Abstract
Background
Workflow interruptions during surgery may cause a threat to patient's safety. Workflow interruptions were tested to predict failure in action regulation that in turn predicts near-accidents in surgery and related health care.
Methods
One-hundred-and-thirty-three theater nurses and physicians from eight Swiss hospitals participated in a cross-sectional questionnaire survey. The study participation rate was 43%.
Results
Structural equation modeling confirmed an indirect path from workflow interruptions through cognitive failure in action regulation on near-accidents (p < 0.05). The indirect path was stronger for workflow interruptions by malfunctions and task organizational blockages compared with workflow interruptions that were caused by persons. The indirect path remained meaningful when individual differences in conscientiousness and compliance with safety regulations were controlled.
Conclusion
Task interruptions caused by malfunction and organizational constraints are likely to trigger errors in surgery. Work redesign is recommended to reduce workflow interruptions by malfunction and regulatory constraints.
Keywords: cognitive failure, occupational stress, patient safety
1. Introduction
Workflow interruptions are common stressors in health care [1]. The consequences of workflow interruptions are not bad per se [2]. Sometimes the need to switch from one task to another more “critical” task is positive even when the first task is delayed [3]. Although such workflow interruptions are sometimes helpful in surgery (e.g., a note about adhering to the principles of asepsis), a majority of interruptions (e.g., nonpatient-related private conversation) are not [4]. Workflow interruptions interfere with the pursuit of tasks and can cause errors in carrying out actions, even in routine tasks that have been finished without error many times previously [5,6]. Thus, workflow interruptions are an avoidable threat to surgery outcomes and patient safety.
In their recent review of 33 studies, Rivera-Rodriguez and Karsh [4] reported only seven studies of interruptions and cognitive function in health care and concluded that more studies should focus on cognitive function because “these cognitive implications of interruptions are at the heart of why the study of interruptions is important” (p. 309). The current study on workflow interruptions tests cognitive failure in the action regulation of routine tasks as the critical link between interruptions and near-accidents.
Workflow interruptions may trigger failure in action regulation [7]. When there is an interruption, attention must be diverted to the interruption agent and away from the current task at hand. The goal of the interrupted action and its position in the action sequence must be stored in working memory. Moreover, the additional goal of restarting the interrupted task at hand at a later time must be stored in prospective memory [7]. The negative consequences of interruptions arise from these growing costs of action regulation while performing routine tasks. A typical error that is caused by workflow interruptions is the error of omission: for example, a theater nurse is interrupted by a nonpatient-related question and forgets to fill out the form while preparing a device because the restart of the action sequence is misplaced (a place-losing error, p. 29) [7]. Wallace and Chen [8] suggested adverse work conditions, including workflow interruptions, make cognitive failure during routine tasks more likely.
It is not only interruptions at work that can cause concern about cognitive failure and near-accidents, but also individual differences in conscientiousness and safety compliance. Indeed, the first conceptualizations considered cognitive failures primarily as randomly appearing or based on individual trait-like cognitive failure proneness [9,10]. Wallace and Chen [8] showed that work-related cognitive failure not only corresponds to work demands, but is also negatively related to individual conscientiousness. Wallace and Chen [8] supposed that conscientiousness was negatively related to workplace cognitive failure, presumably because “individuals higher on conscientiousness should be more attentive to work tasks and thereby not commit as many cognitive failures” (p. 618). In this study, we controlled for individual differences in conscientiousness and safety compliance by including both in the prediction model. We assumed an indirect path from workflow interruptions through failure in action regulation to near-accidents during surgery beyond personal conscientiousness and safety compliance. Therefore, for this study on workflow interruptions in surgery we hypothesized that workflow interruptions are positively associated with failure in action regulation (H1) and near-accidents (H2). Moreover, we expected a significant indirect path from workflow interruptions through failure in action regulation to near-accidents in surgery (H3).
2. Materials and methods
2.1. Study setting
The study design and its aim were presented to the nursing directors of eight hospitals within the German speaking part of Switzerland. All the hospitals agreed to participate in the study. Seven hospitals are from the German speaking part of Switzerland and one hospital is located in a region where half of the population speaks French or German; thus, in terms of language and region they are not representative for the French and Italian speaking parts of Switzerland. The eight hospitals are representative with respect to types of hospitals within Switzerland because the sample includes a large university hospital, three other public hospitals, two smaller, more regional semiprivate hospitals, and two smaller more regional private hospitals—a mixture that is common for hospitals in Switzerland. Two of the authors (P.K. and M.N.) distributed the questionnaires at the hospitals and responded to questions. The questionnaires included postage-paid envelopes. After 2 weeks, P.K. and M.N. sent a written reminder to all those who had received the questionnaire (with a note to ignore the reminder if the questionnaire had already been sent off in the postage-paid envelopes addressed to the first authors' university department).
