Abstract
Background
When treating complex radial head fractures, important goals include prevention of elbow or forearm instability, with restoration of radiocapitellar contact essential. When open reduction and internal fixation cannot achieve this, radial head replacement is routinely employed, but the frequency of and risk factors for prosthesis revision or removal are not well defined.
Questions/purposes
We determined (1) the frequency of prosthesis revision or removal after radial head replacement for acute complex unstable radial head fractures, (2) risk factors for revision or removal, and (3) functional outcomes after radial head replacement.
Methods
We identified from our prospective trauma database all patients over a 16-year period managed acutely for unstable complex radial head fractures with primary radial head replacement. Of the 119 patients identified, 105 (88%) met our inclusion criteria; mean age was 50 years (range, 16–93 years) and 57 (54%) were female. All implants were uncemented monopolar prostheses, of which 86% were metallic and 14% silastic. We recorded further procedures for prosthesis revision or removal for any cause, with a minimum followup of 1 year (n = 105). Cox regression analysis was used to determine independent factors associated with revision or removal when controlling for baseline patient (age, sex, comorbidities) and fracture (location, classification, associated injury) characteristics. Short-term functional outcomes (Broberg and Morrey score, ROM) were determined from retrospective review of clinic followup (n = 74), with a minimum followup of 3 months.
Results
Twenty-nine patients (28%) underwent prosthesis revision (n = 3) or removal (n = 26) at a mean of 6.7 years (range, 1.8–18 years) after injury. Independent risk factors for removal or revision were silastic implant type and lower age. At a mean of 1.1 years (range, 0.3–5.5 years) after surgery, mean Broberg and Morrey score was 80 out of 100 (range, 40–99). Mean elbow flexion was 133° (range, 90°–159°; SD, 13°), extension 21° (range, 0°–80°; SD, 17°), flexion arc 112° (range, 10°–140°; SD, 25°), pronation 84° (range, 0°–90°; SD, 18°), supination 73° (range, 0°–90°; SD, 28°), and forearm rotation arc 156° (range, 0°–180°; SD, 38°).
Conclusions
We demonstrated a high removal or revision rate after radial head replacement for acute unstable complex fractures, with lower age and silastic implants independent risk factors. Younger patients should be counseled regarding the increased risk of requiring further surgery after radial head replacement. Future work should focus on long-term patient-reported outcomes after these injuries.
Level of Evidence
Level IV, therapeutic study. See Instructions for Authors for a complete description of levels of evidence.
Introduction
Unstable fractures of the radial head commonly occur as part of a complex injury pattern, have fragments that are detached and mobile with little or no soft tissue attachments, and are associated with osseous and ligamentous injuries to the elbow or forearm [14]. The primary goal of treatment is to prevent dislocation or subluxation of the elbow and forearm, with restoration of the radiocapitellar contact essential for alignment and stability [8, 36]. When these fractures are not associated with elbow or forearm instability, partial or complete radial head excision is an option [1, 4, 20, 21, 23], although in most cases when instability is present, other options include internal fixation [10, 22, 24, 38, 45] or prosthetic replacement [2, 6, 9, 13, 18, 32, 46].
Two recent prospective randomized trials have demonstrated superior results for replacement over open reduction and internal fixation (ORIF) for unstable complex fractures [9, 39], with several studies finding ORIF to be associated with increased rates of early failure and nonunion and one study determining three fracture fragments as the cutoff point for progressing to replacement [11, 25, 27, 38]. A variety of replacement designs are available, with comparable short- to mid-term clinical results documented for cemented bipolar implants and loose spacers [6, 13, 18, 29]. However, the frequency of and risk factors associated with further surgery for removal and/or revision after this procedure remain incompletely characterized [14, 43].
We therefore determined (1) the frequency of prosthesis removal or revision after radial head replacement for acute complex unstable radial head fractures (primary study outcome), (2) the factors associated with revision or removal of the prosthesis, and (3) the short-term functional outcome after injury (secondary outcome measures).
Patients and Methods
Study Cohort
We performed a retrospective search of a prospective trauma database held at our study center to identify all skeletally mature patients who were managed acutely with a primary radial head replacement for an unstable complex fracture of the radial head over a 16-year period between September 1994 and September 2010. A total of 119 patients were identified (Fig. 1), of which there were 63 females (53%) and 56 males (47%), with a mean age of 50 years (range, 15–93 years; SD, 19 years). Patients were excluded if there was inadequate demographic, fracture characteristic, management, or followup data, including no further record of followup at our institution (n = 8), or if they were from outside our local catchment population (n = 6). Our primary outcome measure was revision or removal of the prosthesis for any reason, with the minimum time from surgery 1 year. All patients needed to be registered at our institution for ongoing medical care with other specialties at the time of the study or have been reviewed within the past year at our institution. Our secondary outcome measure was short-term functional assessment, with the minimum time from surgery 3 months. Fourteen patients did not meet the inclusion criteria and were excluded, leaving 105 (88%) patients who were defined as our study cohort for analysis.
