Abstract
Focus group discussions were conducted to elicit the perceived incentives and barriers to exclusive breastfeeding in Ghana. Thirty-five breastfeeding women were recruited from the Manya and Yilo Krobo districts of the eastern region. Participants had a mean age of 27.5 years and had at least one child < 4 months old. Almost all of the participants believed that exclusive breastfeeding is the superior infant feeding method and should be practiced for the first 6 months postpartum. However, there was widespread belief that infants can be given water if it is clean. Mothers reported that exclusive breastfeeding was easier when breast milk began to flow soon after delivery. The main obstacles to exclusive breastfeeding identified were maternal employment, breast and nipple problems, perceived milk insufficiency, and pressure from family. Addressing the concerns put forward by these participants can be used to enhance exclusive breastfeeding promotion in this region.
Keywords: Africa, exclusive breastfeeding, Ghana, incentives, barriers, focus groups
The short- and long-term health benefits of exclusive breastfeeding (EBF) for both mothers and infants have been substantiated. The World Health Organization (WHO) recommends EBF for the first 6 months of life to achieve optimal health, growth, and development, even for HIV-positive mothers who have no other practical infant feeding option.1 EBF rates in Ghana are still far from optimum. The 2003 Ghana Demographic and Health Survey estimates that 39.2% of children 4 to 5 months old are exclusively breastfed.2 Several studies have been conducted to understand the physical, biological, psychological, social, and cultural factors explaining poor lactation and breastfeeding outcomes.3-7
Studies conducted in the northern regions of Ghana assessing programs developed to promote EBF have documented marked increases in EBF rates at 6 months.8 Another study in southern Ghana observed a 100% increased rate of EBF at 6 months for mothers receiving lactation counseling versus those who did not.9 Clearly, breastfeeding advocacy and support at the community level affect EBF rates, but there is still substantial room for improvement. Thus, it is essential to better understand the determinants of EBF behaviors in sub-Saharan Africa. This was a qualitative study carried out to explore Ghanaian women's knowledge and attitudes toward EBF.
Participants and Methods
Participants in this study were part of the ongoing Research to Improve Infant Nutrition and Growth (RIING) project aimed at improving child health and nutrition in HIV affected communities. The focus groups were carried out with women from the Manya and Yilo Krobo districts of the eastern region in Ghana. The main ethnic groups in these periurban communities, where farming constitutes the main economic activity, are the Krobo, Ewe, and Akan. Most infants are breast-fed from birth to 12 months and beyond. However, introduction of complementary foods starts early.10
The women were recruited from 3 antenatal clinics in the Manya Krobo district, which offered voluntary counseling and testing for HIV while pregnant, and they enrolled into the main RIING study upon delivery. We conducted 4 focus group discussions (FGDs) with a total of 7 to 10 women per group. The HIV status of our participants was 7 HIV positive, 12 HIV negative, and 16 women of unknown HIV status. The selection criterion was participants with an index child under 4 months old at the time of the study. This allowed for the inclusion of women who had recently received information on infant feeding and/or have had personal EBF experience. The sample was composed of mothers and infants with fairly homogeneous sociodemographic characteristics. The 4 FGDs were held every Monday in June 2006. Written informed consent was obtained from all participants of the RIING project, which was approved by the Institutional Review Boards of Iowa State University, the University of Connecticut, and the University of Ghana. In addition, the participants of the focus groups gave verbal consent.
Setting
The FGDs were held at the RIING project office, a private location at Kpong in the eastern region. Participants were provided transportation from their homes to the project office and back. This accessible and quiet location was an ideal setting for the FGD and was not linked to any organization or institution with which participants might have felt uncomfortable. During each FGD, the chairs were arranged in a circular pattern. In an adjacent room, several cots were prepared for the babies. Older children who attended the focus groups with their mothers were entertained with appropriate children's videos in an adjacent room. At the end of each meeting, the participants were given a small gift in appreciation for their time and contributions.
