Abstract
Context
Medicaid is the largest payer of mental health (MH) care in the United States, and this role will increase among states that opt into the Medicaid expansion. However, due to the dearth of MH providers who accept Medicaid, expanded coverage may not increase access to services. Facilities that provide specialty outpatient MH services and accept Medicaid comprise the backbone of the community-based treatment infrastructure for Medicaid enrollees. For states that opt into the expansion, it is important to understand which local communities may face the greatest barriers to access these facilities.
Objective
Examine the availability of outpatient MH facilities that accept Medicaid across U.S. counties, and whether specific types of communities are more likely to lack this infrastructure.
Design
Data from the 2008 National Survey of Mental Health Treatment Facilities and Area Resource File were merged. A generalized ordered logistic regression with state fixed effects was estimated to examine determinants of accessibility of these facilities. Covariates included the percentage of residents who are Black, Hispanic, living in poverty, and living in a rural area.
Participants
U.S. Counties
Main Outcome Measure
An ordered variable assessed whether a county had no access to outpatient MH facilities that accept Medicaid, intermediate access to these facilities (i.e., ≥ one facility, but not top quintile of facility to Medicaid enrollee per capita ratio), or high access (i.e., top quintile of facility to Medicaid enrollee per capita ratio).
Results
Over one-third of counties do not have any outpatient MH facilities that accept Medicaid. Communities with a larger percentage of residents who are Black (Marginal Effect [ME]=3.9%; 95% CI=1.2%,6.6%), Hispanic (ME=4.8%; 95% CI=2.3%,7.4%), or living in a rural area (ME=27.9%; 95% CI=25.3%,30.4%) are more likely to lack these facilities.
Conclusion
Many communities may face constraints on the MH safety-net system as Medicaid is expanded, especially rural communities and communities of color.
INTRODUCTION
Medicaid is the single largest payer of mental health (MH) care in the United States,1 and disproportionately serves the sickest and most disabled group of persons with mental disorders. Compared to general population samples, a higher proportion of Medicaid enrollees have severe mental disorders such as schizophrenia, major depression, and bipolar disorder.2 Under the Patient Protection and Affordable Care Act (PPACA), states that opt into the Medicaid expansion will allow individuals with income below 133% of the federal poverty level (FPL) to enroll in the Medicaid program. If the expansion were implemented nationwide, up to16 million enrollees would be added to Medicaid by 2019 and the proportion of persons with mental disorders who are covered by Medicaid would double from 12.8% to 24.5%.3, 4
Originally, the PPACA compelled states to participate in the expansion by stipulating that all federal funding for the Medicaid program would be withheld from those that did not expand their program. However, the landmark decision by the Supreme Court (i.e., National Federation of Independent Business et al. versus Sebelius et al.) in June, 2012 determined that this provision of the PPACA was unconstitutional, thereby granting states more discretion to participate in the expansion. Although, there is uncertainty as to how many states will opt in,5 there is reason to believe that many states will participate given that the expansion is fully funded by federal dollars in the first three years and 90% funded by federal dollars in 2020 and beyond.6
The potential of the expansion to improve access to and quality of MH care in participating states requires an adequate supply of MH providers who accept Medicaid across local communities. Yet, four out of five U.S. counties were designated by the Health Resources and Services Administration (HRSA) as partial or whole Mental Health Professional Shortage Areas in 2008,7 and this shortage is further exacerbated for Medicaid enrollees by low rates of MH provider participation in Medicaid.8, 9 Although the majority of psychiatrists practice in solo or group office settings (51%),10 only 3% and 8% of patient caseloads in these settings are covered by Medicaid, respectively.11 Rather, MH providers who participate in Medicaid tend to be concentrated in hospital and specialty community-based MH clinic settings.11 Consequently, outpatient clinics that provide specialty MH services and accept Medicaid comprise the backbone of the community-based MH system for Medicaid enrollees.
