Abstract
Aims
The complex relationship between left atrial (LA) structure and function, electrical burden of atrial fibrillation (AF) and stroke risk is not well understood. We aimed to describe LA structure and function in AF.
Methods and results
Left atrial structure and function was assessed in 971 subjects enrolled in the echocardiographic substudy of ENGAGE AF-TIMI 48. Left atrial size, emptying fraction (LAEF), and contractile function were compared across AF types (paroxysmal, persistent, or permanent) and CHADS2 scores as an estimate of stroke risk. The majority of AF patients (55%) had both LA enlargement and reduced LAEF, with an inverse relationship between LA size and LAEF (R = −0.57, P < 0.001). With an increasing electrical burden of AF and higher CHADS2 scores, LA size increased and LAEF declined. Moreover, 19% of AF subjects had impaired LAEF despite normal LA size, and LA contractile dysfunction was present even among the subset of AF subjects in sinus rhythm at the time of echocardiography.
Conclusions
In a contemporary AF population, LA structure and function were increasingly abnormal with a greater electrical burden of AF and higher stroke risk estimated by the CHADS2 score. Moreover, LA dysfunction was present despite normal LA size and sinus rhythm, suggesting that the assessment of LA function may add important incremental information in the evaluation of AF patients. Clinical Trial Registration: http://www.clinicaltrials.gov; ID = NCT00781391.
Keywords: Atrial fibrillation, ENGAGE AF-TIMI 48, Left atrium, Echocardiography, Stroke
Introduction
Atrial fibrillation (AF) is common, increasing in frequency, and is associated with an elevated risk for stroke and death.1 Recent therapeutic advances, including new oral anticoagulant agents and ablation techniques, provide significant improvement in the care of AF patients.2,3 However, identifying patients who are most and least likely to benefit from these therapies remains challenging even with current risk prediction tools.1 Understanding the relationship between cardiac structure and function, electrical burden, and stroke risk in AF may help refine patient selection for anticoagulation and/or rhythm control strategies. However, prior echocardiographic studies have yielded conflicting results regarding the association between cardiac structure, function, and stroke risk in AF.4–7 These studies primarily evaluated left atrial (LA) size, while increasing attention is now being given to LA function.8–10 Therefore, we evaluated LA size and function, according to the electrical burden of AF (paroxysmal, persistent, and permanent) as well as stroke risk expressed in the CHADS2 score (congestive heart failure, hypertension, age ≥ 75 years, diabetes mellitus, stroke/TIA) in subjects enrolled in the Effective aNticoaGulation with factor xA next GEneration in AF-Thrombolysis In Myocardial Infarction 48 (ENGAGE AF-TIMI 48) study.
Methods
Study population
ENGAGE AF-TIMI 48 is a multinational, randomized (1:1:1), double-blind, double-dummy non-inferiority design trial comparing the efficacy and safety of two dosing regimens of edoxaban (high and low dose with dose reductions for patients at a high risk of bleeding) vs. warfarin titrated to an INR of 2.0–3.0 in subjects with a history of AF. The study included AF subjects at moderate-to-high risk for thrombo-embolic events (CHADS2 score ≥2). Inclusion and exclusion criteria have been previously described.11 Briefly, eligible subjects were men or women ≥21 years old with a history of AF of any duration documented by an electrocardiogram within the prior 12 months and in whom anticoagulation was indicated. Key exclusion criteria were: AF due to reversible causes, severe renal dysfunction (creatinine clearance <30 mL/min), high-bleeding risk, and/or moderate-or-severe mitral stenosis. Randomization was stratified by the CHADS2 risk score 2–3 vs. 4–6, and factors requiring a reduced dose of edoxaban. The study protocol complied with the Declaration of Helsinki and was approved by institutional review boards at each site. Written informed consent was obtained in all patients.
The prospectively designed echocardiographic substudy of ENGAGE AF-TIMI 48 was performed at 133 sites worldwide between 2009 and 2011. Subjects were invited prior to randomization to voluntarily participate with echocardiographic imaging obtained within the first week after randomization. Sonographers underwent training in the details of the echocardiographic views and techniques and received a detailed procedure manual. Standard 2D and Doppler transthoracic echocardiography was performed with images sent to the echocardiography core laboratory at Brigham and Women's Hospital, Boston, MA, USA. Conventional echocardiographic analyses were performed according to previously described methods by technicians blinded to clinical information and treatment assignment, with all study measurements confirmed by a board certified cardiologist and echocardiographer.12
Echocardiographic analyses
Echocardiographic quantification was performed according to American Society of Echocardiography guidelines.13,14 Briefly, left ventricular (LV) volumes and ejection fraction (LVEF) were calculated by the modified Simpson's method. The left ventricular mass was calculated from LV linear dimensions using the ASE recommend formula (0.8 × {1.04[(LVIDd + PWTd + SWTd)3 − (LVIDd)3]} + 0.6 g) and indexed to the body surface area, with LV hypertrophy (LVH) defined as LV mass index (LVMI) >115 g/m2 in men or >95 g/m2 in women. Left ventricular geometry was categorized as normal (relative wall thickness ≤0.42 and no LVH) or abnormal (relative wall thickness >0.42 or LVH).
Left atrial diameter was the 2D anterior–posterior length in the parasternal long-axis view. Left atrial maximum volume was measured by the modified Simpson's method using apical four- and two-chamber views at the end-systolic frame preceding mitral valve opening, and was indexed to the body surface area to derive the LA volume index (LAVI). Similarly, LA minimum volume was measured at the end-diastolic frame preceding mitral valve closure, while LA pre A volume was measured at the onset of the electrocardiographic P-wave for subjects not in AF at the time of echocardiography (Supplementary material online, Figure S1). Left atrial phasic functions were derived from following volumetric measurements:
Left atrial emptying fraction (EF): (LA max vol – LA min vol)/LA max vol.
Left atrial conduit or passive EF: (LA max vol – LA pre A vol)/LA max vol.
Left atrial contractile or active EF: (LA pre A vol – LA min vol)/LA pre A vol.
Left atrial expansion index: (LA max vol – LA min vol)/LA min vol.
Early (E) and late (A) transmitral velocities were measured by pulsed wave Doppler from the apical four-chamber view with the sample volume positioned at the tip of the mitral leaflets. Peak lateral and septal mitral annular early relaxation (e′) and atrial contraction (a′) velocities were assessed using tissue Doppler imaging. Left ventricular filling pressures were estimated by E-wave divided by average e′ velocities (E/e′). Reduced LA EF was defined as ≤45%15,16 and abnormal LA active contractile function was defined as TDI a′ ≤7 cm/s.17
Final values were taken as the mean of measurements from three cardiac cycles. Atrial fibrillation at the time of echocardiography was determined by the absence of A-waves on transmitral spectral Doppler flow and tissue Doppler mitral annular velocity profiles, as well as the lack of organized electrocardiographic P-waves. The reproducibility of measurements of LA volumes has been evaluated in the echocardiographic core lab at Brigham and Women's Hospital in 20 subjects: intra-observer intraclass correlation coefficient 0.95 (0.91–0.99) and inter-observer intraclass correlation coefficient 0.84 (0.75–0.93).
