Abstract
Objective
The goals of this research was (1) to analyze the role of emotional eating behavior on weight-loss progression during a 30-week weight-loss program in 1,272 individuals from a large Mediterranean population and (2) to test for interaction between CLOCK 3111 T/C SNP and emotional eating behavior on the effectiveness of the weight-loss program.
Design and Methods
A total of 1,272 overweight and obese participants (BMI: 31±5 kg/m2), aged 20 to 65 years, attending outpatient weight-loss clinics were recruited for this analysis. Emotional eating behavior was assessed by the Emotional Eating Questionnaire (EEQ), a questionnaire validated for overweight and obese Spanish subjects. Anthropometric measures, dietary intake and weight-loss progression were assessed and analyzed throughout the 30-week program. Multivariate analysis and linear regression models were performed to test for gene-environment interaction.
Results
Weight-loss progression during the 30-week program differed significantly according to the degree of emotional eating behavior. Participants classified as ‘very emotional eaters’ experienced more irregular (P = 0.007) weight-loss, with a lower rate of weight decline (−0.002 vs. −0.003, P<0.05) in comparison with less emotional eaters. The percentage of weight-loss was also significantly higher in ‘non-emotional eaters’ (P = 0.009). Additionally, we identified a significant gene-environment interaction associated with weight-loss at the CLOCK 3111 T/C locus (P = 0.017). By dichotomizing the emotional eating behavior score, linear regression analysis indicated that minor C allele carriers with a high emotional score (> = 11), lost significantly less weight than those C carriers with a low emotional score (<11) (P = 0.005).
Conclusions
Emotional eating behavior associates with weight-loss pattern, progression and total weight-loss. Additionally, CLOCK 3111 T/C SNP interacts with emotional eating behavior to modulate total weight loss. These results suggest that the assessment of this locus and emotional eating behavior could improve the development of effective, long-tern weight-management interventions.
Introduction
Lifestyle interventions addressing cognitive behavior and including both dietary and physical activity components are the most effective for the treatment of overweight and obesity [1]–[3]. These interventions achieve short-term weight-loss averaging between 5 to 10 percent, in addition to significant improvements in various health parameters such as blood pressure, cholesterol levels and glycemic control [4]–[6]. However, this modest weight-loss often is followed by subsequent weight regain [2], [7], [8]. As a result, researchers and clinicians now pay close attention to behavioral and psychological factors that may impact the long-term success of weight-loss programs [2], [6], [9]. Factors contributing to low intervention success include emotional eating, previous weight-loss attempts, binge eating, eating disinhibition, body dissatisfaction, lower self-motivation and genetic background [9]–[16].
The association between emotional eating, dietary intake and body weight in particular is becoming an area of increased interest in obesity research [17], [18]. Studies suggest that emotional eaters tend to eat more when experiencing negative emotions such as anger, irritability, fear, sadness, or boredom [19]. As a result, there is a significant association between emotional eating behavior and total weight gain, with a particular increase in the intake of energy dense, nutrient poor foods [9], [20]–[23]. Emotional eaters additionally lose less weight following a weight-loss intervention or program [9]. To complement these results, additional studies are required to assess the role of emotional eating behavior on weight-loss progression and patterns [9], [11], [12], [22].
Abnormalities in the circadian system underlie the development of many illnesses and conditions such as mood disorders, obesity and metabolic syndrome [24]. CLOCK (Circadian Locomotor Output Cycles Kaput) is a component of the circadian system, regulating the expression of other integral circadian genes [25], [26]. Studies have found that variants of the CLOCK gene are associated with human behaviors and depression, particularly the CLOCK 3111 T/C single-nucleotide polymorphism (SNP) [27], [28]. This SNP resides in the 3′ UTR of the gene, and is predicted to affect CTCF transcription factor binding site, as supported by CHIP-seq evidence from the RegulomeDB database [29]. The minor C allele has been associated with psychiatric disorders, shorter sleep duration, increased BMI, higher energy intake and also weight-loss impairment [16], [30]–[32]. Because of the deleterious associations between the minor allele and multiple relevant phenotypes, we hypothesize that CLOCK 3111 T/C SNP modulates the association between emotional eating behavior and total weight-loss loss, where minor allele carriers with high emotional scores will experience lower weight-loss than minor allele carriers with low emotional scores.
The first aim of this study was to analyze the role of emotional eating behavior on weight-loss progression, pattern, and total weight-loss during a 30-week weight-loss program in 1,272 individuals from a large Mediterranean population. The second aim was to test for interaction between CLOCK 3111 T/C SNP and emotional eating behavior, on the effectiveness of the weight-loss program as assessed by the total weight-loss at the end of the program.
Method
Participants
Between 2008 and 2011, 1,550 subjects voluntarily attended five weight loss clinics in Spain for dietetic and behavioural treatment based upon the principles of a Mediterranean diet [33]. All participants were from the Spanish city of Murcia, located on the Southeast coast of the Mediterranean Sea. Participants were excluded (n = 278) for the following reasons; receiving treatment with thermogenic, lipogenic, or contraceptive drugs; diabetes mellitus, chronic renal failure, hepatic diseases, or cancer diagnosis; bulimia diagnosis, prone to binge eating, or undergoing treatment with anxiolytic or antidepressant drugs; or under the age of 14 or above 75 years. A total of 1,272 overweight and obese subjects (226 men and 1046 women; Mean BMI: 31 SD: 5 kg/m2) were finally enrolled in the study. Participants' data were codified to guarantee anonymity. All procedures were in accordance with good clinical practice.
Ethics
Written informed consent was obtained before subjects were enrolled in the study and was performed in accordance with the Helsinki Declaration of Human Studies and approved by the Ethical Committee of the University of Murcia.
