Abstract
Background
The “terrible triad” of the elbow is a complex injury that can lead to pain, stiffness, and posttraumatic arthritis if not appropriately treated. The primary goal of surgery for these injuries is to restore stability of the joint sufficient to permit early motion. Although most reports recommend repair and/or replacement of all coronoid and radial head fractures when possible, a recent cadaveric study demonstrated that type II coronoid fractures are stable unless the radial head is removed and not replaced.
Questions/purposes
The purposes of this study were to determine the (1) range of motion; (2) clinical scores using the Disabilities of the Arm, Shoulder and Hand (DASH) and the Broberg-Morrey questionnaires; and (3) rate of arthritic changes, heterotopic ossification (HO), or elbow instability postoperatively in patients whose terrible triad injuries of the elbow included Reagan-Morrey type I or II coronoid fractures that were treated without fixation.
Methods
Between April 2008 and December 2010, 14 consecutive patients were treated for acute terrible triad injuries that included two Regan-Morrey type I and 12 Regan-Morrey type II coronoid fractures. Based on the senior author’s (DGS) clinical experience that coronoid fractures classified as such do not require fixation to restore intraoperative stability to the posterolaterally dislocated elbow, all injuries were treated by the senior author with a surgical protocol that included radial head repair or prosthetic replacement and repair of the lateral ulnar collateral ligament (LUCL) followed by intraoperative fluoroscopic examination through a range of 20° to 130° of elbow flexion to confirm concentric reduction of the ulnohumeral joint. Using this protocol, intraoperative stability was confirmed in all cases without any attempt at coronoid or anterior capsular repair. Repair of the medial collateral ligament or application of external fixation was not performed in any case. All patients were available for followup at a minimum of 24 months (mean, 41 months; range, 24–56 months). The mean patient age was 52 years (range, 32–58 years). At the followup all patients were evaluated clinically and radiographically by the senior author. Outcome measures included elbow range of motion, forearm rotation, elbow stability, and radiographic evidence of HO or arthritic changes using the Broberg and Morrey scale. Elbow instability was defined as clinical or radiographic evidence of recurrent ulnohumeral dislocation or subluxation at final followup. Clinical outcomes were assessed with the patient-reported DASH questionnaire and the physician-administered Broberg-Morrey elbow rating system.
Results
The mean arc of ulnohumeral motion at final followup was 123° (range, 75°–140°) and mean forearm rotation was 145° (range, 70°–170°). The mean Broberg and Morrey score was 90 of 100 (range, 70–100, higher scores reflecting better results) and the average DASH score was 14 of 100 (range, 0–38, higher scores reflecting poorer results). Radiographs revealed mild arthritic changes in one patient. One patient developed radiographically apparent but asymptomatic HO. None of the patients demonstrated instability postoperatively.
Conclusions
These findings demonstrate that terrible triad injuries with type I and II coronoid process fractures can be effectively treated without fixation of coronoid fractures when repair or replacement of the radial head fracture and reconstruction of the LUCL complex sufficiently restores intraoperative stability of the elbow through a functional range of motion.
Level of Evidence
Level IV, therapeutic study. See Guidelines to Authors for a complete description of levels of evidence.
Introduction
Elbow dislocation with disruption of the lateral ulnar collateral ligament (LUCL) and fractures of both the radial head and the ulnar coronoid process, termed the “terrible triad” of the elbow, is a complex injury with variable outcomes [8, 16]. The majority of these injuries are treated surgically as a result of the inherent instability they cause [8, 12, 13, 15, 16]. The primary goal of surgical reconstruction of terrible triad injuries is to restore sufficient stability to permit early mobilization of the joint. Most published treatment protocols advocate fixation of all radial head and coronoid process fractures and repair of the LUCL to achieve a stable anatomic reduction of the elbow [7, 12, 13, 16, 17, 20]. Rarely, in cases with residual elbow instability, repair of the medial collateral ligament (MCL) and/or application of hinged or static external fixation is recommended [6, 15, 20].
The ideal treatment of Regan-Morrey [14] type I coronoid fractures (tip of the process) is still debated. Some authors recommend excision of the fragment, although most authors prefer to attempt fracture repair [1, 4, 5, 7, 12, 13, 15, 17]. However, a recent cadaveric study demonstrated that type II coronoid fractures are stable unless the radial head is removed, whereas type III fractures are unstable even with an intact radial head and lateral ligamentous complex [10]. Based on their findings, the authors suggested that type II coronoid fractures with intact ligaments and a functional radial head can be clinically stable [10].
Therefore, the following question arises: When treating terrible triad injuries, do Regan-Morrey type I and II coronoid fractures always need to be fixed? To try to answer this, we measured the (1) ROM; (2) clinical scores using the Disabilities of the Arm, Shoulder and Hand (DASH) and the Broberg-Morrey questionnaires; and (3) we assessed radiographically the development of arthritic changes or heterotopic ossification and late elbow instability in patients whose terrible triad injuries of the elbow included Reagan-Morrey type I or II coronoid fractures that were treated without fixation.
