Abstract
Purpose
Tumor-associated neutrophils (TAN) have been reported in a variety of malignancies. We conducted an up-to-date meta-analysis to evaluate the prognostic role of TAN in cancer.
Method
Pubmed, Embase and web of science databases were searched for studies published up to April 2013. Pooled hazard ratios (HRs) and their corresponding 95% confidence intervals (CIs) were calculated. The impact of neutrophils localization and primary antibody were also assessed.
Results
A total of 3946 patients with various solid tumors from 20 studies were included. High density of intratumoral neutrophils were independently associated with unfavorable survival; the pooled HRs were 1.68 (95%CI: 1.36–2.07, I2 = 55.8%, p<0.001) for recurrence-free survival (RFS)/disease-free survival (DFS), 3.36 (95%CI: 2.08–5.42, I2 = 0%, p<0.001) for cancer-specific survival (CSS) and 1.66 (95%CI: 1.37–2.01, I2 = 70.5%, p<0.001) for overall survival (OS). Peritumoral and stromal neutrophils were not statistically significantly associated with survival. When grouped by primary antibody, the pooled HRs were 1.80 (95%CI: 1.47–2.22, I2 = 67.7%, p<0.001) for CD66b, and 1.44 (95%CI: 0.90–2.30, I2 = 45.9%, p = 0.125) for CD15, suggesting that CD66b positive TAN might have a better prognostic value than CD15.
Conclusion
High levels of intratumoral neutrophils are associated with unfavorable recurrence-free, cancer-specific and overall survival.
Introduction
In addition to cancer cells, a tumor lesion contains a number of recruited cells that contribute to the hallmarks of cancer by creating the tumor microenvironment [1]. Stromal cells, blood vessels and infiltrating inflammatory cells are major components of the tumor microenvironment [2]. These cells enable and sustain most of the hallmarks of cancer through reciprocal communications with neoplastic cancer cells [3]. A leukocyte infiltrate, comprising mast cells, T cells, natural killer cells (NK), T-regulatory cells (T-regs), myeloid derived suppressor cells (MDSC), tumor-associated macrophages (TAM) and tumor-associated neutrophils (TAN) are the key participants of the tumor microenvironment where they can promote or inhibit cancer formation and development [4] [5].
Neutrophil granulocytes are the most abundant circulating leukocytes and represent the first line of immune defense against invading pathogens. The role and characteristics of TAN in cancer are poorly defined and has been considered negligible until recently because of their short life span and fully differentiated phenotype [4]. The first report of peripheral blood neutrophils associated with short 5-year survival in humans was published in 1970 [6]. The first study to identify the presence of TAN by use of immunohistochemistry (IHC) as an independent poor prognostic factor in humans and to incorporate TAN into a prognostic risk model based on established clinicopathological features was published in 2006 [7].
Recently, the prognostic role of TAN has been associated with poor clinical outcome in several human cancers, most notably in renal cell carcinoma (RCC) [7], [8], melanoma [9], colorectal cancer (CRC) [10], hepatocellular carcinoma (HCC) [11]–[14], intrahepatic cholangiocarcinoma (ICC) [15], gastric [16], pancreatic ductal carcinoma (PDC) [17] and head and neck cancer (HNC) [18]. However, other studies have demonstrated no relationships between TAN and unfavorable prognosis [19]–[22]. Although compelling, these finding are limited by retrospective design or a single tumor type. In fact, the overall level-1 evidence supporting an excess mortality in patients with high levels of TAN is lacking. Therefore, we performed the first meta-analysis to evaluate the effect of TAN in patients with cancer.
Materials and Methods
Search identification
PubMed, Embase and Web of Science were used to search for the original articles analyzing the prognostic value of TAN in human cancer, by means of keywords variably combined: ‘neutrophil’, ‘tumor-infiltrating neutrophils’, ‘tumor-associated neutrophils’, ‘polymorphonuclear neutrophils’, ‘cancer’, ‘carcinoma’, ‘tumor’, ‘prognosis’, ‘prognostic’, and ‘clinical outcome’. Last search was updated on 25 April 2013, and no lower date limit was used. We also searched for references from the bibliographies of all eligible studies and relevant systematic reviews. At the same time, we contacted the authors of eligible articles whenever the essential data were unavailable from original literatures.
Eligibility criteria
Inclusion and exclusion criteria were made before any meta-analysis of the data. Studies had to meet the following criteria: (1) trials had to deal with human cancer; (2) measure the expression of neutrophils in the tumor tissue; (3) evaluate the association between TAN and the outcome of patients with sufficient details to permit calculation of the hazard ratios (HRs) of each outcome and their 95% confidence intervals (CIs); (4) TAN was dichotomized as ‘high’ and ‘low’ value or equivalent cut-off value; (5) published as a full paper in English. When part or all of the patients were involved in more than one publication, only the most complete or most informative study was included in this analysis.
Data extraction
All the potentially relevant papers were reviewed and extracted independently by two investigators (MX. S. and PP. H.), and the disagreements were resolved by discussion and the controversial parts were adjudicated by a third investigator (JJ. D). In order to ensure the quality of the meta-analysis, we followed the guidelines provided by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [23]. Information retrieved from the researches included author, publication year, country of population, sample size, histology, stage, primary antibody, neutrophils location, cut-off criteria, cut-off value, follow-up time, HR and survival analysis.
Statistical analysis
For the quantitative aggregation of the survival results, we measured the prognostic value of TAN by the HRs and the associated 95% CIs. An extracted HR>1 indicated worse outcome for high level of TAN. The result was considered statistically significant only when the 95% CIs did not overlap with 1. In assessed trials, if HRs and 95% CIs were neither reported directly, nor provided by the authors after request, they were estimated where possible according to the Tierney’s methods [24] (N = 7).
