldano F, Gamba E, Fanin R. Dexamethasone plus rituximab yields higher sustained response rates than dexamethasone monotherapy in adults with primary immune thrombocytopenia. Blood. 2010;115:2755–62. doi: 10.1182/blood-2009-07-229815. [DOI] [PubMed] [Google Scholar]; http://f1000.com/prime/717965659
- 28.Gudbrandsdottir S, Birgens HS, Frederiksen H, Jensen BA, Jensen MK, Kjeldsen L, Klausen TW, Larsen H, Mourits-Andersen HT, Nielsen CH, Nielsen OJ, Plesner T, Pulczynski S, Rasmussen IH, Rønnov-Jessen D, Hasselbalch HC. Rituximab and dexamethasone vs dexamethasone monotherapy in newly diagnosed patients with primary immune thrombocytopenia. Blood. 2013;121:1976–81. doi: 10.1182/blood-2012-09-455691. [DOI] [PubMed] [Google Scholar]; http://f1000.com/prime/717976348
- 29.Saleh MN, Bussel JB, Cheng G, Meyer O, Bailey CK, Arning M, Brainsky A. Safety and efficacy of eltrombopag for treatment of chronic immune thrombocytopenia: results of the long-term, open-label EXTEND study. Blood. 2013;121:537–45. doi: 10.1182/blood-2012-04-425512. [DOI] [PubMed] [Google Scholar]
- 30.Kuter DJ, Bussel JB, Newland A, Baker RI, Lyons RM, Wasser J, Viallard J, Macik G, Rummel M, Nie K, Jun S. Long-term treatment with romiplostim in patients with chronic immune thrombocytopenia: safety and efficacy. Br J Haematol. 2013;161:411–23. doi: 10.1111/bjh.12260. [DOI] [PubMed] [Google Scholar]; http://f1000.com/prime/717991063
- 31.Basciano PA, Bussel JB. Thrombopoietin-receptor agonists. Curr Opin Hematol. 2012;19:392–8. doi: 10.1097/MOH.0b013e328356e909. [DOI] [PubMed] [Google Scholar]
- 32.George JN. How I treat patients with thrombotic thrombocytopenic purpura: 2010. Blood. 2010;116:4060–9. doi: 10.1182/blood-2010-07-271445. [DOI] [PubMed] [Google Scholar]
- 33.Scully M, Goodship T. How I treat thrombotic thrombocytopenic purpura and atypical haemolytic uraemic syndrome. Br J Haematol. 2014;164:759–66. doi: 10.1111/bjh.12718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Swisher KK, Terrell DR, Vesely SK, Kremer Hovinga JA, Lämmle B, George JN. Clinical outcomes after platelet transfusions in patients with thrombotic thrombocytopenic purpura. Transfusion. 2009;49:873–87. doi: 10.1111/j.1537-2995.2008.02082.x. [DOI] [PubMed] [Google Scholar]; http://f1000.com/prime/718390802
- 35.McCrae KR. Thrombocytopenia in pregnancy. Hematology Am Soc Hematol Educ Program. 2010;2010:397–402. doi: 10.1182/asheducation-2010.1.397. [DOI] [PubMed] [Google Scholar]
- 36.Gernsheimer T, James AH, Stasi R. How I treat thrombocytopenia in pregnancy. Blood. 2013;121:38–47. doi: 10.1182/blood-2012-08-448944. [DOI] [PubMed] [Google Scholar]
- 37.Eser B, Guven M, Unal A, Coskun R, Altuntas F, Sungur M, Serin IS, Sari I, Cetin M. The role of plasma exchange in HELLP syndrome. Clin Appl Thromb Hemost. 2005;11:211–7. doi: 10.1177/107602960501100211. [DOI] [PubMed] [Google Scholar]; http://f1000.com/prime/718390803
- 38.Chakravarty EF, Murray ER, Kelman A, Farmer P. Pregnancy outcomes after maternal exposure to rituximab. Blood. 2011;117:1499–506. doi: 10.1182/blood-2010-07-295444. [DOI] [PubMed] [Google Scholar]