Abstract
Background
Decline in oxygen uptake efficiency (OUE), especially during exercise, is found in patients with chronic heart failure. In this study we aimed to test the validity and usefulness of OUE in evaluating gas exchange abnormality of patients with idiopathic pulmonary arterial hypertension (IPAH).
Methods
We retrospectively investigated the cardiopulmonary exercise test (CPET) with gas exchange measurements in 32 patients with confirmed IPAH. All patients also had resting hemodynamic measurements and pulmonary function test (PFT). Sixteen healthy subjects, matched by age, sex, and body size were used as controls, also had CPET and PFT measurements.
Results
In IPAH patients, the magnitude of absolute and percentage of predicted (%pred) oxygen uptake efficiency slope (OUES) and oxygen uptake efficiency plateau (OUEP), as well as several other CPET parameters, were strikingly worse than healthy subjects (P<0.0001). Pattern of changes in OUE in patients is similar to that in controls, In IPAH patients, OUE values at rest, warming up, anaerobic threshold and peak exercise were all significantly lower than in normal (P<0.0001). OUEP%pred, better than OUES%pred, correlated significantly with New York Heart Association (NYHA) functional Class (r = −0.724, P<0.005), Total Pulmonary Vascular Resistance (TPVR) (r = −0.694, P<0.005), diffusing capacity for carbon monoxide (DLCO) (r = 0.577, P<0.05), and the lowest ventilation versus CO2 output ratio during exercise (LowestV˙E/V˙CO2) (r = −0.902, P<0.0001). In addition, the coefficient of variation (COV) of OUEP was lower (20.9%) markedly than OUES (34.3%) (P<0.0001).
Conclusions
In patients with IPAH, OUES and OUEP are both significantly lower than the healthy subjects. OUEP is a better physiological parameter than OUES in evaluating the gas exchange abnormality of patients with IPAH.
Introduction
Idiopathic pulmonary arterial hypertension (IPAH) is a progressive and fatal disease caused by pulmonary vasculopathy [1]–[2]. Low perfusion to the lungs due to inability of the right ventricle to adequately increase pulmonary blood flow (cardiac output [CO]) for O2 exercise demand, gives rise to mismatching of ventilation/perfusion (V/Q) and inefficient lung gas exchange. Cardiopulmonary exercise test (CPET) with gas exchange measurements has proved to be a powerful tool to detect abnormalities in patients with IPAH during exercise [3]. Patients with IPAH can safely undergo noninvasive cycle ergometer testing to their maximal tolerance [4]. The key CPET characteristics in these patients include a diminished aerobic capacity, an impaired ventilatory efficiency and a decreased minute O2 uptake versus heart rate at peak exercise (peak V˙O2/HR) etc [4]–[8]. These CPET parameters have been widely utilized to grade the severity of exercise limitation, to detect exercise-induced right-to-left shunting, to assess responses to therapy, and to predict prognosis in IPAH patients [5]–[8]. Because of the increasing recognition of potential value of CPET in patients with IPAH, more CPET indexes are required in clinical practice.
Oxygen uptake efficiency (OUE) is a recently emerging parameter which is not obvious in the traditional Wasserman CPET 9-panel plots [9]. OUE measures the change in minute oxygen uptake (V˙O2) relative to minute ventilation (V˙E). The most widely studied index of OUE is the oxygen uptake efficiency slope (OUES), which ordinarily mathematically describes a near-linear relationship for V˙O2 versus V˙E after transforming V˙E from a linear to log scale. Thus OUES defines the slope of V˙O2-vs-logV˙E during an entire exercise period [10]. It was used initially in young patients (mean age 12 yrs) with cardiac disease and then later in adults with heart disease to assess exercise capacity, severity and prognosis [11]–[13]. Recently, the other index of OUE, oxygen uptake efficiency plateau (OUEP) was added. It is well known that the relationship between V˙O2 and V˙E during an incremental exercise test is curvilinear due to hyperventilation stimulated by the excess [H+] of the acidosis of heavy exercise [14]. We found that V˙O2/V˙E when plotted against time normally reached its highest and briefly stable values (plateau) near the anaerobic threshold (AT), before declining due to hyperventilation stimulated by the metabolic acidosis [14]. We defined the highest 90 sec average of V˙O2/V˙E as OUEP. In our CHF patients and normal subjects, we found that the OUEP had less variability and higher predictability and test-retest reproducibility than the OUES. It follows that OUEP may have the potential to better assess severity of dysfunction and to better prognosticate mortality and morbidity in patients with either chronic left or right heart failure [15].However, previously we did not investigate this issue in our patients with pulmonary hypertension .
OUE representing the change in V˙2 as related to V˙E, could be affected by cardiac output (CO), difference between systemic and pulmonary arterial blood O2 contents, lung gas exchange, and changes in pH. OUES is the most widely studied index of OUE, but OUEP, which has not been previously studied in IPAH patients, may have advantages. We had already shown V˙O2/V˙E is lower and can decline in the transition from rest to exercise in patients with left heart failure [15]–[16]. We hypothesized that OUEP in IPAH patients could be lower than the normals and decline in the transition from rest to exercise due to inability to adequately increase cardiac output during exercise.
