Abstract
Objective: Minimally invasive approaches to the hip are beneficial to the patient, but reduce the space available for manipulation by the surgeon. Determining the available working space is important for the development of surgical instruments, to track movements during surgery, as well as to classify the invasiveness of the procedure.
Approach: We evaluate three measurement methods to assess the volume of eight surgical sites in a cadaver study. The cavities were filled with an alginate cast to determine its dimensions. Second, the depth, height, and width of the surgical site were measured with a ruler and the volume was calculated. Last, the surface registration method was used to reconstruct the site.
Results: We found that the mold filling method provides accurate results in determining the volume of a surgical site. The manual method using a ruler showed excellent reliability, but the calculations tended to overestimate the volume of the surgical site. In contrast, surface reconstruction tended to underestimate the volume of a surgical site, but the results closer resembled the ones derived from the mold filling method.
Innovation: We presented a new method to assess the size of the surgical site intraoperatively in minimally invasive hip surgery.
Conclusion: The manual method is reliable, but not as accurate as the surface reconstruction, while the mold filling method cannot be used in an intraoperative setup. Although surface reconstruction showed deficits regarding reliability, due to the lack of direct contact to the patient, it remains an appealing technique to measure the surgical site.

David Putzer, PhD
Introduction
During the last 10 years, steady progress has been made in reducing soft tissue damage and skin incision in total hip arthroplasty.1 Patients who undergo a minimally invasive surgical (MIS) approach benefit from a faster recovery and shorter rehabilitation compared with patients operated on with more invasive procedures.2 Other benefits of MIS hip surgery are reduced operative blood loss, less muscle tissue damage, and less postoperative pain.1 Furthermore, the smaller wound size lowers the risk of microbial infection.
The MIS direct anterior approach to the hip is characterized by a significantly reduced working space for the surgeon. To account for the small operating space, special surgical instruments were developed for this procedure.3 With the advent of new surgical techniques in hip arthroplasty, such as robot-assisted surgery, it is important to characterize the available working space for the development of new surgical instruments and to characterize the possible movement of such in the surgical site. Knowing the exact spatial dimension of the operation site created for MIS would also help establish a classification of the impact of different minimally invasive procedures, adding valuable information to other aspects like blood loss, retraction of soft tissue, and muscular damage. An extended working space, like in revision surgeries, implies also a higher invasiveness as more hard or soft tissue structures are affected.
The precise measurement of the operation site proves to be difficult as the visualization of the specific region can be problematic. The accuracy of repeated measurements is challenging, as each measurement has to be performed with the patient in the exact same position.4 Typically, in minimally invasive hip surgery, only the incision length is reported, which solely provides information on skin trauma resulting from the performed surgery. The soft tissue trauma is more difficult to assess and currently, there is no defined measurement system to determine the damage to the muscular soft tissue. The correlation between working space and invasiveness of the procedure has yet to be demonstrated in clinical studies.
Unlike in the surgical field, several measurement devices exist to characterize the wound size in the field of wound care treatment. The most common methods, however, are limited to qualitative and subjective visual evaluation or manual measurement of the wound area in two dimensions.5–8 The outlines of wounds with complex shape have to be traced manually, which is time-consuming and of low accuracy.9,10
To gain in-depth information, the wound size can be easily estimated by simple measurements using a Kundin gauge, a system composed of three rulers aligned orthogonally to each other.7,11 Currently, several other wound measuring methods are described in the literature.12–16 Most of these methods are carried out manually and the measurement instruments come in direct contact with the patient. Contactless measurement devices, which identify the border of the wound automatically, have been developed recently.12,17
One promising technique currently used in nonorthopedic applications is the calculated reconstruction of the surface area of an intended surgical site (see Blais18 for an overview).
Currently, a new generation of time-of-flight (TOF) cameras, the Photonic Mixing Device (PMD), was developed. These devices have the advantage of combining fast imaging and high lateral resolution with in-depth information of the captured scene, yielding a fast and accurate three-dimensional (3D) measurement. The camera is based on an array or line sensor, which can measure the distance to the target for each pixel in parallel, therefore capturing a momentary 3D picture without scanning over the sensor field, which creates an image over time.19 This camera system is thus far typically used for real-time applications like gesture recognition20 or robotic navigation.21
Clinical Problem Addressed
Although many measurement systems exist for evaluating wound size in wound care treatment applications, there is currently no measurement system available on the market for recording the surgical site intraoperatively. PMD cameras are well suited to evaluate the dimensions of smaller surgical spaces such as those opened during MIS hip surgery. In this study, we directly compare the results of different measurement methods used to determine the volume of eight surgical siti of minimally invasive hip surgery on cadavers. We suggest the use of PMD cameras as a novel, fast, and noninvasive system to calculate 3D space models of a surgical site.