We used the I2 statistics to detect the heterogeneity across different subgroups. Pooled estimates of the prognostic value of TAN were calculated by using the random effect model depending on obvious heterogeneity with I2>50%; otherwise, the fixed effect model was used. Assessment of publication bias was performed using a funnel plot with Begg’s test and the trim-and-fill analysis. A sensitivity analysis was also conducted to test the impact of the outcomes from these eligible studies. All statistical tests were two-sided and differences at p<0.05 were considered statistically significant. Stata Statistical Software (version 12.0 Stata Corp., College Station, TX, USA) was used for all analyses in our analysis.
Results
Identification of relevant studies
Totally 3962 potentially relevant studies were identified after initial searches. Based on titles and abstracts screening 3923 studies were excluded, and the remaining 39 were evaluated in full text. After reviewing the bibliographies of these 39 studies, we added 5 studies to the meta-analysis. Of the 44 candidate studies, 9 studies were not directly related to specific outcomes; 2 studies did not provide enough data to calculate the survival data; 9 studies were related to tumor-infiltrating macrophages, eosinophils or lymphocytes instead of neutrophils; only 1 study reported overlapping data; 2 studies did not evaluate the expression of TAN as dichotomous variables; 1 study regarding bronchioloalveolar carcinoma was excluded because neutrophils were measured in bronchoalveolar lavage fluid rather than tumor tissue. Consequently, 20 articles with a total number of 3946 patients were accepted for our meta-analysis (Fig. 1).
Figure 1. Follow diagram of the meta-analysis.
Characteristics of included studies
The characteristics of retained studies are listed in Table 1. In our analysis, neutrophils were further classified into three groups according to the localizations of neutrophils within the tumor compartments: intratumoral (in tumor nests), peritumoral (an area of stroma adjacented to tumor nests was denoted as peritumoral, if at least one tumor cell was observed in the field of view), and stromal (an area was denoted as stromal if no tumor cells were observed in the peritumoral stroma tissue field of view) [25]. Sample size referred to the number of patients assessed for TAN.
Table 1. Characteristics of included studies.
| First Author | Year | Country of population | Sample size | Histology | Stage | First- antibody | Neutrophils location | Cut-off criteria | Cut-off value | Follow-up time | Hazard ratios | Survival analysis |
| Rosario Alberto Caruso | 2002 | Italy | 273 | Gastric | Ib- IV | - (HE) | Intratumoral | Mean | >10cells/20HPF | NM | Reporta | OS |
| Frede Donskov | 2006 | Denmark | 85 | RCC | NM | CD66b | Intratumoral | Median | 0 cells/mm2 | Median:57m(32–73 m) | Reporta, Authora | OS |
| Hanne Krogh Jensen | 2009 | Denmark | 121 | RCC | I-IV | CD66b | Intratumoral | Median | 0 cells/HPF | Median:124 m (74–194 m) | Reporta+b+c, Authora | RFS, OS, CSS |
| Sokratis Trellakis | 2010 | Germany | 40 | HNC | III -IV | CD66b | Intratumoral | NM | Low: −,+; High: ++,+++ | Median:69 m (43–124m) | SR a | OS |
| Dong-Ming Kuang | 2010 | China | 200 | HCC | I-III | CD15 | Intratumoral, Peritumoral, Stromal | Median | Intratumoral:4; Peritumoral:54; Stromal:10 | NM | SRa+d, Survival curvea+d | DFS, OS |
| Yi-Wei Li | 2011 | China | 281 | HCC | I-III | CD66b | Intratumoral Peritumoral | Fixed | Intratumoral:70%, Peritumoral:50% | Median:29 m (1.5–83m) | Reporta+c, Survival curvea+c | RFS, OS |
| Lih-Chyang Chen | 2012 | China | 140 | HNC | NM | - (HE) | Intratumoral | Mean | 10 neutrophils/ 100 epithelial cells | NM | Survival curvec | RFS |
| Qiang Gao | 2012 | China | 240 | HCC | NM | CD66b | Intratumoral | Median | 12 cells/ mm2 | NM | Reportc | RFS |
| Fang-Ming Gu | 2012 | China | 123 | ICC | I/II/IIIa/ IIIc | CD66b | Intratumoral, Peritumoral | Median | 86 cells/ mm2 | Median:13m (4–111m) | Reporta | OS |
| Marius Ilie | 2011 | France | 632 | NSCLC | I – III | CD66b | Intratumoral | Median | 49 cells/mm2 | Median:30m (0–112 m) | Survival curvea | OS |
| Trine O. Jensen | 2011 | Denmark | 186 | Melanoma | I/II | CD66b | Intratumoral | Fixed | 0 cells/2 HPF | Median:12.2y (10.4–14.2 y) | Reporta+b+c | RFS,OS, CSS |
| Hui-Lan Rao | 2012 | China | 229 | CRC | I-IV | CD66b | Intratumoral | Mean | 60 per TMA spot | Average:55.4m Median:60.0m (0.5–98 m) | Reporta, Survival curvea | OS |