Statistical methods
Subjects' electrical burden of AF was classified according to type of AF: paroxysmal, persistent, or permanent, defined in accordance with AHA/ACC/ESC guidelines18 and as determined by the site investigator. Subjects were categorized according to the CHADS2 risk score: 2, 3, or 4–6. Summary statistics were calculated and are presented as medians (inter-quartile ranges) and counts (percentages), for continuous and categorical data, respectively. Statistical comparisons across types of AF were made with Cuzick's non-parametric trend test.19 Multivariate-ordered logistic regression was used to assess for the relationship between cardiac structure and function and CHADS2 risk score, with adjustment for heart rate, blood pressure, and rhythm at the time of echocardiography. Forward stepwise multivariate-ordered logistic regression was used to identify features of cardiac structure and function significantly associated with higher CHADS2 scores. As echocardiograms were obtained within 1 week after randomization and this is a cross-sectional analysis, treatment allocation to edoxaban or warfarin was not included. All analyses were performed using Stata 11.2 (Stata Corp., College Station, TX, USA) with P-values <0.05 considered statistically significant. No adjustments were made for multiple comparisons.
Results
Overall study population
The ENGAGE AF-TIMI 48 echocardiographic substudy enrolled 1120 subjects, of whom 971 (87%) had technically adequate images. These results were obtained prior to the unblinding of subject's study drug allocation. When compared with the 971 subjects included in the echocardiographic analysis, the 149 subjects not included were slightly younger (median 71 vs. 73 years, P = 0.020), had comparable CHADS2 scores (median 3 in both groups), and the proportions with persistent or permanent AF were similar. When compared with the other 20 134 subjects in the parent ENGAGE AF-TIMI 48 trial, the 971 subjects included in the final echocardiographic analysis were older (median 73 vs. 72 years, P < 0.001), but were less likely to be female (34 vs. 38%, P = 0.015), and more frequently Caucasian (92 vs. 80%, P < 0.001). Paroxysmal AF was more common in the echocardiographic cohort (33 vs. 25%, P < 0.001); while permanent AF was less frequent (46 vs. 52%, P = 0.001). However, the CHADS2 score was similar between the echocardiographic substudy and parent trial.
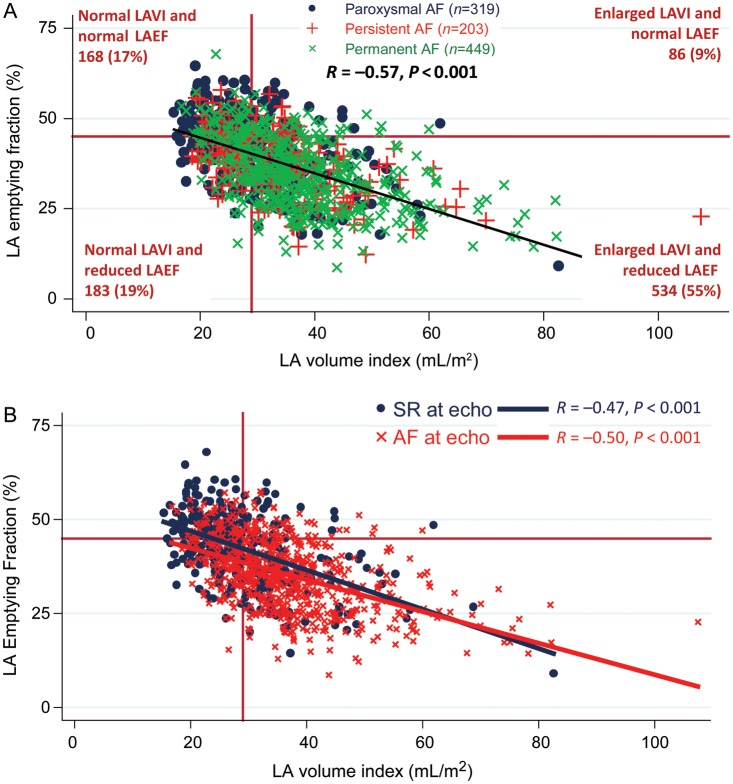
In the echocardiographic substudy, LA enlargement (defined as LAVI ≥29 mL/m2) was present in nearly two-thirds of all subjects and there was a significant inverse relationship between LA function, measured by LAEF, and LAVI according to type of AF (Figure 1A). This relationship was similar when stratified by rhythm at the time echocardiography as well (Figure 1B). However, even among AF subjects with normal LAVI, approximately half had impaired LA EF.
Figure 1.
The relationship between left atrial emptying fraction and left atrial volume index. (A) Left atrial emptying fraction was inversely correlated with left atrial size. Left atrial size was normal (LAVI <29 mL/m2) in 36% of all atrial fibrillation patients and 17% had both normal left atrial size and left atrial emptying fraction (>45%). (B) The inverse relationship between left atrial emptying fraction and left atrial size was similar between subjects in sinus rhythm (n = 321) and atrial fibrillation (n = 650) at the time of echocardiography.
Paroxysmal, persistent, or permanent atrial fibrillation
Paroxysmal, persistent, and permanent AF were present in 33, 21, and 46% of subjects, respectively (Table 1). Approximately 25% of those with permanent AF had a CHADS2 score of 4–6 compared with 18–19% of those with paroxysmal or persistent AF (P = 0.09).
Table 1.
Baseline characteristics according to type of atrial fibrillation
| Characteristic | Overall (n = 971) | Paroxysmal [n = 319 (31)] | Persistent [n = 203 (21)] | Permanent [n = 449 (46)] | P-trend |
|---|---|---|---|---|---|
| Age, years | 73 (65, 79) | 74 (66, 79) | 75 (68, 80) | 72 (64, 78) | 0.19 |
| Age ≥75 years | 442 (45.5) | 147 (46.1) | 109 (53.7) | 186 (41.4) | 0.14 |
| Gender, female | 334 (34.4) | 127 (39.8) | 69 (34.0) | 138 (30.7) | 0.01 |
| Race, Caucasian | 896 (92.3) | 295 (92.5) | 188 (92.6) | 413 (92.0) | 0.79 |
| CHADS2 score | 0.09 | ||||
| 2 | 475 (48.9) | 155 (48.6) | 108 (53.2) | 212 (47.2) | |
| 3 | 283 (29.2) | 104 (32.6) | 57 (28.1) | 122 (27.2) | |
| 4–6 | 213 (21.9) | 60 (18.8) | 38 (18.7) | 115 (25.6) | |
| History of | |||||
| Heart failure | 521 (53.7) | 129 (40.4) | 102 (50.3) | 290 (64.6) | <0.001 |
| Hypertension | 892 (91.9) | 291 (91.2) | 184 (90.6) | 417 (92.9) | 0.38 |
| Diabetes mellitus | 340 (35.0) | 125 (39.2) | 63 (31.0) | 152 (33.9) | 0.16 |
| Stroke or TIA | 258 (26.6) | 92 (28.8) | 44 (21.7) | 122 (27.2) | 0.71 |
| Coronary HD | 359 (37.0) | 127 (39.9) | 63 (31.0) | 169 (37.6) | 0.62 |
| Tobacco, ever | 489 (50.4) | 173 (54.2) | 99 (48.8) | 217 (48.3) | 0.12 |
| Obese | 407 (41.9) | 138 (43.3) | 76 (37.4) | 193 (43.0) | 0.97 |
| CKDa | 325 (33.9) | 116 (36.8) | 65 (32.7) | 144 (32.4) | 0.22 |
| Creatinine clearance | 71 (55, 92) | 70 (54, 93) | 71 (55, 85) | 73 (55, 95) | 0.43 |
| Heart rate, b.p.m. | 72 (63, 82) | 68 (60, 76) | 73 (64, 82) | 75 (66, 86) | <0.001 |
| Systolic BP, mmHg | 130 (120, 140) | 130 (120, 140) | 130 (118, 144) | 130 (120, 140) | 0.22 |
| Diastolic BP, mmHg | 78 (70, 83) | 75 (69, 80) | 78 (70, 84) | 80 (70, 84) | 0.001 |
Data presented as counts (percentages) or median (inter-quartile ranges) for categorical and continuous variables, respectively.
