Abstract
Background
Metal-on-metal hip resurfacing was developed for younger, active patients as an alternative to THA, but it remains controversial. Study heterogeneity, inconsistent outcome definitions, and unstandardized outcome measures challenge our ability to compare arthroplasty outcomes studies.
Questions/purposes
We asked how early revisions or reoperations (within 5 years of surgery) and overall revisions, adverse events, and postoperative component malalignment compare among studies of metal-on-metal hip resurfacing with THA among patients with hip osteoarthritis. Secondarily, we compared the revision frequency identified in the systematic review with revisions reported in four major joint replacement registries.
Methods
We conducted a systematic review of English language studies published after 1996. Adverse events of interest included rates of early failure, time to revision, revision, reoperation, dislocation, infection/sepsis, femoral neck fracture, mortality, and postoperative component alignment. Revision rates were compared with those from four national joint replacement registries. Results were reported as adverse event rates per 1000 person-years stratified by device market status (in use and discontinued). Comparisons between event rates of metal-on-metal hip resurfacing and THA are made using a quasilikelihood generalized linear model. We identified 7421 abstracts, screened and reviewed 384 full-text articles, and included 236. The most common study designs were prospective cohort studies (46.6%; n = 110) and retrospective studies (36%; n = 85). Few randomized controlled trials were included (7.2%; n = 17).
Results
The average time to revision was 3.0 years for metal-on-metal hip resurfacing (95% CI, 2.95–3.1) versus 7.8 for THA (95% CI, 7.2–8.3). For all devices, revisions and reoperations were more frequent with metal-on-metal hip resurfacing than THA based on point estimates and CIs: 10.7 (95% CI, 10.1–11.3) versus 7.1 (95% CI, 6.7–7.6; p = 0.068), and 7.9 (95% CI, 5.4–11.3) versus 1.8 (95% CI, 1.3–2.2; p = 0.084) per 1000 person-years, respectively. This difference was consistent with three of four national joint replacement registries, but overall national joint replacement registries revision rates were lower than those reported in the literature. Dislocations were more frequent with THA than metal-on-metal hip resurfacing: 4.4 (95% CI, 4.2–4.6) versus 0.9 (95% CI, 0.6–1.2; p = 0.008) per 1000 person-years, respectively. Adverse event rates change when discontinued devices were included.
Conclusions
Revisions and reoperations are more frequent and occur earlier with metal-on-metal hip resurfacing, except when discontinued devices are removed from the analyses. Results from the literature may be misleading without consistent definitions, standardized outcome metrics, and accounting for device market status. This is important when clinicians are assessing and communicating patient risk and when selecting which device is most appropriate for individual patients.
Electronic supplementary material
The online version of this article (doi:10.1007/s11999-014-3556-3) contains supplementary material, which is available to authorized users.
Introduction
Metal-on-metal hip resurfacing is an alternative surgical approach to THA, which generally is used for younger and more active patients [95, 143]. Unlike with a THA, the head of the femur is not completely removed in metal-on-metal hip resurfacing but is reshaped to accept a new metal head that fits a metal acetabular component (also referred to as metal-on-metal [MoM] implants). Still considered in the early stages of dissemination, with a limited number of metal-on-metal hip resurfacing studies now reaching 5 years of followup, emerging papers in the literature are a source of critically needed information to determine the degree and severity of adverse events.
Study heterogeneity, inconsistent outcome definitions, and unstandardized outcome measures challenge our ability to compare arthroplasty outcomes studies [124, 136, 143]. To date, there is limited evidence in the literature that compares adverse events across studies using a standardized metric. Without standardized metrics, it is not possible to make valid comparisons that account for differences in study sample sizes and followup times, which can have a substantial effect on the results. Therefore, it is critical to use a standardized metric such as person-years; however, to date this is not common practice in the arthroplasty literature. Additionally, it has not been common practice to analyze outcomes of medical devices according to market status. Our underlying assumption was that market status is a critical factor in assessing safety issues given that currently in-use metal-on-metal hip resurfacing and THA devices likely have greater efficacy and fewer adverse events. As a result, we organized our data analysis based on device market status.
The primary purpose of our systematic review was to compare studies of metal-on-metal hip resurfacing with THA among patients with hip osteoarthritis to determine rates of: (1) early revision or reoperation (within 5 years of surgery) and overall revisions; (2) revisions reported in four major joint replacement registries; (3) adverse events; and (4) postoperative component malalignment. In this review, we used the standardized metric, per 1000 person-years, to address gaps not previously addressed in the literature to compare outcomes between THA studies that had longer-term followups with metal-on-metal hip resurfacing studies with limited followup.
Materials and Methods
Search Strategy and Criteria
Our review protocol was based on well-established guidelines developed by the Centre for Reviews and Dissemination [24]. The following electronic databases were searched: MEDLINE, PubMed, EMBASE, the Cochrane Library, BIOSIS Previews, and Web of Science from 1997 to 2011.
Using the PICO (patient problem or population [P], intervention [I)], comparison [C)], outcome(s) [O)]) framework to define our exclusion and inclusion criteria [116], we defined our population as adult patients (≥ 18 years) with primary osteoarthritis of the hip. Where study population included patients with hip and knee osteoarthritis, the study was included only if results were subdivided into hip and knee groups. The intervention was primary metal-on-metal hip resurfacing prosthesis and the comparator THA. Type of prosthesis used (ie, material components and prosthesis type) was recorded for comparative analysis. Study outcomes reported included adverse events, safety issues, or revision rates (Appendix 1. Supplemental material is available with the online version of CORR®).
Studies were excluded if they were: not English language; studies with fewer than 10 participants or populations younger than 17 years; hemiarthroplasty; preoperative or postoperative interventions for joint arthroplasty (eg, physiotherapy, rehabilitation, drug trials); management of osteoarthritis or related symptoms; variations on specific surgical techniques/procedures in THA or metal-on-metal hip resurfacing; focused on prosthesis modifications (except where studies looked at cement versus cementless prosthesis); or in vitro/in situ studies.
Primary outcomes were adverse events including revisions, reoperations, infections/sepsis, femoral neck fractures, other femoral fractures, dislocations, and mortality (all-cause, within 30 days of surgery). Revision is commonly defined as surgery where the patient underwent a subsequent surgery on their primary prosthesis where the component was replaced. Reoperations are commonly defined as a subsequent surgery on the primary prosthesis but the component was not replaced. These definitions are not standardized and sometimes the terms revision and reoperation are used interchangeably. We report definitions of adverse events as they were presented in the original studies. Rates of early failure outcomes included revisions/reoperations within 5 years after primary THA or metal-on-metal hip resurfacing. Postoperative component alignment data, for acetabular and stem device components, were extracted and included varus alignment, valgus alignment, and mean neck- and stem-shaft angles. Postoperative component alignment was important to include since clinical evidence of poor alignment as a predictor of device failure has been highlighted in the literature [33].
Initial searches revealed few relevant randomized controlled trials. Consequently, we included all quasiexperimental and observational study designs.
Data Extraction
Abstracts were screened by two independent reviewers (DAA, MCM), and each full-text article was screened by one of three reviewers (SH, DAA, MCM). Data were extracted by two independent reviewers (DAA, MCM) and extracted values were compared to identify discrepancies. Data were extracted as reported in the study. Data were quality-checked to reconcile any known discrepancies to the final approved digital data template.
Prosthesis device types were extracted from each article and sorted by market status: those currently in use and those discontinued. The term “in use” referred to metal-on-metal hip resurfacing and THA devices that were available for surgical use in North America when this research was conducted. Conversely, “discontinued” referred to devices not available for surgical use.
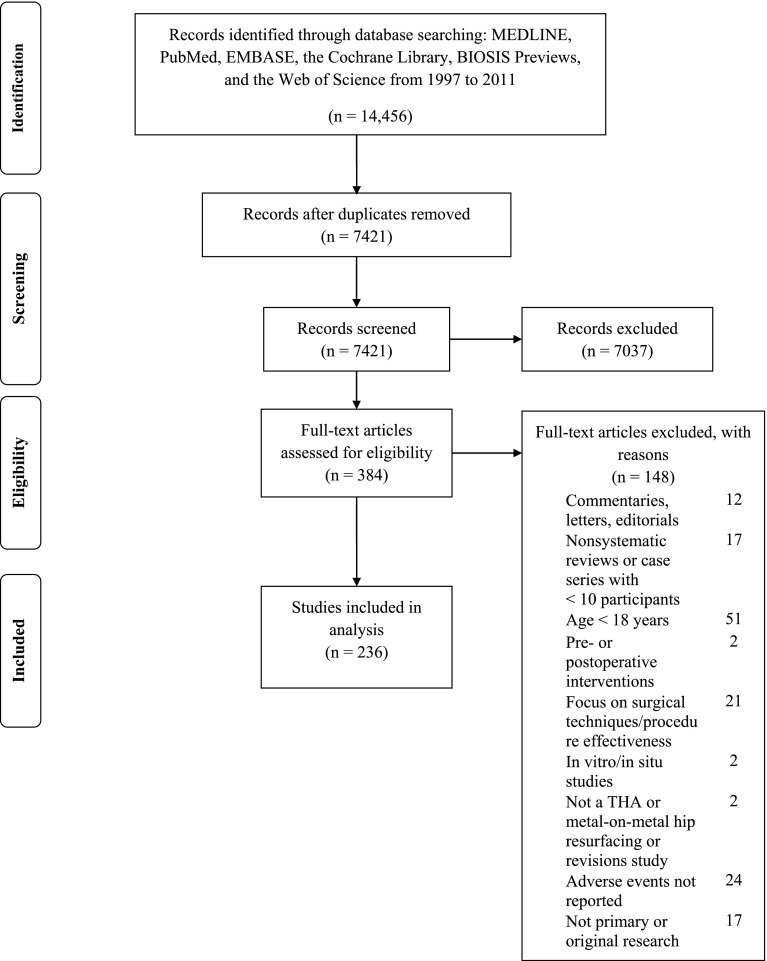
We identified 7421 abstracts, screened, and reviewed 384 full-text articles and included 236 (Fig. 1). Primary reasons for exclusion were: patients younger than 18 years, focus on surgical techniques, or adverse events not reported. None of the articles reviewed reported their findings using a standardized metric (per 1000 person-years). The most common study designs (Table 1) were prospective cohort studies at 46.6% (n = 110) followed by retrospective studies at 36% (n = 85).
Fig. 1.
The flow of articles through the systematic review process using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) [93] is shown.
Table 1.
Distribution of study designs for articles included in systematic review
| Study design | Number of full-text articles | |
|---|---|---|
| Number | Percent | |
| Randomized control trial | 17 | 7.2 |
| Case control | 14 | 5.9 |
| Prospective cohort* | 110 | 46.6 |
| Retrospective cohort† | 85 | 36 |
| Prospective observational (multigroup)‡ | 4 | 1.7 |
| Retrospective observational (multigroup)‡ | 4 | 1.7 |
| Case series (with more than 10 participants) | 2 | 0.8 |
| Total | 236 | 100 |
* Nonrandomized, observational study that follows a group of participants through time to determine the association between a specific exposure and/or intervention (treatment, implanted device, etc) and an outcome, only single intervention-group studies fall in this category.