Intervention
The structure of the program has been described elsewhere in detail [34]. Subjects attended 60-minute therapy sessions once per week. The mean duration of the program was 30-weeks and varied depending on the weight-loss goal. Once the weight-loss goal was achieved, participants followed a five-month maintenance period. Weight was recorded weekly throughout the weight-loss phase of the program. Certified nutritionists led the program sessions. Dietetic treatment was based on the principles of the Mediterranean diet and the distribution of the macronutrient components adhered to the recommendations of the Spanish Society of Community Nutrition [33], [35].
Measures
Emotional eating
Emotional eating was assessed using the Emotional Eating Questionnaire (EEQ), a self-reported questionnaire, administered at the start of the program. The questionnaire was developed and validated directly with Spanish overweight and obese subjects [36]. The questionnaire consists of 10 items designed to assess the extent that emotions affect eating behavior. Examples of the items are: “Do you feel less control over your diet when you are tired after work at night?” and “Do you eat more of your favorite food and with less control when you are alone?” All questions have four possible responses: never, sometimes; generally, and always. Each response was given a score ranging from 0 to 3, with lower scores reflecting healthier behavior.
Initially, subjects were classified into four groups according to scores obtained from the EEQ: (1) scores between 0–5, non-emotional eater; (2) scores between 6–10, low emotional eater; (3) scores between 11–20, emotional eater; and (4) scores between 21–30, very emotional eater. To facilitate additional statistical analyses and future potential clinical application, participants were also dichotomized into emotional and non-emotional eaters using the median emotional score of the population as the cut-off point (<11, non-emotional; ≥11, emotional).
Principal component analysis of the EEQ results identified three factors that explained 60 percent of the total variance in emotional eating. These factors were Disinhibition (Factor 1), which includes questions related to loss of control over one's eating behavior; Type of food (Factor 2), which includes questions such as, “Is it difficult for you to stop eating sweet things, especially chocolate?” and “Do you crave specific foods?”; and finally Guilt (Factor 3), which includes questions such as, “Do you feel guilty when eating ‘forbidden’ foods, such as sweets or snacks?” [36].
Anthropometric measurements
Anthropometric measurements were assessed at baseline, and weight was monitored throughout the 30-week program. Participants were weighed while barefoot, wearing light clothes, on a digital scale that measured to the nearest 0.1 kg. Height was measured at baseline using a Harpenden digital stadiometer (rank, 0.7–2.05). Participants were positioned upright and relaxed with the head in the Frankfurt plane. Both height and weight measurements were collected at the same time of the day for all participants. Initial BMI was calculated using baseline measurements as weight (kg) height (m)−2. Initial total body fat was measured with bioelectrical impedance, using TANITA TBF-300 (Tanita Corporation of America, Arlington Heights, IL, USA) equipment. Subjects were requested not to drink liquids during the two hours prior to measurement collection. Body fat distribution was also assessed throughout the intervention, and included waist circumference at the level of the umbilicus and hip circumference with the greatest circumference over the greater trochanters. These measurements were used to calculate the waist to hip ratio.
Dietary intake
Baseline nutrient intake was determined by means of a 24-hour dietary recall, as described previously [33].
Treatment effectiveness
To assess differences in weight-loss progression and pattern over time among the four emotional eating behavior classifications according to the EEQ questionnaire, repeated analysis of covariance (ANCOVA) measurements for weight and week of treatment were used. Data were adjusted for age, sex, and initial BMI with a post hoc Bonferroni adjustment. In order to compare the rate of weight-loss during the program, the slope of the weight-loss curves was calculated for each group.
Moreover, total weight-loss and weight-loss as a percentage of initial weight was calculated to assess the efficacy of the program. Effective treatment classification was based on two parameters: total weight-loss of more than 10 percent of baseline weight, and program attrition as calculated by the percentage of subjects who dropped out of the program prior to reaching a weight-loss of 10 percent of their baseline weight.
DNA isolation and CLOCK genotyping
DNA was isolated from blood samples using standard procedures (Qiagen, Valencia, CA, USA). We performed genotyping of the CLOCK 3111T/C SNP using a TaqMan assay with allele-specific probes on the ABI Prism 7900HT Sequence Detection System (Applied Biosystems, Foster City, CA, USA) according to the standardized laboratory protocols.
Statistical Analyses
Differences in anthropometric measurements and weight-loss between emotional and non-emotional eaters were compared by analysis of covariance (ANCOVA), after adjustment for age, sex, and initial BMI in every approach, except for the association with obesity that was only corrected for age and sex. Correlation coefficients were generated to evaluate relationships between EEQ score and age. A dominant genetic model was applied for the CLOCK 3111 T/C SNP as previously described [32]. Student t test was applied to compare crude means across genotype groups. Multivariate adjustments of the associations by analysis of covariance and estimated adjusted means were performed. All genetic analyses adjusted for sex, age, clinic and study number. All statistical analyses were performed using R statistical software (v. 3.0.0). A two-tailed P-value of <0.05 was considered statistically significant.
Results
Baseline characteristics of the population studied are shown in Table 1. Briefly, the mean EEQ score in the total sample of 1,272 participants was 11.84 (SD = 5.98). According to the score, about 64% of individuals were classified as ‘emotional eaters’. Additionally, the score was higher in women (M = 12.3, SD = 5.7) than in men (M = 9.19, SD = 6.29) (P<0.05), and decreased significantly with age (r = −0.12; P<0.0001).