Materials and Methods
Five cadavers were used to compare the three methods to detect the opening area and the volume of the surgical site created during minimally invasive surgery. MIS hip surgery was performed on one or both sides of the cadaver. The surgeries were carried out by an experienced hip surgeon. A total of eight hip cavities were evaluated.
Mold filling method
The dental alginate impression material (Henry Schein, Inc., Melville, NY) was used as cast material in compliance with ISO 1563, BS 4269-Part2 to achieve an accurate measurement of the volume of the site.22 The powder was stirred before use and mixed with tap water for 30 s to form an elastic cast material that could be poured into the wound. The material was filled into the cadaver cavities and was left in place for more than 10 min to harden. The volume of the alginate cast was subsequently determined by measuring the amount of water it displaces in a graduated cylinder.22 To avoid errors created by drying out of the alginate and resulting uptake of water, the measurements were carried out immediately after the cast had been produced.
Kundins gauge
The second tested method, used primarily in wound care treatment, utilizes a set of three rulers at orthogonal angles to measure the length, width, and depth of the cavity.11 The depth was measured at the deepest point of the cavity, and the length and width were determined by considering the maximum extensions of the openings.
Using the measured depth d, the maximum width b, and the maximum length l, the volume of the surgical site was approximated to a semiellipsoid shape using the following equation:
 |
and approximated to a tetrahedron shape calculated as follows:
 |
Surface reconstruction
A third and newly tested method to measure the 3D dimension of a wound is the TOF-PMD camera (PMDSK2 V.2.2.1; PMD Technologies GmbH, Siegen, Germany), which consists of an optical transmitter and an optical receiver.19,23 The high acquisition rate (40 frames/sec) and the resolution of 200×200 pixels make this camera suitable for fast and accurate measurements that could be used for continuous intraoperative measurements. An algorithm was developed on MATLAB® (MATLAB R2011b, MathWorks®, Natick, MA) to calculate the area and volume using the PMD camera, to quantify the working space in minimally invasive hip arthroplasty. The PMD camera returns as output, distance, intensity, and an amplitude matrix together with a 3D point cloud, which can be used for surface reconstruction. By using the intensity and amplitude values and by applying various filters and image processing tools, a mask can be created, which is used to select the 3D points corresponding to the hip cavity. The volume of the corresponding space can be calculated from these points.
Image correction
The distance, intensity, and amplitude images, obtained with the TOF-PMD camera and imported to MATLAB with the application programming interface, were scaled to a grayscale image with an intensity range from 0 to 1. The grayscale images were adjusted to values resulting in 1% of data points saturated at low and high intensities of the images to enhance the contrast of the output image. The amplitude image given by a TOF camera has the drawback that, objects further away from the camera appear darker than those located near the camera. This is due to the fact that the power of a light wave decreases with the square of the distance it covers. To compensate for this, the amplitude data were corrected.24
Image filtering
The distance image can be used to remove the extraneous background that is not needed for recognizing the soft tissue envelope border. The background filter proposed in this study eliminates the values that are out of the range±80% of the calculated median of each frame. In this study, a median filter of kernel size 9×9 was used on the distance, amplitude, and intensity values for each frame.
Contour extraction
A Canny edge-detection filter was used to extract the contours of the soft tissue envelope to separate them from the background. Combining the contour of the corrected amplitude and intensity values, the recognition of the contours were further improved. This contour improvement for images obtained with TOF-PMD cameras was described by Danciu et al.25 In this study, a vicinity and operation was used, given by the following formula:
 |
where Ed(i, j) are the edges determined by the distance map and Ei(i, j) the edges determined by the intensity map. Nmax is the maximum number of possible contour points within the two vicinities. The term (i+k, j+l) represents the neighbors of the current pixel, found in its 5×5 vicinity.