Patients and Methods
Between April 2008 and December 2010, 14 patients with acute terrible triad injuries that included Regan-Morrey type I and type II coronoid process fractures were surgically treated by the senior author (DGS). The coronoid fractures were not repaired in any of these patients, because clinical stability was documented intraoperatively following surgical repair of the LUCL and repair or replacement of the radial head in all cases. We retrospectively reviewed the data of these patients at a minimum followup of 24 months (mean, 41 months; range, 24–56 months) after institutional review board approval. None of the patients were lost in the followup period. There were six men and eight women with a mean age of 52 years (range, 32–58 years). Twelve patients had sustained the injury after falls from a height, and two patients had been injured in motor vehicle accidents. The dominant arm was affected in nine of 14 cases (64%). None of the patients had previous elbow trauma or elbow infection.
All 14 patients sustained a posterolateral elbow dislocation combined with fractures of the ulnar coronoid process and radial head (Fig. 1A–B). The coronoid injuries included one or two fragment transverse fractures of coronoid involving less than 50% of the total height (Reagan- Morrey type I and type II). All patients were treated operatively with a lateral approach to the elbow using the Kaplan interval (extensor carpi radialis brevis and extensor digitorum communis) or, when possible, by exploiting or extending traumatic dissection planes. The mean time from injury to surgery was 3 days (range, 1–5 days). None of the 14 coronoid fractures were repaired. The associated radial head fractures were repaired with open reduction and internal fixation using screws in three patients, of which none had any loss of articular bone. In the remaining 11 patients, radial head replacement was performed using an uncemented unipolar prosthesis (Wright Medical Group, Inc, Arlington, TN, USA) as a result of extensive fracture comminution. The LUCL was completely avulsed from its origin on the lateral epicondyle of the humerus in all 14 patients. These injuries were managed with primary anatomic repair of the LUCL using suture anchors. In the majority of these terrible triad cases, the MCL was also injured. However, the senior author (DGS) believes that MCL repair is only necessary if the elbow remains unstable intraoperatively after repair or replacement of the radial head and repair of the LUCL. Therefore, no MCL repairs were performed in these patients. Similarly, external fixation was not required in any case.
Fig. 1A–B.
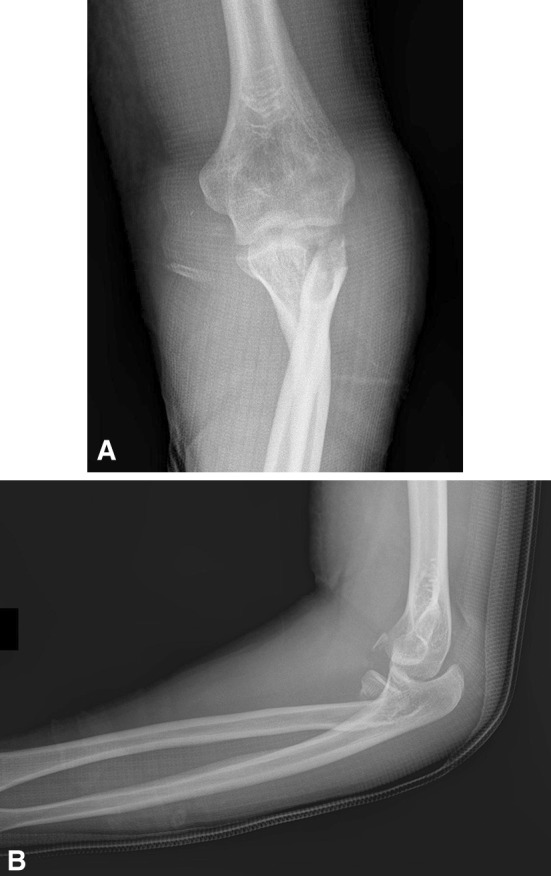
Preoperative AP (A) and lateral (B) left elbow radiographs of a 49-year-old woman after reduction of elbow dislocation, indicating fractures of the radial head and coronoid fracture type II.
Intraoperatively, before definitive closure, the elbow was examined for stability clinically and fluoroscopically. Clinical stability was demonstrated in all patients without coronoid fixation as evidenced by concentric reduction of the ulnohumeral joint through a range of 20° to 130° of flexion-extension. The reduction was confirmed fluoroscopically while the elbow was flexed and extended with the forearm in pronation, supination, and neutral position. No posterior or posterolateral elbow subluxation or dislocation was observed.