Table 1. Initial characteristics of the study population (n = 1,272).
| Characteristics/Measures | M | SD |
| Age (yrs) | 39.4 | 12.1 |
| BMI (kg/m2) | 31.15 | 5.27 |
| Body fat (%) | 37.31 | 6.62 |
| Waist (cm) | 102.2 | 14.6 |
| Hip (cm) | 113.9 | 10.0 |
| Dietary Intake | ||
| Total Energy (kcal/day) | 2075 | 715 |
| Extra calories in snacking (kcal/day) | 372 | 425 |
| Proteins (% total energy) | 17.0 | 4.7 |
| Proteins (g/day) | 86.0 | 33.0 |
| Carbohydrates (% total energy) | 41.6 | 10.5 |
| Carbohydrates (g/day) | 214.2 | 87.8 |
| Fats (% total energy) | 42.5 | 9.4 |
| Fats (g/day) | 99.3 | 44.8 |
| Fiber (g/day) | 18.7 | 11.0 |
| MUFA (% total fat) | 55.5 | 8.0 |
| PUFA (% total fat) | 13.7 | 3.8 |
| SFA (% total fat) | 29.9 | 8.4 |
| Other Characteristics | n | % |
| BMI≥30 kg/m2, n (%) | 673 | 53.6 |
| Drinkers, n (%) | 713 | 56.1 |
| Smokers, n (%) | 295 | 23.2 |
| Sedentary, n (%) | 559 | 44 |
| CLOCK 3111 T/C SNP | n | % |
| CC, n (%) | 104 | 8.17 |
| CT, n (%) | 492 | 38.7 |
| TT, n (%) | 676 | 53.1 |
Note. Data are presented as mean (M) and standard deviation (SD);
BMI = Body Mass Index; MUFA = Monounsaturated Fatty Acids; PUFA = Polyunsaturated Fatty Acids; SFA = Saturated Fatty Acids.
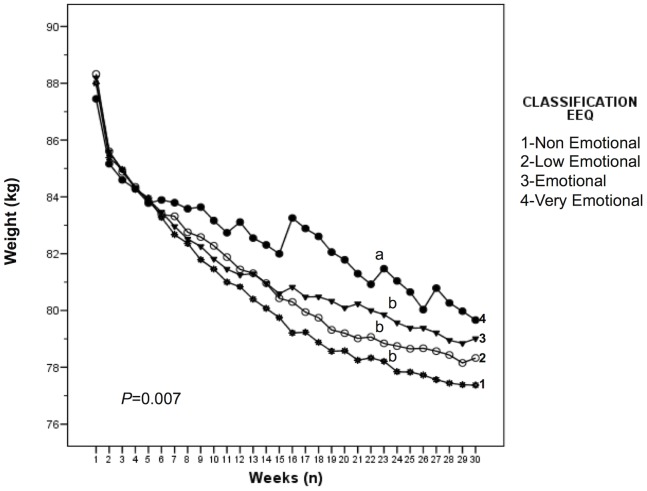
Weight-loss patterns differed significantly among the four classification groups (‘non-emotional eaters’, ‘low emotional eaters’, ‘emotional eaters’, and ‘very emotional eaters’) as assessed by a repeated ANCOVA measures adjusted for sex, age, and initial weight for the outcome of weight loss (P = 0.007) (Figure 1). Moreover, weight-loss analyses within each weekly time point (ANCOVA) among the four classifications indicated significant differences exist in weight loss (P = 0.03). Specifically, post hoc Bonferroni analyses indicated that weight-loss progression significantly differed between the ‘very emotional eaters’ group and each of the other three groups (‘emotional eaters’, ‘low emotional eaters’, and ‘non-emotional eaters’) (P<0.05) (Figure 1). The rate of weight-loss, as assessed by the slope of the weight-loss curves, also differed between the highly emotional group and the other groups (−0.002 vs. −0.003, P<0.05).
Figure 1. Weight-loss progression during the 30-weeks of treatment stratified by emotional eating based on EEQ classification.
Weight-loss analyses within each single time point among the four classifications indicated significant differences exist (P = 0.03). Weight-loss progression differed significantly between the ‘very emotional eaters’ group and the three other groups (‘emotional eaters’, ‘low emotional eaters’, and ‘non-emotional eaters’) (P<0.05). The rate of weight-loss, as assessed by the slope of the weight-loss curves, also differed between the highly emotional group and the other groups (−0.002 vs. −0.003, P<0.05).
Table 2 represents the results from assessing the effectiveness of the program according to the original four levels EEQ classification, as well as the dichotomized classification. In both classifications, treatment was significantly more effective in ‘non-emotional eaters’, where a significantly higher percentage of participants achieved a weight-loss of more than 10 percent of baseline weight. Additionally, EEQ scores were significantly higher among those who dropped out of the program (M = 12.27, SD = 5.91) than those who adhered to treatment and completed the program (M = 11.49, SD = 5.79) (P = 0.026).
Table 2. Treatment effectiveness in different categories of emotional eating.
| NEE-1 | LEE-2 | EE-3 | VEE-4 | P | NEE | EE | P | |
| n = 385 | n = 687 | |||||||
| Parameters (could be Outcomes) | EEQ score classification (Four groups) | Clinical classification (Two groups) Or –Classification based on population median (two groups) | ||||||
| Subjects achieving weight goal (%) | 43.5% | 32.3% | 28.9% | 22.1% | <0.001 | 36.4% | 26.5% | <0.001 |
| Weight loss (% of initial weight) | 9.13±0.48a | 8.17±0.35a | 8.04±0.28a | 6.47±0.61b | 0.009 | 8.45 | 7.44 | 0.007 |
| Attrition (%) | 28.8% | 35.4% | 35.2% | 48.5% | 0.007 | 38.9% | 41.0% | 0.291 |
| Total weight loss (kg) | 7.897±0.415a | 6.980±0.299a | 6.982±0.241a | 5.795±0.525b | 0.021 | 7.17±0.25 | 6.54±0.21 | 0.065 |
Note. EEQ = Emotional Eating Questionnaire; NEE-1 = Non-emotional eaters in four groups criterion (EEQ scores between 0–5); LEE-2 = Low emotional eaters in four groups criterion (EEQ scores between 6–10); EE-3 = Emotional eaters in four groups criterion (EEQ scores between 11–20); VEE-4 = Very emotional eaters in four groups criterion (EEQ scores between 21–30); NEE = Non-emotional eaters median (EEQ scores <11); EE = Emotional eaters in median criterion (EEQ scores ≥11); P = p-values after adjusting for age, sex, and initial BMI. Above – the word clinical implies that you treated them differently (although perhaps this will be your recommendation for the future, that they need different approaches).
