The renin–angiotensin system (RAS) has an important role in the regulation of blood pressure, electrolytes and fluid in the body.1 Accumulating evidence suggests that overactivation of the RAS causes hypertension and other related diseases, such as stroke, heart failure and renal failure.1,2 Therefore, RAS inhibition is one of the critical therapeutical targets in the hypertension field. Currently, the central targets of RAS inhibition in hypertension therapy are angiotensin II (Ang II) and its receptor (AT1) because the main effects of the RAS are largely mediated by these two components. Renin, the rate-limiting enzyme in Ang II production, and aldosterone, a downstream factor of Ang II, are also important therapeutical targets for RAS inhibition in hypertension therapy. In addition, angio-tensinogen (AGT) is the sole substrate of RAS and is also an important factor for RAS regulation. In fact, there is clear evidence from basic and clinical studies that supports the relationships between AGT and hypertension.1,3–8 For example, higher plasma AGT concentrations were correlated with higher blood pressure in humans.7 Also, decreased AGT levels using AGT antibodies or AGT-knockout mice caused a decrease in blood pressure.3,6 AGT infusion or AGT overexpression induced an increase in blood pressure in animals.4,5 Moreover, the AGT gene copy number and blood pressure level were positively correlated in gene-targeted mice.8 As described above, decreased production of AGT appears to be a useful target for novel antihypertensive drugs. However, it would likely be very difficult to develop a drug that suppresses AGT production in humans by conventional methods. Olearczyk et al. have studied the ability of siRNA and lipid nanoparticle (LNP) technologies to inhibit AGT production in the liver, which is the main production site of circulating AGT in the body. Published in this issue of Hypertension Research, their work investigates the effects of LNP-encapsulated AGT siRNA on liver AGT mRNA expression, circulating AGT levels and blood pressure levels in spontaneously hypertensive rats (SHR) and normotensive rats.9
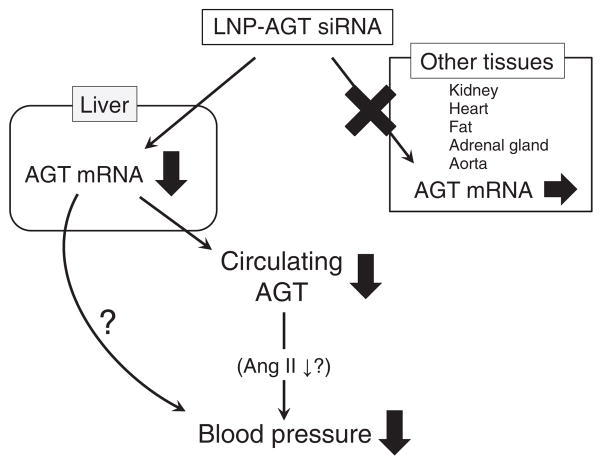
Olearczyk et al.9 used siRNA to reduce AGT production in the liver. For the delivery of AGT siRNA to the liver, the authors used chemically modified LNP. This LNP delivered AGT siRNA into the liver, which induced the reduction of liver AGT mRNA expression by RNA interference. LNPs containing AGT siRNA did not affect AGT mRNA expression in other tissues, such as the heart, kidney, fat, adrenal glands or aorta (Figure 1). In addition, the liver-specific decrease in AGT mRNA resulted in decreased plasma AGT and blood pressure levels in both SHR and normotensive rats. The reduction in plasma AGT levels may have been able to suppress circulating Ang II and RAS activation because of the decreased precursor levels; however, the authors did not measure the plasma Ang II concentrations due to the detection limits of their assay system (Figure 1). These findings demonstrate that inhibition of liver AGT and the subsequent decrease in plasma AGT concentrations lead to a sufficient lowering of blood pressure (Figure 1). As suggested by previous studies, this study reinforces AGT as a useful target for hypertension therapy.3–8 The use of LNP-encapsulated AGT siRNA will likely become a valuable therapeutical tool for the reduction of circulating AGT in vivo.
Figure 1.
Lipid nanoparticle (LNP)-encapsulated angiotensinogen (AGT) siRNA reduced blood pressure by decreasing the liver AGT expression and circulating AGT levels in spontaneously hypertensive and normotensive rats. LNP-encapsulated AGT siRNA does not affect AGT mRNA expression in other tissues. Ang II, angiotensin II.