The elbow was immobilized in a long-arm posterior splint with 90° of elbow flexion and full forearm pronation for 2 weeks. Active and passive motion with a 40° to 45° extension block splint was initiated at 2 weeks in all patients. Each patient wore a hinged brace and was gradually increased to active ROM over a 3- to 4-week period. Forearm rotation was not held locked in the brace. Strengthening was initiated once sufficient bony and ligamentous healing had occurred.
At followup, each patient was evaluated clinically and radiographically. Elbow arc of motion (extension and flexion) and forearm rotation (pronation and supination) were measured with a goniometer by the senior author (DGS), who performed all surgeries. The DASH was completed by each patient, and the Broberg-Morrey rating system was used to assess elbow function. The DASH [9] score potentially ranges from 0 to 100 points with a higher score indicating a higher level of global upper limb disability. The Broberg-Morrey rating system [2] is a physician-administered, elbow-specific rating system that generates a total score ranging from 0 to 100 points. It consists of four parts: motion (40 points), strength (20 points), stability (5 points), and pain (35 points). A total score of 95 to 100 points indicates excellent outcome; 80 to 94 points, good; 60 to 79 points, fair; and 0 to 59 points, poor.
Elbow instability was assessed by clinical examination at 3 to 4 weeks postoperatively, noting any signs or symptoms of subluxation on maximal combined elbow extension and forearm supination. Stress radiographs were not obtained. Elbow radiographs were reviewed for assessment of joint concentricity, fracture reduction, fracture union, implant position, heterotopic ossification, and evidence of arthrosis. The Broberg and Morrey scale [2] was used to assess the presence of arthritic changes. This system, not to be confused with the Broberg-Morrey clinical elbow score, classifies arthritic changes on elbow radiographs. A radiographically normal elbow is considered Grade 0. Slight joint space narrowing with minimum osteophyte formation indicates Grade 1. Moderate joint space narrowing and moderate osteophyte formation is Grade 2. An elbow with severe degenerative changes and gross destruction of the joint is considered Grade 3.
The clinical data of all patients were analyzed using the statistical software package SPSS Version 17.0 (SPSS Inc, Chicago, IL, USA).
Results
The mean elbow flexion at latest followup was 134° (range, 95°–140°) and the mean flexion contracture was 11° (range, 0°–20°) with a mean arc of ulnohumeral motion of 123° (range, 75°–140°). The mean forearm pronation was 82° (range, 50°–90°) and the mean supination was 64° (range, 20°–80°) with a mean forearm rotation arc of 145° (range, 70°–170°). Thirteen of the 14 patients (93%) had an arc of at least 30° to 130° of flexion-extension, 50° of pronation, and 50° of supination, which constitute a functional range of elbow motion.
None of the patients experienced recurrent dislocation or subluxation or demonstrated instability postoperatively. No infections or other complications were encountered.
The mean Broberg-Morrey score was 90 (range, 70–100) with five excellent results, eight good results, and one fair result. The average DASH score was 14 (range, 0–38).
Radiographic review showed bony union of all radial head fractures treated with open reduction and internal fixation and revealed no radial head implant failures (Fig. 2A–B). One patient developed mild heterotopic ossification, which remained clinically asymptomatic, without limitation of elbow motion. At final followup, one patient had mild arthritic changes of the elbow, which was rated as Grade 1 on the Broberg and Morrey scale.
