Abstract
Background
Length of stay (LoS) following elective surgery is being reported as an outcomes quality measure. Regional referral centres may care for patients travelling significant distances. The effect of travel distance on LoS in pancreatic surgery patients was examined.
Methods
National Surgical Quality Improvement Program data on pancreatic surgery patients, operated during the period from 2005 to 2011, were reviewed. Demographics, surgical variables and distance travelled were analysed relative to LoS. The LoS was log-transformed in general linear models to achieve normality.
Results
Of the 243 patients, 53% were male. The mean ± standard deviation (SD) age of the total patient sample was 60.6 ± 14 years. The mean ± SD distance travelled was 203 ± 319 miles (326.7 ± 513.4 km) [median: 132 miles (212.4 km); range: 3–3006 miles (4.8–4837.7 km)], and the mean ± SD LoS was 10.5 ± 7 days (range: 1–46 days). Univariate analysis showed a near significant increase in LoS with increased distance travelled (P = 0.05). Significant variables related to LoS were: age (P = 0.002); relative value units (P < 0.001), and preoperative American Society of Anesthesiologists class (P = 0.005). In a general linear model, for every 100 miles (160.9 km) travelled there is an associated 2% increase in LoS (P = 0.031). When the distance travelled is increased by 500 miles (804.7 km), LoS increases by 10.5%.
Conclusions
Increased travel distance from a patient's home to the hospital was independently associated with an increase in LoS. If LoS is a reportable quality measure in pancreatic surgery, travel distance should be considered in risk adjustments.
Introduction
Hospital length of stay (LoS) following elective surgery is being reported as a quality measure in surgical outcome registries, such as the National Surgical Quality Improvement Program (NSQIP).1 There has been increasing interest in identifying factors related to LoS as both an increasing and a decreasing value. By recognizing and addressing the factors that might influence LoS, a systematic, evidence-based approach to decreasing LoS can be developed, without adversely affecting the quality of care provided and patient satisfaction.
Over the last decade, there has been increased attention to and emphasis on the regionalization of care to higher-volume centres in order to improve outcomes, especially in complex surgical procedures such as pancreaticoduodenectomy.2–4 High-volume centres have seen a 40% increase in median patient travel distances for pancreatic surgery as surgical care is regionalized to specialized centres.5,6
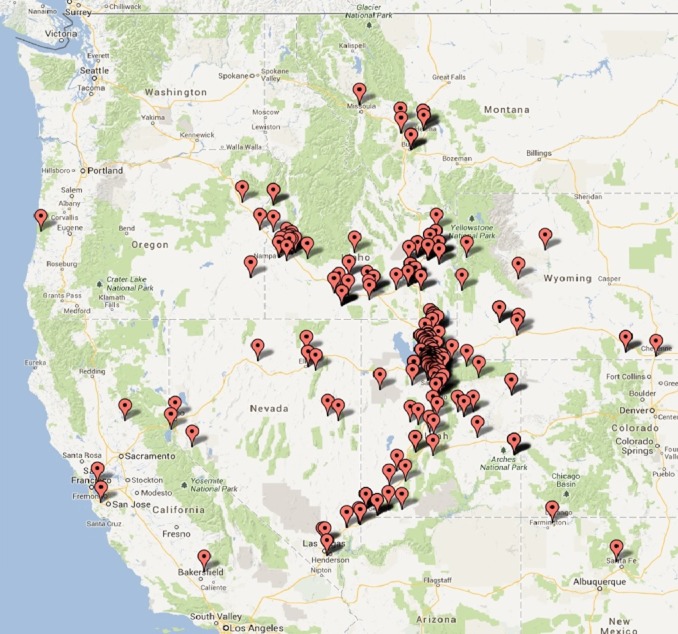
The University of Utah Health Sciences Center (UUHSC) has one of the largest geographic catchment areas of any academic medical centre in the USA.7 The patients treated at UUHSC in Salt Lake City travel from all areas of Utah and from the five nearby states of Idaho, Wyoming, Montana, Nevada and Arizona to receive medical and surgical care. The average distances travelled for specific treatments within Utah alone range from 3 miles (4.8 km) to 318 miles (511.8 km). The vast majority of these patients travel by automotive vehicle.