| CH Richards | 2012 | UK | 130 | CRC | NM | - (HE) | Peritumoral | Median | High: score 2–3, Low: score 0–1 | Median:105m (55–163m) | DEb | CSS |
| Jing-jing Zhao | 2012 | China | 115 | Gastric | I-IV | CD15 | Intratumoral | Median | 21.60 cells/HPF | NM | Reporta | OS |
| Shao-Lai Zhou | 2012 | China | 323 | HCC | NM | CD66b | Intratumoral | NM | Hgih, Low | NM | Reporta+c | OS, RFS |
| Andreas Carus | 2013 | Denmark | 101 | CC | IB-IIA | CD66b | Intratumoral, Peritumoral, Stromal | Median | Intratumoral:23.2cells/mm2, Peritumoral:53.1cells/mm2, Stromal:28.3cells/ mm 2 | NM | Authorc, Reportc | RFS |
| Andreas Carus | 2013 | Denmark | 335 | NSCLC | I–IIIA | CD66b | Intratumoral, Peritumoral, Stromal | Median | Intratumoral:8.7cells/mm2, Stromal:21.0 cells/ mm2 | NM | Authora+c | OS, RFS |
| Claudia A. Dumitru | 2013 | Germany | 97 | HNC | NM | CD66b | Intratumoral | Median | NM | NM | Survival curvea | OS |
| Claudia A. Dumitru | 2013 | Germany | 83 | HNC | I-IV | CD66b | Intratumoral | NM | High: medium and strong, Low: negative, weak | NM | Reporta | OS |
| Y Ino | 2013 | Japan | 212 | PDC | NM | CD66b | Intratumoral | Median | NM | Median:18.8m (2.6–201m) | Reporta+d | OS, DFS |
Abbreviations: Gastric: gastric carcinoma; RCC: renal cell carcinoma; HNC: head and neck carcinoma; HCC: hepatocellular carcinoma; ICC: intrahepatic cholangiocarcinoma; NSCLC: non-small-cell lung cancer; CRC: colorectal carcinomas; CC: cervical cancer; PDC: pancreatic ductal carcinoma; HE: hematoxylin-eosin staining; OS: overall survival; CSS: cancer-specific survival; RFS: recurrence-free survival; DFS: disease-free survival; NM: not mentioned; a: OS; b: CSS; c: RFS; d: DFS; m: months; y: years; DE: data extrapolated; SR: systematic review [36].
Eligible studies included 5 studies for HCC (n = 1044) and ICC (n = 123) [11]–[15], 4 studies for HNC (n = 360) [18], [21], [22], [26], 2 studies for non-small-cell lung cancer (NSCLC, n = 967) [20], [27], 2 studies for RCC (n = 206) [7], [8], 2 studies for gastric carcinoma (n = 388) [16], [19], 2 studies for CRC (n = 359) [10], [28] and 1 study for cervical carcinoma (CC, n = 101) [29], melanoma (n = 186) [9] and PDC (n = 212) [17], respectively.
Clinical outcomes were assessed in each study. 16 studies including 3353 patients had overall survival (OS) as the primary endpoint [7]–[12], [14]–[22], [27]. All of 16 studies assessed intratumoral neutrophils; 2 studies assessed peritumoral neutrophils; and 2 studies assessed stromal neutrophils. One study assessed various neutrophil localizations in tumor compartment and had various survival endpoints was included in the analyses repeatedly [30].
10 studies including 2139 patients reported data on recurrence-free survival (RFS)/disease-free survival (DFS) [8], [9], [11]–[14], [17], [20], [26], [29]. All of the 10 studies assessed intratumoral neutrophils, 3 studies assessed peritumoral neutrophils, and 3 studies assessed stromal neutrophils. In addition, 3 studies [8], [9], [28] including 437 patients had cancer-specific survival (CSS) as an endpoint.
Regarding the method to identify TAN, 17 studies used IHC to detect the expression of TAN. The monoclonal antibody against CD66b was used in 15 studies, and the monoclonal antibody against CD15 was used in 2 studies. Hematoxylin-eosin (H&E) stain was used in 3 studies. Neutrophils were assessed by using stereology (5 studies), automatic computerized quantification (4 studies) and semiquantitative methods (11 studies). The expression of TAN was dichotomized into high and low levels or present and absent groups, and the cut-off values for 20 trials were listed in Table 1. A total of 15 studies used the median or mean levels as cut-off values, 2 studies used fixed cut-off values and 3 studies did not mention the detailed information about cut-off criteria.
Meta-analysis
Among the 20 studies, 9 studies presented HRs and 95% CIs for both unadjusted and adjusted classifiers. When both unadjusted and adjusted HRs were extracted from the original papers, the adjusted HRs were included into our analysis. This analysis was denoted as the maximally adjusted association analysis [31], which we mainly discussed below. Inversely if the unadjusted HRs were included into meta-analysis, this analysis was denoted as crude (unadjusted) analysis [31]. All calculated pooled HRs were shown in Table 2. However, there was no obvious difference in the pooled HRs between the maximally adjusted association analysis and the crude analysis.
Table 2. All calculated pooled HRs in meta-analysis.