Fig. 1.
A flowchart that demonstrates the patient selection process.
We retrospectively reviewed medical case notes and our trauma database to document demographic data including age, sex, mode of injury, and medical comorbidities. Diagnosis and associated injuries were recorded through medical record and radiographic review. Initial radiographs were reviewed where available (n = 66, 63%) to confirm fracture classification and the presence of an associated fracture and/or subluxation/dislocation of the elbow. All fractures were assessed using standard AP and lateral radiographs of the injured elbow and were subsequently classified according to the modified Mason fracture classification system [5]. Further imaging was performed at the discretion of the treating surgeon. Associated injuries were defined as those found on radiographic imaging or at the time of surgery requiring repair.
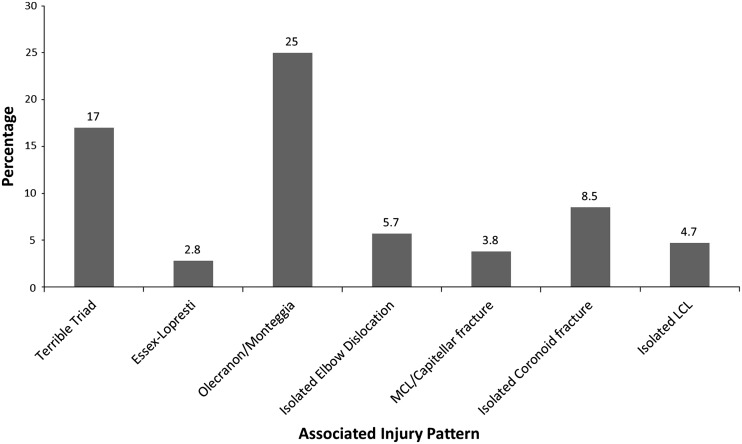
Of the 105 patients in our cohort, there were 57 females (54%) and 48 males (46%), with a mean age was 50 years (range, 16–93 years; SD, 19 years). The mean age at the time of injury was higher (p < 0.001) in females (57 years; range, 16–93 years; SD, 18 years) than in males (40 years; range, 18–81 years; SD, 16 years). One or more comorbidities were documented in 52 patients (50%). The most frequent mechanism of injury was a fall from standing height (n = 57, 54%), followed by a fall from greater than standing height (n = 26, 25%), motor vehicle collision (n = 11, 10.5%), assault (n = 4, 3.8%), sports (n = 4, 3.8%), and other (n = 3, 2.9%). Females most commonly sustained their fractures after a fall from standing height, while males most commonly sustained high-energy injuries, eg, falls from greater than standing height or motor vehicle collisions (p < 0.001). There were 95 (91%) radial head fractures and 10 (9%) radial neck fractures. Four patients (3.8%) had fractures classified as Mason Type 2 (radial head: n = 4; radial neck: n = 0), 88 (84%) Mason Type 3 (radial head: n = 78; radial neck: n = 10), and 13 (12.4%) Mason Type 4 (radial head: n = 13; radial neck: n = 0). There were 98 associated injuries documented in 70 patients (66%) (Fig. 2).
Fig. 2.
A graph that details the associated injury patterns. MCL = medial collateral ligament.
There were 26 patients with an associated elbow dislocation, with 18 of these being a terrible triad type injury and two having an associated fracture of the proximal ulna. There were 24 patients with an associated fracture of the proximal ulna (excluding coronoid). There were 11 patients with an isolated fracture of the coronoid. Three patients had an Essex-Lopresti type injury. There were no differences between the included and excluded cohorts in terms of age (p = 0.99), sex (p = 0.42), mechanism of injury (p = 0.18), comorbidities (p = 0.30), fracture classification (p = 0.34), or fracture location (p = 0.22).
Management
During the study period, multiple surgeons were involved in the care of these patients and the absolute indications for surgery varied. However, our general indications for operative intervention were a confirmed mechanical block to forearm rotation or severe displacement or comminution of the fracture associated with instability of the elbow or forearm. ORIF was performed when it was believed the fracture could be reconstructed, with replacement otherwise performed. Radial head resection was performed without replacement if the radial head was removed and there was no concern over associated elbow or forearm instability.
We recorded the details of operative management, complications, and subsequent surgical procedures. Initial management, surgical technique, and postoperative rehabilitation were determined in all cases by the supervising surgeons, all of whom were experienced consultant orthopaedic trauma surgeons. The median time to surgery after injury was 3 days (range, 0–20 days).