The borders detected by the edge detection filter were enlarged and cleared from attaching pixels afterward. After this operation, the region for the surgical site was selected by the following criteria:
 |
where Aellipse was calculated by determining the minor and major axis length of the recognized regions. The sum of the filled pixels of the mask is A. To eliminate areas that were either too small or too large, another selection criterion was introduced:
 |
where A is again the sum of all filled pixels in the single recognized regions. This selected region was used as a binary mask to select the corresponding 3D values of the point cloud image that correspond to the surgical site.
Volume calculation
Images were taken from different viewing angles by moving the TOF-PMD camera. To compensate for the variability of the results and increase the performance of the algorithm, a temporal filter was introduced. The temporal filter calculated the average of two images registered in two or more successive time steps. The position and camera rotation were corrected by calculating the rototranslation of the mask and applying it to the values of the 3D point cloud. After selecting the 3D points of the surgical site by the mask operation, the area and volume were calculated by using the Delaunay Triangulation. Therefore, the algorithm recognized the border of the soft tissue envelope. The delineation of this envelope was recognized automatically, and no manual corrections were necessary.
Statistical analysis
To compare the volume calculations for the three different methods, 10 measurements were performed for each method by three different observers. The mold filling method provided the ground truth measurement. The intraclass correlation (ICC) and interitem correlation (IIC) between raters were calculated. An ICC>0.75 was considered an excellent reliability for the measurements. The data were analyzed with Excel® 2007 (Microsoft® Office, Redmond, WA; SP2). Analysis of variances (ANOVA) for repeated measurements was used with the Bonferroni correction to pairwise comparison. Correlation was calculated at a two-tailed significance level of 0.05. All statistical calculations were performed using SPSS® (IBM®, Armonk, NY; version 20.0).
Results
Results showed that in comparison to the mold filling method, the manual ruler measurement followed by calculations using a semiellipsoid approximation or a tetrahedron approximation tends to overestimate the volume, while the calculations based on measurements carried out with the TOF camera tend to underestimate the volume (Table 1). Pairwise comparison of the three methods using the ANOVA showed a statistically significant difference between the measurement methods (p<0.001). Variability of the results was highest for the TOF method, while the observed variability was <12.7% for the manual measurements (Table 1). A statistically significant correlation between manual measurements and the measurements carried out with the TOF camera was found in four out of eight cadavers (Table 1).
Table 1.
Volumes of eight different surgical siti were determined with three different methods creating four different calculations
| Operation Site | Mold Filling [cm3] | Tetrahedron Approximation [cm3] | Semiellipsoid Approximation [cm3] | TOF [cm3] | Correlation Between Manual Measurement and TOF (p-Value) |
|---|---|---|---|---|---|
| 1 | 100 | 163±11 (6.5%) | 171±11 (6.5%) | 125±6 (5.2%) | r=0.020 (0.917) |
| 2 | 110 | 198±16 (8.3%) | 207±17 (8.3%) | 104±7 (7.0%) | r=−0.512 (0.004) |
| 3 | 150 | 136±13 (9.2%) | 143±13 (9.2%) | 73±9 (12.5%) | r=−0.006 (0.976) |
| 4 | 150 | 215±16 (7.3%) | 225±16 (7.3%) | 67±10 (14.4%) | r=−0.280 (0.134) |
| 5 | 173 | 496±63 (12.7%) | 519±66 (12.7%) | 164±28 (17.3%) | r=− 0.399 (0.029) |
| 6 | 180 | 212±7 (3.4%) | 222±8 (3.4%) | 135±36 (26.7%) | r=0.439 (0.015) |
| 7 | 200 | 226±10 (4.4%) | 236±10 (4.4%) | 118±35 (29.6%) | r=−0.459 (0.011) |
| 8 | 220 | 341±13 (3.9%) | 357±14 (3.9%) | 186±36 (19.5%) | r=−0.144 (0.448) |
Mean and standard deviation of all measurements, as well as data variability (in brackets) are shown for each method and each site.
TOF, time-of-flight.