Focus Groups
The question guide items used in all FGDs were pretested by applying the questions to 10 breastfeeding women in the study area who were not part of the RIING project.11-13 In each FGD, 10 major areas were addressed to elicit discussions on EBF knowledge and sources of information, the participants' perceived benefits, incentives and barriers to EBF, and expected consequences of early EBF cessation. The questions were open-ended to encourage general discussion and to allow the moderator some flexibility to explore specific issues raised.12 The opening question for all the discussions was on general infant feeding information that the participants received while pregnant and after delivery and the source of that information. Questions on incentives and barriers were asked in reference to lactating mothers in their communities and not to themselves. This indirect approach was followed to prevent a “social desirability” bias.14
The focus groups were led by the study coordinator and a moderator who facilitated the discussion and was fluent in both Krobo and Akan. An assistant fluent in Ewe was also available to interpret as needed. This person, another assistant (in charge of audiotaping), and the study coordinator were present to take field notes and record nonverbal communications. The field notes were essential for identifying quotes and nonverbal communications.13 A third assistant was present to attend to the babies when they were not with their mothers (ie, sleeping in the prepared cots). Each FGD was audiotaped and lasted approximately 2 hours.
Analyses of Findings
The tape-recorded discussions were transcribed verbatim and translated into English. The transcripts were then coded using a codebook developed prior to the start of the focus groups. The results were analyzed using Microsoft Word and Excel. The analytical approach involved grouping together similar codes using different colors for the different FGDs for easy comparison of themes across groups. Similar concepts were then grouped together to form common themes, and each occurrence was labeled as it occurred, noting the context, regularity, specificity, and the abundance of responses. The frequencies of similar words or phrases were noted to assist with identifying important themes that helped in understanding the patterns in the data.13,15 A validity check for the data analysis was provided by a public health researcher and a nutritionist who independently read the transcripts.
Results
The ages of the 35 participants ranged from 19 to 49 years (average, 27.5 ± 6.5 years), and they had 7.2 ± 3.6 years of formal education. The participants had 2.4 ± 1.3 children. The average age of all children was 2.5 ± 0.8 months ranging in age from 1 to 6 months. Almost a quarter of the participants were primiparous (22.9%). The majority of them had a spouse or partner living with them (n = 30, 85%). All but 3 of the women were employed, with about half (n = 17) being traders. The majority of the participants were Krobo speaking (n = 22), but the sample also included 5 Ewe and 5 Akan speakers.
Major Themes
In all 4 FGDs, several similar themes and subthemes emerged. As reported below, the main areas of discussion were the type and source of infant feeding information; knowledge of EBF; reasons, motivations, and benefits of EBF; barriers to EBF; and the consequences of early EBF cessation.
Source and Type of Infant Feeding Information
Most of the infant feeding information was obtained from the hospital either at the antenatal or postnatal pediatric clinics where mothers were also given information on proper maternal care during pregnancy, particularly the prevention of malaria, preparations for childbirth, family planning and the importance of child spacing, and HIV/AIDS. In keeping with WHO recommendations, women were advised to EBF for the first 6 months, followed by continued breastfeeding up to 2 years with appropriate complementary feeding. The following response made by a participant illustrates the type of infant feeding information received prior to delivery:
I understand that truly if you do not give them water or food before 6 months, they are strong. If you give them food by this time, [this may damage] the “strings” [meaning veins] in the brain which is not yet strong. So giving food can affect the child’s brain. It won't develop well. But if you wait till 6 months, they become intelligent.
The nurses sometimes used appealing but often-times inaccurate statements to explain convincingly why water is not necessary and the importance of EBF for 6 months. This was evident in statements such as the following:
The reason is that one breast contains water and the other food. So if you give water, the right proportion of nutrient that the child should get will not be gotten.
Knowledge of Exclusive Breastfeeding
Almost all mothers from all the FGDs knew what EBF was. Even those who were not convinced about EBF defined it as giving only breast milk for 6 months, after which breast milk alone was no longer adequate. Some participants believed water was not recommended because it is not hygienic enough. One participant put it succinctly:
The water itself might not be clean and this can cause sicknesses. I think this is the reason why nurses say we shouldn't give water. But if you can make water neat and give, in my opinion, it's not wrong. Because ancient people gave their babies water and they lived. So why can't ours live now?
Predictors for Exclusive Breastfeeding
“Breast milk is best” was a major motivation for EBF that consistently arose across the FGDs. Participants agreed that breast milk provides all the required nutrients and water needed for proper child growth and development. Reasons given for choosing EBF were grouped into infant, maternal, and environmental factors.
Infant factors
Most mothers reported that they observed decreases in the incidence and duration of illnesses in their babies with EBF, and this motivates them to give only breast milk. Often the participants gave examples from experience.
