Abstract
The study was to assess the correlates for recent HIV testing and HIV/AIDS-related stigmatizing and discriminatory attitudes among men who have sex with men (MSM) in Beijing, China. A cross-sectional study probed demographics, sexual and drug use behaviors, HIV testing, and prevention services. Of 500 participants, 39.3% recently received a test for HIV. Recent testing was independently associated with expressing lower levels of HIV/AIDS-related stigmatizing and discriminatory attitudes, more male sex partners, no female sexual partners and knowing HIV status of their last male partner. Expressing lower levels of HIV/AIDS-related stigmatizing and discriminatory attitudes was independently associated with recent testing, younger age, and knowing HIV status of their last male partner. This study revealed that HIV/AIDS-related stigmatizing and discriminatory attitudes were common and inversely associated with recent HIV testing. Low levels of testing highlighted the urgent needs to reduce HIV/AIDS-related stigma and discrimination and expand HIV testing among Beijing MSM.
Keywords: HIV/AIDS, stigma, discrimination, testing, men who have sex with men
Introduction
As the epidemic has been evolved over 3 decades, stigma and discrimination has been a barrier to HIV prevention and care. The effect of stigma and discrimination on people’s ability to access HIV testing, counseling, diagnosis, care, treatment, and prevention messages varies from setting to setting, but when present, stigma and discrimination can create an environment where people may avoid HIV-related services. HIV continues to spread among men who have sex with men (MSM) on a global level (van Griensven, de Lind van Wijngaarden, Baral, & Grulich, 2009). A literature review revealed that gay men in low and middle income countries have 19.3 (95%CI: 18.8 to 19.8) times higher odds of having HIV compared with general population (Baral, Sifakis, Cleghorn, & Beyrer, 2007). MSM contributed to about half of new HIV infections in many Western countries (Boer IM, Op de Coul, Koedijk, Veen MG, Sighem AI, & Laar MJW,; Hall, Song, Rhodes, Prejean, An, Lee et al., 2008). In China, MSM contributed to a third (33%) of recent estimated new HIV infections in 2009 (Raymond HF, 2007), which was near tripled the estimated number (12%) in 2007. A rapid rise in the prevalence of HIV infection among MSM was observed in recent years in many cities in China, e.g., the prevalence rates among Beijing MSM were increased from 0.4% in 2004 to 5.8% in 2006, and 8.0% in 2009 (X. Ma, Zhang, He, Sun, Yue, Chen et al., 2007b).
HIV testing plays a critical role in containing the epidemic. HIV testing and counseling can help reduce risk behaviors (Leaity, Sherr, Wells, Evans, Miller, Johnson et al., 2000; Weinhardt, Carey, Johnson, & Bickham, 1999), and HIV testing could lead to early diagnosis and timely prevention, linkage-to-care and medical treatment (Janssen, Holtgrave, Valdiserri, Shepherd, Gayle, & De Cock, 2001; Valdiserri, Holtgrave, & West, 1999). However, stigma and discrimination have been identified as major barriers to uptake HIV-related prevention services (Agwu & Ellen, 2009; Mahajan, Sayles, Patel, Remien, Sawires, Ortiz et al., 2008; UNAIDS, Dec 2003). HIV/AIDS-related stigma and discrimination can adversely influence decisions to seek HIV testing (Chesney & Smith, 1999; Kalichman & Simbayi, 2003). Previous studies mainly focused on assessing HIV/AIDS-related stigma and discrimination as perceived experience of HIV-infected individuals (Abadia-Barrero & Castro, 2006; Rahmati-Najarkolaei, Niknami, Aminshokravi, Bazargan, Ahmadi, Hadjizadeh et al., 2010; Thi, Brickley, Vinh, Colby, Sohn, Trung et al., 2008) or assessing the attitudes of the general population against people living with HIV/AIDS (Herek, Capitanio, & Widaman, 2002; Letamo, 2003; Unnikrishnan, Mithra, T, & B, 2010), but limited data are available in assessing the prejudicial attitudes among the MSM community towards PLWHA. HIV-related stigma/discrimination is common in the MSM community (Courtenay-Quirk, Wolitski, Parsons, & Gomez, 2006; Flowers, Duncan, & Frankis, 2000). It is critical to investigate HIV/AIDS related stigma and discrimination among MSM and its impact on seeking HIV testing in containing the epidemic. This study was to assess correlates for recent HIV testing and stigmatizing and discriminatory attitudes towards PLWHA among Beijing MSM.
Methods
Study Participants
A cross-sectional study was conducted among MSM in September and October 2009 in an outpatient clinic affiliated to Beijing Centers for Disease Control and Prevention (CDC). Individuals were eligible for the study if they (1) identified as male, (2) were 18 years of age or older, (3) reported living in Beijing, (4) reported oral, anal sex, or mutual masturbation with a man in the past 12 months, (5) had a valid study recruitment coupon, (6) had not previously participated in the survey, and (7) were able to provide written informed consent. Each study participant was screened for study eligibility prior to enrollment. The study was approved by the Committees for Human Research of the National Center for AIDS of the China CDC, Vanderbilt University and the University of California San Francisco.
Recruitment
Respondent-driven sampling (RDS) was used to recruit MSM participants. Seven seeds were selected from bar, bathroom, park, Internet, grassroots organization, and peer referral. Seeds were selected based on their commitment to recruit 3 eligible peers within their social network, in addition to key demographic characteristics and risk behaviors necessary to ensure diverse sample representation. Each seed received 3 recruitment coupons to recruit MSM peers from their network. The coupon included the project name, address and phone number of the interview site, study identification number, and expiration date. A unique serial number on each coupon linked each subject to his recruiters. The recruits of the seeds also received 3 coupons for additional recruitment. Both seeds and recruited participants received incentives, both to be interviewed (US $4 as “primary incentives”) and to refer additional recruits (US $3 as “secondary incentives”).
Measures
After eligibility screening and obtaining informed consent, each participant received a 20 minute computer-assisted interview. The questionnaire asked participants about general demographics, sexual and drug use behaviors, HIV testing history, and stigmatizing and and discriminatory attitudes towards PLWHA.
(1) Demographics, Sexual Risk Behaviors
Demographic questions included age, ethnicity, education, marital status, employment, sexual orientation, and Beijing residence status. Risk behavior measures included ever engaging in unprotected sexual intercourse, history of substance use (e.g., alcohol or drugs), disclosure of sexual orientation, and the number of male and female sexual partners.
