Abstract
Background
Although mortality following pancreaticoduodenectomy is decreasing, postoperative morbidity remains high. It was hypothesized that culture-directed treatment of bacteriobilia would decrease the incidence of infectious complications following pancreaticoduodenectomy.
Methods
In a retrospective study of 197 pancreaticoduodenectomy patients, those in the control group (n = 128, 2005–2009) were given perioperative prophylactic antibiotics, whereas those in the treatment group (n = 69, 2009–2011) were continued on antibiotics until intraoperative bile culture results became available. Patients with bacteriobilia received 10 days of antibiotic treatment, which was otherwise discontinued in patients without bacteriobilia. Various complication rates were compared using Fisher's exact test for categorical variables, Wilcoxon rank sum test for ordinal variables, and a two-sample t-test for continuous variables.
Results
Demographics, comorbidities, baseline clinical characteristics, and intraoperative and postoperative variables were similar between the two groups. There were higher incidences of elevated creatinine (19% versus 4%; P = 0.004) and preoperative hyperglycaemia (18% versus 7%; P = 0.053) in the control group. Fewer patients in the control group underwent preoperative biliary stenting (48% versus 67%; P = 0.017) and intraperitoneal drains were placed at the time of resection more frequently in the control group (85% versus 38%; P < 0.001). Bacteriobilia was found in 59% of patients. Treatment of bacteriobilia was associated with a decrease in the rate of postoperative wound infections (12% in the control group versus 3% in the treatment group; P = 0.036) and overall complication severity score (1 in the control group versus 0 in the treatment group; P = 0.027).
Conclusions
Prolonged antibiotic therapy for bacteriobilia may decrease postoperative wound infection rates after pancreaticoduodenectomy. A randomized prospective trial is warranted to provide evidence to further support this practice.
Introduction
In recent decades, modifications in operative technique and perioperative management have decreased the mortality associated with pancreaticoduodenectomy from the 30% reported in the 1940s to current rates of <3% at most high-volume centres. Despite improvements in mortality, rates of postoperative complications remain high.1 The most common complications following pancreaticoduodenectomy include pancreatic fistula, delayed gastric emptying, wound infection and intra-abdominal abscess. Infectious complications result in longer hospital stays, higher costs, additional invasive procedures and increased patient morbidity. The implementation of measures to reduce infectious complications after pancreaticoduodenectomy would significantly advance the field of pancreatic surgery.
Preoperative biliary stenting has been associated with an increased risk for various postoperative complications, including wound infections and intra-abdominal abscesses.2–4 It has been hypothesized that bacteriobilia associated with biliary stenting is responsible for the increase in infectious complications.3–5 However, many patients undergo biliary stenting prior to being referred to the pancreatic surgeon. Furthermore, bacteriobilia can occur without biliary stenting, particularly after instrumentation of the bile duct.
Culturing the bile at the time of surgery can diagnose bacteriobilia, determine which organisms are present, and identify antibiotic sensitivities. In the present study, it was hypothesized that treatment of positive intraoperative bile cultures would reduce infectious complications following pancreaticoduodenectomy.
Materials and methods
This study was approved by the institutional review board (IRB) of Baylor College of Medicine and its affiliated hospitals. Subsequently, a retrospective cohort study was performed with 197 consecutive patients who underwent pancreaticoduodenectomy carried out by a single surgeon between the years 2005 and 2011 (Fig. 1). The control group (n = 128) comprised patients who underwent pancreaticoduodenectomy during 2005–2009. All of these patients received a single prophylactic dose of preoperative antibiotic (carbapenem 1 g) and one postoperative dose on the first postoperative morning. Patients who were penicillin-allergic were given ciprofloxacin 500 mg and metronidazole 500 mg. No intraoperative bile cultures were obtained as this practice was not performed routinely during pancreatic resections between 2005 and 2009. Beginning in 2009, intraoperative bile cultures were obtained and infections were treated with culture-directed antibiotics. The treatment group (n = 69) therefore consisted of patients who underwent pancreaticoduodenectomy from 2009 to 2011. This group received prophylactic doses of preoperative antibiotics and were continued on antibiotic therapy until intraoperative bile culture results were available. Patients with bacteriobilia received postoperative antibiotics for a total of 10 days. A 10-day regimen was pursued because culture data results are not normally available for 3 days. Therefore, treatment was empiric initially, but tailored when culture data became available. If treatment was modified, patients received appropriate antibiotic therapy for at least 7 days. In patients with negative bile cultures, antibiotics were promptly discontinued. Intravenous antibiotics were used in the immediate postoperative period and oral antibiotics were continued at the time of discharge. Patients with fungi cultured from the bile were treated with fluconazole for 10 days.