The reason why I believe we shouldn't give water is that I gave my elder child water from birth and was often sick; when I gave birth to my second child, I didn't give water so child didn't get sick often. Not giving water protects them.
Most of the participants said that EBF made the children grow strong and intelligent. According to the participants, EBF encouraged proper development of the brain and bones and also led to appropriate infant weight gain. They also believed that EBF provides immunity against childhood diseases, decreasing their severity and frequency.
Almost all participants believed that breast milk alone is sufficient for the infants and that the babies are not mature enough to handle anything else. However, this sentiment was not shared by all the participants. One mother, who had started her child on infant formula at a month and half, claimed that breast milk was not sufficient. According to her, a sure sign that the baby is not getting enough is when the baby is restless and cries even after breastfeeding.
Maternal factors
In 3 FGDs, many of the participants agreed that breastfeeding allows more time for the mother to care for herself and the baby. EBF also made it easy to travel with the child, as mothers did not need to worry about what they were going to feed the infant while en route without spilling the food on the nearest passenger.
Another major motivation for EBF was that formula feeding was usually more expensive. Infant formula is not easily accessible in these areas, and preparing infant formula in feeding bottles correctly is both tedious and time-consuming.
One participant who was not in favor of EBF said on 2 occasions, there was infant formula available and pointed out that it was “just like breast milk.” Despite disagreement from the rest of the group, this mother remained unconvinced about EBF and stated,
This thing about giving only breast milk, if a child is a sickler [has sickle cell anemia], it's a sickler. Even if you breastfeed 20 times. You may not even give water but the child already is a sick-ler and will be sick anyway.
Another important EBF incentive was the early availability of breast milk following childbirth. When the milk comes in and the breasts are full, many of the participants agreed that breastfeeding relieves this uncomfortable fullness. On the other hand, when breast milk is not flowing and the baby is crying, the mothers are forced to give other foods. Almost all the participants agreed that adequate maternal nutrition is important for breast milk production. It was almost universally agreed that everything the mother eats goes into the breast milk. Therefore, they believed that nutritious meals eaten by the mother would increase milk output and the nutritional value or quality of her milk, thereby making it easy to exclusively breastfeed. In all FGDs, references were made to liquid food, such as soups, porridges, and teas, and consuming them as needed for increasing breast milk production. Not all the participants were in agreement. One participant said that some mothers may experience appetite loss following delivery and are still able to produce milk for the infant; therefore, not being able to eat or not eating well does not necessarily jeopardize breast milk production.
Many of the participants received information from family or had cultural beliefs about what foods help with breast milk production. Some mothers were told to avoid certain foods such as okra, plantain, and mangoes, which are believed to harm either the mother or baby.
Environmental factors
Some mothers believed that poor sanitation and hygiene practices, as well as inadequate preparation of the food and water, are reasons for the 6-month EBF recommendation.
If you observe a child sucking water from the bottles you see that the food in the child's mouth goes into the bottle and you give this to the child. So when water stands for a short time, it gets spoiled. Giving it to the child leads to diarrhea. In my opinion, we shouldn't give water for 6 months. Because the soldiers in the body that fight diseases are not grown in the babies so if any disease enters the body, the baby gets weak and may even die. We should wait till 6 months before giving food and water. Some mothers don't have time to take good care of the children. They may even have the baby's food unattended and flies may even fall into it. This makes the child sick. Not giving them food at this time helps because breast is in clothing and no houseflies can play around it to give child diseases.
Others believed that current use of fertilizers and chemicals in agriculture and in food processing were the reasons for the recommendation not to give water. Another mother articulated,
My grandmother told me that previously grown foods were more concentrated than what we have now due to fertilizer use. So there is no strength in it as previous foods. You can even tell the difference now with some recipe using current food crops and meat. Therefore, if now it is being advised that we give no water, I should believe.
Barriers to Exclusive Breastfeeding
Barriers to EBF were grouped into the following:
Maternal factors: employment, health (breast and nipple and general), and perceived insufficient milk
Infant factors: inability or refusal of the child to breastfeed
Social and cultural factors: refusal to breastfeed, reluctance to breastfeed in public, cultural practices and beliefs, the influence of family and friends, and support from the partners
Maternal factors
In all 4 FGDs, an important EBF barrier identified was breast and nipple problems. These included swollen and painful breasts, breast abscesses, and sore nipples. Some participants recognized that improper breastfeeding and latching techniques may lead to sore nipples. From 2 FGDs, there was an interesting belief that if a baby belches on the breast during breastfeeding, the mother can develop swollen breasts. According to the participants, this may be spiritual, making some women more prone than others. One participant did not agree, even though she was in the minority in that group, because the belching theory appeared to be a longstanding belief. She said,
My reason for disagreeing on that is that, we the mothers have sores within us after delivery. So maybe the sickness is already on its way. So when child belches on breast, then it's said to be the cause.