When participants were dichotomized into ‘emotional eaters’ and ‘non-emotional eaters’, baseline measures of obesity and dietary intake were also different between ‘emotional eaters’ and ‘non-emotional eaters’. ‘Emotional eaters’ had significantly higher BMI (P = 0.001), overall energy intake (P = 0.023), and carbohydrate intake (P = 0.001) than ‘non-emotional eaters’ (Table 3). When we examined the relationship between CLOCK 3111 T/C genotype and emotional eating, no significant differences were found in the frequency of the minor C allele between ‘emotional eaters’ and ‘non-emotional eaters’.
Table 3. Measures of obesity and dietary intake at baseline in emotional and non-emotional eaters.
| Measures | EE (n = 732) | NEE (n = 540) | P |
| BMI (kg/m2) | 31.46±0.20 | 30.70±0.23 | 0.001 |
| Body fat (%) | 37.6±6.5 | 36.6±6.9 | 0.100 |
| Waist (cm) | 102±0.5 | 101±0.6 | 0.203 |
| WHR | 0.89±0.003 | 0.89±0.003 | 0.642 |
| Energy intake (kcal/day) | 2120.20±32 | 2006±37 | 0.023 1 |
| Carbohydrates (g) | 223±4 | 204±4 | 0.001 1 |
| Proteins (g) | 87±1 | 83±1 | 0.1061 |
| Fats (g) | 100±2 | 97±2 | 0.2871 |
| Carbohydrates (% of total energy) | 42.3 | 41.0 | 0.0831 |
| Proteins (% of total energy) | 16.7 | 17.2 | 0.2341 |
| Fats (% of total energy) | 42.1 | 42.7 | 0.3621 |
| CC+CT (%) | 46.4 | 47.4 | 0.917 |
| TT (%) | 53.6 | 52.6 | 0.923 |
Note. NEE = Non-emotional eaters in median criterion (EEQ scores <11); EE = Emotional eaters in median criterion (EEQ scores ≥11); BMI = Body Mass Index; WHR = Waist/Hip ratio; P = p-values adjusted for age and sex;
p-values adjusted for age, sex, and initial BMI.
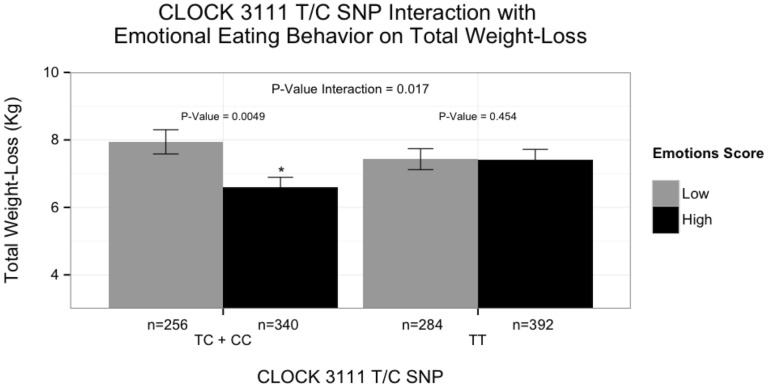
Finally, we examined CLOCK 3111 T/C genotype in the context of emotional eating and identified a significant gene-environment interaction associated with total weight-loss. By dichotomizing the participants into ‘emotional eaters’ and ‘non-emotional eaters’, we found significantly different effects across genotypes at this locus (β±SE: 1.53±0.64; P = 0.017) (Figure 2). Among minor C allele carriers, ‘emotional eaters’ lost significantly less weight than ‘non-emotional eaters’ (β±SE: −1.29±0.46; P = 0.0049). However, no significant differences were identified between ‘emotional eaters’ and ‘non-emotional eaters’ for total weight-loss among non-carriers (β±SE: 0.34±0.46; P = 0.454). Of note, when we tested for gene-environment interactions between CLOCK 3111 T/C genotype and the three different principal component factors of the EEQ (Disinhibition, Type of food, and Guilt) for weight-loss, we found that significance was only achieved for the Disinhibition factor in the gene-environment interaction (P = 0.002; data not shown).
Figure 2. Differences in weight-loss between CLOCK genotypes and emotion eating classification as assessed by EEQ.
By dichotomizing the participants into ‘emotional eaters’ and ‘non-emotional eaters’, we found significantly different effects across genotypes at this locus (P for interaction = 0.017). Among minor C allele carriers, ‘emotional eaters’ lost significantly less weight than ‘non-emotional eaters’ (P = 0.0049). However, no significant differences were identified between ‘emotional eaters’ and ‘non-emotional eaters’ for total weight-loss among noncarriers (P = 0.454). Data are presented as mean ± s.e.m. We used (*) to indicate significant differences between emotional eating groups with the same genotype (P<0.050).
Discussion
This prospective, longitudinal study demonstrates that emotional eating behavior influences the effectiveness of weight-loss treatment, by affecting weight-loss progression and patterns. Moreover, the novelty of this result is further enhanced by the original finding suggesting that the 3111 T/C SNP interacts with emotional eating behavior to modulate total weight-loss. Thus, only those ‘emotional eaters’ carrying the minor C allele lose significantly less weight than those classified as ‘non-emotional eaters.’