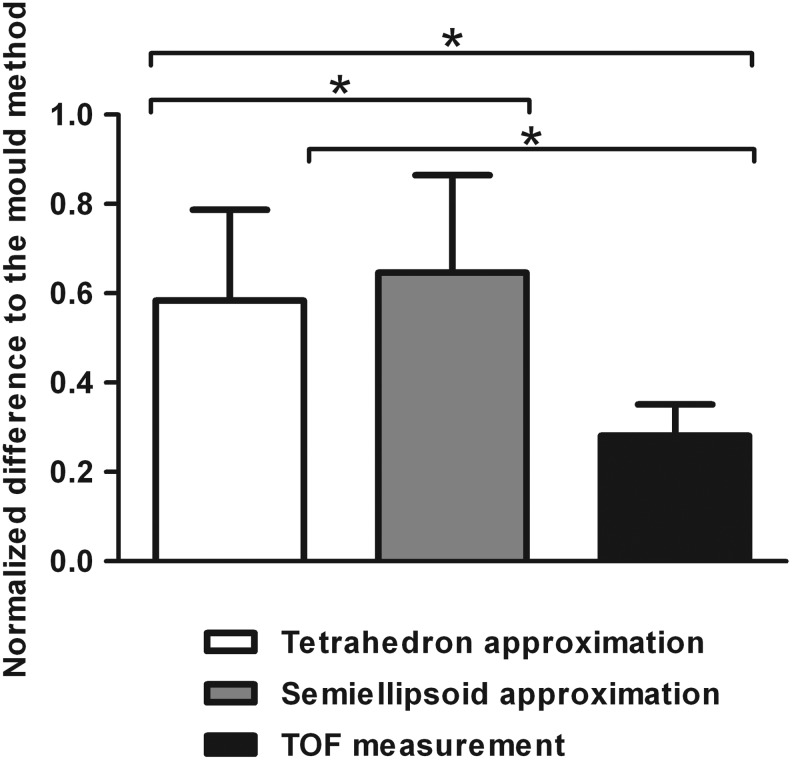
Comparing the normalized difference of each method to the mold method (as standard), it can be deduced that the TOF measurement method is approximating the volume determined by the mold method closer than the method using ruler measurements followed by shape approximating calculations (Fig. 1). Also, the standard deviation of the normalized differences between the TOF measurement and mold method is lower compared with the other two methods. Comparing the results derived from the ruler measurement method, the volume calculations using the tetrahedron approximation closer resembled the values derived from the mold measurement method compared with the calculations using the semiellipsoid approximation (Fig. 1).
Figure 1.
Normalized differences of the values derived from ruler measurement followed by tetrahedron approximation, semiellipsoid approximation, and the calculations from time-of-flight (TOF) camera measurements to the mold method with the corresponding standard deviation. *Indicates a p-value<0.001 using analysis of variances pairwise comparison of the three methods.
Both approximations obtained with the manual measurement method showed good reliability for the thirty repetitive measurements using both single and average measurements when assessing the volume of the eight operation siti. The TOF measurement had a good ICC only for the average of the repeated measurements, while single measurement ICC was <0.75 (Table 2).
Table 2.
Intraclass correlation coefficient for the different measurement methods
| Measurement Method | Single Measurement ICC | Average Measurement ICC |
|---|---|---|
| Tetrahedron approximation | 0.929 | 0.975 |
| Semiellipsoid approximation | 0.929 | 0.975 |
| TOF measurement | 0.650 | 0.848 |
ICC, intraclass correlation; IIC, interitem correlation.
The IIC coefficient was >0.962 for the two calculation methods using the manual measurement data, which indicates that the different observers achieve reliable results when assessing the volume of the surgical site. The TOF measurement achieved an IIC below 0.75, which means that a smaller degree of agreement among observers was obtained (Table 3).
Table 3.
Interitem correlation coefficient for the different measurement methods
| Interitem Correlation | Tetrahedron Approximation | Semiellipsoid Approximation | TOF Measurement |
|---|---|---|---|
| Observer 1–Observer 2 | 0.995 | 0.995 | 0.704 |
| Observer 1–Observer 3 | 0.962 | 0.962 | 0.625 |
| Observer 2–Observer 3 | 0.973 | 0.973 | 0.674 |
Discussion
Different measurement methods were evaluated in a cadaver study to assess the available working volume in minimally invasive hip arthroplasty.