| GROUP | AREA | OS | RFS/DFS | CSS | |||
| HR(95%CI) | I2 | HR(95%CI) | I2 | HR(95%CI) | I2 | ||
| All cancersa | Intratumoral | 1.66(1.37–2.01) | I2 = 70.5% | 1.68(1.36–2.07) | I2 = 55.8% | 3.36(2.08–5.42) | I2 = 0% |
| Peritumoral | 1.66(0.64–4.32) | I2 = 87.2% | 1.80(0.96–3.37) | I2 = 73.5% | ND | ND | |
| Stromal | 1.10(0.76–1.61) | I2 = 56.8% | 1.27(0.75–2.16) | I2 = 76.8% | ND | ND | |
| HCC and ICCa | Intratumoral | 1.80(1.33–2.43) | I2 = 57.7% | 1.58(1.33–1.88 ) | I2 = 36.9% | ND | ND |
| HNCa | Intratumoral | 1.69(1.10–2.60) | I2 = 0% | ND | ND | ND | ND |
| NSCLCa | Intratumoral | 1.16(1.00–1.35) | I2 = 0% | ND | ND | ND | ND |
| RCCa | Intratumoral | 2.69(1.89–3.83) | I2 = 0.0% | ND | ND | ND | ND |
| Gastrica | Intratumoral | 1.20(0.50–2.89) | I2 = 84.6% | ND | ND | ND | ND |
| CD66ba | Intratumoral | 1.80(1.47–2.22) | I2 = 67.7% | ND | ND | ND | ND |
| CD15a | Intratumoral | 1.44(0.90–2.30) | I2 = 45.9% | ND | ND | ND | ND |
| All cancers b | Intratumoral | 1.85(1.42–2.40) | I2 = 85.1% | 1.68(1.20–2.34) | I2 = 80.6% | 4.99(3.13–7.95) | I2 = 10.1% |
| Peritumoral | 1.28(0.62,2.66) | I2 = 87.8% | 1.78(0.97–3.28) | I2 = 81.8% | ND | ND | |
| Stromal | 1.10(0.76,1.61) | I2 = 56.8% | 1.27(0.75–2.16) | I2 = 76.8% | ND | ND | |
Abbreviations: HCC: hepatocellular carcinoma; ICC: intrahepatic cholangiocarcinoma; HNC: head and neck carcinoma, NSCLC: non-small-cell lung cancer; RCC: renal cell carcinoma; Gastric: gastric carcinoma; ND: not done. OS: overall survival; CSS: cancer-specific survival; RFS: recurrence-free survival; DFS: disease-free survival; a: maximally adjusted association HR ( When both unadjusted and adjusted HRs were extracted from the original papers, the adjusted HRs were included into analysis ); b: crude association HR ( When both unadjusted and adjusted HRs were extracted from the original papers, the unadjusted HRs were included into our analysis).
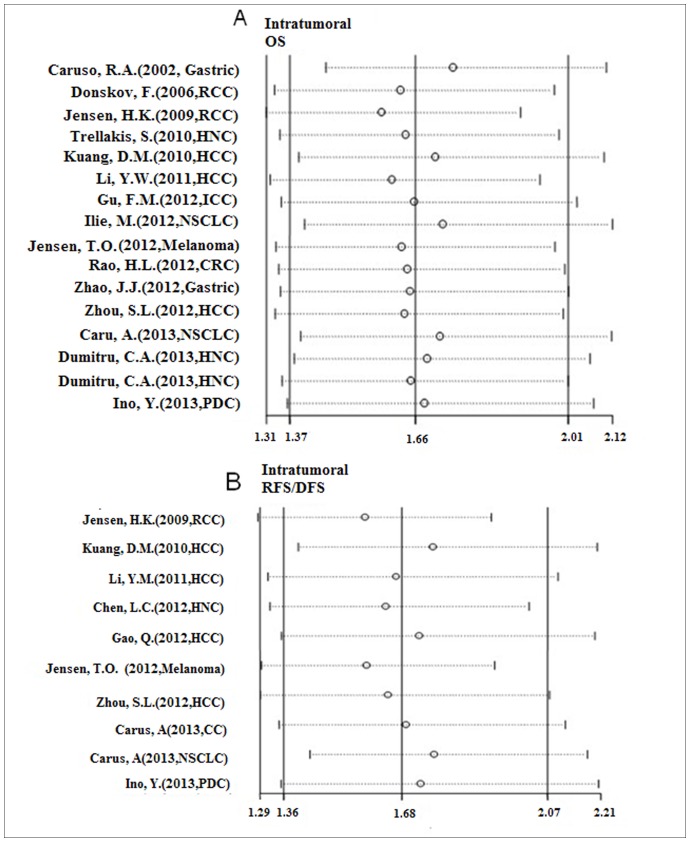
Neutrophils were divided into intratumoral, peritumoral, and stromal in all studies, with survival analyses evaluating OS, CSS, RFS and DFS. For quantitative analyses, we calculated the pooled HRs for all available trials grouped by OS, RFS/DFS, and CSS. Meta-analysis assessing OS as the endpoint were performed in 16 studies, the pooled HR of intratumoral neutrophils was 1.66 (95%CI: 1.37–2.01, I2 = 70.5%) (Fig. 2 A), indicating that high densities of intratumoral neutrophils were independently associated with short survival in various cancers. High densities of neutrophils presented in other areas of the tumor compartments had no statistically significantly association with OS; the combined HRs were 1.66 (95%CI: 0.64–4.32, I2 = 87.2%) for peritumoral and 1.10 (95%CI: 0.76–1.61, I2 = 56.8%) for stromal neutrophils respectively (Table 2).
Figure 2. Forrest plots evaluating maximally adjusted association between TAN and clinical outcomes in all cancers.
(A) Forrest plot to assess the overall effect of TAN on OS in all cancer patients. (B) Forrest plot to assess the overall effect of TAN on RFS/DFS in all cancer patients.
High intratumoral neutrophil levels were significantly associated with short RFS/DFS (HR = 1.68, 95%CI: 1.36–2.07, I2 = 55.8%), whereas peritumoral (HR = 1.80, 95%CI: 0.96–3.37, I2 = 73.5%), and stromal (HR = 1.27, 95%CI: 0.75–2.16, I2 = 76.8%) were not (Fig. 2B). Elevated intratumoral neutrophils densities were also significantly associated with poor CSS (HR = 3.36, 95%CI: 2.08–5.42, I2 = 0%) (Table 2).