Patients were placed in the supine position with the arm supported on a hand table, unless there was an associated olecranon fracture when the patient was routinely placed in the lateral decubitus position with the arm over a bolster. For approaching the radial head, a standard lateral operative exposure of the radial head using the Kocher interval between the extensor carpi ulnaris and anconeus was routinely employed. We often found that the exposure was simplified by mobilizing the lateral collateral ligament (LCL) and extensor digitorum communis, as they had been avulsed from their origins on the lateral epicondyle. Otherwise, care was taken not to damage the lateral ligamentous complex (if not already injured) and to avoid elevation of the anconeus. When dissection was required distally down the neck, care was taken to protect the posterior interosseous nerve by pronating the forearm [12]. Inspection of the coronoid was routinely performed.
Radial head fracture fragments were removed and used to determine the size of the radial head prosthesis. The radial neck was prepared and a trial reduction performed to ensure the radiocapitellar joint was not overstuffed. The radial head prosthesis was then inserted (Fig. 3). All radial head implants were loose monoblock prostheses, with 90 (86%) smooth metal and 15 (14%) silastic. Two implants were inserted with cement as the prosthesis was not adequately captured by the radial neck and at risk of dislocation.
Fig. 3.
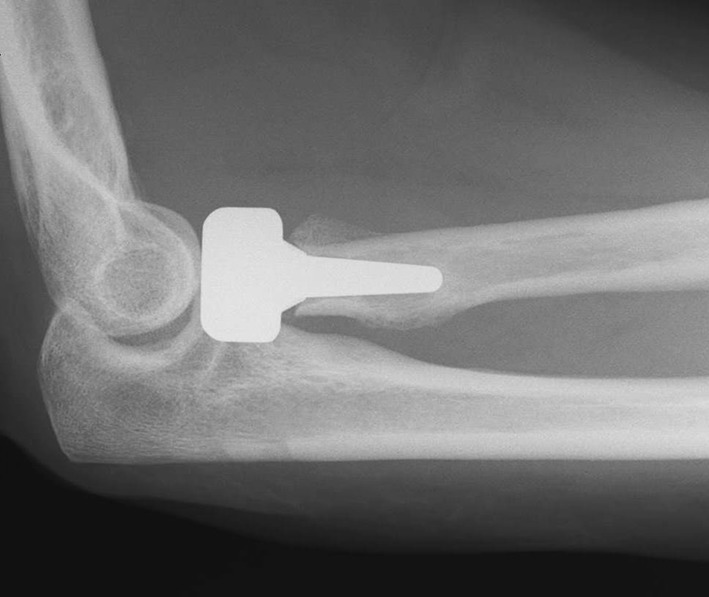
A radiograph shows a metal monoblock radial head replacement. The prosthesis appears large and the joint overstuffed.
The LCL generally was repaired using either sutures placed through drill holes in the lateral epicondyle (n = 24) or using suture anchors (n = 7). The medial collateral ligament was not explored unless the elbow was persistently unstable after replacement and repair of the coronoid with or without the LCL. The coronoid was repaired when it was more than a small avulsion fragment, displaced, and/or necessary for elbow stability, with 29 repaired using sutures placed through drill holes in the proximal ulna and two fixed with screws. Injuries associated with a proximal ulna fracture underwent ORIF through a posterior midline incision. The ulnar nerve was identified and released when indicated but was not routinely transposed. For managing terrible triad injuries, as routine we would use the protocol laid out by Pugh et al. [33]. The coronoid was inspected in all cases to ensure there was no occult injury. A thorough examination of the elbow was performed to test for instability in flexion-extension and varus-valgus.
Postoperatively, patients were immobilized for a period of 2 to 3 weeks and then began active motion exercises. Postoperative physiotherapy was employed for any residual functional deficit and/or elbow stiffness. It is not routine at our institution to remove a radial head prosthesis unless clinically indicated.
Followup and Outcomes
All assessment was performed at our institution, which is the only provider of orthopaedic trauma care throughout the region. The primary outcome measure was revision or removal of the radial head prosthesis for any cause. The minimum time from surgery was 1 year. To determine whether the patient had undergone revision of removal of the prosthesis, the last medical record entry was used. Details of subsequent complications and the requirement for secondary intervention were recorded when encountered. If no further intervention was documented, the followup point was taken as the time of medical note review.
Functional assessment was our secondary outcome measure, using the details from the treating surgeons entry at the last clinic followup when available with a minimum of 3 months’ followup included (n = 74). Outcome at this stage included ROM and Broberg and Morrey score [4, 5]. The 100-point Broberg and Morrey system compromises motion (40 points), strength (20 points), stability (5 points), and pain (35 points). Pain is rated as absent (35 points), mild with activity but requiring no medication (28 points), moderate with or after activity (15 points), or disabling pain that is severe at rest and requires constant medication (0 points). Categorical ratings are assigned according to the score achieved: excellent, 95 to 100 points; good, 80 to 94 points; fair, 60 to 70 points; and poor, less than 60 points.