Studies assessing human circadian systems have identified polymorphisms in circadian clock genes that associate with mood disorders. The CLOCK 3111 T/C SNP, located in the 3′-UTR region of the CLOCK gene, associates with a higher recurrence rate of major depressive episodes in bipolar depression patients, and with greater insomnia and decreased need for sleep in bipolar patients [27], [37]. Additionally, significant associations between this polymorphism and Attention deficit hyperactivity disorder (ADHD) scores indicate a possible link between CLOCK 3111 T/C SNP with adult ADHD [38]. These and other studies suggest that the circadian system, and specifically this genetic variant, have a great impact on mood and behavior.
Furthermore, our previous findings consistently suggest the influence of the circadian system, including this variant, on obesity, obesogenic behaviors, and total weight loss. Studies in several populations indicate that carriers of the minor C allele are more susceptible to higher BMI, have higher energy intakes, higher prevalence of obesity, lower adherence to Mediterranean diet, and experience lower weight-loss [16], [30], [31], [39], [40]. Additionally, variants of core circadian clock genes are associated with greater withdrawal from behavioral weight-reduction program and attrition [41].
Likewise, emotional eating has been previously associated with weight-loss. Individuals classified as low emotional eaters tend to lose significantly more weight than those individuals classified as high emotional eaters [9], [11], [12], [42], [43]. Conversely, emotional eating appears to be associated with more barriers to weight-loss and greater weight-loss difficulties [33], [44]. In accordance with these previous findings, our results indicate that the weight-loss program was significantly more effective in non-emotional eaters, as assessed by total weight-loss and attrition. Furthermore, our results suggest that differences also exist in weight-loss progression and pattern among individuals of different emotional eating behavior classification, as assessed by weekly weight record through the 30-week period (Figure 1). Individuals classified as ‘very emotional eaters’ display the most irregular weight-loss patterns with fluctuating changes in weight, along with lower weight-loss success. This pattern suggests that weight-loss is inconsistent among highly emotional individuals during the 30-week period, possibly resulting in greater withdrawal.
In addition to the longitudinal data from the current study and previous studies that illustrate the importance of emotional eating in weight loss success, the baseline data from the current study are also suggestive. Although no consistent evidence support that obese individuals are more prone to emotional eating than normal weight individuals, our data indicate that at baseline, more than half of the obese individuals (64 percent) are classified as emotional eaters [18], [45], [46]. Moreover, our baseline findings are consistent with previous cross-sectional and experimental studies suggesting that emotional eaters have higher BMI than non-emotional eaters, and consume more sweet and energy-dense foods [19], [21]–[23], [47], [48].
Physiological and psychological mechanisms have been proposed to explain the relationship between emotions and eating behaviors [17], [49]. These theories hypothesize that emotional eaters eat in response to environmental influences instead of hunger cues, and rely on food as a coping strategy for dealing with unpleasant emotions [50]. In response to certain emotions, emotional eaters may be more likely to consume energy dense foods that are high in fat and added sugars, and whose palatability triggers endorphin release that leads to positive shifts in emotion [19], [51]. Although emotional responses may contribute to less healthy eating behaviors, evidence suggests that, the emotion itself is not eliciting dietary intake, instead it is the way emotions are managed that leads to excessive dietary intake [17], [22].
The mechanistic links between genetic variants and eating behaviors may be similarly complex. Various epigenetic and chronobiological mechanisms could explain the interaction between CLOCK and emotional eating behavior for weight-loss. Differences in methylation status of CpG sites located in CLOCK genes are associated with differences in BMI and weight loss as well as dietary intake [52]. More importantly, these changes are highly related to behavioral changes related to emotions such as constant snacking or eating when bored [52]. Altered methylation status could induce changes in the expression of circadian clock genes, influencing metabolic pathways regulating weight-loss. Alternatively, differences in total weight-loss could be explained by phenotypic differences in chronotypes (eg, behaviors related to morning and evening preferences). Carriers of the CLOCK 3111 T/C minor C allele have reduced sleep duration, elevated ghrelin concentrations and are characterized as evening chronotype [32]. These characteristics, combined with emotional eating behaviors could result in a decreased weight-loss.
Although emotional eating is generally related to less weight loss, closer examination of the components of emotional eating reveals more specific findings. One important barrier to weight-loss is disinhibition, an eating behavior associated with reduced ability to control dietary intake, resulting in increased tendency to high caloric intake. Our results indicate that the CLOCK 3111 T/C SNP specifically interacts with disinhibition, a principal component of emotional eating behavior. This suggests that high disinhibition is the main driver for this gene-environment interaction. In fact, previous works have suggested that disinhibition is associated with a higher BMI, poor food choices, and low effectiveness of weight-loss programs [53], [54].
The current study had a number of strengths and limitations. This was the first prospective, longitudinal study to assess weight-loss pattern and progression during a 30-week weight-loss program in a large cohort. Additionally, emotional eating was assessed using a questionnaire validated directly with the Spanish overweight and obese population [36]. Study limitations should also be taken into account in interpreting the findings presented here. One limitation is the exclusive use of self-reported data to measure emotional eating. However, the broad definition of ‘emotional eating’ used in the EEQ classification has demonstrated great ability in classifying emotional eaters in the present study. Therefore, the use of EEQ should be confined to healthy subjects with no relevant eating disorders. Findings from the current study have potential implications for future research and clinical practice. Current results imply that assessing EEQ and genetic variation together with other classical approaches such as assessment of energy intake and expenditure, behavioral characteristics related to barriers of weight loss [55] as well as other newer ones such as chronotype assessments [56] or timing of food intake [57] may improve weight-loss.
