Abstract
Background
Carpal tunnel syndrome (CTS) is a common work-related peripheral neuropathy. In addition to grip force and repetitive hand exertions, wrist posture (hyperextension and hyperflexion) may be a risk factor for CTS among workers. However, findings of studies evaluating the relationship between wrist posture and CTS are inconsistent. The purpose of this paper was to conduct a meta-analysis of existing studies to evaluate the evidence of the relationship between wrist posture at work and risk of CTS.
Methods
PubMed and Google Scholar were searched to identify relevant studies published between 1980 and 2012. The following search terms were used: “work related”, “carpal tunnel syndrome”, “wrist posture”, and “epidemiology”. The studies defined wrist posture as the deviation of the wrist in extension or flexion from a neutral wrist posture. Relative risk (RR) of individual studies for postural risk was pooled to evaluate the overall risk of wrist posture on CTS.
Results
Nine studies met the inclusion criteria. All were cross-sectional or case–control designs and relied on self-report or observer's estimates for wrist posture assessment. The pooled RR of work-related CTS increased with increasing hours of exposure to wrist deviation or extension/flexion [RR = 2.01; 95% confidence interval (CI): 1.646–2.43; p < 0.01: Shore-adjusted 95% CI: 1.32–2.97].
Conclusion
We found evidence that prolonged exposure to non-neutral wrist postures is associated with a twofold increased risk for CTS compared with low hours of exposure to non-neutral wrist postures. Workplace interventions to prevent CTS should incorporate training and engineering interventions that reduce sustained non-neutral wrist postures.
Keywords: carpal tunnel syndrome, meta-analysis, systematic review
1. Introduction
Carpal tunnel syndrome (CTS) is the most common form of work-related peripheral neuropathy among blue-collar workers who perform hand-intensive tasks [1–4]. In addition to grip force and hand repetition, wrist posture (sustained or repeated extension or flexion) may lead to an increased risk of CTS among workers [5,6]. However, the findings of previous studies evaluating the relationship between wrist posture and CTS are inconsistent. Silverstein et al [7] found that working with an awkward wrist posture is not a significant predictor of CTS, whereas Viikari-Juntura and Silverstein [8] reported a significant association between risk of CTS and awkward wrist posture.
Distal upper-extremity musculoskeletal injuries among workers are an important cause of work-related disability, cost, and reduced productivity. Common distal upper extremity injuries are medial/lateral epicondylitis (elbow), wrist tendonitis, and CTS. The CTS affects approximately 5 million workers in the United States [9] and the cost of medical care has been estimated to be over $2 billion annually [10]. In addition, these disorders impact the quality of workers' lives and may lead to job change [11].
The CTS occurs when the median nerve is compressed within the tight space of the carpal tunnel. Forceful hand-intensive work can lead to elevated pressures within the carpal tunnel and persistent tissue edema and nerve compression [6]. Keir et al [12,13] reported that the median nerve can be damaged due to high pressure on the carpal tunnel from extreme wrist extension or flexion. This physiological evidence supports a hypothesis that sustained awkward wrist postures may lead to CTS among workers. However, according to a 1997 National Institute of Occupational Science and Health (NIOSH) review, there was insufficient evidence to link sustained wrist deviation to CTS incidence [14].
The present meta-analysis reviews evidence of an association between CTS and wrist posture in epidemiologic studies. The main question addressed was whether or not there are consistent associations between CTS incidence and prolonged exposure to non-neutral wrist extension or flexion among workers.
2. Materials and methods
2.1. Search
For this meta-analysis, a systematic search was conducted using PubMed and Google Scholar for studies published from 1980 to 2011. The keywords of the search included “work related”, “carpal tunnel syndrome”, “wrist posture”, and “epidemiology”.