Statistical Methods
A Student’s unpaired t-test was employed to analyze parametric continuous data. The Mann-Whitney U test was used to compare nonparametric continuous data. A one-way ANOVA was used to compare parametric continuous data among several categories, with the Kruskal-Wallis test being used for nonparametric data. Categorical binary data were analyzed using either the chi-square test (all observed frequencies in each cell > 5) or the Fisher’s exact test (one cell had an observed frequency of ≤ 5).
Cox regression analysis was used to determine independent factors associated with revision or removal of the prosthesis when controlling for baseline patient (age, sex, comorbidities) and fracture (fracture location, fracture classification, associated injury) characteristics. Two-tailed p values were reported and statistical significance was set at p values of less than 0.05, with 95% CIs presented.
Results
Failures
By a mean of 6.7 years after injury (range, 1.8–18 years; SD, 3.9 years), 29 patients (28%) had undergone revision (n = 3) or removal (n = 26) of the prosthesis. The median time to secondary surgery was 7 months (range, 0–65 months). Within the first year postsurgery, 21 patients (20%) had undergone revision (n = 3) or removal (n = 18) of the prosthesis. The three patients who underwent revision were for persistent subluxation of the radial head, with one associated with an inappropriately size prosthesis. The most common reason for removal was persistent stiffness with or without pain (n = 12, 41%), followed by prosthetic loosening (n = 5, 17%) (Table 1). Five patients underwent arthrolysis for persistent stiffness. Two patients underwent ulnar nerve decompression and transposition for persistent ulnar neuritis.
Table 1.
Reason for revision or removal of the radial head prosthesis in 29 patients
| Reason for revision or removal of the prosthesis | Number of patients (% of 105 patients) |
|---|---|
| Stiffness ± pain | 12 (11.4) |
| Painful loosening | 5 (4.8) |
| Pain alone | 4 (3.8) |
| Radial head subluxation | 3 (2.9) |
| Synovitis | 2 (1.9) |
| Ulnar neuritis | 2 (1.9) |
| Deep infection | 1 (1.0) |
Risk Factors for Failure
Cox regression analysis found two independent predictors of revision or removal of the implant after adjusting for confounding variables: silastic implant type (p = 0.004) and lower age (p = 0.002). Silastic implants had a higher removal rate (60% versus 22%) than metallic implants (odds ratio, 5.25; 95% CI, 1.67–16.52; p = 0.002). The mean age of patients undergoing further surgery (45 years; range, 16–81 years; SD, 19.1 years) was lower than that of patients who did not undergo further surgery (52 years; range, 17–93 years; SD, 18.9 years; p = 0.10).
On subanalysis of the metallic implants alone (n = 90), when controlling for other factors using Cox regression analysis, lower age (p = 0.001) and the absence of preexisting comorbidities (p = 0.014) were independent predictors of removal or revision. The mean age of patients undergoing further surgery (45 years; range, 18–69 years; SD, 17 years) was lower than that of patients who did not undergo further surgery (52 years; range, 17–93 years; SD, 19 years; p = 0.11).
Short-term Functional Outcomes
At a mean short-term followup of 1.1 years (range, 0.3–5.5 years; SD, 1 years) after surgery, the mean Broberg and Morrey score was 80 (range, 40–99; SD, 12), with 43 of 74 patients (58%) achieving an excellent (n = 4) or good (n = 39) outcome. However, 26 patients had a fair outcome and five a poor outcome. The mean elbow flexion was 133° (range, 90°–159°; SD, 13°), the mean extension was 21° (range, 0°–80°; SD, 17°), and the mean flexion arc was 112° (range, 10°–140°; SD, 25°). The mean pronation was 84° (range, 0°–90°; SD, 18°), the mean supination was 73° (range, 0°–90°; SD, 28.°), and the mean forearm rotation arc was 156° (range, 0°–180°; SD, 38°).
Discussion
For the majority of complex radial head fractures, restoration of radiocapitellar contact is essential and the choice is between radial head fixation [10, 15, 22, 24, 25, 38, 45] and replacement [2, 6, 13, 18, 32], with recent data from prospective randomized trials suggesting replacement is superior [9, 39]. There is good short- and mid-term data supporting metal and pyrocarbon prostheses [6, 10, 13, 18, 32, 35, 46]; however, the reoperation rates after radial head replacement are largely unknown. We demonstrated a high rate of removal or revision for both metallic and silastic implants, with silastic implants and younger patients being at the greatest risk of requiring further surgery for revision or removal. Our data provide useful prognostic information for both the patient and the surgeon managing these complex injuries.