Methods
Patients and control subjects
We retrospectively investigated the exercise pathophysiology in 32 patients with IPAH referred for evaluation and treatment in Shanghai Pulmonary Hospital between 2009 and 2012. For comparison purposes, the CPET and pulmonary function test (PFT) data of 16 healthy subjects of similar age, sex, and body size were also analyzed (6 men and 10 women; mean age 37.88±16.76 yrs). All CPET study participants signed written informed consent. This study was approved by the Institution of Human Subjects Committee at Shanghai Pulmonary Hospital. The diagnosis of IPAH was based on clinical and laboratory data, including right heart catheterization (RHC), according to currently accepted diagnostic criteria (Dana Point, 2008) [17]. Patients with disorders other than IPAH were excluded according to the recommended diagnostic guidelines for IPAH [17]. The patients were non-smokers at the time of study and most had never smoked. The data included only the first PFT and CPET measurements made after referral to our hospital, nearly always prior to the initiation of pulmonary vasodilator therapy.
PFT Measurements
Each patient and normal subject underwent resting measurements of forced vital capacity (FVC), forced expiratory volume in 1 sec (FEV1), maximum voluntary ventilation (MVV), diffusing capacity for carbon monoxide (DLCO) and total lung capacity (TLC) using standard methodology[18]–[19] and equipments (Masterscreen-PFT, Jaeger, Hoechberg, Germany; Masterscreen-plethysmography, Jaeger, Hoechberg, Germany). All PFT values were reported in absolute terms and normalized to percentage of predicted (%pred). Predicted spirometry values, TLC and DLCO were calculated using accepted equations for Chinese adults [20].
CPET Procedure and Data Collection
Each patient performed PFT and CPET, after familiarization with the exercise apparatus, on the same day. Before each test, the equipment was calibrated according to manufacturer's specifications using reference and calibration gases. Standard 12 lead electrocardiograms (ECGs) and pulse oximetry were continuously monitored. Blood pressure at the brachial artery was measured every two minutes with an automatic cuff. The exercise protocol consisted of 3 min of rest, 3 min of unloaded cycling at 60 rpm, followed by uniform increase in resistance of 5 to 15 W/min for the patients and 20 to 25 W/min for the normal subjects to maximal tolerance on an electromagnetically braked cycle ergometer (Ergoselect 100, ergoline GmbH, Bitz, Germany) [9]. The rate of increasing work depended on the estimated exercise capacity of the subjects. Subjects were encouraged to exercise to the limits of their functional capacities or until the physician stopped the test because of severe adverse events, such as chest pain, light-headedness, potentially life-threatening arrhythmias, ST-segment changes, or marked systolic hypotension. Most CPET values were reported in absolute terms and normalized to percentage of predicted (%pred). Predicted values were calculated using accepted equations [9].
CPET data Calculations
Carbon dioxide output (V˙CO2, ml/min, STPD), V˙O2 (ml/min, STPD), V˙E (l/min, BTPS), tidal volume (l, BTPS), were measured continuously on a breath-by-breath basis using a CPX Metabolic Measurement Cart (Masterscreen-CPX, Jaeger, Hoechberg, Germany) that was equipped with rapidly-responding O2 and CO2 analyzers. Data were averaged every 10 sec. Peak V˙O2 was defined as the highest 30 sec average of V˙O2, and other peak parameters were calculated at the same time. Each AT was determined by the V-slope method [21]. V˙E-V˙CO2 slope was determined by linear regression analysis of the relation between V˙E and V˙CO2 during exercise, excluding data above the ventilatory compensation point [22]. Lowest V˙E/V˙CO2 was determined by averaging the lowest consecutive 90 sec data points [22].
In addition, to show patterns of gas exchange change in patients as related to time and exercise intensity during CPET, V˙O2/V˙E, V˙E/V˙CO2 and PETCO2 values at 4 periods were respectively averaged: the last minute of rest, last minute of unloaded cycling, 1 min before the AT was reached (only for V˙O2/V˙E), 1 min after the AT was reached (only for V˙E/V˙CO2 and PETCO2) and for 30 sec at peak exercise.