2.2. Inclusion and exclusion criteria
The following inclusion and exclusion criteria were used. Papers were published in English. Only epidemiological studies that used case–control, cohort, and cross-sectional designs were included; anecdotes or case series were excluded. Studies of office workers were excluded because their risks factors, sustained awkward postures, and contact stress, are substantially different from industrial work. Studies were excluded if they did not report the size of difference between the groups (effect size) with its 95% confidence interval (CI) and odds ratio (OR) or relative risk (RR) adjusted to age and gender. Studies were excluded if they did not report a quantitative or semiquantitative measure of exposure of wrist angle. A summary of inclusion and exclusion criteria is provided in Table 1. Nine studies met the inclusion criteria based on study design and exposure measurement methods.
Table 1.
Inclusion and exclusion criteria for study selection
| Inclusion | Exclusion |
|---|---|
| Study design: Case control, cross sectional, cohort | Anecdotes or case series |
| Participants: Workers | Unadjusted by age or gender |
| Outcome: CTS (measure of effect: OR and RR) | Missing RR and CI |
| Adjusted by age/gender | — |
| Measure of exposure to wrist posture | — |
| Published after 1980 | — |
| Article in English | — |
CI, confidence interval; CTS, carpal tunnel syndrome; OR, odds ratio; RR, relative risk.
2.3. Definition of outcome and exposure
A typical CTS case definition included: (1) the presence of paresthesia (numbness, tingling, burning, or pain) in the fingers of the median nerve distribution in the hand (one or more of the thumb, index, or middle finger) and (2) abnormal median nerve conduction test result consistent with CTS [15]. Some studies used both symptoms and abnormal nerve conduction tests to diagnose CTS, but two studies used just symptoms consistent with CTS.
The exposure variable of the reviewed studies was wrist deviation in extension or flexion from a neutral wrist posture or duration of time at work with the wrist in a non-neutral posture. Wrist posture was estimated by: (1) direct observation of workers performing their usual work; (2) direct measurement from videos of the workers performing their usual work; (3) worker self-report of wrist angle and time or frequency in non-neutral wrist postures; or (4) use of job title surrogate to infer the wrist posture.
2.4. Statistical analysis
This study pooled RR values between the reference groups and the highest exposure group of each study. Measures of effect (OR and RR), the 95% CI values, and sample size were summarized in tables. The summary effects of specific exposure risks were calculated using STATA, version 12 (StataCorp, College Station, TX, USA). A fixed-effects model was applied after a test for heterogeneity quantified by the Chi-square value and degree of freedom. Publication bias analysis was conducted using funnel plot and Egger test.
3. Results
The nine studies that met the inclusion criteria are summarized in Table 2. Six were cross-sectional and three were case–control study designs. The exposure assessment methods of wrist posture included direct observation, measurement from video of the job, job title surrogate, and self-reported (Table 3). The definition of the exposure groups varied between studies [16–18]. Five studies defined the exposure groups based on estimated specific wrist extension or flexion angles [16,17,19–21]. Two studies also defined the exposure groups based on working for a prolonged period with non-neutral posture [16,22]. The pooled RR from nine studies demonstrated positive associations of increased RR of CTS with increased exposure to wrist extension/flexion [Fig. 1; RR = 2.01 (1.66–2.43)].
Table 2.
Method of exposure assessment by study
| Study | Exposure assessment method | Definition of exposed group |
|---|---|---|
| Barnhart et al (1991) [19] | Job classification based on provided job list from the company | Exposed group: flexion, extension, or ulnar deviation >45° or radial deviation >30° (including repetitive movement, reference group: nonrepetitive job group) |
| de Krom et al (1990) [16] | Self-reported questionnaire |
Exposed: extended wrist angle 20–40 hours/week Reference: 0 hours/week |
|
Exposed: flexed wrist angle 20–40 hours/week Reference: 0 hours/week | ||
| English et al (1995) [18] | Self-reported questionnaire | Awkward wrist postures (Yes/No) |
| Feldman et al (1987) [17] | Self-reported questionnaire, video analysis confirmation (two random workers among the high-risk work group) | Neutral, extension, or flexion: >45°, 15°–45° |
| Marras and Schoenmarklin (1993) [20] | Measurement of wrist motions: position, angular velocity of movement and angular acceleration (goniometer) | Extension or Flexion (high risk vs. low risk group: dichotomized as a function of incidence risk) |
| Moore and Garg (1994) [3] | Observation (video analysis) | Hazardous job versus safe job (force, wrist position, grip, and pace of work) |
| Osorio et al (1994) [21] | Job classification (categories are ranked by CTS risk factors) | Wrist flexion/extension combined with high grasping force and repetition (reference group: repeated wrist flexion) |
| Tanaka et al (1995) [22] | Self-reported job title | Bending/twisting hand or wrist (Yes/No) |
CTS, carpal tunnel syndrome.