Undoubtedly, the primary limitation of our study is the retrospective design, along with the variable followup times of patients over both the short and longer terms that can lead to both over- and underestimating the benefits of replacement. Specific problems with our retrospective design include multiple surgeons over a long period involved in both the management and postoperative assessment of the patient, which can lead to both selection and assessor bias along with an evolving management protocol over time. The subjective nature of prosthesis removal is noted and it could be argued that our findings are most applicable to our practice, although we believe our data provide valuable prognostic information for all surgeons managing these injuries. We acknowledge that some would argue that using no further intervention as our primary outcome measure is limited, as patients may have gone to another hospital for treatment. However, we are the only orthopaedic trauma service for the local population, patients were still registered and/or undergone recent review for other medical complaints at the time of retrospective note review, and all patients from outside our catchment area were excluded. Although a minimum of 3 months is short for functional followup, we acknowledge our data are short term and the literature has suggested that most patients regain the majority of their function within 3 to 6 months after injury [16]. The type and number of associated injuries are difficult to determine accurately using retrospective review, as they are dependent on the treating surgeon clearly documenting the presence and management, especially in the absence of the original imaging. The number of radiographs available was satisfactory, given our regional policy of culling hard-copy radiographs older than 5 years when the patient is not under regular clinical assessment. The frequency of associated injuries was probably underestimated from our series, given our strict definition for classifying associated injuries and the lack of further imaging in all patients.
The primary strength of our study is that we have reported on a large cohort of patients undergoing acute radial replacement for a complex fracture of the radial head, in contrast to other studies that include a heterogeneous cohort of acute and chronic radial head replacements and a range of differing implant types [43]. We have documented mid- to long-term followup from a defined population, with only one center providing an acute musculoskeletal trauma service for the region.
We have reported a high rate of revision or removal for radial head prostheses used in the management of acute complex fractures of the radial head, although the rate in the literature is both wide ranging (0%–32%) and unclear [13, 18, 19, 29]. Our overall rate of 28%, with a rate of 22% for metal prostheses, is in keeping with Doornberg et al. [13] who reported a rate of 32% at a mean of 40 months postsurgery using a modular metal spacer. Harrington et al. [19] reported a removal rate of 20% at a mean of 12 years after metal radial head replacement for unstable elbow fractures, with removal having no correlation to outcome. The exact cause for the variable rates in the literature is unclear, but we would suggest this is likely multifactorial with important factors including surgeon preference, patient and injury characteristics, the type of prostheses used, and most importantly the length of followup. We found the most common cause for revision or removal of the prosthesis was persistent stiffness, followed by unexplained and prosthetic loosening, which is consistent with other studies [3, 40, 43]. Persistent pain can be associated with radiographic loosening [31, 43], although our study, along with others, found this to affect a small number of patients when the prostheses are intentionally loose [13, 37]. Other noted complications associated with removal of the prosthesis include neuritis, deep infection, or persistent instability (subluxation/dislocation), which were all observed in our series [7, 13, 18, 19, 26].
To our knowledge, this is the first study to identify independent factors associated with prosthesis revision or removal. One study reported that a delay in surgery after injury (> 1 week) was associated with a reduced ROM and associated complications [43]. Interestingly, we found that younger patients were more likely to require further surgery for removal or revision. We would suggest that the threshold for progressing to implant removal and further surgery for stiffness is likely reduced in younger patients with higher functional demands. Younger patients should be counseled regarding the increased risk of further surgery being required. Silicone was the first radial head prosthetic replacement to be marketed but has since been found to be associated with fragmentation and destructive synovitis [17, 28, 30, 34, 41, 42, 44]. These studies are consistent with our findings that demonstrated silicone implants were associated with an increased rate of complications leading to an increased rate of removal or revision.
Our reported short-term outcome scores and ROM are similar to those of previous studies [13, 18, 19, 29], with an overall satisfactory outcome reported after the use of a loose metallic radial head spacer. Grewal et al. [18] reported mean elbow flexion of 138° and elbow extension of 25° at 2 years postinjury, with a large majority of this recovery occurring within the first 6 months after injury. We found that almost ½ of the patients in our series had a poor or fair short-term outcome, which is probably related to the short followup and the overall severity of these injuries [43]. Harrington et al. [19] found that 80% of patients had attained an excellent or good outcome at a mean of 12 years after injury. This would suggest that patients can expect ongoing improvement even several years after their injury.