OUE definitions and measurements
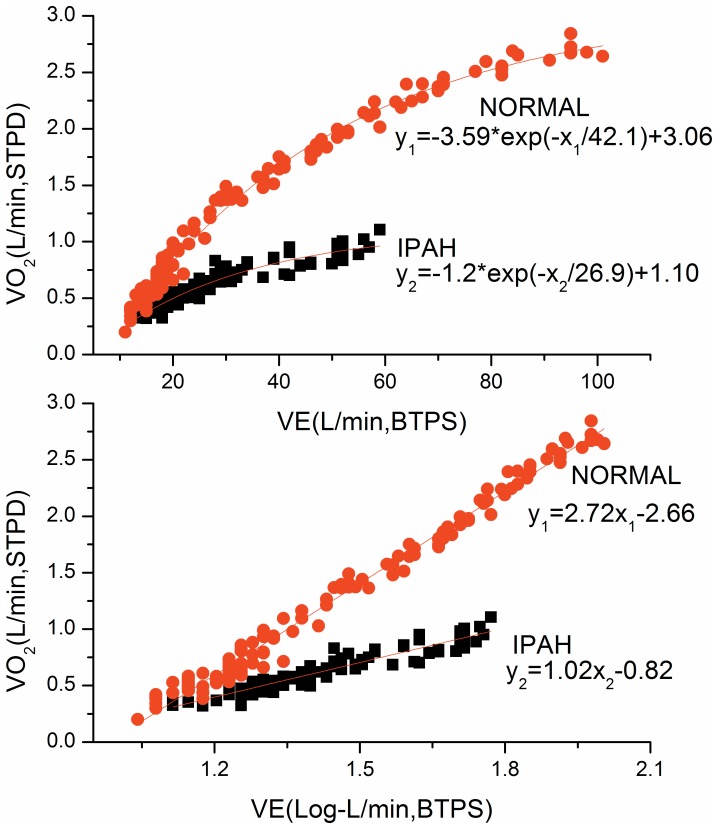
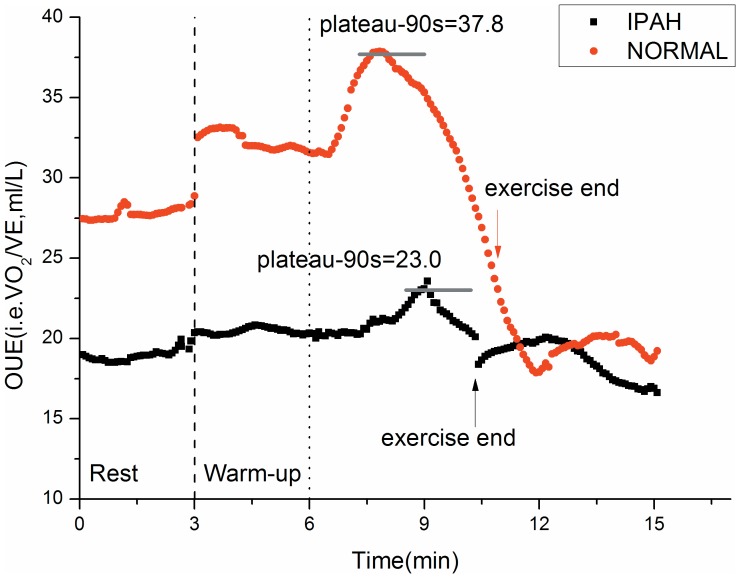
The OUES was defined as the regression slope “a” in V˙O2 = a×log10V˙E+b. A steeper slope or higher OUES represents a more efficient oxygen uptake per volume of ventilation (Figure 1). The OUEP was defined as the 90 sec average of the highest consecutive measurements of V˙O2/V˙E near the AT (Figure 2) [14].
Figure 1. Difference of OUES between a typical IPAH patient and a control subject.
Linear (upper panel) and single-segment logarithmic (lower panel) relation between V˙O2 (ml/min) and V˙E (ml/min) for 2 different subjects. Steeper slopes represents more efficient oxygen uptake. The control subject (steeper slopes, aged 24 years; height, 158 cm; weight, 45 kg), has an oxygen uptake efficiency slope (OUES) of 2.72 whereas the IPAH patient (shallower slopes, aged 21 years; height, 161 cm; weight, 47 kg) has an OUES of 1.02.
Figure 2. Difference of OUEP and OUE between a typical IPAH patient and a control subject.
The kinetics of changes in oxygen uptake efficiency (OUE) for the same tests and subjects as depicted in Figure 1. OUE typically increase during exercise from rest to plateau in normal subjects and then decrease gradually until exercise end. It then decreases further in the immediate recovery period and begin stabilizing after about 2 minutes. In IPAH patients, OUE changes in a similar way as the controls, but is always lower than the controls in the transition from rest to exercise end.
Statistical analysis
Microsoft Office-2000, SPSS-10.0 and Origin-7.0 computer software were used. Data are expressed as mean ±SD, except where specifically noted. Most PFT and CPET values are expressed in absolute terms and %pred. P<0.05 was considered significant. Unpaired Student t-test was used for comparison between IPAH patients and normal subjects, whereas X2 test was performed for gender analysis. The differences in OUE, V˙E/V˙CO2 and PETCO2 at each time period were respectively assessed by repeated-measures analysis of variance (ANOVA). Correlations between OUE and other variables were determined by Pearson's correlation test, except for NYHA functional classification by Spearman rank correlation test.
Results
Baseline clinical and demographic characteristics
Characteristics of patients and healthy subjects are detailed in Table 1. The female-to-male ratio of the IPAH patients and healthy subjects in this study were about 2∶1. The PFT and CPET parameters of the healthy group were within normal limits. The DLCO values were significantly lower in the IPAH patients compared with the normals. The FEV1/FVC in the IPAH group was significantly lower than the control group, but still within normal limit. Other PFT values were normal. 69% of IPAH patients were NYHA functional class 2 while 75% had cardiac index below 2.5.
Table 1. Demographics, hemodynamics, Pulmonary Function Testing and Cardiopulmonary Exercise Testing parameters in IPAH patients and Control subjects.