TIA, transient ischaemic attack; HD, heart disease; CKD, chronic kidney disease; BMI, body mass index.
aCKD, defined by creatinine clearance <60 mL/min at randomization.
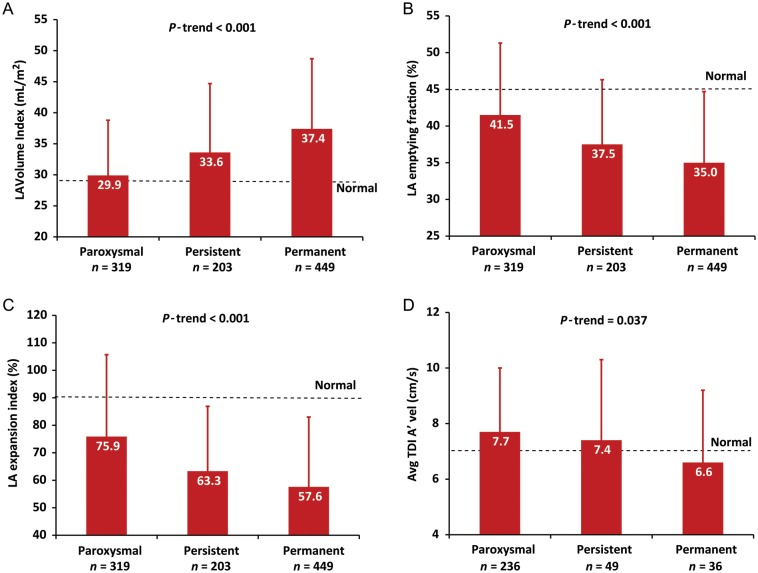
Left atrial size, as determined by LAVIs, increased across AF types (Figure 2A) with 48, 60, and 77% of paroxysmal, persistent, and permanent AF having enlarged LA, respectively (Table 2). Left atrial function, assessed by EF, significantly declined across the spectrum of AF types (Figure 2B). There was a corresponding decrease in LA compliance or reservoir function as assessed by the expansion index across AF types (Figure 2C). Left atrial conduit function, as determined by transmitral E-wave velocities, increased according to type of AF (Table 2). In the subset of subjects who were not in AF at the time of echocardiography, LA contractile function, determined by transmitral spectral Doppler A-wave velocities and mitral annular tissue Doppler a′ velocities, declined with progression from paroxysmal to persistent to permanent AF (Figure 2D).
Figure 2.
Left atrial size and function according to type of atrial fibrillation. (A) Left atrial size measured by the volume index significantly increased. (B) Left atrial emptying fraction significantly declined. (C) The left atrial expansion index, a measure of reservoir function and left atrial compliance, significantly declined. (D) Among those in sinus rhythm at the time of echocardiography, left atrial contractile function, assessed by tissue Doppler imaging A′ velocities, was lowest in those with permanent atrial fibrillation.
Table 2.
Cardiac structure and function according to type of atrial fibrillation
| Characteristic | Overall (n = 971) | Paroxysmal [n = 319 (31)] | Persistent [n = 203 (21)] | Permanent [n = 449 (46)] | P-trend |
|---|---|---|---|---|---|
| AF during echo | 650 (66.9) | 83 (26.0) | 154 (75.9) | 413 (92.0) | <0.001 |
| Left ventricular structure and function | |||||
| LVEF, % | 59 (53, 61) | 59 (57, 61) | 59 (54, 60) | 58 (46, 60) | <0.001 |
| LVEF <50% | 217 (22.4) | 45 (14.1) | 43 (21.2) | 129 (28.7) | <0.001 |
| LV EDVI, mL/m2 | 56 (51, 62) | 56 (51, 62) | 56 (50, 62) | 56 (50, 53) | 0.53 |
| LV ESVI, mL/m2 | 23 (21, 28) | 23 (20, 26) | 24 (20, 28) | 24 (21, 31) | 0.041 |
| LV EDD, cm | 4.6 (4.4, 4.9) | 4.6 (4.3, 4.8) | 4.6 (4.3, 4.8) | 4.7 (4.4, 4.9) | <0.001 |
| LVMI, g/m2 | 68 (58, 88) | 68 (57, 84) | 67 (57, 88) | 69 (59, 91) | 0.040 |
| Abnormal LV geometrya | 276 (28.4) | 91 (28.5) | 58 (28.6) | 127 (28.3) | 0.94 |
| LV sphericity index | 1.63 (1.53, 1.75) | 1.68 (1.58, 1.81) | 1.63 (1.54, 1.75) | 1.60 (1.49, 1.71) | <0.001 |
| Left atrial structure and function | |||||
| LA diameter, cm | 3.6 (3.4, 3.8) | 3.4 (3.3, 3.7) | 3.6 (3.4, 3.8) | 3.7 (3.5, 4.0) | <0.001 |
| LAVI, mL/m2 | 33 (26, 39) | 28 (24, 35) | 32 (26, 38) | 35 (30, 43) | <0.001 |
| LAVI >29 mL/m2 | 620 (63.9) | 152 (47.7) | 121 (59.6) | 347 (77.3) | <0.001 |
| LA min vol, mL | 41 (29, 54) | 34 (23, 43) | 37 (29, 52) | 47 (35, 60) | <0.001 |
| LA emptying fraction, % | 38 (31, 45) | 42 (35, 49) | 38 (32, 44) | 35 (28, 43) | <0.001 |
| LA expansion index, % | 61 (44, 83) | 74 (53, 96) | 61 (46, 79) | 53 (38, 76) | <0.001 |
| LA pre A vol, mL | 40 (30, 51) | 40 (29, 51) | 41 (32, 50) | 39 (31, 56) | 0.39 |
| LA passive EF, % | 25 (20, 31) | 26 (20, 31) | 22 (18, 29) | 24 (17, 27) | 0.032 |
| LA active EF, % | 23 (16, 29) | 23 (17, 29) | 22 (16, 26) | 18 (14, 27) | 0.12 |
| Doppler | |||||
| TDI A′ avg, cm/s | 7.4 (5.9, 9.1) | 7.6 (6.1, 9.1) | 7.3 (5.6, 8.7) | 6.6 (5.0, 8.4) | 0.037 |
| E-wave vel, cm/s | 84 (70, 98) | 76 (61, 90) | 88 (77, 103) | 88 (74, 100) | <0.001 |
| A-wave vel, cm/s | 71 (55, 89) | 72 (58, 91) | 66 (56, 84) | 56 (44, 81) | 0.005 |
| TDI E′ avg, cm/s | 7.7 (6.2, 9.1) | 6.7 (5.4, 8.1) | 8.0 (6.7, 9.5) | 8.2 (6.7, 9.5) | <0.001 |
| E/e′ avg | 10.7 (8.6, 13.7) | 10.7 (8.6, 13.9) | 10.8 (8.4, 14.5) | 10.7 (8.6, 13.5) | 0.64 |
| Mitral regurgitation | |||||
| Mild | 691 (75.3) | 192 (64.0) | 156 (80.4) | 343 (80.9) | <0.001 |
| Moderate or severe | 99 (10.8) | 34 (11.3) | 16 (8.3) | 49 (11.6) | 0.84 |
Data presented as counts (percentages) or median (inter-quartile ranges) for categorical and continuous variables, respectively.