Maternal employment is another barrier to EBF. The general consensus was that working mothers would not have enough time to breastfeed their infants exclusively either because of the short maternity leave or the inability to find a convenient feeding location. This was especially the case for mothers who hawk their products or are busy trading in the market. The participants agreed that maternal hunger affects the ability of the mother to exclusively breastfeed her child. According to them, hunger makes the mothers so angry that they lose interest in breastfeeding. Unnecessary worrying was also reported to affect breast milk production.
The nurse said that breast milk flow is not only dependent on eating well. Breast milk originates from the brain. So when you are pregnant, so when you don’t worry the breast milk comes in plenty. But some people start to worry when they are pregnant and continue worrying after giving birth. She will eat all these foods and still not get enough breast milk.
Maternal sickness and death were cited as a barrier to exclusive breastfeeding. However, HIV as a barrier to breastfeeding was brought up in only 1 FGD.
Now, the coming of the disease called the HIV makes breastfeeding difficult. To prevent transmission to child, you will be asked not to breast-feed. The breast may be full and painful but you can't breastfeed. It's difficult, even if the baby is crying, you can't give breast milk because the nurses advise that you shouldn't.
Infant factors
From our discussions, any infant sickness that prevents suckling impairs mothers’ ability to breastfeed exclusively. According to 1 participant, some infants may have weak jaws, impairing their ability to suckle, which in turn leads to infant crying and prompts the mother to give other foods. Sick babies lose interest in breastfeeding and may become irritated when the mother attempts to breastfeed. The mothers are then forced to try other foods to prevent the child from losing weight or getting worse. In some cases, the child simply refuses to latch onto the breast, forcing the mother to introduce other foods.
Social and cultural factors
In all 4 FGDs, it emerged that unwanted body changes was another reason why some mothers might refuse to breastfeed their babies at all. One mother said,
I know a mother who is neither sick nor has any excuse. She said that if she breastfed her breasts will sag and become big so she won't breastfeed. She wants her breasts to stay as firm as they were so she won't breastfeed.
Another barrier to EBF reported at all 4 focus groups was that the mother is uncomfortable breast-feeding in public.
Some mothers too don't want to breastfeed in cars, even when baby is crying. They don't want people to see their breasts.
Some mothers may receive pressure from family and friends. The most influential person identified was the grandmother. According to some of our participants, mixed feeding appeared to be the norm among the older generation, and they prefer the younger generations to adopt the same feeding options for their grandchildren. This is made worse when the grandmothers are present when the baby is crying as they infer that breast milk is inadequate. One participant said that some mothers become confused with the conflicting messages they received from family and friends and resort to adding water. However, this participant acknowledged that a determined mother could still refuse to give water and continue with EBF.
In the third FGD, it emerged that lack of support from the babies’ fathers could hinder EBF. One participant gave the example of a mother abandoning her baby at the father's house because he refused to support her. When this happens, such a child is given other foods. It was also revealed that some fathers prefer to spend money on the babies rather than on the mothers, preferring instead to buy infant formula for the child.
Consequence of Early Cessation of Exclusive Breastfeeding
According to all FGDs, the consequences of ending EBF to the child were severe to dire. These range from child sicknesses and general ill health to poor growth and death. The participants agreed that the introduction of other foods can result in the child having kwashiorkor. Although the focus of our study was early infant feeding, some participants also spoke about what to give the child after 6 months. All participants agreed that children after 6 months should be given a variety of foods such as corn porridge fortified with egg yolk, fish powder, groundnut paste, and soy bean. There were also suggestions of mixing cereals and beans to make more nutritious porridges. In 1 FGD, the participants noted that at 6 months, some exclusively breastfed infants refuse all foods and would only begin to eat when the mother stops breastfeeding completely. The general consensus was that lack of variety, poor quality, and taste of the complementary foods may be responsible.