LNP-encapsulated AGT siRNA aims to reduce blood pressure by inhibiting liver AGT mRNA expression. This mechanism is a completely novel method for RAS inhibition when compared with current RAS inhibitors; thus, there may be combinational effects between LNPs that contain AGT siRNA and other RAS inhibitors or antihy-pertensive drugs, such as diuretics and calcium channel blockers. Olearczyk et al. report some combinational effects on lowering blood pressure between the LNP-encapsulated AGT siRNA and candesartan, an angio-tensin receptor blocker (ARB), in SHR. Further assessment of the combinational effects of LNP-encapsulated AGT siRNA and other antihypertensive drugs on efficacy, availability and safety are required in future studies. In addition, the long-term effects of this siRNA therapy on Ang II and/or aldos-terone production will be important with regard to Ang II/aldosterone breakthrough.10 A clinical study reported that some patients who received long-term treatment with an angiotensin-converting enzyme inhibitor (ACEi) and/or an ARB exhibited a restoration of plasma Ang II and/or aldosterone levels that had been decreased by RAS inhibitors; furthermore, these breakthroughs reduced the beneficial effects of RAS inhibitors.10 The precise mechanisms of these breakthroughs remain unclear; however, some possible pathways have been suggested. For example, ACE-independent Ang II production and AT2 receptor stimulation by Ang II, which are not blocked by ACEi and ARB, respectively, may be involved in the restoration of Ang II and aldosterone levels.11,12 It seems more likely that AGT siRNA decreases Ang II and/or aldosterone breakthrough better than an ACEi or ARB because the direct suppression of AGT, the precursor of Ang II, reduces Ang II production even for long-term treatments. In the study by Olearczyk et al., liver-specific AGT inhibition by LNP-encapsulated siRNA did not affect AGT production in other tissues, indicating that a restoration of plasma AGT levels by tissues other than the liver is not possible. Additional long-term studies and the evaluation of plasma Ang II and/or aldosterone levels are important issues that need to be addressed.
In the study by Olearczyk et al., chemically modified LNP-encapsulated AGT siRNA selectively inhibited AGT mRNA expression in the liver but not in other tissues, such as the heart or the kidney (Figure 1). These results are concerning because LNP-encapsulated AGT siRNA treatment may not suppress the local activation of the RAS, such as the intrarenal RAS.1 The local intrarenal RAS is independent from the circulating RAS, and intrarenal RAS activation is one of the critical triggers for kidney injury in various pathological conditions, such as hypertension, diabetes and obesity.1 An increase in renal AGT mRNA expression is one of the critical factors for intrarenal RAS activation and subsequent renal injury.1 Indeed, it was proven that renal AGT expression is enhanced in animal kidney injury models and kidney disease patients.1 Thus, there is a possibility that LNP-encapsulated AGT siRNA cannot sufficiently suppress local intrarenal RAS activation, although it effectively reduces blood pressure by inhibiting the circulating RAS. In addition, the local RAS is found in other tissues, such as the heart and the kidney. These findings indicate that LNP-encapsulated AGT siRNA may be less efficient in inhibiting local RAS activation and organ injuries such as kidney injury when compared with current RAS inhibitors. By contrast, if AGT siRNA encapsulated by other chemical chaperones can be effectively incorporated into the kidney, the siRNA could potentially suppress intrarenal RAS activation and subsequent renal injury better than current RAS inhibitors. Further investigation is required to evaluate the efficacy of LNP-encapsulated AGT siRNA on local RAS activation-induced organ damage.
Previous research has revealed the importance of blood pressure control and RAS inhibition for the prevention of multiple forms of hypertension-related organ damage, such as brain, cardiovascular and kidney injuries.1,2 The use of several RAS inhibitors, such as a direct renin inhibitor, ACEi, ARB and a mineralocorticoid receptor antagonist, was shown to successfully reduce blood pressure and cardiovascular event outcomes in clinical studies.2 It may appear that these various RAS inhibitors are a sufficient treatment option for hypertensive patients. However, it is impossible to cure all hypertensive patients using current antihypertensive drugs, and there are still some patients resistant to this form of medication. In addition, hypertensive patients are required to take antihypertensive drugs daily; therefore, improvements in compliance and medical costs can still be found. Further research into the development of novel RAS inhibitors is necessary and important for the next-generation of hypertension therapies that will improve on the drawbacks of current treatments. Olearczyk et al.9 reported that the novel therapeutical approach of using LNP-encapsulated AGT siRNA produced a significant and sustained reduction in blood pressure via inhibition of liver AGT production in hypertensive and normo-tensive rats. Specifically, the blood pressure-lowering effects of AGT siRNA were sustained for >1 week, indicating that this siRNA treatment does not need to be administered daily, which could improve the compliance and long-term blood pressure control of hypertensive patients. Taken together, the tissue-specific inhibition of AGT by siRNA is a novel and useful target for future hypertension therapies; however, further detailed studies, such as toxicity, side effects, reproducibility and efficacy in humans, are required.