| IPAH patients (n = 32) | Control subjects (n = 16) | |
| Age, yrs | 40.3±14.8 | 37.9±16.8 |
| Gender, F/M | 20/12 | 10/6 |
| Height, cm | 162±7.8 | 160±9.0 |
| Weight, kg | 60.3±13.7 | 53.2±9.9 |
| Body mass index, kg/m2 | 22.8±3.9 | 20.7±2.2 |
| NYHA functional class | 2.3±0.48 | NA |
| mPAP, mm Hg | 59.0±14.2 | NA |
| mRAP, mm Hg | 11.2±4.8 | NA |
| mPWP, mmHg | 8.6±4.4 | NA |
| TPVR, mm Hg/L/min | 13.1±5.7 | NA |
| Cardiac index, L/min/m2 | 2.48±0.85 | NA |
| FVC, L (%pred) | 3.30±0.85 (95±20) | 3.45±0.84 (100±14) |
| FEV1, L (%pred) | 2.56±0.61(87±17) | 2.93±0.62(101±15) |
| FEV1/FVC (%pred) | 78.1±6.7(96±5) * | 85.6±5.9(101±6) |
| MVV, L/min (%pred) | 86±25 (98±19) | 98±30 (116±18) |
| DLCO, ml/mm Hg/min (%pred) | 17.1±6.5 (79±23) ‡ | 23.9±5.2(117±15) |
| TLC, L (%pred) | 5.14±0.92 (99±11) | 5.13±1.17 (100±12) |
| Peak V˙O2, ml/min (%pred) | 920±298(49±14) ‡ | 1617±547 (95±15) |
| Peak work rate, W (%pred) | 72±26(54±16) ‡ | 137±52(102±26) |
| AT, ml/min (%pred) | 615±165(76±14) ‡ | 937±255(111±10) |
| Peak heart rate, beats/min (%pred) | 146±17(80±7) † | 166±12(90±7) |
| Peak O2 pulse, ml/beat (%pred) | 6.2±1.7(63±17) ‡ | 9.6±2.8(97±7) |
| Peak V˙E, L/min (%MVV) | 49±13(59±16) | 61±23(62±7) |
| Peak PETCO2, mm Hg | 23.2±8.0‡ | 40.9±2.9 |
| V˙E-V˙CO2 slope | 51.7±28.1* | 27.9±5.9 |
| Lowest V˙E/V˙CO2, (%pred) | 49.4±14.9(183±49) ‡ | 27.7±2.2(106±9) |
| OUES, L/min/log(L/min) (%pred) | 1.08±0.37(58±19) ‡ | 1.98±0.44(98±13) |
| OUEP, ml/L (%pred) | 23.4±4.9(60±12) ‡ | 37.8±4.8(98±12) |
Values are expressed as mean ± SD and percentage of measured to predicted values (%pred).
*p<0.05, †p<0.005, ‡p<0.0001, vs. controls using unpaired t test. NA = not applicable.
NYHA = New York Heart Association functional classification; mPAP = mean pulmonary artery pressure; mRAP = mean right atrial pressure; mPWP = mean pulmonary artery wedge pressure; TPVR = total pulmonary vascular resistance; FVC = forced vital capacity; FEV1 = forced expiratory volume in 1 second; MVV = maximum voluntary ventilation; DLCO = gas transfer index or diffusing capacity for carbon monoxide; TLC = total lung capacity; AT = anaerobic threshold; %MVV = percentage of maximum voluntary ventilation; PETCO2 = partial pressure of end-tidal carbon dioxide; OUES = oxygen uptake efficiency slope; OUEP = oxygen uptake efficiency plateau; IPAH = idiopathic pulmonary arterial hypertension; %pred = percent of predicted; V˙O2 = peak oxygen uptake, STPD = standard temperature pressure dry; V˙E = minute ventilation, BTPS = body temperature pressure saturated; V˙CO2 = carbon dioxide output, STPD.
All individuals completed their CPET studies without accident or untoward effects. Nearly all patients stopped exercise because of fatigue and/or acute shortness of breath; uncommonly, patients noted palpitations or light-headedness and recovered after resting for several minutes. All subjects declared they had done their best. In IPAH group, except for peak heart rate and peak ventilation, the magnitude of the absolute and percentage of all CPET parameters of oxygen uptake and ventilatory efficiency were strikingly abnormal.
Decrease of OUES in IPAH
As shown in Figure 1, the typical case of IPAH had a lower OUES than the matched normal subject. The OUES of IPAH group was 1.08±0.37 which was significantly lower than 1.98±0.44 of control (p<0.0001).
Changes and contributions in OUE and V˙E/V˙CO2 during CPET
As shown in Figure 2, the OUE response of IPAH patient to exercise was clearly different from that of the matched normal subject. At all times, the OUE values of IPAH patient were lower than those of control.
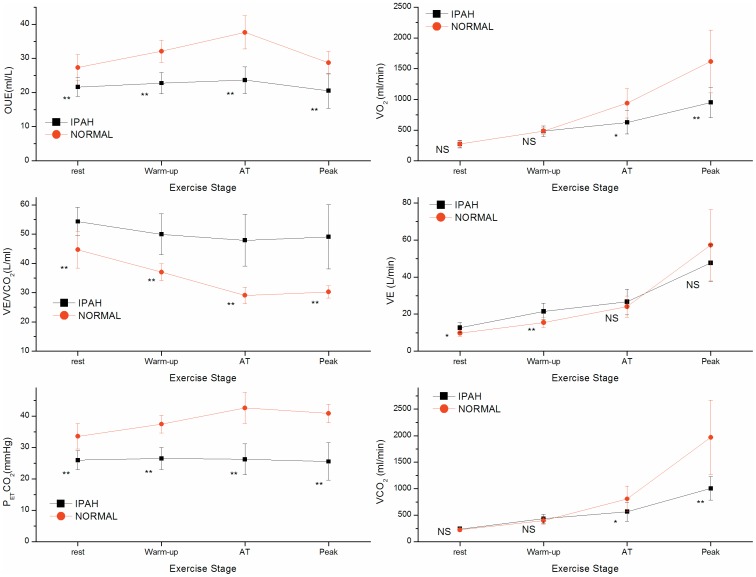
The left top portion of Figure 3 shows OUE values for patients and normal subjects at four time periods. OUE values at all time periods were markedly lower in IPAH patients than in normal subjects (P<0.001). In control group, the differences in OUE values at four time periods were significant (P<0.001), and changes between adjacent periods were evident (P<0.001). However in IPAH group, the differences in OUE values at four time periods were also significant (P = 0.023), but the magnitude of OUE changes was much smaller than the control group.