(2) HIV Testing Behaviors
All participants were asked if they had ever tested for HIV and, if applicable, the number of prior tests, and the date and results of their most recent test. Recent testers were defined as participants received a test for HIV in the past year.
(3) HIV/AIDS-Related Stigma and Discrimination
Individual attitudes towards PLWHA were measured by asking participants about their agreement and disagreement (1=‘yes’, 2=‘no’) with 22 statements. The scale was adapted from two pilot investigations conducted in Thailand and Zimbabwe.(Genberg, Kawichai, Chingono, Sendah, Chariyalertsak, Konda et al., 2008) This scale measured 3 dimensions of HIV/AIDS-related stigma and discrimination: shame, blame, and social isolation; perceived discrimination; and equity. The scale included such questions as “People living with HIV/AIDS should be ashamed”; “People living with HIV/AIDS face neglect from their family”; “People living with HIV/AIDS do not deserve any support”. Items were summed to create total scale scores, with a range of 22-44 (some items were reverse-scored so that a higher score indicates a lower level of HIV/AIDS-related stigma and discrimination). Acceptable reliability was supported by an alpha value of 0.83.
(4) Laboratory Testing
Serum samples were screened for HIV-1 antibodies by enzyme-linked immunosorbent assay (ELISA; Vironostika HIV Uni-Form plus O, bioMerieux, Holland) and confirmed as positive by Western Blot test (HIV Blot 2.2 WBTM, Genelabs Diagnostics). Syphilis screening was performed by rapid plasma regain (RPR; Shanghai Rongsheng, Shanghai, China) and confirmed by Treponemapallidum particle assay test (TPPA; Fujirebioinc, Japan).
Statistical Analyses
Respondent-Driven Sampling Analysis Tool (RDSAT 5.6, Cornell University, Ithaca, NY, USA) was used to generate weighted point estimates and 95% confidence intervals (95%CI) (Volz, Wejnert, Degani, & Heckathorn, 2007). Statistical Analysis Software (SAS 9.1 for Windows; SAS Institute Inc, Cary, NC) was used for all analyses. Univariate and multivariable analysis were conducted after assigning cases individual weights for recent HIV testing and HIV/AIDS-related stigma and discrimination which were exported from RDSAT. The factors associated with recent testing were assessed using a univariate analysis, then multivariable logistic regression analysis. Odds ratios (ORs) and 95%CIs were calculated in the multiple logistic regression analysis using a stepwise method. Statistical significance was determined at p<0.05 in the final model. The weighted mean scale scores of HIV-related stigma and discrimination were first calculated for each variable level. Subsequently, simple and multiple linear regression analysis were applied to determine which predictors (demographic factors, sexual behaviors, recent testing) were independently associated with total scale scores after controlling for all potential confounders.
Results
Characteristics of Participants
A total of 500 MSM were recruited and interviewed. About half (50.4%) of them were younger than 30 years old, more than two-third (68.1%) received high school or higher levels of education, 79.9% were employed with a full time job, 61.7% self-identified as homosexual, 41.8% had three or more male partners, 25.8% had female sexual partners, and 22.8% knew HIV status of their last male partner.
Sexual and Substance Use Behaviors
The rates of unprotected insertive or receptive anal sex with their last male partner in the past 6 months were 34.8% and 40.5%, respectively. Of the participants, 0.1% had used drugs in the past 12 months. Of those who had sex with females, 80.0% had unprotected sex with female sexual partner in the past 6 months (Table 1).
Table 1. Recent HIV testing, stigmatizing and discriminatory attitudes towards people living with HIV/AIDS among men who have sex with men, Beijing, 2009.
| Variable | Total | HIV testing in P12M | Stigma/discrimination | ||
|---|---|---|---|---|---|
|
|
|||||
| N | Weighted % (95%CI) |
N | Weighted % (95%CI) |
Weighted Mean (95%CI) |
|
| Age (years) | Median: 29; range from 18 to 71 | ||||
| 18-29 | 268 | 50.4(42.8-58.1) | 145 | 40.6(33.1-50.1) | 37.7(37.2-38.1) |
| 30-71 | 232 | 49.6(41.9-57.2) | 121 | 37.8(29.4-48.3) | 35.9(35.5-36.3) |
| Education | |||||
| Middle school and lower | 163 | 31.5(25.4-38.1) | 74 | 30.5(22.0-41.4) | 35.5(34.9-36.1) |
| High school or higher | 337 | 68.5(61.9-74.6) | 192 | 43.9(36.3-52.6) | 37.4(37.0-37.8) |
| Current marital status | |||||
| Married | 104 | 27.2(20.8-36.0) | 45 | 28.7(17.5-41.5) | 35.7(35.0-36.4) |
| Unmarried | 396 | 72.8(64.0-79.2) | 221 | 42.3(36.6-50.9) | 37.2(36.8-37.6) |
| Employment status | |||||
| Full time | 406 | 79.9(74.1-85.4) | 218 | 43.1(37.4-52.1) | 36.8(36.5-37.2) |