Subsequently, in order to further investigate the prognostic role of intratumoral neutrophils in different types of cancers, we grouped eligible studies by cancer types. In HCC and ICC, data demonstrated high intratumoral neutrophils as a prognostic indicator of unfavourable prognosis compared to those with low levels, the pooled HR = 1.80 for OS (95%CI: 1.33–2.43, I2 = 57.7%), and HR = 1.58 (95%CI: 1.33–1.88, I2 = 36.9%) for RFS/DFS (Fig. 3A). High density of TAN was associated with short OS in HNC (HR = 1.69, 95%CI: 1.10–2.60, I2 = 0%) (Fig. 3B), in NSCLC (HR = 1.16, 95%CI: 1.00–1.35, I2 = 0%) (Fig. 3C), in RCC (HR = 2.69, 95%CI: 1.89–3.83, I2 = 0%) (Fig. 3D), but not in gastric carcinoma (HR = 1.20, 95%CI: 0.50–2.89, I2 = 84.6%) (Fig. 3E). Owing to the limitation of the number of eligible studies, the subgroup analyses of melanoma, CC, PDC, and CRC were not performed.
Figure 3. Forrest plots evaluating maximally adjusted association between intratumoral neutrophils and clinical outcomes in subgroups.
HRs of HCC patients are reported as (A). HRs of HNC patients are reported as (B). HRs of NSCLC patients are reported as (C). HRs of RCC patients are reported as (D). HRs of Gastric carcinoma patients are reported as (E).
To evaluate the effect of the primary antibody, studies were grouped according to the primary antibody used. The pooled HR of the studies evaluating OS for intratumoral neutrophils was 1.80 (95%CI: 1.47–2.22, I2 = 67.7%) for CD66b, and 1.44 (95%CI: 0.90–2.30, I2 = 45.9%) for CD15 (Table 2).
Heterogeneity was observed among the 16 indepedent trials which had OS as the endpoint (I2 = 70.5% for intratumral, I2 = 87.2% for peritmoral, and I2 = 56.8% for stromal neutrophils), as well as 10 independent trials which had RFS/DFS as the endpoint (I2 = 55.8% for intratumral, I2 = 73.5% for peritmoral, and I2 = 76.8% for stromal neutrophils). In subgroup analyses of tumor types, heterogeneity was seen in HCC and ICC (I2 = 57.7%) and gastric carcinoma (I2 = 84.6%) evaluating OS for intratumoral neutrophils while no heterogeneity was observed in other subgroups.
Publication bias and Sensitivity analysis
Publication bias was assessed by a funnel plot with Begg’s test and the trim-and-fill analysis. Among involved 16 studies evaluating OS for intratumoral neutrophils, the p value was 0.260 for Begg’s test. And the trim-and-fill analysis imputed 5 studies, which would not alter the results. These methods suggested that no publication bias were observed in the subgroup evaluating OS for intratumoral neutrophils. Moreover, our data indicated that no publication bias were observed among 10 studies evaluating RFS/DFS and intratumoral neutrophils (p = 0.152 for Begg’s test; the trim-and-fill analysis imputed 2 studies, which would not alter the results).
Sensitivity analysis investigates the influence of a single study on the overall meta-analysis estimate, which computes the pooled HRs by omitting one study in each turn. The results of sensitivity analysis show whether the studies are convincing and stable. In our analysis, it demonstrated that all data assessing the prognostic role of intratumoral neutrophil levels in all cancer patients were stable with OS as the endpoint (Fig. 4A), also RFS/DFS as the endpoint (Fig. 4B).
Figure 4. Sensitivity analysis of subgroups.
(A) Sensitivity analysis of studies evaluated intratumoral neutrophils expression on OS. (B) Sensitivity analysis of studies evaluated intratumoral neutrophils expression on RFS/DFS.
Discussion
To our knowledge, this is the first meta-analysis to analyze high levels of intratumoral neutrophils as an independent prognostic factor for short RFS/DFS, CSS, and OS in patients with cancer. Heterogeneity in patient outcomes to surgery or medical intervention has been a challenge for many years. This meta-analysis emphasizes a significant component of that heterogeneity came from differences at the level of neutrophil infiltration within the tumor microenvironment. The fact that different histological types of cancers all share in common the infiltration of neutrophils may point at TAN as a new prognostic factor in cancer that should be further assessed.
The implication of the meta-analysis is that the risk of recurrence or death is increased by at least 66% if elevated levels of intratumoral neutrophils are detected. Thus, patients with intratumoral neutrophils should have a closer follow-up. Intratumoral neutrophils may also serve as a new stratification factor in randomized trials. Moreover, the incorporation of intratumoral neutrophils into current prognostic models based on established and validated clinicopathological features remains a priority.
Inflammatory responses play an important role at different stages of tumor development, invasiveness, and metastasis. However, the role of neutrophils in the tumor microenvironment has been considered negligible until recently [4], in contrast to the well-characterized TAM [30]. Nevertheless, within recent years new data have emphasized an important role of TAN in cancer patients. These clinical observations are strongly supported by functional studies showing that cancer cells and/or other cells within the tumor microenvironment modulate neutrophils to infiltrate the tumor tissue and to acquire tumor-promoting activities, such as angiogenesis [32], migration, invasion, metastasis, mutagenesis or immunosuppression [33]. Neutrophils cross-talk with tumor cells through the production of cytokines and other molecules [34] and through the interaction with other cells in the tumor microenvironment [35]. Importantly, in well-established invasive human cancer the negative prognostic role of TAN has been surprisingly consistent and clear [36]. The present meta-analysis adds to this evidence and should prompt further research in this area.