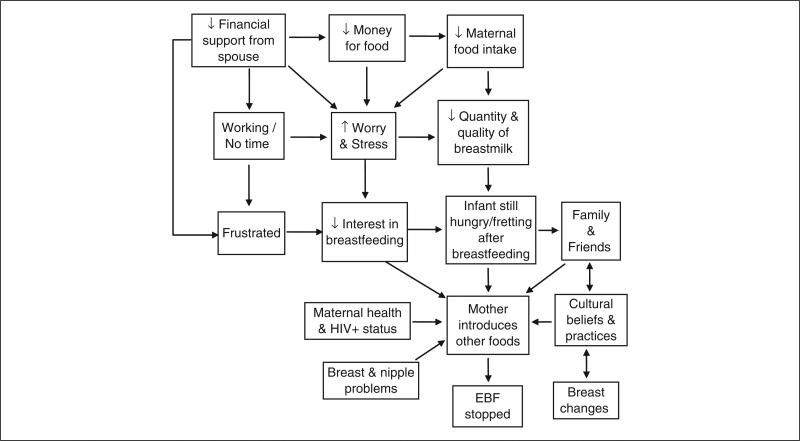
The results from all 4 FGDs were integrated to develop a conceptual framework depicting the factors influencing EBF as perceived by the study participants (Figure 1).
Figure 1.
Schematic representation of the participants’ concept of the factors influencing exclusive breastfeeding. The figure shows the factors that the mothers from the eastern region of Ghana perceived as influencing exclusive breastfeeding (EBF) in their communities. This is an integration of results from all 4 focus groups.
Discussion
The findings of this study indicate significant barriers to and motivations for EBF, many of which have been previously identified.3-5,16,17 Our study is the first in sub-Saharan Africa to integrate the findings into a “participant” conceptual framework. The views and suggestions of our participants can be used to formulate an EBF strategy to address local needs. Our findings show that incentives to EBF include the perception of stronger and healthier children, the early availability of breast milk (ie, onset of lactation), access of mother to nutritious foods, and perception of this infant feeding method as relatively inexpensive and less time-consuming. By contrast, barriers to EBF include perceived breast milk insufficiency, breast and nipple problems, infant's inability to suckle, maternal employment, maternal and infant health, lack of support from spouse, reluctance to breastfeed in public, and opposition from family and friends.
Mothers who participated in our study could define the term EBF correctly. In all FGDs, the main motive for EBF was the belief that breast milk is best for the infant, providing all the required nutrients and water. This is in agreement with what other studies in Africa have found.18,19
Perceived insufficient breast milk, which the participants identified as infant crying after breastfeeding or the child not being able to sleep through the night, implies that the mother cannot satisfy the child and thus needs to supplement breast milk with other foods. Similar findings have been previously reported in Mexico.17,20 Consistent with these studies, participants believed that a mother not eating enough can cause insufficient milk and that improving maternal nutrition through intake of nutritious and/or liquid foods can prevent this problem. Certain foods and fluids are considered to increase milk production and should be consumed by the lactating mother, whereas others, such as okra and mangoes, depending on the ethnic group the mother belongs to, are forbidden. A similar finding was reported in Nigeria,6 where lactating women were banned from eating plantains and bananas. It was believed that sweet things eaten by the mother get into the breast milk, causing diarrhea in the breastfeeding infant, and okra would make the baby drool excessively.
All FGDs identified breast and nipple conditions such as breast pain and discomfort, breast abscesses, and sore nipples as barriers to EBF. Poor latching and improper positioning of the baby was correctly identified by some of the participants as the cause of sore nipples, which can further discourage the mothers from EBF. Most of these problems are preventable and need appropriate assistance, starting during the pregnancy period and beyond.16
Our findings make it clear that women who attend antenatal and postnatal clinics receive their infant feeding knowledge from the hospital. At the hospitals, they are given information on EBF and when to start complementary feeding. It is therefore important for pregnant women and mothers to receive consistent information on infant feeding through the health care system.
Family and friends seem to play an important role in the early infant feeding choices of women. Our findings indicate that mothers are most influenced by their babies’ grandmothers. Probably not exposed to EBF themselves, the grandmothers may believe that breast milk alone is not satisfying the baby. In addition, grandmothers would like to stick with the traditional infant feeding methods. For some mothers, this makes it difficult to leave the child with his or her parents, fearing that in their absence, the child may be given water or other foods.
Although there is no known association between the intake of fluids and increased breast milk volume,21 almost all our focus group participants concurred that the intake of fluid foods such as soups, porridges, and teas increases breast milk production. This is information that they have received from the nurses at the health centers as well as their parents. Several statements were also based on their personal experience as well.