2.2. Study sample
All participants gave their informed consent prior to when questionnaires were distributed. Questionnaires were addressed to 312 theater nurses and physicians from eight surgical units. The questionnaires were distributed during regular team meetings of theater nurses. In these meetings, members were predominantly theater nurses with only two or three anesthetists and surgeons as members. There was no difference in agreement to participate between nurses and physicians as members of the theater nurse team meetings. In the questionnaire, most participants (87%) did not fill out the text field that asked for their professional title, presumably to reduce their identifiability within surgery teams. Therefore, the exact number of physicians is unclear but with respect to group composition in theater nurse's group meetings, it can be estimated to be between 10 and 15. The response rate was 42.6% with 133 questionnaires being returned. There were 21 male participants and 112 female participants. The mean age was 40.2 years [standard deviation (SD) = 11.7 years]. The mean job tenure was 15 years (SD = 10.6 years) and participants had worked for, on average, 9.2 years in their current position (SD = 8.1 years). This study was carried out in accordance with the Code of Ethics of the World Medical Association (Declaration of Helsinki) and was approved by the Ethics Committee of Kanton Bern, Switzerland (KEK No. Z001/13).
Sixty-five percent of the sample worked between 90% and full-time (42 contracted hours/week), 24% worked part-time for more than 50% and less than 90% of full-time hours, and 11% worked 50% or less of full-time hours.
2.3. Assessment of workflow interruptions
Interruptions in workflow were assessed using 15 items from the activity and work analysis in hospitals-self-report version (TAA-KH-S) [11]. The TAA-KH-S is theoretically based on the action regulation theory that emphasizes interruptions as work stressors that impede goal attainment. The TAA-KH-S is a condition-related work analysis instrument, developed for the analysis of work in hospitals. The internal consistency of the total interruption scale is adequate (Cronbach α = 0.87). Three subscales measured interruptions by persons (six items, Cronbach α = 0.74), interruptions by malfunctions (four items, Cronbach α = 0.84), and interruptions by blockages arising from organizational constraints, such as interruptions because materials and instruments did not arrive in time (five items, Cronbach α = 0.79). The response format was 1 = never to 5 = very often.
2.4. Assessment of cognitive failure in action regulation
The failure in action execution subscale of the Workplace Cognitive Failure Scale was used to measure slips and lapses in routine action execution [8,12]. The scale included five items (e.g., “Unintentionally press control switches on machines?”). The response format was 1 = never to 5 = very often. The internal consistency of the scale was satisfactory (Cronbach α = 0.77). All were paper–pencil form of questionnaires.
2.5. Assessment of near-accidents in the past 4 weeks
For this study, a near-accident was defined as an occurrence that deviates from the normal course of events and might give rise to an accident [13]. The question about near-accidents was preceded by an annotation that was an adapted version of the statement Musahl and Bendig [14] introduced for describing near-accidents: “The following question refers to near-accidents during your work. Near-accidents characterize situations when you or the patient had a narrow escape from experiencing an accident.” The item was “How many near-accidents do you remember in the past 4 weeks?” The response format was a number.
2.6. Assessment of conscientiousness
Conscientiousness is part of the five-factor model of personality [15]. The five-factor model questionnaire used in this study was based on an adjective-rating list developed by Ostendorf [16] and Ostendorf and Angleitner [17]. Schallberger and Venetz [18] validated a shorter adjective-rating scale questionnaire that was fitting in its factorial structure and internal consistency of scales. The questionnaire consists of bipolar items on a six-point scale, with higher values indicating higher conscientiousness. Conscientiousness included six items [meticulous vs. imprecise (reverse scored), careless vs. conscientious, regular vs. disorderly (reverse scored), inaccurate vs. thorough, disregarding vs. regardful, and hardworking vs. lazy (reverse scored)]. The conscientiousness scale was reliable (Cronbach α = 0.83).
2.7. Assessment of compliance with safety regulations
This was a single questionnaire item that included a comment in parentheses about safe working behavior: “I pay attention to safety at work (compliance with safety regulations, consideration of recommended means to procedures, etc.),” with responses on a five-point Likert scale ranging from 1 = seldom to 5 = always [19].