In our analysis, we pooled 20 studies including 3946 patients and observed high densities of intratumoral neutrophils statistically associated with unfavorable OS. This was apparent for all cancers combined and for all subtypes of cancers except gastric carcinoma. The conflicting results in gastric carcinoma emphasize the importance of using modern IHC in the assessments of intratumoral neutrophils. Though the result in NSCLC was borderline value with 95%CI of 1.0–1.35, many meta-analyses would consider this statistically significant [37] [38]. More research is needed to validate results as the number of studies in each type of cancer was small. In addition, high levels of intratumoral neutrophils were significantly associated with short RFS/DFS and CSS especially in HCC. However, the pooled HRs of peritumoral and stromal neutrophils were not statistically significant. These results may suggest that neutrophils infiltrated in the tumor nests were the most accurate predictor of poor outcome in human cancer. However, the results obtained in the peritumoral and stromal compartments should be interpreted cautiously as the number of studies assessing neutrophils in various tumor compartment localizations was low (n = 4) and HRs for the peritumoral neutrophil had approximately the same level (HR range 1.66–1.8) as for the intratumoral neutrophil assessments. This may reflect the importance of neutrophil activity in the tumor nests and the migrating tumor border where the reciprocal communications between tumor cells and infiltrating neutrophils may be anticipated to be high and this should be further studied. However, systematic assessments of neutrophils in the different compartments, i.e, intratumoral, peritumoral and stromal, and the correlation of these cell subsets with other clinicopathological features and clinical outcome are cumbersome and technically challenging. It has been suggested that a simple estimate of the overall number of neutrophils relative to the overall number of CD8+ lymphocytes in the global tumor area is easier and faster and clinically translatable in terms of prognostic significance [29].
We assessed the impact of the primary antibody. Data indicated that CD66b positive TAN might have better prognostic value than CD15. However, in the subgroup which had OS as the endpoint, data should be interpreted cautiously as the number of studies assessing intratumoral neutrophils with the CD15 antibody was small (n = 2). Leukocytes express many cell surface markers, but CD66b is restricted to activated neutrophils [39] [40]. While CD15, also called sialyl Lewis x (sLex), is expressed on the surface of leukocytes [41], mainly in neutrophils, eosnophils, and part of monocytes, and do not reflect the activation status of neutrophils. In addition, CD15 has been demonstrated to be expressed occasionally on tumor cells [42], [43]. No study has assessed both antibodies in parallel.
The assessment methods of TAN were varied in the present study. Semiquantitative methods are easy and fast but subjective and inter-observer variations may exist. Stereology assessments are objective and reproducible but laborious, cumbersome and require specialized training. Digital image analysis (DIA) is an emerging, high-throughput method for automated quantitative assessments of immunostained sections but may still be sensitive to variation by tissue processing, IHC protocols, nonspecific staining, and definition of region-of-interest. However, for clinical relevance and applicability of TAN assessments more efficient methods are warranted. Recently, a comparative study demonstrated DIA protocols to provide fast, robust, and potentially clinically applicable results with prognostic information comparable to the considerably cumbersome stereology method [44].
Several sources of heterogeneity should be considered in the present study. Statistical heterogeneity may due to the differences in the types of carcinomas, the method and evaluation of staining, primary antibody, neutrophil localization, assessment method, cut-off criteria, cut-off value, the variables used for matching and adjustment. Though all mentioned potential biases, the data were stable and convincing, as demonstrated by sensitivity analysis and the trim-and-fill analysis.
We did not estimate the pooled HRs in all adjusted data as the HRs of some negative results were not reported in stepwise Cox regression analyses because they were not in the equation. Cut-off values were different in each study. 14 studies used the median or mean levels as cut-off values, and only 1 study used fixed cut-off value. It emphasizes the importance of confirming a “standardized” cut-off value for future studies. Furthermore, different primary antibodies and methods for evaluating staining might result in different results. Therefore, to improve the quality of researches, future standardized protocols are needed.
Our study has limitations. First, all eligibly literatures in this meta-analysis were published in English. This may under represent negative studies in the meta-analysis [45]. Second, several elements might affect the pooled HRs, such as the differences in the country of population, characteristics of patients, follow-up time, cut-off criteria, cut-off value and the variables used for matching and adjustment. Third, there were some minor differences between the exact HR and the extrapolated data, according to Tierney’s method [24].
Conclusion
In summary, the meta-analysis demonstrated high levels of intratumoral neutrophils were significantly associated with unfavorable survival and recurrence in human cancer, especially in HCC and ICC, HNC, NSCLC and RCC. Moreover, the CD66b primary antibody might be a better choice for evaluating the prognostic role of TAN rather than CD15 since the CD66b-positive antigen is assigned to activated neutrophils. Further research to understand the mechanism and functionality of TAN in cancer are encouraged.
Supporting Information
PRISMA Checklist.
(DOC)
Acknowledgments
The authors would like to thank all the investigators of the primary studies and all the members of our team. In addition, we thank FD, Hanne Krogh Jensen, and Andreas Carus for providing us the unpublished data.