| Part time, student, unemployed, or retired | 94 | 20.1(14.5-25.9) | 48 | 23.6(13.1-36.2) | 36.7(35.9-37.6) |
| Monthly income (U.S. dollar), P12M | |||||
| <150 | 105 | 23.8(17.6-29.5) | 47 | 20.1(11.1-31.2) | 36.3(35.5-37.2) |
| ≥150 | 395 | 76.2(70.5-82.4) | 219 | 44.1(38.2-52.9) | 36.9(36.6-37.3) |
| Have health insurance | |||||
| Yes | 236 | 45.6(39.3-52.6) | 126 | 39.8(31.1-50.3) | 37.4(37.0-37.8) |
| No | 264 | 54.4(47.4-60.7) | 140 | 38.4(31.1-47.7) | 36.3(35.8-36.8) |
| Self-reported sexual orientation | |||||
| Homosexual | 346 | 61.7(55.4-68.3) | 188 | 41.4 (34.7-50.0) | 36.6(36.2-37.0) |
| Bisexual, straight, or undecided | 154 | 38.3(31.9-44.4) | 78 | 34.3(25.0-44.7) | 37.1(36.5-37.7) |
| No. of male partners, P6M | |||||
| <3 | 236 | 58.2(50.6-63.8) | 114 | 36.2 (27.9-43.9) | 37.1(36.6-37.5) |
| ≥3 | 264 | 41.8(36.2-49.4) | 152 | 44.5 (37.3-55.7) | 36.4(36.0-36.9) |
| Had female sexual partner, P6M | |||||
| Yes | 104 | 25.8(19.3-31.6) | 46 | 22.7(14.9-32.8) | 36.4(35.7-37.0) |
| No | 396 | 74.2(68.4-80.6) | 220 | 45.2(38.7-53.6) | 36.9(36.6-37.3) |
| Type of last male partner, P6M | |||||
| Regular partner | 309 | 60.8(53.8-67.8) | 169 | 45.4 (38.8-54.8) | 36.9(36.5-37.3) |
| Casual partner | 179 | 39.2(32.2-46.2) | 90 | 30.8 (22.5-41.1) | 36.7(36.2-37.3) |
| Found male sex partners through Internet | |||||
| Yes | 189 | 38.1(32.2-47.0) | 109 | 49.1 (40.8-60.6) | 37.9(37.4-38.4) |
| No | 296 | 61.9(53.0-67.8) | 149 | 33.8(25.2-40.9) | 36.1(35.7-36.5) |
| Unprotected insertive anal sex with last male partner, P6M |
|||||
| Yes | 127 | 34.8(28.2-41.6) | 58 | 37.8(27.3-50.1) | 36.8(36.1-37.5) |
| No | 220 | 65.2(58.1-72.1) | 127 | 42.8(34.0-51.9) | 36.8(36.3-37.3) |
| Unprotected receptive anal sex with last male partner, P6M |
|||||
| Yes | 115 | 40.5(31.3-48.4) | 51 | 32.9(21.5-45.3) | 37.4(36.8-38.0) |
| No | 170 | 59.5(51.7-68.5) | 99 | 35.8(26.1-46.2) | 36.9(36.3-37.4) |
| Venue of sex with last male partner, P6M | |||||
| Bathhouse/ Sauna/ Park/ Public rest room | 60 | 13.9(8.9-18.0) | 26 | 25.3(15.1-41.8) | 35.7(34.7-36.7) |
| Residence / Bar / Club/ Hotel | 428 | 86.1(82.0-91.1) | 233 | 41.7 (34.6-48.7) | 37.0(36.7-37.4) |
| Known HIV status of last male sex partner | |||||
| Yes | 129 | 22.8(18.1-28.3) | 88 | 58.0(44.5-69.8) | 37.7(37.2-38.2) |
| No | 359 | 77.2(71.8-81.9) | 171 | 34.2(28.0-41.9) | 36.6(36.2-37.0) |
| Disclosed HIV status with last male partner | |||||
| Yes | 236 | 45.6(38.5-52.1) | 143 | 46.2(36.3-55.6) | 37.4(37.0-37.8) |
| No | 252 | 54.4(47.6-61.0) | 116 | 33.6 (26.8-43.1) | 36.4(35.9-36.9) |
| Unprotected sex with female partner, P6M | |||||
| Yes | 75 | 79.6(66.5-97.9) | 31 | 10.9(0.3-28.2) | 36.3(35.4-37.1) |
| No | 29 | 20.4(2.1-33.0) | 15 | 40.8(0-100.0) | 36.7(35.8-37.6) |
| Ever got drunk | |||||
| Yes | 152 | 47.3(36.8-57.0) | 74 | 37.4(25.3-50.7) | 36.8(36.2-37.3) |
| No | 167 | 52.7(43.0-63.2) | 94 | 42.9(33.2-61.7) | 36.3(35.7-37.0) |
| Received free condoms/lubricant, P12M | |||||
| Yes | 436 | 78.0(72.8-84.5) | 256 | 49.2 (42.1-57.0) | 36.8(36.5-37.2) |
| No | 64 | 22.0(15.4-27.2) | 10 | 9.1 (3.0-17.0) | 36.7(35.7-37.7) |
| Fear of knowing HIV-positive testing result | |||||
| Yes | 413 | 83.6(79.2-87.7) | 218 | 37.2 (31.0-44.5) | 36.8(36.5-37.2) |
| No | 87 | 16.4(12.3-20.8) | 48 | 50.5 (36.1-64.0) | 36.6(35.6-37.5) |
| Known where to get HIV test | |||||
| Yes | 470 | 89.0(83.8-94.3) | 263 | 43.4(37.2-50.7) | 36.9(36.6-37.2) |
| No | 29 | 11.0(6.0-15.9) | 3 | 3.8(0-11.3) | 35.7(34.0-37.4) |
| Stigmatizing and discriminatory attitudes | 500 | NA | 1.1(1.0-1.1) | NA | |
| Ever tested for HIV | |||||
| Yes | 334 | 51.4(43.8-58.4) | NA | 37.2(36.8-37.6) | |
| No | 166 | 48.6(41.4-56.6) | 36.3(35.7-36.9) | ||
| Received a test for HIV, P12M | |||||
| Yes | 266 | 39.3(33.2-46.3) | NA | 37.2(36.8-37.7) | |
| No | 234 | 60.7(53.8-66.8) | 36.5(36.0-37.0) | ||
| Drug use, P12M | 4 | 0.1(0-0.1) | 3 | 41.2(0-100.0) | 37.3(35.3-39.4) |
| HIV positive | 36 | 8.0(4.7-12.0) | 16 | 33.1(15.7-51.9) | 37.0(35.9-38.1) |
| Syphilis positive | 110 | 22.0(16.8-27.3) | 59 | 35.8(24.9-50.1) | 37.4(36.7-38.0) |
Note: The subtotals may not add up to 500 due to missing values; Recent HIV testing indicated the participants have ever received a test for HIV in the past 12 months; P12M: in the past 12 months; P6M: in the past 6 months; NA: not applicable.
HIV Testing and HIV/AIDS-related Stigma and Discrimination
Of the participants, 39.3% received a recent HIV test and a third (33.2%) had never received a test for HIV in the past 12 months. The weighted prevalence of HIV was 8.0% (95%CI: 4.7-12.0%) with 86.1% of them unaware of their infection, syphilis was at 22.0% (95%CI: 16.8-27.3%) (Table 1).