The present study was based on the hypothesis that increased travel distance from a patient's primary residence to UUHSC represents a non-medical cause of a potential delay in discharge, leading to an extended hospital LoS. To test this hypothesis, the effect of patient distance travelled, from primary residence to a major tertiary care hospital, on LoS in patients undergoing elective pancreatic surgery was examined.
Materials and methods
This study was reviewed and approved by the University of Utah Institutional Review Board. A total of 243 patients submitted to elective pancreatic surgery between January 2005 and October 2011 were identified from the local NSQIP database using Current Procedural Terminology (CPT) codes (Table 1). Additional data were obtained from patient chart review. Patients were excluded from the study if they had undergone emergency surgery, or if patient demographic or clinical data were incomplete. Patients submitted to emergency surgery were excluded in order to maintain a more standardized patient population. Discharge criteria were not standardized because of the retrospective nature of this study.
Table 1.
Current Procedural Terminology (CPT) codes and relative value unit (RVU) data for elective pancreatic surgery patients (n = 243)
| RVU | CPT code | n | Description |
|---|---|---|---|
| 18.41 | 48120 | 12 | Excision of lesion of pancreas (e.g. cyst, adenoma) |
| 20.39 | 48148 | 6 | Excision of ampulla of Vater |
| 26.32 | 48140 | 33 | Pancreatectomy, distal subtotal, with or without splenectomy, without pancreaticojejunostomy |
| 27.39 | 48145 | 8 | Pancreatectomy, distal subtotal, with or without splenectomy, with pancreaticojejunostomy |
| 30.6 | 48146 | 1 | Pancreatectomy, distal, near-total with preservation of duodenum (Child-type procedure) |
| 48.65 | 48152 | 5 | Whipple-type procedure without pancreaticojejunostomy |
| 48.88 | 48154 | 6 | Pylorus-sparing, Whipple-type procedure without pancreaticojejunostomy |
| 48.88 | 48155 | 1 | Pancreatectomy, total |
| 52.84 | 48150 | 66 | Whipple-type procedure with pancreaticojejunostomy |
| 52.79 | 48153 | 105 | Pylorus-sparing, Whipple-type procedure with pancreaticojejunostomy |
Travel distance was calculated from the five-digit zipcode of the patient's primary residence to the address and five-digit zipcode of the hospital (50 North Medical Drive, Salt Lake City, Utah 84132, USA). The distance travelled was recorded as the paved road mileage with the shortest travel time.8
Data collected and analysed included: patient demographics (age on admission, gender, marital status, zipcode of primary residence, rural versus urban location of primary residence); dates of admission and discharge, and preoperative surgery-related variables [American Society of Anesthesiologists (ASA) class, relative value units (RVU) for each surgical group, and emergency or elective surgery status] as defined by NSQIP. Groups were categorized based on marital status so that patients were assumed to have help at home (i.e. were married or partnered) or were assumed to live alone (i.e. single, divorced or widowed). Rural versus urban location was calculated using the 2006 ZIP Version 2.0 Rural Urban Commuting Area (RUCA) codes based on the five-digit zipcode of the patient's primary residence.9 A RUCA code of ≥7 was categorized as indicating residence in a rural location.10
Data were compiled using Microsoft Excel 2007 (Microsoft Corp., Redmond, WA, USA) and analysed using pasw Statistics 18 (SPSS, Inc., Chicago, IL, USA). Data are reported as the mean ± standard deviation (SD); the median and range are reported for right-skewed distance. Univariate analysis employing t-tests was performed with continuous variables and the non-parametric Mann–Whitney U-test was used for non-normally distributed measures. Categorical variables were analysed using chi-squared tests and Fisher's exact test for cell counts of < 5. A P-value of < 0.05 was considered to indicate statistical significance.