†Nonrandomized, observational study that uses historical data for a group of participants to determine the association between a specific exposure and/or intervention (treatment, implanted device, etc) and an outcome, only single intervention-group studies fall in this category.
‡Study designs are similar to the prospective and retrospective cohort but include more than one group of participants.
We used the most recent registry reports available to extract revision data from four major joint replacement registries as a comparison for revision findings: the Australian Orthopaedic Association National Joint Replacement Registry, New Zealand National Joint Register, Swedish Hip Arthroplasty Register, and National Joint Registry for England and Wales [9, 47, 98, 102]. These registries were selected because of the homogeneity of available data (revision rates and followups) compared with other registries.
Data Analysis Methods
The observed counts of adverse events are assumed to have a Poisson distribution with a rate parameter for each study and/or adverse event given in units of events per 1000 person-years. Estimates and 95% CI for each rate parameter are made using the relationship between the chi-square and Poisson distributions as per Ulm [135]. Comparisons between adverse event rates for metal-on-metal hip resurfacing and THA are made using a quasilikelihood generalized linear model with log link [64], with p values less than 0.05 considered statistically significant. The quasilikelihood generalized linear model accounts for the significant overdispersion of the data; the data are observed to be overdispersed in that the mean and variance of event counts for each adverse event are not near equal. Thus, we use the quasilikelihood model p values to determine statistical significance of comparisons, as this method accounts for the overdispersion of the data. We also included 95% CIs for reference.
Results
Rates of Early Revisions/Reoperations (within 5 years of surgery) and Average Time to Revision
For all devices, revisions occurred earlier in patients treated with metal-on-metal hip resurfacing devices (3.0 years; 95% CI, 2.95–3.1) compared with THA (7.8 years; 95% CI, 7.2–8.3; p < 0.001) (Table 2). When discontinued devices were removed from the analysis, revisions still occurred earlier in metal-on-metal hip resurfacing devices (Table 2).
Table 2.
Summary of findings comparing market status groups
| Adverse events | All devices (in-use and discontinued) | Currently in-use devices | ||||
|---|---|---|---|---|---|---|
| THA (95% CI) | Metal-on-metal hip resurfacing (95% CI) | p value (THA vs metal-on-metal hip resurfacing) | THA (95% CI) | Metal-on-metal hip resurfacing (95% CI) | p value (THA vs metal-on-metal hip resurfacing) | |
| The average time to revision (years) | 7.8 (7.2–8.3) | 3.0 (2.95–3.1) | <0.001 | 5.7 (5.0–6.6) | 2.9 (2.8–3.0) | < 0.001 |
| Number | 10 | 9 | 2 | 7 | ||
| Early revisions/reoperation within 5 years of surgery (per 1000 person-years) | 3.1 (2.3–4.2) | 14.5 (12.7–16.5) | 0.003 | 3.9 (2.4–6.1) | 10.0 (8.3–11.9) | 0.121 |
| Number | 21 | 19 | 8 | 12 | ||
| Revisions (per 1000 person-years) | 7.1 (6.7–7.6) | 10.7 (10.1–11.3) | 0.068 | 7.6 (6.5–8.8) | 5.7 (5.2–6.2) | 0.268 |
| Number | 85 | 52 | 24 | 36 | ||
| Reoperations (per 1000 person-years) | 1.8 (1.3–2.2) | 7.9 (5.4–11.3) | 0.084 | 4.7 (2.2–8.9) | 8.1 (5.5–11.4) | 0.455 |
| Number | 15 | 8 | 3 | 7 | ||
| Dislocations (per 1000 person-years) | 4.4 (4.2–4.6) | 0.9 (0.6–1.2) | 0.008 | 4.8 (3.5–6.5) | 1.1 (0.8–1.6) | 0.010 |
| Number | 55 | 28 | 12 | 22 | ||
| Infections/sepsis (per 1000 person-years) | 2.1 (2.0–2.3) | 1.4 (1.1–1.8) | 0.160 | 3.2 (2.0–4.8) | 1.2 (0.8–1.8) | 0.180 |
| Number | 43 | 30 | 10 | 22 | ||
| Femoral neck fractures (per 1000 person-years) | 2.9 (1.6–4.8) | 2.0 (1.6–2.6) | 0.654 | 1.7 (0.04–9.7) | 2.4 (1.6–3.4) | 0.912 |
| Number | 7 | 22 | 2 | 15 | ||
Early revisions/reoperations (within 5 years of surgery) were more frequent for metal-on-metal hip resurfacing (14.5 per 1000 person-years; 95% CI, 12.7–16.5) compared with THA (3.1 per 1000 person-years; 95% CI, 2.3–4.2; p = 0.003) for all devices (Table 2). When discontinued devices were removed from the analysis, early revisions/reoperations were still more frequent for metal-on-metal hip resurfacing compared with THA, with nonoverlapping CIs, but a nonsignificant p value (Table 2).
Revisions
The average number of revisions per 1000 person-years was greater for all metal-on-metal hip resurfacing devices (10.7; 95% CI, 10.1–11.3) than for THA devices (7.1; 95% CI, 6.7–7.6; p = 0.068), with nonoverlapping CIs, but a nonsignificant p value (Table 2). For currently in-use devices, revisions per 1000 person-years were greater for THA (7.6; 95% CI, 6.5–8.8) than for metal-on-metal hip resurfacing (5.7; 95% CI, 5.2–6.2; p = 0.268). When discontinued devices were removed from the analysis, the average number of revisions for THA devices increased from 7.1 revisions per 1000 person-years (95% CI, 6.7–7.6) (Table 3), (Fig. 2. Supplemental material is available with the online version of CORR®) to 7.6 (95% CI, 6.5–8.8) (Table 4), (Fig. 3. Supplemental material is available with the online version of CORR®). For metal-on-metal hip resurfacing, removing discontinued devices decreased the average number of revisions from 10.7 per 1000 person-years (95% CI, 10.1–11.3) (Table 5), (Fig. 4. Supplemental material is available with the online version of CORR) to 5.7 (95% CI, 5.2–6.2) (Table 6), (Fig. 5. Supplemental material is available with the online version of CORR).
Table 3.
Revision rate per 1000 person-years for each THA study (all devices) with 95% confidence intervals
| Study | Sample size (n) | Upper bound | Lower bound | Revision rate |
|---|---|---|---|---|
| Fowble et al. [44] | 44 | 33.5 | 0.0 | 0.0 |
| Lachiewicz & Soileau [77] | 65 | 28.4 | 0.0 | 0.0 |
| Nayak et al. [99] | 226 | 4.1 | 0.0 | 0.0 |
| Zywiel et al. [147] | 33 | 29.8 | 0.0 | 0.0 |
| Kim [71] | 601 | 1.7 | 0.1 | 0.6 |
| Lübbeke et al [82] | 2495 | 2.1 | 0.9 | 1.4 |
| Kim [70] | 140 | 6.6 | 0.2 | 1.8 |
| Konstantoulakis et al. [74] | 102 | 10.3 | 0.0 | 1.8 |
| Nilsdotter & Isaksson [103] | 151 | 6.8 | 0.2 | 1.9 |
| Kalairajah et al. [66] | 196 | 7.4 | 0.2 | 2.0 |
| D’Lima et al. [39] | 174 | 6.3 | 0.4 | 2.2 |
| Garcia-Cimbrelo et al. [46] | 104 | 7.5 | 0.5 | 2.6 |
| D’Angelo et al. [31] | 225 | 6.1 | 0.8 | 2.6 |
| Mella-Sousa et al. [92] | 417 | 5.8 | 1.1 | 2.8 |
| Nilsdotter et al. [105] | 198 | 10.1 | 0.3 | 2.8 |
| Nilsdotter & Lohmander [104] | 196 | 10.2 | 0.3 | 2.8 |
| Ragab et al. [114] | 97 | 10.5 | 0.4 | 2.9 |
| Vendittoli et al. [139] | 102 | 16.4 | 0.1 | 2.9 |
| Schreiner et al. [121] | 335 | 5.7 | 1.4 | 3.0 |
| Bascarevic et al. [13] | 157 | 11.0 | 0.4 | 3.0 |
| Devane et al. [38] | 139 | 11.3 | 0.4 | 3.1 |
| Jacobs et al. [61] | 171 | 11.4 | 0.4 | 3.2 |
| Clohisy & Harris [27] | 90 | 9.0 | 1.0 | 3.5 |
| Herrera et al. [53] | 232 | 7.3 | 1.4 | 3.5 |
| Callaghan et al. [18] | 327 | 5.1 | 2.5 | 3.6 |
| Korovessis et al. [75] | 350 | 8.7 | 1.5 | 4.0 |
| Clohisy & Harris [26] | 100 | 10.2 | 1.1 | 4.0 |
| Tarasevicius et al. [130] | 1597 | 4.9 | 3.2 | 4.0 |
| Vendittoli et al. [138] | 100 | 15.5 | 0.5 | 4.3 |
| Castoldi et al. [23] | 135 | 9.7 | 1.6 | 4.4 |
| Saito et al. [119] | 90 | 10.5 | 1.5 | 4.5 |
| Saito et al. [120] | 38 | 12.0 | 1.3 | 4.7 |
| Firestone et al. [43] | 149 | 10.8 | 1.8 | 5.0 |
| Paleochorlidis et al. [109] | 99 | 12.4 | 1.7 | 5.3 |
| Long et al. [81] | 161 | 12.5 | 2.1 | 5.7 |
| Horne et al. [55] | 104 | 12.6 | 2.1 | 5.8 |
| Streit et al. [128] | 354 | 8.1 | 4.1 | 5.8 |
| Nagi et al. [96] | 102 | 11.5 | 2.5 | 5.9 |
| Neumann et al. [101] | 94 | 13.2 | 2.2 | 6.1 |
| Ollivere et al. [107] | 234 | 9.8 | 3.8 | 6.2 |
| Sinha et al. [123] | 123 | 14.6 | 2.0 | 6.3 |
| Fender et al. [42] | 1080 | 9.0 | 4.5 | 6.5 |
| Aldinger et al. [1] | 321 | 9.6 | 4.2 | 6.5 |
| Gollwitzer et al. [48] | 76 | 17.1 | 1.8 | 6.7 |
| Radcliffe et al. [113] | 65 | 20.8 | 1.5 | 7.1 |
| Sharma et al. [122] | 209 | 12.8 | 3.6 | 7.2 |
| Nercessian et al. [100] | 52 | 18.8 | 2.0 | 7.3 |
| Baker et al. [11] | 69 | 15.2 | 3.3 | 7.7 |
| Kim et al. [73] | 219 | 11.2 | 5.4 | 7.9 |
| Parvizi et al. [110] | 90 | 14.7 | 4.1 | 8.2 |
| Callaghan et al. [19] | 138 | 12.1 | 5.6 | 8.4 |
| Delaunay [35] | 98 | 19.8 | 2.8 | 8.5 |
| Archibeck et al. [7] | 92 | 17.1 | 3.8 | 8.7 |
| Beldame et al. [15] | 106 | 19.3 | 3.2 | 8.8 |
| Vassan et al. [137] | 94 | 19.8 | 3.3 | 9.1 |
| Descamps et al. [37] | 117 | 20.3 | 3.4 | 9.3 |
| Stulberg et al. [129] | 266 | 21.9 | 3.1 | 9.4 |
| Lazennec et al. [80] | 134 | 17.4 | 5.1 | 10.0 |
| Gaffey et al. [45] | 120 | 15.8 | 5.9 | 10.0 |
| Russell et al. [118] | 127 | 18.2 | 5.7 | 10.7 |
| Hulleberg et al. [57] | 138 | 17.2 | 6.8 | 11.1 |
| Mont et al. [94] | 54 | 41.2 | 1.4 | 11.4 |
| Pollard et al. [111] | 51 | 30.1 | 3.2 | 11.8 |
| Laupacis et al. [79] | 250 | 18.8 | 7.3 | 12.1 |
| Haraguchi et al. [51] | 119 | 18.1 | 8.1 | 12.3 |
| Haidukewych et al. [50] | 21 | 71.7 | 0.3 | 12.9 |
| Kim et al. [72] | 116 | 21.0 | 7.6 | 13.1 |
| Tompkins et al. [132] | 173 | 21.3 | 8.6 | 14.0 |
| Bjorgul et al. [17] | 151 | 21.4 | 10.4 | 15.1 |
| Baker et al. [12] | 54 | 29.6 | 7.1 | 15.6 |
| Nakamura et al. [97] | 50 | 27.8 | 8.2 | 15.9 |
| Almeida et al. [2] | 75 | 27.9 | 8.3 | 16.0 |
| Corten et al. [28] | 238 | 20.7 | 13.1 | 16.6 |
| de Kam et al. [34] | 168 | 25.6 | 11.9 | 17.8 |
| Dearborn & Murray [32] | 86 | 31.2 | 9.2 | 17.9 |
| Vigler et al. [141] | 43 | 58.3 | 4.1 | 19.9 |
| Cho et al. [25] | 86 | 36.9 | 11.5 | 21.6 |
| Sporer et al. [126] | 45 | 42.7 | 9.4 | 21.7 |
| Howie et al. [56] | 13 | 79.3 | 5.6 | 27.1 |
| Meldrum et al. [91] | 125 | 37.3 | 21.1 | 28.3 |
| Langdon & Bannister [78] | 35 | 44.2 | 17.5 | 28.6 |
| McLaughlin & Lee [90] | 94 | 52.1 | 31.0 | 40.6 |
| Illgen et al. [58] | 163 | 88.5 | 17.3 | 42.9 |
| McLaughlin & Lee [89] | 114 | 75.6 | 46.3 | 59.6 |
| Theis & Beadel [131] | 12 | 301.0 | 10.1 | 83.3 |
| Grouped revision rate | 7.6 | 6.7 | 7.1 |
Table 4.