For states that opt into the expansion, it is especially important to know which communities may face the greatest constraints in access to facilities that accept Medicaid enrollees. Prior studies on the supply and distribution of other types of healthcare resources suggest that community characteristics –especially racial/ethnic composition and rural residence -- may affect accessibility to care. More specifically, communities of color are more likely to experience physician shortages, and closures of hospitals, emergency departments, and trauma centers, controlling for socioeconomic factors.12–15 Furthermore, rural communities have chronically suffered from shortages of all types of health care providers.16
To examine the geographic distribution of MH facilities that provide outpatient care for Medicaid enrollees, we merge national data from two sources to examine which communities are most likely to have these crucial resources. Specifically, we explore associations between community sociodemographic characteristics and the availability of outpatient MH treatment facilities that accept Medicaid, controlling for state-level confounders. We hypothesize that communities of color and rural communities are less likely to have outpatient MH treatment facilities that serve Medicaid clients.
METHOD
Data
Data come from the 2008 National Survey of Mental Health Treatment Facilities (NSMHTF) and the Area Resource File (ARF). The NSMHTF is a survey conducted by the Substance Abuse and Mental Health Services Administration (SAMHSA) in all 50 states, Washington D.C., and U.S. territories to provide key information about MH treatment facilities that meet the following criteria: (1) Formal establishment by law, regulation, charter, license, or agreement; (2) An established organizational structure, including a staffing structure; (3) A primary goal for all or part of the facility of improving the MH of its clientele; (4) A clientele with psychiatric, psychological, or associated social adjustment impairments; and (5) Provision of MH services.
Facilities that are surveyed include psychiatric hospitals, nonfederal general hospitals with separate psychiatric inpatient units, Veterans Affairs medical centers with separate psychiatric services, residential treatment centers, freestanding outpatient clinics/partial care facilities, and multiservice mental health facilities. Individual and small group mental health practices, correctional facilities, military facilities that are not operated by the Veterans Affairs, and Indian Health Service facilities are excluded from the survey. To build the sampling framework for the 2008 survey, SAMHSA used 14 sources of information including lists from State Mental Health Agencies, the National Council for Community Behavioral Healthcare, the National Association of Psychiatric Health Systems, and the National Association of Children’s Behavioral Healthcare. Of 13,068 facilities that were surveyed, a response rate of 74.2% was obtained.
Facility-level data were aggregated to the county level using the facility zip code. County-level data from the 2008 NSMHTF were merged with data from the ARF, a county-specific health resources data file that also contains county-level sociodemographic measures.7
Measures
Dependent Variable
The NSMHTF includes facility-level measures of the type of health insurance that the facility accepts and the settings in which services are provided (e.g. inpatient, residential treatment, and outpatient). Using this information, we calculated the number of outpatient MH facilities that accepted Medicaid in the county and divided this number by the number of Medicaid enrollees in the county in 2007 (mean=2.4 facilities per 10,000 Medicaid enrollees). Based on this ratio, we divided counties into the following three categories: (1) No access -- Counties with no outpatient MH facilities that accept Medicaid; (2) Intermediate access -- Counties with at least one MH facility that accepts Medicaid, but not classified in the top quintile of this ratio (i.e., fewer than 3.1 of these facilities per 10,000 Medicaid enrollees); and (3) High access – Counties with at least one MH facility that accepts Medicaid and classified in the top quintile of this ratio.
Independent Variables
County-level covariates were assessed with the most recent year of data available preceding the year in which the dependent variable was measured (i.e., 2008). County racial/ethnic composition was assessed with the percentage of county residents who are Black (2007) and Hispanic (2007). Rurality was measured by the percentage of county residents living in a rural area as defined by the U.S. Census Bureau (2000).17 Analyses also adjusted for the percentage of residents living in poverty in 2007 (i.e., below 100% of the federal poverty level).
Data Analysis
We derived an analytic sample of 3,141 U.S. counties with complete information on analytic variables from all 50 U.S. states. One county in Virginia, Clifton Forge City, was excluded due to missing demographic information in the ARF. Within this analytic sample of 3,141 U.S. counties, 9,595 facilities responded to the survey and 7,143 provided outpatient MH services. Of the facilities that provided outpatient services, 6,149 (i.e., 86.1%) accepted Medicaid.