Figure 1.
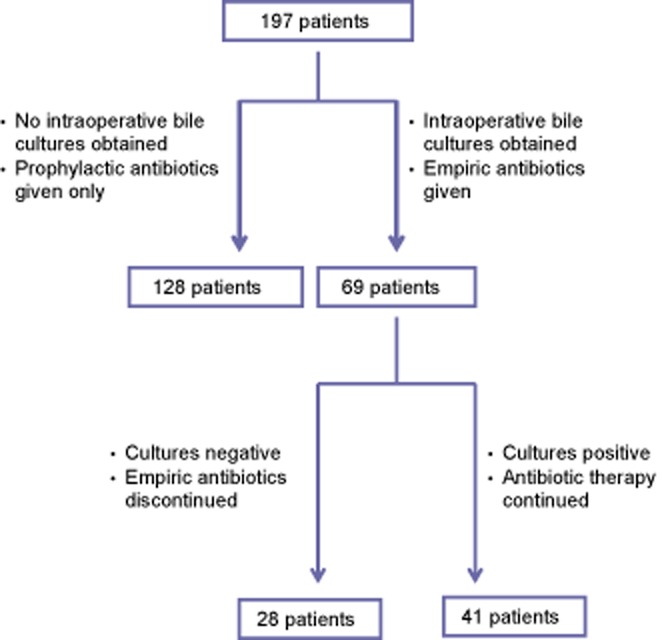
Study design
Outcomes were recorded in a prospectively maintained database and data compared with Fisher's exact test for categorical variables, the Wilcoxon rank sum test for ordinal variables, and a two-sample t-test for continuous variables. A trained data analyst entered data into an IRB-approved prospective database under the supervision of the surgeon. All data were confirmed by source documents and the accuracy of data entered into the electronic database was periodically reviewed.
Demographic information including patient age and gender were obtained from the medical record. A stated medical history of, or presence in the medical record of a history of diabetes mellitus, chronic obstructive pulmonary disease, obesity, smoking, preoperative neoadjuvant chemotherapy or radiation, and preoperative laboratory values including haematocrit, serum creatinine and albumin were recorded. Obesity was defined as a body mass index (BMI) of ≥30 kg/m2. Tobacco status was recorded according to whether the patient had never been, ever been or was currently a smoker. Preoperative anaemia was defined by a haematocrit value of <36%. Renal insufficiency was defined as preoperative serum creatinine of ≥1.2 mg/dl. Hypoalbuminaemia was defined as serum albumin of <3.2 mg/dl. The American Society of Anesthesiologists (ASA) class was obtained from the anaesthesia record. The presence of preoperative biliary stenting was also recorded.
Intraoperative characteristics recorded from the anaesthesia record included administration of preoperative antibiotic within 1 h of incision, intraoperative blood transfusions and operative time, defined as the time from incision to the application of the final wound dressing. Intraoperative hypothermia was defined as a single temperature recording of <36.5 °C. Intraoperative hyperglycaemia was defined as a single blood glucose reading of ≥200 mg/dl. Intraoperative estimated blood loss (EBL) was also obtained from the anaesthesia record, not from the surgeon's operative report. The presence or absence of vein resection and drain insertion were obtained from the surgeon's operative report. All specimens were submitted for pathologic analysis, and the diagnosis and staging were recorded.
All complications occurring within 90 days of the date of surgery were recorded using specific and standardized definitions. Complications were defined and graded in severity using the Common Terminology Criteria for Adverse Events (CTCAE) Version 4.06 (Grades 1–5) unless otherwise stated. Pancreatic fistula was defined and graded using the three-tiered definition proposed by the International Study Group on Pancreatic Fistula (ISGPF).7 Delayed gastric emptying was defined and graded using the schema proposed by the International Study Group of Pancreatic Surgery (ISGPS).8 To calculate the median complication severity composite score (sum of all complication grades for each patient), grades A, B, and C were converted to scores of 1, 2 and 3, respectively, for these complications. The median and interquartile range for the treatment group, control group and entire study population were determined and reported. Hospital length of stay (LoS) was calculated from the day of surgery through to and including the day of discharge during the index admission.