Table 3.
Studies included in the meta-analysis
| Study | Type∗ | Case definition for CTS†,‡ | Types of industry or occupation |
|---|---|---|---|
| Barnhart et al (1991) [19] | CS | Electrophysiologic study, physical examination criteria, and symptoms | Ski manufacturing |
| de Krom et al (1990) [16] | CC | Electrophysiologic study and symptoms (>twice/week) | Industry plant workers (reference group: general population) |
| de Krom et al (1990) | CC | Electrophysiologic study and symptoms (>twice/week) | Industry plant workers (reference group: general population) |
| English et al (1995) [18] | CC | Diagnosed as CTS case | Various occupations |
| Feldman et al (1987) [17] | CS | Electrophysiologic study, symptoms, and physical examination (sensation, finger grip, strength of the thenar muscle) | Electronic assembly workers |
| Marras and Schoenmarklin (1993) [20] | CS | Determined by US OSHA 200 log (diagnosed high-risk group) | Industrial plant workers |
| Moore and Garg (1994) [3] | CS | Electrophysiologic study and symptoms (from US OSHA logs and employee medical records) | Pork processing plant workers |
| Osorio et al (1994) [21] | CS | Electrophysiologic study or CTS symptoms | Grocery store workers |
| Tanaka et al (1995) [22] | CS | Symptoms; diagnosed as CTS case | Industry plant workers |
CTS, carpal tunnel syndrome; OSHA = Occupational Safety and Health Administration.
Type: CS: cross-sectional study CC: case–control study.
Physical examination criteria: Phalen's sign or Tinel's sign.
Symptoms: Numbness, tingling, burning in digits 1, 2, or 3.
Fig. 1.
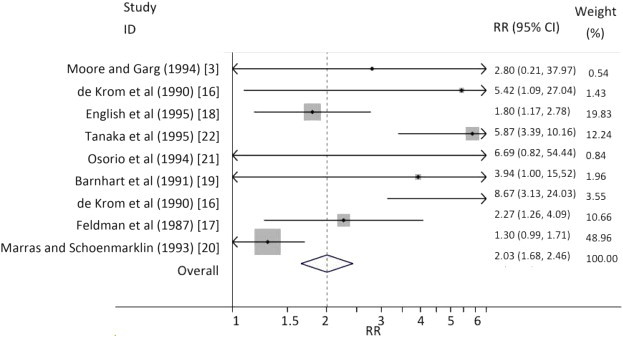
A forest plot of nine studies. The meta-analysis shows a twofold increase of CTS risk among workers of the risk group. Each line represents one study and horizontal lines indicate range of 95% CI. Solid circles indicate RR of the study. Statistical weight of the study is expressed by proportional size (gray boxes) based on sample size. Right column shows numerical value of forest plot. CI, confidence interval; CTS, carpal tunnel syndrome; RR, relative risk.
3.1. Selection bias
There were twice as many cross-sectional studies as case–control studies, and no cohort studies were identified. For the six cross-sectional studies, the pooled RR was 1.87 (1.50–2.32) (Table 4). For the three case–control studies, the pooled RR was 2.38 (1.63–3.48) (Table 4).
Table 4.