The mold filling method is the most accurate in determining the volume of a surgical site. Thus, the measurements obtained with this method were used as a reference value for the other methods that estimate the real size of the operation site by different calculations. Although the mold filling method provides reliable data on the volume of a surgical site, it is rarely used in an intraoperative setting as it introduces the risk of infection, irritation, or allergic reactions.16 In this study, the mold filling method provided a ground truth measurement for comparison.
The manual method, where length, width, and depth are determined using a ruler, is an inexpensive and simple method, which is reported with good inter-rater and intrarater reliability in the literature.26 In our study, where the wound volume was approximated to a tetrahedron and a semielipsoid shape, the ICC and IIC showed excellent reliability. Variability of the measurements was lower than that from TOF camera images. Still, results showed an overestimation of the actual size of the volume using both shape approximations. Similar results can also be found in literature, where reports show that manual measurements tend to overestimate the wound size.27 Although having a better reliability and a reduced variability of the measurements, both approximations showed values that would stray further from the ground truth than the TOF measurements. Average variability of the manual measurement was around 7% and comparable to the findings in a study by Treuillet et al.16
TOF measurements underestimated the volume of the operation site. Volume calculation depends mostly on the viewing angle to the surgical site as maximum depth changes with it. In each measurement, an average of 250 pictures from different viewing angles was used to calculate the volume of the surgical site. A better way would be to reconstruct a map out of the 250 pictures, which would result in a longer calculation time, but should also lead to a more accurate measurement. As a further drawback, areas that are not in the direct line of sight of the TOF camera were not considered in the volume calculation. Minimally invasive hip surgery is characterized by a deep and narrow surgical site, where sight is impaired partially by the skin incision. An underestimation of the wound size resulting from TOF camera images is an intrinsic problem that cannot be compensated for completely.
A significant correlation between the manual method and the surface reconstruction method was found in four out of eight cadavers. The accuracy of both measurement methods is probably too low to be correlated to each other. Average variability of the TOF measurement was approximately twice as high (16%) as the average variability of manual measurement (7%). The TOF measurement method has several limitations, which could influence the high variability of the results. A limitation was the low resolution of the used TOF-PMD camera. The volume of the operation site could be calculated more precisely from images providing a higher image resolution. This can be addressed by using the TOF-PMD camera in combination with a common digital camera, where image resolutions are much higher.28 Automatic recognition of the envelope of the surgical site will also need to be improved to reduce variability. In measurement systems found in literature, the delineation had to be corrected manually in some cases.12 Part of the variability of the results could be influenced by the operator of the camera, as the IIC coefficient was lower than the one for the manual method. The use of a support, where the camera is mounted and which allows different viewing angles for registration, is recommended. The ICC coefficient was also lower than the manual measurements, which indicates that the results are less reproducible. The challenge of measuring the volume of the operation site intraoperatively was simplified by approximating the incision area to a semiellipsoid shape. In the surgical situation, retractors would be introduced, and the shape of the surgical site would vary from the approximated semiellipsoid shape to an extent that would depend on the number of retractors inserted into the hip cavity.
Limitations of the study were the limited number of cadavers available and that only three observers were involved in the study. The inter-rater reliability of the measurement may change with more investigators. In the mold filling method, repeated measurements were not carried out as the use of this method intraoperatively is questionable and we do not expect large variations throughout the measurements. Reliability of the measurements carried out with the TOF camera may be influenced more by the recognition algorithm than the observers. Increasing the recognition rate of the surgical site may improve significantly its performance in calculating the available working space.
Currently, no such intraoperative measurement system is available on the market, which could be used to estimate the extensions of the working space during surgery continuously. Using a TOF camera has a great benefit in comparison to the other two methods investigated in this study, as it is contactless and can continuously record the surgical site. Manual measurement is easy to carry out, but it is limited to single measurements during surgery. The mold filling method is not suitable for an intraoperative setting as it introduces the risk of infection, irritation, or allergic reactions. In conclusion, the manual method is a reliable and reproducible measurement method, even though it tends to overestimate the volume of a surgical site. Measurements carried out with the TOF camera tend to underestimate the volume of a surgical site. Still, the values obtained from calculations of TOF image data closer resemble the actual wound size determined by the mold filling method.
Key Findings.