Revision rate per 1000 person-years for each THA study (currently in-use devices) with 95% confidence intervals
| Study | Sample size (number) | Upper bound | Lower bound | Revision rate |
|---|---|---|---|---|
| Fowble et al. [44] | 44 | 33.5 | 0.0 | 0.0 |
| Nayak et al. [99] | 226 | 4.1 | 0.0 | 0.0 |
| Zywiel et al. [147] | 33 | 29.8 | 0.0 | 0.0 |
| Garcia-Cimbrelo et al. [46] | 104 | 7.5 | 0.5 | 2.6 |
| D’Angelo et al. [31] | 225 | 6.1 | 0.8 | 2.6 |
| Vendittoli et al. [139] | 102 | 16.4 | 0.1 | 2.9 |
| Bascarevic et al. [13] | 157 | 11.0 | 0.4 | 3.0 |
| Herrera et al. [53] | 232 | 7.3 | 1.4 | 3.5 |
| Korovessis et al. [75] | 350 | 8.7 | 1.5 | 4.0 |
| Vendittoli et al. [138] | 100 | 15.5 | 0.5 | 4.3 |
| Castoldi et al. [23] | 135 | 9.7 | 1.6 | 4.4 |
| Saito et al. [119] | 90 | 10.5 | 1.5 | 4.5 |
| Paleochorlidis et al. [109] | 99 | 12.4 | 1.7 | 5.3 |
| Neumann et al. [101] | 94 | 13.2 | 2.2 | 6.1 |
| Radcliffe et al. [113] | 65 | 20.8 | 1.5 | 7.1 |
| Nercessian et al. [100] | 52 | 18.8 | 2.0 | 7.3 |
| Baker et al. [11] | 69 | 15.2 | 3.3 | 7.7 |
| Delaunay [35] | 98 | 19.8 | 2.8 | 8.5 |
| Stulberg et al. [129] | 266 | 21.9 | 3.1 | 9.4 |
| Mont et al. [94] | 54 | 41.2 | 1.4 | 11.4 |
| Laupacis et al. [79] | 250 | 18.8 | 7.3 | 12.1 |
| Corten et al [28] | 238 | 20.7 | 13.1 | 16.6 |
| Vigler et al. [141] | 43 | 58.3 | 4.1 | 19.9 |
| Theis & Beadel [131] | 12 | 301.0 | 10.1 | 83.3 |
| Grouped revision rate | 8.8 | 6.5 | 7.6 |
Table 5.
Revision rate per 1000 person-years for each metal-on-metal hip resurfacing study (all devices) with 95% confidence intervals
| Study | Sample size (n) | Upper bound | Lower bound | Revision rate |
|---|---|---|---|---|
| Ollivere et al. [108] | 98 | 7.4 | 0.0 | 0.0 |
| Xu et al. [144] | 63 | 63.6 | 0.0 | 0.0 |
| Yang et al. [145] | 21 | 87.8 | 0.0 | 0.0 |
| Zywiel et al. [147] | 33 | 31.9 | 0.0 | 0.0 |
| Back et al. [10] | 230 | 8.1 | 0.0 | 1.4 |
| McBryde et al. [87] | 909 | 2.5 | 0.8 | 1.5 |
| Hing et al. [54] | 230 | 6.3 | 0.2 | 1.7 |
| Amstutz et al. [3] | 686 | 4.0 | 1.4 | 2.4 |
| Aulakh et al. [8] | 202 | 6.5 | 1.1 | 3.0 |
| Treacy et al. [133] | 144 | 12.2 | 0.9 | 4.2 |
| Rahman et al. [115] | 329 | 8.5 | 2.2 | 4.6 |
| Carrothers et al. [21] | 5000 | 5.9 | 4.4 | 5.1 |
| Carrothers et al. [22] | 106 | 13.6 | 1.4 | 5.3 |
| Vendittoli et al. [140] | 64 | 32.2 | 0.1 | 5.8 |
| Vendittoli et al. [139] | 103 | 21.1 | 0.7 | 5.8 |
| Amstutz & Le Duff [5] | 1000 | 8.2 | 4.1 | 5.9 |
| Heilpern et al. [52] | 110 | 15.8 | 1.7 | 6.2 |
| Fowble et al. [44] | 50 | 34.8 | 0.2 | 6.3 |
| Treacy et al. [134] | 144 | 11.7 | 3.1 | 6.4 |
| McAndrew et al. [86] | 179 | 18.8 | 1.3 | 6.4 |
| Khan et al. [67] | 679 | 10.2 | 4.8 | 7.1 |
| Ollivere et al. [106] | 463 | 13.3 | 4.2 | 7.8 |
| Vendittoli et al. [138] | 109 | 20.1 | 2.1 | 7.9 |
| Amstutz et al. [4] | 400 | 15.9 | 4.9 | 9.3 |
| Pritchett [112] | 561 | 11.0 | 7.8 | 9.3 |
| Amstutz et al. [6] | 100 | 16.8 | 4.7 | 9.4 |
| Spencer et al. [125] | 40 | 34.1 | 1.1 | 9.4 |
| Marulanda et al. [85] | 230 | 28.7 | 2.0 | 9.8 |
| Witzleb et al. [142] | 300 | 21.8 | 3.7 | 10.0 |
| Baker et al. [12] | 54 | 24.0 | 3.3 | 10.3 |
| Madhu et al. [84] | 110 | 20.5 | 4.5 | 10.4 |
| Mont et al. [94] | 54 | 41.2 | 1.4 | 11.4 |
| Pollard et al. [111] | 63 | 32.0 | 3.4 | 12.5 |
| Jameson et al. [63] | 231 | 28.4 | 6.2 | 14.4 |
| Kim et al. [68] | 97 | 45.2 | 3.2 | 15.5 |
| McGrath et al. [88] | 165 | 34.5 | 8.3 | 18.2 |
| Bergeron et al. [16] | 209 | 37.7 | 8.3 | 19.1 |
| Jameson et al. [62] | 214 | 35.3 | 12.9 | 22.1 |
| Isaac et al. [60] | 77 | 66.5 | 7.1 | 26.0 |
| Kim et al. [69] | 200 | 45.2 | 14.7 | 26.9 |
| Gross & Liu [49] | 19 | 72.8 | 7.8 | 28.4 |
| Della Valle et al. [36] | 537 | 50.3 | 16.4 | 30.0 |
| Falez et al. [41] | 60 | 72.8 | 10.1 | 31.2 |
| Stulberg et al. [129] | 337 | 53.0 | 22.8 | 35.6 |
| Beaulé et al. [14] | 42 | 64.3 | 20.9 | 38.3 |
| Costi et al. [29] | 268 | 53.3 | 40.2 | 46.4 |
| Cutts et al. [30] | 65 | 85.0 | 27.7 | 50.7 |
| Meldrum et al. [91] | 141 | 64.1 | 44.5 | 53.6 |
| Duijsens et al. [40] | 114 | 76.4 | 45.5 | 59.5 |
| Ritter et al. [117] | 65 | 89.2 | 46.4 | 65.2 |
| Howie et al. [56] | 11 | 168.6 | 36.9 | 85.6 |
| Yue et al. [146] | 75 | 137.9 | 83.2 | 108.0 |
| Grouped revision rate | 11.3 | 10.1 | 10.7 |
Table 6.