Summary showing individual studies and RR for the risk of CTS for the high-risk wrist angle group
| Study | RR | [95% LCI] | [95% UCI] | N | Effect size | [95% LCI] | [95% UCI] | % Weight |
|---|---|---|---|---|---|---|---|---|
| Barnhart et al (1991) [19] | 3.95 | 1.00 | 15.80 | 173 | 3.94 | 1.00 | 15.52 | 1.96 |
| de Krom et al (1990) [16] | 5.40 | 1.10 | 27.40 | 629 | 5.42 | 1.09 | 27.04 | 1.43 |
| de Krom et al (1990) [16] | 8.70 | 3.10 | 24.10 | 629 | 8.67 | 3.13 | 24.03 | 3.55 |
| English et al (1995) [18] | 1.80 | 1.20 | 2.80 | 1,167 | 1.80 | 1.17 | 2.78 | 19.83 |
| Feldman et al (1987) [17] | 2.26 | 1.40 | 4.46 | 586 | 2.27 | 1.26 | 4.09 | 10.66 |
| Marras and Schoenmarklin (1993) [20] | 1.30 | 1.00 | 1.70 | 40 | 1.30 | 0.99 | 1.71 | 48.96 |
| Moore and Garg (1994) [3] | 2.80 | 0.20 | 36.70 | 230 | 2.80 | 0.21 | 37.97 | 0.54 |
| Osorio et al (1994) [21] | 6.70 | 0.80 | 52.90 | 56 | 6.69 | 0.82 | 54.44 | 0.84 |
| Tanaka et al (1995) [22] | 5.90 | 3.40 | 10.20 | 127 Million | 5.87 | 3.39 | 10.16 | 12.24 |
| Pooled result | 2.01 | — | — | — | — | 1.66 | 2.43 | 100.00 |
CTS, carpal tunnel syndrome; LCI, lower confidence interval; RR, relative risk; UCI, upper confidence interval.
3.2. Information bias
Information bias was evaluated and may be influenced by exposure assessment methods. The pooled RRs for studies with common exposure assessment methods were: (1) self-report exposure studies [RR = 2.95 (2.24–3.89) p < 0.005], and (2) observational exposure studies [RR = 1.44 (1.13–1.83) p < 0.005].
3.3. Confounding bias
None of the studies separately evaluated the relationships between exposure to wrist posture and exposures to other biomechanical factors such as applied hand force or repetition rate. Therefore, confounding bias may exist. That is, RR will be increased if expose to non-neutral wrist postures occurred with forceful or highly repetitive work or RR may decrease in the opposite situation. There was no way to estimate whether an important confounding factor was present or not.
3.4. Consistency of findings
The heterogeneity test result of nine studies showed χ2 = 37.06 (p < 0.01). However, all studies demonstrated a positive association between CTS and increased exposure to non-neutral wrist posture. The pooled RR of the random effects model is 3.13 (95% CI: 1.84–5.33; Shore-adjusted 95% CI: 1.32–2.97.)
3.5. Publication bias
Seven studies are located on the right side of funnel graph and its risk estimations are clustered near the pooled RR estimate. However, only two studies are on the left top side of the funnel plot and smaller size studies with increased risks or reduced risks seem to be missing. The asymmetrical funnel plot indicates a potential publication bias (Fig. 2) [23] and also shows evidence of a small study effect root-mean-square error of 1.62 (p = 0.04; Fig. 3).
Fig. 2.
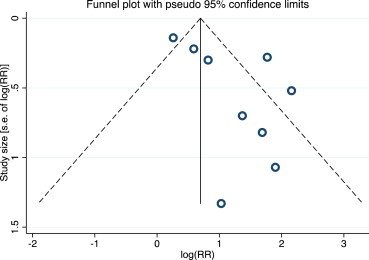
A funnel plot of log risk ratio (RR) of the incidence in the studies of carpal tunnel syndrome among workers is used for explorative tool to inspect publication bias. The plot shows treatment effects versus the study size that is estimated from standard error (s.e.) of log(RR). Open circles indicate individual studies in this meta-analysis. The broken line is pseudo 95% confidence interval of measure of effect in the study. The asymmetrical plot indicates smaller studies with stronger effects missing. RR, relative risk.
Fig. 3.