To account for the non-normal distribution of LoS, this variable underwent log transformation. A general linear model was created to examine the relationship between travel distance and hospital LoS, controlling for variables found in univariate testing to have a P-value of < 0.2.
Results
Data were collected for 243 elective pancreatic surgery patients, 53% of whom were male. The mean ± SD age of all patients included was 60.6 ± 14 years. Patients’ primary residences were categorized using RUCA codes as rural (16%) or urban (84%). Patients were assumed to have or not to have help at home in 69% and 31% of cases, respectively. The mean ± SD LoS was 10.5 ± 7 days (range: 1–46 days). The mean ± SD distance travelled from the patient's primary residence to the hospital was 203 ± 319 miles (326.7 ± 513.4 km) [median: 132 miles (212.4 km); range: 3–3006 miles (4.8–4837.7 km)] (Table 2 and Fig. 1). A total of 83 (34%) patients had travelled further than 100 miles (160.9 km) and 13 (5%) patients had travelled further than 500 miles (804.7 km). Taking into account the right-skewed distance distribution, the median distance travelled was 132 miles (212.4 km) [interquartile range (IQR): 27–246 miles (43.5–395.9 km)].
Table 2.
Demographic and clinical variables in elective pancreatic surgery patients (n = 243)
| Variable | Range | |
|---|---|---|
| Gender, male, % | 53 | N/A |
| Age, years, mean | 60.6 years | 16–88 years |
| Rural location, % | 16 | N/A |
| Assumed help at home, % | 69 | N/A |
| Length of stay, days, mean | 10.5 days | 1–46 days |
| Travel distance, miles (km), mean | 203 miles (326.7 km) | 3–3006 miles (4.8–4847.8 km) |
| ASA class of 1 or 2, % | 41 | N/A |
| ASA class of 3 or 4, % | 59 | N/A |
| RVU score of <40, % | 25 | N/A |
| RVU score of >40, % | 75 | N/A |
ASA, American Society of Anesthesiologists; RVU, relative value unit.
Figure 1.
Zipcode distribution of patients undergoing elective pancreatic surgery at the University of Utah Hospital between January 2005 and October 2011 (n = 243)
The ASA physical status classification scoring system was used as a surrogate marker of patient comorbidities. A total of 100 (41%) patients had ASA classes of 1 or 2, and 143 (59%) patients had ASA classes of 3 or 4. The RVU for surgical procedures is considered a measure of value based on resources required and is used by Medicare to calculate financial reimbursement. The RVU was used as a marker of case complexity and thus patients were divided into groups according to whether their RVU was <40 or >40 (Table 1).
Univariate linear regression analysis showed a near significant relationship between the increase in log-LoS with increased distance travelled (P = 0.052). Age was related to log-LoS (P = 0.002) (Fig. 2). Univariate analysis of LoS and gender (P = 0.675), having or not having live-in help (P = 0.214) and living in a rural or urban location (P = 0.295) showed no significant findings (Table 3). An increasing ASA class was associated with a statistically significant increase in LoS (P < 0.001). There was a direct relationship between LoS and increasing case complexity as indicated by the RVU (P ≤ 0.001) (Table 3).
Figure 2.
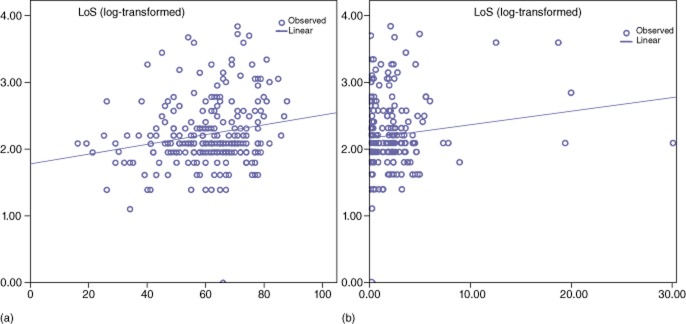
Univariate analysis of associations between (a) age (years) (P = 0.002) and (b) distance travelled (per 100 miles) (P = 0.052), and length of stay (LoS) in elective pancreatic surgery patients (n = 243)
Table 3.