To our knowledge, this is the largest reported series in the literature documenting the rate and risk factors associated with revision or removal of radial head replacement for acute complex unstable fractures of the radial head. We documented a satisfactory short-term functional outcome despite the severity of these injuries; however, there was a high rate of removal or revision of radial head replacements, especially in younger patients and those with silastic implants. Our data allow younger patients to be counseled regarding the increased risk of requiring further surgery after radial head replacement. We are unable to comment on the long-term functional and radiographic outcomes of these injuries, including patient-reported outcomes and the rate of osteoarthritis, and this should be an area of future research.
Acknowledgments
We thank the Scottish Orthopaedic Research Trust into Trauma for their assistance in performing this study.
Footnotes
Each author certifies that he or she, or a member of his or her immediate family, has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research ® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA approval status, of any drug or device before clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Antuna SA, Sanchez-Marquez JM, Barco R. Long-term results of radial head resection following isolated radial head fractures in patients younger than forty years old. J Bone Joint Surg Am. 2010;92:558–566. doi: 10.2106/JBJS.I.00332. [DOI] [PubMed] [Google Scholar]
- 2.Ashwood N, Bain GI, Unni R. Management of Mason type-III radial head fractures with a titanium prosthesis, ligament repair, and early mobilization. J Bone Joint Surg Am. 2004;86:274–280. doi: 10.2106/00004623-200402000-00009. [DOI] [PubMed] [Google Scholar]
- 3.Birkedal JP, Deal DN, Ruch DS. Loss of flexion after radial head replacement. J Shoulder Elbow Surg. 2004;13:208–213. doi: 10.1016/j.jse.2003.11.007. [DOI] [PubMed] [Google Scholar]
- 4.Broberg MA, Morrey BF. Results of delayed excision of the radial head after fracture. J Bone Joint Surg Am. 1986;68:669–674. [PubMed] [Google Scholar]
- 5.Broberg MA, Morrey BF. Results of treatment of fracture-dislocations of the elbow. Clin Orthop Relat Res. 1987;216:109–119. [PubMed] [Google Scholar]
- 6.Burkhart KJ, Mattyasovszky SG, Runkel M, Schwarz C, Kuchle R, Hessmann MH, Rommens PM, Lars MP. Mid- to long-term results after bipolar radial head arthroplasty. J Shoulder Elbow Surg. 2010;19:965–972. doi: 10.1016/j.jse.2010.05.022. [DOI] [PubMed] [Google Scholar]
- 7.Butler MA, Holt GE, Crosby SN, Weikert DR. Late posterior interosseous nerve palsy associated with loosening of radial head implant. J Shoulder Elbow Surg. 2009;18:e17–e21. doi: 10.1016/j.jse.2009.03.007. [DOI] [PubMed] [Google Scholar]
- 8.Charalambous CP, Stanley JK, Mills SP, Hayton MJ, Hearnden A, Trail I, Gagey O. Comminuted radial head fractures: aspects of current management. J Shoulder Elbow Surg. 2011;20:996–1007. doi: 10.1016/j.jse.2011.02.013. [DOI] [PubMed] [Google Scholar]
- 9.Chen X, Wang SC, Cao LH, Yang GQ, Li M, Su JC. Comparison between radial head replacement and open reduction and internal fixation in clinical treatment of unstable, multi-fragmented radial head fractures. Int Orthop. 2011;35:1071–1076. doi: 10.1007/s00264-010-1107-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Clembosky G, Boretto JG. Open reduction and internal fixation versus prosthetic replacement for complex fractures of the radial head. J Hand Surg Am. 2009;34:1120–1123. doi: 10.1016/j.jhsa.2008.12.031. [DOI] [PubMed] [Google Scholar]
- 11.Davidson PA, Moseley JB, Jr, Tullos HS. Radial head fracture: a potentially complex injury. Clin Orthop Relat Res. 1993;297:224–230. [PubMed] [Google Scholar]
- 12.Diliberti T, Botte MJ, Abrams RA. Anatomical considerations regarding the posterior interosseous nerve during posterolateral approaches to the proximal part of the radius. J Bone Joint Surg Am. 2000;82:809–813. doi: 10.2106/00004623-200006000-00007. [DOI] [PubMed] [Google Scholar]