Wound infections were defined as drainage from the operative site with a positive culture or Gram stain. However, if the patient required an intervention such as a bedside incision and drainage procedure, or was documented at another institution to have obvious signs of infection, such as purulent drainage, even if culture data were not obtained, the event was recorded as a wound infection. Pancreaticoduodenectomy patients were followed up by the operating surgeon for 60 days.
Results
Higher incidences of elevated creatinine (19% versus 4%; P = 0.004) and preoperative hyperglycaemia (18% versus 7%; P = 0.053) were observed in the control group, but there was no significant difference in the prevalence of diabetes between the two groups (22% versus 13%; P = 0.156). Fewer patients in the control group underwent preoperative biliary stenting (48% versus 67%; P = 0.017) and intra-peritoneal drains were placed at the time of resection more frequently in the control group (85% versus 38%; P < 0.0001). The treatment and control groups were otherwise similar (Tables 1 and 2).
Table 1.
Demographics and clinical characteristics of the study population
| All patients (n = 197) n (%) | Treated group (n = 69) n (%) | Control group (n = 128) n (%) | P-value | |
|---|---|---|---|---|
| Male | 90 (46) | 40 (58) | 50 (39) | 0.016 |
| Age ≥65 years | 93 (47) | 69 (38) | 57 (46) | 0.370 |
| Obesity (body mass index of ≥30 kg/m2) | 51 (26) | 20 (29) | 31 (24) | 0.499 |
| Diabetes mellitus | 32 (16) | 15 (22) | 17 (13) | 0.156 |
| Preoperative hyperglycaemia (≥200 mg/dl) | 28 (14) | 5 (7) | 23 (18) | 0.053 |
| Chronic obstructive pulmonary disease | 8 (4) | 1 (1) | 7 (6) | 0.265 |
| Smoking history | 117 (59) | 38 (55) | 79 (62) | 0.392 |
| Never | 80 (40) | 31 (45) | 49 (38) | |
| Ever | 72 (37) | 26 (38) | 46 (36) | |
| Current | 45 (23) | 12 (17) | 33 (26) | |
| Preoperative serum albumin <3.2 mg/kl | 17 (8) | 9 (13) | 8 (6) | 0.117 |
| Preoperative anaemia (haematocrit <36) | 85 (43) | 25 (36) | 60 (47) | 0.226 |
| Preoperative serum creatinine ≥1.2 mg/dL | 27 (14) | 3 (4) | 24 (19) | 0.004 |
| Preoperative neoadjuvant therapy | 3 (2) | 3 (4) | 0 | 0.077 |
| ASA class ≥3 | 134 (68) | 49 (71) | 85 (66) | 0.527 |
| Preoperative biliary stent placement | 108 (55) | 46 (67) | 62 (48) | 0.017 |
ASA, American Society of Anesthesiologists.
Table 2.
Intraoperative characteristics of the study population
| All patients (n = 197) | Treated group (n = 69) | Control group (n = 128) | P-value | |
|---|---|---|---|---|
| Preoperative antibiotic within 1 h of incision, n (%) | 197 (100%) | 69 (100%) | 128 (100%) | |
| Intraoperative blood transfusion, n (%) | 37 (19%) | 11 (16%) | 26 (20%) | 0.567 |
| Intraoperative hypothermia (<36.5 °C), n (%) | 193 (98%) | 68 (99%) | 125 (97%) | 1.000 |
| Intraoperative hyperglycaemia (≥200 mg/dl), n (%) | 9 (5%) | 5 (7%) | 4 (3%) | 0.477 |
| Length of operation, min, mean ± SEM | 458 ± 8 | 459 ± 12 | 457 ± 11 | 0.896 |
| Blood loss, ml, mean ± SEM | 541 ± 44 | 471 ± 53 | 579 ± 62 | 0.186 |
| Vein resection, n (%) | 26 (13%) | 12 (17%) | 14 (11%) | 0.270 |
| Drain used, n (%) | 135 (69%) | 26 (38%) | 109 (85%) | <0.001 |
| Pathology, n (%) | 0.003 | |||
| Adenocarcinoma | 104 (53%) | 47 (68%) | 57 (45%) | |
| Pancreatitis | 28 (14%) | 3 (4%) | 25 (20%) | |
| IPMN | 24 (12%) | 5 (7%) | 19 (15%) | |
| Neuroendocrine tumour | 10 (5%) | 4 (6%) | 6 (5%) | |
| Other | 22 (11%) | 8 (12%) | 14 (11%) | |
SEM, standard error of the mean; IPMN, intraductal papillary mucinous neoplasm.