Figure 3. Difference of CPET parameters between IPAH and control groups at different stages of exercise.
The group mean±SD Values of IPAH) and control (NORMAL) groups are shown at stages of rest, unloaded cycling, AT, and peak exercise during incremental cycle ergometry tests. Values are. On the left side from top to bottom, they are OUE, V˙E/V˙CO2 and PETCO2.; on the right side from top to bottom they are V˙O2, V˙CO2 and V˙E. Statistically significant differences between groups at the same stage are shown as NS for no significance, * for P<0.05, ** for P<0.005, below value symbol.
Figure 3 left center, shows V˙E/V˙CO2 values at similar times. IPAH patients had significantly greater V˙E/V˙CO2 than normal subjects at all activity levels (P<0.001). From rest to the AT, V˙E/V˙CO2 values in control group reduced greatly, however in IPAH group decreased hardly. Compared with V˙E/V˙CO2 values at AT, there was no obvious reduction at peak either for controls or patients.
Figure 3 left bottom, shows the significantly reduced PETCO2 values at all levels of activity in the IPAH group compared with the control group (P<0.001). In the control group, PETCO2 values distinctively increased with increasing level of activity until AT, thereafter decreased mildly at peak. On the contrary, PETCO2 values in IPAH patients did not increase at all from resting values.
Figure 3 right side, shows the similarities of both IPAH and Control groups for V˙O2 and V˙CO2 at rest and warm-up (P>0.05). There were significant differences at AT (P<0.05) and peak exercise (P<0.001). However, for V˙E, IPAH patients had higher values than those of Control subjects at rest (P<0.05) and warm-up (P<0.001), but no difference at AT and peak exercise (P>0.05). This indicates that at any required metabolic rate (as V˙O2 and V˙CO2), the ventilation is over driven by lung compensation for a limited heart function, i.e. mismatched Q/VA. The low and unchanged PETCO2 is the evidence of hyperventilation in patients with IPAH.
OUE as related to key abnormal parameters for IPAH patients
The correlations between OUE and other key parameters for IPAH patients are shown in Table 2. OUEP %pred correlated significantly with NYHA functional Class (r = −0.724, P<0.005), Total Pulmonary Vascular Resistance (TPVR) (r = −0.694, P<0.005), DLco %pred (r = 0.577, P<0.05), peak PETCO2 (r = 0.68, P<0.005), and lowest V˙E/V˙CO2 (r = −0.902, P<0.0001). In contrast, the OUES %pred did not correlate significantly with above parameters (r = 0.125, −0.015, 0.493, 0.179, −0.136, all P>0.05).
Table 2. Correlations between OUE and key abnormal parameters for IPAH patients (N = 32).
| OUEP %pred | OUES %pred | |
| NYHA | −0.724** | 0.125 |
| mPAP, mm Hg | −0.338 | −0.351 |
| TPVR, mm Hg/L/min | −0.694** | −0.015 |
| CI, L/min/m2 | 0.295 | 0.047 |
| DLco, ml/mm Hg/min | 0.577* | 0.493 |
| PeakV˙O2, (%pred) | 0.460 | 0.009 |
| Peak PETCO2, mm Hg | 0.680** | 0.179 |
| Lowest V˙E/V˙CO2 (%pred) | −0.902** | −0.136 |
*P<0.05, **P<0.005.
The abbreviation definitions are same as Table 1.
Comparison between OUEP and OUES for IPAH patients
Table 3 compares the mean and variability of the OUEP and OUES values in the 32 IPAH patients. The coefficient of variation(COV) of the OUEP (20.9%) was significantly lower than that of the OUES (34.3%) (P<0.0001).
Table 3. Mean, SD, range and COV of OUE measurements during Cardiopulmonary Exercise Testing in IPAH patients (N = 32).
| OUEP (ml/L) | OUES [L/min/log(L/min)] | |
| Mean±SD | 23.4±4.9 | 1.1±0.4 |
| Range | 11.0-31.0 | 0.51-1.76 |
| COV | 20.9%*** | 34.3% |
***P<0.0001 by paired t test, versus OUES.
COV = coefficient of variation (SD/mean); all other abbreviation definitions are same as Table 1.
Discussion
Although previous studies have demonstrated the clinical utility of CPET in patients with IPAH [3], our study is the first to evaluate the value of OUE measurements driven from CPET in these patients. In addition, our study is the first to show that the decreased OUE can also be a marker representing impaired gas exchange in patients with IPAH. Moreover, we have shown that, beyond the traditional measurements of exercise capacity and ventilatory efficiency, OUEP is better than OUES, because it is less variable and is more significantly correlated with resting pulmonary hemodynamics in these patients.