In a culture where breastfeeding is the norm and where it is socially acceptable for women to breastfeed in public, it was a surprise to find that one of the barriers to EBF identified in all of the FGDs was the reluctance to breastfeed or expose the breast in public and that breastfeeding can produce undesirable body changes, such as sagging breasts. Our participants reported these as barriers that they believed other mothers in their communities would experience, and this may have been missed if the questions were not asked indirectly.14 These barriers may also reflect the increased influence of urbanization in health behaviors, including breastfeeding in sub-Saharan Africa.22 In our focus groups, most of the mothers (except those whose babies slept throughout the session) at some point during our discussions breastfed their babies.
Maternal HIV was mentioned as an EBF barrier in only one of the focus groups. Considering that these mothers at some point in their pregnancy have been offered voluntary counseling and testing for HIV (this being a requirement for inclusion into the RIING project), we were expecting more discussion on this subject. On the other hand, the lack of discussion on this subject was not surprising considering the fact that HIV/AIDS is still highly stigmatized in these communities.
Kwashiorkor was identified as a possible consequence of ending EBF earlier than recommended. Citing this may be indicative that the usual foods traditionally used to supplement breast milk may be deficient in protein and energy. In fact, the commonest food given to infants is koko, which is a thin, fermented corn-based porridge.
This study was conducted in a periurban community, and thus results might vary from those of mothers in rural and urban communities. Our results, however, are likely to apply to Ghanaian women who receive their infant feeding knowledge from health centers. Asking our participants the questions in reference to other women in their communities enhanced the possibility of uncovering a wider range of experiences and perception on the research topic.14
In summary, the focus group methodology was especially suited to our study because our findings provided insight on the benefits, incentives, and barriers to EBF faced by women in the study community. Indeed, we were able to achieve data saturation with the 4 focus groups. Our study found that all mothers attending ante-natal care clinics receive and are aware of the benefits of EBF, but their ability to abide by it depends on family and outside influences, as well as their physical, emotional, and financial status. These findings have important implications for EBF promotion efforts in Ghana.
Acknowledgments
This project was funded by the RIING Project through NIH/NICHD grant HD43620. The authors acknowledge the participation of all mothers in this study. They are grateful to Deda Ogum, Mary Ohipeni, Richlove Ocansey, and Emelia Asamoah for the assistance with the focus group discussions.
Contributor Information
Gloria E. Otoo, recent graduate of the Department of Nutritional Sciences at the University of Connecticut, Storrs..
Anna A. Lartey, associate professor and head of the Department of Nutrition and Food Science at the University of Ghana, Legon..
Rafael Pérez-Escamilla, professor of Nutritional Sciences & Public Health at the University of Connecticut, Storrs, and the director of the National Institutes of Health (NIH) EXPORT Center for Eliminating Health Disparities among Latinos (CEHDL)..
References
- 1.WHO HIV Infant Feeding Technical Consultation Held on Behalf of the Inter-Agency Task Team (IATT) on Prevention of HIV Infection in Pregnant Women, Mothers, and Their Infants. World Health Organization; Geneva, Switzerland: 2006. Consensus statement. [Google Scholar]
- 2.Demographic and Health Survey (DHS) [February 9, 2007]; http://www.measuredhs.com/.