Bivariate analysis was conducted using one-way analysis of variance (ANOVA) and χ2 tests. Generalized ordered logistic regression was performed to estimate the association between each explanatory variable and the likelihood that a county is classified as having no access to outpatient MH facilities that accept Medicaid or high access to these facilities. This model was selected instead of an ordered logistic regression because the proportional odds assumption failed.18
To adjust for state-level heterogeneity in demographics and policies that may influence the availability of MH care resources across local communities,19, 20 regressions were estimated with state fixed effects using Stata version 11 (StataCorp LP).21 Marginal effects were calculated for each explanatory variable at the mean value of other predictor variables in the model. Independent variables were standardized for ease of interpretation such that marginal effects correspond to a one standard deviation increase in the measure above the mean value.
To control for differences in missing information at the facility-level across counties, regressions also included an indicator variable for counties that have any facility with missing survey information precluding it from inclusion in the creation of the dependent variables (i.e., facility did not respond to survey or had missing information on measures used to create dependent variable). Note that 26.5% of facilities had missing information due to survey non-response or missing survey information, and 35.1% of counties have at least one facility with missing information. Counties that have facilities with missing information have a higher proportion of Black residents, but a lower proportion of residents who are living in poverty or rural communities (p<0.001).
Results
A total of 34.8% of U.S. counties have no outpatient MH treatment facilities that accept Medicaid (Table 1); this figure is nearly identical when the data are limited to counties with complete facility-level information (N=2,037, not shown). Results from the one-way ANOVA indicate that counties with no outpatient MH facilities that accept Medicaid have a higher percentage of residents who live in rural communities and who live in poverty compared to counties with intermediate and high access to these facilities (p<0.001). Additionally, counties classified as having high access to Medicaid MH facilities have a lower percentage of Black and Hispanic residents than counties with no access or intermediate access to these facilities (p<0.05).
Table 1.
County Sociodemographic Characteristics by Access to Mental Health Outpatient Treatment Facilities that Accept Medicaid
| Characteristic | Total N=3,141 |
No Access N=1,094 |
Intermediate Access N=1,410 |
High Access N=637 |
P-value |
|---|---|---|---|---|---|
|
| |||||
| Mean (SD), % | Mean (SD), % | Mean (SD),% | Mean (SD), % | ||
| Black | 9.1 (14.4) | 9.1 (15.3) | 10.9 (14.8) | 5.1 (10.8) | <0.001 |
| Hispanic | 7.5 (12.7) | 7.6 (13.4) | 7.9 (12.5) | 6.3 (11.5) | 0.03 |
| Living in Poverty | 15.1 (6.2) | 15.7 (6.5) | 15.1 (6.1) | 14.0 (6.1) | <0.001 |
| Living in Rural Community | 59.9 (31.0) | 76.0 (27.1) | 45.5 (27.8) | 64.8 (28.9) | <0.001 |
Notes: One-way analyses of variance were performed; p < 0.05 suggests that at least one of the three categories is significantly different from the others. Access categories were defined by dividing the number of mental health outpatient treatment facilities that accept Medicaid by the number of Medicaid enrollees in the county and classifying each county as offering: (1) No access –i.e., no outpatient mental health facility that accepts Medicaid; (2) Intermediate access – i.e, at least one facility, but not classified in the top quintile of this ratio [3.1 facilities per 10,000 Medicaid enrollees]; (3) High access – i.e., at least one facility and classified in the top quintile of this ratio.
Consistent with our hypothesis, communities of color have less access to outpatient MH facilities that accept Medicaid (Table 2). Counties with a higher percentage of Black residents (ME = 3.9%, 95% CI=1.2%, 6.6%) and Hispanic residents (ME= 4.8%, 95% CI= 2.3%, 7.4%) are more likely to lack these facilities than counties with a lower percentage of Black residents and Hispanic residents, respectively. Similarly, counties with a higher percentage of Black residents (ME= −2.7%, 95% CI= −4.6%, −0.8%) and Hispanic residents (ME= −3.4%, 95% CI= −5.1%, −1.6%) are less likely to have high access to these facilities than counties with a lower percentage of Black residents and Hispanic residents, respectively.
Table 2.