In conclusion, findings from the current study have possible implications for both future research and clinical practice. Indeed, considering pre-treatment psychosocial assessment that includes eating behaviors, combined with genetic assessment could provide tailored weight-loss recommendations to obese and overweight individuals. These factors may be useful in the development of alternative weight-loss approaches to those at high risk of weight-loss failure [14], [58].
Acknowledgments
We would like to thank Dolores Corbalan Tutau and Manuel Canteras for their contribution to the initial draft of the manuscript. We also acknowledge the contributions of the certified nutritionists: Teresa Hernandez, Alberto Esteban and Purificacion Gomez-Abellan, for their efforts at the clinics and special thanks to all the participants in the current study.
Funding Statement
This study was supported by grants from the Tomás Pascual and Pilar Gómez-Cuétara Foundations, the Spanish Government of Science and Innovation (BFU2011-24720), and Séneca Foundation from the Government of Murcia (15123/PI/10). National Heart, Lung, and Blood Institute grants HL-54776, National Institute of Diabetes and Digestive and Kidney Diseases, Grant Number DK075030 and by contracts 53-K06-5-10 and 58-1950-9-001 from the US Department of Agriculture Research. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Barte JCM, Bogt ter NCW, Bogers RP, Teixeira PJ, Blissmer B, et al. (2010) Maintenance of weight loss after lifestyle interventions for overweight and obesity, a systematic review. Obes Rev 11: 899–906 10.1111/j.1467-789X.2010.00740.x [DOI] [PubMed] [Google Scholar]
- 2. Carter FA, Jansen A (2012) Improving psychological treatment for obesity. Which eating behaviours should we target? Appetite 58: 1063–1069 10.1016/j.appet.2012.01.016 [DOI] [PubMed] [Google Scholar]
- 3. Mann T, Tomiyama AJ, Westling E, Lew A-M, Samuels B, et al. (2007) Medicare's search for effective obesity treatments: diets are not the answer. Am Psychol 62: 220–233 10.1037/0003-066X.62.3.220 [DOI] [PubMed] [Google Scholar]
- 4. Goldstein DJ (1992) Beneficial health effects of modest weight loss. Int J Obes Relat Metab Disord 16: 397–415. [PubMed] [Google Scholar]
- 5. Tuomilehto J, Lindström J, Eriksson JG, Valle TT, Hämäläinen H, et al. (2001) Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med 344: 1343–1350 10.1056/NEJM200105033441801 [DOI] [PubMed] [Google Scholar]
- 6. Hainer V, Toplak H, Mitrakou A (2008) Treatment modalities of obesity: what fits whom? Diabetes Care 31 Suppl 2 S269–S277 Available: http://eutils.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&id=18227496&retmode=ref&cmd=prlinks. [DOI] [PubMed] [Google Scholar]
- 7. Diabetes Prevention Program Research Group (2009) Knowler WC, Fowler SE, Hamman RF, Christophi CA, et al. (2009) 10-year follow-up of diabetes incidence and weight loss in the Diabetes Prevention Program Outcomes Study. Lancet 374: 1677–1686 10.1016/S0140-6736(09)61457-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Wing RR, Phelan S (2005) Long-term weight loss maintenance. Am J Clin Nutr 82: 222S–225S. [DOI] [PubMed] [Google Scholar]
- 9. Elfhag K, Rössner S (2005) Who succeeds in maintaining weight loss? A conceptual review of factors associated with weight loss maintenance and weight regain. Obes Rev 6: 67–85 10.1111/j.1467-789X.2005.00170.x [DOI] [PubMed] [Google Scholar]
- 10. Teixeira PJ, Palmeira AL, Branco TL, Martins SS, Minderico CS, et al. (2004) Who will lose weight? A reexamination of predictors of weight loss in women. Int J Behav Nutr Phys Act 1: 12 10.1186/1479-5868-1-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Teixeira PJ, Silva MN, Coutinho SR, Palmeira AL, Mata J, et al. (2009) Mediators of weight loss and weight loss maintenance in middle-aged women. Obesity 18: 725–735 Available: http://eutils.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&id=19696752&retmode=ref&cmd=prlinks. [DOI] [PubMed] [Google Scholar]
- 12. Karlsson J, Hallgren P, Kral J, Lindroos AK, Sjöström L, et al. (1994) Predictors and effects of long-term dieting on mental well-being and weight loss in obese women. Appetite 23: 15–26 10.1006/appe.1994.1031 [DOI] [PubMed] [Google Scholar]
- 13. Teixeira PJ, Going SB, Houtkooper LB, Cussler EC, Martin CJ, et al. (2002) Weight loss readiness in middle-aged women: psychosocial predictors of success for behavioral weight reduction. J Behav Med 25: 499–523. [DOI] [PubMed] [Google Scholar]
- 14. Teixeira PJ, Going SB, Sardinha LB, Lohman TG (2005) A review of psychosocial pre-treatment predictors of weight control. obesity reviews 6: 43–65 Available: http://eutils.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&id=15655038&retmode=ref&cmd=prlinks. [DOI] [PubMed] [Google Scholar]