In the present study, the usual parameters of exercise capacity and gas exchange (V˙peak O2, peak work rate, anaerobic threshold, peak heart rate, peak O2 pulse, peak PETCO2, V˙E-V˙CO2 slope and lowest V˙E/V˙CO2) were all abnormal in the IPAH patients (Table 1). Peak V˙O2, anaerobic threshold, V˙E-V˙CO2 slope, lowest V˙E/V˙CO2, and PETCO2 are the most commonly used clinical parameters for diagnostic and prognostic information [8], [15]. Peak V˙O2 is reduced in patients with higher total pulmonary vascular resistance and lower cardiac index and is highly correlated with the amount of functional pulmonary vascular bed [23]. However, it is strongly influenced by the patients' motivation and supervisors' subjective choice of ending test. In searching for more objective, reliable sub-maximal variables, anaerobic threshold (AT) has been tested. Although AT is significantly correlated with peak V˙O2 [24], it is often not easy to identify, as was the case with 5 of our patients. The AT is also subject to substantial inter-observer and intra-observer variability [25]. Recently, the values of V˙E/V˙CO2 during moderate exercise have been demonstrated as diagnostic and prognostic values in heart failure patients [26].The mechanism responsible for elevated V˙E/V˙CO2 in IPAH patients is considered to be multifactorial. In normal subjects, the ventilatory response (V˙E) is approximately linear with the CO2 output (V˙CO2) during exercise before ventilatory compensation point [22]. In IPAH patients, elevated V˙E/V˙CO2 levels manifest that the ventilation of underperfused alveoli causes an increase in dead space ventilation [4]. Increased V˙E/V˙CO2 levels have also been significantly correlated with decreased cardiac output, elevated pulmonary arterial pressures, decreased alveolar-capillary membrane conductance, and diminished heart rate variability [27]–[29]. In patients with severe IPAH, the V˙E/V˙CO2 ratio correlates significantly with pulmonary vascular resistance but not with mean pulmonary arterial pressure or cardiac index [30]. Additionally, both resting and peak exercise PETCO2 values have prognostic value in patients with heart failure [31]–[32]. However PETCO2 values are susceptible to multiple factors such as acute hyperventilation, increased dead space (due to emphysema or other lung diseases), or rapid shallow breathing patterns, all of which will reduce the PETCO2 independently of cardiac function [3]. Compared with all of the above CPET variables, the analysis of OUE has been limited, especially in patients with IPAH.
Neither OUES nor OUEP is included in the traditional 9-panel plots [9]. However, they can be measured noninvasively without additional patient effort [4]–[6]. The OUE may have important prognostic value in exercise physiology in patients with chronic heart failure [15], [33]. Davies et al[33] assessed OUES in 243 patients with chronic heart failure and found that only OUES was identified as the sole significant independent prognostic variable in a multivariable model, compared with standard exercise variables. We calculated reference values for OUEP and found that OUEP was the best predictor of mortality (P<0.0001) in a study of patients with left heart failure, better than OUES or any other CPET variables. When combined with oscillatory breathing, the odds ratio for death in 6 months increased to 56.3[14]–[15].
The OUE during exercise in normal subjects is mainly impacted by several factors including cardiac output; alveolar and dead space ventilation; and the matching of the changes in cardiac output and pulmonary blood flow with the increase in alveolar ventilation [14]. We postulate that decreased OUE during CPET in IPAH patients in our present study might be due to an abnormally high pulmonary vascular resistance, leading to the greater right ventricular afterload and reducing cardiac output as well as pulmonary blood flow. The highest OUE usually occurs near AT in normal subjects, because at that time ventilation is often most efficient and matching of perfusion to ventilation is optimal. However, in IPAH patients the volume of pulmonary capillary bed is reduced and the distal pulmonary arteries lose their ability to dilate during exercise. The lower ratio of V˙O2 to V˙E during CPET may be predominantly attributed to the inability to improve ventilation/perfusion match and distribution of blood flow to the metabolizing muscles for IPAH patients. Furthermore, we found that OUEP was sub-maximal exercise parameter, better than the OUES, and did not require maximal exertion, so the OUEP might be more fitted for IPAH patients unable to perform maximal exercise test. As shown in figure 2 and Table 3 in our present study, the OUEP was relatively easier to visualize, recognize, calculate and had less variability than OUES. Our study demonstrated that OUEP %pred was correlated negatively with NYHA functional class (r = −0.724, P<0.005), TPVR (r = −0.694, P<0.005), and lowest V˙E/V˙CO2 (r = −0.902, P<0.0001) and positively with DLco %pred (r = 0.577, P<0.05) and peak PETCO2 (r = 0.68, P<0.005). In contrast, the OUES did not significantly correlate with above parameters. We also demonstrated that OUEP had less variability and higher predictability than OUES for normal subjects regardless of the age, gender, or height[14].
Recently,we were the first one to investigate the full exercise response pattern, exercise physiology and predictions of oxygen uptake efficiency (OUE, i.e. V˙O2/V˙E, ml/L) and ventilatory efficiency of carbon dioxide elimination (V˙E/V˙CO2), their key measurements OUEP and the lowest V˙E/V˙CO2, in normal subjects[14], [22] and described their pathophysiological evidence and prognostic importance of early death, specifically as %pred, in patients with left ventricular heart failure[14]–[16]. We also identified that oscillatory breathing did not interfere with measurements of OUEP, OUE@AT, lowest V˙E/V˙CO2 and V˙E/V˙CO2@AT. However, the OUE response during exercise and the OUEP and OUE@AT were not investigated for IPAH patients. As shown in Figure 3 in our present study, both OUE and V˙E/V˙CO2 abnormalities indicate lower ventilatory efficiency of oxygen uptake and carbon dioxide elimination in IPAH patients. They result from the compensative over driven hyperventilation in order to maintain the required metabolic rate of V˙O2 and V˙CO2 mainly due to the limitation of blood flow perfusion, i.e. Q/VA mismatch. This is a similar mechanism as we previously described in patients with left ventricular heart failure and IPAH[4], [6], [14]–[16]. This gas exchange pathophysiology is more clear and easy understanding after we created the new theoretical system of “Holistic Integrative Physiology and Medicine”, which demonstrates the intra-coupling pulmonary and cardiovascular systems for the maintenance of metabolic homeostasis in whole body, and gas exchange measurement of CPET is one typical clinical example[34]–[35]. V˙E can be performed by lungs only, but V˙O2 and V˙CO2 gas exchange needs lung-heart to work in coordination. In primary cardiovascular diseases without the malfunction of other systems, the heart function is limited (as lower V˙O2) and the lungs will compensate with hyperventilation (as higher V˙E). Therefore in this regard, the OUEP may be advantageous in evaluating cardiovascular function and gas exchange abnormality for patients with IPAH.