LVEF, left ventricular ejection fraction; LV, left ventricular; EDVI, end-diastolic volume index; ESVI, end-systolic volume index; EDD, end-diastolic diameter; LVMI, left ventricular mass index; LA, left atrial; LAVI, left atrial volume index; TDI A′, tissue Doppler imaging mitral annular A′; TDI E′, tissue Doppler imaging mitral annular E; E/e′, E-wave/TDI E′; aAbnormal LV geometry defined as hypertrophy or concentric remodelling.
Left ventricular and ejection fraction was preserved in most subjects (78%) regardless of AF type, although the prevalence of reduced LVEF (<50%) was twice as high in permanent when compared with paroxysmal AF. There was a corresponding trend towards a larger LV size and a higher LVMI in those with permanent AF, although the prevalence of abnormal LV geometry, defined as hypertrophy or concentric remodelling, did not differ. Left ventricular filling pressures (E/e′) were also similar across groups (Table 2).
CHADS2 score
CHADS2 scores of 2, 3, and 4–6 were present in 49, 29, and 22% of subjects, respectively (Table 3). The frequency of reduced LVEF (<50%) was similar regardless of the CHADS2 score (Table 4). Abnormal LV geometry increased in frequency with higher CHADS2 scores. There was an inverse relationship between LV early diastolic relaxation (e′) velocities and CHADS2 score with a corresponding increase in LV filling pressures (E/e′) across CHADS2 categories. Similarly, LA size increased with higher CHADS2 scores, with a parallel decline in LA EF. In forward stepwise multivariate-ordered logistic regression analyses, higher LV filling pressures (E/e′), larger LAVI, and the presence of abnormal LV geometry were significantly associated with higher CHADS2 score as a measure of stroke risk (Table 5). While both the burden of AF and the CHADS2 score were related to LA size and function (Figure 3A and B), the electrical burden of AF appeared to be a stronger contributor than the CHADS2 score. Lastly, as the CHA2DS2-VASc score20 is a validated method for assessing stroke risk in AF, we also evaluated LA structure and function according to this system and found similar results as with CHADS2, namely that LAVI increased, LAEF decreased, and LA TDI A′ velocities declined with a greater CHA2DS2-VASc score (Supplementary material online, Table S1).
Table 3.
Baseline characteristics according to the CHADS2 score
| Characteristic | Overall (n = 971) | CHADS2= 2 [n = 475 (49)] | CHADS2= 3 [n = 283 (29)] | CHADS2= 4–6 [n = 213 (22)] | P-trend |
|---|---|---|---|---|---|
| Age, years | 73 (65, 79) | 70 (63, 77) | 75 (67, 80) | 76 (70, 80) | <0.001 |
| Age ≥75 years | 442 (45.5) | 168 (35.4) | 145 (51.2) | 129 (60.6) | <0.001 |
| Gender, F | 334 (34.4) | 150 (31.6) | 106 (37.5) | 78 (36.6) | 0.13 |
| Race, Caucasian | 896 (92.3) | 440 (92.6) | 260 (91.9) | 196 (92.0) | 0.74 |
| Type of AF | 0.09 | ||||
| Paroxysmal | 319 (32.9) | 155 (32.6) | 104 (36.8) | 60 (28.2) | |
| Persistent | 203 (20.9) | 108 (22.7) | 57 (20.1) | 38 (17.8) | |
| Permanent | 449 (46.2) | 212 (44.6) | 122 (43.1) | 115 (54.0) | |
| History of | |||||
| Heart failure | 521 (53.7) | 222 (46.7) | 176 (62.2) | 123 (57.8) | 0.001 |
| Hypertension | 892 (91.9) | 421 (88.6) | 264 (93.3) | 207 (97.2) | <0.001 |
| Diabetes mellitus | 340 (35.0) | 92 (19.4) | 142 (50.2) | 106 (49.8) | <0.001 |
| Stroke or TIA | 258 (26.6) | 26 (5.5) | 60 (21.2) | 172 (80.8) | <0.001 |
| Coronary HD | 359 (37.0) | 146 (30.7) | 111 (39.4) | 102 (47.9) | <0.001 |
| Tobacco, ever | 489 (50.4) | 236 (49.7) | 153 (54.1) | 100 (47.0) | 0.74 |
| Obese | 407 (41.9) | 189 (39.8) | 130 (45.9) | 88 (41.3) | 0.47 |
| CKDa | 325 (33.9) | 118 (25.2) | 108 (38.6) | 99 (47.1) | <0.001 |
| Creatinine clearance | 71 (55, 92) | 77 (60, 100) | 68 (53, 91) | 62 (48, 79) | <0.001 |
| Heart rate, b.p.m. | 72 (63, 82) | 70 (62, 82) | 72 (64, 83) | 72 (65, 80) | 0.14 |
| Systolic BP, mmHg | 130 (120, 140) | 130 (120, 140) | 130 (119, 142) | 130 (118, 142) | 0.56 |
| Diastolic BP, mmHg | 78 (70, 83) | 78 (70, 83) | 78 (70, 84) | 77 (69, 82) | 0.18 |
Data presented as counts (percentages) or median (inter-quartile ranges) for categorical and continuous variables, respectively.
TIA, transient ischaemic attack; HD, heart disease; CKD, chronic kidney disease; BMI, body mass index.
aCKD defined by creatinine clearance <60 mL/min at randomization.
Table 4.