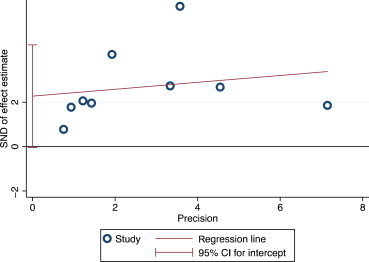
An Egger plot that shows regression of RR difference of each study over standard error. Precision is estimated from inverse of standard error. The intercept of regression line is suggestive for publication bias; 2.14 [standard error: 0.85; p = 0.04, 95% confidence interval (CI) 0.18–4.11]. RR, relative risk; SND, standardize.
4. Discussion
This systematic review has found evidence for an association between non-neutral wrist posture in extension or flexion and work-related CTS. The overall risk of CTS was two times that in workers exposed to non-neutral postures compared with controls. The level of evidence was tested by examining: (1) the heterogeneity of the identified studies, (2) the pooled RR analysis, (3) the pattern of the forest plot, (4) the shape of the funnel plot for publication bias, and (5) Egger test for small study effects. Overall, the findings were consistent and the effect sizes moderate.
These findings match previous reviews that found more than a twofold increased risk of CTS among workers working under non-neutral wrist posture for prolonged periods during the workday [24–26]. New studies have been published since the NIOSH review in 1997, which, if incorporated into a repeated review process today, would likely change the conclusions on the NIOSH review to a positive association with wrist posture.
Several limitations to the review should be noted. None of the studies reviewed were prospective in design. In four studies, exposure assessment was based on worker recollection of wrist posture, and therefore, there may be a recall bias. Subgroup analysis of self-reported studies showed higher RR than the pooled study or observational studies' RR. Exposure recall bias is likely to bias the findings away from the null because cases may have formed opinions about wrist posture and their CTS. However, a review examined the extent of recall bias for exposure assessment, considering different interviewing technique, study protocol, and questionnaire design, and reported limited evidence of recall bias [27]. Interestingly, the observational studies showed lower pooled RR than the entire studies' pooled RR value. That might cause moderate pooled RR value of nine studies compared with two subgroups' RR values. Differences in CTS case definition are a potential limitation. Marras and Schoenmarklin [20] and English et al [18] identified CTS cases from the Occupational Safety and Health Administration (OSHA) log whereas other studies used the case definition of an abnormal electrophysiology test and symptoms in the median nerve distribution. It is possible that the use of the OSHA log would lead to more case than expected due to overdiagnosis. As it was described in the including criteria, the CTS case was defined by different methods through the identified studies. Using unified CTS case definition significantly decreases the number of possible papers to review. Therefore, papers that applied the generally accepted CTS case diagnosis method were pooled for the meta-analysis. However, only one study used median nerve symptoms as a case definition in our meta-analysis. Other studies used median nerve symptoms, nerve conduction test, and physical test as its case definition criteria. Therefore, effect of case misclassification bias must be subtle in this meta-analysis.
The reviewed studies also used different methods for wrist posture assessment and different thresholds for high exposure and low exposure. Among the nine studies, four studies defined the exposed group as “deviated (twisted), extended, or flexed (bended) wrist angle” in categorical format (e.g., Yes and No). Two studies used specific wrist angles to define the exposure groups (for flexion and extension >45°, 15°–45°; for ulnar deviation >45°; or for radial deviation >30°). Two studies defined the exposure groups based on the self-reported time spent performing work with the wrist in extension or flexion. Another limitation may be the effect of confounding exposure factors. In at least one study [21], non-neutral wrist posture was combined with forceful work in the high-exposure group; therefore, wrist posture was not examined as an independent variable. It is not clear how exposure misclassification differed between methods, but it is likely that misclassification was not systematic and would, therefore, bias toward the null.
Overall, the studies reviewed provide evidence of an association between non-neutral wrist posture in extension/flexion and CTS. Future studies should evaluate this risk using prospective study designs with exposure estimates at the individual level considering both posture deviation from neutral and duration of non-neutral posture over the workday. To reduce the risk for CTS among workers who perform hand-intensive tasks, employers should consider job and tool modifications and employee education that reduce the duration of exposure to non-neutral wrist postures.
Conflicts of interest
The authors have no conflicts of interest relevant to this article.
Acknowledgments
We thank Dr Craig Steinmaus for his support with the statistical analysis.