Footnotes
CONFLICT OF INTEREST
The authors declare no conflict of interest.
References
- 1.Kobori H, Urushihara M. Augmented intrarenal and urinary angiotensinogen in hypertension and chronic kidney disease. Pflugers Arch. 2013;465:3–12. doi: 10.1007/s00424-012-1143-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.von Lueder TG, Krum H. RAAS inhibitors and cardiovascular protection in large scale trials. Cardiovasc Drugs Ther. 2013;27:171–179. doi: 10.1007/s10557-012-6424-y. [DOI] [PubMed] [Google Scholar]
- 3.Gardes J, Bouhnik J, Clauser E, Corvol P, Menard J. Role of angiotensinogen in blood pressure homeostasis. Hypertension. 1982;4:185–189. doi: 10.1161/01.hyp.4.2.185. [DOI] [PubMed] [Google Scholar]
- 4.Kimura S, Mullins JJ, Bunnemann B, Metzger R, Hilgenfeldt U, Zimmermann F, Jacob H, Fuxe K, Ganten D, Kaling M. High blood pressure in transgenic mice carrying the rat angiotensinogen gene. EMBO J. 1992;11:821–827. doi: 10.1002/j.1460-2075.1992.tb05119.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Menard J, el Amrani AI, Savoie F, Bouhnik J. Angio-tensinogen: an attractive and underrated participant in hypertension and inflammation. Hypertension. 1991;18 :705–707. doi: 10.1161/01.hyp.18.5.705. [DOI] [PubMed] [Google Scholar]
- 6.Tanimoto K, Sugiyama F, Goto Y, Ishida J, Takimoto E, Yagami K, Fukamizu A, Murakami K. Angiotensinogen-deficient mice with hypotension. J Biol Chem. 1994;269:31334–31337. [PubMed] [Google Scholar]
- 7.Walker WG, Whelton PK, Saito H, Russell RP, Hermann J. Relation between blood pressure and renin, renin substrate, angiotensin II, aldosterone and urinary sodium and potassium in 574 ambulatory subjects. Hypertension. 1979;1:287–291. doi: 10.1161/01.hyp.1.3.287. [DOI] [PubMed] [Google Scholar]
- 8.Kim HS, Krege JH, Kluckman KD, Hagaman JR, Hodgin JB, Best CF, Jennette JC, Coffman TM, Maeda N, Smithies O. Genetic control of blood pressure and the angiotensinogen locus. Proc Natl Acad Sci USA. 1995;92:2735–2739. doi: 10.1073/pnas.92.7.2735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Olearczyk J, Gao S, Eybye M, Yendluri S, Andrews L, Bartz S, Cully D, Tadin-Strapps M. Targeting of hepatic angiotensinogen using chemically modified siRNAs results in significant and sustained blood pressure lowering in a rat model of hypertension. Hypertens Res. doi: 10.1038/hr.2013.155. (e-pub ahead of print 12 December 2013) [DOI] [PubMed] [Google Scholar]
- 10.Bomback AS, Klemmer PJ. The incidence and implications of aldosterone breakthrough. Nat Clin Pract Nephrol. 2007;3:486–492. doi: 10.1038/ncpneph0575. [DOI] [PubMed] [Google Scholar]
- 11.Hollenberg NK. Pharmacologic interruption of the renin-angiotensin system and the kidney: differential responses to angiotensin-converting enzyme and renin inhibition. J Am Soc Nephrol. 1999;10(Suppl 11):S239–S242. [PubMed] [Google Scholar]
- 12.Naruse M, Tanabe A, Sato A, Takagi S, Tsuchiya K, Imaki T, Takano K. Aldosterone breakthrough during angiotensin II receptor antagonist therapy in stroke-prone spontaneously hypertensive rats. Hypertension. 2002;40:28–33. doi: 10.1161/01.hyp.0000022606.52221.2f. [DOI] [PubMed] [Google Scholar]