2.8. Data analysis
We first tested whether hospitals differed in the study variables. There were no significant differences in workflow interruptions, failure in action regulation, and near-accidents, and therefore we did not control for organization in the structural equation testing. SPSS Amos 18.0 (SPSS: An IBM Company, Chicago, IL) was used to: (1) test a measurement model of all constructs involved in the mediation hypothesis and (2) model the latent path structure of the hypothesized mediation model. Unless an indicator is a near-perfect measure of the latent variable, several indicators are needed for representation. Preferably, these are subscales, as in workflow interruption, with the three subscales as indicators of interruptions by persons, by malfunction, and by blockages. For the measurement modeling of conscientiousness, the parceling method was used [20]. Six items from the conscientiousness scale were divided into three parcels of two items. The five items of the cognitive failure in action execution scale were divided into two parcels of two items and one parcel of one item. For near-accidents during work, no modeling was necessary because it is a single-item manifest variable. The indirect path hypotheses were tested through AMOS 18.0, which included a bootstrap test of the indirect effects. Preacher and Hayes proposed bootstrapping because it is more robust in small samples than other approaches [21]. Bootstrapping, a nonparametric resampling procedure, is an additional method advocated for testing indirect effects that does not impose the assumption of the normality of the sampling distribution. Bootstrapping is a computationally intensive method that involves repeated sampling from the data set and estimating the indirect effect on each resampled data set. By repeating this process very often (we scheduled 10,000 times), an empirical approximation of the sampling distribution of the indirect (mediation) path is built and used to construct confidence intervals (CIs) for the indirect effect.
A test of a hypothesized structural equation model should also include a test of a plausible alternative model. A plausible alternative approach is the person-oriented accident-prone person model, which postulates the opposite direction of causality, namely that an individual trait such as conscientiousness induces stable individual differences in action regulation. The idea of an accident-prone person “… implies that, irrespective of environment, that individual is more likely at all times to incur an accident than his colleagues even though exposed to equal risk, and that this is due to some characteristic or summation of characteristics associated with corporeal dexterity, sensori-motor skill, personality, or higher conative or cognitive function” [22]. Thus, the assumption in the accident-prone person model is that cognitive failure during action execution induces workflow interruptions; that is, more interruptions at work are self-induced by giving priority to less important task execution while important tasks should have been done first. Hence, interruptions might then mediate the effects of cognitive failure on task execution in near-accidents. The accident-prone person model is compared with the hypothesized mediation model [23,24]. A nonsignificant mediation and significantly worse fit of data for the alternative accident-prone person model than in the hypothesized mediation model would increase the plausibility of the latter. Because of the directional hypothesis, the 5% alpha level was one tailed [25].
3. Results
Table 1 shows the mean values and SDs of the study variables. One or more near-accidents during surgery in the past 4 weeks were reported by more than half of the nurses (mean = 1.19, SD = 2.00). The mean level of total workflow interruptions was 2.13 on the five-point scale (SD = 0.50). Interruptions by persons including patients were also moderate (mean = 2.24, SD = 0.58). Interruptions by malfunction (mean = 2.25, SD = 0.64) and interruptions by blockages (mean = 1.90, SD = 0.61) were also moderate. The mean level of failure in action regulation was low (mean = 1.87, SD = 0.45), whereas the mean levels of safety compliance (mean = 4.01, SD = 0.82) and conscientiousness in the study sample were high (mean = 5.01, SD = 0.68).
Table 1.
Descriptive statistics and internal consistencies (cronbach α) for all study variables
| Variable | Items | Range | M | SD | Cronbach α |
|---|---|---|---|---|---|
| Number of near-accidents at work during the past 4 wk | 1 | Count | 1.19 | 2.00 | n.a. |
| Workflow interruptions total | 15 | 1–5 | 2.13 | 0.50 | 0.87 |
| Interruptions by other persons | 6 | 1–5 | 2.24 | 0.58 | 0.74 |
| Interruptions by malfunction | 4 | 1–5 | 2.25 | 0.64 | 0.84 |
| Interruptions by blockages | 5 | 1–5 | 1.90 | 0.61 | 0.79 |
| Cognitive failure in action regulation (WCFS action) | 5 | 1–5 | 1.87 | 0.45 | 0.68 |
| Compliance with safety regulations | 1 | 1–5 | 4.01 | 0.82 | n.a. |
| Conscientiousness | 6 | 1–6 | 5.01 | 0.68 | 0.82 |
| Age | 1 | Count | 40.15 | 11.66 | n.a. |
| Gender (females: 112; males: 21) | 1 | 1–2 | n.a. | n.a. | n.a. |
M, mean; n.a., not applicable; SD, standard deviation; WCFS, Workplace Cognitive Failure Scale.
Table 2 shows correlations between study variables. In line with the hypotheses, total workflow interruptions and failure in action regulation were positively related. Near-accidents during surgery were also positively related to cognitive failure in action regulation but not to workflow interruptions. Conscientiousness corresponded to higher safety compliance and fewer failures in action regulation.
Table 2.