Measurement system to determine the size of the surgical site in minimally hip arthroplasty which
• can be used intraoperatively and without contact to the patient
• calculates the volume in real time
• allows to classify soft tissue damage
Innovation
The measurements using the TOF camera can be carried out fully automatically and without contacting the patient. The algorithm used in this study can still be adjusted, further improving data precision. The TOF camera allows the collection of a vast amount of data about the visible zone in a surgical site in real time. These data can be stored digitally and organized with patient data. We therefore recommend the use of the here described method of calculating wound size from TOF camera data in minimally invasive hip arthroplasty.
Abbreviations and Acronyms
- 3D
three dimensional
- ANOVA
analysis of variances
- ICC
intraclass correlation
- IIC
interitem correlation
- MIS
minimally invasive surgery
- PMD
photonic mixing device
- TOF
time-of-flight
Acknowledgments and Funding Sources
We thank Mag.rer.nat. Dennis Huber, scientific collaborator, and Christian Keller and Sebi Kellner, medical students. This study was carried out with internal funds from Experimental Orthopedics, Innsbruck Medical University.
Author Disclosures and Ghostwriting
D.P., S.K., M.H., and M.N. are paid employees of Innsbruck Medical University. M.N. is a paid consultant of Stryker IMT; D.P. is principal investigator of Stryker IMT. No competing financial interests exist. The content of this article was expressly written by the authors listed. No ghostwriters were used to write this article.
About the Authors
David Putzer received his PhD degree in musculoskeletal sciences from the Innsbruck Medical University in 2013. Currently he is working as a postdoctoral research fellow at the Unit of Experimental Orthopedics, which is part of the Department of Orthopedics at the Medical University Innsbruck, Austria. Matthias Haselbacher graduated as MD at the Innsbruck Medical University in 2012 and is currently working at the Department of Trauma Surgery of the Innsbruck Medical University. Sebastian Klug received his PhD in Computer Science from the Technische Universität Darmstadt in 2009. He is working as a postdoctoral research fellow at the Unit of Experimental Orthopaedics at the Medical University Innsbruck, Austria. Michael Nogler was habilitated in 2001 and was promoted to Full Professor of Experimental Orthopaedics in 2009. Currently he is vice chairman of the department of Orthopaedics and head of the unit of Experimental Orthopaedics at the Medical University Innsbruck, Austria.
References
- 1.Nogler M, Mayr E, and Krismer M: [The direct anterior approach to the hip revision]. Oper Orthop Traumatol 2012; 24: 153. [DOI] [PubMed] [Google Scholar]
- 2.Berger RA, Jacobs JJ, Meneghini RM, Della Valle C, Paprosky W, and Rosenberg AG: Rapid rehabilitation and recovery with minimally invasive total hip arthroplasty. Clin Orthop Relat Res 2004; 429: 239. [DOI] [PubMed] [Google Scholar]
- 3.Nogler M, Krismer M, Hozack WJ, Merritt P, Rachbauer F, and Mayr E: A double offset broach handle for preparation of the femoral cavity in minimally invasive direct anterior total hip arthroplasty. J Arthroplasty 2006; 21: 1206. [DOI] [PubMed] [Google Scholar]
- 4.Melhuish J, Plassman P, and Harding K: Circumference, area and volume of the healing wound. J Wound Care 1994; 3: 380. [DOI] [PubMed] [Google Scholar]
- 5.Goldman RJ. and Salcido R: More than one way to measure a wound: an overview of tools and techniques. Adv Skin Wound Care 2002; 15: 236. [DOI] [PubMed] [Google Scholar]
- 6.Griffin JW, Tolley EA, Tooms RE, Reyes RA, and Clifft JK: A comparison of photographic and transparency-based methods for measuring wound surface area. Phys Ther 1993; 73: 117. [DOI] [PubMed] [Google Scholar]