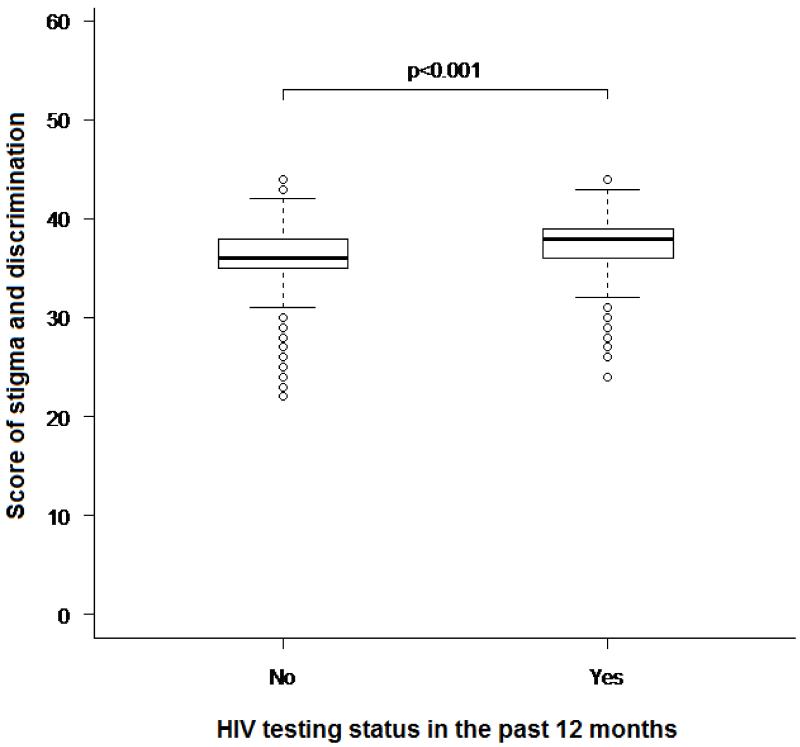
A comparison of stigma and discrimination scores for recent HIV testers and non-recent testers indicated that recent testers among had significant higher score of stigma and discrimination (p<0.001), expressing as lower negative attitudes towards PLWHA, than non-recent testers (Fig. 1).
Fig. 1.
Comparison of the degree of stigma and discriminaiton between participants ever received and never received a test for HIV in the past 12 months
Correlates for Recent HIV Testing
Univariate analysis revealed that MSM who had a higher education level, were unmarried, sought male sex partners through the Internet, had sex with their last male partner in low-risk places, knew HIV status of their last male partner, and disclosed HIV status with their last male partner were more likely to have recently received a test for HIV (Table 2). Multivariable logistic regression analysis indicated that recent HIV testing was associated with lower levels of HIV/AIDS-related stigma and discrimination (AOR=1.1, 95%CI: 1.0-1.2), having ≥3 male partners in the past 6 months (AOR=1.9, 95%CI: 1.1-3.3), having no female sexual partners in the past 6 months (AOR=3.0, 95%CI: 1.6-5.8), and knowing the HIV status of their last male partner (AOR=3.6, 95%CI: 1.9-6.5).
Table 2. Correlates of recent HIV testing among men who have sex with men, Beijing, 2009.
| Variable | B | Wald χ2 | OR(95%CI) | P | β | Wald χ2 | AOR(95%CI) | P |
|---|---|---|---|---|---|---|---|---|
| Higher level education (vs < high school) | 0.6 | 8.245 | 1.8(1.2-2.7) | 0.004 | ||||
| Married | −0.5 | 6.118 | 0.6(0.4-0.9) | 0.013 | ||||
| Full time employed | 0.7 | 8.572 | 2.1(1.3-3.4) | 0.003 | ||||
| Monthly income (≥150 U.S. dollar) | 1.0 | 17.003 | 2.7(1.7-4.3) | <0.001 | ||||
| Had ≥3 male partners, P6M | 0.4 | 5.031 | 1.5(1.1-2.2) | 0.025 | 0.7 | 5.960 | 1.9(1.1-3.3) | 0.015 |
| Had no female sexual partner, P6M | 1.1 | 21.283 | 3.0(1.9-4.8) | <0.001 | 1.1 | 11.294 | 3.0(1.6-5.8) | 0.001 |
| Casual partner, P6M | −0.5 | 7.439 | 0.6(0.4-0.9) | 0.006 | ||||
| Found male sex partners through Internet | 0.6 | 9.596 | 1.8(1.2-2.6) | 0.002 | ||||
| Sex with last male partner at Bathhouse/ Sauna/ Park/ Public rest room, P6M |
−0.7 | 5.506 | 0.5(0.3-0.9) | 0.019 | ||||
| Knew HIV status of last male partner | 0.5 | 16.975 | 2.5(1.6-3.8) | <0.001 | 0.6 | 16.755 | 3.6(1.9-6.5) | <0.001 |
| Disclosed HIV status w/ last male partner | 0.2 | 7.023 | 1.6(1.1-2.4) | 0.008 | ||||
| Unprotected sex with female partner, P6M | −0.8 | 3.382 | 0.4(0.2-1.1) | 0.066 | ||||
| Ever got drunk | −0.6 | 6.900 | 0.5(0.3-0.9) | 0.009 | ||||
| Received free condoms/lubricant, P12M | 1.2 | 43.402 | 10.5(5.2-21.2) | <0.001 | ||||
| Fear of knowing HIV-positive result | −0.3 | 5.166 | 0.6(0.4-0.9) | 0.023 | ||||
| Lower level of stigma and discrimination (continuous scale) |
0.1 | 4.274 | 1.1(1.0-1.1) | 0.039 | 0.1 | 4.538 | 1.1(1.0-1.2) | 0.033 |
Note: Recent HIV testing indicated the participants have ever received a test for HIV in the past 12 months; P6M: in the past 6 months; P12M: in the past 12 months; OR: odds ratio; 95%CI: confidence interval; AOR: adjusted odds ratio; Multivariable logistic regression analysis was applied for HIV recent testing, in which the data weighted with the respondent driven sampling analysis tool (RDSAT) were applied.
Correlates for Stigmatizing and Discriminatory Attitudes towards PLWHA
Univariate analysis revealed that recent testers were less likely to have negative attitudes towards PLWHA, MSM who had a full time job, higher income, ≥3 male partners in the past 6 months, no female partners in the past 6 months, a regular partner, never got drunk, received free condoms/lubricant in the past 12 months, and did not fear an HIV-positive test result, had lower degree of negative attitudes towards PLWHA. MSM who were younger and knew where to receive HIV testing were more likely to have lower degree of negative attitudes towards PLWHA. The multivariate linear regression analysis suggested that MSM who had recent HIV testing (β =0.7, p <0.05), were younger (β =1.8, p <0.001), and knew HIV infection status of their last male partner (β =0.9, p <0.05) were more likely to express lower levels of stigmatizing and discriminatory attitudes towards PLWHA (Table 3).