Cardiac structure and function according to the CHADS2 score
| Characteristic | Overall (n = 971) | CHADS2= 2 [n = 475 (49)] | CHADS2= 3 [n = 283 (29)] | CHADS2= 4–6 [n = 213 (22)] | P-valuea |
|---|---|---|---|---|---|
| AF during echo | 321 (33.1) | 161 (33.9) | 98 (34.6) | 62 (29.1) | 0.29 |
| Left ventricular structure and function | |||||
| LVEF, % | 59 (53, 61) | 59 (54, 61) | 58 (48, 60) | 58 (54, 61) | 0.73 |
| LVEF < 50% | 217 (22.4) | 99 (20.8) | 73 (25.8) | 45 (21.1) | 0.66 |
| LV EDVI, mL/m2 | 56 (51, 62) | 56 (50, 62) | 57 (51, 64) | 56 (52, 62) | 0.044 |
| LV ESVI, mL/m2 | 23 (21, 28) | 23 (20, 27) | 24 (21, 30) | 24 (21, 28) | 0.23 |
| LVEDD, cm | 4.6 (4.4, 4.9) | 4.6 (4.4, 4.9) | 4.7 (4.4, 4.9) | 4.6 (4.3, 4.8) | 0.66 |
| LVMI, g/m2 | 68 (58, 88) | 67.2 (57.6, 83.6) | 68.1 (58.0, 89.5) | 74.4 (59.6, 97.3) | 0.009 |
| Abnormal LV geometrya | 276 (28.4) | 120 (25.3) | 81 (28.6) | 75 (35.2) | 0.015 |
| LV sphericity index | 1.63 (1.53, 1.75) | 1.64 (1.53, 1.76) | 1.62 (1.50, 1.75) | 1.63 (1.53, 1.77) | 0.38 |
| Left atrial structure and function | |||||
| LA diameter, cm | 3.6 (3.4, 3.8) | 3.6 (3.4, 3.8) | 3.6 (3.4, 3.9) | 3.6 (3.4, 3.9) | 0.046 |
| LAVI, mL/m2 | 33 (26, 39) | 31 (26, 38) | 34 (27, 40) | 34 (27, 41) | 0.007 |
| LAVI ≥29 mL/m2 | 620 (63.9) | 281 (59.2) | 194 (68.6) | 145 (68.1) | 0.016 |
| LA min volume, mL | 41 (29, 54) | 39 (28, 53) | 42 (29, 53) | 42 (29, 55) | 0.09 |
| LA emptying frac, % | 38 (31, 45) | 39 (32, 46) | 37 (29, 45) | 37 (29, 45) | 0.041 |
| LA expansion index, % | 61 (44, 83) | 63 (47, 83) | 58 (41, 82) | 59 (40, 83) | 0.16 |
| LA pre A vol, mL | 40 (30, 51) | 39 (30, 48) | 41 (31, 55) | 39 (32, 52) | 0.12 |
| LA passive EF, % | 25 (20, 31) | 25 (21, 31) | 25 (19, 32) | 23 (18, 30) | 0.31 |
| LA active EF, % | 23 (16, 29) | 23 (17, 29) | 21 (16, 27) | 25 (15, 29) | 0.96 |
| Doppler | |||||
| TDI A′ average, cm/s | 7.4 (5.9, 9.1) | 7.5 (6.1, 9.1) | 7.4 (5.5, 9.4) | 6.8 (5.7, 8.4) | 0.09 |
| E wave velocity, cm/s | 84 (70, 98) | 82 (69, 96) | 86 (73, 100) | 74 (87, 98) | 0.31 |
| A wave velocity, cm/s | 71 (55, 89) | 71 (55, 92) | 73 (56, 93) | 64 (55, 83) | 0.45 |
| TDI E′ average, cm/s | 7.7 (6.2, 9.1) | 7.8 (6.4, 9.3) | 7.6 (6.1, 9.2) | 7.2 (6.0, 8.6) | <0.001 |
| E/e′ average | 10.7 (8.6, 13.7) | 10.1 (8.1, 13.4) | 11.1 (9.1, 14.8) | 11.6 (9.5, 14.2) | <0.001 |
| Mitral regurgitation | |||||
| Mild | 691 (75.3) | 341 (75.8) | 187 (70.3) | 163 (80.7) | 0.72 |
| Moderate or severe | 99 (10.8) | 47 (10.4) | 35 (13.2) | 17 (8.4) | 0.25 |
Data presented as counts (percentages) or median (inter-quartile ranges) for categorical and continuous variables, respectively.
LVEF, left ventricular ejection fraction; LV, left ventricular; EDVI, end-diastolic volume index; ESVI, end-systolic volume index; EDD, end-diastolic diameter; ESD, end-systolic diameter; LVMI, left ventricular mass index; LA, left atrial; LAVI, left atrial volume index; TDI A′, tissue Doppler imaging mitral annular A′; TDI E′, tissue Doppler imaging mitral annular E; E/e′, E-wave/TDI E′; abnormal LV geometry defined as hypertrophy or concentric remodellinga.
Table 5.
Features of cardiac structure and function associated with higher CHADS2 scores as a measure of stroke risk from forward stepwise multivariate logistic regression
| Characteristic | Odds ratio | 95% CI | P-value |
|---|---|---|---|
| E/e′ avg (per 4.7) | 1.24 | 1.09–1.37 | 0.001 |
| LAVI, mL/m2 (per 11.2) | 1.22 | 1.06–1.34 | 0.005 |
| Abnormal LV geometry | 1.16 | 1.01–1.39 | 0.035 |
LAVI, left atrial volume index; LV, left ventricular; abnormal LV geometry defined as concentric remodelling or hypertrophy.
Covariates entered into model: heart rate, systolic BP, diastolic BP, rhythm at the time of echocardiography, LVEF, LV end-diastolic volume, LV end-systolic volume, LV end-diastolic diameter, LV end-systolic diameter, LV wall thickness, LV mass index, LV geometry, LA width, LA volume index, LA minimum volume, LA emptying fraction, LA expansion index, E-wave velocity, E-wave deceleration time, tissue Doppler imaging E′ velocity, LV filling pressures (E/e′), and mitral regurgitation.
Model characteristics: log likelihood = −860; χ2 = 25.7, P < 0.001.
Figure 3.
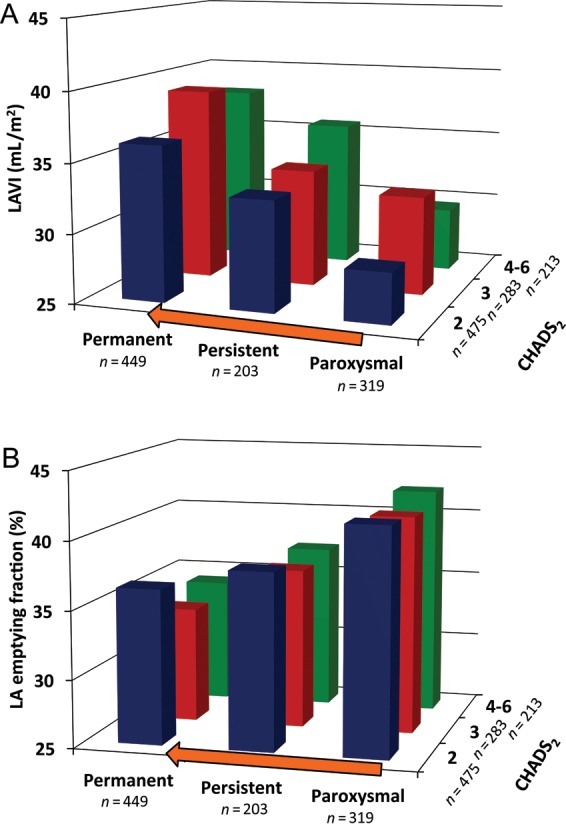
Relationship between left atrial size and function according to type of atrial fibrillation and stroke risk expressed in the CHADS2 score. (A) Increasing left atrial size, measured by left atrial volume index, appears more strongly related to type of atrial fibrillation (P < 0.001) than to stroke risk expressed in the CHADS2 score (P = 0.007). (B) Worsening left atrial emptying fraction appears more strongly related to type of atrial fibrillation (P < 0.001), than to the CHADS2 score (P = 0.041).