Univariate analysis of dichotomous demographic and clinical variables and length of stay in elective pancreatic surgery patients (n = 243)
| Variable | Length of stay, days, mean ± SD | P-value |
|---|---|---|
| Male | 10.8 ± 7.6 | 0.675 |
| Female | 10.1 ± 5.8 | |
| ASA class of 1 or 2 | 9 ± 4.6 | 0.005 |
| ASA class of 3 or 4 | 11.6 ± 7.9 | |
| RVU score of <40 | 7 ± 3.1 | <0.001 |
| RVU score of >40 | 11.7 ± 7.3 | |
| Assumed help | 10.7 ± 6.9 | 0.214 |
| Assumed alone | 10 ± 6.8 | |
SD, standard deviation; ASA, American Society of Anesthesiologists; RVU, relative value unit.
Univariate analyses showed no statistically significant difference in patient travel distance according to RVU or major complication rate. Among patients with an RVU of < 40, the mean ± SD travel distance was 180 ± 161 miles (289.7 ± 259.1 km), whereas among patients with an RVU of >40, the mean ± SD travel distance was 210 ± 353 miles (338.0 ± 568.1 km) (P = 0.722). Among the 68 patients who suffered a major complication, the mean ± SD travel distance was 242 ± 415 miles (389.5 ± 667.9 km) and among the 175 patients without a major complication the mean ± SD distance travelled was 187 ± 273 miles (301.0 ± 439.4 km) (P = 0.863).
Based on the univariate results, a general linear model was created for log-LoS using age, ASA class, RVU grouping and distance travelled as model variables. The results are summarized in Fig. 3 and Table 4.
Figure 3.
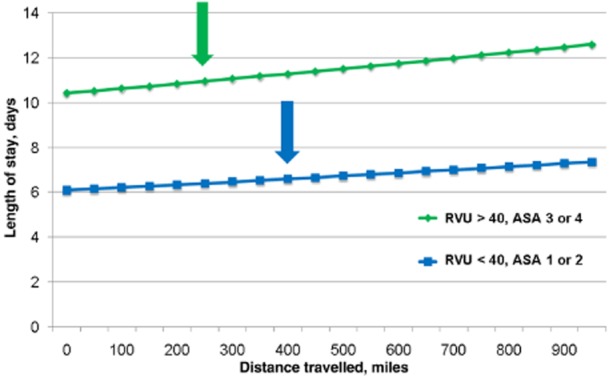
Results of model for effect of distance travelled on length of stay in high- and low-risk elective pancreatic surgery patients of the average age (61 years). RVU, relative value unit; ASA, American Society of Anesthesiologists
Table 4.
General linear model results of variables affecting length of stay (LoS) in elective pancreatic surgery patients (n = 243)
| Variable | P-value | Change in LoS |
|---|---|---|
| Age | 0.110 | Increased by 0.4% |
| ASA class of 3 or 4 vs. 1 or 2 | 0.064 | Increased by 12% |
| RVU score of >40 vs. <40 | <0.001 | Increased by 53% |
| Distance: per each 100-mile (160.9-km) increase in travel distance | 0.031 | Increased by 2% |
ASA, American Society of Anesthesiologists; RVU, relative value unit.
In this model, age was not found to be a significant determinant of LoS. Analysis of ASA class status showed a trend towards significance with a potential increase of 12% in LoS within the model for patients with an ASA class of 3 or 4 (P = 0.064). Patients with an RVU score of >40 were significantly more likely to have an increased LoS (P ≤ 0.001). The distance travelled from the patient's primary residence to the treating hospital was found to be a significant predictor of an increased hospital LoS (P = 0.031). The model revealed that, for each additional 100 miles (160.9 km) travelled, the LoS increased by 2%. Figure 3 demonstrates the general linear model that employs two groups of patients based on model variables and shows a progressive increase in LoS in line with an increase in the distance travelled. In those patients of average age (61 years) with both an RVU score of < 40 and an ASA class of 1 or 2, LoS is increased by half a day at 400 miles (643.7 km). In patients of average age with an RVU of >40 and an ASA class of 3 or 4, LoS is increased by half a day at 250 miles (402.3 km).