- 3.Sibeko L, Dhansay MA, Charlton KE, Johns T, Gray-Donald K. Beliefs, attitudes, and practices of breastfeeding mothers from a peri-urban community in South Africa. J Hum Lact. 2005;21:31–38. doi: 10.1177/0890334404272388. [DOI] [PubMed] [Google Scholar]
- 4.Kakute PN, Ngum J, Mitchell P, et al. Cultural barriers to exclusive breastfeeding by mothers in a rural area of Cameroon, Africa. J Midwifery Womens Health. 2005;50:324–328. doi: 10.1016/j.jmwh.2005.01.005. [DOI] [PubMed] [Google Scholar]
- 5.Cohen RJ, Brown KH, Rivera LL, Dewey KG. Promoting exclusive breastfeeding for 4-6 months in Honduras: attitudes of mothers and barriers to compliance. J Hum Lact. 1999;15:9–18. doi: 10.1177/089033449901500107. [DOI] [PubMed] [Google Scholar]
- 6.Davies-Adetugbo AA. Sociocultural factors and the promotion of exclusive breastfeeding in rural Yoruba communities of Osun State, Nigeria. Soc Sci Med. 1997;45:113–125. doi: 10.1016/s0277-9536(96)00320-6. [DOI] [PubMed] [Google Scholar]
- 7.Semega-Janneh IJ, Bohler E, Holm H, Matheson I, Holmboe-Ottesen G. Promoting breastfeeding in rural Gambia: combining traditional and modern knowledge. Health Policy Plan. 2001;16:199–205. doi: 10.1093/heapol/16.2.199. [DOI] [PubMed] [Google Scholar]
- 8.Quinn VJ, Guyon AB, Schubert JW, Stone-Jimenez M, Hainsworth MD, Martin LH. Improving breastfeeding practices on a broad scale at the community level: success stories from Africa and Latin America. J Hum Lact. 2005;21:345–354. doi: 10.1177/0890334405278383. [DOI] [PubMed] [Google Scholar]
- 9.Aidam BA, Perez-Escamilla R, Lartey A. Lactation counseling increases exclusive breast-feeding rates in Ghana. J Nutr. 2005;135:1691–1695. doi: 10.1093/jn/135.7.1691. [DOI] [PubMed] [Google Scholar]
- 10.Nti CA, Lartey A. Young child feeding practices and child nutritional status in rural Ghana. Int J Consumer Stud. 2007;31:326–332. [Google Scholar]
- 11.Krueger KA. Focus Group Kit. Vol. 3. Sage; Thousand Oaks, CA: 1998. Developing Questions for Focus Groups. [Google Scholar]
- 12.Krueger KA. Moderating Focus Groups. Vol. 4. Sage; Thousand Oaks, CA: 1998. Focus Group Kit. [Google Scholar]
- 13.de Negri B, Thomas E. Making Sense of Focus Group Findings: A Systematic Participatory Analysis Approach. Academy for Educational Development; Washington, DC: 2003. [Google Scholar]
- 14.McLennan JD. Early termination of breast-feeding in periurban Santo Domingo, Dominican Republic: mothers’ community perceptions and personal practices. Rev Panam Salud Publica. 2001;9:362–367. doi: 10.1590/s1020-49892001000600002. [DOI] [PubMed] [Google Scholar]
- 15.Krueger KA. Focus Group Kit. Vol. 6. Sage; Thousand Oaks, CA: 1998. Analyzing & Reporting Focus Group Results. [Google Scholar]
- 16.Giugliani ER. Common problems during lactation and their management. J Pediatr (Rio J) 2004;80(suppl):S147–S154. doi: 10.2223/1248. [DOI] [PubMed] [Google Scholar]
- 17.Sacco LM, Caulfield LE, Gittelsohn J, Martinez H. The conceptualization of perceived insufficient milk among Mexican mothers. J Hum Lact. 2006;22:277–286. doi: 10.1177/0890334406287817. [DOI] [PubMed] [Google Scholar]
- 18.Orne-Gliemann J, Mukotekwa T, Miller A, et al. Community-based assessment of infant feeding practices within a programme for prevention of mother-to-child HIV transmission in rural Zimbabwe. Public Health Nutr. 2006;9:563–569. doi: 10.1079/phn2005881. [DOI] [PubMed] [Google Scholar]
- 19.Manuela de Paoli M, Manongi R, Klepp KI. Are infant feeding options that are recommended for mothers with HIV acceptable, feasible, affordable, sustainable and safe? Pregnant women's perspectives. Public Health Nutr. 2004;7:611–619. doi: 10.1079/phn2003596. [DOI] [PubMed] [Google Scholar]
- 20.Segura-Millan S, Dewey KG, Perez-Escamilla R. Factors associated with perceived insufficient milk in a low-income urban population in Mexico. J Nutr. 1994;124:202–212. doi: 10.1093/jn/124.2.202. [DOI] [PubMed] [Google Scholar]
- 21.Lawrence RA, Lawrence RM. Breastfeeding: A Guide for the Medical Profession. 6th ed. Elsevier Mosby; Philadelphia: 2005. [Google Scholar]
- 22.Perez-Escamilla R. Breastfeeding in Africa and the Latin American and Caribbean region: the potential role of urbanization. J Trop Pediatr. 1994;40:137–143. doi: 10.1093/tropej/40.3.137. [DOI] [PubMed] [Google Scholar]