Intercorrelations of all study variables (N = 165)
| Variable | (1) | (2) | (3) | (4) | (5) | (6) | (7) | (8) | (9) |
|---|---|---|---|---|---|---|---|---|---|
| (1) Number of near-accidents at work in past 4 weeks | — | — | — | — | — | — | — | — | — |
| (2) Total workflow interruptions | 0.09 | — | — | — | — | — | — | — | — |
| (3) Interruptions by other persons | 0.02 | 0.81* | — | — | — | — | — | — | — |
| (4) Interruptions by malfunction | 0.10 | 0.87* | 0.57* | — | — | — | — | — | — |
| (5) Interruptions by blockages | 0.12 | 0.81* | 0.39* | 0.65* | — | — | — | — | — |
| (6) WCFS: action | 0.22† | 0.36* | 0.29* | 0.35* | 0.27‡ | — | — | — | — |
| (7) Compliance with safety regulations | 0.06 | 0.01 | −0.11 | 0.02 | 0.12 | −0.11 | — | — | — |
| (8) Conscientiousness | −0.01 | 0.09 | 0.04 | 0.05 | 0.12 | −0.19† | 0.39†,‡ | — | — |
| (9) Age | −0.05 | −0.07 | 0.02 | −0.21† | −0.01 | 0.02 | 0.12 | 0.23‡ | — |
| (10) Gender (females: 151; males: 14) | −0.06 | −0.11 | −0.07 | −0.05 | −0.16† | 0.05 | 0.12 | 0.04 | −0.10 |
*p < 0.001 one tailed.
† p < 0.05.
‡ p < 0.01.
WCFS, Workplace Cognitive Failure Scale.
3.1. Structural equation analysis
Table 3 shows the results of the tests of structural equation modeling including several indicators of model fit, with notes to explain when fit indices can be considered to represent a good model fit. A model that assumes independence (zero correlations) between manifest variables and latent variables has a very poor fit and thus does not represent the data. By contrast, a saturated model that estimates all relations between variables achieves a maximal fit. Both an independence model and a saturated model provide a frame of reference for specific model tests. Hypothesis testing started with a test of the measurement model. The measurement model included interruptions, failure in action execution, and conscientiousness as latent variables, each with three manifest indicator variables (near-accidents and safety compliance were included as manifest variables). All associations between variables were nondirectional. The measurement model represented the empirical data well [χ2 (36) = 48.18, χ2/df = 1.34, p = 0.08]. The root-mean-square error of approximation (RMSEA), an indicator of model fit that is often reported because it is not biased by sample size, was 0.06 (RMSEA values of 0.05 or below reflect a good model fit, and values between 0.05 and 0.08 indicate an adequate model fit) [26]. Thus, the confirmatory factor analyses within the measurement model confirmed the hypothetical factor structure of the latent variables. The hypothesized mediation model also represented the empirical data very well [χ2 (37) = 48.62, χ2/df = 1.31, p = 0.10, RMSEA = 0.05]. Indeed, the difference in the deviation of individual value as predicted by the model and empirical values expressed in χ2 values between the measurement value and the mediation model was not statistically significant [Δχ2 (1) = 0.44, ns]. Thus, both models were comparable in fit. As shown in Fig. 1, significant direct paths were observed from work interruptions to cognitive failure in action regulation (β = 0.41, p < 0.01), and from cognitive failure in action regulation to near-accidents (β = 0.26, p < 0.05). The test of indirect mediation effects using a bootstrapping approach within AMOS resulted in a significant indirect “total workflow interruptions → failure in action regulation → near-accident” path (H3, β = 0.11, CI 90 = 0.01–0.23). A separate model test for each type of workflow interruption showed an indirect effect of interruptions from malfunction and blockages that is comparable with the indirect effect of total workflow interruptions. The indirect effect when only interruptions from persons were included was smaller and did not reach a significant level (Table 3). The hypothesized model of indirect effect represented the empirical data well; however, alternative models may be equally good or even better. Hence, a hypothesized model should be compared with a plausible alternative model. Initial concepts of cognitive failure have viewed it primarily as a consequence of stable individual differences in self-regulation [9,27]. Thus, a plausible alternative model is the person-oriented accident-prone person model, which postulates that individuals high in cognitive failure increase interruptions at work by themselves; for example, by wrongly giving priority to less important tasks, the more important tasks may be likely to intrude. In the accident-prone person model, the directional path from interruptions to near-accidents was not significant and the test of the indirect path from failure in action regulation through workflow interruptions to near-accidents was also not significant (β = −0.01, CI 90 = −0.103–0.08).
Table 3.