Discussion
In this study of 243 patients submitted to elective pancreatic surgery, an increase in travel distance from primary residence to the treating hospital was associated with an increase in LoS, even when a number of significant demographic and perioperative clinical variables were accounted for.
It is difficult to predict the exact LoS for a particular group of surgical patients and, as a result, discharge planning discussions often occur close to the day of discharge. It would seem likely that the discharge criteria desired by both the physician and the patient will be more stringent for patients who must travel a long distance to their primary residence and that this may lead to additional time spent in hospital. For example, there are concerns about travel time, pain control, complications that may ensue and the medical facilities available to manage these issues, should they arise, if the patient is geographically isolated. The discharge of a patient to a distant location may also require more time and the organization of multiple services. Other considerations that may represent barriers to discharge may include the mode and availability of transportation, as well as local weather and road conditions. Whether these concerns are real or perceived, they may be barriers to timely discharge in patients from distant locations and must be addressed and overcome.
Curiously, increasing age was not significantly associated with increased LoS in this analysis model. It is possible that plans to transfer older patients to skilled nursing facilities may have been in place or that the assistance of relatives at discharge was organized. Overall, physicians, patients and relatives may have been more forward thinking about discharge plans in elderly patients.
Living in a rural location has been previously documented to be associated with increased travel distance and increased LoS in some subsets of medical and surgical diagnoses.10–12 This was not found to be the case in this model, but this finding may reflect the relatively small size of the sample in this group.
Marital status has been shown to be a significant surrogate marker for the degree of social support available to a patient at discharge.13 Patients who are assumed to be discharged to home without assistance are required to attain higher levels of independence in mobility and daily living activities before discharge. In the present study, those patients with assumed help at home had a hospital LoS similar to those who were assumed not to have help at home. This may indicate that the use of marital status as a surrogate for social support in this patient population is limited in the strength of its correlation to discharge planning.
Increasing ASA class, which was used as a surrogate marker of perioperative comorbidities, trended towards statistical significance with an increase in LoS in the model. In this study, factors that were available preoperatively were examined. Patient ASA class has previously been shown to be a significant predictor for the occurrence of a major postoperative complication in pancreatoduodenectomy patients.14 It may be that patients with a higher ASA class were more likely to experience a complication that would increase their LoS. Neither increasing ASA class nor the occurrence of a major complication were related to increased travel distance.
A higher RVU score has previously been validated as a predictor of an increased LoS in paediatric patients undergoing cardiac surgery.15 This relationship was confirmed by this model: a comparison of the group with a lower RVU (<40) with the group with a higher RVU (>40) showed an independent increase in LoS in the higher RVU group, confirming that undergoing a more complex procedure can result in a longer hospitalization.
The hospital examined in the present study is situated in a major urban area, in which many local facilities are available for overnight accommodation. Recently, a hotel has been situated on campus within walking distance of the hospital, giving patients and their relatives easy access to the entire hospital system. This facility, as well as other nearby accommodations, could easily be utilized as a transitional placement prior to returning patients to their primary residences, thereby avoiding patient accrual of additional costly and unnecessary time in hospital.
Strengths and weaknesses of the study
This study is the first to identify patient travel distance as a significant and relevant factor related to an increased LoS in elective pancreatic surgery patients. In terms of strengths, this study identified preoperative variables that are easily available to health care staff, who can identify potential patients at potential risk for an increased LoS. This knowledge of risk for a prolonged stay can allow for earlier discharge planning in these individuals.
The present study is limited mainly by its retrospective design. Although complications have been described as affecting LoS in pancreatic surgery, they were excluded from this analysis because its goal was to assess preoperative variables that may be used to predict LoS. Regardless, patients who suffered a complication were compared with those who did not. The mean distance travelled did not differ between these groups. It was therefore concluded that data on the occurrence of complications would not have significantly confounded the analysis of distance travelled in relation to LoS.