Discussion
In a pre-specified echocardiographic substudy of the ENGAGE AF-TIMI 48 trial, we identified strong correlations between increasing abnormalities of LA structure and function with greater burdens of AF and higher CHADS2 score, an estimate of stroke risk. While the majority of AF subjects had LA enlargement, we also demonstrated impaired LA function among a sizeable number of subjects with normal LA size. Furthermore, we found that LA contractile function was abnormal even in subjects in sinus rhythm. These findings suggest that the assessment of LA function may add important new information in the evaluation of the AF patient.
In an effort to improve stroke risk stratification beyond that achieved with conventional clinical characteristics,21 others have explored the importance of LA size, but with mixed results in predicting stroke.4–7 While the majority of AF patients have enlarged LA,4–7 36% of AF subjects in this study had normal LA size, suggesting that a substantial number of AF patients are at moderate-to-high risk for stroke based on the CHADS2 score despite normal LA size. Given the limitations of LA size, increasing attention has been given to LA function in AF.8 We identified LA dysfunction in approximately half of subjects with normal LAVI, suggesting not only that LA mechanical dysfunction may precede LA enlargement, but also that those with LA dysfunction may be at a higher risk for stroke despite normal LA size. This raises the possibility that the evaluation of LA function may be helpful in assessing stroke risk and in the identification of those who may benefit from anticoagulation strategies.22–24 Importantly, we also found that 17% of AF subjects had both normal LA size and function, which may not only represent a subgroup at a lower risk for stroke, but also patients most likely to respond to rhythm control strategies,25–28 although, these hypotheses remain to be formally tested in outcomes based studies.
Several studies demonstrate a similar risk of stroke regardless of intermittent or sustained forms of AF,29–34 hence, current guidelines recommend anticoagulation regardless of whether AF is paroxysmal, persistent, or permanent.18 However, these studies did not include evaluations of cardiac structure and function to potentially explain the clinical findings. In this study, we identified LA contractile dysfunction in the subset of subjects in sinus rhythm at the time of echocardiography, including those with paroxysmal AF, suggesting electro-mechanical dissociation. While previously described in the post-cardioversion period,35 our findings suggest that electro-mechanical dissociation may be common in the broader AF population, including those with paroxysmal AF.36 Left atrial contractile dysfunction among paroxysmal AF patients may not only help to explain the similar risk of stroke between intermittent and sustained forms of AF, but also raises the possibility that patients with abnormal LA contractile function may have a higher risk of stroke than those with normal contractile function. Additionally, we found that features of cardiac structure and function associated with a higher CHADS2 score, including greater LV filling pressures and abnormal LV geometry, were similar across paroxysmal, persistent, and permanent AF. These results are consistent with proposed mechanisms for thrombus formation in AF, including stasis and endothelial dysfunction,37 and are congruent with existing data from smaller studies.23,38,39 Together, these findings may partially explain the previously reported similarities in stroke risk despite differing burdens of AF. However, whether these factors are of prognostic importance in the stratification of stroke risk needs to be prospectively tested.
While we evaluated a relatively large contemporary AF population, limitations should be noted. The cross-sectional design precludes the assessment of causal relationships between cardiac structure and function and AF type. The irregular rhythm of AF may lead to beat-to-beat variability in echocardiographic measurements; however, our assessments were averaged over multiple cardiac cycles. Cardiac structure and function may differ between those in AF and those not in AF at the time of echocardiography, although we performed sensitivity analyses with stratification by rhythm at the time of echocardiography and the results did not substantially change (Supplementary material online, Table S2). Assessing LA deformation and function with strain imaging may provide additional information and is a future direction. While we cannot exclude misclassification bias with respect to AF type, as paroxysmal, persistent, and permanent designations were determined by site investigators, our results are largely consistent with registries of AF patients.40,41 By design, ENGAGE AF-TIMI 48 enrolled an AF population at moderate-to-high risk for stroke (CHADS2 ≥2), therefore our assessment does not include the entire spectrum of CHADS2 scores. Furthermore, we utilized CHADS2 as a surrogate for stroke risk and therefore our findings need prospective evaluation in relation to clinical thrombo-embolic events.
In conclusion, we identified increasing abnormalities of LA structure and function with greater burdens of AF and stroke risk estimated by the CHADS2 score. Moreover, we found that impairments in LA function were present even among subjects with normal LA size and sinus rhythm. These findings suggest that the assessment of LA function may add important incremental information to the evaluation of AF patients.
Supplementary material
Supplementary material is available at European Heart Journal online.
Funding
The ENGAGE AF-TIMI 48 study was funded by Daiichi Sankyo Pharma Development (Edison, NJ, USA). Support was provided by the NIH training grant (T32 HL094301-02).
Conflict of interest: R.P.G. is the co-principal investigator for the ENGAGE AF-TIMI 48 study. R.P.G., E.M.A., E.B., and S.D.S. have received research support from Daiichi Sankyo. R.P.G., C.T.R., and S.D.S. have consulted for Daiichi Sankyo. I.P., M.S., and M.M. are employees of Daiichi Sankyo. R.P.G. has received honoraria for consulting regarding novel anticoagulants from Janssen. C.T.R. has received honoraria for consulting from Alere, Beckman Coulter, and Boerhinger-Ingelheim. V.M. has received research support, honoraria, or consulted for Novartis, Bayer, GlaxoSmithKline, CardioPep, and Cardiorentis.