Regression Results Examining Relationship Between County Sociodemographic Characteristics and Access to Mental Health Outpatient Treatment Facilities that Accept Medicaid
| Characteristic | No Access (Predicted Pct=29.1%) | High Access (Predicted Pct=17.4%) |
|---|---|---|
|
| ||
| Marginal Effect (95% CI), % | Marginal Effect (95% CI), % | |
| Black | 3.9** (1.2, 6.6) | −2.7** (−4.6, −0.8) |
| Hispanic | 4.8*** (2.3, 7.4) | −3.4*** (−5.1, −1.6) |
| Living in Poverty | −2.1 (−4.3, 0.1) | 1.5 (−0.1, 3.0) |
| Living in Rural Community | 27.9*** (25.3, 30.4) | 3.4*** (1.6, 5.3) |
Note: N=3,141 Counties;
p<0.05,
p<0.01,
p<0.001
Generalized ordered logistic regression model estimated with state fixed effects. Marginal effect indicates the predicted change in the percentage of counties classified as having no access or high access to mental health outpatient treatment facilities that accept Medicaid associated with a 1 S.D. increase in the explanatory variable, holding the covariates at their mean value.
Results are slightly mixed when examining whether rural counties have less access to outpatient MH facilities that accept Medicaid (Table 2). Consistent with our hypothesis, counties with a higher percentage of rural residents are more likely to lack these facilities than counties with a lower percentage of rural residents (ME=27.9%, 95% CI=25.3%, 30.4%). However, counties with a higher percentage of rural residents are also more likely to be classified as having high access to these facilities than counties with a lower percentage of rural residents (ME=3.4%, 95% CI=1.6%, 5.3%).
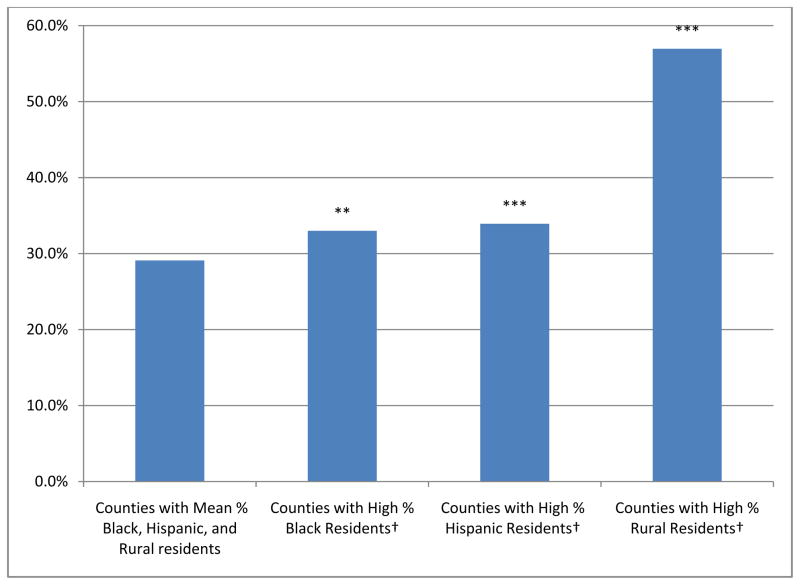
Using the model-based predicted values, results depicting which counties are most likely to lack outpatient MH facilities that accept Medicaid are presented in Figure 1. When all covariates are held constant at their mean value, the model-based predicted probability indicates that 29.1% of counties do not have any access to these facilities. Among counties with a high percentage of Black or Hispanic residents (i.e., a one standard deviation increase above the mean value of each respective measure), the predicted percentage of counties without access to these facilities increases to 33.0% and 33.9%, respectively. The effect size for percentage of residents living in rural areas is especially pronounced; among counties with a high percentage of residents living in rural areas (i.e., one standard deviation increase above the mean value), 57.0% of counties lack access to these facilities.
Figure 1.
Predicted Percentage of Counties with No Access to Outpatient Mental Health Facilities that Accept Medicaid
Note: **p<0.01, ***p<0.001; Predicted values estimated from generalized ordered regression model with state fixed effects controlling for county poverty (N=3,141 Counties).
†Predicted values associated with a one standard deviation increase in each measure above the mean, holding other covariates at their mean value.