- 15. Bond DS, Phelan S, Leahey TM, Hill JO, Wing RR (2009) Weight-loss maintenance in successful weight losers: surgical vs non-surgical methods. Int J Obes (Lond) 33: 173–180 10.1038/ijo.2008.256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Garaulet M, Corbalán MD, Madrid JA, Morales E, Baraza JC, et al. (2010) CLOCK gene is implicated in weight reduction in obese patients participating in a dietary programme based on the Mediterranean diet. Int J Obes (Lond) 34: 516–523 10.1038/ijo.2009.255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Evers C, Marijn Stok F, de Ridder DTD (2010) Feeding your feelings: emotion regulation strategies and emotional eating. Pers Soc Psychol Bull 36: 792–804 10.1177/0146167210371383 [DOI] [PubMed] [Google Scholar]
- 18. Geliebter A, Aversa A (2003) Emotional eating in overweight, normal weight, and underweight individuals. Eat Behav 3: 341–347. [DOI] [PubMed] [Google Scholar]
- 19. Macht M (2008) How emotions affect eating: a five-way model. Appetite 50: 1–11 10.1016/j.appet.2007.07.002 [DOI] [PubMed] [Google Scholar]
- 20. Hays NP, Roberts SB (2008) Aspects of eating behaviors “disinhibition” and “restraint” are related to weight gain and BMI in women. Obesity (Silver Spring) 16: 52–58 10.1038/oby.2007.12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Nguyen-Michel ST, Unger JB, Spruijt-Metz D (2007) Dietary correlates of emotional eating in adolescence. Appetite 49: 494–499 10.1016/j.appet.2007.03.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Konttinen H, Männistö S, Sarlio-Lähteenkorva S, Silventoinen K, Haukkala A (2010) Emotional eating, depressive symptoms and self-reported food consumption. A population-based study. Appetite 54: 473–479 10.1016/j.appet.2010.01.014 [DOI] [PubMed] [Google Scholar]
- 23. Oliver G, Wardle J, Gibson EL (2000) Stress and food choice: a laboratory study. Psychosom Med 62: 853–865. [DOI] [PubMed] [Google Scholar]
- 24. Garaulet M, Madrid JA (2010) Chronobiological aspects of nutrition, metabolic syndrome and obesity. Adv Drug Deliv Rev 62: 967–978 10.1016/j.addr.2010.05.005 [DOI] [PubMed] [Google Scholar]
- 25. Schantz Von M (2008) Phenotypic effects of genetic variability in human clock genes on circadian and sleep parameters. J Genet 87: 513–519. [DOI] [PubMed] [Google Scholar]
- 26. Scott EM, Carter AM, Grant PJ (2008) Association between polymorphisms in the Clock gene, obesity and the metabolic syndrome in man. Int J Obes (Lond) 32: 658–662 10.1038/sj.ijo.0803778 [DOI] [PubMed] [Google Scholar]
- 27. Benedetti F, Serretti A, Colombo C, Barbini B, Lorenzi C, et al. (2003) Influence ofCLOCK gene polymorphism on circadian mood fluctuation and illness recurrence in bipolar depression. Am J Med Genet 123B: 23–26 10.1002/ajmg.b.20038 [DOI] [PubMed] [Google Scholar]
- 28. Kripke DF, Nievergelt CM, Joo E, Shekhtman T, Kelsoe JR (2009) Circadian polymorphisms associated with affective disorders. J Circadian Rhythms 7: 2 10.1186/1740-3391-7-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Boyle AP, Hong EL, Hariharan M, Cheng Y, Schaub MA, et al. (2012) Annotation of functional variation in personal genomes using RegulomeDB. Genome Res 22: 1790–1797 10.1101/gr.137323.112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Garaulet M, Lee Y-C, Shen J, Parnell LD, Arnett DK, et al. (2009) CLOCK genetic variation and metabolic syndrome risk: modulation by monounsaturated fatty acids. Am J Clin Nutr 90: 1466–1475 10.3945/ajcn.2009.27536 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Garaulet M, Lee Y-C, Shen J, Parnell LD, Arnett DK, et al. (2010) Genetic variants in human CLOCK associate with total energy intake and cytokine sleep factors in overweight subjects (GOLDN population). Eur J Hum Genet 18: 364–369 10.1038/ejhg.2009.176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Garaulet M, Sánchez-Moreno C, Smith CE, Lee Y-C, Nicolás F, et al. (2011) Ghrelin, Sleep Reduction and Evening Preference: Relationships to CLOCK 3111 T/C SNP and Weight Loss. PLoS ONE 6: e17435 10.1371/journal.pone.0017435 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Jordana MC, Aza MG (2009) Major barriers to weight loss in patients attending a Mediterranean diet-based behavioural therapy: the Garaulet method. Revista Española de Obesidad 7: 144–154. [Google Scholar]
- 34. Garaulet M, Llamas FP (1999) Weight loss and possible reasons for dropping out of a dietary behavioural programme in the treatment of overweight patients. Journal of Human Nutrition and Dietetics 12: 219–227. [Google Scholar]
- 35. Serra-Majem L, Aranceta J (2001) SENC Working Group on Nutritional Objectives for the Spanish Population. Spanish Society of Community Nutrition (2001) Nutritional objectives for the Spanish population. Consensus from the Spanish Society of Community Nutrition. Public Health Nutrition 4: 1409–1413. [DOI] [PubMed] [Google Scholar]
- 36. Garaulet M, Canteras M, Morales E, López-Guimera G, Sánchez-Carracedo D, et al. (2012) Validation of a questionnaire on emotional eating for use in cases of obesity: the Emotional Eater Questionnaire (EEQ). Nutr Hosp 27: 645–651 10.1590/S0212-16112012000200043 [DOI] [PubMed] [Google Scholar]
- 37. Serretti A, Benedetti F, Mandelli L, Lorenzi C, Pirovano A, et al. (2003) Genetic dissection of psychopathological symptoms: insomnia in mood disorders and CLOCK gene polymorphism. Am J Med Genet B Neuropsychiatr Genet 121B: 35–38 10.1002/ajmg.b.20053 [DOI] [PubMed] [Google Scholar]