Revision rate per 1000 person-years for each metal-on-metal hip resurfacing study (currently in-use devices) with 95% confidence intervals
| Study | Sample size (n) | Upper bound | Lower bound | Revision rate |
|---|---|---|---|---|
| Ollivere et al. [108] | 98 | 7.4 | 0.0 | 0.0 |
| Yang et al. [145] | 21 | 87.8 | 0.0 | 0.0 |
| Zywiel et al. [147] | 33 | 31.9 | 0.0 | 0.0 |
| Back et al. [10] | 230 | 8.1 | 0.0 | 1.4 |
| McBryde et al. [87] | 909 | 2.5 | 0.8 | 1.5 |
| Hing et al. [54] | 230 | 6.3 | 0.2 | 1.7 |
| Amstutz et al. [3] | 686 | 4.0 | 1.4 | 2.4 |
| Aulakh et al. [8] | 202 | 6.5 | 1.1 | 3.0 |
| Treacy et al. [133] | 144 | 12.2 | 0.9 | 4.2 |
| Rahman et al. [115] | 329 | 8.5 | 2.2 | 4.6 |
| Carrothers et al. [21] | 5000 | 5.9 | 4.4 | 5.1 |
| Carrothers et al. [22] | 106 | 13.6 | 1.4 | 5.3 |
| Vendittoli et al. [140] | 64 | 32.2 | 0.1 | 5.8 |
| Vendittoli et al. [139] | 103 | 21.1 | 0.7 | 5.8 |
| Amstutz & Le Duff [5] | 1000 | 8.2 | 4.1 | 5.9 |
| Heilpern et al. [52] | 110 | 15.8 | 1.7 | 6.2 |
| Fowble et al. [44] | 50 | 34.8 | 0.2 | 6.3 |
| Treacy et al. [134] | 144 | 11.7 | 3.1 | 6.4 |
| McAndrew et al. [86] | 179 | 18.8 | 1.3 | 6.4 |
| Khan et al. [67] | 679 | 10.2 | 4.8 | 7.1 |
| Ollivere et al. [106] | 463 | 13.3 | 4.2 | 7.8 |
| Vendittoli et al. [138] | 109 | 20.1 | 2.1 | 7.9 |
| Amstutz et al. [4] | 400 | 15.9 | 4.9 | 9.3 |
| Amstutz et al. [6] | 100 | 16.8 | 4.7 | 9.4 |
| Spencer et al. [125] | 40 | 34.1 | 1.1 | 9.4 |
| Marulanda et al. [85] | 230 | 28.7 | 2.0 | 9.8 |
| Witzleb et al. [142] | 300 | 21.8 | 3.7 | 10.0 |
| Madhu et al. [84] | 110 | 20.5 | 4.5 | 10.4 |
| Mont et al. [94] | 54 | 41.2 | 1.4 | 11.4 |
| Kim et al. [68] | 97 | 45.2 | 3.2 | 15.5 |
| McGrath et al. [88] | 165 | 34.5 | 8.3 | 18.2 |
| Kim et al. [69] | 200 | 45.2 | 14.7 | 26.9 |
| Gross & Liu [49] | 19 | 72.8 | 7.8 | 28.4 |
| Della Valle et al. [36] | 537 | 50.3 | 16.4 | 30.0 |
| Stulberg et al. [129] | 337 | 53.0 | 22.8 | 35.6 |
| Cutts et al. [30] | 65 | 85.0 | 27.7 | 50.7 |
| Grouped revision rate | 6.2 | 5.2 | 5.7 |
Three national registries (Australia, Sweden, and England and Wales) reported higher revision rates for metal-on-metal hip resurfacing devices compared with THA devices. The New Zealand registry was the only registry that showed a higher revision rate per 1000 person-years for THA (2.7; 95% CI, 2.6–2.8) compared with metal-on-metal hip resurfacing (2.4; 95% CI, 1.7–3.4) (Table 7). The registry revision rates were lower than those found in our systematic review for THA and metal-on-metal hip resurfacing devices, with the exception of THA and metal-on-metal hip resurfacing revision rates for the England and Wales registry (Table 7).
Table 7.
Revisions per 1000 person-years
| Procedure | National Joint Replacement Registry | Number of revisions during registry period | Time (years) | Revisions (per 1000 person years) | 95% CI | p value (THA vs metal-on-metal hip resurfacing) | Current study revisions (per 1000 person-years; all devices) | 95% CI | p value (THA vs metal-on-metal hip resurfacing) |
|---|---|---|---|---|---|---|---|---|---|
| THA | |||||||||
| AOANJRR | 6321 | 10 | 3.2 | 3.1–3.3 | |||||
| NZNJR | 2278 | 12 | 2.7 | 2.6–2.8 | |||||
| SHAR | 27,134 | 31 | 2.64 | 2.61–2.7 | |||||
| NJREW | 6104 | 827,276 observed years | 7.4 | 7.2–7.6 | |||||
| Grouped | 3.01 | 2.98–3.03 | 0.350 | 7.1 | 6.7–7.6 | 0.068 | |||
| Metal-on-metal hip resurfacing | |||||||||
| AOANJRR | 660 | 10 | 4.6 | 4.3–5.0 | |||||
| NZNJR | 32 | 12 | 2.4 | 1.7–3.4 | |||||
| SHAR | 72 | 10 | 4.1 | 3.2–5.1 | |||||
| NJREW | 867 | 61,170 observed years | 14.2 | 13.2–15.1 | |||||
| Grouped | 6.9 | 6.6–7.3 | 0.350 | 10.7 | 10.1–11.3 | 0.068 | |||
AOANJRR = Australian Orthopaedic Association National Joint Replacement Registry; NZNJR = New Zealand National Joint Registry; SHAR = Swedish Hip Arthroplasty Register; NJREW = National Joint Registry for England and Wales.
Reoperations
For all devices, reoperations were more frequent in metal-on-metal hip resurfacing (7.9 per 1000 person-years; 95% CI, 5.4–11.3) than THA devices (1.8 per 1000 person years; 95% CI, 1.3–2.2; p = 0.084) (Table 2). When discontinued devices were removed from the analysis, reoperations remained higher in metal-on-metal hip resurfacing devices (Table 2). The most common reasons reported for reoperation in metal-on-metal hip resurfacing were fracture (femoral neck, greater trochanter, subtrochanteric femur fracture), heterotopic ossification, and component mismatch. The most common reasons reported for reoperation for THAs were heterotopic ossification, osteolysis, excessive polyethylene wear, and infection.
Dislocations
Dislocations were more frequent for THA than metal-on-metal hip resurfacing devices for currently in-use devices (4.8; 95% CI, 3.5–6.5 versus 1.1, 95% CI, 0.8–1.6 per 1000 person-years; p = 0.01) and all devices (4.4; 95% CI, 4.2–4.6 versus 0.8, 95% CI, 0.6–1.2 per 1000 person-years; p = 0.008) (Table 2).
Other Adverse Events
For currently in-use devices, infections/sepsis per 1000 person-years were more frequent for THA (3.2 per 1000 person-years; 95% CI, 2.0–4.8) compared with metal-on-metal hip resurfacing (1.2 per 1000 person-years; 95% CI, 0.8–1.8; p = 0.18) (Table 2). When discontinued devices were removed from the analysis, infections/sepsis remained higher in THA devices (Table 2).
For all devices, femoral neck fractures were more frequent for THA devices (2.9 per 1000 person-years; 95% CI, 1.6–4.8) compared with metal-on-metal hip resurfacing (2.0 per 1000 person-years; 95% CI, 1.6–2.6; p = 0.654) (Table 2). For currently in-use devices, femoral neck fractures were more frequent for metal-on-metal hip resurfacing devices compared with THA (Table 2). Although femoral neck fractures are extremely rare with THA devices, they still were reported in studies (N = 2 for currently in-use THA devices and N = 7 for all THA devices) as adverse events.
There was a lack of comparable data to analyze other femoral fractures and mortality (all-cause, 30-day).
Rates of Postoperative Component Alignment
We were unable to draw conclusions for postoperative component alignment owing to limited comparable data in both market status groups.
Discussion
In the United States, nearly 203,000 primary hip surgeries were performed in 2003 and this figure is projected to increase to more than 500,000 surgeries annually by 2030, and consequently the number of revisions will increase [76]. The majority of individuals who require primary hip replacement undergo THA [9, 47, 98, 102]. Metal-on-metal hip resurfacing is used less often, targeted toward younger, more active patients as an alternative to THA, but remains controversial [65, 124, 127, 136, 143]. We believe there is limited evidence thus far in the literature that compares adverse events across studies of metal-on-metal hip resurfacing and THA using a standardized metric. Without standardized metrics, it is not possible to make valid comparisons that account for differences in study sample sizes and followup times, which can have a substantial effect on the results. In this review, we used the standardized metric, per 1000 person-years, to address gaps not previously addressed in the literature to compare outcomes between THA studies that had longer-term followups with metal-on-metal hip resurfacing studies with limited followup. We aimed to determine rates of (1) early revision or reoperation (within 5 years of surgery) and overall revisions; (2) revisions reported in four major joint replacement registries; (3) adverse events; and (4) postoperative component malalignment using standardized metrics and stratifying results by device market status.
The literature on joint arthroplasty is challenging because definitions of outcomes are not consistent (eg, revisions versus reoperations). Additionally, metrics are not standardized or comparable (eg, studies have varying followup periods). We were able to draw comparisons between heterogeneous studies by reporting averages per 1000 person-years. This is unique in the arthroplasty literature. Other limitations include underreporting of prosthesis type, some studies were not able to be grouped into market status categories and therefore were excluded from our analysis, and exclusion of non-English literature.
Furthermore, studies did not report outcomes consistently (eg, number of hips operated on versus number of patients). We standardized adverse event rates to the extent possible by using the number of participants in the study population and, if this was not available, the number of hips. Patients who receive metal-on-metal hip resurfacing devices tend to be male, younger, and more active compared with those who receive THA devices. Finally, when analyzing data from the literature, the inclusion of discontinued devices can dramatically skew findings. To date, it has not been common practice to analyze outcomes of medical devices according to market status. Our findings suggest that this type of analysis is important for continued implementation of medical devices or adoption of new devices. For example, we noted higher revision rates for all metal-on-metal hip resurfacing devices compared with currently in-use devices, which may reflect the inclusion of devices that have been discontinued. By removing discontinued metal-on-metal hip resurfacing devices, the average revisions per 1000 person-years was lower.
Revisions are more frequent (all devices market status group) and occur much earlier for all metal-on-metal hip resurfacing devices (in-use and discontinued market status groups). The average time to revision would be considered poor for metal-on-metal hip resurfacing and THA devices which supports the ongoing need for long-term followup studies on clinical outcomes. Four of five metal-on-metal hip resurfacing systematic reviews published since 2006 noted promising revision rates and pain relief [65, 124, 127, 136, 143]. Time to revision (in years) has not been reported in other reviews comparing metal-on-metal hip resurfacing with THA [65, 124, 127, 136]. According to data from the Canadian Joint Replacement Registry [20, 83], 88% of patients who received metal-on-metal hip resurfacing were younger than 65 years. Smith et al. [124] determined it is unclear how patient age might influence the incidence of adverse events when comparing THA and metal-on-metal hip resurfacing devices.
Lower revision rates noted among most registries, in comparison to our review, may reflect the larger sample size and higher participation rates in registry data. The International Society of Arthroplasty Registries requires national registries to have greater than 90% of procedures reported to obtain a full membership [59]. Additionally, registries may define revisions differently than clinical studies and lack study protocols with controlled followup.
As anticipated as a result of the ball and socket design of THA devices, dislocation rates were higher than metal-on-metal hip resurfacing for both market status groups. This is consistent with other reviews of this literature [65, 124, 127, 136]. The number of femoral neck fractures was greater for metal-on-metal hip resurfacing devices (currently in-use devices) and these findings are consistent with the literature [65, 127].
Postoperative component alignment was not commonly reported in the literature, and thus no comparisons could be made. This finding is important because, even with the large number of studies included in our analysis, we still were unable to draw any conclusions regarding postoperative component malalignment in both market status groups. Methods of measuring component alignment are not standardized, further complicating comparisons across studies. Further studies assessing component alignment are needed in this area of research since the clinical evidence of poor alignment as a predictor of device failure has been highlighted in the literature [33].
The strengths of our study were threefold. First, we used averages per 1000 person-years to standardize findings and make valid comparisons. Second, we examined a large body of evidence, and third, we analyzed results by market status. The findings from our systematic review show that revisions and reoperations are more frequent and occur much earlier for metal-on-metal hip resurfacing, except when discontinued devices are removed from the analyses. Dislocations are more frequent with THA, even after removing discontinued devices from the analyses. We found that outcome definitions were reported inconsistently in the studies we identified, and that those studies rarely differentiated their findings regarding adverse events according to the market status of the device(s) in question. These deficiencies can result in clinicians drawing misleading conclusions and misinforming patients. We tried to mitigate the risk of this by using specific design elements in this study, including stratification by market status and standardization of event frequencies per 1000 person-years. Standardized comparative outcomes for metal-on-metal hip resurfacing and THA should be considered when selecting which device is most appropriate for individual patients.