Supplementary Material
References
- 1.Lip GY, Tse HF, Lane DA. Atrial fibrillation. Lancet. 2012;379:648–661. doi: 10.1016/S0140-6736(11)61514-6. [DOI] [PubMed] [Google Scholar]
- 2.Stulak JM, Dearani JA, Sundt TM, III, Daly RC, Schaff HV. Ablation of atrial fibrillation: comparison of catheter-based techniques and the Cox-Maze III operation. Ann Thorac Surg. 2011;91:1882–1888. doi: 10.1016/j.athoracsur.2011.02.035. discussion 1888–9. [DOI] [PubMed] [Google Scholar]
- 3.Dogliotti A, Paolasso E, Giugliano RP. Novel oral anticoagulants in atrial fibrillation: a meta-analysis of large, randomized, controlled trials vs warfarin. Clin Cardiol. 2013;36:61–67. doi: 10.1002/clc.22081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dittrich HC, Pearce LA, Asinger RW, McBride R, Webel R, Zabalgoitia M, Pennock GD, Safford RE, Rothbart RM, Halperin JL, Hart RG. Left atrial diameter in nonvalvular atrial fibrillation: an echocardiographic study. Stroke Prevention in Atrial Fibrillation Investigators. Am Heart J. 1999;137:494–499. doi: 10.1016/S0002-8703(99)70498-9. [DOI] [PubMed] [Google Scholar]
- 5.Gage BF, Waterman AD, Shannon W, Boechler M, Rich MW, Radford MJ. Validation of clinical classification schemes for predicting stroke: results from the National Registry of Atrial Fibrillation. JAMA. 2001;285:2864–2870. doi: 10.1001/jama.285.22.2864. [DOI] [PubMed] [Google Scholar]
- 6.Echocardiographic predictors of stroke in patients with atrial fibrillation: a prospective study of 1066 patients from three clinical trials. Arch Intern Med. 1998;158:1316–1320. doi: 10.1001/archinte.158.12.1316. [DOI] [PubMed] [Google Scholar]
- 7.Olshansky B, Heller EN, Mitchell LB, Chandler M, Slater W, Green M, Brodsky M, Barrell P, Greene HL. Are transthoracic echocardiographic parameters associated with atrial fibrillation recurrence or stroke? Results from the Atrial Fibrillation Follow-Up Investigation of Rhythm Management (AFFIRM) study. J Am Coll Cardiol. 2005;45:2026–2033. doi: 10.1016/j.jacc.2005.03.020. [DOI] [PubMed] [Google Scholar]
- 8.Kojima T, Kawasaki M, Tanaka R, Ono K, Hirose T, Iwama M, Watanabe T, Noda T, Watanabe S, Takemura G, Minatoguchi S. Left atrial global and regional function in patients with paroxysmal atrial fibrillation has already been impaired before enlargement of left atrium: velocity vector imaging echocardiography study. Eur Heart J Cardiovasc Imaging. 2012;13:227–234. doi: 10.1093/ejechocard/jer281. [DOI] [PubMed] [Google Scholar]
- 9.Gupta S, Matulevicius SA, Ayers CR, Berry JD, Patel PC, Markham DW, Levine BD, Chin KM, de Lemos JA, Peshock RM, Drazner MH. Left atrial structure and function and clinical outcomes in the general population. Eur Heart J. 2013;34:278–285. doi: 10.1093/eurheartj/ehs188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Abhayaratna WP, Fatema K, Barnes ME, Seward JB, Gersh BJ, Bailey KR, Casaclang-Verzosa G, Tsang TS. Left atrial reservoir function as a potent marker for first atrial fibrillation or flutter in persons > or = 65 years of age. Am J Cardiol. 2008;101:1626–1629. doi: 10.1016/j.amjcard.2008.01.051. [DOI] [PubMed] [Google Scholar]
- 11.Ruff CT, Giugliano RP, Antman EM, Crugnale SE, Bocanegra T, Mercuri M, Hanyok J, Patel I, Shi M, Salazar D, McCabe CH, Braunwald E. Evaluation of the novel factor Xa inhibitor edoxaban compared with warfarin in patients with atrial fibrillation: design and rationale for the Effective aNticoaGulation with factor xA next GEneration in Atrial Fibrillation-Thrombolysis In Myocardial Infarction study 48 (ENGAGE AF-TIMI 48) Am Heart J. 2010;160:635–641. doi: 10.1016/j.ahj.2010.06.042. [DOI] [PubMed] [Google Scholar]
- 12.Solomon SD, Foster E, Bourgoun M, Shah A, Viloria E, Brown MW, Hall WJ, Pfeffer MA, Moss AJ. Effect of cardiac resynchronization therapy on reverse remodeling and relation to outcome: multicenter automatic defibrillator implantation trial: cardiac resynchronization therapy. Circulation. 2010;122:985–992. doi: 10.1161/CIRCULATIONAHA.110.955039. [DOI] [PubMed] [Google Scholar]
- 13.Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA, Picard MH, Roman MJ, Seward J, Shanewise JS, Solomon SD, Spencer KT, Sutton MS, Stewart WJ. Recommendations for chamber quantification: a report from the American Society of Echocardiography's Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr. 2005;18:1440–1463. doi: 10.1016/j.echo.2005.10.005. [DOI] [PubMed] [Google Scholar]
- 14.Nagueh SF, Appleton CP, Gillebert TC, Marino PN, Oh JK, Smiseth OA, Waggoner AD, Flachskampf FA, Pellikka PA, Evangelista A. Recommendations for the evaluation of left ventricular diastolic function by echocardiography. J Am Soc Echocardiogr. 2009;22:107–133. doi: 10.1016/j.echo.2008.11.023. [DOI] [PubMed] [Google Scholar]
- 15.Abhayaratna WP, Seward JB, Appleton CP, Douglas PS, Oh JK, Tajik AJ, Tsang TS. Left atrial size: physiologic determinants and clinical applications. J Am Coll Cardiol. 2006;47:2357–2363. doi: 10.1016/j.jacc.2006.02.048. [DOI] [PubMed] [Google Scholar]
- 16.Gutman J, Wang YS, Wahr D, Schiller NB. Normal left atrial function determined by 2-dimensional echocardiography. Am J Cardiol. 1983;51:336–340. doi: 10.1016/S0002-9149(83)80061-7. [DOI] [PubMed] [Google Scholar]
- 17.Wang M, Yip GW, Wang AY, Zhang Y, Ho PY, Tse MK, Lam PK, Sanderson JE. Peak early diastolic mitral annulus velocity by tissue Doppler imaging adds independent and incremental prognostic value. J Am Coll Cardiol. 2003;41:820–826. doi: 10.1016/S0735-1097(02)02921-2. [DOI] [PubMed] [Google Scholar]
- 18.Fuster V, Ryden LE, Cannom DS, Crijns HJ, Curtis AB, Ellenbogen KA, Halperin JL, Le Heuzey JY, Kay GN, Lowe JE, Olsson SB, Prystowsky EN, Tamargo JL, Wann S, Smith SC, Jr, Jacobs AK, Adams CD, Anderson JL, Antman EM, Hunt SA, Nishimura R, Ornato JP, Page RL, Riegel B, Priori SG, Blanc JJ, Budaj A, Camm AJ, Dean V, Deckers JW, Despres C, Dickstein K, Lekakis J, McGregor K, Metra M, Morais J, Osterspey A, Zamorano JL. ACC/AHA/ESC 2006 Guidelines for the Management of Patients with Atrial Fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the European Society of Cardiology Committee for Practice Guidelines (Writing Committee to Revise the 2001 Guidelines for the Management of Patients With Atrial Fibrillation): developed in collaboration with the European Heart Rhythm Association and the Heart Rhythm Society. Circulation. 2006;114:e257–e354. doi: 10.1161/CIRCULATIONAHA.106.177292. [DOI] [PubMed] [Google Scholar]
- 19.Cuzick J. A Wilcoxon-type test for trend. Stat Med. 1985;4:87–90. doi: 10.1002/sim.4780040112. [DOI] [PubMed] [Google Scholar]