Funding Statement
The work was supported by Provincial science and technology development plan of Shandong (2012GG0021836), Provincial Natural Science Foundation of Shandong (ZR2013HZ001). FD has received research grant from Health Research Fund of Central Denmark Region and the Danish Cancer Society. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Hanahan D, Weinberg RA (2011) Hallmarks of cancer: the next generation. Cell 144: 646–674. [DOI] [PubMed] [Google Scholar]
- 2. Mantovani A, Allavena P, Sica A, Balkwill F (2008) Cancer-related inflammation. Nature 454: 436–444. [DOI] [PubMed] [Google Scholar]
- 3. Hanahan D, Coussens LM (2012) Accessories to the crime: functions of cells recruited to the tumor microenvironment. Cancer Cell 21: 309–322. [DOI] [PubMed] [Google Scholar]
- 4. Galdiero MR, Bonavita E, Barajon I, Garlanda C, Mantovani A, et al. (2013) Tumor associated macrophages and neutrophils in cancer. Immunobiology 218: 1402–1410. [DOI] [PubMed] [Google Scholar]
- 5. Donskov F, Bennedsgaard KM, Hokland M, Marcussen N, Fisker R, et al. (2004) Leukocyte orchestration in blood and tumour tissue following interleukin-2 based immunotherapy in metastatic renal cell carcinoma. Cancer Immunol Immunother 53: 729–739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Riesco A (1970) Five-year cancer cure: relation to total amount of peripheral lymphocytes and neutrophils. Cancer 25: 135–140. [DOI] [PubMed] [Google Scholar]
- 7. Donskov F, von der Maase H (2006) Impact of immune parameters on long-term survival in metastatic renal cell carcinoma. J Clin Oncol 24: 1997–2005. [DOI] [PubMed] [Google Scholar]
- 8. Jensen HK, Donskov F, Marcussen N, Nordsmark M, Lundbeck F, et al. (2009) Presence of intratumoral neutrophils is an independent prognostic factor in localized renal cell carcinoma. J Clin Oncol 27: 4709–4717. [DOI] [PubMed] [Google Scholar]
- 9. Jensen TO, Schmidt H, Moller HJ, Donskov F, Hoyer M, et al. (2012) Intratumoral neutrophils and plasmacytoid dendritic cells indicate poor prognosis and are associated with pSTAT3 expression in AJCC stage I/II melanoma. Cancer 118: 2476–2485. [DOI] [PubMed] [Google Scholar]
- 10. Rao HL, Chen JW, Li M, Xiao YB, Fu J, et al. (2012) Increased intratumoral neutrophil in colorectal carcinomas correlates closely with malignant phenotype and predicts patients' adverse prognosis. PLoS One 7: e30806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Li YW, Qiu SJ, Fan J, Zhou J, Gao Q, et al. (2011) Intratumoral neutrophils: a poor prognostic factor for hepatocellular carcinoma following resection. J Hepatol 54: 497–505. [DOI] [PubMed] [Google Scholar]
- 12. Kuang DM, Zhao Q, Wu Y, Peng C, Wang J, et al. (2011) Peritumoral neutrophils link inflammatory response to disease progression by fostering angiogenesis in hepatocellular carcinoma. J Hepatol 54: 948–955. [DOI] [PubMed] [Google Scholar]
- 13. Gao Q, Zhao YJ, Wang XY, Qiu SJ, Shi YH, et al. (2012) CXCR6 upregulation contributes to a proinflammatory tumor microenvironment that drives metastasis and poor patient outcomes in hepatocellular carcinoma. Cancer Res 72: 3546–3556. [DOI] [PubMed] [Google Scholar]
- 14. Zhou SL, Dai Z, Zhou ZJ, Wang XY, Yang GH, et al. (2012) Overexpression of CXCL5 mediates neutrophil infiltration and indicates poor prognosis for hepatocellular carcinoma. Hepatology 56: 2242–2254. [DOI] [PubMed] [Google Scholar]
- 15. Gu FM, Gao Q, Shi GM, Zhang X, Wang J, et al. (2012) Intratumoral IL-17(+) cells and neutrophils show strong prognostic significance in intrahepatic cholangiocarcinoma. Ann Surg Oncol 19: 2506–2514. [DOI] [PubMed] [Google Scholar]
- 16. Zhao JJ, Pan K, Wang W, Chen JG, Wu YH, et al. (2012) The prognostic value of tumor-infiltrating neutrophils in gastric adenocarcinoma after resection. PLoS One 7: e33655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Ino Y, Yamazaki-Itoh R, Shimada K, Iwasaki M, Kosuge T, et al. (2013) Immune cell infiltration as an indicator of the immune microenvironment of pancreatic cancer. Br J Cancer 108: 914–923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Trellakis S, Bruderek K, Dumitru CA, Gholaman H, Gu X, et al. (2010) Polymorphonuclear granulocytes in human head and neck cancer: enhanced inflammatory activity, modulation by cancer cells and expansion in advanced disease. Int J Cancer 129: 2183–2193. [DOI] [PubMed] [Google Scholar]
- 19. Caruso RA, Bellocco R, Pagano M, Bertoli G, Rigoli L, et al. (2002) Prognostic value of intratumoral neutrophils in advanced gastric carcinoma in a high-risk area in northern Italy. Mod Pathol 15: 831–837. [DOI] [PubMed] [Google Scholar]
- 20. Carus A, Ladekarl M, Hager H, Pilegaard H, Nielsen PS, et al. (2013) Tumor-associated neutrophils and macrophages in non-small cell lung cancer: No immediate impact on patient outcome. Lung Cancer 81(1): 130–137. [DOI] [PubMed] [Google Scholar]