Table 3. Correlates for HIV/AIDS-related stigmatizing and discriminatory attitudes among Beijing’s men who have sex with men.
| Variable | β (95%CI) | P | Adjusted β(95%CI) | P |
|---|---|---|---|---|
| Younger age (v.s. >29 years) | 1.8(1.2-2.4) | <0.001 | 1.8(1.2-2.4) | <0.001 |
| Higher level education (v.s. <high school level) | 1.9(1.2-2.6) | <0.001 | ||
| Unmarried | 1.5(0.8-2.3) | <0.001 | ||
| Have health insurance | 1.1(0.4-1.7) | 0.001 | ||
| Had <3 male partners, P6M | 0.6(−0.01-1.3) | 0.056 | ||
| Found male sex partners through Internet | 1.8(1.2-2.5) | <0.001 | ||
| Had sex with last male partner at Bathhouse/ Sauna/ Park/ Public rest room, P6M |
−1.3(−2.3- −0.4) | 0.006 | ||
| Knew the HIV status of last male partner | 1.1(0.3-1.9) | 0.006 | 0.9(0.1-1.7) | 0.022 |
| Disclosed HIV status with last male partner | 1.1(0.4-1.7) | 0.002 | ||
| Knew where to get HIV test | 1.2(0.1-2.2) | 0.029 | ||
| Ever received a test for HIV, P12M | 0.8(0.1-1.4) | 0.026 | 0.7(0.03-1.3) | 0.041 |
Note: P6M: in the past 6 months; P12M: in the past 12 months; Multivariable linear regression was performed for HIV/AIDS-related stigmatizing and discriminatory attitudes, in which the data weighted with the respondent driven sampling analysis tool (RDSAT) were applied.
Discussion
This is the first study in China in assessing stigmatizing and discriminatory attitudes towards PLWHA and its relationship with HIV testing among Beijing MSM. This study revealed that stigmatizing and discriminatory attitudes against PLWHA were common and inversely associated with recent HIV testing among Beijing MSM. Confronting a rapid rise of HIV epidemic among MSM in China, common negative attitudes towards PLWHA, low levels of testing and high levels of undiagnosed infections among this group has become emerging challenges in containing the epidemic. The negative attitudes towards PLTHA could be a critical barrier in expanding testing and reduce the levels of undiagnosed HIV infections. Studies demonstrated that stigma and discrimination remains significant barriers to HIV testing in diverse settings(Fortenberry, McFarlane, Bleakley, Bull, Fishbein, Grimley et al., 2002; W. Ma, Detels, Feng, Wu, Shen, Li et al., 2007a) and that lack of HIV testing was associated with greater negative attitudes towards PLWHA (Genberg, Hlavka, Konda, Maman, Chariyalertsak, Chingono et al., 2009; Kalichman & Simbayi, 2003). The findings of the present study underlined the urgent needs to reduce the stigmatizing and discriminatory attitudes towards PLWHA, expand HIV testing and reduce the levels of undiagnosed HIV infections among this group.
This study showed that having multiple sex partners was independently associated with HIV testing. Other reports showed that MSM who have sex with multiple partnerships acknowledge their higher risk and undergo testing to determine whether this behavior has resulted in infection (Do, Chen, McFarland, Secura, Behel, MacKellar et al., 2005; Jin, Prestage, Law, Kippax, Van de Ven, Rawsthorne et al., 2002; McGarrigle, Mercer, Fenton, Copas, Wellings, Erens et al., 2005). A survey in Baltimore where reported the highest HIV prevalence among MSM in the United States suggested that young MSM with a greater number of lifetime male partners were more likely to receive HIV testing (Sifakis, Hylton, Flynn, Solomon, MacKellar, Valleroy et al., 2010). The findings of the present study suggested that common multiple sex partners and existing sexual network among this group could offer an intervention opportunity in expanding HIV testing.
This study revealed that recent HIV testing was independently associated with the awareness of HIV status of one’s last male partner. It is consistent with other reports from Australia and the United States (Jin et al., 2002),(MacKellar, Valleroy, Anderson, Behel, Secura, Bingham et al., 2006). Other studies on stigmatizing attitudes of the general population against PLWHA have shown that HIV/AIDS-related stigma are inversely related to discussion about HIV/AIDS (Dias, Matos, & Goncalves, 2006; Genberg et al., 2009), disclosure of HIV status (Maman, Mbwambo, Hogan, Weiss, Kilonzo, & Sweat, 2003), and ever tested for HIV (Genberg et al., 2009; Kalichman & Simbayi, 2003). Common multiple sex partners, non-disclosure of HIV status, and negative attitudes towards PLWHA showed in this study highlighted the urgent needs in focused efforts to encourage disclosure of HIV status between partners, promote HIV testing, and decrease stigmatizing and discriminatory attitudes towards PLWHA.
The low levels of testing and high levels of undiagnosed infections found in this study indicated that prevention programs would not yet operate effectively for MSM in Beijing. A third of MSM had never tested for HIV. This figure is more than three times the level measured among MSM in 21 cities of the United States in 2008 (10%) (Deiss, Brouwer, Loza, Lozada, Ramos, Firestone Cruz et al., 2007). Low testing uptake and high levels of undiagnosed infection would have a significant impact on the epidemic, because men with undiagnosed HIV infection were also more likely to engage in unprotected anal sex and have unknown serostatus partners (Branson, Handsfield, Lampe, Janssen, Taylor, Lyss et al., 2006). Men with undiagnosed HIV infection were also unaware of their most recent partner’s serostatus and held higher negative attitudes towards safe sex practices. The findings of this study underscored the urgent needs in intensifying the intervention effort to improve not only testing coverage but testing frequency among MSM to link and retain HIV infected individuals in prevention, care and treatment programs.
HIV testing plays an important role in prevention and control epidemic, HIV testing and counseling can help reduce risk behaviors (Leaity et al., 2000; Weinhardt et al., 1999), and expanding HIV testing could facilitate early diagnosis and timely prevention, linkage-to-care and medical treatment (Janssen et al., 2001; Valdiserri et al., 1999). However, stigma and discrimination have been identified as major barriers to uptake HIV-related prevention services (Agwu & Ellen, 2009; Mahajan et al., 2008; UNAIDS, Dec2003). HIV/AIDS-related stigma and discrimination can adversely influence decisions to seek HIV testing (Chesney & Smith, 1999; Kalichman & Simbayi, 2003). Recently community-based clinic trials results have provided proof of antiretroviral treatment as prevention (Abdool Karim, Abdool Karim, Frohlich, Grobler, Baxter, Mansoor et al.,; Cohen, Chen, McCauley, Gamble, Hosseinipour, Kumarasamy et al., 2011; Grant, Lama, Anderson, McMahan, Liu, Vargas et al.,; NIAID/NIH., 2011), which have given us new biological tools to control the epidemic. The early initiation of antiretroviral therapy reduced rates of sexual transmission of HIV-1 and clinical events, indicating both personal and public health benefits from such therapy (Cohen et al., 2011). It is time to address various barriers in scaling up the effort to link the best advancements in science to the needs of the community. It is very critical to better understand stigmatizing and discrimination attitudes towards PLWHA when expanding HIV testing, prevention, care and treatment in controlling epidemic among this group.