Of the 69 patients in the treatment group from whom intraoperative bile cultures were obtained, 41 (59%) were found to have bacteriobilia (Table 3). Aerobic bacteria were cultured in 32 (78%) patients, anaerobic bacteria in two (5%), mixed aerobic and anaerobic bacteria in six (15%), and fungal organisms in 18 (44%) patients. In the group of patients with bacteriobilia, 34 (83%) had undergone preoperative biliary stenting; among those with biliary candidiasis, six (37%) had undergone preoperative biliary stenting (Table 4).
Table 3.
Microbiology of positive bile, wound, and intra-abdominal abscess cultures
| Bile (n = 41) n (%) | Wound infections (n = 15)a n (%) | Intra-abdominal abscess (n = 13) n (%) | |
|---|---|---|---|
| Anaerobic | 2 (5) | 4 (27) | 4 (27) |
| Aerobic | 32 (78) | 7 (47) | 7 (47) |
| Mixed (anaerobic and aerobic bacteria) | 6 (15) | 3 (20) | 4 (27) |
| Indeterminate culture | 0 | 1 (7) | 0 |
| Fungal | 18 (44) | 1 (7) | 2 (13) |
| Mono-organism | 7 (17) | 11 (73) | 9 (60) |
| Polyorganism | 34 (83) | 4 (27) | 4 (27) |
| Enterococcus spp. | 25 (61) | 7 (47) | 6 (40) |
| Escherichia coli | 11 (27) | 2 (13) | 2 (13) |
| Klebsiella spp. | 16 (39) | 0 | 3 (20) |
| Enterobacter spp. | 9 (22) | 2 (13) | 2 (13) |
| Vancomycin-resistant Enterococcus spp. | 6 (15) | 0 | 2 (13) |
| Streptococcus viridians | 16 (39) | 0 | 0 |
| Other | 32 (78) | 6 (40) | 7 (47) |
| Candida albicans | 13 (72) | 1 (7) | 1 (7) |
| Candida perfingens | 3 (17) | 0 | 0 |
| Candida glabrata | 2 (11) | 0 | 1 (7) |
For three wound infections, culture data were not obtained.
Table 4.
Bile culture positivity among patients with and without preoperative stenting
| Positive bacterial culture n (%) | Positive fungal culture n (%) | |
|---|---|---|
| Preoperative stent | 34 (83) | 6 (37) |
| No preoperative stent | 5 (13) | 1 (2) |
Treatment of positive intraoperative bile cultures with a 10-day course of antibiotics was associated with a decrease in the rate of postoperative wound infections, experienced by 16 (12%) patients in the control group and two (3%) in the treatment group (P = 0.036). Overall complication severity also decreased from a score of 1 in the control group to 0 in the treatment group (P = 0.017) (Table 5). There was no significant difference in the rate of other infectious complications. Hospital LoS was similar in both groups (9.6 days in the control group versus 9.7 days in the treatment group).
Table 5.