Electronic supplementary material
Acknowledgments
We thank Denis Ako-Arrey DAA; MHA, MPH (McMaster University, Hamilton, Ontario, Canada), and Monica Cepoiu-Martin MCM; MD (University of Calgary, Calgary, Alberta, Canada) for their work reviewing abstracts and full-text articles for this systematic review. We also thank Gavin Steininger BSc, MASc, PhD (University of Victoria, Victoria, British Columbia, Canada) for biostatistics expertise and assistance.
Footnotes
This study was funded by a Canadian Institutes of Health Research (CIHR) Knowledge Synthesis grant (grant number 228369). The study funder had no involvement in the study design, collection, analysis, or interpretation of the data.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
This work was performed at the University of Calgary, Calgary, Alberta, Canada.
References
- 1.Aldinger PR, Breusch SJ, Lukoschek M, Mau H, Ewerbeck V, Thomsen M. A ten-to 15-year follow-up of the cementless spotorno stem. J Bone Joint Surg Br. 2003;85:209–214. doi: 10.1302/0301-620x.85b2.13216. [DOI] [PubMed] [Google Scholar]
- 2.Almeida F, Pino L, Silvestre A, Gomar F. Mid- to long-term outcome of cementless total hip arthroplasty in younger patients. J Orthop Surg (Hong Kong). 2010;18:172–178. doi: 10.1177/230949901001800208. [DOI] [PubMed] [Google Scholar]
- 3.Amstutz HC, Ball ST, Le Duff MJ, Dorey FJ. Resurfacing THA for patients younger than 50 year: results of 2- to 9-year followup. Clin Orthop Relat Res. 2007;460:159–164. doi: 10.1097/BLO.0b013e318041f0e7. [DOI] [PubMed] [Google Scholar]
- 4.Amstutz HC, Beaule PE, Dorey FJ, Le Duff MJ, Campbell PA, Gruen TA. Metal-on-metal hybrid surface arthroplasty: two to six-year follow-up study. J Bone Joint Surg Am. 2004;86:28–39. [PubMed] [Google Scholar]
- 5.Amstutz HC, Le Duff MJ. Cementing the metaphyseal stem in metal-on-metal resurfacing: when and why. Clin Orthop Relat Res. 2009;467:79–83. doi: 10.1007/s11999-008-0570-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Amstutz HC, Le Duff MJ, Campbell PA, Gruen TA, Wisk LE. Clinical and radiographic results of metal-on-metal hip resurfacing with a minimum ten-year follow-up. J Bone Joint Surg Am. 2010;92:2663–2671. doi: 10.2106/JBJS.I.01715. [DOI] [PubMed] [Google Scholar]
- 7.Archibeck MJ, Berger RA, Jacobs JJ, Quigley LR, Gitelis S, Rosenberg AG, Galante JO. Second-generation cementless total hip arthroplasty: eight to eleven-year results. J Bone Joint Surg Am. 2001;83:1666–1673. doi: 10.2106/00004623-200111000-00008. [DOI] [PubMed] [Google Scholar]
- 8.Aulakh TS, Rao C, Kuiper JH, Richardson JB. Hip resurfacing and osteonecrosis: results from an independent hip resurfacing register. Arch Orthop Trauma Surg. 2010;130:841–845. doi: 10.1007/s00402-009-0963-0. [DOI] [PubMed] [Google Scholar]
- 9.Australian Orthopaedic Association National Joint Replacement Registry. Annual Report 2011. Available at: https://aoanjrr.dmac.adelaide.edu.au/annual-reports-2011. Accessed January 30, 2014
- 10.Back DL, Dalziel R, Young D, Shimmin A. Early results of primary Birmingham hip resurfacings: an independent prospective study of the first 230 hips. J Bone Joint Surg Br. 2005;87:324–329. doi: 10.1302/0301-620x.87b3.15556. [DOI] [PubMed] [Google Scholar]
- 11.Baker PN, McMurtry IA, Chuter G, Port A, Anderson J. THA with the ABG I prosthesis at 15 years: excellent survival with minimal osteolysis. Clin Orthop Relat Res. 2010;468:1855–1861. doi: 10.1007/s11999-009-1066-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Baker RP, Pollard TC, Eastaugh-Waring SJ, Bannister GC. A medium-term comparison of hybrid hip replacement and Birmingham hip resurfacing in active young patients. J Bone Joint Surg Br. 2011;93:158–163. doi: 10.1302/0301-620X.93B2.25625. [DOI] [PubMed] [Google Scholar]
- 13.Bascarevic Z, Vukasinovic Z, Slavkovic N, Dulic B, Trajkovic G, Bascarevic V, Timotijevic S. Alumina-on-alumina ceramic versus metal-on-highly cross-linked polyethylene bearings in total hip arthroplasty: a comparative study. Int Orthop. 2010;34:1129–1135. doi: 10.1007/s00264-009-0899-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Beaule PE, Le Duff M, Campbell P, Dorey FJ, Park SH, Amstutz HC. Metal-on-metal surface arthroplasty with a cemented femoral component: a 7-10 year follow-up study. J Arthroplasty. 2004;19(8 suppl 3):17–22. doi: 10.1016/j.arth.2004.09.004. [DOI] [PubMed] [Google Scholar]
- 15.Beldame J, Carreras F, Oger P, Beaufils P. Cementless cups do not increase osteolysis risk in metal-on-metal total hip arthroplasty: apropos of 106 cases. Orthop Traumatol Surg Res. 2009;95:478–490. doi: 10.1016/j.otsr.2009.07.007. [DOI] [PubMed] [Google Scholar]
- 16.Bergeron SG, Desy NM, Nikolaou VS, Debiparshad K, Antoniou J. The early results of metal-on-metal hip resurfacing: a prospective study at a minimum two-year follow-up. Bull NYU Hosp Jt Dis. 2009;67:132–134. [PubMed] [Google Scholar]
- 17.Bjorgul K, Novicoff WM, Andersen ST, Brevig K, Thu F, Wiig M, Ahlund O. No differences in outcomes between cemented and uncemented acetabular components after 12–14 years: results from a randomized controlled trial comparing Duraloc with Charnley cups. J Orthop Traumatol. 2010;11:37–45. doi: 10.1007/s10195-010-0082-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Callaghan JJ, Albright JC, Goetz DD, Olejniczak JP, Johnston RC. Charnley total hip arthroplasty with cement: minimum twenty-five-year follow-up. J Bone Joint Surg Am. 2000;82:487–497. doi: 10.2106/00004623-200004000-00004. [DOI] [PubMed] [Google Scholar]
- 19.Callaghan JJ, Forest EE, Sporer SM, Goetz DD, Johnston RC. Total hip arthroplasty in the young adult. Clin Orthop Relat Res. 1997;344:257–262. [PubMed] [Google Scholar]
- 20.Canadian Institute for Health Information. The effect of bearing surface on early revisions following total hip arthroplasty. Available at: https://secure.cihi.ca/free_products/AiB_CJRR_Bearing-Surface-Revisions_July2013_EN.pdf. Accessed July 18, 2013.
- 21.Carrothers AD, Gilbert RE, Jaiswal A, Richardson JB. Birmingham hip resurfacing: the prevalence of failure. J Bone Joint Surg Br. 2010;92:1344–1350. doi: 10.1302/0301-620X.92B10.23504. [DOI] [PubMed] [Google Scholar]
- 22.Carrothers AD, Gilbert RE, Richardson JB. Birmingham hip resurfacing in patients who are seventy years of age or older. Hip Int. 2011;21:217–224. doi: 10.5301/HIP.2011.6500. [DOI] [PubMed] [Google Scholar]
- 23.Castoldi F, Rossi R, La Russa M, Sibelli P, Rossi P, Ranawat AS. Ten-year survivorship of the Anatomique Benoist Girard I total hip arthroplasty. J Arthroplasty. 2007;22:363–368. doi: 10.1016/j.arth.2006.05.022. [DOI] [PubMed] [Google Scholar]
- 24.Centre for Reviews and Dissemination. Systematic Reviews: CRD’s guidance for undertaking reviews in health care. York, England: CRD, University of York; 2009. Available at: http://www.york.ac.uk/inst/crd/pdf/Systematic_Reviews.pdf. Accessed January 30, 2014.