We conducted additional sensitivity analyses with alternative thresholds to classify “high access” as outpatient MH facilities that accept Medicaid using the top decile and quartile of facility to Medicaid enrollee per capita ratio. The results were consistent across these thresholds for percentage Black residents and percentage living in rural areas. The negative relationship between percentage Hispanic residents and high access to these facilities, however, was not significant when using these other thresholds and should therefore be interpreted with caution. We also conducted sensitivity analyses in which we limited the analytic sample to counties in urban and suburban areas (i.e., N=1,787) using the Office of Management and Budget definition of core-based statistical areas.22 Regression results using this analytic sample were similar to those presented for the full model with one exception; urban/surburban counties with a higher percentage of residents living in poverty were significantly less likely to lack these facilities than urban/suburban counties with a lower percentage of residents living in poverty (p<0.01).
DISCUSSION
Results highlight extensive gaps in the community-based MH treatment infrastructure for Medicaid enrollees across many U.S. counties. Over one-third of counties did not have any outpatient MH facilities that accept Medicaid. Furthermore, counties with a higher percentage of Black residents, Hispanic residents, and residents living in rural communities are significantly more likely to lack geographic access to these facilities.
Among states that opt into the Medicaid expansion, our results suggest that communities with a high percentage of racial/ethnic minorities may face particular constraints on their Medicaid MH safety-net system. Not only does Medicaid currently play an especially important role in providing insurance coverage for Black and Hispanic individuals, but this role will continue to grow as the PPACA is implemented. In 2009, 27% of Black and Hispanic individuals were covered by Medicaid, compared to only 11% of White individuals.23, 24 Furthermore, when considering racial differences in the population of nonelderly persons living in poverty who would be eligible for the Medicaid expansion (i.e., <133% of the Federal Poverty Level), 41% of Black and Hispanic individuals are living in poverty relative to only 17% of White individuals. Therefore, Black and Hispanic individuals may see the largest increase in Medicaid enrollment under the PPACA.25 If communities with a high concentration of Black and/or Hispanic residents experience higher than average Medicaid enrollment but are more likely to lack these facilities, policies will need to be implemented to ensure that the Medicaid expansion does not exacerbate disparities in the accessibility of services for these communities.
Because models adjusted for county poverty, the findings associated with county racial/ethnic composition appear to be independent of differences in county socioeconomic status. To ensure that these findings were not an artifact of multicollinearity, we also assessed unadjusted correlations, alternative model specifications, and variance inflation factors. These additional analyses indicated that multicollinearity was not a concern for this analysis.
When examining which counties have no access to these facilities, the effect size was by far the largest for communities with a high percentage of residents living in a rural community. A one standard deviation increase in the percentage of rural residents nearly doubled the likelihood that a county did not have an outpatient MH facility that accepts Medicaid. Although there was also a positive association between rurality and high access to the Medicaid MH safety-net, the effect size for this relationship is substantially smaller than the effect size for the relationship between rurality and having no access to these facilities. Furthermore, because “high access” counties were classified by dividing the number of facilities by the number of Medicaid enrollees in the county, rural counties with a single facility would have been more likely to be classified as offering high access to these facilities due to a lower population density. Considered together, our findings suggest that a handful of rural counties provide access to community-based MH specialty facilities that accept Medicaid, while most rural counties do not have access to this system.
To assess how these gaps in the county-level infrastructure translate into lack of access for Medicaid enrollees at the individual level, we calculated the percentage of Medicaid enrollees who live in a county without a facility. Overall, 8.2% of Medicaid enrollees live in a county without an outpatient MH facility that accepts Medicaid. Consistent with our findings, we also found that Medicaid enrollees living in rural communities are disproportionately affected by these infrastructure gaps. More than one-third (34.6%) of Medicaid enrollees who reside in rural areas live in a county that lacks one of these facilities compared to 6.1% of Medicaid enrollees who live in urban/suburban areas.