Fig. 2A–B.
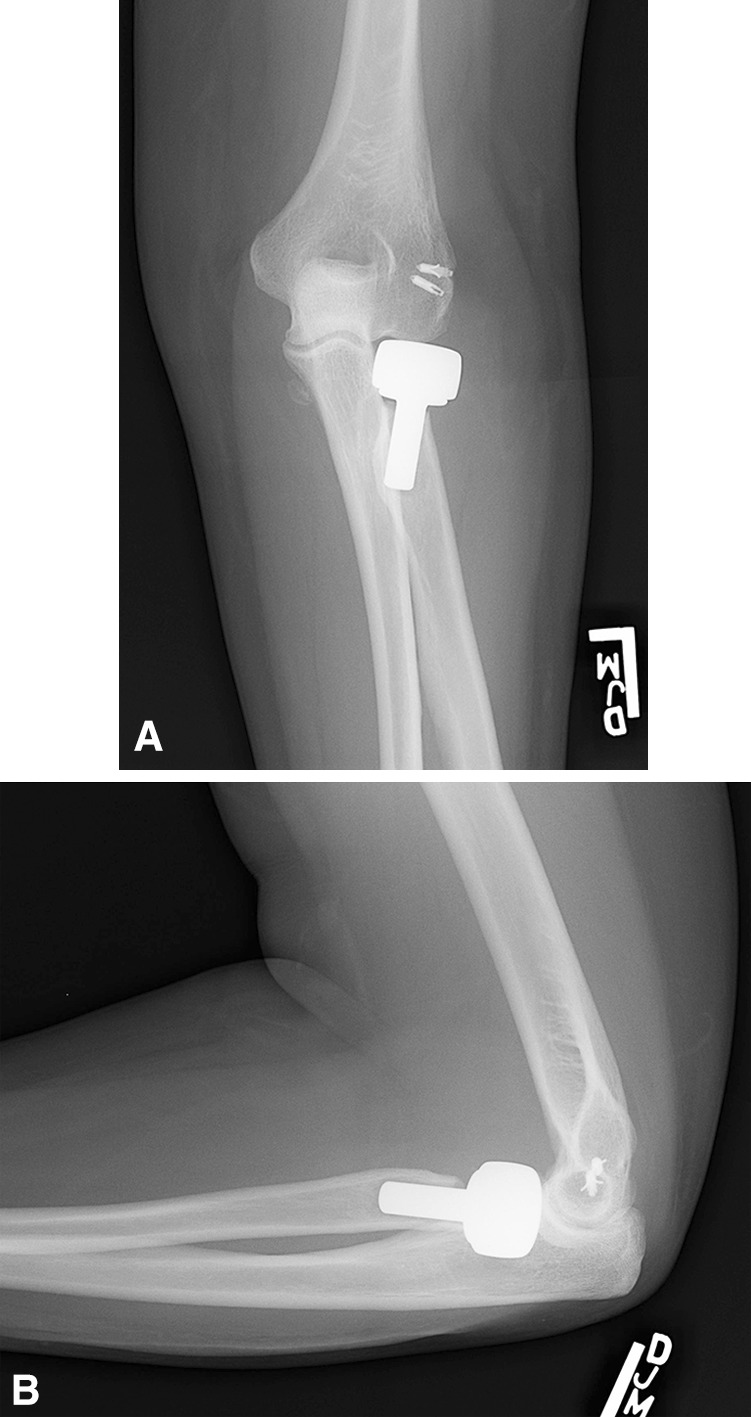
Two-year postoperative AP (A) and lateral (B) left elbow radiographs showing stable concentric reduction of the ulnohumeral joint after replacement of the radial head and repair of the LUCL with two suture anchors without repair of the coronoid fracture.
Meaningful subgroup analysis for comparison of outcomes between patients treated with radial head repair (three patients) and those treated with radial head replacement (11 patients) was not possible as a result of small numbers. At final followup, functional results were comparable between the two groups. The patient who developed mild, asymptomatic heterotopic ossification and the patient who developed mild arthritic changes were both treated with radial head replacement.
Discussion
The goal of reconstruction of terrible triad injuries is to restore sufficient elbow stability to allow early mobilization within a stable elbow arc of motion [8, 12, 13, 15, 16]. The literature supports a consensus that to achieve such stability, the surgeon should fix or replace the radial head and repair the injured LUCL [7, 12, 13, 16, 17, 20]. Similarly, many authors agree that any associated coronoid fracture, regardless of fracture classification, should also be fixed [6, 7, 11, 13]. However, debate still exists regarding best treatment of these fractures, particularly the treatment of small or very comminuted coronoid fragments. Some published information suggests there might be a role for excision or benign neglect [3, 10, 17, 18], including a recent cadaver study that suggests that in some situations, stability can be maintained without surgical fixation of the coronoid [1]. One must exercise caution when attempting to apply the results of biomechanical studies to the clinical setting, because the complexity and intricacy of injury, coupled in vivo motion, and the stresses across the human elbow, particularly a posttraumatic elbow, in a live subject cannot be completely replicated in the laboratory setting. We therefore sought to evaluate ROM and clinical outcomes scores in patients with terrible triad injuries and associated Regan-Morrey type I and II coronoid fractures undergoing surgical treatment of an elbow fracture that did not include coronoid fixation.
This study had a number of limitations. First, this cohort had no comparison group and included a relatively small number of patients. The absence of a control group precludes making definitive therapeutic recommendations, and the small size of the series would make it less likely we would detect uncommon complications of treatment. Furthermore, as elaborated on in the text subsequently, direct comparison with other terrible triad treatment studies that included coronoid fixation may be difficult to interpret as a result of the small and retrospective nature of such studies.
In this small group treated without coronoid fixation, elbow ROM and forearm rotation generally were restored to within a functional arc. Mean ranges for flexion-extension arc, mean flexion contracture, and forearm rotation compare favorably with the results of similar clinical series of terrible triad injuries treated with surgical protocols that involved coronoid and/or anterior capsular fixation (Table 1). Details of the comparative studies are summarized (Table 2).
Table 1.