Structural equation models fit to empirical data and key indirect paths tested∗
| Model | χ2 | df | χ2/df | p | CFI | RMSEA | AIC | Interruptions → WCFS action → Number of near accidents β (CI 90) |
|---|---|---|---|---|---|---|---|---|
| Independence model | 350.64 | 55 | 6.38 | 0.00 | 0 | 0.23 | 394.64 | — |
| Saturated model | 0 | 0 | 0 | — | 1.00 | 0.00 | 154.00 | — |
| Measurement model | 48.18 | 36 | 1.34 | 0.08 | 0.96 | 0.06 | 108.18 | — |
| Hypothesized indirect path model | 48.62 | 37 | 1.31 | 0.10 | 0.96 | 0.05 | 106.62 | 0.11 (0.01–0.23) |
| Only interruptions by persons included | 76.25 | 70 | 1.09 | 0.28 | 0.98 | 0.03 | 146.25 | 0.07 (−0.01 to 0.19) |
| Only interruptions by malfunction included | 34.12 | 37 | 0.92 | 0.60 | 1.00 | 0.04 | 92.12 | 0.12 (0.004–0.28) |
| Only interruptions by blockings included | 75.39 | 58 | 1.30 | 0.06 | 0.95 | 0.00 | 141.39 | 0.11 (0.001–0.23) |
| Alternative accident-prone person model | 48.21 | 37 | 1.30 | 0.10 | 0.96 | 0.05 | 106.21 | WCFS action → Interruptions → Number of near-accidents: −0.01 (−0.103 to 0.08) |
AIC, Akaike information criterion, which should be as low as possible. A nonsignificant χ2 and CFI higher than 0.90 in the indirect path model reflect an acceptable fit between the model and the data [26]. The comparably low Akaike information criterion attests to the parsimonious informative modeling in the hypothesized indirect path model; CFI, comparative fit index; CI, confidence interval; df, degrees of freedom; p, probability of the discrepancy to differ from zero (should be nonsignificant in a good model); p value of minimum discrepancy divided by its degrees of freedom, which should be nonsignificant; RMSEA, root-mean-square error of approximation, a measure of fit that takes into account the population moments rather than sample moments, RMSEA ≤ 0.05 can be considered a good fit; values between 0.05 and 0.08 indicate an adequate fit [26]; WCFS, Workplace Cognitive Failure Scale; χ2, indicates the minimum discrepancy between empirical covariance structures and those implied by the model; χ2/df, minimum discrepancy divided by its degrees of freedom, as an indicator of fit.
The models are as follows: (1) independence model: no associations between study variables were assumed; (2) saturated model: assumes all variables were interrelated—estimates best possible fit of model variables and empirical data; (3) measurement model: all latent variables were specified and assumed to be nondirectionally interrelated; (4) hypothesized indirect path model: model as shown in Fig. 1; and (5) alternative accident-prone person model: trait model, conscientiousness predicts WCFS action and compliance with safety regulations, and WCFS action predicts interruptions that directly link to near-accidents.
Fig. 1.
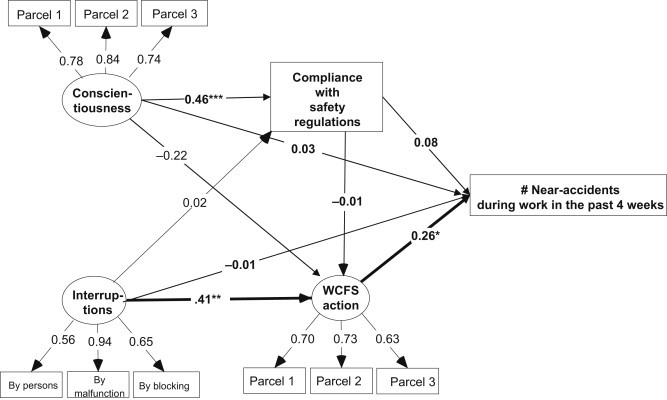
Model of work-related cognitive failure in action regulation (WCFS action) as a mediator of the effects of interruptions and conscientiousness on near-accidents. WCFS, Workplace Cognitive Failure Scale. ∗p < 0.05, ∗∗p < 0.01, ∗∗∗p < 0.001 one tailed.