Local and state policy makers should evaluate the capacity of the MH treatment infrastructure in each community to meet the impending increased demand for MH services by Medicaid enrollees, with special attention to communities with a high concentration of Black, Hispanic, and rural residents. Policies addressing these gaps will need to ensure that Medicaid coverage expansions translate into improved access to needed MH services. At present, 86.1% of responding MH facilities that provide outpatient MH treatment already accept Medicaid, and this participation rate varies little across states. Furthermore, there is little difference between the percentage of counties that have access to an outpatient MH facility (66.3%) and the percentage of counties that have access to an outpatient MH facility that accepts Medicaid (i.e., 65.2%). Thus, efforts aimed at improving access to MH treatment by increasing the participation of these facilities in the Medicaid program will likely be insufficient to meet the increased demand for services. At least three additional approaches could be considered to increase rates of access to MH services among Medicaid enrollees: (1) building new specialty MH facilities that serve Medicaid enrollees; (2) revising Medicaid policies to encourage more MH providers in solo or group practices to accept Medicaid; and (3) providing more resources to primary care safety net facilities to expand their capabilities to provide MH specialty services.
In the current fiscal climate, the first two policy options would be especially challenging to implement. Because many of the existing MH facilities were constructed several decades ago with federal funds from the Community Mental Health Centers Construction Act of 1963,26 it is unlikely that states would be able to construct and staff new facilities at a time when many local communities and states are facing budget shortfalls. Similarly, given concerns about the impact of the impending Medicaid expansion on their budgets,27 states are unlikely to be able to increase MH provider reimbursement rates to a sufficient level to greatly improve participation in the program.
A more practical strategy to improve access to community-based MH services for Medicaid enrollees in vulnerable communities would be to allocate more funds for primary care safety net facilities to improve their capacity to provide specialty MH services. Additional descriptive analyses (not shown) indicate that approximately three-fourths of counties classified as having “no access” to outpatient Medicaid MH treatment facilities have at least one federally-funded community health center (CHC) (i.e, a federally qualified health center or a rural health clinic). Community health centers have been increasingly providing onsite MH services, and approximately three-fourths of CHC grantees offered some type of mental health services as of 2007.28, 29 In spite of this trend towards greater provision of MH services in CHCs, there is cause for concern that they may not currently have the resources or capacity to fully address infrastructure gaps in the Medicaid MH safety-net system. Only a small percentage of CHC patients receive any MH services (i.e., 4% of CHC patients received MH services in 2010),30 and CHCs typically care for individuals with less serious mental disorders than MH specialty clinics.29, 31
The PPACA allocates $11 billion in new funding over a period of five years to bolster and expand the capacity of existing CHCs to provide oral health, pharmacy, and behavioral health services to CHC clients and to construct new CHCs in medically underserved areas.32 This funding provides an important opportunity to expand the capacity of these facilities to treat those with MH disorders, which would be especially important in local communities that face gaps in the specialty MH safety-net system. Thus, local, state, and federal policy makers should work to ensure that this provision of the PPACA is used both to increase both the overall volume of mental health treatment, and CHC’s capacity to treat more serious and complex mental conditions.
Several study limitations are noted. First, causality cannot be established in these relationships because the data are cross-sectional. The survey response rate, 74.2%, poses another limitation. However, the regressions presented above control for whether a county had a facility with incomplete survey information due to non-response or missing information on key analytic variables. Third, we were not able to incorporate facility capacity in our regression models because a high percentage of facilities are missing data on the related survey measure (i.e., 35.9% of facilities in our analytic sample). Lastly, it would have been preferable if the data measuring Medicaid enrollees per county were available for the same year in which the dependent variable was assessed (2008). Yet, the most recent year of county-level Medicaid enrollment data available in the Area Resource File is 2007. We were able, however, to assess the correlation between county-level Medicaid enrollment data across years between 2006 and 2007; as expected, the correlation is very high (R=0.95, p<0.001).
Notwithstanding limitations, this is the first study, to our knowledge, to document the accessibility of outpatient MH treatment facilities that serve Medicaid clients across communities and to highlight which communities face the greatest risk for reduced access to these crucial resources. Although the expansion of Medicaid will provide an opportunity to increase insurance coverage for vulnerable populations in need of MH services, many communities may face constraints on the Medicaid MH safety-net system to meet the increased demand for services – especially rural communities and communities of color. Policy makers need to recognize the continued importance of enhancing behavioral health services in primary care safety-net facilities to help meet the increased demand for MH services among states that opt into Medicaid, especially in communities that lack an adequate MH safety-net system.