This study also found that younger MSM were more likely to express lower negative attitudes towards PLWHA. The reasons for this could be that the younger MSM have higher levels of education, lower perceived stigmatizing and discriminatory social pressure, and have greater access to HIV/AIDS message and health information. Studies on stigmatizing attitudes of the general population against PLWHA showed that HIV/AIDS-related stigma are inversely related to knowledge about modes of HIV transmission,(Dias et al., 2006) and educational attainment (Dias et al., 2006; Kalichman, Simbayi, Jooste, Toefy, Cain, Cherry et al., 2005), and but positively related to age (Genberg et al., 2008). The present study also found that bisexual MSM were inversely associated with HIV testing. Our other study among Shandong MSM found that bisexual men are more likely to be older and have lower levels of HIV-related knowledge than men who have sex with men-only.(Liao, Kang, & Jia, 2011) The common bisexual practice showed in the present study were consistent with our previous study and other reports in China (Choi, Gibson, Han, & Guo, 2004; Gu, Qu, Lu, Luo, Wang, & Gu, 2004; Jiang, Cao, Zhang, Xia, Gong, Xue et al., 2006; Liao et al., 2011; X. Ma et al., 2007b; Ruan, Yang, Zhu, Ma, Li, Zhao et al., 2008), it is more common than a corresponding figure obtained in the West (Hightow, Leone, Macdonald, McCoy, Sampson, & Kaplan, 2006). Chinese culture is still relatively conservative in discussing homosexuality as a open subject (Liu & Choi, 2006). Stigma and discrimination against MSM in Chinese societies may be still quite serious (Choi, Hudes, & Steward, 2008), it may explain partially the observed common bisexual behaviors (Liao et al., 2011). Common stigmatizing and discriminatory attitudes against PLWHA and common bisexual practice among Beijing gay men highlighted the challenges in effectively expanding HIV testing.
This is the first study in China described HIV/AIDS-related stigmatizing and discriminatory attitudes towards PLWHA and its correlates and relationship with HIV testing among Beijing MSM. This study highlighted an important area that warrants HIV prevention and research work. We also recognized the limitations of this study. First, the stigma/discrimination scale may provoke socially desirable answers from respondents. Participants may feel embarrassed to be open expressing stigmatizing and discriminatory attitudes towards PLWHA during the face-to-face interviews, thus, this study might underestimate the true levels of negative attitudes and the risk behavior. Second, the nature of the cross-sectional study design precluded the ascertainment of causal relationship. Other limitations may stem from the monetary incentive having relatively stronger draw among persons of lower socio-economic status, as noted in other RDS surveys (Johnston, Malekinejad, Kendall, Iuppa, & Rutherford, 2008).
In conclusion, this study revealed that stigmatizing and discriminatory attitudes towards PLWHA inversely associated with recent testing among Beijing MSM. Common HIV/AIDS-related stigmatizing and discriminatory attitudes, low levels of testing, and high levels of undiagnosed infections among this group have become emerging challenges containing the epidemic. The stigmatizing and discrimination attitudes towards PLWHA could be a critical barrier to expanding testing and reduce the levels of undiagnosed HIV infections. The findings of this study highlighted the urgent needs to reduce HIV/AIDS related stigma and discrimination, encourage disclosure of HIV status, and expand HIV testing among this group.
Acknowledgements
This study was supported, in part, by grants from the National Institutes of Health (#R01 AI078933 and # 5D43TW001035-13), the Ministry of Science and Technology of China (2012ZX10001-002 and 2009DFB30420), and Chinese State Key Laboratory for Infectious Disease Develop Grant (2011SKLID102).
Footnotes
Conflicts of Interest
No.
References
- Abadia-Barrero CE, Castro A. Experiences of stigma and access to HAART in children and adolescents living with HIV/AIDS in Brazil. Soc Sci Med. 2006;62(5):1219–1228. doi: 10.1016/j.socscimed.2005.07.006. [DOI] [PubMed] [Google Scholar]
- Abdool Karim Q, Abdool Karim SS, Frohlich JA, Grobler AC, Baxter C, Mansoor LE, et al. Effectiveness and safety of tenofovir gel, an antiretroviral microbicide, for the prevention of HIV infection in women. Science. 329(5996):1168–1174. doi: 10.1126/science.1193748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Agwu A, Ellen J. Rising rates of HIV infection among young US men who have sex with men. Pediatr Infect Dis J. 2009;28(7):633–634. doi: 10.1097/INF.0b013e3181afcd22. [DOI] [PubMed] [Google Scholar]
- Baral S, Sifakis F, Cleghorn F, Beyrer C. Elevated risk for HIV infection among men who have sex with men in low- and middle-income countries 2000-2006: a systematic review. PLoS Med. 2007;4(12):e339. doi: 10.1371/journal.pmed.0040339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boer IM d., Op de Coul E, Koedijk F, Veen MG v., Sighem AI v., Laar MJW v. d. HIV and Sexually Transmitted Infections in the Netherlands in 2005. RIVM report [Google Scholar]
- Branson BM, Handsfield HH, Lampe MA, Janssen RS, Taylor AW, Lyss SB, et al. Revised recommendations for HIV testing of adults, adolescents, and pregnant women in health-care settings. MMWR Recomm Rep. 2006;55(RR-14):1–17. quiz CE11-14. [PubMed] [Google Scholar]
- Chesney MA, Smith AW. Critical Delays in HIV Testing and Care. American Behavioral Scientist. 1999;42(7):1162–1174. [Google Scholar]
- Choi KH, Gibson DR, Han L, Guo Y. High levels of unprotected sex with men and women among men who have sex with men: a potential bridge of HIV transmission in Beijing, China. AIDS Educ Prev. 2004;16(1):19–30. doi: 10.1521/aeap.16.1.19.27721. [DOI] [PubMed] [Google Scholar]