- 13.Doornberg JN, Parisien R, van Duijn PJ, Ring D. Radial head arthroplasty with a modular metal spacer to treat acute traumatic elbow instability. J Bone Joint Surg Am. 2007;89:1075–1080. doi: 10.2106/JBJS.E.01340. [DOI] [PubMed] [Google Scholar]
- 14.Duckworth AD, McQueen MM, Ring D. Fractures of the radial head. Bone Joint J. 2013;95:151–159. doi: 10.1302/0301-620X.95B2.29877. [DOI] [PubMed] [Google Scholar]
- 15.Esser RD, Davis S, Taavao T. Fractures of the radial head treated by internal fixation: late results in 26 cases. J Orthop Trauma. 1995;9:318–323. doi: 10.1097/00005131-199509040-00008. [DOI] [PubMed] [Google Scholar]
- 16.Giannicola G, Polimanti D, Bullitta G, Sacchetti FM, Cinotti G. Critical time period for recovery of functional range of motion after surgical treatment of complex elbow instability: prospective study on 76 patients. Injury. 2013;pii: S0020-1383(13)00571-8. [DOI] [PubMed]
- 17.Gordon M, Bullough PG. Synovial and osseous inflammation in failed silicone-rubber prostheses. J Bone Joint Surg Am. 1982;64:574–580. [PubMed] [Google Scholar]
- 18.Grewal R, MacDermid JC, Faber KJ, Drosdowech DS, King GJ. Comminuted radial head fractures treated with a modular metallic radial head arthroplasty: study of outcomes. J Bone Joint Surg Am. 2006;88:2192–2200. doi: 10.2106/JBJS.E.00962. [DOI] [PubMed] [Google Scholar]
- 19.Harrington IJ, Sekyi-Otu A, Barrington TW, Evans DC, Tuli V. The functional outcome with metallic radial head implants in the treatment of unstable elbow fractures: a long-term review. J Trauma. 2001;50:46–52. doi: 10.1097/00005373-200101000-00009. [DOI] [PubMed] [Google Scholar]
- 20.Herbertsson P, Josefsson PO, Hasserius R, Besjakov J, Nyqvist F, Karlsson MK. Fractures of the radial head and neck treated with radial head excision. J Bone Joint Surg Am. 2004;86:1925–1930. doi: 10.2106/00004623-200409000-00010. [DOI] [PubMed] [Google Scholar]
- 21.Iftimie PP, Calmet Garcia J, de Loyola Garcia Forcada I, Gonzalez Pedrouzo JE, Gine Goma J. Resection arthroplasty for radial head fractures: long-term follow-up. J Shoulder Elbow Surg. 2011;20:45–50. [DOI] [PubMed]
- 22.Ikeda M, Yamashina Y, Kamimoto M, Oka Y. Open reduction and internal fixation of comminuted fractures of the radial head using low-profile mini-plates. J Bone Joint Surg Br. 2003;85:1040–1044. doi: 10.1302/0301-620X.85B7.13823. [DOI] [PubMed] [Google Scholar]
- 23.Janssen RP, Vegter J. Resection of the radial head after Mason type-III fractures of the elbow: follow-up at 16 to 30 years. J Bone Joint Surg Br. 1998;80:231–233. doi: 10.1302/0301-620X.80B2.8255. [DOI] [PubMed] [Google Scholar]
- 24.Khalfayan EE, Culp RW, Alexander AH. Mason type II radial head fractures: operative versus nonoperative treatment. J Orthop Trauma. 1992;6:283–289. doi: 10.1097/00005131-199209000-00003. [DOI] [PubMed] [Google Scholar]
- 25.King GJ, Evans DC, Kellam JF. Open reduction and internal fixation of radial head fractures. J Orthop Trauma. 1991;5:21–28. doi: 10.1097/00005131-199103000-00004. [DOI] [PubMed] [Google Scholar]
- 26.Knight DJ, Rymaszewski LA, Amis AA, Miller JH. Primary replacement of the fractured radial head with a metal prosthesis. J Bone Joint Surg Br. 1993;75:572–576. doi: 10.1302/0301-620X.75B4.8331111. [DOI] [PubMed] [Google Scholar]
- 27.Lindenhovius AL, Felsch Q, Doornberg JN, Ring D, Kloen P. Open reduction and internal fixation compared with excision for unstable displaced fractures of the radial head. J Hand Surg Am. 2007;32:630–636. doi: 10.1016/j.jhsa.2007.02.016. [DOI] [PubMed] [Google Scholar]
- 28.Mayhall WS, Tiley FT, Paluska DJ. Fracture of silastic radial-head prosthesis: case report. J Bone Joint Surg Am. 1981;63:459–460. [PubMed] [Google Scholar]
- 29.Moro JK, Werier J, MacDermid JC, Patterson SD, King GJ. Arthroplasty with a metal radial head for unreconstructible fractures of the radial head. J Bone Joint Surg Am. 2001;83:1201–1211. doi: 10.2106/00004623-200108000-00010. [DOI] [PubMed] [Google Scholar]