90-day outcomes in the study population
| All patients (n = 197) | Treated group (n = 69) | Control group (n = 128) | P-value | |
|---|---|---|---|---|
| Complication severity composite score, median (IQR) | 0 (0–2) | 0 (0–1) | 1 (0–3) | 0.027 |
| Wound infection, n (%) | 18 (9%) | 2 (3%) | 16 (12%) | 0.036 |
| Intra-abdominal abscess, n (%) | 13 (8%) | 7 (10%) | 6 (5%) | 0.227 |
| Wound dehiscence, n (%) | 2 (1%) | 0 | 2 (2%) | 0.543 |
| Pancreatic fistula ≥2, n (%) | 24 (12%) | 6 (9%) | 18 (14%) | 0.363 |
| Grade A (1) | 35 (18%) | 4 (6%) | 31 (24%) | |
| Grade B (2) | 21 (11%) | 4 (6%) | 17 (13%) | |
| Grade C (3) | 3 (2%) | 2 (3%) | 1 (1%) | |
| Delayed gastric emptying, n (%) | 24 (12%) | 6 (9%) | 18 (14%) | 0.363 |
| Pneumonia, n (%) | 4 (2%) | 2 (3%) | 2 (2%) | 0.613 |
| Clostridium difficile colitis, n (%) | 1 (1%) | 1 (1%) | 0 | 0.350 |
| Biliary leak, n (%) | 1 (1%) | 0 | 1 (1%) | 1.000 |
| Myocardial infarction, n (%) | 2 (1%) | 1 (1%) | 1 (1%) | 1.000 |
| New arrhythmia, n (%) | 3 (2%) | 0 | 3 (2%) | 0.553 |
| Urinary tract infection, n (%) | 5 (3%) | 2 (3%) | 3 (2%) | 1.000 |
| Haemorrhage, n (%) | 2 (1%) | 0 | 2 (1%) | 0.541 |
| Acute respiratory distress syndrome, n (%) | 2 (1%) | 0 | 2 (2%) | 0.543 |
| Thrombosis, n (%) | 3 (2%) | 2 (3%) | 1 (1%) | 0.281 |
| Line infection, n (%) | 2 (1%) | 2 (3%) | 0 | 0.122 |
| Length of stay, days, mean ± SEM | 9.6 ± 1 | 9.7 ± 1 | 9.6 ± 1 | 0.930 |
| Readmission within 30 days, n (%) | 24 (12%) | 10 (14%) | 14 (11%) | 0.500 |
| Reoperation within 30 days, n (%) | 5 (3%) | 2 (3%) | 3 (2%) | 1.000 |
IQR, interquartile range; SEM, standard error of the mean.
Discussion
Prior studies have shown that preoperative biliary stenting and bacteriobilia are associated with an increased risk for wound and intra-abdominal infectious complications following pancreaticoduodenectomy.2–5 In this retrospective cohort study of 197 consecutive patients undergoing pancreaticoduodenectomy, culture-directed treatment of bacteriobilia reduced the incidence of wound infections from 12% to 3%. The overall score for complication severity also decreased between the two groups. There was no statistically significant reduction in the incidence of other specific infectious complications.
Recent initiatives such as the National Surgical Quality Improvement Program (NSQIP) and the Surgical Care Improvement Project (SCIP) have focused on controlling factors associated with perioperative infections in an effort to reduce additional health care costs. Furthermore, medical care has now entered an era in which reimbursement is denied when certain ‘preventable’ complications, such as postoperative infections, occur. An analysis of the economic impact of postoperative infections by Duke University reported that these infections are responsible for additional annual hospital charges of US$1.6 bn in the USA alone.9 Patients with methicillin-resistant Staphylococcus aureus (MRSA) surgical site infections have extended hospital stays (median additional days: 5) and incur a 1.19-fold increase in hospital charges per patient.9 At the present study institution, the cost of culture-directed treatment of positive bile cultures was estimated to be around US$400 per patient and although the exact cost to the hospital system of each postoperative infection cannot be calculated, it is estimated to be significantly higher than the cost of treating bacteriobilia, especially if patients with infections require hospital admissions, diagnostic radiology services, interventional radiology procedures, repeated laboratory tests or i.v. antibiotic therapy. Given the incidence of wound infection following pancreaticoduodenectomy, the study of strategies that might potentially reduce this complication is clearly important.
A number of factors have been reported to influence the incidence of postoperative infectious complications. These include smoking, skin preparation, prophylactic antibiotic administration, intraoperative temperature regulation, and blood glucose control.10 These factors were assessed in the current study, but no differences between the two cohorts were identified. However, not all potential confounding factors could be controlled in this retrospective cohort study. The use of preoperative biliary stenting was more frequent in the treatment group. Increased use of biliary stenting would normally be associated with an increase in infectious complications in the treatment group, but, interestingly, there was a decrease in the rate of infectious complications in this group.