Comparison with available literature
| Study | Number of terrible triad injuries | Mean age (years) | Mean followup (months) | Mean arc flexion-extension | Mean flexion contracture | Mean maximum flexion | Mean forearm rotation | Recurrent instability/2° surgical intervention | Broberg-Morrey score | DASH score | HO | Mild arthritis | Moderate arthritis | Severe arthritis |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pugh et al. [13] | 36 | 41.4 | 34 (20–65) | 112° ± 11° | 19° ± 9° | 131° | 136° ± 16° | 6%/22% | N/A | N/A | 3 | 8 | 5 | 1 |
| Garrigues et al. [7] | 40 | 48 | 24 (18–53) | 115° (75°–140°) | 21° | 136° | N/A | 8%/28% | 90 (64–100) | 16 | 5 | 8 | 3 | – |
| Forthman et al. [6] | 22 | 48 | 29 (12–46) | 117° (75°–145°) | 17° (0°–45°) | 134° | 137° (0°–180°) | 5%/27% (instability in 1 noncompliant patient) | 88 (53–100) | N/A | 3 | 6 | 1 | – |
| Lindenhovius et al. [11] acute treatment group | 18 | 47 | 29 | 119° (75°–145°) | 17° (0°–45°) | 135° | 141° (70°–180°) | 0%/28% | 90 (64–100) | 15 | 2 | 9 | 3 | – |
| Current study | 14 | 52 | 41 (24–56) | 123° (75°–140°) | 11° (0°–20°) | 134° | 146° (70°–170°) | 0%/0% | 90 (70–100) | 14 | 1 | 1 | – | – |
Values are mean ± SD or mean with range in parentheses; DASH = Disabilities of the Arm, Shoulder and Hand; HO = heterotopic ossification; N/A = not available.
Table 2.
Details of comparative studies
| Study | Number of terrible triad injuries | Coronoid classification | Coronoid fixation | Radial head | LUCL | MCL Repair | External fixation | Average time between injury and surgery (days) | Approach | Comments |
|---|---|---|---|---|---|---|---|---|---|---|
| Pugh et al. [13] | 36 | Type I: 10, type II: 18, type III: 8 |
18: type II and III: ORIF with screws, 18: type I or comminuted II and III: anterior capsule repair with suture technique |
3: débrided small marginal fragments, 13: ORIF, 20: prosthetic replacement |
Repair in all 36 | 6 | 3 hinged | 4.5 | Posterior midline: 8, lateral only: 26, lateral + medial: 2 |
– |
| Forthman et al. [6] | 22 | Type I: 0, type II: 22, type III: 0 |
18: suture repair through capusle and bone tunnels, 3: suture + screws, 1: plate and screws |
1: ORIF, 21: prosthetic replacement |
Repair in all 22 | 0 | 0 | 7 | All posterior midline | Specifically excluded 4 patients with coronoid fragments too small to repair |
| Lindenhovius et al. [11] acute treatment | 18 | Type I: 0, type II: 18, type III: 0 |
16: suture repair through capusle and bone tunnels, 2: suture + screws |
1: ORIF, 2: prosthetic replacement |
Repair in all 18 | 0 | 0 | 6 | All posterior midline | This cohort includes patients also included in the Forthman et al. study; 4 patients had additional ipsilateral arm injuries |
| Garrigues et al. [7] | 40 | Type I: 2, type II: 36, type III: 2 |
28: suture lasso, 7: suture anchors, 5: lag screws |
9: ORIF, 30: prosthetic replacement, 1: not reported |
Repair in all 40 | 2 | 3 hinged | Not reported | Posterior midline or lateral in all; 3 with additional medial incision | Authors recommend coronoid lasso fixation regardless of fracture type |
| Current study | 14 | Type I: 2, type II: 12, type III: 0 |
None | 3: ORIF, 11: prosthetic replacement |
Repair in all 14 | 0 | 0 | 3 | All lateral only | – |
LUCL = lateral ulnar collateral ligament; MCL = medial collateral ligament; ORIF = open reduction and internal fixation.
Pugh et al. [13] reported a mean arc of elbow motion of 112°, mean flexion contracture of 19°, and mean forearm rotation of 136° in 36 terrible triad injuries surgically managed with a protocol including attempted repair of all associated coronoid fractures. Garrigues et al. [7] reported a mean flexion-extension elbow arc of 115° with mean flexion contracture of 21° in 40 patients with terrible triad injuries treated with coronoid fracture fixation. Both of these studies included patients with type III coronoid fractures, and each series included three elbows that required hinged external fixators to be placed to achieve intraoperative stability. This could suggest that these series may have, on average, dealt with higher energy injuries prone to less favorable ROM outcomes. Furthermore, these studies all exercised protocols that attempted coronoid or anterior capsular fixation regardless of coronoid fracture classification, including capsular repair in the setting of small or comminuted coronoid fragments. This may explain why the current study, which treated similar injuries without any anterior fixation, resulted in a lower mean flexion contracture. The clinical significance of such improvement in the setting of a functional arc of elbow motion is unknown.