- 25.Cho JH, Garino JP, Choo SK, Han KY, Kim JH, Oh HK. Seven-year results of a tapered, titanium, hydroxyapatite-coated cementless femoral stem in primary total hip arthroplasty. Clin Orthop Surg. 2010;2:214–220. doi: 10.4055/cios.2010.2.4.214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Clohisy JC, Harris WH. Primary hybrid total hip replacement, performed with insertion of the acetabular component without cement and a precoat femoral component with cement: an average ten-year follow-up study. J Bone Joint Surg Am. 1999;81:247–255. doi: 10.2106/00004623-199902000-00012. [DOI] [PubMed] [Google Scholar]
- 27.Clohisy JC, Harris WH. Matched-pair analysis of cemented and cementless acetabular reconstruction in primary total hip arthroplasty. J Arthroplasty. 2001;16:697–705. doi: 10.1054/arth.2001.24447. [DOI] [PubMed] [Google Scholar]
- 28.Corten K, Bourne RB, Charron KD, Au K, Rorabeck CH. What works best, a cemented or cementless primary total hip arthroplasty? Minimum 17-year followup of a randomized controlled trial. Clin Orthop Relat Res. 2011;469:209–217. doi: 10.1007/s11999-010-1459-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Costi K, Howie DW, Campbell DG, McGee MA, Cornish BL. Long-term survival and reason for revision of Wagner resurfacing hip arthroplasty. J Arthroplasty. 2010;25:522–528. doi: 10.1016/j.arth.2009.04.007. [DOI] [PubMed] [Google Scholar]
- 30.Cutts S, Datta A, Ayoub K, Rahman H, Lawrence T. Early failure modalities in hip resurfacing. Hip Int. 2005;15:155–158. doi: 10.1177/112070000501500305. [DOI] [PubMed] [Google Scholar]
- 31.D’Angelo F, Murena L, Vulcano E, Zatti G, Cherubino P. Seven to twelve year results with Versys ET cementless stem: a retrospective study of 225 cases. Hip Int. 2010;20:81–86. doi: 10.1177/112070001002000112. [DOI] [PubMed] [Google Scholar]
- 32.Dearborn JT, Murray WR. Arthopor 2 acetabular component with screw fixation in primary hip arthroplasty: a 7- to 9-year follow-up study. J Arthroplasty. 1998;13:299–310. doi: 10.1016/s0883-5403(98)90176-0. [DOI] [PubMed] [Google Scholar]
- 33.De Haan R, Campbell PA, Su EP, De Smet KA. Revision of metal-on-metal resurfacing arthroplasty of the hip: the influence of malpositioning of the components. J Bone Joint Surg Br. 2008;90:1158–1163. doi: 10.1302/0301-620X.90B9.19891. [DOI] [PubMed] [Google Scholar]
- 34.de Kam DC, Gardeniers JW, Veth RP, Schreurs BW. Good results with cemented total hip arthroplasty in patients between 40 and 50 years of age. Acta Orthop. 2010;81:165–170. doi: 10.3109/17453671003717831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Delaunay CP. Metal-on-metal bearings in cementless primary total hip arthroplasty. J Arthroplasty. 2004;19(8 suppl 3):35–40. doi: 10.1016/j.arth.2004.09.002. [DOI] [PubMed] [Google Scholar]
- 36.Della Valle CJ, Nunley RM, Raterman SJ, Barrack RL. Initial American experience with hip resurfacing following FDA approval. Clin Orthop Relat Res. 2009;467:72–78. doi: 10.1007/s11999-008-0563-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Descamps S, Bouillet B, Boisgard S, Levai JP. High incidence of loosening at 5-year follow-up of a cemented metal-on-metal acetabular component in THR. Eur J Orthop Surg Traumatol. 2009;19:559–563. [Google Scholar]
- 38.Devane PA, Robinson EJ, Bourne RB, Rorabeck CH, Nayak NN, Horne JG. Measurement of polyethylene wear in acetabular components inserted with and without cement: a randomized trial. J Bone Joint Surg Am. 1997;79:682–689. doi: 10.2106/00004623-199705000-00007. [DOI] [PubMed] [Google Scholar]
- 39.D’Lima DD, Oishi CS, Petersilge WJ, Colwell CW, Walker RH. 100 cemented versus 100 noncemented stems with comparison of 25 matched pairs. Clin Orthop Relat Res. 1998;348:140–148. [PubMed] [Google Scholar]
- 40.Duijsens AW, Keizer S, Vliet-Vlieland T, Nelissen RG. Resurfacing hip prostheses revisited: failure analysis during a 16-year follow-up. Int Orthop. 2005;29:224–228. doi: 10.1007/s00264-005-0652-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Falez F, Favetti F, Casella F, Panegrossi G. Hip resurfacing: why does it fail? Early results and critical analysis of our first 60 cases. Int Orthop. 2008;32:209–216. doi: 10.1007/s00264-006-0313-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Fender D, Harper WM, Gregg PJ. Outcome of Charnley total hip replacement across a single health region in England: the results at five years from a regional hip register. J Bone Joint Surg Br. 1999;81:577–581. doi: 10.1302/0301-620x.81b4.9859. [DOI] [PubMed] [Google Scholar]
- 43.Firestone DE, Callaghan JJ, Liu SS, Goetz DD, Sullivan PM, Vittetoe DA, Johnston RC. Total hip arthroplasty with a cemented, polished, collared femoral stem and a cementless acetabular component: a follow-up study at a minimum of ten years. J Bone Joint Surg Am. 2007;89:126–132. doi: 10.2106/JBJS.E.01214. [DOI] [PubMed] [Google Scholar]
- 44.Fowble VA, dela Rosa MA, Schmalzried TP. A comparison of total hip resurfacing and total hip arthroplasty: patients and outcomes. Bull NYU Hosp Jt Dis. 2009;67:108–112. [PubMed]
- 45.Gaffey JL, Callaghan JJ, Pedersen DR, Goetz DD, Sullivan PM, Johnston RC. Cementless acetabular fixation at fifteen years: a comparison with the same surgeon’s results following acetabular fixation with cement. J Bone Joint Surg Am. 2004;86:257–261. [PubMed] [Google Scholar]
- 46.Garcia-Cimbrelo E, Cruz-Pardos A, Madero R, Ortega-Andreu M. Total hip arthroplasty with use of the cementless Zweymuller Alloclassic system: a ten to thirteen-year follow-up study. J Bone Joint Surg Am. 2003;85:296–303. doi: 10.2106/00004623-200302000-00017. [DOI] [PubMed] [Google Scholar]
- 47.Garellick G, Karrholm J, Rogmark C, Herberts P. Swedish Hip Arthroplasty Register 2010 Annual Report. Available at: http://www.shpr.se/Libraries/Documents/AnnualReport-2010-2-eng.sflb.ashx. Accessed January 30, 2014.
- 48.Gollwitzer H, Gerdesmeyer L, Horn C, Diehl P, Topfer A, Gradinger R. 8-year follow-up after cementless hip arthroplasty with a second generation spongy metal total hip replacement. Hip Int. 2009;19:359–366. doi: 10.1177/112070000901900410. [DOI] [PubMed] [Google Scholar]
- 49.Gross TP, Liu F. Metal-on-metal hip resurfacing with an uncemented femoral component: a seven-year follow-up study. J Bone Joint Surg Am. 2008;90(suppl 3):32–37. doi: 10.2106/JBJS.H.00614. [DOI] [PubMed] [Google Scholar]
- 50.Haidukewych GJ, Jacofsky DJ, Hanssen AD, Lewallen DG. Intraoperative fractures of the acetabulum during primary total hip arthroplasty. J Bone Joint Surg Am. 2006;88:1952–1956. doi: 10.2106/JBJS.E.00890. [DOI] [PubMed] [Google Scholar]
- 51.Haraguchi K, Sugano N, Nishii T, Sakai T, Yoshikawa H, Ohzono K. Analysis of survivorship after total hip arthroplasty using a ceramic head. Clin Orthop Relat Res. 2001;391:198–209. doi: 10.1097/00003086-200110000-00022. [DOI] [PubMed] [Google Scholar]
- 52.Heilpern GN, Shah NN, Fordyce MJ. Birmingham hip resurfacing arthroplasty: a series of 110 consecutive hips with a minimum five-year clinical and radiological follow-up. J Bone Joint Surg Br. 2008;90:1137–1142. doi: 10.1302/0301-620X.90B9.20524. [DOI] [PubMed] [Google Scholar]
- 53.Herrera A, Canales V, Anderson J, Garcia-Araujo C, Murcia-Mazon A, Tonino AJ. Seven to 10 years followup of an anatomic hip prosthesis: an international study. Clin Orthop Relat Res. 2004;423:129–137. doi: 10.1097/01.blo.0000128973.73132.0b. [DOI] [PubMed] [Google Scholar]
- 54.Hing CB, Back DL, Bailey M, Young DA, Dalziel RE, Shimmin AJ. The results of primary Birmingham hip resurfacings at a mean of five years: an independent prospective review of the first 230 hips. J Bone Joint Surg Br. 2007;89:1431–1438. doi: 10.1302/0301-620X.89B11.19336. [DOI] [PubMed] [Google Scholar]
- 55.Horne G, Culliford N, Adams K, Devane P. Hybrid total hip replacement: outcome after a mean follow up of 10 years. ANZ J Surg. 2007;77:638–641. doi: 10.1111/j.1445-2197.2007.04177.x. [DOI] [PubMed] [Google Scholar]
- 56.Howie DW, McGee MA, Costi K, Graves SE. Metal-on-Metal Resurfacing versus total hip replacement: the value of a randomized clinical trial. Orthop Clin North Am. 2005;36:195–201. doi: 10.1016/j.ocl.2004.12.001. [DOI] [PubMed] [Google Scholar]
- 57.Hulleberg G, Aamodt A, Espehaug B, Benum P. A clinical and radiographic 13-year follow-up study of 138 Charnley hip arthroplasties in patients 50–70 years old: comparison of university hospital data and registry data. Acta Orthop. 2008;79:609–617. doi: 10.1080/17453670810016614. [DOI] [PubMed] [Google Scholar]
- 58.Illgen RL, Heiner JP, Squire MW, Conrad DN. Large-head metal-on-metal total hip arthroplasty using the Durom acetabular component at minimum 1-year interval. J Arthroplasty. 2010;25(6 suppl):26–30. doi: 10.1016/j.arth.2010.04.005. [DOI] [PubMed] [Google Scholar]
- 59.International Society of Arthroplasty Registers. International Society of Arthroplasty Registries Report (revised February 2007). Available at: http://www.isarhome.org/statements. Accessed March 7, 2013.