- 7.Langemo D, Anderson J, Hanson D, Hunter S, and Thompson P: Measuring wound length, width, and area: which technique? Adv Skin Wound Care 21: 42–45; quiz 45–47, 2008 [DOI] [PubMed] [Google Scholar]
- 8.Plassmann P, Melhuish JM, and Harding KG: Methods of measuring wound size: a comparative study. Ostomy Wound Manage 1994; 40: 50–52, 54, 56–60 [PubMed] [Google Scholar]
- 9.Bohannon RW. and Pfaller BA: Documentation of wound surface area from tracings of wound perimeters. Clinical report on three techniques. Phys Ther 1983; 63: 1622. [DOI] [PubMed] [Google Scholar]
- 10.Bolton L: Re: Measuring wound length, width, and area: which technique? Adv Skin Wound Care 21: 450; author reply 450–452, 2008 [DOI] [PubMed] [Google Scholar]
- 11.Kundin JI: A new way to size up a wound. Am J Nurs 1989; 89: 206. [PubMed] [Google Scholar]
- 12.Duckworth M, Patel N, Joshi A, and Lankton S: A clinically affordable non-contact wound measurement device. Presented at RESNA Annual Meeting, Phoenix, AZ, 2007 [Google Scholar]
- 13.Liu X, Kim W, Schmidt R, Drerup B, and Song J: Wound measurement by curvature maps: a feasibility study. Physiol Meas 2006; 27: 1107. [DOI] [PubMed] [Google Scholar]
- 14.Patete PV, Bulgrin JP, Shabani MM, and Smith DJ: A non-invasive, three-dimensional, diagnostic laser imaging system for accurate wound analysis. Physiol Meas 1996; 17: 71. [DOI] [PubMed] [Google Scholar]
- 15.Plassmann P. and Jones TD: MAVIS: a non-invasive instrument to measure area and volume of wounds. Measurement of area and volume instrument system. Med Eng Phys 1998; 20: 332. [DOI] [PubMed] [Google Scholar]
- 16.Treuillet S, Albouy B, and Lucas Y: Three-dimensional assessment of skin wounds using a standard digital camera. IEEE Trans Med Imaging 2009; 28: 752. [DOI] [PubMed] [Google Scholar]
- 17.Sprigle S, Nemeth M, and Gajjala A: Iterative design and testing of a hand-held, non-contact wound measurement device. J Tissue Viability 2012; 21: 17. [DOI] [PubMed] [Google Scholar]
- 18.Blais F: Review of 20 years of range sensor development. J Electron Imaging 2004; 13: 231 [Google Scholar]
- 19.Ringbeck T, Möller T, and Hagebeuker B: Multidimensional measurement by using 3-D PMD sensors. Adv Radio Sci 2007; 5: 135 [Google Scholar]
- 20.Kollorz E, Penne J, Hornegger J, and Barke A: Gesture recognition with a time-of-flight camera. Int J Intelligent Syst Technol Appl 2008; 5: 334 [Google Scholar]
- 21.Prusak A, Melnychuk O, Roth H, Schiller I, and Koch R: Pose estimation and map building with a time-of-flight-camera for robot navigation. Int J Intelligent Syst Technol Appl 2008; 5: 355 [Google Scholar]
- 22.Covington JS, Griffin JW, Mendius RK, Tooms RE, and Clifft JK: Measurement of pressure ulcer volume using dental impression materials: suggestion from the field. Phys Ther 1989; 69: 690. [DOI] [PubMed] [Google Scholar]
- 23.Stefan Fuchs SM: Calibration and registration for precise surface reconstruction with TOF cameras. Int J Intelligent Syst Technol Appl 2008; 5: 274 [Google Scholar]
- 24.Oprisescu S, Falie D, Ciuc M, and Buzuloiu V: Measurements with ToE cameras and their necessary corrections. In: Proceedings of International Symposium on Signals, Circuits and Systems2007; 1: 1 [Google Scholar]
- 25.Danciu G, Ivanovici M, and Buzuloiu V: Improved contours for ToF cameras based on vicinity logic operations. In: 12th International Conference on Optimization of Electrical and Electronic Equipment2010; 989 [Google Scholar]
- 26.Langemo DK, Melland H, Olson B, et al.: Comparison of 2 wound volume measurement methods. Adv Skin Wound Care 2001; 14: 190. [DOI] [PubMed] [Google Scholar]
- 27.Thawer HA, Houghton PE, Woodbury MG, Keast D, and Campbell K: A comparison of computer-assisted and manual wound size measurement. Ostomy Wound Manage 2002; 48: 46. [PubMed] [Google Scholar]
- 28.Lindner M, Kolb A, and Hartmann K: Data-fusion of PMD-based distance-information and high-resolution RGB-images. In: International Symposium on Signals, Circuits and Systems,2007; 1: 1 [Google Scholar]