A study by Forthman et al. [6] examined 22 terrible triad injuries with type II coronoid fractures. After fixation or replacement of all radial head fractures, repair of the LUCL, and fixation of all coronoid fractures, they noted mean arc of ulnohumeral motion of 117°, mean flexion contracture of 17°, and mean arc of forearm rotation of 137°. Lindenhovius et al. [11] compared the acute treatment of 18 versus the subacute treatment (3 or more weeks after injury) of 14 terrible triad injuries. The acute treatment group most closely parallels the treatment protocol in the current study. All coronoid fractures in this group were classified as type II, and all were repaired. The mean flexion arc was 119°, mean flexion contracture was 17°, and the mean forearm rotation was 141° at final followup. Of note, the cohort studied by Forthman et al. [6] includes, at least partially, the same subjects studied by Lindenhovius et al. [11]. Therefore, any characteristics such as patient demographics or severity of injury unique to these cohorts relative to the current study may skew interpretation of the outcome data to overestimate the current cohort’s departure from prior published trends. Four patients in the Lindenhovius et al. study [11] had ipsilateral upper extremity injuries, including three fractures and one case of carpal tunnel syndrome. Although not specifically stated, some of these patients may be included in the Forthman et al. [6] cohort. Perhaps this further hints at a higher energy level of injury to the elbows of these patients, setting the stage for poorer ROM outcomes relative to the current study. The concomitant injuries themselves and/or their treatment and sequelae may also influence the outcome measures independent of severity of the terrible triad injuries.
The reason for a higher mean arc of forearm rotation in the current cohort similarly remains unclear but may be a consequence of one or several attributes of the cohort itself such as smaller potential for scarring secondary to lower energy elbow injuries, less concomitant upper extremity injuries, and higher mean age or may be a consequence of the treatment protocol itself.
One potential downside of a protocol that addresses radial head fixation or replacement and LUCL repair before addressing the coronoid is that should the elbow remain unstable intraoperatively prompting the surgeon to pursue coronoid repair, access to the coronoid provided by the lateral tissue disruption and radial head fracture is lost, necessitating a medial approach. The consequence on outcomes in terrible triad injuries for dual medial and lateral incisions versus a posterior midline “global” incision or lateral only approach is unknown. The current study used a lateral incision only in all cases, whereas each of the comparative studies that involved coronoid repair used a posterior midline approach exclusively or a mixture of approaches that included a posterior midline in some cases. Although maximum terminal flexion figures reported by each study were quite similar, the current study reported better arc of flexion and extension and smaller flexion contractures on average (Table 1). The influence of surgical approach to these outcomes as opposed to that of other factors such as anterior capsular repair versus none is unknown but suggests that a posterior midline approach does not necessarily limit elbow flexion and that some other factor that contributes to increased flexion contracture in the coronoid fixation cohorts is responsible for poorer arc of motion in those groups.
Clinical outcomes using the DASH and Broberg-Morrey scores were good to excellent in 13 of 14 patients (93%) in this cohort. Like with the ROM outcomes, these scores were comparable but favorable to those of previous studies in which the coronoid fractures were repaired (Table 1). Forthman et al. [6] reported a mean Broberg-Morrey score of 88 with 17 of 22 patients (77%) rated good to excellent. Lindenhovius et al. [11] reported mean Broberg-Morrey score for their acute treatment group of 90 with 15 of 18 (83%) good or excellent. Garrigues et al. [7] reported a mean Broberg-Morrey score of 90 without elaborating on the number of good or excellent scores. The mean DASH score in the current study is 14, which is comparable to mean scores of 15 and 16 reported by Lindenhovius et al. [11] and Garrigues et al. [7], respectively. The minimum clinically important difference (MCID) for the Broberg-Morrey rating system is not available, and the MCID for the DASH questionnaire is 10 points [19]. These results suggest that on average, terrible triad patients in this cohort with unrepaired type I and II coronoid fractures, have better elbow-specific functional scores, but rate their global upper extremity function similarly to patients managed with coronoid or anterior capsule repair. The reason for superior elbow-specific function scores in the current cohort is unknown. For similar reasons as previously described for the ROM outcomes, it may be that this cohort represents a series of patients with lower energy injuries more prone to favorable outcomes regardless of treatment protocols. It may be, however, that when surgical stability is otherwise restored without coronoid or anterior capsular fixation, patients experience improved outcomes as some consequence of the treatment protocol itself and the internal milieu of the elbow created by not surgically manipulating the coronoid or anterior capsular tissues.