- Choi KH, Hudes ES, Steward WT. Social discrimination, concurrent sexual partnerships, and HIV risk among men who have sex with men in Shanghai, China. AIDS Behav. 2008;12(4 Suppl):S71–77. doi: 10.1007/s10461-008-9394-0. [DOI] [PubMed] [Google Scholar]
- Cohen MS, Chen YQ, McCauley M, Gamble T, Hosseinipour MC, Kumarasamy N, et al. Prevention of HIV-1 infection with early antiretroviral therapy. N Engl J Med. 2011;365(6):493–505. doi: 10.1056/NEJMoa1105243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Courtenay-Quirk C, Wolitski RJ, Parsons JT, Gomez CA. Is HIV/AIDS stigma dividing the gay community? Perceptions of HIV-positive men who have sex with men. AIDS Educ Prev. 2006;18(1):56–67. doi: 10.1521/aeap.2006.18.1.56. [DOI] [PubMed] [Google Scholar]
- Deiss RG, Brouwer KC, Loza O, Lozada RM, Ramos R, Firestone Cruz MA, et al. High-Risk Sexual and Drug Using Behaviors Among Male Injection Drug Users Who Have Sex With Men in 2 Mexico-US Border Cities. Sex Transm Dis. 2007 doi: 10.1097/OLQ.0b013e31815abab5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dias SF, Matos MG, Goncalves AC. AIDS-related stigma and attitudes towards AIDS-infected people among adolescents. AIDS Care. 2006;18(3):208–214. doi: 10.1080/09540120500456177. [DOI] [PubMed] [Google Scholar]
- Do TD, Chen S, McFarland W, Secura GM, Behel SK, MacKellar DA, et al. HIV testing patterns and unrecognized HIV infection among young Asian and Pacific Islander men who have sex with men in San Francisco. AIDS Educ Prev. 2005;17(6):540–554. doi: 10.1521/aeap.2005.17.6.540. [DOI] [PubMed] [Google Scholar]
- Flowers P, Duncan B, Frankis J. Community, responsibility and culpability: HIV risk-management amongst Scottish gay men. Journal of Community & Applied Social Psychology. 2000;10(4):285–300. [Google Scholar]
- Fortenberry JD, McFarlane M, Bleakley A, Bull S, Fishbein M, Grimley DM, et al. Relationships of stigma and shame to gonorrhea and HIV screening. Am J Public Health. 2002;92(3):378–381. doi: 10.2105/ajph.92.3.378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Genberg BL, Hlavka Z, Konda KA, Maman S, Chariyalertsak S, Chingono A, et al. A comparison of HIV/AIDS-related stigma in four countries: negative attitudes and perceived acts of discrimination towards people living with HIV/AIDS. Soc Sci Med. 2009;68(12):2279–2287. doi: 10.1016/j.socscimed.2009.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Genberg BL, Kawichai S, Chingono A, Sendah M, Chariyalertsak S, Konda KA, et al. Assessing HIV/AIDS stigma and discrimination in developing countries. AIDS Behav. 2008;12(5):772–780. doi: 10.1007/s10461-007-9340-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant RM, Lama JR, Anderson PL, McMahan V, Liu AY, Vargas L, et al. Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. N Engl J Med. 363(27):2587–2599. doi: 10.1056/NEJMoa1011205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gu Y, Qu P, Lu S, Luo M, Wang X, Gu J. Survey of knowledge, attitude behavior and practice related to STI/HIV among male homosexuals in Shenyang. Chinese Journal of Public Health. 2004;20:573–574. [Google Scholar]
- Hall HI, Song R, Rhodes P, Prejean J, An Q, Lee LM, et al. Estimation of HIV incidence in the United States. Jama. 2008;300(5):520–529. doi: 10.1001/jama.300.5.520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herek GM, Capitanio JP, Widaman KF. HIV-related stigma and knowledge in the United States: prevalence and trends, 1991-1999. Am J Public Health. 2002;92(3):371–377. doi: 10.2105/ajph.92.3.371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hightow LB, Leone PA, Macdonald PD, McCoy SI, Sampson LA, Kaplan AH. Men who have sex with men and women: a unique risk group for HIV transmission on North Carolina College campuses. Sex Transm Dis. 2006;33(10):585–593. doi: 10.1097/01.olq.0000216031.93089.68. [DOI] [PubMed] [Google Scholar]
- Janssen RS, Holtgrave DR, Valdiserri RO, Shepherd M, Gayle HD, De Cock KM. The Serostatus Approach to Fighting the HIV Epidemic: prevention strategies for infected individuals. Am J Public Health. 2001;91(7):1019–1024. doi: 10.2105/ajph.91.7.1019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiang J, Cao N, Zhang J, Xia Q, Gong X, Xue H, et al. High prevalence of sexually transmitted diseases among men who have sex with men in Jiangsu Province, China. Sex Transm Dis. 2006;33(2):118–123. doi: 10.1097/01.olq.0000199763.14766.2b. [DOI] [PubMed] [Google Scholar]
- Jin FY, Prestage G, Law MG, Kippax S, Van de Ven P, Rawsthorne P, et al. Predictors of recent HIV testing in homosexual men in Australia. HIV Med. 2002;3(4):271–276. doi: 10.1046/j.1468-1293.2002.00121.x. [DOI] [PubMed] [Google Scholar]
- Johnston LG, Malekinejad M, Kendall C, Iuppa IM, Rutherford GW. Implementation challenges to using respondent-driven sampling methodology for HIV biological and behavioral surveillance: field experiences in international settings. AIDS Behav. 2008;12(4 Suppl):S131–141. doi: 10.1007/s10461-008-9413-1. [DOI] [PubMed] [Google Scholar]
- Kalichman SC, Simbayi LC. HIV testing attitudes, AIDS stigma, and voluntary HIV counselling and testing in a black township in Cape Town, South Africa. Sex Transm Infect. 2003;79(6):442–447. doi: 10.1136/sti.79.6.442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalichman SC, Simbayi LC, Jooste S, Toefy Y, Cain D, Cherry C, et al. Development of a brief scale to measure AIDS-related stigma in South Africa. AIDS Behav. 2005;9(2):135–143. doi: 10.1007/s10461-005-3895-x. [DOI] [PubMed] [Google Scholar]