Study Limitations
It is a single center study with smaller sample size; a higher ratio of female distribution (F20/M12). So we plan to do a future investigation to retrospectively and prospectively analyze all IPAH patients from our center.
Conclusion
In conclusion, the OUEP, which can be calculated from retrospective data could offers a new, objective and effort-independent method for evaluating the gas exchange abnormality in patients with IPAH.
Acknowledgments
The authors thank Hai-Jian Liu and Shu-Juan Chen for invaluable support and collaboration in this study. The authors thank Dr. James E. Hansen at Los Angeles Biomedical Research Institute at Harbor-UCLA Medical Center, Torrance, CA, USA for his generous and professional editing.
Funding Statement
This retrospective CPET data reanalysis is partially supported by Chinese Academy of Medical Sciences (No. 2012-YJR02), Key Project Starting Grant from National Center for Cardiovascular Diseases. CPET data collected at Shanghai Pulmonary Hospital were partially supported from Chinese Medicine Association (No. 08020420120) and science and technology commission of shanghai municipality (NO. 11411951302 and 114119a3000). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Rich S, Dantzker DR, Ayres SM, Bergofsky EH, Brundage BH, et al. (1987) Primary pulmonary hypertension: a national prospective study. Ann Intern Med 107: 216–223. [DOI] [PubMed] [Google Scholar]
- 2. Rubin LJ (1997) Current concepts: primary pulmonary hypertension. N Engl J Med 336: 111–117. [DOI] [PubMed] [Google Scholar]
- 3. American Thoracic Society, American College of Chest Physicians (2003) ATS/ACCP statement on cardiopulmonary exercise testing. Am J Respir Crit Care Med 167: 211–277. [DOI] [PubMed] [Google Scholar]
- 4. Sun XG, Hansen JE, Oudiz RJ, Wasserman K (2001) Exercise pathophysiology in patients with primary pulmonary hypertension. Circulation 104: 429–435. [DOI] [PubMed] [Google Scholar]
- 5. Yasunobu Y, Oudiz RJ, Sun XG, Hansen JE, Wasseeman K (2005) End-tidal Pco2 abnormality and exercise limitation in patients with primary pulmonary hypertension. Chest 127: 1637–1646. [DOI] [PubMed] [Google Scholar]
- 6. Sun XG, Hansen JE, Oudiz RJ, Wasseeman K (2002) Gas exchange detection of exercise-induced right-to-left shunt in patients with primary pulmonary hypertension. Circulation 105: 54–60. [DOI] [PubMed] [Google Scholar]
- 7. Oudiz RJ, Roveran G, Hansen JE, Sun XG, Wasserman K (2007) Effect of sildenafil on ventilatory efficiency and exercise tolerance in pulmonary hypertension. Eur J Heart Fail 9: 917–921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Oudiz RJ, Middle R, Hovanesyan A, Sun XG, Roveran G, et al. (2010) Usefulness of right-to-left shunting and poor exercise gas exchange for predicting prognosis in patients with pulmonary arterial hypertension. Am J Cardiol 105(8): 1186–1191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wasserman K, Hansen JE, Sue DY, Stringer WW, Whipp BJ (2011) Principles of Exercise Testing and Interpretation, 5th ed. Philadelphia: Lippincott, Williams & Wilkins 568.