Arthrosis and clinically important heterotopic ossification were not observed in this small group, unlike the cohorts that included repair of the coronoid [6, 7, 11, 13] (Table 1). Pugh et al. [13] reported elbow arthrosis in 14 patients (39%) and heterotopic ossification in three patients (8%). Garrigues et al. [7] observed arthritic changes of the elbow in 11 patients (28%) and heterotopic ossification in five (13%). Forthman et al. [6] noted radiographic signs of arthrosis in seven patients (32%) and heterotopic ossification in three (14%). Lindenhovius et al. [11] documented elbow arthrosis in 12 patients (67%) and heterotopic ossification in two patients (11%) in their acute treatment group. Like with the ROM and clinical scores outcomes, one can speculate that superior rates of arthrosis and heterotopic ossification are reflective of an overall lower severity of injury in the current cohort, a notion further supported by the fact that no patients in this cohort required MCL repair or external fixation to achieve intraoperative stability. On the other hand, perhaps the omission of coronoid or capsular repair and the ulnar drilling required to achieve such fixation portends superior results in these injuries by minimizing heterotopic ossification formation or somehow decreasing the chance of arthrosis. The current cohort had a slightly higher mean age by an average of 6 years relative to the other cohorts (Table 1). Although the current cohort is in the preretirement age range, higher age could conceivably be related to lower potential for scar formation, lower level of energy required to cause elbow dislocation, or lower functional demands postoperatively, all of which could influence outcomes after terrible triad injuries. Although our mean followup time of 41 months (range, 24–56 months) was longer than that of the comparative studies by an average of 12 months, late development of elbow arthrosis may yet occur. Lastly, the mean time from injury to surgery was 3 days shorter on average for the current study, which may have some effect on outcome including posttraumatic arthrosis, heterotopic ossification, and/or ROM, although a causal relationship or effect magnitude cannot be inferred from this study (Table 2).
Late instability was not observed in this small group. No patients required subsequent reoperation as of the drafting of this manuscript. Pugh et al. [13] documented a rate of recurrent instability of 6% and their overall reoperation rate was 22% despite methods that included repair of the MCL and application of an external frame in some cases. Forthman et al. [6] noted elbow instability in one noncompliant patient. Garrigues et al. [7] observed no instability in patients with suture lasso fixation of the coronoid fracture, 29% instability in patients with coronoid suture anchor fixation, and 20% instability in patients with coronoid screw fixation. Lindenhovius et al. [11] restored elbow stability in all patients managed acutely.
Although recurrent instability rates were low (5%–8%) for all comparative studies, the reoperation rate was 22% to 28% in those series (Table 1). Indications for secondary procedures in the comparative studies included ulnar nerve dysfunction, elbow contracture, heterotopic ossification, and a few instances of late instability or reinjury [6, 7, 11, 13]. The reason for this large discrepancy in rates of secondary operations is unclear but is certainly influenced by the lower rates of late instability, clinically significant heterotopic ossification, and elbow stiffness in this cohort. The current study did not document any cases of significant ulnar nerve dysfunction in the postoperative period. This may be related to the surgical approach, which was lateral in all cases, or may be indirectly related to higher postoperative ROM and lower heterotopic ossification and arthrosis rates in this study. In addition, the current study’s authors may have a higher threshold for reoperation for ulnar nerve dysfunction.
The best surgical protocol to treat terrible triad injuries of the elbow remains unclear, but a general consensus exists that the primary goal of surgery is to reestablish sufficient stability of the joint to permit early mobilization. The results of this study suggest that terrible triad injuries can be successfully managed without fixation of Regan-Morrey type I and II coronoid fractures if the radial head and LUCL are addressed. In conjunction with previous biomechanical findings [10], our clinical results challenge the accepted belief that the coronoid must be fixed in all terrible triad injuries. As such, these results support the notion that if coronoid or anterior capsular repair is not required for restoration of elbow stability in select cases, avoidance of unnecessary surgical fixation in these instances may positively affect functional outcomes.