4. Discussion
The objective of this study was to examine workflow interruptions in surgery and surgery assistance and cognitive failures in action regulation and their potential consequences for safety in surgery. This study adds evidence to the research field by confirming a model that is focused on the cognitive consequences of workflow interruptions as precursors of near-accidents. The indirect path for near-accidents remained significant when individual differences in conscientiousness and safety compliance were accounted for in the model. The size of the indirect paths is small but meaningful. Near-accidents often have many antecedents and are the result of numerous patient-related (body mass index and comorbidities) and procedure-related factors (type of surgery and its duration), and errors in routine tasks are only one specific proximal antecedent [28]. Moreover, errors in routine tasks are only one risky consequence of workflow interruption; other types of errors that are related to interruptions and safety in health care might also occur including, errors in complex problem solving [28]. Finally, workflow interruptions are only one type of work demand that contributes to near-accidents (e.g., time pressure can also increase the risk of near-accidents) [23]. Overall, the tested model was the archetypal one where specific work characteristics are related to specific errors in task regulation that could in turn be related to near-accidents in surgery. Allowing for the complexity of safety in health care, the size of the specific indirect path in the particular model tested is highly relevant. Results differed according to the source of interruptions. Therefore, workflow interruptions that were caused by malfunctions and task organization blockages showed a stronger indirect path for near-accidents than workflow interruptions by persons. Apparently, when colleagues interrupt during surgery, the consequences are not primarily negative but there are also positive ones that improve care or avoid harm. Therefore, work and task redesign resulting in the reduction of interruptions by malfunction and the organization of tasks are especially promising. However, no task redesign will completely prevent interruptions by malfunction and blockages. Therefore, task redesign should also aim to prevent errors in the aftermath of interruptions by decreasing the overall load of action regulation [29]. Important goals are to increase the ease of information availability [e.g., documentation of the steps of a surgical procedure, necessary medical devices for surgery, use of the WHO surgical safety checklist and implementation manual, 2008 [30], increase mandatory attention checks that have to be done to proceed with the task (e.g., presurgical verification of work flow), amplify use of memory helpers (e.g., electronic patient data available), and provide clear signals and distinctive choice alternatives (e.g., use of different plugs and sockets for different functions, use of distinctive labels for different medications, and distinctive labels for surgical accessories including loops, sutures, dressings, and implants). Most interruptions are irrelevant to the task and therefore mistimed [31]. Therefore, work design should provide interruption-free periods for certain interference-prone tasks (e.g., during preparation of the operating table). Equally as important as reducing unnecessary interruptions to prevent medical error is supporting a work design that promotes error management; that is, a work design that simplifies error detection and helps to keep the consequences of errors small while learning from near-errors [7]. For example, work design should increase job control, which has two benefits. First, job control increases options to better respond to interruptions (e.g., time control facilitates the handling of tasks with situational priority); namely, restarting the interrupted primary task at hand is easier when interference from other—less important—following tasks can be avoided. Second, time control helps to reduce the consequences of interruptions. This can be accomplished by, for example, increasing the time when nurses and physicians have influence over when and in what sequence tasks can be done; thus, tasks with situational priority can be done first while lower priority task can be delayed. It is important that nurses and physicians, who have expert knowledge concerning interruptions, should have regular discussions in health circles about types of interruptions, frequent antecedents and consequences, and about ways of reducing them [32]. In an analysis of near misses, Frese and Hofmann [33] have made a strong claim for analyzing not only individual but also collective failure modes. Individuals and collectives (e.g., teams, organizations) seem to function in a way that is, at least in part, based on similar information-processing-based language and action cycles. Because communication has been listed as being among the three most frequent causes of errors for so many types of sentinel events in health care, many errors can be avoided when the information and communication procedures (backup behavior, closed-loop communication, and others) are improved by team training [34,35]. Experience with crew resource management (CRM) training and the training derivatives of CRM have shown training to be effective not only in aviation but also in health care [36].
This study has several limitations. First, the design is correlational and cross sectional. The structural equation model with indirect paths should preferably be tested with experimental data where interruptions and cognitive function precede near-accidents. Second, correlations between study variables were small and all assessments were done by questionnaire. Bias from common source variance may have boosted even small correlations in this study. Nurses and physicians may perceive more near-accidents in the same way as they perceive their own level of cognitive failure in task regulation and more frequent interruptions—just because they are more pessimistic than others about everything in their work [37]. Thus, further studies should also refer to task observation [1,19]. Moreover, response rate was only moderate and thus bias cannot be excluded. Finally, no severity grading of near-accidents was made and that the study did not differentiate between the near-accidents of patients and those that occurred to nurses and physicians. There is, however, good evidence that the model is valid for both. Recent evidence shows working conditions to be a common antecedent in both nurses' and patients' injuries [38].
The study also has some advantages. The study comprised eight smaller and larger hospitals whereas most research findings are derived from very large organizations that might not be representative of working conditions in health care [39]. Finally, the use of a structural equation approach estimated associations between latent variables and measurement error was excluded from the analysis.
To summarize, cognitive failure in action regulation seems to be a promising intervening cognitive process in cognitive-oriented research on safety in health care [12]. An action regulation approach with a focus on the nature and consequences of interruptions may help to make hospitals safer places for nurses, physicians, and patients [40].
Conflicts of interest
No potential conflict of interest relevant to this article was reported.
Footnotes
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
References
- 1.Weigl M., Müller A., Zupanc A., Glaser J., Angerer P. Hospital doctors' workflow interruptions and activities: an observation study. BMJ Qual Saf. 2011;20:491–497. doi: 10.1136/bmjqs.2010.043281. [DOI] [PubMed] [Google Scholar]
- 2.Grundgeiger T., Sanderson P. Interruptions in healthcare: theoretical views. Int J Med Inform. 2009;78:293–307. doi: 10.1016/j.ijmedinf.2008.10.001. [DOI] [PubMed] [Google Scholar]
- 3.Semmer NK, Grebner S, Elfering A. Psychische Kosten von Arbeit. In: Enzyklopädie der Psychologie. Band: Arbeitspsychologie (Bd. D-III-1). [Psychological costs of work. In: German Encyclopedia of psychology. Vol. D-III-1 Work Psychology]. Göttingen (Germany): Hogrefe; 2010. p. 325–370. [in German].