Prior studies have focused on the use of preoperative biliary stenting, including the type of stent used, the length of time from stenting to operation, and its effect on infectious complications.11 In clinical practice, a majority of patients undergo biliary stenting prior to referral and preoperative biliary stenting is necessary to allow a patient to travel to a high-volume pancreatic treatment centre at which superior surgical outcomes have been documented.12 In the current study, preoperative biliary stenting confirmed the known association with bacteriobilia.13 However, bacteriobilia also occurs without stenting and is probably secondary to the spread of bacteria or fungus from the stomach or intestine. Bacteriobilia seen in the absence of stenting may also occur secondary to biliary instrumentation or bacteraemia. In the present study, 13% of patients without preoperative biliary stenting had positive bile cultures. Therefore, even if preoperative biliary stenting could be avoided, the problem of bacteriobilia at the time of pancreaticoduodenectomy would persist in some cases.
To the present authors' knowledge, this is the first study to evaluate the impact of treatment of intraoperatively obtained bile cultures during pancreaticoduodenectomy on short-term postoperative outcomes. In this study, there was a non-significant increase in abdominal abscess formation in the treatment group. Interestingly, all but three of the patients who developed an abdominal abscess also had a pancreatic fistula. Prior studies have shown that pancreatic fistula is a significant risk factor for abdominal abscess and these abscesses are often polymicrobial and include non-enteric organisms.13 Treatment of bacteriobilia may be insufficient to prevent abdominal abscess in the setting of a postoperative pancreatic fistula.
The present study is also the first to evaluate the incidence of fungal organisms detected by intraoperative bile culture in patients undergoing pancreaticoduodenectomy. The term ‘biliary candidiasis’ is used to describe the presence of yeast in otherwise sterile bile. Reports of biliary candidiasis over the last few years have increased interest in its prevalence and clinical significance.14 Patients with cancer who have undergone neoadjuvant chemoradiation may be immunosuppressed and at risk for biliary candidiasis.
Among the observed infectious complications, fungi were cultured from one wound infection and two intra-abdominal abscesses. The significance of biliary candidiasis and the value of its treatment are more controversial than the concept of treating bacteriobilia. However, a recent study by Lenz et al. found that Candida is commonly detected in bile, often in association with immunosuppression.14 This group states that positive bile fungal cultures do not simply signify colonization, but are to be considered true infections, and recommend screening for and treating of biliary candidiasis. In this study, patients were not given preoperative anti-fungal therapy. Although the incidence of infections secondary to Candida in this study was relatively low, the effect of treating biliary candidiasis on postoperative complication rates warrants further study.
Inappropriate use of antibiotics has been associated with an increased incidence of colitis and the development of antibiotic resistance.15 The current study did not detect any apparent increase in the incidence of antibiotic-associated colitis when bacteriobilia was treated for 10 days.
The present study was retrospective and subject to associated biases. For example, the administration of empiric antibiotic therapy against bacteriobilia was not randomized and, beginning in 2009, all patients were treated empirically while awaiting intraoperatively obtained bile culture results. The treatment group was therefore compared with a historic control group operated in previous years at the study institution. Over the study period, practice patterns also evolved and the use of intra-abdominal drains following pancreaticoduodenectomy decreased significantly throughout the study period and may confound the interpretation of the impact of treatment of bacteriobilia on the incidence of postoperative infections. However, the two groups comprised a balanced distribution of clinical and operative variables. The authors are also confident that all infections, whether diagnosed during the index admission or in the outpatient clinic setting or at a remote institution closer to the patient's home, were appropriately documented in the database. The sample sizes for the subgroup of patients with bacterial growth from wound infections or abdominal abscesses are small, and a larger study should be conducted to further investigate any potentially causal relationship. It is also unclear whether the provision of empiric, rather than directed, antibiotic therapy would yield different results. Further studies might focus on alternative durations of antibiotic therapy to determine the optimal treatment course. This retrospective cohort study demonstrates that culture-directed treatment of intraoperative bacteriobilia was associated with a decreased incidence of postoperative wound infections among patients undergoing pancreaticoduodenectomy. This retrospective study establishes a foundation upon which future randomized prospective studies further investigating the relationship of bacteriobilia with short-term postoperative infectious complications will be conducted.
Conflicts of interest
There are no conflicts of interest for any of the authors.