Footnotes
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Beingessner DM, Stacpoole RA, Dunning CE, Johnson JA, King GJ. The effect of suture fixation of type I coronoid fractures on the kinematics and stability of the elbow with and without medial collateral ligament repair. J Shoulder Elbow Surg. 2007;16:213–217. doi: 10.1016/j.jse.2006.06.015. [DOI] [PubMed] [Google Scholar]
- 2.Broberg MA, Morrey BF. Results of delayed excision of the radial head after fracture. J Bone Joint Surg Am. 1986;68:669–674. [PubMed] [Google Scholar]
- 3.Closkey RF, Goode JR, Kirschenbaum D, Cody RP. The role of the coronoid process in elbow stability. A biomechanical analysis of axial loading. J Bone Joint Surg Am. 2000;82:1749–1753. doi: 10.2106/00004623-200012000-00009. [DOI] [PubMed] [Google Scholar]
- 4.Cohen MS. Fractures of the coronoid process. Hand Clin. 2004;20:443–453. doi: 10.1016/j.hcl.2004.07.004. [DOI] [PubMed] [Google Scholar]
- 5.Egol KA, Immerman I, Paksima N, Tejwani N, Koval KJ. Fracture-dislocation of the elbow functional outcome following treatment with a standardized protocol. Bull NYU Hosp Jt Dis. 2007;65:263–270. [PubMed] [Google Scholar]
- 6.Forthman C, Henket M, Ring DC. Elbow dislocation with intra-articular fracture: the results of operative treatment without repair of the medial collateral ligament. J Hand Surg Am. 2007;32:1200–1209. doi: 10.1016/j.jhsa.2007.06.019. [DOI] [PubMed] [Google Scholar]
- 7.Garrigues GE, Wray WH, 3rd, Lindenhovius AL, Ring DC, Ruch DS. Fixation of the coronoid process in elbow fracture-dislocations. J Bone Joint Surg Am. 2011;93:1873–1881. doi: 10.2106/JBJS.I.01673. [DOI] [PubMed] [Google Scholar]
- 8.Hotchkiss RN. Fractures and dislocations of the elbow. In: Rockwood CA Jr, Green DP, Bucholz RW, Heckman JD, editors. Rockwood and Green’s Fractures in Adults. 4. Philadelphia, PA, USA: Lippincott-Raven; 1996. pp. 929–1024. [Google Scholar]
- 9.Hudak PL, Amadio PC, Bombardier C. Development of an upper extremity outcome measure: the DASH (Disabilities of the Arm, Shoulder and Hand) [corrected]. The Upper Extremity Collaborative Group (UECG) Am J Ind Med. 1996;29:602–608. doi: 10.1002/(SICI)1097-0274(199606)29:6<602::AID-AJIM4>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 10.Jeon IH, Sanchez-Sotelo J, Zhao K, An KN, Morrey BM. The contribution of the coronoid and radial head to the stability of the elbow. J Bone Joint Surg Br. 2012;94:86–92. doi: 10.1302/0301-620X.94B1.26530. [DOI] [PubMed] [Google Scholar]
- 11.Lindenhovius AL, Jupiter JB, Ring D. Comparison of acute versus subacute treatment of terrible triad injuries of the elbow. J Hand Surg Am. 2008;33:920–926. doi: 10.1016/j.jhsa.2008.02.007. [DOI] [PubMed] [Google Scholar]
- 12.Mathew PK, Athwal GS, King GJ. Terrible triad injury of the elbow: current concepts. J Am Acad Orthop Surg. 2009;17:137–151. doi: 10.5435/00124635-200903000-00003. [DOI] [PubMed] [Google Scholar]
- 13.Pugh DM, Wild LM, Schemitsch EH, King GJ, McKee MD. Standard surgical protocol to treat elbow dislocations with radial head and coronoid fractures. J Bone Joint Surg Am. 2004;86:1122–1130. doi: 10.2106/00004623-200406000-00002. [DOI] [PubMed] [Google Scholar]
- 14.Regan W, Morrey B. Fractures of the coronoid process of the ulna. J Bone Joint Surg Am. 1989;71:1348–1354. [PubMed] [Google Scholar]
- 15.Ring D, Hannouche D, Jupiter JB. Surgical treatment of persistent dislocation or subluxation of the ulnohumeral joint after fracture-dislocation of the elbow. J Hand Surg Am. 2004;29:470–480. doi: 10.1016/j.jhsa.2004.01.005. [DOI] [PubMed] [Google Scholar]
- 16.Ring D, Jupiter JB, Zilberfarb J. Posterior dislocation of the elbow with fractures of the radial head and coronoid. J Bone Joint Surg Am. 2002;84:547–551. doi: 10.2106/00004623-200204000-00006. [DOI] [PubMed] [Google Scholar]
- 17.Schneeberger AG, Sadowski MM, Jacob HA. Coronoid process and radial head as posterolateral rotatory stabilizers of the elbow. J Bone Joint Surg Am. 2004;86:975–982. doi: 10.2106/00004623-200405000-00013. [DOI] [PubMed] [Google Scholar]
- 18.Steinmann SP. Coronoid process fracture. J Am Acad Orthop Surg. 2008;16:519–529. [PubMed] [Google Scholar]
- 19.Wright RW, Baumgarten KM. Shoulder outcomes measures. J Am Acad Orthop Surg. 2010;18:436–444. doi: 10.5435/00124635-201007000-00006. [DOI] [PubMed] [Google Scholar]
- 20.Zeiders GJ, Patel MK. Management of unstable elbows following complex fracture-dislocations—the ‘terrible triad’ injury. J Bone Joint Surg Am. 2008;90(Suppl 4):75–84. doi: 10.2106/JBJS.H.00893. [DOI] [PubMed] [Google Scholar]