The data available did not facilitate the distinguishing of those patients who did not return directly to their listed primary residence. This information may either increase or decrease the distance of travel undertaken by patients and this may impact the findings of the study. The use of a patient's marital status as a proxy marker for whether he or she lives alone and without assistance has limitations, but this characteristic has been shown in previous studies to be a significant predictor of a patient's access to social support.13 The travel distance calculations were potentially limited because they were based on a single geographic area covered by individual postal codes.
Implications of the study findings
The postoperative hospital LoS in patients who live a significant distance from the hospital may be addressed in multiple ways. Increased physician awareness of this relationship and the promotion of discussions about discharge plans with patients in the preoperative period may in themselves decrease hospital stay. Preoperative discussion about expected time in hospital, state of health at discharge, and the possibility of staying locally for a short period may facilitate timely discharge in patients who live further away. In patients with travel distances of >100 miles (160.9 km), a preoperative meeting with a case manager might prove to represent a cost-effective method of reducing hospital stay overall. Discharge planning and related discussions should be incorporated into daily rounds and into the documented patient plan.
Insurance companies should consider including the cost of local accommodation within their coverage if this would facilitate earlier discharge because this might potentially reduce the overall costs of care. Accommodations such as guest houses or hotels are significantly cheaper than additional days spent in hospital and would be likely to result in a decrease in overall medical expenses.
Areas for future research
This study identifies increased travel distance as a factor predictive of an increased hospital LoS, but it does not identify the reason for this relationship. There is likely to be a multifactorial relationship in which both quantitative and qualitative variables are involved. Undertaking a qualitative survey of physician and patient opinions on the discharge of patients might help to identify specific factors that could be addressed to decrease hospital stay. The prospective collection of data on a patient's social support network, living arrangements and the location to which he or she will be discharged would provide further useful information. It is also important to prospectively evaluate the effect of decreasing LoS on readmission rates and patient satisfaction scores.16,17
Documenting the financial impact of an increased LoS may be a way to stimulate increased interest in this area and provide incentives to make additional resources available to patients, such as preoperative case management consultations and local accommodation discounts. A multi-institution study of patient travel distances and hospital LoS with different patient populations and catchment areas to confirm and validate the findings of this study will be necessary to ensure that these data are applicable on a national level. If travel distance were to remain a significant variable with respect to LoS in comparison with the other risk factors accounted for in the NSQIP, it should be included in the NSQIP risk adjustment model.
Conclusions
In a model that controlled for demographic and preoperative variables, increased travel distance from a patient's primary residence to the hospital of surgery was associated with an increase in LoS. For patients who must travel lengthy distances, discharge planning should be discussed both pre- and postoperatively in order to negotiate the potential difficulties that might lead to an increase in LoS. As hospital LoS is considered a reportable quality measure in surgery patients, significant travel distance should be considered in risk adjustment model calculations.
Conflicts of interest
None declared.