- 60.Isaac GH, Siebel T, Oakeshott RD, Lennan-Smith R, Cobb AG, Schmalzried TP, Vail TP. Changes in whole blood metal ion levels following resurfacing: serial measurements in a multi-centre study. Hip Int. 2009;19:330–337. doi: 10.1177/112070000901900406. [DOI] [PubMed] [Google Scholar]
- 61.Jacobs M, Gorab R, Mattingly D, Trick L, Southworth C. Three- to six-year results with the Ultima metal-on-metal hip articulation for primary total hip arthroplasty. J Arthroplasty. 2004;19(7 suppl 2):48–53. doi: 10.1016/j.arth.2004.06.021. [DOI] [PubMed] [Google Scholar]
- 62.Jameson SS, Langton DJ, Nargol AV. Articular surface replacement of the hip: a prospective single-surgeon series. J Bone Joint Surg Br. 2010;92:28–37. doi: 10.1302/0301-620X.92B1.22769. [DOI] [PubMed] [Google Scholar]
- 63.Jameson SS, Langton DJ, Natu S, Nargol TV. The influence of age and sex on early clinical results after hip resurfacing: an independent center analysis. J Arthroplasty. 2008;23(6 suppl 1):50–55. doi: 10.1016/j.arth.2008.03.019. [DOI] [PubMed] [Google Scholar]
- 64.Jiang J. Linear and Generalized Linear Mixed Models and Their Applications. New York, NY: Springer; 2007. [Google Scholar]
- 65.Jiang Y, Zhang K, Die J, Shi Z, Zhao H, Wang K. A systematic review of modern metal-on-metal total hip resurfacing vs standard total hip arthroplasty in active young patients. J Arthroplasty. 2011;26:419–426. doi: 10.1016/j.arth.2010.07.008. [DOI] [PubMed] [Google Scholar]
- 66.Kalairajah Y, Azurza K, Molloy S, Hulme C, Cronin M, Drabu KJ. Is the Charnley evolution working? A five-year outcome study. Acta Orthop Belg. 2004;70:315–321. [PubMed] [Google Scholar]
- 67.Khan M, Kuiper JH, Edwards D, Robinson E, Richardson JB. Birmingham hip arthroplasty: five to eight years of prospective multicenter results. J Arthroplasty. 2009;24:1044–1050. doi: 10.1016/j.arth.2008.07.016. [DOI] [PubMed] [Google Scholar]
- 68.Kim PR, Beaule PE, Dunbar M, Lee JK, Birkett N, Turner MC, Yenugadhati N, Armstrong V, Krewski D. Cobalt and chromium levels in blood and urine following hip resurfacing arthroplasty with the Conserve Plus implant. J Bone Joint Surg Am. 2011;93(suppl 2):107–117. doi: 10.2106/JBJS.J.01721. [DOI] [PubMed] [Google Scholar]
- 69.Kim PR, Beaule PE, Laflamme GY, Dunbar M. Causes of early failure in a multicenter clinical trial of hip resurfacing. J Arthroplasty. 2008;23(6 suppl 1):44–49. doi: 10.1016/j.arth.2008.05.022. [DOI] [PubMed] [Google Scholar]
- 70.Kim Y. Bilateral cemented and cementless total hip arthroplasty. J Arthroplasty. 2002;17:434–440. doi: 10.1054/arth.2002.31073. [DOI] [PubMed] [Google Scholar]
- 71.Kim YH. The results of a proximally-coated cementless femoral component in total hip replacement: a five- to 12-year follow-up. J Bone Joint Surg Br. 2008;90:299–305. doi: 10.1302/0301-620X.90B3.20096. [DOI] [PubMed] [Google Scholar]
- 72.Kim YH, Kim JS, Cho SH. Primary total hip arthroplasty with a cementless porous-coated anatomic total hip prosthesis: 10- to 12-year results of prospective and consecutive series. J Arthroplasty. 1999;14:538–548. doi: 10.1016/s0883-5403(99)90074-8. [DOI] [PubMed] [Google Scholar]
- 73.Kim YH, Kim JS, Park JW, Joo JH. Comparison of total hip replacement with and without cement in patients younger than 50 years of age: the results at 18 years. J Bone Joint Surg Br. 2011;93:449–455. doi: 10.1302/0301-620X.93B4.26149. [DOI] [PubMed] [Google Scholar]
- 74.Konstantoulakis C, Anastopoulos G, Papaeliou A, Tsoutsanis A, Asimakopoulos A. Uncemented total hip arthroplasty in the elderly. Int Orthop. 1999;23:334–336. doi: 10.1007/s002640050385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Korovessis P, Petsinis G, Repanti M. Zweymueller with metal-on-metal articulation: clinical, radiological and histological analysis of short-term results. Arch Orthop Trauma Surg. 2003;123:5–11. doi: 10.1007/s00402-002-0456-x. [DOI] [PubMed] [Google Scholar]
- 76.Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89:780–785. doi: 10.2106/JBJS.F.00222. [DOI] [PubMed] [Google Scholar]
- 77.Lachiewicz PF, Soileau ES. Dislocation of primary total hip arthroplasty with 36 and 40-mm femoral heads. Clin Orthop Relat Res. 2006;453:153–155. doi: 10.1097/01.blo.0000238851.31368.e7. [DOI] [PubMed] [Google Scholar]
- 78.Langdon IJ, Bannister GC. Cemented hip replacements in patients younger than 50 years: 16–24 year results. Hip Int. 1999;9:151–153. [Google Scholar]
- 79.Laupacis A, Bourne R, Rorabeck C, Feeny D, Tugwell P, Wong C. Comparison of total hip arthroplasty performed with and without cement: a randomized trial. J Bone Joint Surg Am. 2002;84:1823–1828. doi: 10.2106/00004623-200210000-00013. [DOI] [PubMed] [Google Scholar]
- 80.Lazennec JY, Boyer P, Poupon J, Rousseau MA, Roy C, Ravaud P, Catonne Y. Outcome and serum ion determination up to 11 years after implantation of a cemented metal-on-metal hip prosthesis. Acta Orthop. 2009;80:168–173. doi: 10.3109/17453670902947408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Long WT, Dorr LD, Gendelman V. An American experience with metal-on-metal total hip arthroplasties: a 7-year follow-up study. J Arthroplasty. 2004;19(8 suppl 3):29–34. doi: 10.1016/j.arth.2004.09.018. [DOI] [PubMed] [Google Scholar]
- 82.Lubbeke A, Stern R, Garavaglia G, Zurcher L, Hoffmeyer P. Differences in outcomes of obese women and men undergoing primary total hip arthroplasty. Arthritis Rheum. 2007;57:327–334. doi: 10.1002/art.22542. [DOI] [PubMed] [Google Scholar]
- 83.MacIntosh C. Metal-on metal hip implants more likely to need replacement. Available at: http://www.cbc.ca/news/health/metal-on-metal-hip-implants-more-likely-to-need-replacement-1.1330007. Accessed July 18, 2013.
- 84.Madhu TS, Akula MR, Raman RN, Sharma HK, Johnson VG. The Birmingham hip resurfacing prosthesis: an independent single surgeon’s experience at 7-year follow-up. J Arthroplasty. 2011;26:1–8. doi: 10.1016/j.arth.2009.10.010. [DOI] [PubMed] [Google Scholar]
- 85.Marulanda GA, Wilson MS, Edwards P, Raterman S. Early clinical experience with the use of the Birmingham hip resurfacing system. Orthopedics. 2008;31(12 suppl 2). pii: orthosupersite.com/view.asp?rID = 37184 [PubMed]
- 86.McAndrew AR, Khaleel A, Bloomfield MD, Aweid A. A district general hospital’s experience of hip resurfacing. Hip Int. 2007;17:1–3. doi: 10.1177/112070000701700101. [DOI] [PubMed] [Google Scholar]
- 87.McBryde CW, Revell MP, Thomas AM, Treacy RB, Pynsent PB. The influence of surgical approach on outcome in Birmingham hip resurfacing. Clin Orthop Relat Res. 2008;466:920–926. doi: 10.1007/s11999-008-0121-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.McGrath MS, Desser DR, Ulrich SD, Seyler TM, Marker DR, Mont MA. Total hip resurfacing in patients who are sixty years of age or older. J Bone Joint Surg Am. 2008;90(suppl 3):27–31. doi: 10.2106/JBJS.H.00464. [DOI] [PubMed] [Google Scholar]
- 89.McLaughlin JR, Lee KR. Total hip arthroplasty with an uncemented femoral component. Excellent results at ten-year follow-up. J Bone Joint Surg Br. 1997;79:900–907. doi: 10.1302/0301-620x.79b6.7482. [DOI] [PubMed] [Google Scholar]
- 90.McLaughlin JR, Lee KR. Total hip arthroplasty with an uncemented tapered femoral component in patients younger than 50 years. J Arthroplasty. 2011;26:9–15. doi: 10.1016/j.arth.2009.11.021. [DOI] [PubMed] [Google Scholar]
- 91.Meldrum RD, Maiers GP, Feinberg JR, Parr JA, Capello WN, Park JJ. Long-term outcome of surface replacement with comparison to an age- and time-matched primary total hip arthroplasty cohort. J Arthroplasty. 2008;23:1–9. doi: 10.1016/j.arth.2006.12.102. [DOI] [PubMed] [Google Scholar]
- 92.Mella-Sousa M, Aguilar-Cortes F, Bocanegra E, Domecq G, Moleon M. Mid-term results in total hip arthroplasty with the basic noncemented hip prosthesis. Orthopedics. 2001;24):1053–1056. [DOI] [PubMed]
- 93.Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group. Preferred reporting items for systematic reviews and meta‐analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. [DOI] [PMC free article] [PubMed]
- 94.Mont MA, Marker DR, Smith JM, Ulrich SD, McGrath MS. Resurfacing is comparable to total hip arthroplasty at short-term follow-up. Clin Orthop Relat Res. 2009;467:66–71. doi: 10.1007/s11999-008-0465-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Murray D, Grammatopoulos G, Pandit H, Gundle R, Gill H, McLardy-Smith P. The ten-year survival of the Birmingham hip resurfacing. J Bone Joint Surg Br. 2012;94:1180–1186. doi: 10.1302/0301-620X.94B9.29462. [DOI] [PubMed] [Google Scholar]
- 96.Nagi ON, Kumar S, Aggarwal S. The uncemented isoelastic/isotitan total hip arthroplasty: a 10–15 years follow-up with bone mineral density evaluation. Acta Orthop Belg. 2006;72:55–64. [PubMed] [Google Scholar]
- 97.Nakamura Y, Mitsui H, Kikuchi A, Toh S, Katano H. Total hip arthroplasty using a cylindrical cementless stem in patients with a small physique. J Arthroplasty. 2011;26:77–81. doi: 10.1016/j.arth.2009.10.014. [DOI] [PubMed] [Google Scholar]
- 98.National Joint Registry. National Joint Registry for England and Wales 8th Annual Report 2011. Available at: http://www.njrcentre.org.uk/njrcentre/portals/0/documents/njr%208th%20annual%20report%202011.pdf. Accessed January 30, 2014.
- 99.Nayak KN, Mulliken B, Rorabeck CH, Bourne RB, Woolfrey MR. Prevalence of heterotopic ossification in cemented versus noncemented total hip joint replacement in patients with osteoarthrosis: a randomized clinical trial. Can J Surg. 1997;40:368–374. [PMC free article] [PubMed] [Google Scholar]
- 100.Nercessian OA, Wu WH, Sarkissian H. Clinical and radiographic results of cementless AML total hip arthroplasty in young patients. J Arthroplasty. 2001;16:312–316. doi: 10.1054/arth.2001.21503. [DOI] [PubMed] [Google Scholar]
- 101.Neumann DR, Thaler C, Hitzl W, Huber M, Hofstadter T, Dorn U. Long-term results of a contemporary metal-on-metal total hip arthroplasty: a 10-year follow-up study. J Arthroplasty. 2010;25:700–708. doi: 10.1016/j.arth.2009.05.018. [DOI] [PubMed] [Google Scholar]
- 102.New Zealand Orthopaedic Association. The New Zealand Joint Registry Twelve Year Report: January 1999 to December 2010. Available at: http://nzoa.org.nz/system/files/NJR%2012%20Year%20Report%20Jan%2099%20-%20Dec%202010.pdf. Accessed February 5, 2014.