- 20.Lip GY, Nieuwlaat R, Pisters R, Lane DA, Crijns HJ. Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: the euro heart survey on atrial fibrillation. Chest. 2010;137:263–272. doi: 10.1378/chest.09-1584. [DOI] [PubMed] [Google Scholar]
- 21.Comparison of 12 risk stratification schemes to predict stroke in patients with nonvalvular atrial fibrillation. Stroke. 2008;39:1901–1910. doi: 10.1161/STROKEAHA.107.501825. [DOI] [PubMed] [Google Scholar]
- 22.Shih JY, Tsai WC, Huang YY, Liu YW, Lin CC, Huang YS, Tsai LM, Lin LJ. Association of decreased left atrial strain and strain rate with stroke in chronic atrial fibrillation. J Am Soc Echocardiogr. 2011;24:513–519. doi: 10.1016/j.echo.2011.01.016. [DOI] [PubMed] [Google Scholar]
- 23.Park JH, Joung B, Son NH, Shim JM, Lee MH, Hwang C, Pak HN. The electroanatomical remodelling of the left atrium is related to CHADS2/CHA2DS2VASc score and events of stroke in patients with atrial fibrillation. Europace. 2011;13:1541–1549. doi: 10.1093/europace/eur135. [DOI] [PubMed] [Google Scholar]
- 24.Blume GG, McLeod CJ, Barnes ME, Seward JB, Pellikka PA, Bastiansen PM, Tsang TS. Left atrial function: physiology, assessment, and clinical implications. Eur J Echocardiogr. 2011;12:421–430. doi: 10.1093/ejechocard/jeq175. [DOI] [PubMed] [Google Scholar]
- 25.Marchese P, Bursi F, Delle Donne G, Malavasi V, Casali E, Barbieri A, Melandri F, Modena MG. Indexed left atrial volume predicts the recurrence of non-valvular atrial fibrillation after successful cardioversion. Eur J Echocardiogr. 2011;12:214–221. doi: 10.1093/ejechocard/jeq176. [DOI] [PubMed] [Google Scholar]
- 26.den Uijl DW, Delgado V, Bertini M, Tops LF, Trines SA, van de Veire NR, Zeppenfeld K, Schalij MJ, Bax JJ. Impact of left atrial fibrosis and left atrial size on the outcome of catheter ablation for atrial fibrillation. Heart. 2011;97:1847–1851. doi: 10.1136/hrt.2010.215335. [DOI] [PubMed] [Google Scholar]
- 27.Matsuo S, Lellouche N, Wright M, Bevilacqua M, Knecht S, Nault I, Lim KT, Arantes L, O'Neill MD, Platonov PG, Carlson J, Sacher F, Hocini M, Jais P, Haissaguerre M. Clinical predictors of termination and clinical outcome of catheter ablation for persistent atrial fibrillation. J Am Coll Cardiol. 2009;54:788–795. doi: 10.1016/j.jacc.2009.01.081. [DOI] [PubMed] [Google Scholar]
- 28.Schneider C, Malisius R, Krause K, Lampe F, Bahlmann E, Boczor S, Antz M, Ernst S, Kuck KH. Strain rate imaging for functional quantification of the left atrium: atrial deformation predicts the maintenance of sinus rhythm after catheter ablation of atrial fibrillation. Eur Heart J. 2008;29:1397–1409. doi: 10.1093/eurheartj/ehn168. [DOI] [PubMed] [Google Scholar]
- 29.Risk factors for stroke and efficacy of antithrombotic therapy in atrial fibrillation. Analysis of pooled data from five randomized controlled trials. Arch Intern Med. 1994;154:1449–1457. doi: 10.1001/archinte.1994.00420130036007. [DOI] [PubMed] [Google Scholar]
- 30.Flaker G, Ezekowitz M, Yusuf S, Wallentin L, Noack H, Brueckmann M, Reilly P, Hohnloser SH, Connolly S. Efficacy and safety of dabigatran compared to warfarin in patients with paroxysmal, persistent, and permanent atrial fibrillation: results from the RE-LY (Randomized Evaluation of Long-Term Anticoagulation Therapy) study. J Am Coll Cardiol. 2012;59:854–855. doi: 10.1016/j.jacc.2011.10.896. [DOI] [PubMed] [Google Scholar]
- 31.Banerjee A, Taillandier S, Olesen JB, Lane DA, Lallemand B, Lip GY, Fauchier L. Pattern of atrial fibrillation and risk of outcomes: The Loire Valley Atrial Fibrillation Project. Int J Cardiol. 2013;167:2682–2687. doi: 10.1016/j.ijcard.2012.06.118. [DOI] [PubMed] [Google Scholar]
- 32.Hohnloser SH, Pajitnev D, Pogue J, Healey JS, Pfeffer MA, Yusuf S, Connolly SJ. Incidence of stroke in paroxysmal versus sustained atrial fibrillation in patients taking oral anticoagulation or combined antiplatelet therapy: an ACTIVE W Substudy. J Am Coll Cardiol. 2007;50:2156–2161. doi: 10.1016/j.jacc.2007.07.076. [DOI] [PubMed] [Google Scholar]
- 33.Hart RG, Pearce LA, Rothbart RM, McAnulty JH, Asinger RW, Halperin JL. Stroke with intermittent atrial fibrillation: incidence and predictors during aspirin therapy. Stroke Prevention in Atrial Fibrillation Investigators. J Am Coll Cardiol. 2000;35:183–187. doi: 10.1016/S0735-1097(99)00489-1. [DOI] [PubMed] [Google Scholar]
- 34.The Boston Area Anticoagulation Trial for Atrial Fibrillation Investigators. The effect of low-dose warfarin on the risk of stroke in patients with nonrheumatic atrial fibrillation. N Engl J Med. 1990;323:1505–1511. doi: 10.1056/NEJM199011293232201. [DOI] [PubMed] [Google Scholar]
- 35.Manning WJ, Leeman DE, Gotch PJ, Come PC. Pulsed Doppler evaluation of atrial mechanical function after electrical cardioversion of atrial fibrillation. J Am Coll Cardiol. 1989;13:617–623. doi: 10.1016/0735-1097(89)90602-5. [DOI] [PubMed] [Google Scholar]
- 36.Henein M, Zhao Y, Henein MY, Lindqvist P. Disturbed left atrial mechanical function in paroxysmal atrial fibrillation: a speckle tracking study. Int J Cardiol. 2012;155:437–441. doi: 10.1016/j.ijcard.2011.10.007. [DOI] [PubMed] [Google Scholar]
- 37.Watson T, Shantsila E, Lip GY. Mechanisms of thrombogenesis in atrial fibrillation: Virchow's triad revisited. Lancet. 2009;373:155–166. doi: 10.1016/S0140-6736(09)60040-4. [DOI] [PubMed] [Google Scholar]
- 38.Boyd AC, McKay T, Nasibi S, Richards DA, Thomas L. Left ventricular mass predicts left atrial appendage thrombus in persistent atrial fibrillation. Eur Heart J Cardiovasc Imaging. 2013;14:269–275. doi: 10.1093/ehjci/jes153. [DOI] [PubMed] [Google Scholar]
- 39.Benjamin EJ, D'Agostino RB, Belanger AJ, Wolf PA, Levy D. Left atrial size and the risk of stroke and death. The Framingham Heart Study. Circulation. 1995;92:835–841. doi: 10.1161/01.CIR.92.4.835. [DOI] [PubMed] [Google Scholar]
- 40.Chiang CE, Naditch-Brule L, Murin J, Goethals M, Inoue H, O'Neill J, Silva-Cardoso J, Zharinov O, Gamra H, Alam S, Ponikowski P, Lewalter T, Rosenqvist M, Steg PG. Distribution and risk profile of paroxysmal, persistent, and permanent atrial fibrillation in routine clinical practice: insight from the real-life global survey evaluating patients with atrial fibrillation international registry. Circ Arrhythm Electrophysiol. 2012;5:632–639. doi: 10.1161/CIRCEP.112.970749. [DOI] [PubMed] [Google Scholar]
- 41.Nieuwlaat R, Prins MH, Le Heuzey JY, Vardas PE, Aliot E, Santini M, Cobbe SM, Widdershoven JW, Baur LH, Levy S, Crijns HJ. Prognosis, disease progression, and treatment of atrial fibrillation patients during 1 year: follow-up of the Euro Heart Survey on atrial fibrillation. Eur Heart J. 2008;29:1181–1189. doi: 10.1093/eurheartj/ehn139. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.