Footnotes
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
References
- 1.Stapleton M.J. Occupation and carpal tunnel syndrome. ANZ J Surg. 2006;76:494–496. doi: 10.1111/j.1445-2197.2006.03770.x. [DOI] [PubMed] [Google Scholar]
- 2.Harris C., Eisen E.A., Goldberg R., Krause N., Rempel D. 1st place, PREMUS best paper competition: workplace and individual factors in wrist tendinosis among blue-collar workers—the San Francisco study. Scand J Work Environ Health. 2011;37:86–98. doi: 10.5271/sjweh.3147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Moore J.S., Garg A. Upper extremity disorders in a pork processing plant: relationships between job risk factors and morbidity. Am Ind Hyg Assoc J. 1994;55:703–715. doi: 10.1080/15428119491018592. [DOI] [PubMed] [Google Scholar]
- 4.Burt S., Crombie K., Jin Y., Wurzelbacher S., Ramsey J., Deddens J. Workplace and individual risk factors for carpal tunnel syndrome. Occup Environ Med. 2011;68:928–933. doi: 10.1136/oem.2010.063677. [DOI] [PubMed] [Google Scholar]
- 5.Rempel D., Keir P.J., Smutz W.P., Hargens A. Effects of static fingertip loading on carpal tunnel pressure. J Orthop Res. 1997;15:422–426. doi: 10.1002/jor.1100150315. [DOI] [PubMed] [Google Scholar]
- 6.Rempel D., Dahlin L., Lundborg G. Pathophysiology of nerve compression syndromes: response of peripheral nerves to loading. J Bone Joint Surg Am. 1999;81:1600–1610. doi: 10.2106/00004623-199911000-00013. [DOI] [PubMed] [Google Scholar]
- 7.Silverstein B.A., Fine L.J., Armstrong T.J. Occupational factors and carpal tunnel syndrome. Am J Ind Med. 1987;11:343–358. doi: 10.1002/ajim.4700110310. [DOI] [PubMed] [Google Scholar]
- 8.Viikari-Juntura E., Silverstein B. Role of physical load factors in carpal tunnel syndrome. Scand J Work Environ Health. 1999;25:163–185. doi: 10.5271/sjweh.423. [DOI] [PubMed] [Google Scholar]
- 9.Luckhaupt S.E., Dahlhamer J.M., Ward B.W., Sweeney M.H., Sestito J.P., Calvert G.M. Prevalence and work-relatedness of carpal tunnel syndrome in the working population, United States, 2010 National Health Interview Survey. Am J Ind Med. 2013;56:615–624. doi: 10.1002/ajim.22048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dale A.M., Harris-Adamson C., Rempel D., Gerr F., Hegmann K., Silverstein B., Burt S., Garg A., Kapellusch J., Merlino L., Thiese M.S., Eisen E.A., Evanoff B. Prevalence and incidence of carpal tunnel syndrome in US working populations: pooled analysis of six prospective studies. Scand J Work Environ Health. 2013;39:495–505. doi: 10.5271/sjweh.3351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Turner J.A., Franklin G., Heagerty P.J., Wu R., Egan K., Fulton-Kehoe D., Gluck J.V., Wickizer T.M. The association between pain and disability. Pain. 2004;112:307–314. doi: 10.1016/j.pain.2004.09.010. [DOI] [PubMed] [Google Scholar]
- 12.Keir P.J., Wells R.P., Ranney D.A., Lavery W. The effects of tendon load and posture on carpal tunnel pressure. J Hand Surg Am. 1997;22:628–634. doi: 10.1016/S0363-5023(97)80119-0. [DOI] [PubMed] [Google Scholar]
- 13.Keir P.J., Bach J.M., Rempel D.M. Effects of finger posture on carpal tunnel pressure during wrist motion. J Hand Surg Am. 1998;23:1004–1009. doi: 10.1016/S0363-5023(98)80007-5. [DOI] [PubMed] [Google Scholar]