- 103.Nilsdotter AK, Isaksson F. Patient relevant outcome 7 years after total hip replacement for OA: a prospective study. BMC Musculoskelet Disord. 2010;11:47. doi: 10.1186/1471-2474-11-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Nilsdotter AK, Lohmander LS. Patient relevant outcomes after total hip replacement: a comparison between different surgical techniques. Health Qual Life Outcomes. 2003;1:21. doi: 10.1186/1477-7525-1-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Nilsdotter AK, Petersson IF, Roos EM, Lohmander LS. Predictors of patient relevant outcome after total hip replacement for osteoarthritis: a prospective study. Ann Rheum Dis. 2003;62:923–930. doi: 10.1136/ard.62.10.923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Ollivere B, Darrah C, Barker T, Nolan J, Porteous MJ. Early clinical failure of the Birmingham metal-on-metal hip resurfacing is associated with metallosis and soft-tissue necrosis. J Bone Joint Surg Br. 2009;91:1025–1030. doi: 10.1302/0301-620X.91B8.21701. [DOI] [PubMed] [Google Scholar]
- 107.Ollivere B, Darrah C, Brankin RC, Donell ST, Donnell ST, Walton NP. The continued value of clinical and radiological surveillance: the Charnley Elite Plus hip replacement system at 12 years. J Bone Joint Surg Br. 2009;91:720–724. doi: 10.1302/0301-620X.91B6.21417. [DOI] [PubMed] [Google Scholar]
- 108.Ollivere B, Duckett S, August A, Porteous M. The Birmingham Hip Resurfacing: 5-year clinical and radiographic results from a District General Hospital. Int Orthop. 2010;34:631–634. doi: 10.1007/s00264-009-0821-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Paleochorlidis IS, Badras LS, Skretas EF, Georgaklis VA, Karachalios TS, Malizos KN. Clinical outcome study and radiological findings of Zweymuller metal on metal total hip arthroplasty: a follow-up of 6 to 15 years. Hip Int. 2009;19:301–308. doi: 10.1177/112070000901900402. [DOI] [PubMed] [Google Scholar]
- 110.Parvizi J, Sullivan T, Duffy G, Cabanela ME. Fifteen-year clinical survivorship of Harris-Galante total hip arthroplasty. J Arthroplasty. 2004;19:672–677. doi: 10.1016/j.arth.2004.01.005. [DOI] [PubMed] [Google Scholar]
- 111.Pollard TC, Baker RP, Eastaugh-Waring SJ, Bannister GC. Treatment of the young active patient with osteoarthritis of the hip: a five- to seven-year comparison of hybrid total hip arthroplasty and metal-on-metal resurfacing. J Bone Joint Surg Br. 2006;88:592–600. doi: 10.1302/0301-620X.88B5.17354. [DOI] [PubMed] [Google Scholar]
- 112.Pritchett JW. Curved-stem hip resurfacing: minimum 20-year followup. Clin Orthop Relat Res. 2008;466:1177–1185. doi: 10.1007/s11999-008-0165-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Radcliffe GS, Wilson JI, Ashford RU, De Boer PG. Hip replacement in patients younger than 65 years: results of the CLS prosthesis. Hip Int. 2003;13:133–141. [Google Scholar]
- 114.Ragab AA, Kraay MJ, Goldberg VM. Clinical and radiographic outcomes of total hip arthroplasty with insertion of an anatomically designed femoral component without cement for the treatment of primary osteoarthritis: a study with a minimum of six years of follow-up. J Bone Joint Surg Am. 1999;81:208–210. doi: 10.2106/00004623-199902000-00008. [DOI] [PubMed] [Google Scholar]
- 115.Rahman L, Muirhead-Allwood SK, Alkinj M. What is the midterm survivorship and function after hip resurfacing? Clin Orthop Relat Res. 2010;468:3221–3227. doi: 10.1007/s11999-010-1438-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Richardson WS, Wilson MC, Nishikawa J, Hayward RS. The well-built clinical question: a key to evidence-based decisions. ACP J Club. 1995;123:A12–A13. [PubMed] [Google Scholar]
- 117.Ritter MA, Lutgring JD, Berend ME, Pierson JL. Failure mechanisms of total hip resurfacing: implications for the present. Clin Orthop Relat Res. 2006;453:110–114. doi: 10.1097/01.blo.0000238849.23744.8e. [DOI] [PubMed] [Google Scholar]
- 118.Russell RC, Ghassemi A, Dorrell JH, Powles DP. The Bimetric cementless total hip replacement: 7–18 year follow-up assessing the influence of acetabular design on survivorship. Int Orthop. 2009;33:933–937. doi: 10.1007/s00264-008-0592-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Saito S, Ishii T, Mori S, Hosaka K, Ootaki M, Tokuhashi Y. Long-term results of metasul metal-on-metal total hip arthroplasty. Orthopedics. 2010;33. doi: 10.3928/01477447-20100625-11 [DOI] [PubMed]
- 120.Saito S, Ishii T, Mori S, Hosaka K, Tokuhashi Y. The Harris-Galante cementless THA: a 19- to 25-year follow-up study. Orthopedics. 2011;34:12. doi: 10.3928/01477447-20101123-08. [DOI] [PubMed] [Google Scholar]
- 121.Schreiner U, Scheller G, Herbig J, Jani L. Mid-term results of the cementless CLS stem: a 7- to 11-year follow-up study. Arch Orthop Trauma Surg. 2001;121:321–324. doi: 10.1007/s004020000253. [DOI] [PubMed] [Google Scholar]
- 122.Sharma S, Vassan U, Bhamra MS. Metal-on-metal total hip joint replacement: a minimum follow-up of five years. Hip Int. 2007;17:70–77. doi: 10.1177/112070000701700203. [DOI] [PubMed] [Google Scholar]
- 123.Sinha RK, Dungy DS, Yeon HB. Primary total hip arthroplasty with a proximally porous-coated femoral stem. J Bone Joint Surg Am. 2004;86:1254–1261. doi: 10.2106/00004623-200406000-00019. [DOI] [PubMed] [Google Scholar]
- 124.Smith TO, Nichols R, Donell ST, Hing CB. The clinical and radiological outcomes of hip resurfacing versus total hip arthroplasty: a meta-analysis and systematic review. Acta Orthop. 2010;81:684–695. doi: 10.3109/17453674.2010.533933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Spencer S, Carter R, Murray H, Meek RM. Femoral neck narrowing after metal-on-metal hip resurfacing. J Arthroplasty. 2008;23:1105–1109. doi: 10.1016/j.arth.2007.10.014. [DOI] [PubMed] [Google Scholar]
- 126.Sporer SM, Callaghan JJ, Olejniczak JP, Goetz DD, Johnston RC. Hybrid total hip arthroplasty in patients under the age of fifty: a five- to ten-year follow-up. J Arthroplasty. 1998;13:485–491. doi: 10.1016/s0883-5403(98)90045-6. [DOI] [PubMed] [Google Scholar]
- 127.Springer BD, Connelly SE, Odum SM, Fehring TK, Griffin WL, Mason JB. Cementless femoral components in young patients: review and meta-analysis of total hip arthroplasty and hip resurfacing. J Arthroplasty. 2009;24(6 suppl):2–8. doi: 10.1016/j.arth.2009.04.032. [DOI] [PubMed] [Google Scholar]
- 128.Streit MR, Merle C, Clarius M, Aldinger PR. Late peri-prosthetic femoral fracture as a major mode of failure in uncemented primary hip replacement. J Bone Joint Surg Br. 2011;93:178–183. doi: 10.1302/0301-620X.93B2.24329. [DOI] [PubMed] [Google Scholar]
- 129.Stulberg BN, Trier KK, Naughton M, Zadzilka JD. Results and lessons learned from a United States hip resurfacing investigational device exemption trial. J Bone Joint Surg Am. 2008;90(suppl 3):21–26. doi: 10.2106/JBJS.H.00718. [DOI] [PubMed] [Google Scholar]
- 130.Tarasevicius S, Kesteris U, Robertsson O, Smailys A, Janusonis V, Wingstrand H. Introduction of total hip arthroplasty in Lithuania: results from the first 10 years. Acta Orthop. 2007;78:454–457. doi: 10.1080/17453670710014077. [DOI] [PubMed] [Google Scholar]
- 131.Theis JC, Beadel G. Changes in proximal femoral bone mineral density around a hydroxyapatite-coated hip joint arthroplasty. J Orthop Surg (Hong Kong). 2003;11:48–52. doi: 10.1177/230949900301100111. [DOI] [PubMed] [Google Scholar]
- 132.Tompkins GS, Jacobs JJ, Kull LR, Rosenberg AG, Galante JO. Primary total hip arthroplasty with a porous-coated acetabular component: seven-to-ten-year results. J Bone Joint Surg Am. 1997;79:169–176. doi: 10.2106/00004623-199702000-00002. [DOI] [PubMed] [Google Scholar]
- 133.Treacy RB, McBryde CW, Pynsent PB. Birmingham hip resurfacing arthroplasty: a minimum follow-up of five years. J Bone Joint Surg Br. 2005;87:167–170. doi: 10.1302/0301-620x.87b2.15030. [DOI] [PubMed] [Google Scholar]
- 134.Treacy RB, McBryde CW, Shears E, Pynsent PB. Birmingham hip resurfacing: a minimum follow-up of ten years. J Bone Joint Surg Br. 2011;93:27–33. doi: 10.1302/0301-620X.93B1.24134. [DOI] [PubMed] [Google Scholar]
- 135.Ulm K. A simple method to calculate the confidence interval of a standardized mortality ratio (SMR) Am J Epidemiol. 1990;131:373–375. doi: 10.1093/oxfordjournals.aje.a115507. [DOI] [PubMed] [Google Scholar]
- 136.van der Weegen W, Hoekstra HJ, Sijbesma T, Bos E, Schemitsch EH, Poolman RW. Survival of metal-on-metal hip resurfacing arthroplasty: a systematic review of the literature. J Bone Joint Surg Br. 2011;93:298–306. doi: 10.1302/0301-620X.93B3.25594. [DOI] [PubMed] [Google Scholar]
- 137.Vassan UT, Sharma S, Chowdary KP, Bhamra MS. Uncemented metal-on-metal acetabular component: follow-up of 112 hips for a minimum of 5 years. Acta Orthop. 2007;78:470–478. doi: 10.1080/17453670710014103. [DOI] [PubMed] [Google Scholar]
- 138.Vendittoli PA, Ganapathi M, Roy AG, Lusignan D, Lavigne M. A comparison of clinical results of hip resurfacing arthroplasty and 28 mm metal on metal total hip arthroplasty: a randomised trial with 3–6 years follow-up. Hip Int. 2010;20:1–13. doi: 10.1177/112070001002000101. [DOI] [PubMed] [Google Scholar]
- 139.Vendittoli PA, Lavigne M, Roy AG, Lusignan D. A prospective randomized clinical trial comparing metal-on-metal total hip arthroplasty and metal-on-metal total hip resurfacing in patients less than 65 years old. Hip Int. 2006;16(suppl 4):73–81. doi: 10.1177/112070000601604S14. [DOI] [PubMed] [Google Scholar]
- 140.Vendittoli PA, Mottard S, Roy AG, Dupont C, Lavigne M. Chromium and cobalt ion release following the Durom high carbon content, forged metal-on-metal surface replacement of the hip. J Bone Joint Surg Br. 2007;89:441–448. doi: 10.1302/0301-620X.89B4.18054. [DOI] [PubMed] [Google Scholar]
- 141.Vigler M, Greental A, Kaminsky AJ, Shauer L, Salai M, Soudry M. Early results of total hip replacement with the Metasul metal-on-metal cementless prosthesis. Bull NYU Hosp Jt Dis. 2010;68:11–14. [PubMed] [Google Scholar]
- 142.Witzleb WC, Arnold M, Krummenauer F, Knecht A, Ranisch H, Gunther KP. Birmingham Hip Resurfacing arthroplasty: short-term clinical and radiographic outcome. Eur J Med Res. 2008;13:39–46. [PubMed] [Google Scholar]
- 143.Wyness L, Vale L, McCormack K, Grant A, Brazzelli M. The effectiveness of metal on metal hip resurfacing: a systematic review of the available evidence published before 2002. BMC Health Serv Res. 2004;4:39. doi: 10.1186/1472-6963-4-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Xu WD, Chen G, Li J, Xu L, Liang ZM. Metal-to-metal hip surface arthroplasty in 63 cases: a follow-up assessment. J Clin Rehabil Tissue Eng Res. 2008;12:4373–4376. [Google Scholar]
- 145.Yang J, Shen B, Zhou Z, Pei F, Kang P. Changes in cobalt and chromium levels after metal-on-metal hip resurfacing in young, active Chinese patients. J Arthroplasty. 2011;26:65–70. doi: 10.1016/j.arth.2009.11.019. [DOI] [PubMed] [Google Scholar]
- 146.Yue EJ, Cabanela ME, Duffy GP, Heckman MG, O’Connor MI. Hip resurfacing arthroplasty: risk factors for failure over 25 years. Clin Orthop Relat Res. 2009;467:992–999. doi: 10.1007/s11999-008-0506-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Zywiel MG, Marker DR, McGrath MS, Delanois RE, Mont MA. Resurfacing matched to standard total hip arthroplasty by preoperative activity levels: a comparison of postoperative outcomes. Bull NYU Hosp Jt Dis. 2009;67:116–119. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.