- 10. Baba R, Nagashima M, Goto M, Nagano Y, Yokota M, et al. (1996) Oxygen uptake efficiency slope: a new index of cardiorespiratory functional reserve derived from the relation between oxygen uptake and minute ventilation during incremental exercise. J Am Coll Cardiol 28: 1567–1572. [DOI] [PubMed] [Google Scholar]
- 11. Hollenberg M, Tager IB (2000) Oxygen uptake efficiency slope: an index of exercise performance and cardiopulmonary reserve requiring only submaximal exercise. J Am Coll Cardiol 36: 194–201. [DOI] [PubMed] [Google Scholar]
- 12. Baba R, Tsuyuki K, Kimura Y, Ninomiya K, Aihara M, et al. (1999) Oxygen uptake efficiency slope as a useful measure of cardiorespiratory functional reserve in adult cardiac patients. Eur J Appl Physiol Occup Physiol 80: 397–401. [DOI] [PubMed] [Google Scholar]
- 13. Van Laethem C, Van De Veire N, De SJ, Bartunek J, De Backer G, et al. (2006) Prospective evaluation of the oxygen uptake efficiency slope as a submaximal predictor of peak oxygen uptake in aged patients with ischemic heart disease. Am Heart J 152: 297–315. [DOI] [PubMed] [Google Scholar]
- 14. Sun XG, Hansen JE, Sringer WW (2012) Oxygen uptake efficiency plateau: physiology and reference values. Eur J Appl Physiol 112: 919–928. [DOI] [PubMed] [Google Scholar]
- 15. Sun XG, Hansen JE, Sringer WW (2012) Oxygen uptake efficiency plateau best predicts early death in heart failure. Chest 141: 1284–1294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Sun XG, Hansen JE, Sringer WW (2012) A simple new visualization of exercise data discloses pathophysiology and severity of heart failure. J Am Heart Assoc 1: e001883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Simonneau G, Robbins IM, Beghetti M, Channick RN, Delcroix M, et al. (2009) Updated clinical classification of pulmonary hypertension. J Am Coll Cardiol 54: S43–S54. [DOI] [PubMed] [Google Scholar]
- 18. Cotes JE, Chinn DJ, Quanjer PH, Roca J, Yernault JC (1993) Standardization of the measurement of transfer factor (diffusing capacity). Report Working Party Standardization of Lung Function Tests, European Community for Steel and Coal. Official Statement of the European Respiratory Society. Eur Respir J 6: Suppl. 16, S41–S52. [PubMed] [Google Scholar]
- 19. Stocks J, Quanjer PH (1995) Reference values for residual volume, functional residual capacity and total lung capacity. ATS workshop on lung volume measurements. Official Statement of the European Respiratory Society. Eur Respir J 8: 492–506. [DOI] [PubMed] [Google Scholar]
- 20. Mu K, Liu S (1990) Summary of Chinese pulmonary function normal values. Beijing Medical University and Peking Union Medical College Press 2: 83–86. [Google Scholar]
- 21. Beaver WL, Wasserman K, Whipp BJ (1986) A new method for detecting anaerobic threshold by gas exchange. J Appl Physiol 60: 2020–2027. [DOI] [PubMed] [Google Scholar]
- 22. Sun XG, Hansen JE, Garatachea N, Storer TW, Wasserman K (2002) Ventilatory efficiency during exercise in healthy subjects. Am J Respir Crit Care Med 166: 1443–1448. [DOI] [PubMed] [Google Scholar]
- 23. Guazzi M, Myers J, Arena R (2005) Cardiopulmonary exercise testing in the clinical and prognostic assessment of diastolic heart failure. J Am Coll Cardiol 46: 1883–1890. [DOI] [PubMed] [Google Scholar]
- 24. Itoch H, Taniguchi K, Koike A, Doi M (1990) Evaluation of severity of heart failure using ventilatory gas analysis. Circulation 81 suppl31–7. [PubMed] [Google Scholar]
- 25. Shimizu M, Myers J, Buchanan N (1991) The ventilatory threshold: method, protocol, and evaluator agreement. Am Heart J 122: 509–516. [DOI] [PubMed] [Google Scholar]
- 26. Arena R, Myers J, Guazzi M (2008) The clinical and research applications of aerobic capacity and ventilatory efficiency in heart failure: an evidence-based review. Heart Fail Rev 13: 245–269. [DOI] [PubMed] [Google Scholar]
- 27. Reindl I, Werneck KD, Opitz C (1998) Impaired ventilatory efficiency in chronic heart failure: possible role of pulmonary vasoconstriction. Am Heart J 136: 778–85. [DOI] [PubMed] [Google Scholar]
- 28. Mortara A, La Rovere MT, Pinna GD (1997) Arterial baroreflex modulation of heart rate in chronic heart failure: clinical and hemodynamic correlates and prognostic implications. Circulation 96: 3450–8. [DOI] [PubMed] [Google Scholar]
- 29. Ponikowski P, Anker SD, Chua TP (1997) Depressed heart rate variability as an independent predictor of death in chronic congestive heart failure secondary to ischemic or idiopathic dilated cardiomyopathy. Am J Cardiol 79: 1645–50. [DOI] [PubMed] [Google Scholar]
- 30. Ting H, Sun XG, Chuang ML, Lewis DA, Hansen JE, et al. (2011) A noninvasive assessment of pulmonary perfusion abnormality in patients with primary pulmonary hypertension. Chest 119: 824–832. [DOI] [PubMed] [Google Scholar]
- 31. Arena R, Myers J, Abella J, Pinkstaff S, Brubaker P, et al. (2008) The partial pressure of resting end-tidal carbon dioxide predicts major cardiac events in patients with systolic heart failure. Am Heart J 156: 982–988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Arena R, Guazzi M, Myers J (2007) Prognostic value of end-tidal carbon dioxide during exercise testing in heart failure. Int J Cardiol 117: 103–108. [DOI] [PubMed] [Google Scholar]
- 33. Davies LC, Wensel R, Georgiadou P, Cicoira M, Coats AJ (2006) Enhanced prognostic value from cardiopulmonary exercise testing in chronic heart failure by non-linear analysis: oxygen uptake efficiency slope. Eur Heart J 27: 684–690. [DOI] [PubMed] [Google Scholar]
- 34. Sun XG (2013) New theoretical system of holistic integrative physiology and medicine: integrative control and regulation of human functions in whole body. Chinese Circulation Journal 28: 88–92. [Google Scholar]
- 35. Sun XG (2013) New theoretical system of holistic control and regulation for life and cardiopulmonary exercise testing. Medicine and Philosophy 34: 22–27. [Google Scholar]