- 14.NIOSH . NIOSH (National Institute of Occupational Safety and Health); 1997. Musculoskeletal disorders and workplace factors: a critical review of epidemiologic evidence for work-related musculoskeletal disorders of the neck, upper extremity, and low back; pp. 97–141. [Google Scholar]
- 15.Rempel D., Evanoff B., Amadio P.C., de Krom M., Franklin G., Franzblau A., Gray R., Gerr F., Hagberg M., Hales T., Katz J.N., Pransky G. Consensus criteria for the classification of carpal tunnel syndrome in epidemiologic studies. Am J Public Health. 1998;88:1447–1451. doi: 10.2105/ajph.88.10.1447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.de Krom M.C., Kester A.D., Knipschild P.G., Spaans F. Risk factors for carpal tunnel syndrome. Am J Epidemiol. 1990;132:1102–1110. doi: 10.1093/oxfordjournals.aje.a115753. [DOI] [PubMed] [Google Scholar]
- 17.Feldman R.G., Travers P.H., Chirico-Post J., Keyserling W.M. Risk assessment in electronic assembly workers: carpal tunnel syndrome. J Hand Surg Am. 1987;12:849–855. doi: 10.1016/s0363-5023(87)80247-2. [DOI] [PubMed] [Google Scholar]
- 18.English C.J., Maclaren W.M., Court-Brown C., Hughes S.P., Porter R.W., Wallace W.A., Graves R.J., Pethick A.J., Soutar C.A. Relations between upper limb soft tissue disorders and repetitive movements at work. Am J Ind Med. 1995;27:75–90. doi: 10.1002/ajim.4700270108. [DOI] [PubMed] [Google Scholar]
- 19.Barnhart S., Demers P.A., Miller M., Longstreth W.T., Jr., Rosenstock L. Carpal tunnel syndrome among ski manufacturing workers. Scand J Work Environ Health. 1991;17:46–52. doi: 10.5271/sjweh.1735. [DOI] [PubMed] [Google Scholar]
- 20.Marras W.S., Schoenmarklin R.W. Wrist motions in industry. Ergonomics. 1993;36:341–351. doi: 10.1080/00140139308967891. [DOI] [PubMed] [Google Scholar]
- 21.Osorio A.M., Ames R.G., Jones J., Castorina J., Rempel D., Estrin W., Thompson D. Carpal tunnel syndrome among grocery store workers. Am J Ind Med. 1994;25:229–245. doi: 10.1002/ajim.4700250209. [DOI] [PubMed] [Google Scholar]
- 22.Tanaka S., Wild D.K., Seligman P.J., Halperin W.E., Behrens V.J., Putz-Anderson V. Prevalence and work-relatedness of self-reported carpal tunnel syndrome among U.S. workers: analysis of the Occupational Health Supplement data of 1988 National Health Interview Survey. Am J Ind Med. 1995;27:451–470. doi: 10.1002/ajim.4700270402. [DOI] [PubMed] [Google Scholar]
- 23.Sterne J.A.C., Harbord R.M. Funnel plots in meta-analysis. Stata J. 2004;4:127–141. [Google Scholar]
- 24.Palmer K.T., Harris E.C., Coggon D. Carpal tunnel syndrome and its relation to occupation: a systematic literature review. Occup Med (Lond) 2007;57:57–66. doi: 10.1093/occmed/kql125. [DOI] [PubMed] [Google Scholar]
- 25.van Rijn R.M., Huisstede B.M., Koes B.W., Burdorf A. Associations between work-related factors and the carpal tunnel syndrome—a systematic review. Scand J Work Environ Health. 2009;35:19–36. doi: 10.5271/sjweh.1306. [DOI] [PubMed] [Google Scholar]
- 26.Barcenilla A., March L.M., Chen J.S., Sambrook P.N. Carpal tunnel syndrome and its relationship to occupation: a meta-analysis. Rheumatology (Oxford) 2012;51:250–261. doi: 10.1093/rheumatology/ker108. [DOI] [PubMed] [Google Scholar]
- 27.Coughlin S.S. Recall bias in epidemiologic studies. J Clin Epidemiol. 1990;43:87–91. doi: 10.1016/0895-4356(90)90060-3. [DOI] [PubMed] [Google Scholar]