- 4.Rivera-Rodriguez A.J., Karsh B.T. Interruptions and distractions in healthcare: review and reappraisal. Qual Saf Health Care. 2010;19:304–312. doi: 10.1136/qshc.2009.033282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dieckmann P., Reddersen S., Wehner T., Rall M. Prospective memory failures as an unexplored threat to patient safety: results from a pilot study using patient simulators to investigate the missed execution of intentions. Ergonomics. 2006;49:526–543. doi: 10.1080/00140130600568782. [DOI] [PubMed] [Google Scholar]
- 6.Elfering A., Grebner S. Stress and patient safety. In: Halbesleben J.R.B., editor. The handbook of stress and burnout in health care. Nova Science Publishers; Hauppauge (NY): 2008. pp. 173–186. [Google Scholar]
- 7.Hofmann D.A., Frese M. Routledge; New York (NY): 2011. Errors in organizations. 365 p. [Google Scholar]
- 8.Wallace J.C., Chen G. Development and validation of a work-specific measure of cognitive failure: implications for occupational safety. J Occup Organ Psychol. 2005;78:615–632. [Google Scholar]
- 9.Reason J. Stress and cognitive failure. In: Fisher S., Reason J., editors. Handbook of life stress, cognition, and health. Wiley; New York (NY): 1988. pp. 405–421. [Google Scholar]
- 10.Reason J. Cambridge University Press; New York (NY): 1990. Human error. 302 p. [Google Scholar]
- 11.Büssing A., Glaser J. Hogrefe; Göttingen (Germany): 2002. Das tätigkeits-und arbeitsanalyseverfahren für das krankenhaus-selbstbeobachtungsversion (TAA-KH-S) [Activity and work analysis in hospitals-self-report version (TAA-KH-S)] 276 p. [in German] [Google Scholar]
- 12.Elfering A., Grebner S., Dudan A. Job characteristics in nursing and work specific cognitive failure. Saf Health Work. 2011;2:194–200. doi: 10.5491/SHAW.2011.2.2.194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lagerlöf E. Accident research: theories and methods. Ambio. 1974;4:51–55. [Google Scholar]
- 14.Musahl H.-P., Bendig M. Universität Duisburg-Essen; Duisburg (Germany): 2005. Von der Wohnung zur Arbeit und zurück. Eine Studie zu Arbeitswegen und zum Wegeunfallgeschehen [From home to work and back home: a study on commuting and commuting accidents] 140 p. [in German] [Google Scholar]
- 15.Costa P.T., Jr., McCrae R.R. Psychological Assessment Resources; Odessa (FL): 1985. The NEO personality inventory manual. 44 p. [Google Scholar]
- 16.Ostendorf F. Roderer; Regensburg (Germany): 1990. Sprache und persönlichkeitsstruktur: zur validität des fünf-faktoren-modells der persönlichkeit [Language and the structure of personality: about the validity of the five-factor model] 226 p. [in German] [Google Scholar]
- 17.Ostendorf F., Angleitner A. On the generality and comprehensiveness of the five-factor model of personality. Evidence for five robust factors in questionnaire data. In: Caprara G.V., van Heck G.L., editors. Modern personality psychology: critical reviews and new directions. Harvester Wheatsheaf; New York (NY): 1992. pp. 73–109. [Google Scholar]
- 18.Schallberger U., Venetz M. vol. 30. University of Zurich. Reports of Department of Applied Psychology; Zurich (Switzerland): 1999. pp. 1–51. (Kurzversionen des MRS-inventars von Ostendorf (1999) zur erfassung der fünf “grossen” persönlichkeitsfaktoren [Brief versions of Ostendorf's MRS inventory for the assessment of the big-five personality factors]). [in German] [Google Scholar]
- 19.Elfering A., Semmer N.K., Grebner S. Work stress and patient safety: observer-rated work stressors as predictors of characteristics of safety-related events reported by young nurses. Ergonomics. 2006;49:457–469. doi: 10.1080/00140130600568451. [DOI] [PubMed] [Google Scholar]
- 20.Kelloway E.K. Common practices in structural equation modeling. In: Cooper C.L., Robertson I.T., editors. International review of industrial and organizational psychology. Wiley; Chichester (UK): 1996. pp. 141–180. [Google Scholar]
- 21.Preacher K.J., Hayes A.F. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behav Res Methods. 2008;40:879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- 22.Cresswell W.L., Frogatt P. Accident proneness, or variable accident tendency? J Stat Soc Inq Soc Ireland. 1962;20:152–171. [Google Scholar]