References
- 1.Khuri SF, Henderson WG, Daley J, Jonasson O, Jones RS, Campbell DA, et al. Successful implementation of the Department of Veterans Affairs’ National Surgical Quality Improvement Program in the private sector: the Patient Safety in Surgery study. Ann Surg. 2008;248:329–336. doi: 10.1097/SLA.0b013e3181823485. [DOI] [PubMed] [Google Scholar]
- 2.Dudley RA, Johansen KL, Brand R, Rennie DJ, Milstein A. Selective referral to high-volume hospitals: estimating potentially avoidable deaths. JAMA. 2000;283:1159–1166. doi: 10.1001/jama.283.9.1159. [DOI] [PubMed] [Google Scholar]
- 3.Birkmeyer JD, Siewers AE, Finlayson EV, Stukel TA, Lucas FL, Batista I, et al. Hospital volume and surgical mortality in the United States. N Engl J Med. 2002;346:1128–1137. doi: 10.1056/NEJMsa012337. [DOI] [PubMed] [Google Scholar]
- 4.Urbach DR, Bell CM, Austin PC. Differences in operative mortality between high- and low-volume hospitals in Ontario for five major surgical procedures: estimating the number of lives potentially saved through regionalization. CMAJ. 2003;168:1409–1414. [PMC free article] [PubMed] [Google Scholar]
- 5.Stitzenberg KB, Sigurdson ER, Egleston BL, Starkey RB, Meropol NJ. Centralization of cancer surgery: implications for patient access to optimal care. J Clin Oncol. 2009;27:4671–4678. doi: 10.1200/JCO.2008.20.1715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Livingston EH, Burchell I. Reduced access to care resulting from centres of excellence initiatives in bariatric surgery. Arch Surg. 2010;145:993–997. doi: 10.1001/archsurg.2010.218. [DOI] [PubMed] [Google Scholar]
- 7.Huntsman Cancer Institute. Annual Report, 2009. Available at http://healthcare.utah.edu (last accessed 30 May 2012)
- 8.Google Maps. Google Maps, 2012. Available at http://maps.google.com (last accessed 14 December 2012)
- 9.Rural Health Research Center Instructions for downloading 2004 zip data. ZIP version 2.0 Rural Urban Commuting Area codes, 2006. Available at http://depts.washington.edu/uwruca/ruca-download.php (last accessed 20 July 2012)
- 10.Gamble JM, Eurich DT, Ezekowitz JA, Kaul P, Quan H, McAlister FA. Patterns of care and outcomes differ for urban versus rural patients with newly diagnosed heart failure, even in a universal healthcare system. Circ Heart Fail. 2011;4:317–323. doi: 10.1161/CIRCHEARTFAILURE.110.959262. [DOI] [PubMed] [Google Scholar]
- 11.Doty B, Zuckerman R, Finlayson SRG, Jenkins P, Rieb N, Heneghan S. How does degree of rurality impact the provision of surgical services at rural hospitals? J Rural Health. 2008;24:306–310. doi: 10.1111/j.1748-0361.2008.00173.x. [DOI] [PubMed] [Google Scholar]
- 12.Finlayson SRG, Birkmeyer JD, Toteson ANA, Nease RF. Patient preferences for localization of care: implications for regionalization. Med Care. 1999;37:204–209. doi: 10.1097/00005650-199902000-00010. [DOI] [PubMed] [Google Scholar]
- 13.Hasan O, Meltzer DO, Shaykevich SA, Bell CM, Kaboli PJ, Auerbach AD, et al. Hospital readmission in general medicine patients: a prediction model. J Gen Intern Med. 2010;25:211–219. doi: 10.1007/s11606-009-1196-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Braga M, Capretti G, Pecorelli N, Balzano G, Doglioni C, Ariotti R, et al. A prognostic score to predict major complications after pancreaticoduodenectomy. Ann Surg. 2011;254:702–707. doi: 10.1097/SLA.0b013e31823598fb. [DOI] [PubMed] [Google Scholar]
- 15.Jenkins KJ, Gauvreau K, Newburger JW, Kyn LB, Iezzoni LI, Mayer JE. Validation of relative value scale for congenital heart operations. Ann Thorac Surg. 1998;66:860–869. doi: 10.1016/s0003-4975(98)00495-0. [DOI] [PubMed] [Google Scholar]
- 16.Gawlas I, Sethi M, Winner M, Epelboym I, Lee JL, Schrope BA, et al. Readmission after pancreatic resection is not an appropriate measure of quality. Ann Surg Oncol. 2012;20:1781–1787. doi: 10.1245/s10434-012-2763-y. [DOI] [PubMed] [Google Scholar]
- 17.Borghans I, Kleefstra SM, Kool RB, Westert GP. Is the length of stay in hospital correlated with patient satisfaction? Int J Qual Health Care. 2012;24:443–451. doi: 10.1093/intqhc/mzs037. [DOI] [PubMed] [Google Scholar]