- Leaity S, Sherr L, Wells H, Evans A, Miller R, Johnson M, et al. Repeat HIV testing: high-risk behaviour or risk reduction strategy? AIDS. 2000;14(5):547–552. doi: 10.1097/00002030-200003310-00010. [DOI] [PubMed] [Google Scholar]
- Letamo G. Prevalence of, and factors associated with, HIV/AIDS-related stigma and discriminatory attitudes in Botswana. J Health Popul Nutr. 2003;21(4):347–357. [PubMed] [Google Scholar]
- Liao M, Kang D, Jia Y. Bisexual behavior and infection with HIV and syphilis among men who have sex with men along the east coast of China. AIDS PATIENT CARE and STDs. 2011;25 doi: 10.1089/apc.2010.0371. DOI: 10.1089/apc.2010.0371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu JX, Choi K. Experiences of social discrimination among men who have sex with men in Shanghai, China. AIDS Behav. 2006;10(4 Suppl):S25–33. doi: 10.1007/s10461-006-9123-5. [DOI] [PubMed] [Google Scholar]
- Ma W, Detels R, Feng Y, Wu Z, Shen L, Li Y, et al. Acceptance of and barriers to voluntary HIV counselling and testing among adults in Guizhou province, China. AIDS. 2007a;21(Suppl 8):S129–135. doi: 10.1097/01.aids.0000304708.64294.3f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma X, Zhang Q, He X, Sun W, Yue H, Chen S, et al. Trends in prevalence of HIV, syphilis, hepatitis C, hepatitis B, and sexual risk behavior among men who have sex with men. Results of 3 consecutive respondent-driven sampling surveys in Beijing, 2004 through 2006. J Acquir Immune Defic Syndr. 2007b;45(5):581–587. doi: 10.1097/QAI.0b013e31811eadbc. [DOI] [PubMed] [Google Scholar]
- MacKellar DA, Valleroy LA, Anderson JE, Behel S, Secura GM, Bingham T, et al. Recent HIV testing among young men who have sex with men: correlates, contexts, and HIV seroconversion. Sex Transm Dis. 2006;33(3):183–192. doi: 10.1097/01.olq.0000204507.21902.b3. [DOI] [PubMed] [Google Scholar]
- Mahajan AP, Sayles JN, Patel VA, Remien RH, Sawires SR, Ortiz DJ, et al. Stigma in the HIV/AIDS epidemic: a review of the literature and recommendations for the way forward. AIDS. 2008;22(Suppl 2):S67–79. doi: 10.1097/01.aids.0000327438.13291.62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maman S, Mbwambo JK, Hogan NM, Weiss E, Kilonzo GP, Sweat MD. High rates and positive outcomes of HIV-serostatus disclosure to sexual partners: reasons for cautious optimism from a voluntary counseling and testing clinic in Dar es Salaam, Tanzania. AIDS Behav. 2003;7(4):373–382. doi: 10.1023/b:aibe.0000004729.89102.d4. [DOI] [PubMed] [Google Scholar]
- McGarrigle CA, Mercer CH, Fenton KA, Copas AJ, Wellings K, Erens B, et al. Investigating the relationship between HIV testing and risk behaviour in Britain: National Survey of Sexual Attitudes and Lifestyles 2000. AIDS. 2005;19(1):77–84. doi: 10.1097/00002030-200501030-00009. [DOI] [PubMed] [Google Scholar]
- NIAID/NIH [Accessed on May 25, 2011];Treating HIV-infected People with Antiretrovirals Protects Partners from Infection: Findings Result from NIH-funded International Study. 2011 Available at: http://www.niaid.nih.gov/news/newsreleases/2011/Pages/HPTN052.aspx.
- Rahmati-Najarkolaei F, Niknami S, Aminshokravi F, Bazargan M, Ahmadi F, Hadjizadeh E, et al. Experiences of stigma in healthcare settings among adults living with HIV in the Islamic Republic of Iran. J Int AIDS Soc. 2010;13:27. doi: 10.1186/1758-2652-13-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raymond HF CS, Truong HM, Knapper KB, Klausner JD, Choi KH, McFarland W. Trends in sexually transmitted diseases, sexual risk behavior, and HIV infection among Asian/Pacific Islander men who have sex with men, San Francisco, 1999-2005. Sex Transm Dis. 2007;34(5):262–264. doi: 10.1097/01.olq.0000237854.25406.ad. [DOI] [PubMed] [Google Scholar]
- Ruan S, Yang H, Zhu Y, Ma Y, Li J, Zhao J, et al. HIV prevalence and correlates of unprotected anal intercourse among men who have sex with men, Jinan, China. AIDS Behav. 2008;12(3):469–475. doi: 10.1007/s10461-008-9361-9. [DOI] [PubMed] [Google Scholar]
- Sifakis F, Hylton JB, Flynn C, Solomon L, MacKellar DA, Valleroy LA, et al. Prevalence of HIV infection and prior HIV testing among young men who have sex with men. The Baltimore young men’s survey. AIDS Behav. 2010;14(4):904–912. doi: 10.1007/s10461-007-9317-5. [DOI] [PubMed] [Google Scholar]
- Thi MD, Brickley DB, Vinh DT, Colby DJ, Sohn AH, Trung NQ, et al. A qualitative study of stigma and discrimination against people living with HIV in Ho Chi Minh City, Vietnam. AIDS Behav. 2008;12(4 Suppl):S63–70. doi: 10.1007/s10461-008-9374-4. [DOI] [PubMed] [Google Scholar]
- UNAIDS Fact sheet on stigma and discrimination. 2003 Dec; [Google Scholar]
- Unnikrishnan B, Mithra PP, T R, B R. Awareness and Attitude of the General Public Toward HIV/AIDS in Coastal Karnataka. Indian J Community Med. 2010;35(1):142–146. doi: 10.4103/0970-0218.62580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valdiserri RO, Holtgrave DR, West GR. Promoting early HIV diagnosis and entry into care. AIDS. 1999;13(17):2317–2330. doi: 10.1097/00002030-199912030-00003. [DOI] [PubMed] [Google Scholar]
- van Griensven F, de Lind van Wijngaarden JW, Baral S, Grulich A. The global epidemic of HIV infection among men who have sex with men. Curr Opin HIV AIDS. 2009;4(4):300–307. doi: 10.1097/COH.0b013e32832c3bb3. [DOI] [PubMed] [Google Scholar]
- Volz E, Wejnert C, Degani I, Heckathorn DD. Respondent-Driven Sampling Analysis Tool (RDSAT) Version 5.6. Cornell University; Ithaca, NY: [Accessed on August 28, 2011]. 2007. Available at: http://www.respondentdrivensampling.org. [Google Scholar]
- Weinhardt LS, Carey MP, Johnson BT, Bickham NL. Effects of HIV counseling and testing on sexual risk behavior: a meta-analytic review of published research, 1985-1997. Am J Public Health. 1999;89(9):1397–1405. doi: 10.2105/ajph.89.9.1397. [DOI] [PMC free article] [PubMed] [Google Scholar]