- 38. Kissling C, Retz W, Wiemann S, Coogan AN, Clement RM, et al. (2008) A polymorphism at the 3′-untranslated region of the CLOCK gene is associated with adult attention-deficit hyperactivity disorder. Am J Med Genet B Neuropsychiatr Genet 147: 333–338 10.1002/ajmg.b.30602 [DOI] [PubMed] [Google Scholar]
- 39.Bandín C, Martinez-Nicolas A, Ordovás JM, Ros Lucas JA, Castell P, et al.. (2012) Differences in circadian rhythmicity in CLOCK 3111T/C genetic variants in moderate obese women as assessed by thermometry, actimetry and body position. Int J Obes (Lond). doi:10.1038/ijo.2012.180. [DOI] [PMC free article] [PubMed]
- 40. Garaulet M, Esteban Tardido A, Lee Y-C, Smith CE, Parnell LD, et al. (2012) SIRT1 and CLOCK 3111T>C combined genotype is associated with evening preference and weight loss resistance in a behavioral therapy treatment for obesity. Int J Obes (Lond) 36: 1436–1441 10.1038/ijo.2011.270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Garaulet M, Corbalán-Tutau MD, Madrid JA, Baraza JC, Parnell LD, et al. (2010) PERIOD2 variants are associated with abdominal obesity, psycho-behavioral factors, and attrition in the dietary treatment of obesity. J Am Diet Assoc 110: 917–921 10.1016/j.jada.2010.03.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Blair AJ, Lewis VJ, Booth DA (1990) Does emotional eating interfere with success in attempts at weight control? Appetite 15: 151–157. [DOI] [PubMed] [Google Scholar]
- 43. Lavery MA, Loewy JW (1993) Identifying predictive variables for long-term weight change after participation in a weight loss program. J Am Diet Assoc 93: 1017–1024. [DOI] [PubMed] [Google Scholar]
- 44. Sherwood NE, Jeffery RW, Wing RR (1999) Binge status as a predictor of weight loss treatment outcome. Int J Obes Relat Metab Disord 23: 485–493. [DOI] [PubMed] [Google Scholar]
- 45. Jansen A, Vanreyten A, van Balveren T, Roefs A, Nederkoorn C, et al. (2008) Negative affect and cue-induced overeating in non-eating disordered obesity. Appetite 51: 556–562 10.1016/j.appet.2008.04.009 [DOI] [PubMed] [Google Scholar]
- 46. Torres SJ, Nowson CA (2007) Relationship between stress, eating behavior, and obesity. Nutrition 23: 887–894 10.1016/j.nut.2007.08.008 [DOI] [PubMed] [Google Scholar]
- 47. Wallis DJ, Hetherington MM (2004) Stress and eating: the effects of ego-threat and cognitive demand on food intake in restrained and emotional eaters. Appetite 43: 39–46 10.1016/j.appet.2004.02.001 [DOI] [PubMed] [Google Scholar]
- 48. Wallis DJ, Hetherington MM (2009) Emotions and eating. Self-reported and experimentally induced changes in food intake under stress. Appetite 52: 355–362 Available: http://www.researchgate.net/publication/23652077_Emotions_and_eating._Self-reported_and_experimentally_induced_changes_in_food_intake_under_stress/file/d912f50f713b7257bc.pdf. [DOI] [PubMed] [Google Scholar]
- 49. Gibson EL (2006) Emotional influences on food choice: sensory, physiological and psychological pathways. Physiol Behav 89: 53–61 10.1016/j.physbeh.2006.01.024 [DOI] [PubMed] [Google Scholar]
- 50. Royal JD, Kurtz JL (2010) I ate what?! The effect of stress and dispositional eating style on food intake and behavioral awareness. Personality and Individual Differences 49: 565–569. [Google Scholar]
- 51. Macht M, Gerer J, Ellgring H (2003) Emotions in overweight and normal-weight women immediately after eating foods differing in energy. Physiol Behav 80: 367–374. [DOI] [PubMed] [Google Scholar]
- 52. Milagro FI, Gómez-Abellán P, Campión J, Martínez JA, Ordovas JM, et al. (2012) CLOCK, PER2 and BMAL1 DNA methylation: association with obesity and metabolic syndrome characteristics and monounsaturated fat intake. Chronobiol Int 29: 1180–1194 10.3109/07420528.2012.719967 [DOI] [PubMed] [Google Scholar]
- 53. Bryant EJ, King NA, Blundell JE (2008) Disinhibition: its effects on appetite and weight regulation. Obes Rev 9: 409–419 10.1111/j.1467-789X.2007.00426.x [DOI] [PubMed] [Google Scholar]
- 54. Leblanc V, Provencher V, Bégin C, Corneau L, Tremblay A, et al. (2012) Impact of a Health-At-Every-Size intervention on changes in dietary intakes and eating patterns in premenopausal overweight women: results of a randomized trial. Clin Nutr 31: 481–488 10.1016/j.clnu.2011.12.013 [DOI] [PubMed] [Google Scholar]
- 55. Corbalán MD, Morales EM, Canteras M, Espallardo A, Hernández T, et al. (2009) Effectiveness of cognitive–behavioral therapy based on the Mediterranean diet for the treatment of obesity. Nutrition 25: 861–869 10.1016/j.nut.2009.02.013 [DOI] [PubMed] [Google Scholar]
- 56.Bandín C, Martinez-Nicolas A, Ordovás JM, Madrid JA, Garaulet M (2013) Circadian rhythmycity as a predictor of weight loss effectiveness. Int J Obes (Lond). doi:10.1038/ijo.2013.211. [DOI] [PubMed]
- 57. Garaulet M, Gómez-Abellán P, Alburquerque-Béjar JJ, Lee Y-C, Ordovás JM, et al. (2013) Timing of food intake predicts weight loss effectiveness. Int J Obes (Lond) 37: 604–611 10.1038/ijo.2012.229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Bacon L, Aphramor L (2011) Weight science: evaluating the evidence for a paradigm shift. Nutr J 10: 9 10.1186/1475-2891-10-9 [DOI] [PMC free article] [PubMed] [Google Scholar]