Acknowledgments
The authors are grateful for the helpful comments and suggestions by Jason Hockenberry and Neetu Chawla. This work was supported by the National Institute of Mental Health (5K24MH07586705, 1K01MH09582301).
Footnotes
Previous Presentation: None
Disclosures: The authors have no conflicts of interest to disclose.
References
- 1.Mark TL, Coffey RM, Vandivort-Warren R, Harwood HJ, King EC. U.S. spending for mental health and substance abuse treatment, 1991–2001. Health Aff (Millwood) 2005 Jan-Jun;(Suppl Web Exclusives):W5-133–W135-142. doi: 10.1377/hlthaff.w5.133. [DOI] [PubMed] [Google Scholar]
- 2.Buck J, Miller K, Bae J. Mental Health and Substance Use Services in Medicaid, 1994. Rockville, MD: Center for Mental Health Service; 2000. [Google Scholar]
- 3.Garfield RL, Zuvekas SH, Lave JR, Donohue JM. The impact of national health care reform on adults with severe mental disorders. Am J Psychiatry. 2011 May;168(5):486–494. doi: 10.1176/appi.ajp.2010.10060792. [DOI] [PubMed] [Google Scholar]
- 4.Kaiser Family Foundation. Medicaid and Children’s Health Insurance Program Revisions in the New Health Reform Law. Menlo Park, CA: Kaiser Family Foundation; 2010. [Google Scholar]
- 5.Kaiser Family Foundation. A Guide to the Supreme Court’s Affordable Care Act Decision. Menlo Park, CA: Kaiser Family Foundation; 2012. [Google Scholar]
- 6.Jost TS, Rosenbaum S. The Supreme Court and the Future of Medicaid. The New England journal of medicine. 2012;367(11):983–985. doi: 10.1056/NEJMp1208219. [DOI] [PubMed] [Google Scholar]
- 7.Bureau of Health Professions, Health Resources and Services Adminstration. . Area Resource File. Rockville, MD: US Department of Health and Human Services; 2008. [Google Scholar]
- 8.Cunningham P, McKenzie K, Taylor EF. The struggle to provide community-based care to low-income people with serious mental illnesses. Health Aff (Millwood) 2006 May-Jun;25(3):694–705. doi: 10.1377/hlthaff.25.3.694. [DOI] [PubMed] [Google Scholar]
- 9.Wilk JE, West JC, Narrow WE, Rae DS, Regier DA. Access to psychiatrists in the public sector and in managed health plans. Psychiatr Serv. 2005 Apr;56(4):408–410. doi: 10.1176/appi.ps.56.4.408. [DOI] [PubMed] [Google Scholar]
- 10.Zarin DA, Pincus HA, Peterson BD, et al. Characterizing psychiatry with findings from the 1996 National Survey of Psychiatric Practice. Am J Psychiatry. 1998 Mar;155(3):397–404. doi: 10.1176/ajp.155.3.397. [DOI] [PubMed] [Google Scholar]
- 11.Jacobs S, Wilk J, Chen D, Rae D, Steiner J. Datapoints: medicaid as a payer for services provided by psychiatrists. Psychiatr Serv. 2005 Nov;56(11):1356. doi: 10.1176/appi.ps.56.11.1356. [DOI] [PubMed] [Google Scholar]
- 12.Schatzkin A. The relationship of inpatient racial composition and hospital closure in New York City. Med Care. 1984 May;22(5):379–387. doi: 10.1097/00005650-198405000-00002. [DOI] [PubMed] [Google Scholar]
- 13.Shen YC, Hsia R, Kuzma K. Understanding the risk factors of trauma center closures: Do financial pressure and community characteristics matter? Medical Care. 2009 Sep;47(9):968–978. doi: 10.1097/MLR.0b013e31819c9415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Komaromy M, Grumbach K, Drake M, et al. The role of black and Hispanic physicians in providing health care for underserved populations. The New England journal of medicine. 1996 May 16;334(20):1305–1310. doi: 10.1056/NEJM199605163342006. [DOI] [PubMed] [Google Scholar]
- 15.Hsia RY-J, Shen Y-C. Rising Closures Of Hospital Trauma Centers Disproportionately Burden Vulnerable Populations. Health Affairs. 2011 Oct 1;30(10):1912–1920. doi: 10.1377/hlthaff.2011.0510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Office of Rural Health Policy, Health Resources and Services Administration. . Office of Rural Health Policy Rural Guide to Federal Health Professions Funding. Rockville, MD: Department of Health and Human Services; Jan, 2011. [Google Scholar]
- 17.U.S. Census Bureau. [Accessed January 16, 2011];Census 2000 Geographic Terms and Concepts. 2000 http://www.census.gov/geo/reference/pdfs/glossry2.pdf.