- 30.Morrey BF, Askew L, Chao EY. Silastic prosthetic replacement for the radial head. J Bone Joint Surg Am. 1981;63:454–458. [PubMed] [Google Scholar]
- 31.O’Driscoll SW, Herald JA. Forearm pain associated with loose radial head prostheses. J Shoulder Elbow Surg. 2012;21:92–97. doi: 10.1016/j.jse.2011.05.008. [DOI] [PubMed] [Google Scholar]
- 32.Popovic N, Lemaire R, Georis P, Gillet P. Midterm results with a bipolar radial head prosthesis: radiographic evidence of loosening at the bone-cement interface. J Bone Joint Surg Am. 2007;89:2469–2476. doi: 10.2106/JBJS.F.00723. [DOI] [PubMed] [Google Scholar]
- 33.Pugh DM, Wild LM, Schemitsch EH, King GJ, McKee MD. Standard surgical protocol to treat elbow dislocations with radial head and coronoid fractures. J Bone Joint Surg Am. 2004;86:1122–1130. doi: 10.2106/00004623-200406000-00002. [DOI] [PubMed] [Google Scholar]
- 34.Pugliese D, Bush D, Harrington T. Silicone synovitis: longer term outcome data and review of the literature. J Clin Rheumatol. 2009;15:8–11. doi: 10.1097/RHU.0b013e318190f979. [DOI] [PubMed] [Google Scholar]
- 35.Ricon FJ, Sanchez P, Lajara F, Galan A, Lozano JA, Guerado E. Result of a pyrocarbon prosthesis after comminuted and unreconstructable radial head fractures. J Shoulder Elbow Surg. 2012;21:82–91. doi: 10.1016/j.jse.2011.01.032. [DOI] [PubMed] [Google Scholar]
- 36.Ring D. Radial head fracture: open reduction-internal fixation or prosthetic replacement. J Shoulder Elbow Surg. 2011;20:S107–S112. doi: 10.1016/j.jse.2010.11.011. [DOI] [PubMed] [Google Scholar]
- 37.Ring D, King G. Radial head arthroplasty with a modular metal spacer to treat acute traumatic elbow instability: surgical technique. J Bone Joint Surg Am. 2008;90(suppl 2 pt 1):63–73. doi: 10.2106/JBJS.G.01248. [DOI] [PubMed] [Google Scholar]
- 38.Ring D, Quintero J, Jupiter JB. Open reduction and internal fixation of fractures of the radial head. J Bone Joint Surg Am. 2002;84:1811–1815. doi: 10.2106/00004623-200210000-00011. [DOI] [PubMed] [Google Scholar]
- 39.Ruan HJ, Fan CY, Liu JJ, Zeng BF. A comparative study of internal fixation and prosthesis replacement for radial head fractures of Mason type III. Int Orthop. 2009;33:249–253. doi: 10.1007/s00264-007-0453-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Smets S, Govaers K, Jansen N, van Riet R, Schaap M, van Glabbeek F. The floating radial head prosthesis for comminuted radial head fractures: a multicentric study. Acta Orthop Belg. 2000;66:353–358. [PubMed] [Google Scholar]
- 41.Swanson AB, Jaeger SH, La Rochelle D. Comminuted fractures of the radial head. the role of silicone-implant replacement arthroplasty. J Bone Joint Surg Am. 1981;63:1039–1049. [PubMed] [Google Scholar]
- 42.Trepman E, Ewald FC. Early failure of silicone radial head implants in the rheumatoid elbow: a complication of silicone radial head implant arthroplasty. J Arthroplasty. 1991;6:59–65. doi: 10.1016/S0883-5403(06)80158-0. [DOI] [PubMed] [Google Scholar]
- 43.van Riet RP, Sanchez-Sotelo J, Morrey BF. Failure of metal radial head replacement. J Bone Joint Surg Br. 2010;92:661–667. doi: 10.1302/0301-620X.92B5.23067. [DOI] [PubMed] [Google Scholar]
- 44.Vanderwilde RS, Morrey BF, Melberg MW, Vinh TN. Inflammatory arthritis after failure of silicone rubber replacement of the radial head. J Bone Joint Surg Br. 1994;76:78–81. [PubMed] [Google Scholar]
- 45.Zarattini G, Galli S, Marchese M, Di ML, Pazzaglia UE. The surgical treatment of isolated Mason Type 2 fractures of the radial head in adults: comparison between radial head resection and open reduction and internal fixation. J Orthop Trauma. 2012;26:229–235. doi: 10.1097/BOT.0b013e318220a227. [DOI] [PubMed] [Google Scholar]
- 46.Zunkiewicz MR, Clemente JS, Miller MC, Baratz ME, Wysocki RW, Cohen MS. Radial head replacement with a bipolar system: a minimum 2-year follow-up. J Shoulder Elbow Surg. 2012;21:98–104. doi: 10.1016/j.jse.2011.05.012. [DOI] [PubMed] [Google Scholar]