- 21. Dumitru CA, Bankfalvi A, Gu X, Eberhardt WE, Zeidler R, et al. (2013) Neutrophils Activate Tumoral CORTACTIN to Enhance Progression of Orohypopharynx Carcinoma. Front Immunol 4: 33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Dumitru CA, Bankfalvi A, Gu X, Zeidler R, Brandau S, et al. (2013) AHNAK and inflammatory markers predict poor survival in laryngeal carcinoma. PLoS One 8: e56420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Group P (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6: e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Tierney JF, Stewart LA, Ghersi D, Burdett S, Sydes MR (2007) Practical methods for incorporating summary time-to-event data into meta-analysis. Trials 8: 16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Nedergaard BS, Nielsen K, Nyengaard JR, Ladekarl M (2007) Stereologic estimation of the total numbers, the composition and the anatomic distribution of lymphocytes in cone biopsies from patients with stage I squamous cell carcinoma of the cervix uteri. APMIS 115: 1321–1330. [DOI] [PubMed] [Google Scholar]
- 26. Chen LC, Wang LJ, Tsang NM, Ojcius DM, Chen CC, et al. (2012) Tumour inflammasome-derived IL-1beta recruits neutrophils and improves local recurrence-free survival in EBV-induced nasopharyngeal carcinoma. EMBO Mol Med 4: 1276–1293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Ilie M, Hofman V, Ortholan C, Bonnetaud C, Coelle C, et al. (2012) Predictive clinical outcome of the intratumoral CD66b-positive neutrophil-to-CD8-positive T-cell ratio in patients with resectable nonsmall cell lung cancer. Cancer 118: 1726–1737. [DOI] [PubMed] [Google Scholar]
- 28. Richards CH, Flegg KM, Roxburgh CSD, Going JJ, Mohammed Z, et al. (2012) The relationships between cellular components of the peritumoural inflammatory response, clinicopathological characteristics and survival in patients with primary operable colorectal cancer. British Journal of Cancer 106: 2010–2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Carus A, Ladekarl M, Hager H, Nedergaard BS, Donskov F (2013) Tumour-associated CD66b neutrophil count is an independent prognostic factor for recurrence in localised cervical cancer. Br J Cancer 108(10): 2116–2122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Zhang QW, Liu L, Gong CY, Shi HS, Zeng YH, et al. (2012) Prognostic significance of tumor-associated macrophages in solid tumor: a meta-analysis of the literature. PLoS One 7: e50946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Castillo JJ, Dalia S, Shum H (2011) Meta-analysis of the association between cigarette smoking and incidence of Hodgkin's Lymphoma. J Clin Oncol 29: 3900–3906. [DOI] [PubMed] [Google Scholar]
- 32. Tazzyman S, Niaz H, Murdoch C (2013) Neutrophil-mediated tumour angiogenesis: subversion of immune responses to promote tumour growth. Semin Cancer Biol 23: 149–158. [DOI] [PubMed] [Google Scholar]
- 33. Dumitru CA, Lang S, Brandau S (2013) Modulation of neutrophil granulocytes in the tumor microenvironment: mechanisms and consequences for tumor progression. Semin Cancer Biol 23: 141–148. [DOI] [PubMed] [Google Scholar]
- 34. Tecchio C, Scapini P, Pizzolo G, Cassatella MA (2013) On the cytokines produced by human neutrophils in tumors. Semin Cancer Biol 23: 159–170. [DOI] [PubMed] [Google Scholar]
- 35. Brandau S, Moses K, Lang S (2013) The kinship of neutrophils and granulocytic myeloid-derived suppressor cells in cancer: cousins, siblings or twins? Semin Cancer Biol 23: 171–182. [DOI] [PubMed] [Google Scholar]
- 36. Donskov F (2013) Immunomonitoring and prognostic relevance of neutrophils in clinical trials. Semin Cancer Biol 23(3): 200–207. [DOI] [PubMed] [Google Scholar]
- 37. Kliiman K, Altraja A (2010) Predictors and mortality associated with treatment default in pulmonary tuberculosis. Int J Tuberc Lung Dis 14: 454–463. [PubMed] [Google Scholar]
- 38. Chlebowski RT, Anderson GL, Gass M, Lane DS, Aragaki AK, et al. (2010) Estrogen plus progestin and breast cancer incidence and mortality in postmenopausal women. JAMA 304: 1684–1692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Murdoch C, Muthana M, Coffelt SB, Lewis CE (2008) The role of myeloid cells in the promotion of tumour angiogenesis. Nat Rev Cancer 8: 618–631. [DOI] [PubMed] [Google Scholar]
- 40. Skubitz KM, Campbell KD, Skubitz AP (1996) CD66a, CD66b, CD66c, and CD66d each independently stimulate neutrophils. J Leukoc Biol 60: 106–117. [DOI] [PubMed] [Google Scholar]
- 41. Phillips ML, Nudelman E, Gaeta FC, Perez M, Singhal AK, et al. (1990) ELAM-1 mediates cell adhesion by recognition of a carbohydrate ligand, sialyl-Lex. Science 250: 1130–1132. [DOI] [PubMed] [Google Scholar]
- 42. Jang TJ, Park JB, Lee JI (2013) The Expression of CD10 and CD15 Is Progressively Increased during Colorectal Cancer Development. Korean J Pathol 47: 340–347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Tori A, Harada A, Nakao A, Nonami T, Ito M, et al. (1995) Expression of sialyl Lewis(x) in hepatocellular carcinoma. Hepatogastroenterology 42: 939–943. [PubMed] [Google Scholar]
- 44.Carus A, Donskov F, Nielsen PS, Hager H, Nedergaard BS, et al.. (2014) Strong prognostic value of tumor-infiltrating neutrophils and lymphocytes assessed by automated digital image analysis in early stage cervical cancer: A comparator study with observer-assisted stereological assessments. J OncoPathology 2:1-9.
- 45. Egger M, Zellweger-Zahner T, Schneider M, Junker C, Lengeler C, et al. (1997) Language bias in randomised controlled trials published in English and German. Lancet 350: 326–329. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
PRISMA Checklist.
(DOC)