References
- 1.Halloran CM, Ghaneh P, Bosonnet L, Hartley MN, Sutton R, Neoptolemos JP. Complications of pancreatic cancer resection. Dig Surg. 2002;19:138–146. doi: 10.1159/000052029. [DOI] [PubMed] [Google Scholar]
- 2.Heslin MJ, Brooks AD, Hochwald SN, Harrison LE, Blumgart LH, Brennan MF. A preoperative biliary stent is associated with increased complications after pancreaticoduodenectomy. Arch Surg. 1998;133:149–154. doi: 10.1001/archsurg.133.2.149. [DOI] [PubMed] [Google Scholar]
- 3.van der Gaag NA, Rauws EAJ, van Eijck CHJ, Bruno MJ, van der Harst E. Preoperative biliary drainage for cancer of the head of the pancreas. N Engl J Med. 2010;362:129–137. doi: 10.1056/NEJMoa0903230. [DOI] [PubMed] [Google Scholar]
- 4.Tol JA, Busch ORC, van der Gaag NA, van Gulik TM, Gouma DJ. The quandary of preresection biliary drainage for pancreatic cancer. Cancer J. 2012;18:550–554. doi: 10.1097/PPO.0b013e31827568b6. [DOI] [PubMed] [Google Scholar]
- 5.Povoski SP, Karpeh MS, Conlon KC, Blumgert LH, Brennan MF. Association of preoperative biliary drainage with postoperative outcome following pancreaticoduodenectomy. Ann Surg. 1999;230:131–142. doi: 10.1097/00000658-199908000-00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.US Department of Health and Human Services. Washington, DC: US DoHHS; 2010. Common Terminology Criteria for Adverse Events (CTCAE) Version 4.03. [Google Scholar]
- 7.Bassi C, Dervenis C, Butturini G, Fingerhut A, Yeo C, Izbicki J, et al. Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery. 2005;138:8–13. doi: 10.1016/j.surg.2005.05.001. [DOI] [PubMed] [Google Scholar]
- 8.Wente MN, Bassi C, Dervenis C, Fingerhut A, Gouma DJ, Izbicki J, et al. Delayed gastric emptying (DGE) after pancreatic surgery: a suggested definition by the International Study Group of Pancreatic Surgery (ISGPS) Surgery. 2007;142:761–768. doi: 10.1016/j.surg.2007.05.005. [DOI] [PubMed] [Google Scholar]
- 9.Engemann JJ, Carmeli Y, Cosgrove SE, Fowler VG, Bronstein MZ, Trivette SL, et al. Adverse clinical and economic outcomes attributable to methicillin resistance among patients with Staphylococcus aureus surgical site infection. Clin Infect Dis. 2003;36:592–598. doi: 10.1086/367653. [DOI] [PubMed] [Google Scholar]
- 10.Lavu H, Klinge MJ, Nowcid LJ, Cohn HE, Grenda DR, Suater PK, et al. Perioperative surgical care bundle reduces pancreaticoduodenectomy wound infections. J Surg Res. 2011;174:215–221. doi: 10.1016/j.jss.2011.09.028. [DOI] [PubMed] [Google Scholar]
- 11.van der Gaag NA, Kloek JJ, de Castro SM, Busch OR, van Gulik TM, Gouma DJ. Preoperative biliary drainage in patients with obstructive jaundice: history and current status. J Gastrointest Surg. 2009;13:814–820. doi: 10.1007/s11605-008-0618-4. [DOI] [PubMed] [Google Scholar]
- 12.Lieberman MD, Kilburn H, Lindsey M, Brennan MF. Relation of perioperative deaths to hospital volume among patients undergoing pancreatic resections for malignancy. Ann Surg. 1995;222:638–645. doi: 10.1097/00000658-199511000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Behrman SW, Zarzaur BL. Intra-abdominal sepsis following pancreatic resection: incidence, risk factors, diagnosis, microbiology, management, and outcome. Am Surg. 2008;74:572–578. [PubMed] [Google Scholar]
- 14.Lenz P, Conrad B, Kucharzik T, Hilker E, Fegeler W, Ullerich H, et al. Prevalence, associations, and trends of biliary tract candidiasis: a prospective observational study. Gastrointest Endosc. 2009;70:480–487. doi: 10.1016/j.gie.2009.01.038. [DOI] [PubMed] [Google Scholar]
- 15.Muto CA, Pokrywka M, Shutt K, Mendelsohn AB, Nouri K, Posey K, et al. A large outbreak of Clostridium difficile-associated disease with an unexpected proportion of deaths and colectomies at a teaching hospital following increased fluoroquinolone use. Infect Control Hosp Epidemiol. 2005;26:273–280. doi: 10.1086/502539. [DOI] [PubMed] [Google Scholar]