- 18.Williams R. Generalized ordered logit/partial proportional odds models for ordinal dependent variables. The Stata Journal. 2006;6(1):58–82. [Google Scholar]
- 19.Miller EA. State health policy making determinants, theory, and methods: a synthesis. Soc Sci Med. 2005 Dec;61(12):2639–2657. doi: 10.1016/j.socscimed.2005.05.006. [DOI] [PubMed] [Google Scholar]
- 20.Grogan CM. Political-Economic Factors Influencing State Medicaid Policy. Polit Res Quart. 1994 Sep;47(3):589–622. [Google Scholar]
- 21.Williams RL. A note on robust variance estimation for cluster-correlated data. Biometrics. 2000 Jun;56(2):645–646. doi: 10.1111/j.0006-341x.2000.00645.x. [DOI] [PubMed] [Google Scholar]
- 22.Office of Management and Budget. [Accessed September 21, 2010];Statistical Programs and Standards. http://www.whitehouse.gov/omb/inforeg_statpolicy.
- 23.Kaiser Commission on Medicaid Facts. Medicaid’s Role for Black Americans. Washington, D.C: Kaiser Family Foundation; 2011. [Google Scholar]
- 24.Kaiser Commission on Medicaid Facts. Medicaid’s Role for Hispanic Americans. Washington, D.C: Kaiser Family Foundation; 2011. [Google Scholar]
- 25.Kaiser Family Foundation. Health Reform and Communities of Color: Implications for Racial and Ethnic Health Disparities. Menlo Park, CA: Kaiser Family Foundation; Sep, 2010. [Google Scholar]
- 26.Urff J. Public Mental Health Systems: Structures, Goals, and Constraints. In: Lubotsky Levin B, Petrila J, Hennessy KD, editors. Mental Health Services: A Public Health Perspective. 2. Oxford: Oxford University Press; 2004. pp. 72–87. [Google Scholar]
- 27.Ku L. Ready, set, plan, implement: executing the expansion of Medicaid. Health Aff (Millwood) 2010 Jun;29(6):1173–1177. doi: 10.1377/hlthaff.2010.0417. [DOI] [PubMed] [Google Scholar]
- 28.Druss BG, Bornemann T, Fry-Johnson YW, McCombs HG, Politzer RM, Rust G. Trends in Mental Health and Substance Abuse Services at the Nation’s Community Health Centers: 1998–2003. American journal of public health. 2006 Oct;96(10):1779–1784. doi: 10.2105/AJPH.2005.076943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wells R, Morrissey JP, Lee IH, Radford A. Trends in behavioral health care service provision by community health centers, 1998–2007. Psychiatr Serv. 2010 Aug;61(8):759–764. doi: 10.1176/appi.ps.61.8.759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Health Resources and Services Administration. Primary Care: The Health Center Program. 2010 National Data. Rockville, MD: U.S. Department of Health and Human Services; 2011. [Google Scholar]
- 31.Health Resources and Services Administration. Primary Care: The Health Center Program: Table 6A - Selected Diagnoses and Services Rendered: 2011 National Data. Rockville, MD: US Department of Health and Human Services; 2011. [Google Scholar]
- 32.National Association of Community Health Centers. [Accessed March 23, 2010];Health Reform Hub. http://www.nachc.com/healthreform.cfm.