- 23.Elfering A., Grebner S., de Tribolet-Hardy F. The long arm of time pressure at work: cognitive failure and commuting near-accidents. Eur J Work Org Psychol. 2013;22:737–749. [Google Scholar]
- 24.Elfering A., Grebner S., Haller M. Railway-controller-perceived mental work load, cognitive failure and risky commuting. Ergonomics. 2012;55:1463–1475. doi: 10.1080/00140139.2012.718802. [DOI] [PubMed] [Google Scholar]
- 25.Wonnacott T.H., Wonnacott R.J. Wiley; New York (NY): 1990. Introductory statistics for business and economics. 1137 p. [Google Scholar]
- 26.Schermelleh-Engel K., Moosbrugger H., Müller H. Evaluating the fit of structural equation models: test of significance and descriptive goodness-of-fit measures. Methods Psychol Res. 2003;8:23–74. [Google Scholar]
- 27.Broadbent D.E., Cooper P.F., Fitzgerald P., Parkes K.R. The Cognitive Failures Questionnaire (CFQ) and its correlates. Br J Clin Psychol. 1982;21:1–16. doi: 10.1111/j.2044-8260.1982.tb01421.x. [DOI] [PubMed] [Google Scholar]
- 28.Healey A.N., Sevdalis N., Vincent C.A. Measuring intra-operative interference from distraction and interruption observed in the operating theatre. Ergonomics. 2006;49:589–604. doi: 10.1080/00140130600568899. [DOI] [PubMed] [Google Scholar]
- 29.Fitts P.M. Function of man in complex systems. Aerospace Eng. 1962;21:34–39. [Google Scholar]
- 30.WHO; Geneva (Switzerland): 2008. World Health Organisation (WHO). WHO surgical safety checklist and implementation manual. 2012 [cited 2012 Nov 21]. Available from: http://www.who.int/patientsafety/safesurgery/ss_checklist/en/ [Google Scholar]
- 31.Kahneman D. Prentice Hall; Englewood Cliffs (NJ): 1973. Attention and effort. 246 p. [Google Scholar]
- 32.Baethge A., Rigotti T. Work flow interruptions as daily stressors: the mediating role of time pressure and mental demand. Work Stress. 2013;27:43–63. [Google Scholar]
- 33.Frese M., Hofmann D.A. A new look on errors, error prevention, and error management in organizations. In: Hofmann D.A., Frese M., editors. Errors in organizations. Routledge; New York (NY): 2011. pp. 317–326. [Google Scholar]
- 34.Joint Commission on Accreditation of Healthcare Organizations. Root causes for sentinel events, 2004 to 2012 [Internet]. Oakbrook Terrace (IL): The Joint Commission; 2012. [cited 2012 Nov 21]. Available from: http://www.jointcommission.org/assets/1/18/Root_Causes_Event_Type_2004_2Q2012.pdf. 29 p.
- 35.Weaver S.J., Bedwell W.L., Salas E. Team training as an instructional mechanism to enhance reliability and manage errors. In: Hofmann D.A., Frese M., editors. Errors in organizations. Routledge; New York (NY): 2011. pp. 143–176. [Google Scholar]
- 36.Wilson K., Burke C., Priest H., Salas E. Promoting health care safety through training high reliability teams. Qual Saf Health Care. 2005;14:303–309. doi: 10.1136/qshc.2004.010090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Semmer N.K., Grebner S., Elfering A. Beyond self-report: using observational, physiological, and situation-based measures in research on occupational stress. In: Perrewé P.L., Ganster D.C., editors. Emotional and physiological processes and positive intervention strategies. Vol. 3. JAI; Amsterdam (Netherlands): 2004. pp. 205–263. (Research in occupational stress and well-being). [Google Scholar]
- 38.Taylor J.A., Dominici F., Agnew J., Gerwin D., Morlock L., Miller M.R. Do nurse and patient injuries share common antecedents? An analysis of associations with safety climate and working conditions. BMJ Qual Saf. 2012;21:101–111. doi: 10.1136/bmjqs-2011-000082. [DOI] [PubMed] [Google Scholar]
- 39.Kelloway E.K., Cooper C.L. Edward Elgar Publishing; Cheltenham (UK): 2011. Occupational health and safety in small and medium sized enterprises; pp. 1–6. [Google Scholar]
- 40.Tschan F., Vetterli M., Semmer N.K., Hunziker S., Marsch S.C. Activities during interruptions in cardiopulmonary resuscitation: a simulator study. Resuscitation. 2011;82:1419–1423. doi: 10.1016/j.resuscitation.2011.06.023. [DOI] [PubMed] [Google Scholar]


